
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
OPINION article
Front. Public Health , 09 May 2023
Sec. Infectious Diseases: Epidemiology and Prevention
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1049986
Over the past two decades, Sub-Saharan Africa (SSA) has faced multiple public health emergencies (1). A public health emergency (PHE) is a situation with health consequences too severe for conventional community response (2). Between 2001 and 2022, the region reported 1,800 PHEs, most of them emerging infectious diseases (3). Emerging infectious diseases are new or resurgent diseases in the population (4). Cholera, meningitis, Ebola, measles, yellow fever, monkeypox, Zika, Rift valley fever, and COVID-19 were some of the reported emerging infectious diseases (5). Multiple factors contribute to the rise in SSA's emerging infectious diseases. These include microorganisms adapting to climate and weather changes, shifting ecosystems, and human susceptibility to infection due to immunosuppression, malnutrition, and poor immunization (4).
The region has also seen a rise in zoonotic pathogen outbreaks caused by monkeypox and Ebola viruses. From 2012 to 2022, zoonotic disease outbreaks in SSA rose 63% compared to 2001–2011. From 2001 to 2022, 33% of PHEs were zoonotic disease outbreaks (3). Almost 70% were caused by Ebola virus disease (EVD) and other viral hemorrhagic fevers and 30% by dengue fever, anthrax, plague, monkeypox, and others (3). A growing population driving greater demand for animal-derived food is associated with zoonotic disease outbreaks. Population growth and urbanization have reduced wildlife habitats. SSA has the lowest per-capita health spending and healthcare worker (HCW) availability, which exacerbates health problems and makes emerging infectious disease outbreaks difficult to manage (4). In this opinion piece, we discuss the problems SSA encountered during prior and current emerging infectious disease outbreaks, the strengths realized, and our recommendations to better prepare the region for future emerging infectious disease outbreaks.
In this section, we unpack challenges faced during previous outbreaks grouped into individual, health system, and community-level challenges.
Poor socioeconomic status (SES), stigma, low-risk perception, limited access to healthcare, and cultural beliefs contribute to emerging infectious disease outbreaks in SSA (6). About 34% of SSA households were in extreme poverty living on <$1.90/day in 2021 (7). Overcrowding and the resultant poor hygiene have been associated with emerging infectious diseases such as cholera, measles, monkeypox, EVD, and COVID-19 (8, 9). About 20% of the African population was undernourished in 2019 (10), thereby increasing population vulnerability to infectious diseases, and reducing treatment response due to diminished immunity (11, 12).
Poor SES is linked to low health literacy, limiting infection prevention and control knowledge. Reduced awareness leads to fewer immunizations and delayed treatment, possibly contributing to emerging infectious disease spread (13). Some people have a low-risk perception and don't take infectious disease precautions (8). Delays in seeking medical care raise the community disease burden (14, 15). Some traditional burial practices such as washing dead bodies contributed to the rapid spread of EVD in West Africa during the 2014–2016 outbreak (6).
Underinvestment in health (16), conflicts (5, 17, 18), inadequate disease surveillance systems (6, 19), and a surge in non-communicable diseases (18) disrupted SSA healthcare systems. Critical shortages of HCWs, personal protective equipment (PPE), and testing platforms created weaknesses in active surveillance. The lack of electronic databases contributed to poor data quality due to inconsistency and incompleteness (5, 18). Several SSA countries are categorized as fragile states, and they are struggling to grow due to weak institutions, bad governance, political instability, and frequently ongoing violence or the after-effects of previous conflicts (17). Conflicts disrupt healthcare delivery due to the closure of healthcare facilities, loss of medical equipment, and migration of HCWs (17).
Poor disease surveillance has been attributed to a lack of experienced HCWs, heavy workloads, and low HCW motivation. The lack of PPE and isolation rooms complicates infection control, resulting in patient-to-HCW cross-infections (6). Low laboratory testing capacity in SSA's vulnerable populations contributes to virus spread (20). PHEs disrupt normal childhood immunizations, resulting in disease outbreaks (21).
