- 1Department of Health Education and Behavioral Sciences, Faculty of Public Health, Mahidol University, Bangkok, Thailand
- 2Department of Public Health, Sefako Makgatho Health Sciences University, Pretoria, South Africa
- 3Department of Psychology, University of the Free State, Bloemfontein, South Africa
- 4Department of Psychology, College of Medical and Health Sciences, Asia University, Taichung, Taiwan
Background: The study aimed to assess the prevalence and associated factors of cross-sectional and incident arthritis or rheumatism among a national community sample of middle-aged and older adults in Thailand.
Methods: We analyzed cross-sectional and longitudinal data from two consecutive waves (2015 and 2017) of the Health, Aging, and Retirement in Thailand (HART) study. Arthritis or rheumatism (SRA) was assessed by self-reported health care provider diagnosis.
Results: The cross-sectional (baseline) sample included 5,616 participants (≥45 years, median age 66 years, interquartile range 57 to 76 years) and the incident (follow-up) sample included 3,545 participants. The prevalence of SRA in the cross-sectional sample (baseline) was 4.0% and in the incident (follow-up) sample 5.3%. In the cross-sectional multivariable model, obesity class I (aOR: 1.78, 95% CI: 1.19 to 2.67), obesity class II (aOR: 1.82, 95% CI: 1.02 to 3.25), hypertension (aOR: 1.90, 95% CI: 1.35 to 2.66), brain disease and/or psychiatric problems (aOR: 4.79, 95% CI: 2.27 to 10.62), sleep problem (aOR: 1.45, 95% CI: 1.01 to 2.07) and prescription drug use (aOR: 1.63, 95% CI: 1.14 to 2.33) were positively associated, and not in the labor force (aOR: 0.53, 95% CI: 0.34 to 0.84), and employed (aOR: 0.63, 95% CI: 0.41 to 0.99) were negatively associated with SRA. In the incident multivariable model, obesity class I (aOR: 1.78, 95% CI: 1.17 to 3.61), obesity class II (aOR: 2.01, 95% CI: 1.12 to 3.61), poor mental health (aOR: 1.69, 95% CI: 1.19 to 2.41), and functional disability (aOR: 2.04, 95% CI: 1.01 to 4.13) were positively associated, and current alcohol use (aOR: 0.50, 95% CI: 0.25 to 0.99) was negatively associated with SRA.
Conclusion: The middle and older Thai adults had a low prevalence and incidence of SRA, and several physical and mental risk factors for cross-sectional and/or incident SRA were identified.
Introduction
A significant global burden of disability can be attributed to arthritis (1, 2). Worldwide, in the adult population, the prevalence of knee osteoarthritis was 3.8% (16.0% in persons ≥40 years), hip osteoarthritis 0.85% and rheumatoid arthritis was 0.24% (1–3). Among predominantly older adults in six low-and middle-income countries, the prevalence of self-reported arthritis (SRA) was 19.9% among women and 14.1% among men (4). Among older adults (≥50 years) in South Africa, 24.7% had SRA (5), in India (≥50 years) 14.7% (6), and in China (≥45 years) 31.4% had SRA (7). We were unable to identify national data on the prevalence, incidence, and correlates of SRA among the aging population in Thailand, which led to the study.
According to previous studies (7–22), factors associated with arthritis include sociodemographic factors, health risk behaviors, poor mental health, and chronic conditions. Sociodemographic factors associated with arthritis include older age (7–11), female sex (7–11), higher economic status (9) and lower education (10, 12). Specific health risk behaviors, such as smoking (13), low physical activity or sedentary behavior (12, 14–16), non-alcohol use (17) and obesity (5, 8, 14, 18) have shown to increase the risk of arthritis. Moreover, poor mental health (5, 19, 20), including sleep problems (19) and depressive symptoms (10, 18, 21), increased the odds of arthritis. Certain chronic conditions, such as hypertension (7, 10), cardiovascular disease (7, 22), kidney and chronic lung disease (7), and functional disability (10, 11, 19) were also found to be associated with arthritis. Factors associated with incident arthritis include increasing age (7, 23), female sex (7, 23), physical activity (7), physical inactivity (23) cardiovascular disease (7), obesity (24, 25), lower well-being (26), sleep problems (27) and depression (23, 28).
The study aimed to assess for the first time the prevalence, incidence, and factors associated with SRA among middle-aged and older adults in a national community-based sample in Thailand in 2015 and 2017.
