- 1Research Team, The Neo Child Initiative, Lagos, Nigeria
- 2Lagos University Teaching Hospital, Lagos, Nigeria
- 3Team Lead, The Neo Child Initiative, Lagos, Nigeria
- 4Senior Clinical Research Associate, XCene Research, Lagos, Nigeria
- 5Founder, The Neo Child Initiative, Lagos, Nigeria
- 6Department of Medicine and Surgery, College of Medicine, University of Lagos, Lagos, Nigeria
- 7Faculty of Dental Sciences, College of Medicine, University of Lagos, Lagos, Nigeria
- 8Department of Community Health and Primary Care, College of Medicine, University of Lagos, Lagos, Nigeria
Objectives: In order to achieve herd immunity against COVID-19, a significant proportion of the population will need to be vaccinated. Experts have recommended that African children be allowed to get vaccinated to protect them from emerging variants of COVID-19 infection. This study investigated Nigerian parents and caregivers’ knowledge, attitude, and willingness to vaccinate their children against COVID-19 once the vaccines are made available to them.
Methods: A cross-sectional online survey of 500 parents/caregivers was conducted in Nigeria. Participants were asked to complete a questionnaire about their sociodemographic characteristics, knowledge of and attitude toward COVID-19 infection and vaccination, willingness to vaccinate their child and factors that could influence their decision to vaccinate their child. A scoring system was used to classify the level of knowledge and attitude of participants into 2 categories, namely poor, and good. We analyzed data obtained using SPSS Version 22.
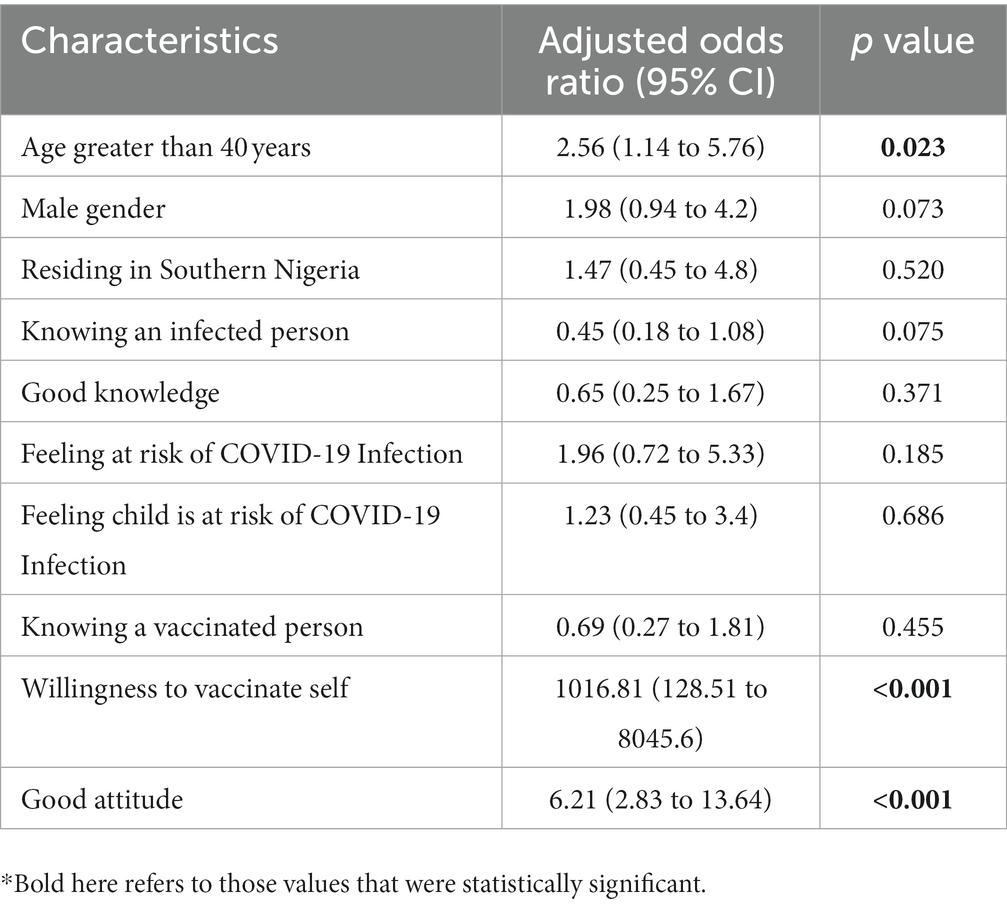
Results: Majority of the participants were females (63.6%). Analysis of responses revealed good knowledge and attitude in 265 (53.0%) and 266 (53.2%) respondents, respectively. Overall, less than half of the parents/caregivers (48.4%) expressed intention to vaccinate their children against COVID-19. Factors associated with willingness to vaccinate children against COVID-19 included age greater than 40 years, male gender, residing in Southern Nigeria, having good knowledge, knowing an infected person or a vaccinated person, feeling they or their child is at risk of contracting COVID-19 infection, willingness to vaccinate self against COVID-19 and good attitude. Significant predictors of willingness to vaccinate their child include age greater than 40 years [AOR: 2.56; 95% CI = (1.14–5.76)], willingness to vaccinate self [AOR: 1016.81; 95% CI = (128.51–8045.60)] and good attitude [AOR: 6.21; 95% CI = (2.83–13.64)].
Conclusion: This study revealed that parental willingness to vaccinate their children against COVID-19 is low and identified factors influencing it. It is important to develop and implement health education programs iterating the risk of children getting infected with SARS-CoV-2 and its emerging variants to ensure optimal uptake of the COVID-19 vaccine in Nigerian children.
Introduction
The novel coronavirus disease 2019 (COVID-19) infection was first reported in December, 2019 (1). Ever since, it has continued to spread across the globe with over 680 million cases and 6 million deaths reported in 231 countries (2, 3). In Nigeria, as of March 10, 2023, the country has recorded a total number of 266,598 and 3,155 cases and deaths, respectively (4). Notably, in the past year, there have been reports of the emergence of SARS-CoV-2 variants potentially more infectious and virulent than the original strain responsible for the initial outbreak (5). At the beginning of the pandemic, public health measures were recommended to prevent and reduce the transmission of COVID-19, including frequent hand-washing, use of face masks and social distancing while vaccines were in development (1, 2).
Vaccination is a cost-effective way of boosting immunity against pathogens (2). In December 2020, the SARS-CoV-2 vaccine was rolled out with the hope that it would reduce the disease burden on healthcare systems globally and put an end to the pandemic (1). The COVID-19 vaccination program in Nigeria has been implemented in both urban and rural areas, with primary healthcare centers across all 774 local government areas providing free vaccines (6). The first batch of COVID-19 vaccines (Oxford-AstraZeneca) was received from the Japanese government in March 2021, with additional doses received from various sources throughout 2021 and 2022 (7).
