- 1Department of Health Policy and Management, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
- 2Lineberger Comprehensive Cancer Center, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
- 3Patient Advocate Foundation, Hampton, VA, United States
- 4Division of Hematology and Oncology, Department of Medicine, University of Alabama-Birmingham, Birmingham, AL, United States
Background: Despite the use of interventions (e.g., monetary incentives, educational campaigns, on-site workplace vaccination) to increase COVID-19 vaccination, differences in uptake persist by poverty level, insurance status, geography, race, and ethnicity, suggesting that these interventions may not be adequately addressing the barriers faced by these populations. Among a sample of resource-limited individuals with chronic illnesses, we (1) described the prevalence of different types of barriers to the COVID-19 vaccination and (2) identified associations between patients' sociodemographic characteristics and barriers to vaccination.
Methods: We surveyed a national sample of patients with chronic illness and demonstrated healthcare affordability and/or access challenges about barriers to COVID-19 vaccination in July 2021. We categorized participant responses into cost, transportation, informational, and attitudinal barrier domains and assessed the prevalence of each domain, both overall and by self-reported vaccination status. Using logistic regression models, we examined unadjusted and adjusted associations between respondent characteristics (sociodemographic, geographic, and healthcare access) and self-reported barriers to vaccination.
Results: Of 1,342 respondents in the analytic sample, 20% (264/1,342) reported informational barriers and 9% (126/1,342) reported attitudinal barriers to COVID-19 vaccination. Transportation and cost barriers were reported much less commonly, by only 1.1% (15/1,342) and 0.7% (10/1,342) of the sample, respectively. Controlling for all other characteristics, respondents with either a specialist as their usual source of care or no usual source of care had an 8.4 (95% CI: 1.7–15.1) and 18.1 (95% CI: 4.3–32.0) percentage point higher predicted probability, respectively, of reporting informational barriers to care. Compared to females, males had an 8.4% point (95% CI: 5.5–11.4) lower predicted probability of reporting attitudinal barriers. Only attitudinal barriers were associated with COVID-19 vaccine uptake.
Conclusion: Among a sample of adults with chronic illnesses who had received financial assistance and case management services from a national non-profit, informational and attitudinal barriers were more commonly reported than logistical or structural access barriers (i.e., transportation and cost barriers). Interventions should target attitudinal barriers among patients with chronic illness, who may have particular concerns about the interaction of the vaccine with ongoing medical care. Additionally, interventions targeting informational barriers are particularly needed among individuals without a usual source of care.
Introduction
As of January 2023, more than 30% of individuals in the US have not been fully vaccinated against COVID-19; furthermore, 84% have not received a booster (1). Despite the use of interventions (e.g., monetary incentives, educational campaigns, on-site workplace vaccination) to increase COVID-19 vaccine rates, differences in uptake persist by poverty level, geography, and race in the United States (2). Substantial geographic disparities exist in COVID-19 vaccination uptake at the county-level, with rural areas having 16% lower vaccination than urban areas (3). Similarly, poorer, more disadvantaged counties have a 32% lower vaccination rate than their higher socioeconomic counterparts (4). Despite experiencing higher COVID-19 incidence and mortality due to a host of structural inequities, Black and Hispanic individuals have been consistently shown to be less likely to be vaccinated than White individuals (5–8). These disparities suggest that interventions to increase vaccine uptake may not be adequately addressing the barriers faced by individuals already underserved by the US healthcare system.
Barriers to vaccination may be informational, attitudinal, or structural in nature. Attitudinal barriers, including vaccine hesitancy, have been a major deterrent to COVID-19 vaccination uptake. A scoping review on COVID-19 vaccine hesitancy found that common vaccine-specific factors associated with increased vaccine hesitancy included beliefs that vaccines are not safe/effective and concerns about the rapid development of COVID-19 vaccines (9). Disparate populations, including people of color and those without insurance, often face structural, access-related barriers, further reducing their vaccine uptake (10, 11). For example, despite the execution of Operation Warp Speed, which aimed to make the vaccine widely available to the public at no cost (12), historically marginalized and resource-limited communities continue to face access barriers (8, 11, 13). In a study of over 87,000 participants, Black individuals had significantly lower vaccine uptake, even among those willing to receive the vaccine (8). Qualitative studies have pointed to access-related concerns related to cost and insurance status, language barriers, and the unavailability and logistical complexities of vaccine appointments (11, 13).