Methods
Sample and procedure
We analyzed cross-sectional and longitudinal data from two consecutive waves in 2015 and 2017 of the Health, Aging, and Retirement in Thailand (HART) study. From the total population and household data from the Department of Provincial Administration (DOPA), Ministry of Interior, in Thailand, a three-stage stratified random sampling was used. In stage 1, in each of 6 regions (Bangkok & Vicinity, East, North, Northeast, and South) in Thailand, one small province (< 250,000 people ≥45 years) and one large province (>250,000 people ≥45 years) was selected, except for the East where only one province was selected. In stage 2, each province is classified into urban areas (number of blocks) and rural areas (number of villages). In stage 3, 5,600 households were selected from the sampled blocks and villages. In each household, one person (≥45 years) was randomly selected, which was the inclusion criterium. Proxy interviews were conducted for frail participants (29). The 2015 survey (from February to July) (N = 5,616), and the 2017 survey (from January to June 2017) included 3,708 members of the 2015 HART cohort (192 died during follow-up or 4.3% of the baseline respondents who were in the study area; 1,554 moved away from the study area; 270 declined participation and the response rate: 72.33% and the retention rate: 66.03%). Attrition analysis found that those who were not followed-up were more likely more educated, Buddhist and male, while there were no significant differences in terms of other sociodemographic and all health variables. Participants were interviewed at their homes by trained field workers after written informed consent was obtained. The study was approved by the “Ethics Committee in Human Research, National Institute of Development Administration – ECNIDA (ECNIDA 2020/00012).”
Measures
Arthritis or rheumatism was assessed with self-reported health care provider diagnosis. Self-report is a reliable method of identifying arthritis or rheumatism in large population-based surveys (7).
Other chronic conditions were evaluated by self-reported health care provider diagnosed conditions, including hypertension, diabetes, lung diseases, emphysema, cardiovascular diseases, heart disease, heart failure, kidney diseases, liver diseases, emotional/nervous or psychiatric disease, brain diseases and Alzheimer's disease.
Sociodemographic information included age, sex, educational level, religion, and annual income quartile (30).
Employment status. First, participants were asked if they had a job (working for an employed, self-employed, or working for family or relative's business) now (Yes/No). Participants who had no job currently were asked if they worked before but retired, worked before and intended to work in the future but were currently not looking for a job, or never had a job. Retired individuals were defined as having no job at the moment and not intending to work in the future, those without a job and intending to work in the future as unemployed, and those who never had a job as ‘not in the workforce' (31).
Tobacco smoking was sourced from the item, “Have you ever smoked cigarettes?” (response options: “1 = yes, and still smoke now, 2 = yes, but quit smoking, and 3 = never”).
Alcohol use was sourced from the item, “Have you ever drunk alcoholic beverages such as liquor, beer or wine?” (response options: 1 = yes, and still drinking now, 2 = yes, but do not drink now, and 3 = never).
Physical activity in the past week was classified as “none = inactivity, 1–149 min/week = low activity, and ≥150 min/week = high activity” (32).
Body Mass Index (BMI) was assessed by self-reported body weight and height, and classified into “underweight (< 18.5 kg/m2), normal weight (18.5–22.9 kg/m2), overweight (23–24.9 kg/m2), obesity class I (25–29.9 kg/m2), and obesity class II (30 kg/m2)” (33).
Prescription drug use was assessed with the question, “In the last 2 years, did you use any prescription drug?” (Yes/No).
Functional disability was defined as any of four activity of daily living (ADL) limitations (34), previously found a valid measure in older adults in Thailand (35) (Cronbach's α = 0.94 at wave 1).
Probable depression (≥10 scores) was assessed using the Center for Epidemiologic Studies Depression (CES-D-10) scale (36), previously found a valid measure in Thailand (37, 38).
Factors associated with incident arthritis include increasing age [7/23], female sex (7, 23), physical activity (7), physical inactivity (23) cardiovascular disease (7), obesity (24, 25), lower well-being (26), sleep problems (27) and depression (23, 28). The CES-D10 had a reliability coefficient of 0.78.
Mental health status was assessed with the question: “In general, how would you rate your mental health status?” Responses ranged from 0 = very poor to 100 excellent, and poor mental health was defined as 0 to < 80 and good mental health as 80–100.
Sleep problem was defined as almost always or often (vs. sometimes or very rarely or never) having trouble falling asleep/insomnia in the past week.
Data analysis
The proportion of older adults with cross-sectional and incident SRA are presented with frequencies and percent. Pearson Chi-square tests are used to compare characteristics among groups. The first logistic regression model estimated odds ratios (OR) and confidence intervals (CI) for cross-sectional SRA, and the second model compared baseline without SRA with incident SRA. Variables significant in univariable analysis were included in the multivariable models. p ≤ 0.05 was considered statistically significant. All statistical analyzes were performed with StataSE 15.0 (College Station, TX, USA).