As Nigeria is the most populous African country, its COVID-19 vaccination coverage will have significant subregional and regional impacts (6). Nigeria’s goal was to vaccinate at least 70% of the eligible population with COVID-19 vaccines by the end of December 2022. However, as at 20th January, 2023, the country had only fully vaccinated 65,143,040 (56%) eligible individuals, while 76,957,026 (66.4%) had received at least one vaccine dose. Vaccine hesitancy due to misinformation about the vaccine’s safety and efficacy poses a significant challenge to achieving this target. Vaccination is critical toward mitigating the outbreak as it ensures herd immunity (8). To achieve herd immunity for COVID-19 infection, there is a need to expand vaccine coverage to include children (1). A number of mRNA vaccines have been approved for use in children aged 18 years and below including Comirnaty (Pfizer-BioNTech’s BNT162b2) and Spikevax (Moderna’s mRNA-1273) (5). In 2020, the COVID-19 vaccination program in Nigeria granted a waiver for children aged 16–17 years to receive the vaccine for educational purposes, and as at February 2023, a total of 2,229,295 children had received the vaccine for this purpose (9).
Children aged 14 years and younger account for over 89 million Nigerians, almost half (44%) of the total population (10). Children and adolescents of all ages are vulnerable to SARS-CoV-2 infection. They may be at increased risk of getting infected by SARS-CoV-2 variants such as Delta and Omicron, especially if they are not vaccinated (5). COVID-19 presents with a milder course of acute illness in children compared to adults, however, there is a potential risk for severe complications that can affect their health on the long term (5). Asides these, children in LMICs like Nigeria have a higher prevalence of co-morbidities and as such, these children at increased risk of severe disease should be vaccinated against COVID-19 (11). Thus, experts have recommended that African children be allowed to get vaccinated against COVID-19 especially those with significant risk of severe disease and death, given the emerging variants of SARS-CoV-2 infection (8).
Parents significantly influence their child’s vaccine uptake, and as such to increase the vaccination rate amongst children, parental hesitancy must be considered (1). Several research has been done to investigate parental willingness to vaccinate children since the vaccine was introduced. In a meta-analysis of 44 studies including 317,055 parents, parental intention to accept COVID-19 vaccine for their child ranged from 25.6 to 92.2%. However, the vast majority of the papers included were done in high-income countries, and it may be difficult to generalize their findings to Sub Saharan African population (12). In a rapid review carried out by Olu-Abiodun et al., in Nigeria in 2022, the vaccine acceptance rate among adults varied across the six geopolitical zones of the country, ranging from 20.0 to 58.2%. The non-acceptance of the vaccine was attributed to several factors such as propaganda, concerns over adverse effects, conspiracy theories, disbelief, and queries over vaccine safety (13). The factors that might be pertinent to the decision-making of parents regarding whether to vaccinate their children or not include vaccine side effects, conspiracy theories, disbelief, and fear of vaccine safety (Figure 1).
In June 2022, Nigeria reported fears of a fifth wave of COVID-19 outbreak amidst abysmally low vaccine uptake amongst adults. This poor uptake has been linked to vaccine hesitancy. A nationwide survey of 3,076 Nigerians reported a 50.7% vaccine acceptance rate (2). Reluctance to get vaccinated against COVID-19 can significantly impact outbreak control in the country. For minors aged under 18 years, parents and caregivers are the decision-makers and as such, it is important to determine their willingness to accept COVID-19 vaccination for their children and its determinants. This epidemiological landscape presents the urgent need to report determinants of parental willingness to vaccinate their children as identifying factors associated with parental acceptability will guide public health officials and other stakeholders on strategies to improve vaccination rates and achieve herd immunity. To address this gap in knowledge, the study was conducted by the Neo Child Initiative for Africa (TNCI), a non-governmental organization focused on improving the lives of Nigerian children through various initiatives that promote child health and education for sustainable development (14). The present study aimed to investigate the willingness of Nigerian parents and caregivers to vaccinate their children against COVID-19. We also compared the sociodemographic characteristics of parents and caregivers willing to vaccinate their child with those who were not willing to vaccinate their child.
Materials and methods
Study design
A country-wide cross-sectional survey was conducted, using a survey tool distributed via online media sites to all six geopolitical zones in Nigeria to assess parents and caregivers knowledge, attitude, and willingness to vaccinate their children against COVID-19 infection.
Population and sample size
Convenient sampling was utilized for this research. Minimum sampling size was determined to be 363. This was calculated by assuming a prevalence level of 72.6 from a previous study done by Zhang et al., confidence level of 95%, margin of error of 5% and a non-response rate of 20% (15, 16).
The survey was designed on Google Form and shared on social media platforms, including Twitter, Instagram, WhatsApp, Facebook over a period of 1 month social media influencers and volunteers of the Neo Child Initiative residing in the six geopolitical zones of the country were recruited to ensure dissemination in every region. The inclusion criteria of the study were as follows: participants aged at least 18 years, parent and/caregiver of at least one child, and currently residing in Nigeria, ability to read and understand English and being a user of any of the following social media platforms – Facebook, Twitter, Instagram or WhatsApp. Participants whose children were not residing in Nigeria, and those who had no digital literacy were excluded from the study.
Measures
The questionnaire used for this survey was developed with adaptations of relevant sections from previous studies that have sought to address similar objectives (17–20). It was initially piloted with 15 parents and caregivers selected from the six geopolitical zones with further refinement based on feedback gotten from these respondents and public health experts. The final questionnaire was then designed and disseminated using the application Google Form from the 1st of June 2021 to 28th of June 2021.
The questionnaire was self-administered and consisted of 47 questions divided into four sections: in the first part, socio-economic background was explored, including age, gender, educational level, occupation, marital status, and income. In the second part, knowledge of COVID-19 infection was asked. Respondents were also asked their opinion on the credibility of information sources for COVID-19. This question was collected on a 4-point Likert scale, ranging from not credible at all to very credible. In the third part, attitudes toward COVID-19 infection were asked, including perception of risk of infection for themselves and their child. In the fourth part, the respondents were asked if they had ever been diagnosed with COVID-19, or knew someone who had been diagnosed, whether they were willing to vaccinate themselves, and if they were willing to vaccinate their child, and reasons why they do not want to collect the vaccine. Knowledge and attitude variables were scored (A score of 1 was given for correct answers and a score of 0 for wrong answers). Using the mean values of the scores from all respondents, we created dichotomized measures for knowledge and attitude. Knowledge and attitude were categorized as good if the respondent had a score equal to or above the mean value and poor if score was lower than the mean value (19).
Data analysis
We analyzed survey responses using the Statistical Package for the Social Sciences (SPSS) V. 21.0 (SPSS, Chicago, Illinois, United States). Descriptive statistics, including frequency, measures of central tendency and variations were used to report information about participants socio-economic characteristics, knowledge and attitudes toward COVID-19 vaccination, willingness to vaccinate their children, and factors influencing willingness to vaccinate.