People unlawfully cross SSA's porous borders (22). Without effective port-of-entry surveillance, persons can import/export emerging infectious diseases across countries, complicating contact tracing (6). Mistrust of governments and the healthcare system led to a drop in immunization and COVID-19 treatment (23). Furthermore, even some people may not seek healthcare for fear of social stigma as was common in the EVD-affected communities in Sierra Leone, Guinea, and Liberia (6).
There were also some notable strengths, which we stratified into individual-level, health system-level, and community-level strengths.
In 2018, SSA had 44% mobile phone penetration (24). Cell phone technology has made social media platforms easier to use. This means that more people can now be reached with messaging about interrupting infection chains and refuting rumors, misunderstandings, and misconceptions about emerging infectious diseases (25). The relatively youthful populations in SSA meant that those who got the infections recovered quickly if there were no underlying immunosuppressive conditions (1).
Several SSA nations have had an emerging infectious disease outbreak, therefore they have response strategies for PHEs. HCWs with prior experience in handling emerging infectious disease outbreaks are valuable in managing ongoing emerging infectious disease outbreaks (26). As part of emergency response operations in SSA, non-governmental organizations (NGOs) provided technical, financial, and logistical aid to health facilities, reducing the financial load on afflicted countries (27).
During the EVD and COVID-19 epidemics, SSA nations cooperated to improve disease testing (28). The majority of SSA nations also have community health workers who were employed during prior emerging infectious disease outbreaks to warn their communities and health authorities about probable cases (29). Instead of focusing on contacts, mass immunization initiatives showed the potential in limiting emerging infectious diseases (30, 31).
During COVID-19, SSA increased genomic surveillance, and South Africa and Botswana detected the Beta and Omicron variants. Transparency in reporting revealed SSA countries were ready to collaborate to control emerging infectious diseases (32). Despite numerous challenges, there has been progress in the utilization of the integrated disease surveillance and response (IDSR) framework in SSA. In the past two decades, 94% of the countries used the framework to enhance surveillance capacity for priority diseases (19).
Past PHEs in Africa resulted in structures for future emerging infectious disease outbreaks (6). Re-engaging local community members who had been trained to distribute information about the EVD outbreak in the Republic of Congo boosted community awareness of the messaging. Communities accepted HCWs, tolerated prescribed behaviors, and felt more comfortable reporting cases (30). During the EVD outbreak in Cote d'Ivoire, community-led education about infection control helped people wash their hands more often and stop unhealthy practices associated with shaking hands and burying their dead. This education was then used during subsequent outbreaks (30).
From the challenges and strengths experienced during the previous and current emerging infectious disease outbreaks, we came up with recommendations on how SSA might better prepare for future emerging infectious disease outbreaks.
SSA's low SES worsens conflict and disease outbreaks. SSA countries should come up with plans to raise their populations' SES. Strategies include increasing industrialization, maximizing agricultural potential, and integrating regional markets (33). Improved economic activity creates jobs, improves food security, and increases investment in basic utilities like water and sanitation, reducing emerging infectious disease outbreaks (7). Table 1 summarizes each strategy and the required actions.