Results
Sample characteristics
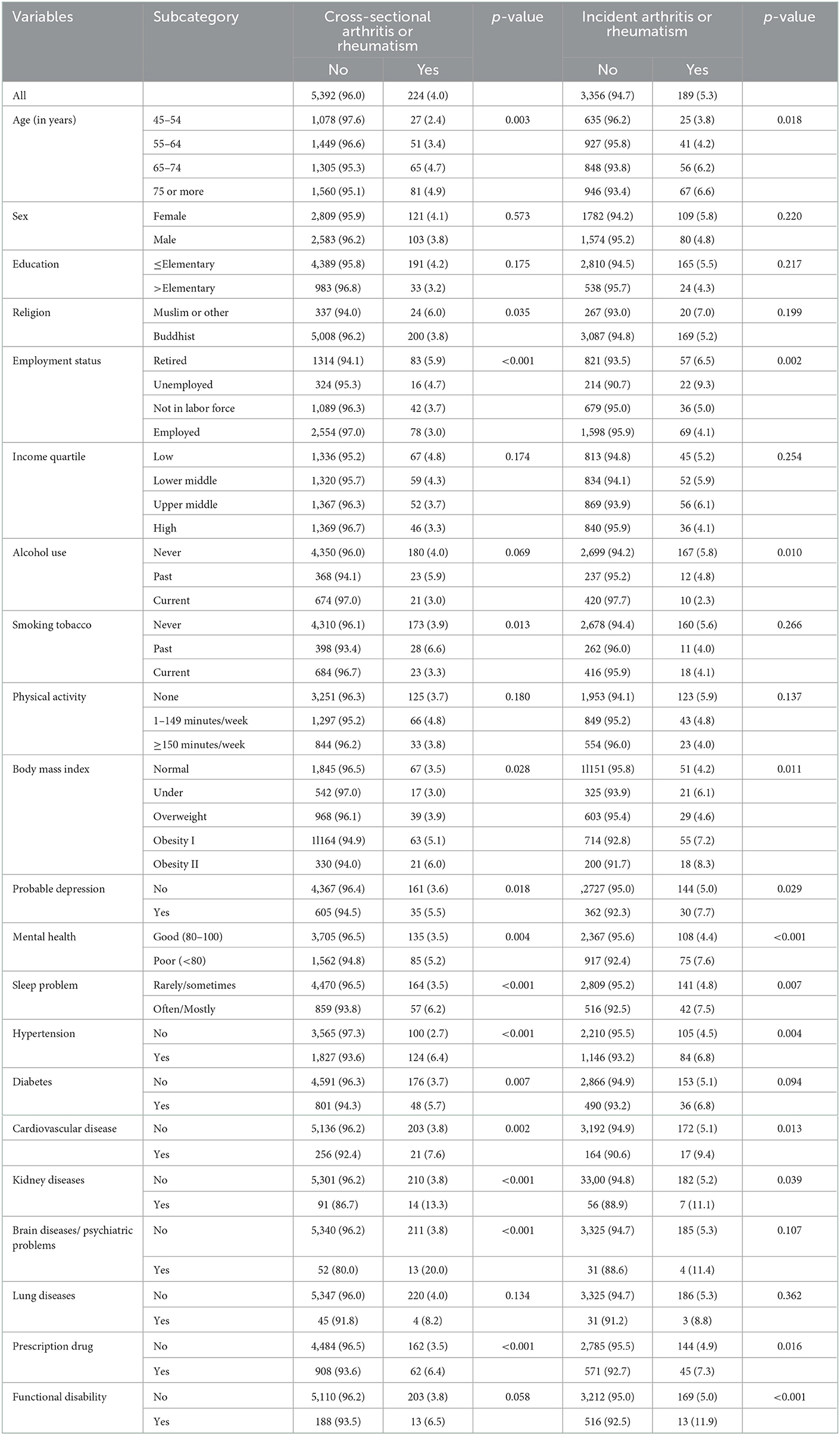
The cross-sectional (baseline) sample in 2015 included 5,616 participants (≥45 years, median age 66 years, interquartile range 57 to 76 years) and the incident (follow-up) sample in 2017 included 3,545 participants. The prevalence of SRA in the cross-sectional sample (baseline) was 4.0% and in the incident (follow-up) sample 5.3%. The binary analysis in the cross-sectional sample found that age, religion, employment status, smoking status, body mass index, probable depression, mental health, sleep problem, hypertension, diabetes, cardiovascular disease, kidney disease, brain disease or psychiatric problems, and prescription drug use differed significantly between people with SRA and without SRA. Binary analysis in the incident sample found that age, employment status, alcohol use, body mass index, probable depression, mental health status, sleep problem, hypertension, cardiovascular disease, kidney disease, prescription drug use and functional disability differed significantly between people with SRA and without SRA (see Table 1).