Bivariate analysis was used to compare the characteristics of parents and caregivers who were willing to vaccinate their child with those who were not willing. Associations between categorical variables were analyzed using the Chi-Square and Fisher’s exact test. Bivariate logistic regression analysis was used to identify the predictors of parent and caregivers being willing to vaccinate their child and adjusted odds ratios (AORs) and 95% CIs were reported.
Ethics approval
Ethical approval for this study was obtained from the Institutional Review Board at the Lagos University Teaching Hospital with the ethical approval number ADM/DCST/HREC/APP/4200. Implicit consent to be a part of this survey was considered when participants completed the online questionnaire.
Results
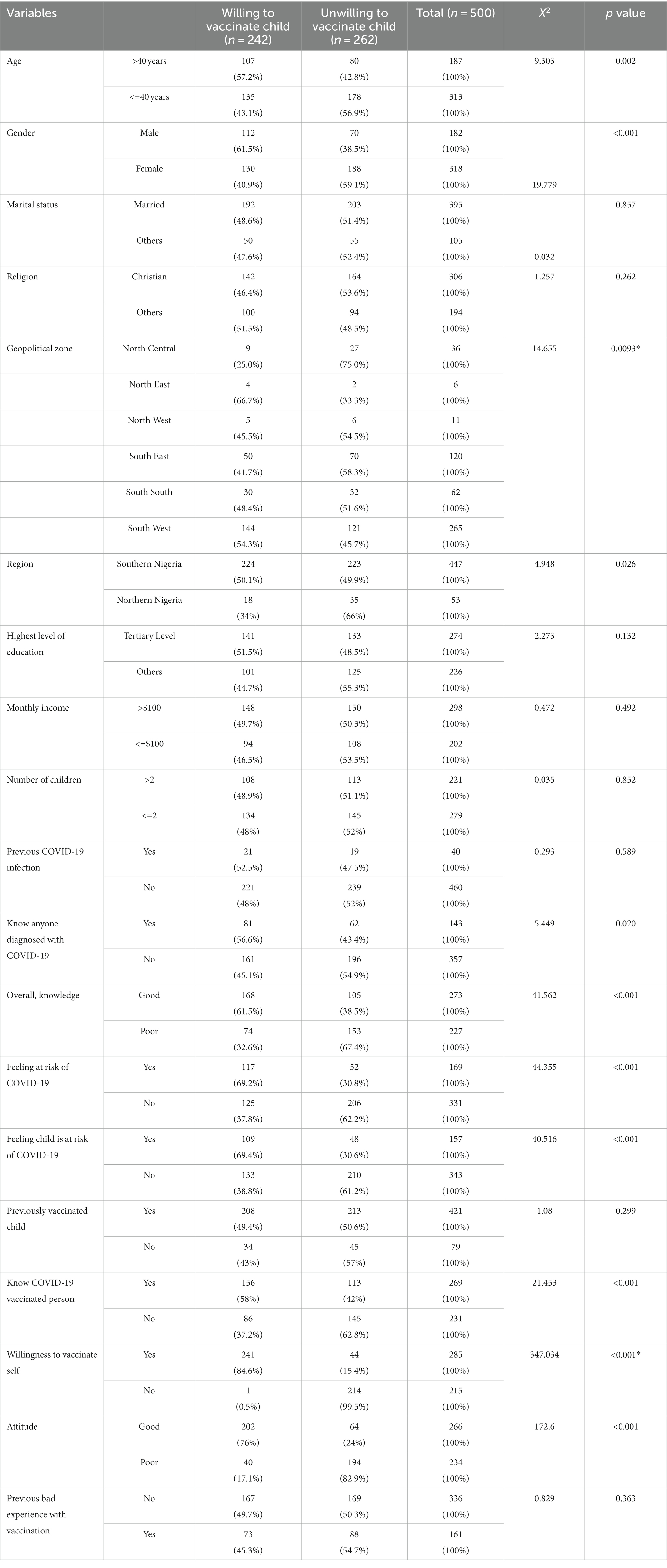
A total of 500 adults filled the online form for data collection. There were no missing data. Most of the respondents were aged between 31 and 40 years (34.6%), Female (63.6%), married (79%) and from the Southern part of the country (89.4%). They were mostly parents (70.4%) and had tertiary level of education (54.8%). About one third of them knew a person that had been diagnosed with COVID-19 infection. Approximately half of them had good knowledge and attitude (53 and 53.2% respectively). Only a third of them (33.8%) perceived that they were at risk of COVID-19 infection and less than one-third of them (31.4%) felt that their child was at risk of COVID-19 infection. Almost all the parents/caregivers had previously vaccinated their child from birth (84.2%). Only one-tenth of them had previous side effects after vaccination (Table 1).
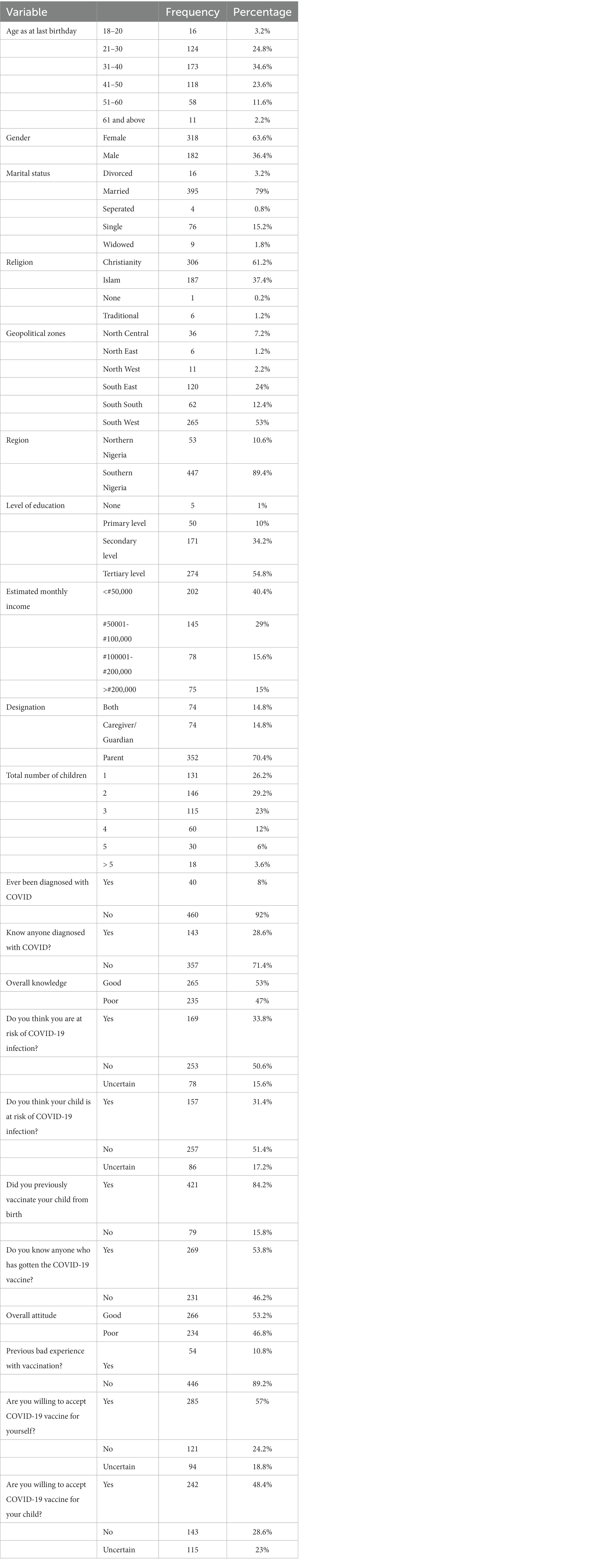
Table 1. Participant’s sociodemographic characteristics, overall knowledge, attitude, and willingness to vaccinate their child against COVID-19.