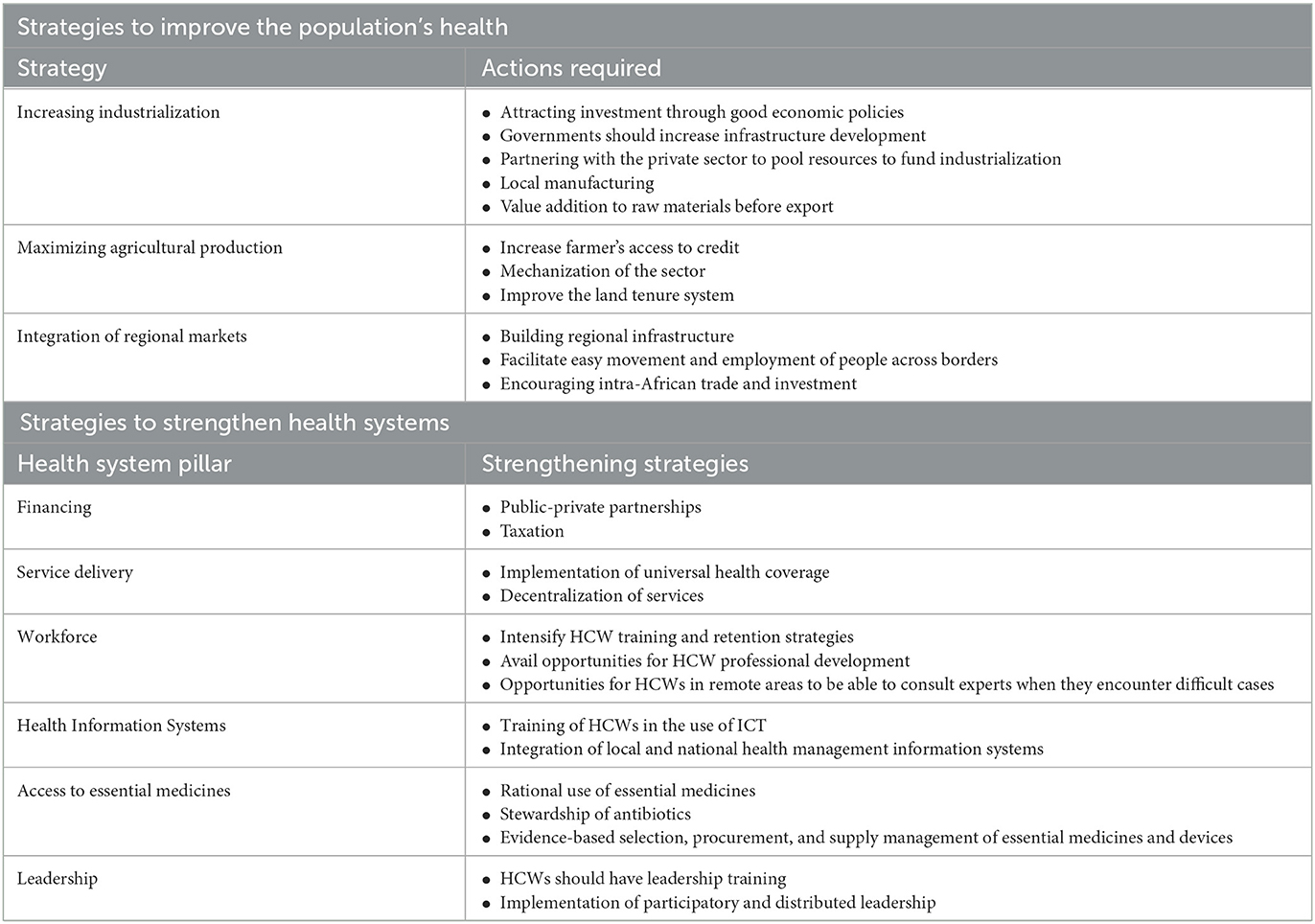
Table 1. Strategies to improve the population's socio-economic status and strengthen health systems.
We advocate improving access to education and initiating health education in preschool to increase health literacy. With more health knowledge, the population's risk perception may rise, leading to more vaccinations and healthcare utilization (34).
The health system recommendations include the implementation and strengthening of the One Health approach, strengthening health systems, and improving disease surveillance.
SSA countries should strengthen the One Health Approach. One Health Approach addresses zoonoses where people, animals, and the environment intersect. It aims to create interdisciplinary, cross-sectoral, and cross-regional collaboration to predict emerging infectious disease outbreaks (35). Domestic and wild animals harbor diseases that cause emerging infectious diseases. Integrated human, animal, and environmental surveillance can explain pathogen-sharing paths, allowing for more complete treatments that prioritize prevention at the source. Increasing cross-sectoral cooperation can help encourage science-based decision-making, reduce wasteful duplication, and address external variables driving disease burden (36). Animal handlers are prone to emerging infectious diseases and often disseminate new diseases to other people. Regular surveillance of these individuals is critical in preventing emerging infectious disease outbreaks. To improve early warning systems and emerging infectious disease outbreak detection, proactive animal handler surveillance can be an important addition to hospital surveillance (37).