Cross-sectional associations with SRA
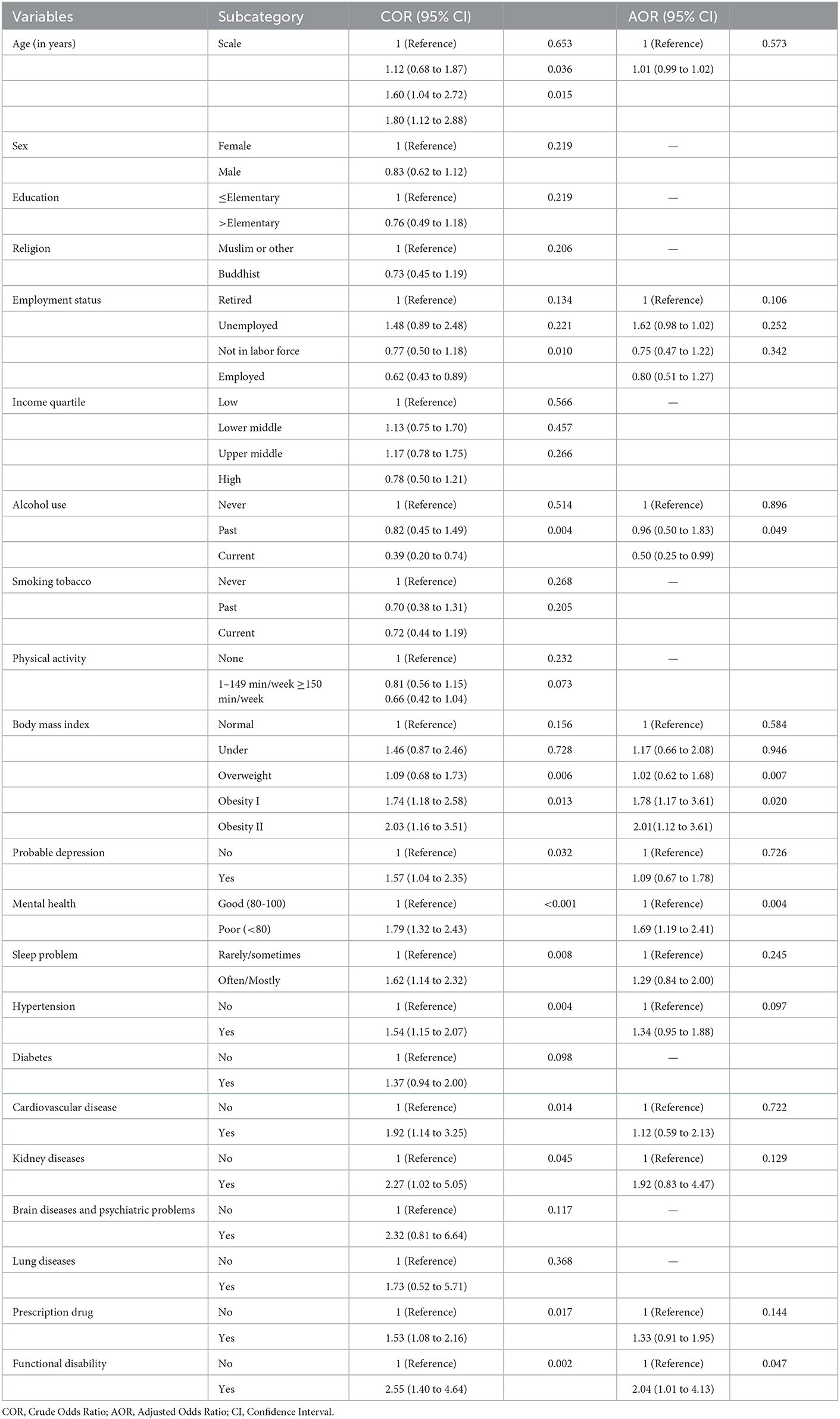
In the multivariable model, brain disease and/or psychiatric problems (aOR: 4.79, 95% CI: 2.27 to 10.62), hypertension (aOR: 1.90, 95% CI: 1.35 to 2.66), obesity class II (aOR: 1.82, 95% CI: 1.02 to 3.25), obesity class I (aOR: 1.78, 95% CI: 1.19 to 2.67), prescription drug use (aOR: 1.63, 95% CI: 1.14 to 2.33), and sleep problem (aOR: 1.45, 95% CI: 1.01 to 2.07) were positively associated, and not in the labor force (aOR: 0.53, 95% CI: 0.34 to 0.84), and employed (aOR: 0.63, 95% CI: 0.41 to 0.99) were negatively associated with SRA (see Table 2).
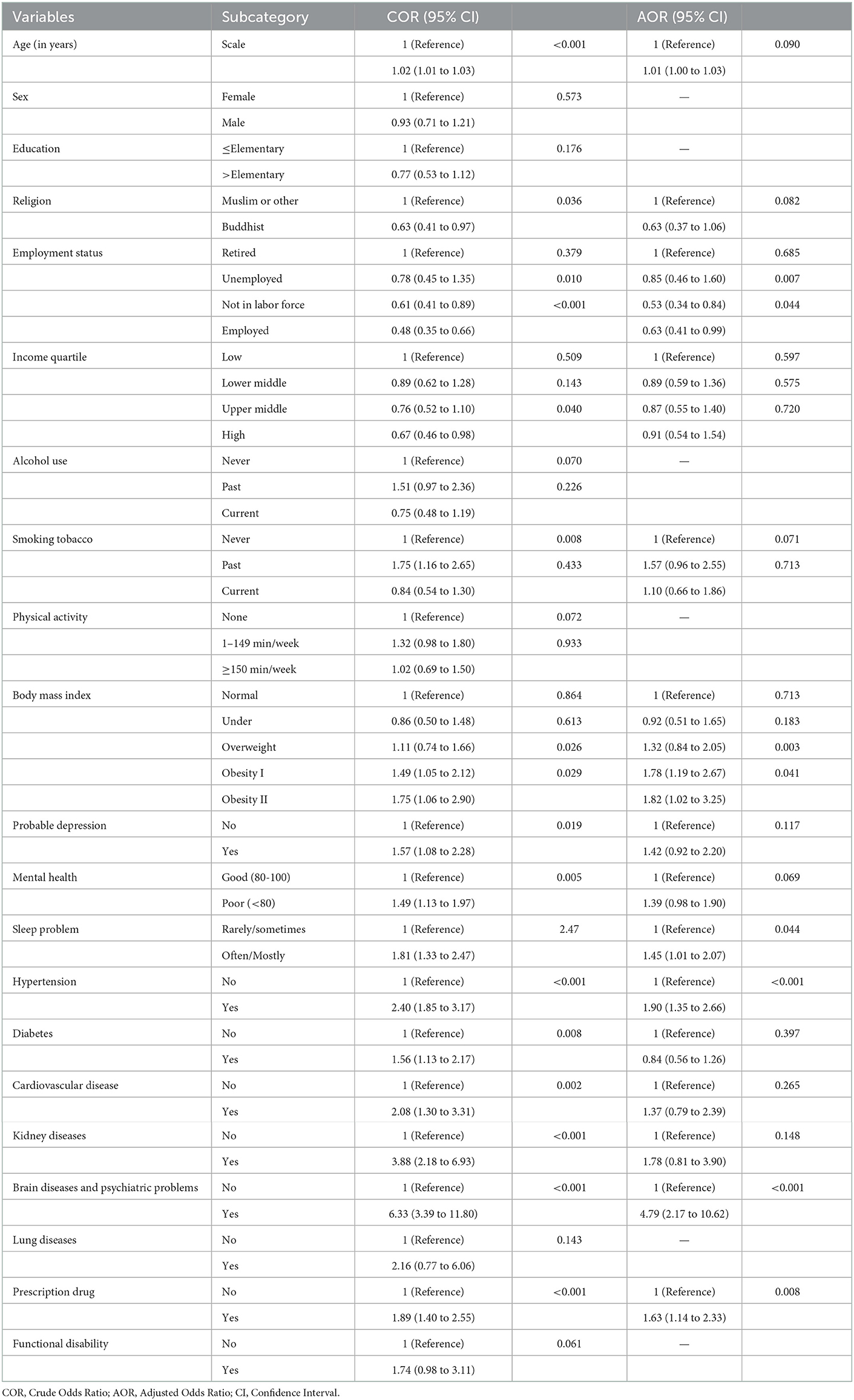
Table 2. Cross-sectional associations with arthritis, Health, Aging, and Retirement in Thailand (HART).
Associations with incident SRA
In the multivariable model, functional disability (aOR: 2.04, 95% CI: 1.01 to 4.13), obesity class II (aOR: 2.01, 95% CI: 1.12 to 3.61), obesity class I (aOR: 1.78, 95% CI: 1.17 to 3.61), and poor mental health (aOR: 1.69, 95% CI: 1.19 to 2.41), were positively associated, and current alcohol use (aOR: 0.50, 95% CI: 0.25 to 0.99) was negatively associated with SRA (see Table 3).
Discussion
The study found that the cross-sectional prevalence of SRA (4.0%) was lower than in previous studies among middle-aged and older adults in India (14.7%) (6), in six lower resourced countries (19.9% among women and 14.1% among men) (4), in China (31.4%) (7), in South Africa (24.7%) (5), and in Mexico (18). The lower prevalence of SRA in Thailand may be attributed to a lower rate of some risk factors, such as obesity, compared to other middle-income countries (7). Some other explanation for these country