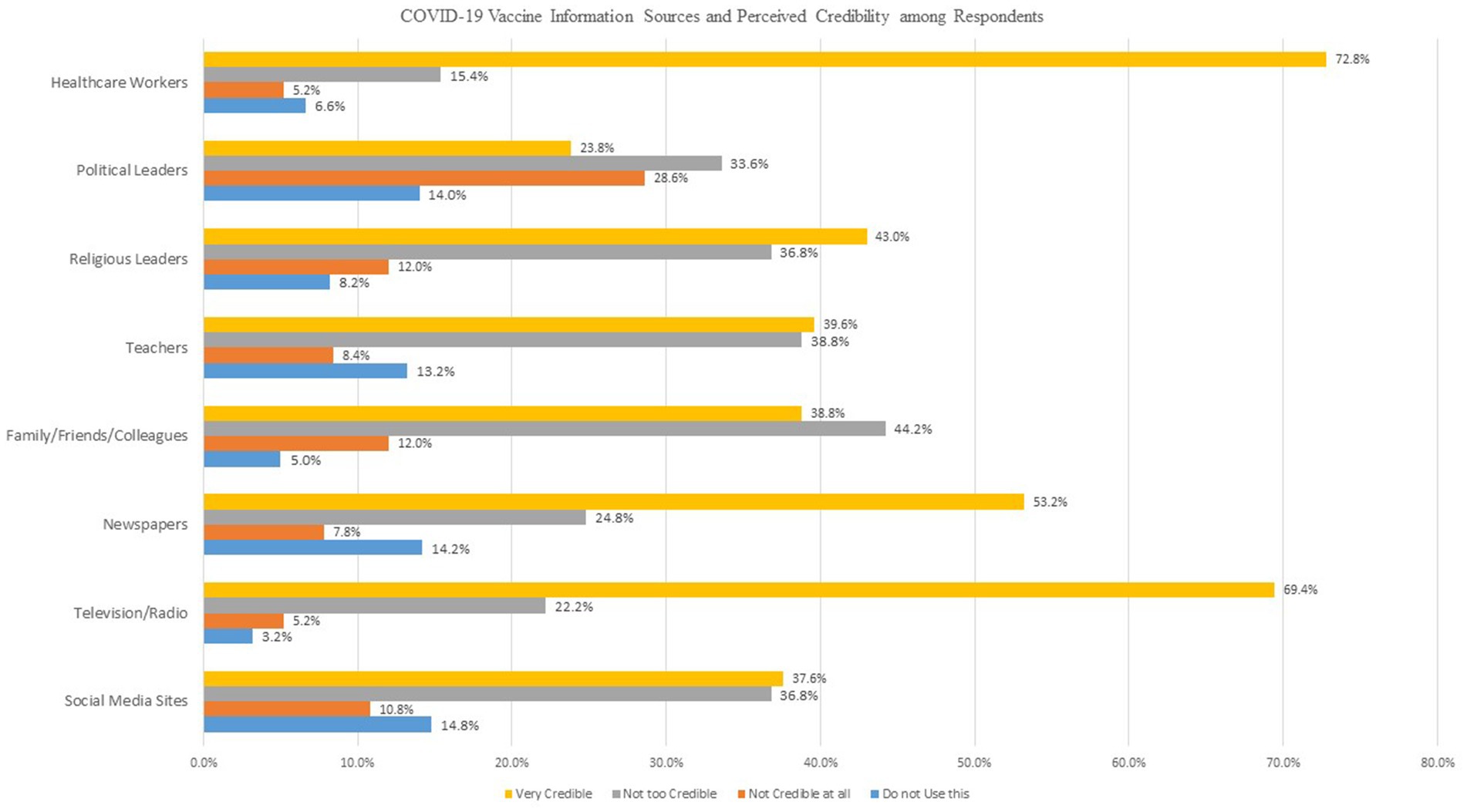
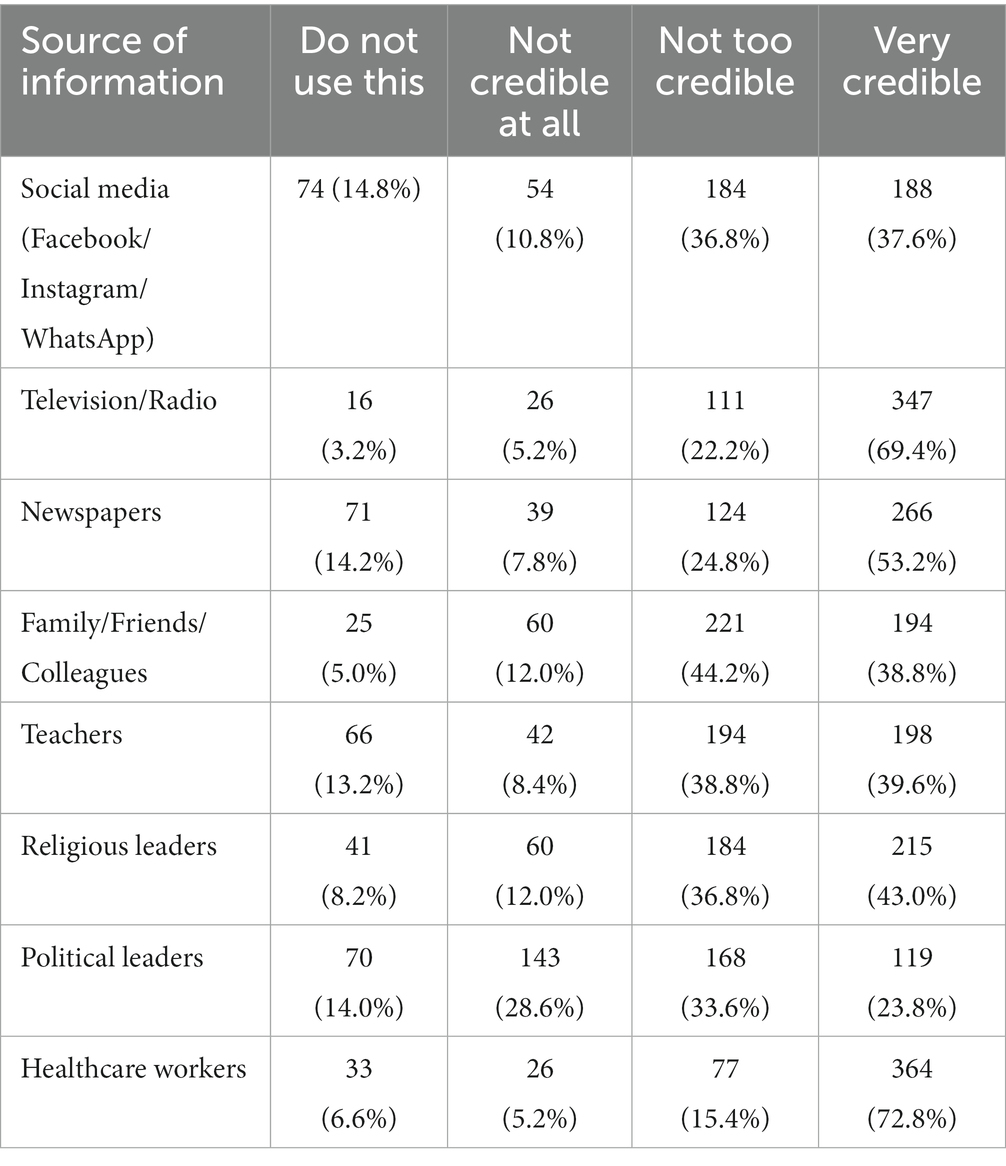
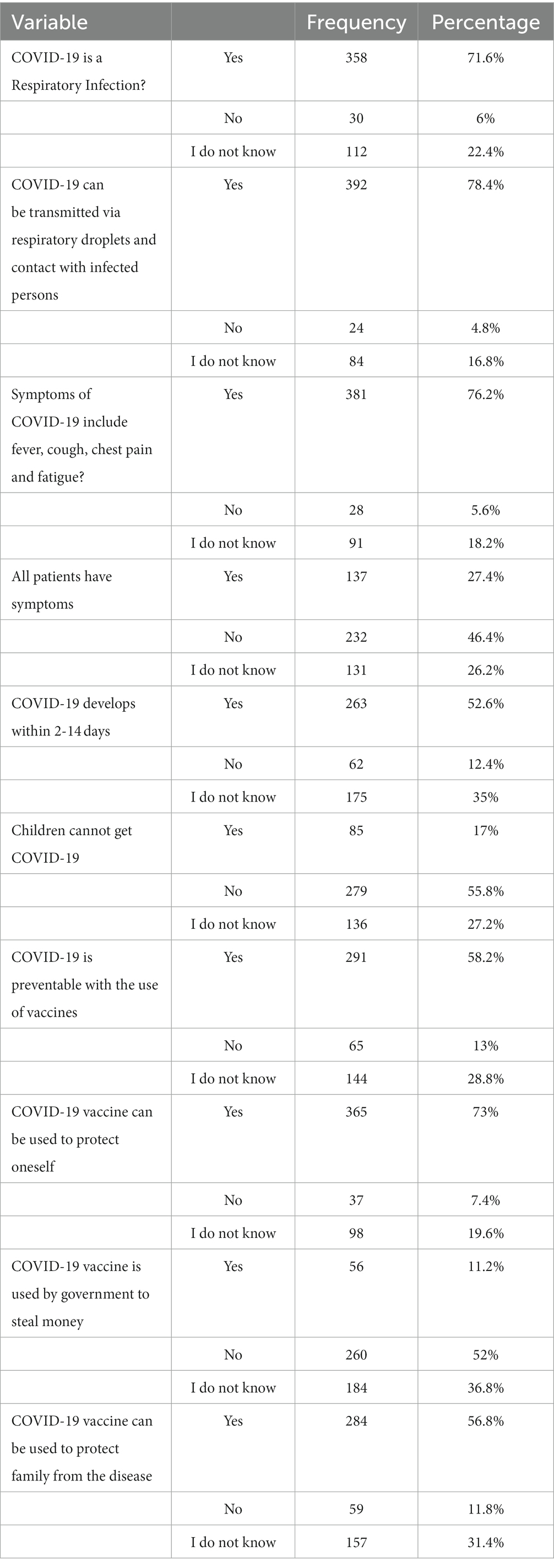
Among 500 respondents, 242 (48.4%) were willing to vaccinate their child and 285 (57%) respondents were willing to vaccinate themselves against COVID-19 disease while 23 and 18.8% were unsure of vaccinating their child and themselves against the disease (Table 1). Most parents/caregivers felt that healthcare workers were the most credible source of information regarding COVID-19, followed by mass media (Television/Radio). Social media was regarded as the least credible source of information (Table 2). Approximately half of the surveyed parents/caregivers (58.2%) knew that COVID-19 is preventable with vaccines; however, 73% believed that the COVID-19 vaccine can be used to protect oneself against severe disease. Only 56.8% of surveyed respondents believed that receiving the COVID-19 vaccine can be used to protect other family members (Table 3).