Sub-Saharan Africa should enhance its health systems to handle future emerging infectious disease outbreaks. Workforce, service delivery, health information systems, access to essential medicines, health financing, and leadership and governance should be reinforced. These initiatives should be localized (3, 5, 38–41). Table 1 shows the strategies that can be used to strengthen the health systems in SSA.
Laboratories' capacity needs to be improved to be able to identify a variety of pathogens. Furthermore, it is important to create laboratory networks that link national, regional, and research reference laboratories (38). More HCWs should receive training in disease surveillance and epidemiology to improve emerging infectious disease surveillance in SSA. Refresher courses or the development of online public health programs that are flexible for full-time HCWs could accomplish this. A robust public health workforce should be formed to collect, access, share, and act on high-quality data, including making use of cutting-edge technologies like genetic sequencing and informatics.
SSA countries must upgrade their information, communication, and technology (ICT) infrastructure to gather and send patient health data. By reducing data volume and automating data collection, validation, and analysis, ICT can reduce errors. Local health management information systems (HMIS) should be integrated with national HMIS, and data should be used at every level of the healthcare system to enable ICT uptake and use. Data should be aggregated and summarized to offer summary indicators for planning and resource allocation (19). The national HMIS should have multiple sources. Antimicrobial resistance surveys, systematic surveys, environmental data, vital statistics, civil registrations, vital statistics, and research data are examples of these sources (19).
Big data and artificial intelligence (AI) can transform emerging infectious disease surveillance and response by improving the current traditional systems and strengthening outbreak detection and response (11). Digital disease surveillance (DDS) data from outside the public health system should be used. DDS aggregates and analyzes internet data unrelated to patient conditions or medical contacts. This information is available on search engines, social media, and mobile devices. DDS improves the timeliness and breadth of monitoring information in high-income countries. Thailand and New Zealand used DDS to detect, trace, and isolate COVID-19 cases (19). Community-based surveillance (CBS) should be promoted because it leads to early detection and rapid reporting of emerging infectious disease cases to the health system. Community-based surveillance helps detect risk groups and enumerate cases (42).
SSA countries should inform local populations about emerging infectious diseases using billboards, mainstream media, and social media platforms in their native languages (25). Social scientists should develop a strong capacity for community engagement to change unhealthy behaviors such as eating uncooked or raw food, as well as promiscuous sexual behavior (38). Engaging communities improve priority planning, resource allocation, and adoption of emerging infectious disease-related healthcare treatments, such as immunizations. It also deepens discussions and raises accountability.
SSA has had multiple PHEs in the past two decades, most of them emerging infectious disease outbreaks. Emerging infectious disease outbreaks were caused by microorganism adaptation and alteration due to climatic and environmental changes, shifting habitats, and increased human susceptibility to infection due to immunosuppression, undernourishment, and poor vaccination. The bulk of emerging infectious disease outbreaks was caused by zoonotic pathogens, and their rise has been related to urbanization, a fast-expanding population, increased demand for animal food, and invasion of natural habitats. When managing and containing the emerging infectious disease outbreaks, the countries in the region encountered several challenges at the individual, health system, and community levels. Furthermore, the management and control of these outbreaks also revealed several strengths the region has. Based on these challenges and strengths, we suggest that the region implement and strengthen the One Health approach, improve the socioeconomic status of the population, strengthen its health systems, improve disease surveillance, and involve and educate communities about emerging infectious diseases.