differences could be differences in the measurement of SRA, however, in all the studies cited here in India (6), China (7), Mexico (18), South Africa (5), and the six-country study (4) used exactly the same SRA, as in this study. However, the relatively low rate of SRA in Thailand appears to be confirmed in a community study in rural Thailand (≥15 years) with a prevalence of 11.3% osteoarthritis (based on radiographic and serological examinations) (39), and the global observation age-standardized incidence rates were the lowest in Southeast Asia (6.2), and the highest in high-income North America (22.5), South Asia (20.7), and Western Europe (20.4) (40).
We found that among women and those of older age, the prevalence of SRA was higher than among men and younger participants; however, this was not significant, unlike some previous research (7–11, 23). Some research studies found an association between lower education (10, 12) and SRA, but we did not find a significant association. The employment and higher economic status were in the unadjusted analysis protective against SRA, while in a study among older adults in Ghana the higher wealth status was associated with arthritis (9). In unadjusted analysis, being a Muslim or other increased the odds of SRA, which is contrary to a finding from a study in Thailand that found that the prevalence of radiographic knee osteoarthritis was significantly higher in Buddhists than in Muslims (41). The authors (41) attribute these differences to religious practices (“Muslims pray since childhood by forcing the knees into deep flexion, stretching the soft tissue surrounding the knee and decrease stiffness and contact pressure of the articular cartilage”).