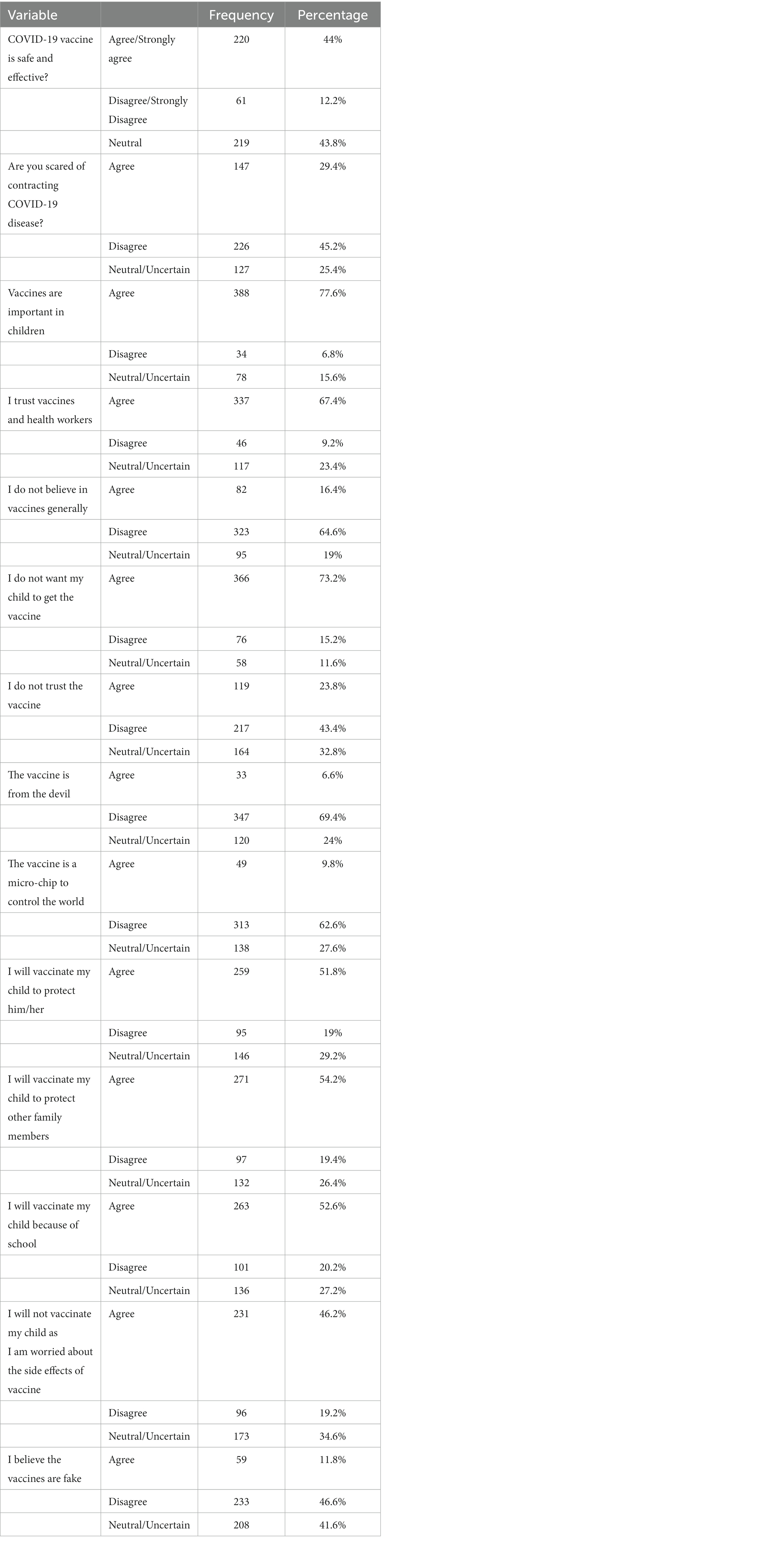
Less than half of the respondents agreed that the COVID-19 vaccine is safe and effective; however, when queried on vaccines in general, majority of them (77.6%) agreed that vaccines are generally important in children. Eighty-two respondents (16.4%) reported that they do not believe in vaccines while 231 respondents (46.2%) reported that they would not vaccinate their child as they are worried about the side effects of the vaccine (Table 4). It is noteworthy that having a good attitude toward COVID-19 vaccination was significantly associated with willingness to vaccinate oneself against the disease (p < 0.001). Likewise, respondents who had a good attitude toward COVID-19 vaccination were also found to be six times more likely to be willing to vaccinate their child compared to those who had a poor attitude toward COVID-19 vaccination, and this relationship was statistically significant.
Willingness to vaccinate self was strongly associated with willingness to vaccinate their child (p < 0.001). Only 0.5% of those who did not want to vaccinate themselves were willing to vaccinate their children while 84.6% of those willing to vaccinate themselves were willing to vaccinate their children. Good knowledge and attitude were also strongly associated with willingness to vaccinate children (p < 0.001 and p < 0.001 respectively) (Table 5).
Willingness to vaccinate self was strongly associated with willingness to vaccinate their child. Only 0.5% of those who did not want to vaccinate themselves were willing to vaccinate their children while 84.6% of those willing to vaccinate themselves were willing to vaccinate their children. Good knowledge and attitude were also strongly associated with willingness to vaccinate children (Table 5).
Univariate analysis also showed that age greater than 40 years, male gender, knowledge of a person previously diagnosed with COVID-19, being from Southern Nigeria, having good knowledge of COVID-19 disease and vaccine, having good attitude toward COVID-19 vaccination, presence of perceived risk of COVID-19 infection for themselves and risk of infection for their child, knowledge of someone who had gotten vaccinated and willingness to vaccinate self were significantly associated with higher odds of parental vaccine acceptability. After adjusting for covariates, willingness to vaccinate self, good attitude and age greater than 40 years were still associated with higher odds of vaccine acceptance. Compared to those unwilling to vaccinate themselves, those who were willing to receive the vaccine were a thousand times more likely to vaccinate their child [AOR: 1016.81; 95% CI = (128.51–8045.60)]. People aged greater than 40 years and those with good attitude were twice more likely and six times more likely to accept the vaccine than those aged younger than 40 years [AOR: 2.56; 95% CI = (1.14–5.76)], and those with bad attitude, respectively [AOR: 6.21; 95% CI = (2.83–13.64)] (Table 6).
Discussion
Our study showed that less than half of Nigerian parents are willing to vaccinate their children against COVID-19. This is much lower than what obtains in high income countries (21, 22). Bianco et al. (21) found that 82% of parents surveyed in Italy were willing to vaccinate their children against COVID-19 while Goldman et al. (22) found that 61.1% of parents surveyed in Canada were willing to vaccinate their child. We found that willingness to vaccinate self was a strong predictor of willingness to vaccinate their children, which is similar to previous findings (1, 23–25). However, more than one-tenth of respondents who were willing to vaccinate themselves were still not willing to vaccinate their children, alluding to the need for intensified parental education about COVID-19 vaccine’s safety and efficacy in children to ensure uptake when it is rolled out. We also found that having good attitude toward COVID-19 vaccination and good knowledge of COVID-19 disease was associated with willingness to vaccinate their child. This is in line with findings from a similar study by Hunyh et al. that examined vaccine hesitancy amongst the general population and parents (23).
In our study, older parents/caregivers aged greater than 40 years were more likely to vaccinate their child against COVID-19, similar to previous findings (2, 26). In a scoping review that summarized the evidence on vaccine hesitancy in Africa, it was reported that being a male was associated with positive attitude toward the vaccine (27). Our study also showed that men were more likely to vaccinate their child, similar to previous studies that have reported women to be less likely to be willing to vaccinate their child (1, 28). Gender disparities across various sectors of the economy in Nigeria, characterized by lower rates of female labor force participation and inadequate investment in women’s human capital, may account for the greater likelihood of men vaccinating their children compared to women (29). This disparity translates to men having enhanced access to healthcare information, and as such, may be a key factor responsible for their increased inclination toward vaccinating their children. In order to convince men who are disinclined to vaccinate their children, healthcare providers should be encouraged to employ diverse strategies such as targeted educational interventions via social media and inclusive involvement of fathers in the vaccination decision-making process for children from infancy. We believe this may be due to fear of adverse side effect of the virus amongst women. Further research to investigate specific cause of this gender difference should be done and public health professionals should develop gender-specific messages to promote vaccine acceptance amongst women.