EM and MM: conceptualization and writing original draft. PM: writing original draft. TD: conceptualization, supervision, and writing review and editing. IC and GM: writing review and editing. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Bitanihirwe B, Ssewanyana D, Ddumba-Nyanzi I. Pacing forward in the face of fragility: lessons from african institutions and governments' response to public health emergencies. Front Public Health. (2021) 9:714812. doi: 10.3389/fpubh.2021.714812
2. Nelson C, Lurie N, Wasserman J, Zakowski S. Conceptualizing and defining public health emergency preparedness. Am J Public Health. (2007) 97:S9–S11. doi: 10.2105/AJPH.2007.114496
3. World Health Organization Africa (WHO Africa). In Africa, a 63% Jump in Diseases Spread From Animals to People Seen in the Last Decade. (2022). Available online at: https://www.afro.who.int/news/africa-63-jump-diseases-spread-animals-people-seen-last-decade#:~:text=There%20has%20been%20a%2063,in%20the%20WHO%20African%20region (accessed September 12, 2022).
4. Fenolla F, Mediannikov O. Emerging infectious diseases in Africa in the 21st century. New Microbes New Infect. (2018) 26:S10–8. doi: 10.1016/j.nmni.2018.09.004
5. Nyaruaba R, Okoye CO, Akan CD, Mwaliko C, Ebiko CC, Ayoola A, et al. Socio-economic impacts of emerging infectious diseases in Africa. Infect Dis. (2022) 54:315–24. doi: 10.1080/23744235.2021.2022195
6. Buseh A, Stevens P, Bromberg M, Kelber S. The Ebola epidemic in West Africa: challenges, opportunities, and policy priority areas. Nurs Outlook. (2015) 63:30–40. doi: 10.1016/j.outlook.2014.12.013
7. United Nations (UN),. Reaping the Potential Benefits of the African Continental Free Trade Area for Inclusive Growth. (2021). Available online at: https://unctad.org/system/files/official-document/aldcafrica2021_en.pdf (accessed September 15, 2022).
8. Bambra C. Pandemic inequalities: emerging infectious diseases and health equity. Int J Equity Health. (2022) 21:6. doi: 10.1186/s12939-021-01611-2
9. Tambo E, Al-Nazawi A. Combating the global spread of poverty-related Monkeypox outbreaks and beyond. Infect Dis Poverty. (2022) 11:80. doi: 10.1186/s40249-022-01004-9
10. Food Agricultural Organization of the United Nations (FAO). Executive Summary: Food Security and Nutrition Around the World in 2020. (2020). Available online at: https://www.fao.org/3/ca9692en/online/ca9692en.html#chapter-executive_summary (accessed September 12, 2022).
11. Agrebi S, Larbi A. Use of artificial intelligence in infectious diseases. Artif Intell Precis Med. (2020) 2020:415–38. doi: 10.1016/B978-0-12-817133-2.00018-5
12. Hove-Musekwa SD, Nyabadza F, Chiyaka C, Das P, Tripathi A, Mukandavire A. Modelling and analysis of the effects of malnutrition in the spread of cholera. Math Comput Model. (2011) 53:1583–95. doi: 10.1016/j.mcm.2010.11.060
13. Matterne U, Egger N, Tempes J, Tischer C, Lander J, Dierks M, et al. Health literacy in the general population in the context of epidemic or pandemic coronavirus outbreak situations: rapid scoping review. Patient Educ Couns. (2021) 104:223–34. doi: 10.1016/j.pec.2020.10.012