In line with previous findings (5, 8, 14, 18, 24, 25), this study found a cross-sectional and incident association between obesity and SRA. Obesity may 'exhibit a chronic subclinical inflammatory state' increasing the risk of rheumatoid arthritis (42). Some studies found an association between physical inactivity and arthritis (12, 14, 15, 23, 43), while this study did not find this association. The non-significant association between physical inactivity and SRA in this study may be related to how physical activity was measured, it only included exercise and no other physical activity. In analyzing incident SRA, we found that current alcohol use was protective against arthritis, which is consistent with a review (17). The protective effect of alcohol use against arthritis may be explained “via attenuation of the innate inflammatory response” (17).
Furthermore, the study found associations between poor mental health (neurological or psychiatric problems, sleep symptoms, poor mental health and in unadjusted analysis probable depression) and SRA, which is consistent with previous results (5, 10, 18–21, 26–28). The association between sleep problems and arthritis may be related to pain at night (19). Prothero et al. (19) showed that “psychological interventions resulted in small to moderate improvement in biopsychosocial outcomes for patients with rheumatoid arthritis in addition to those achieved by standard care.” Furthermore, the relationship between poor mental health, such as depression, and SRA may also be bidirectional (44).
Consistent with some previous research (7, 10, 11, 19, 22), this study found a positive association between functional disability, hypertension, and in unadjusted analysis diabetes, cardiovascular disease, kidney disease and arthritis. It is possible that in these various physical conditions there is an underlying connection through pain and associated inflammatory dysfunction (10). Some determinants, such as sleep problems, or hypertension (7, 10), may also be consequences. For example, in this study, hypertension and sleep problems were positively associated with SRA in cross-sectional analysis but not in incident analysis. Furthermore, we found that the prevalence of SRA was higher among those who used prescription drugs, which is consistent with a study in the USA (43).
Study limitations include self-report evaluation, including diagnosed arthritis or rheumatism by a health care provider. The self-reported outcome may be limited due to common-method variance bias, recall or social desirability bias. Since only SRA was assessed, we cannot distinguish between different types of arthritis. The high attrition rate is a limitation for the longitudinal data. The study cannot establish causality due to confounding and reverse causality. Some variables that may affect arthritis, such as diet, were not included in this study but hopefully in the future. Future research should include multiple waves of HART to establish trajectories of SRA.
Conclusion
One in twenty middle-aged and older Thai adults had SRA. Factors associated with cross-sectional and/or incident SRA included obesity, mental problems, sleep problems, prescription drug use, and functional disability. This information may be taken into account in the prevention and management of arthritis in Thailand and provide hints for future research.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: Gateway to Global Aging Data, Health, Aging, and Retirement in Thailand: https://g2aging.org/?section=study&studyid=44.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee in Human Research, National Institute of Development Administration dmECNIDA (ECNIDA 2020/00012). The patients/participants provided their written informed consent to participate in this study.
Author contributions
SP and KP conceived and designed the research, performed statistical analysis, drafted the manuscript, and made critical revision of the manuscript for key intellectual content. All authors fulfill the criteria for authorship, read and approved the final version of the manuscript, have agreed to authorship, and order of authorship for this manuscript.
Funding
The Health, Aging, and Retirement in Thailand (HART) study is sponsored by Thailand Science Research and Innovation (TSRI) and National Research Council of Thailand (NRCT).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. (2014) 73:1323–30. doi: 10.1136/annrheumdis-2013-204763
2. Cross M, Smith E, Hoy D, Carmona L, Wolfe F, Vos T, et al. The global burden of rheumatoid arthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. (2014) 73:1316–22. doi: 10.1136/annrheumdis-2013-204627
3. Cui A, Li H, Wang D, Zhong J, Chen Y, Lu H. Global, regional prevalence, incidence, and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine. (2020) 3:29–30. doi: 10.1016/j.eclinm.2020.100587
4. Brennan-Olsen SL, Cook S, Leech MT, Bowe SJ, Kowal P, Naidoo N, et al. Prevalence of arthritis according to age, sex and socioeconomic status in six low and middle income countries: analysis of data from the World Health Organization study on global ageing and adult health (SAGE) Wave 1. BMC Musculoskelet Disord. (2017) 18:271. doi: 10.1186/s12891-017-1624-z
5. Peltzer K, Phaswana-Mafuya N. Arthritis and associated factors in older adults in South Africa. Turk J Geriatr. (2013) 16:389–94.
6. Peltzer K, Pengpid S. Prevalence and correlates of arthritis among a nationally representative population-based sample of older adults in India. Int J Disabil Hum Dev. (2022) 21:81–8.