Interestingly, the present study did not find a significant relationship between level of education, marital status, and willingness to vaccinate children. This contrasts with previous findings that identified that parents with secondary or lower education and those who were single were more willing to vaccinate their child against COVID-19 (21, 30). Padhi et al. (25) in their study reported conflicting findings that people with higher levels of education were more willing to vaccinate their child (25). However, this was not observed in our study; this may be because our surveyed population mainly consisted of young parents age less than 40 years. This inconsistency has been previously reported when evaluating the educational level of parents and intention to vaccinate; hence it is possible that education may not always be a key determinant of willingness to accept vaccine (19).
In addition to the previously discussed sociodemographic factors related to parental willingness to vaccinate their child, we also investigated the role of the perceived risk of COVID-19 infection. Past research has shown that people who perceived they or their child were at risk of getting infected with COVID-19 were more likely to be willing to vaccinate their child (31, 32). In this present study, we also found that parents who perceived themselves or their child could get infected with the SARS-CoV-2 virus were more willing to accept the vaccine. Majority of our respondents found healthcare workers to be the most credible source of information regarding COVID-19. Public health campaigns aiming to improve willingness need to find ways to tailor their message using healthcare workers for community outreaches and campaigns on mass media platforms. Future research should investigate the impact of information sources on parental vaccination intention.
Strength and limitations
The strength of this study is that it was a nationwide survey of parents and caregivers with children in Nigeria. The COVID-19 vaccine was recently approved for use among 16- and 17-year-old Nigerian children for educational and travel purposes, and it is likely that in the light of the recent fear of the fifth wave of the virus, the vaccine may soon be expanded to include other children older than 12 years. Hence, the findings of our survey will be useful to guiding public health professionals and other stakeholders on targeted campaigns to promote vaccine uptake amongst Nigerian children.
However, our findings should be interpreted in the light of certain limitations. Firstly, it was an internet-based survey and, as such is subject to selection bias. People who may have participated are internet-savvy and are likely to be more educated than the average Nigerian and as such, the generalizability of our findings is limited. Further research using the identified factors related to vaccine acceptability should consider targeting people with no access to the internet. Secondly, this was a cross-sectional survey, and we cannot infer causality for the reported associations. Third, according to the data collected, respondents that took this survey were mostly from southern Nigeria. Northern Nigeria was the least represented and seeing as vaccine hesitancy is rifer in that region, it is possible that our findings may not be applicable to parents and caregivers in that part of Nigeria. Further research to investigate their willingness to accept COVID-19 vaccine for their children and associated factors is recommended. Fourth, our study did not explore the impact of co-morbidities on parental willingness. Studies investigating the role of co-morbidities as a determinant in vaccine acceptance have reported conflicting findings. While some have shown that parents were less willing to vaccinate a child with co-morbidities (23), others have shown parent’s being more willing to vaccinate a child with co-morbidities (33). These studies have mostly been done in high income countries and as such, there is a need to replicate it in the African population. Lastly, our study did not investigate the impact of the various types of information sources on parental vaccination intention and as such, we cannot determine whether it influences parental decision.
Conclusion
The present study investigated the knowledge, attitude, and willingness of Nigerian parents to vaccinate their children against COVID-19 disease. It was shown that less than half of parents were willing to vaccinate their child. We found that willingness to vaccinate self, being aged greater than 40 years and a good attitude toward COVID-19 vaccine were significant predictors of vaccine acceptability. In the context of expanding COVID-19 vaccine access to children in the future, the results point to the importance of considering these factors in the design of evidence-based vaccine promotion campaigns targeted toward improving uptake.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
AA, CA, AI, TD, TK, BR, MA, OO, YS, and AR: idea, design, and editing. AA, CA, AI, TD, and AR: prepared the questionnaires. AA, CA, and AI: analyzes. All authors collected the data, wrote the draft, and approved the final draft.
Funding
This study was funded by the Neo Child Initiative, Lagos, Nigeria.
Acknowledgments
We would like to acknowledge all the core team members and volunteers of the Neo Child Initiative, Lagos, Nigeria for their contribution toward this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Horiuchi, S, Sakamoto, H, Abe, SK, Shinohara, R, Kushima, M, Otawa, S, et al. Factors of parental COVID-19 vaccine hesitancy: a cross sectional study in Japan. PLoS One. (2021) 16:e0261121. doi: 10.1371/journal.pone.0261121
2. Al-Mustapha, AI, Okechukwu, O, Olayinka, A, Muhammed, OR, Oyewo, M, Owoicho, SA, et al. A national survey of COVID-19 vaccine acceptance in Nigeria. Vaccine. (2022) 40:4726–31. doi: 10.1016/j.vaccine.2022.06.050
3. Worldometer. COVID - Coronavirus Statistics – Worldometer. (2023). Available at: https://www.worldometers.info/coronavirus/#countries (Accessed March 10, 2023).
4. Worldometer. Nigeria COVID - Coronavirus Statistics – Worldometer. (2023). Available at: https://www.worldometers.info/coronavirus/country/nigeria/ (Accessed March 10, 2023).
5. Nathanielsz, J, Toh, ZQ, Do, LAH, Mulholland, K, and Licciardi, PV. SARS-CoV-2 infection in children and implications for vaccination. Pediatr Res. (2022) 93:1177–87. doi: 10.1038/s41390-022-02254-x
6. Ozoh, OB, Akinkugbe, AO, Olukoya, MA, and Adetifa, IMO. Enablers and barriers to COVID-19 vaccine uptake in an urban slum in Lagos, Nigeria: informing vaccine engagement strategies for the marginalized. Int Health. (2023):ihad009. doi: 10.1093/inthealth/ihad009
7. Bartholomew, DC, Nwaigwe, CC, Orumie, UC, and Nwafor, GO. Intervention analysis of COVID-19 vaccination in Nigeria: the Naive solution versus interrupted time series. Ann Data Sci. (2023) 19:1–26. doi: 10.1007/s40745-023-00462-8
8. Sam-Agudu, NA, Quakyi, NK, Masekela, R, Zumla, A, and Nachega, JB. Children and adolescents in African countries should also be vaccinated for COVID-19. BMJ Glob Health. (2022) 7:e008315. doi: 10.1136/bmjgh-2021-008315
9. Online, Tribune. COVID-19: over two million teenagers already vaccinated in Nigeria — Shuaib, NPHDA executive director. Tribune, (2023). Available at: https://tribuneonlineng.com/covid-19-over-two-million-teenagers-already-vaccinated-in-nigeria-shuaib-nphda-executive-director/ (Accessed March 1, 2023).