14. Takeyama N, Muzembo B, Jahan Y, Moriyama M. Health-seeking behaviors in mozambique: a mini-study of ethnonursing. Int J Environ Res Public Health. (2022) 19:2462. doi: 10.3390/ijerph19042462
15. Pomerai K, Mudyiradima R, Gombe N. Measles outbreak investigation in Zaka, Masvingo Province, Zimbabwe, 2010. BMC Res Notes. (2012) 5:687. doi: 10.1186/1756-0500-5-687
16. Gautier L, Ridde V. Health financing policies in Sub-Saharan Africa: government ownership or donors' influence? A scoping review of policymaking processes. Glob Health Res Policy. (2017) 2:23. doi: 10.1186/s41256-017-0043-x
17. Bruckner C, Checchi F. Detection of infectious disease outbreaks in twenty-two fragile states, 2000-2010: a systematic review. Confl Health. (2011) 5:13. doi: 10.1186/1752-1505-5-13
18. Gouda HN, Charlson F, Sorsdahl K, Ahmadzada S, Ferrari A, Erskine H, et al. Burden of non-communicable diseases in sub-Saharan Africa, 1990–2017: results from the Global Burden of Disease Study 2017. Lancet Glob Health. (2019) 7:E1375–87. doi: 10.1016/S2214-109X(19)30374-2
19. Mremi IR, George J, Rumisha SF, Sindato C, Kimera SI, Mboera LE. Twenty years of integrated disease surveillance and response in Sub-Saharan Africa: challenges and opportunities for effective management of infectious disease epidemics. One Health Outlook. (2021) 3:22. doi: 10.1186/s42522-021-00052-9
20. Schubert G, Achi V, Ahuka S, Belarbi E, Bourhaima O, Eckmanns T, et al. The African network for improved diagnostics, epidemiology and management of common infectious agents. BMC Infect Dis. (2021) 21:539. doi: 10.1186/s12879-021-06238-w
21. Dzinamarira T, Moyo E, Moyo P, Pierre G, Mpabuka E, Kahere M, et al. Childhood immunization services accessibility and utilization during the COVID-19 pandemic in Africa. J Infect. (2022) 85:436–80. doi: 10.1016/j.jinf.2022.07.020
22. Murewanhema G. COVID-19 control pitfalls and challenges and drivers of SARS-CoV-2 transmission in Zimbabwe. Pan Afr Med J. (2021) 38:28. doi: 10.11604/pamj.2021.38.28.25758
23. Bisung E, Meshack A, Dassah E, Kuuire V. Public health response to COVID-19 pandemic and drivers of mistrust in Ghana. Afr Geogr Rev. (2021) 1–12. doi: 10.1080/19376812.2021.2007411
24. Mitchell J. Will Mobile Phone Penetration Maintain African Momentum? FDI Intelligence (2020). Available online at: https://www.fdiintelligence.com/content/feature/will-mobile-phone-penetration-maintain-african-momentum-76565 (accessed August 29, 2022).
25. Hossain L, Kam D, Kong F, Wigand RT, Bossomaier T. Social media in Ebola outbreak. Epidemiol Infect. (2016) 144:2136–43. doi: 10.1017/S095026881600039X
26. Chimusoro A, Maphosa S, Manangazira P, Phiri I, Nhende T, Danda S, et al. Responding to Cholera Outbreaks in Zimbabwe: Building Resilience Over Time. Intechopen (2018). Available online at: https://www.intechopen.com/books/current-issues-in-global-health/responding-to-cholera-outbreaks-in-zimbabwe-building-resilience-over-time (accessed September 10, 2022).