7. Li C, Liu T, Sun W, Wu L, Zou ZY. Prevalence and risk factors of arthritis in a middle-aged and older Chinese population: the China health and retirement longitudinal study. Rheumatology. (2015) 54:697–706. doi: 10.1093/rheumatology/keu391
8. Silverwood V, Blagojevic-Bucknall M, Jinks C, Jordan JL, Protheroe J, Jordan KP. Current evidence on risk factors for knee osteoarthritis in older adults: a systematic review and meta-analysis. Osteoarth Cartil. (2015) 23:507–15. doi: 10.1016/j.joca.2014.11.019
9. Nakua EK, Otupiri E, Dzomeku VM, Owusu-Dabo E, Agyei-Baffour P, Yawson AE, et al. Gender disparities of chronic musculoskeletal disorder burden in the elderly Ghanaian population: study on global ageing and adult health (SAGE WAVE 1). BMC Musculoskelet Disord. (2015) 16:204. doi: 10.1186/s12891-015-0666-3
10. Blay SL, Fillenbaum GG, Andreoli SB, Gastal FL. Prevalence and concomitants of arthritis in the elderly in Rio Grande do Sul, Brazil. PLoS ONE. (2012) 7:e45418. doi: 10.1371/journal.pone.0045418
11. French HP, Galvin R, Horgan NF, Kenny RA. Prevalence and burden of osteoarthritis amongst older people in Ireland: findings from The Irish longitudinal study on ageing (TILDA). Eur J Public Health. (2016) 26:192–8. doi: 10.1093/eurpub/ckv109
12. Arokiasamy P, Uttamacharya, Kowal P, Capistrant BD, Gildner TE, Thiele E, et al. Chronic noncommunicable diseases in 6 low- and middle-income countries: findings from wave 1 of the world health organization's study on global ageing and adult health (SAGE). Am J Epidemiol. (2017) 185:414e–28. doi: 10.1093/aje/kww125
13. Sugiyama D, Nishimura K, Tamaki K, Tsuji G, Nakazawa T, Morinobu A, et al. Impact of smoking as a risk factor for developing rheumatoid arthritis: a meta-analysis of observational studies. Ann Rheum Dis. (2010) 69:70–81. doi: 10.1136/ard.2008.096487
14. Patel S, Ram F, Patel SK, Kumar K. Association of behavioral risk factors with self-reported and symptom or measured chronic diseases among adult population (18–69 years) in India: evidence from SAGE study. BMC Public Health. (2019) 19:560. doi: 10.1186/s12889-019-6953-4
15. Tierney M, Fraser A, Kennedy N. Physical activity in rheumatoid arthritis: a systematic review. J Phys Act Health. (2012) 9:1036–48. doi: 10.1123/jpah.9.7.1036
16. Fenton SAM. Veldhuijzen van Zanten JJCS, Duda JL, Metsios GS, Kitas GD. Sedentary behaviour in rheumatoid arthritis: definition, measurement and implications for health. Rheumatology. (2018) 57:213–26. doi: 10.1093/rheumatology/kex053
17. Scott IC, Tan R, Stahl D, Steer S, Lewis CM, Cope AP. The protective effect of alcohol on developing rheumatoid arthritis: a systematic review and meta-analysis. Rheumatology. (2013) 52:856–67. doi: 10.1093/rheumatology/kes376
18. Pengpid S, Peltzer K. Prevalence and correlates of arthritis among a nationally representative population-based sample of older adults in Mexico. Int J Disabil Hum Dev. (2020) 19:603–10.
19. Machado GM, Barreto SM, Passos VM, Lima-Costa MF. Health status indicators among community-dwelling elders with arthritis: the Bambuí health and aging study. J Rheumatol. (2006) 33:342–7.
20. Prothero L, Barley E, Galloway J, Georgopoulou S, Sturt J. The evidence base for psychological interventions for rheumatoid arthritis: a systematic review of reviews. Int J Nurs Stud. (2018) 82:20–9. doi: 10.1016/j.ijnurstu.2018.03.008
21. Vennu V, Misra H, Misra A. Depressive symptoms and the risk of arthritis: a survival analysis using data from the osteoarthritis initiative. Indian J Psychiatry. (2019) 61:444–50. doi: 10.4103/psychiatry.IndianJPsychiatry_241_18
22. Hossain MB, Kopec JA, Atiquzzaman M, Karim ME. The association between rheumatoid arthritis and cardiovascular disease among adults in the United States during 1999-2018, and age-related effect modification in relative and absolute scales. Ann Epidemiol. (2022) 71:23–30. doi: 10.1016/j.annepidem.2022.03.005
23. Seavey WG, Kurata JH, Cohen RD. Risk factors for incident self-reported arthritis in a 20 year followup of the Alameda county study cohort. J Rheumatol. (2003) 30:2103–11.
24. Berry KM, Neogi T, Baker JF, Collins JM, Waggoner JR, Hsiao CW, et al. Obesity progression between young adulthood and midlife and incident arthritis: a retrospective cohort study of US adults. Arthritis Care Res. (2021) 73:318–27. doi: 10.1002/acr.24252
25. Okely JA, Cooper C, Gale CR. Wellbeing and arthritis incidence: the survey of health, ageing and retirement in Europe. Ann Behav Med. (2016) 50:419–26. doi: 10.1007/s12160-015-9764-6
27. Poole L, Jackowska M. The association between depressive and sleep symptoms for predicting incident disease onset after 6-year follow-up: findings from the English longitudinal study of ageing. Psychol Med. (2019) 49:607–16. doi: 10.1017/S0033291718001290
28. Ke C, Qiao Y, Liu S, Rui Y, Wu Y. Longitudinal research on the bidirectional association between depression and arthritis. Soc Psychiatry Psychiatr Epidemiol. (2021) 56:1241–7. doi: 10.1007/s00127-020-01994-7
29. Anantanasuwong D, Theerawanviwat D, Siripanich P. Panel survey and study on health and aging, and retirement in Thailand. In: Gu D and Dupre M (Eds) Encyclopedia of Gerontology and Population Aging. Cham: Springer (2019).