10. UNESCO. Nigeria. [Internet]. (2016). Available at: http://uis.unesco.org/en/country/ng (Accessed August 16, 2022).
11. Osakuade, OW, and Anyam, NV. Major considerations in vaccinating children in Africa against COVID-19. Vaccine X. (2022) 12:100199. doi: 10.1016/j.jvacx.2022.100199
12. Galanis, P, Vraka, I, Siskou, O, Konstantakopoulou, O, Katsiroumpa, A, and Kaitelidou, D. Willingness, refusal and influential factors of parents to vaccinate their children against the COVID-19: a systematic review and meta-analysis. Prev Med. (2022) 157:106994. doi: 10.1016/j.ypmed.2022.106994
13. Olu-Abiodun, O, Abiodun, O, and Okafor, N. COVID-19 vaccination in Nigeria: a rapid review of vaccine acceptance rate and the associated factors. PLoS One. (2022) 17:e0267691. doi: 10.1371/journal.pone.0267691
14. Impact Africa Summit. The neo child initiative. Impact Africa Summit Impact Africa Summit. (2020). Available at: https://www.impactafricasummit.org/the-neo-child-initiative/ (Accessed March 1, 2023).
15. Zhang, KC, Fang, Y, Cao, H, Chen, H, Hu, T, Chen, YQ, et al. Parental acceptability of COVID-19 vaccination for children under the age of 18 years: cross-sectional Online survey. JMIR Pediatr Parent. (2020) 3:e24827. doi: 10.2196/24827
16. Taherdoost, H. Determining sample size; how to calculate survey sample size. Int. J. Econ. Manag. (2017). 2:237–9.
17. Bell, S, Clarke, R, Mounier-Jack, S, Walker, JL, and Paterson, P. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: a multi-methods study in England. Vaccine. (2020) 38:7789–98. doi: 10.1016/j.vaccine.2020.10.027
18. Al-Hanawi, MK, Angawi, K, Alshareef, N, Qattan, AMN, Helmy, HZ, Abudawood, Y, et al. Knowledge, attitude and practice toward COVID-19 among the public in the Kingdom of Saudi Arabia: a cross-sectional study. Front Pub Health. (2020) 8. doi: 10.3389/fpubh.2020.00217
19. Iloanusi, NJR, Iloanusi, S, Mgbere, O, Ajayi, A, and Essien, E. Covid-19 related knowledge, attitude and practices in a Southeastern city in Nigeria: a cross-sectional surve. (2020). Available at: https://europepmc.org/article/PPR/PPR243167 (Accessed April 7, 2023).
20. Ehoche, EE, Adejoh, J, Idoko, J, and Madu, C. Preliminary survey on Knowledge, attitudes, and practices about the COVID-19 pandemic among residents in north Central Nigeria. Borneo J Pharm. (2020) 3:121–9. doi: 10.33084/bjop.v3iSpecial-1.1413
21. Bianco, A, Della Polla, G, Angelillo, S, Pelullo, CP, Licata, F, and Angelillo, IF. Parental COVID-19 vaccine hesitancy: a cross-sectional survey in Italy. Expert Rev Vacc. (2022) 21:541–7. doi: 10.1080/14760584.2022.2023013
22. Goldman, RD, Krupik, D, Ali, S, Mater, A, Hall, JE, Bone, JN, et al. Caregiver willingness to vaccinate their children against COVID-19 after adult vaccine approval. Int J Environ Res Public Health. (2021) 18:10224. doi: 10.3390/ijerph181910224
23. Huynh, G, Nguyen, HTN, Van Tran, K, Le An, P, and Tran, TD. Determinants of COVID-19 vaccine hesitancy among parents in Ho Chi Minh City. Vietnam Postgrad Med. (2022) 134:303–8. doi: 10.1080/00325481.2022.2044142
24. Ruiz, JB, and Bell, RA. Parental COVID-19 vaccine hesitancy in the United States. Public Health Rep. (2022) 137:1162–9. doi: 10.1177/00333549221114346
25. Padhi, BK, Satapathy, P, Rajagopal, V, Rustagi, N, Vij, J, Jain, L, et al. Parents’ perceptions and intention to vaccinate their children against COVID-19: results from a cross-sectional National Survey in India. Front Med. (2022) 9:806702. doi: 10.3389/fmed.2022.806702
26. Lazarus, JV, Ratzan, SC, Palayew, A, Gostin, LO, Larson, HJ, Rabin, K, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. (2021) 27:225–8. doi: 10.1038/s41591-020-1124-9
27. Ackah, BBB, Woo, M, Stallwood, L, Fazal, ZA, Okpani, A, Ukah, UV, et al. COVID-19 vaccine hesitancy in Africa: a scoping review. Glob Health Res Policy. (2022) 7:21. doi: 10.1186/s41256-022-00255-1
28. Yigit, M, Ozkaya-Parlakay, A, and Senel, E. Evaluation of COVID-19 vaccine refusal in parents. Pediatr Infect Dis J. (2021) 40:e134–6. doi: 10.1097/INF.0000000000003042
29. Ewubare, DB, and Ogbuagu, AR. Unemployment rate, gender inequality and economic growth in Nigeria “A short-run impact analysis”. Glob J Hum Res Manag. (2017) 5:12–41.
30. Ng, DLC, Gan, GG, Chai, CS, Anuar, NAB, Sindeh, W, Chua, WJ, et al. The willingness of parents to vaccinate their children younger than 12 years against COVID-19: a cross-sectional study in Malaysia. BMC Public Health. (2022) 22:1265. doi: 10.1186/s12889-022-13682-z
31. Miraglia del Giudice, G, Napoli, A, Corea, F, Folcarelli, L, and Angelillo, IF. Evaluating COVID-19 vaccine willingness and hesitancy among parents of children aged 5–11 years with chronic conditions in Italy. Vaccine. (2022) 10:396. doi: 10.3390/vaccines10030396
32. Lee, H, Choe, YJ, Kim, S, Cho, HK, Choi, EH, Lee, J, et al. Attitude and acceptance of COVID-19 vaccine in parents and adolescents: a nationwide survey. J Adolesc Health. (2022) 71:164–71. doi: 10.1016/j.jadohealth.2022.05.018
Keywords: COVID-19, vaccination, children, parent, willingness, Nigeria
Citation: Ajose A, Akinde C, Ilo A, Durojaiye T, Shittu Y, Kadiri T, Raheem B, Alamutu MK, Ojo O and Roberts AA (2023) Nigerian parents and caregivers knowledge, attitude and willingness to vaccinate their children against COVID-19. Front. Public Health. 11:1047285. doi: 10.3389/fpubh.2023.1047285
Edited by:
Goran Tešović, University of Zagreb, CroatiaCopyright © 2023 Ajose, Akinde, Ilo, Durojaiye, Shittu, Kadiri, Raheem, Alamutu, Ojo and Roberts. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Azeezat Ajose, YWpvc2VhemVlemF0QGdtYWlsLmNvbQ==
 Azeezat Ajose
Azeezat Ajose Cassandra Akinde
Cassandra Akinde Azizat Ilo
Azizat Ilo Tobi Durojaiye
Tobi Durojaiye Yusuf Shittu
Yusuf Shittu Tolani Kadiri1
Tolani Kadiri1 Bisola Raheem
Bisola Raheem Mujidat Kehinde Alamutu
Mujidat Kehinde Alamutu Olamide Ojo
Olamide Ojo