27. Shin Y, Yeo J, Jung K. The effectiveness of international non-governmental organizations' response operations during public health emergency: lessons learned from the 2014 Ebola Outbreak in Sierra Leone. Int J Environ Res Public Health. (2018) 15:650. doi: 10.3390/ijerph15040650
28. Arunga G, Ca T, Odero P, Bashir A, Somda SM, Adan F, et al. Experience in fostering regional collaboration and coordination to use data for battling infectious diseases in sub-Saharan Africa. East Afr Health Res J. (2021) 5:114–22. doi: 10.24248/eahrj.v5i2.660
29. Ballard M, Johnson A, Mwanza I, Ngwira H, Schechter J, Odera M, et al. Community health workers in pandemics: evidence and investment implications. Glob Health Sci Pract. (2022) 10:e2100648. doi: 10.9745/GHSP-D-21-00648
30. Owoyemi A, Okolie EA, Omitiran K, Amaechi UA, Sodipo BO, Ajumobi O, et al. Importance of community-level interventions during the COVID-19 pandemic: lessons from Sub-Saharan Africa. Am J Trop Med Hyg. (2021) 105:879–83. doi: 10.4269/ajtmh.20-1533
31. Nomhwange T, Jean Baptiste AE, Ezebilo O, Oteri J, Olajide L, Emelife K. The resurgence of yellow fever outbreaks in Nigeria: a 2-year review 2017–2019. BMC Infect Dis. (2021) 21:1054. doi: 10.1186/s12879-021-06727-y
32. Banerjee I, Robinson J, Banerjee I, Sathian B. Omicron: the pandemic propagator and lockdown instigator – what can be learnt from South Africa and such discoveries in future. Nepal J Epidemiol. (2021) 11:1126–9. doi: 10.3126/nje.v11i4.41569
33. African Development Bank (AFDB). The High 5: Improve the Quality of Life for the People of Africa. (2022). Available online at: https://www.afdb.org/en/the-high-5/improve-the-quality-of-life-for-the-people-of-africa (accessed August 15, 2022).
34. Gatobu S, Brockett E, Sider S. Health literacy education in Sub-Saharan African: a scoping review. Int J Humanit Soc Sci Educ. (2022) 9:312–21. doi: 10.20431/2349-0381.0904029
35. Zinsstag J, Schelling E, Waltner-Toews D, Tanner M. From “one medicine” to “one health” and systemic approaches to health and well-being. Prev Vet Med. (2011) 101:148–56. doi: 10.1016/j.prevetmed.2010.07.003
36. Lebov J, Grieger K, Womack D, Zaccaro D, Whitehead N, Kowalcyk B, et al. A framework for One Health research. One Health. (2017) 3:44–50. doi: 10.1016/j.onehlt.2017.03.004
37. Wu Q, Li Q, Lu J. A One Health strategy for emerging infectious diseases based on the COVID-19 outbreak. J Biosaf Biosec. (2022) 4:5–11. doi: 10.1016/j.jobb.2021.09.003
38. World Health Organization Africa (WHO Africa). Everyone's Business-Strengthening Health Systems to Improve Health Outcomes: WHO's Framework for Action. (2007). Available online at: https://apps.who.int/iris/handle/10665/43918 (accessed August 30, 2022).
39. Nkengasong J, Tessema S. Africa needs a new public health order to tackle infectious disease threats. Cell. (2020) 83:296–300. doi: 10.1016/j.cell.2020.09.041
40. Gilson L, Agyepong I. Strengthening health system leadership for better governance: what does it take? Health Policy Plan. (2018) 33:ii1–4. doi: 10.1093/heapol/czy052
41. Takoutsing BD, Ikwuegbuenyi C, Umutoni A, Ogunfolaji O, Bankole ND, Mpokota R, et al. Health systems strengthening, dissemination, and implementation science in Africa: quo vadis? Pan Afr Med J. (2021) 40:51. doi: 10.11604/pamj.2021.40.51.30399
Keywords: emerging infectious diseases, Sub-Saharan Africa, public health response, preparedness and response, outbreak
Citation: Moyo E, Mhango M, Moyo P, Dzinamarira T, Chitungo I and Murewanhema G (2023) Emerging infectious disease outbreaks in Sub-Saharan Africa: Learning from the past and present to be better prepared for future outbreaks. Front. Public Health 11:1049986. doi: 10.3389/fpubh.2023.1049986
Received: 21 September 2022; Accepted: 13 March 2023;
Published: 09 May 2023.
Edited by:
Annalisa Pantosti, National Institute of Health (ISS), ItalyReviewed by:
Mingke Wang, Naval Medical Center, ChinaCopyright © 2023 Moyo, Mhango, Moyo, Dzinamarira, Chitungo and Murewanhema. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tafadzwa Dzinamarira, dTE5Mzk1NDE5QHVwLmFjLnph
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.