30. Anantanasuwong D, Pengpid S, Peltzer K. Prevalence and associated factors of successful ageing among people 50 years and older in a national community sample in Thailand. Int J Environ Res Public Health. (2022 7) 19:10705. doi: 10.3390/ijerph191710705
31. Jang SN, Cho SI, Chang J, Boo K, Shin HG, Lee H, et al. Employment status and depressive symptoms in Koreans: results from a baseline survey of the Korean longitudinal study of aging. J Gerontol B Psychol Sci Soc Sci. (2009) 64:677–83. doi: 10.1093/geronb/gbp014
32. WHO. World Health Organization (WHO) guidelines on physical activity and sedentary behavior. Licence: CC BY-NC- SA3.0 IGO. (2020). Available online at: https://file:///C:/Users/user/Downloads/9789240015128-eng%20(2).pdf (accessed June 20, 2022).
33. Wen CP, David Cheng TY, Tsai SP. Are Asians at greater mortality risks for being overweight than Caucasians? Redefining obesity for Asians. Public Health Nutr. (2009) 12:497–506. doi: 10.1017/S1368980008002802
34. Katz S, Ford AB, Heiple KG, Newill VA. Studies of illness in the aged: recovery after fracture of the hip. J Gerontol. (1964) 19:285–93. doi: 10.1093/geronj/19.3.285
35. Senanarong V, Harnphadungkit K, Prayoonwiwat N, Poungvarin N, Sivasariyanonds N, Printarakul T, et al. new measurement of activities of daily living for Thai elderly with dementia. Int Psychogeriatr. (2003) 15:135–48. doi: 10.1017/s1041610203008822
36. Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (center for epidemiologic studies depression scale). Am J Prev Med. (1994) 10:77–84.
37. Nilmanut S, Kuptniratsaikul V, Pekuman P, Tosayanonda O. The Study of The Center for Epidemiologic Studies-Depression Scale (CES-D) in Thai People Siriraj Hospital. ASEAN J Rehabil Med. (1997) 6:3.
38. Mackinnon A, McCallum J, Andrews G, Anderson I. The center for epidemiological studies depression scale in older community samples in Indonesia, North Korea, Myanmar, Sri Lanka, and Thailand. J Gerontol B Psychol Sci Soc Sci. (1998) 53:P343–52. doi: 10.1093/geronb/53b.6.p343
39. Chaiamnuay P, Darmawan J, Muirden KD, Assawatanabodee P. Epidemiology of rheumatic disease in rural Thailand: a WHO-ILAR COPCORD study. community oriented programme for the control of rheumatic disease. J Rheumatol. (1998) 25:1382–7.
40. Safiri S, Kolahi AA, Hoy D, Smith E, Bettampadi D, Mansournia MA, et al. Global, regional and national burden of rheumatoid arthritis 1990-2017: a systematic analysis of the global burden of disease study 2017. Ann Rheum Dis. (2019) 78:1463–71. doi: 10.1136/annrheumdis-2019-215920
41. Chokkhanchitchai S, Tangarunsanti T, Jaovisidha S, Nantiruj K, Janwityanujit S. The effect of religious practice on the prevalence of knee osteoarthritis. Clin Rheumatol. (2010) 29:39–44. doi: 10.1007/s10067-009-1295-8
42. George MD, Baker JF. The obesity epidemic and consequences for rheumatoid arthritis care. Curr Rheumatol Rep. (2016) 18:6. doi: 10.1007/s11926-015-0550-z
43. Lane NE, Ivanova J, Emir B, Mobasheri A, Jensen MG. Characterization of individuals with osteoarthritis in the United States and their use of prescription and over-the-counter supplements. Maturitas. (2021) 145:24–30. doi: 10.1016/j.maturitas.2020.12.001
Keywords: arthritis (MeSH), aging, rheumatoid arthritis, survey, Thailand
Citation: Pengpid S and Peltzer K (2023) Prevalence and associated factors of cross-sectional and incident self-reported arthritis or rheumatism among a national community sample of middle-aged and older adults in Thailand. Front. Public Health 11:1064751. doi: 10.3389/fpubh.2023.1064751
Received: 08 October 2022; Accepted: 11 January 2023;
Published: 01 February 2023.
Edited by:
Enno Nowossadeck, Robert Koch Institute (RKI), GermanyReviewed by:
Lambert Zixin Li, Stanford University, United StatesFaizan Z. Kashoo, Majmaah University, Saudi Arabia
Copyright © 2023 Pengpid and Peltzer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Karl Peltzer,  a2ZwZWx0emVyQGdtYWlsLmNvbQ==
a2ZwZWx0emVyQGdtYWlsLmNvbQ==
 Supa Pengpid
Supa Pengpid Karl Peltzer
Karl Peltzer