Approximately 1 in 6 adults in the US have a chronic health condition (14). Chronic diseases (e.g., cancer, HIV, diabetes, heart disease, hypertension, respiratory disease), by definition, last longer than a year, are functionally debilitating, and require constant monitoring and/or treatment (15). Furthermore, individuals with chronic illnesses that have not have been vaccinated are at heightened risk of experiencing complications, and potential mortality, due to COVID-19 (16). As such, vaccine uptake is a particularly critical preventive measure for this population; in the US, it is estimated that over 32% of individuals with HIV are unvaccinated (17). In other countries, vaccination rates among individuals with cancer, diabetes, and respiratory diseases range from 8 to 39% (18–20).
Several previous studies have described the attitudinal and access barriers to COVID-19 vaccine uptake faced by the general population (11, 21, 22). Outside of the US, individuals with chronic illnesses have pointed to concerns about adverse events, disease decline, and vaccine safety as reasons for vaccine hesitancy (23, 24). In the US, it is critical to determine which types of barriers are faced by individuals with chronic illness to develop targeted and effective interventions (10, 11). In the current study, among a sample of resource-limited individuals with chronic illnesses, we (1) describe the prevalence of different types of barriers to COVID-19 vaccination and (2) identify associations between socio-demographic characteristics and barriers to vaccination.
Methods
We analyzed cross-sectional survey data from the COVID-19 Impact Survey series collected by Patient Advocate Foundation (PAF) in July 2021. PAF is a national non-profit organization providing financial assistance and case management services to individuals with chronic or life-threatening illnesses, such as cancer, HIV/AIDS, and cardiovascular conditions. PAF emailed the survey to eligible individuals, followed by two reminder emails over the course of 3 weeks.
Eligible individuals had previously received services from PAF (between June 2019 and June 2020) and had opted in to receive survey communications. As PAF provides services to patients living throughout the United States, this sample aims to represent a national sample of patients with limited financial or physical resources. Because this was the third in a series of COVID-19-related surveys, PAF only sent the survey to respondents who completed the first survey, which was administered between May–July 2020. Of the 4,151 individuals who completed the first survey, 1,373 (33%) completed the survey used for this analysis. After excluding 31 individuals (2%) due to missing data for predictor variables included in the multivariable analysis with <10 missing responses, our final analytic sample included 1,342 participants. Supplemental Table 1 includes a comparison of the demographic characteristics between the analytic cohort and the overall cohort of patients served by PAF between June 2019 and June 2020. Compared to the overall cohort of patients served by PAF, the analytic cohort included a higher proportion of individuals who were 36–55 years of age, Non-Hispanic White or Other race, and income ≥$24,000. The University of North Carolina Institutional Review Board deemed this secondary analysis to be non-human subjects research.
Analyses
Our primary outcome, barriers to COVID-19 vaccination, was measured using the survey question, “Did you have any trouble accessing or receiving the COVID-19 vaccine for any of the following reasons?” which was asked of all participants, regardless of vaccination status. Participants could select multiple response options which we categorized into four domains; specifically, (1) cost barriers included “concerns about cost” and “no insurance,” (2) transportation barriers included “no transportation to get to appointment,” (3) information barriers included “not able to find an available appointment,” “not sure how to make an appointment or where to get vaccinated,” and “not eligible for vaccination,” and (4) attitudinal barriers included “afraid or nervous about the vaccine” and “no time or too busy.” Participants could also select “Other,” which prompted a free-text response. Free-text other responses were coded into these domains by two independent coders (LPS, CBB), and discrepancies were resolved by a third reviewer (SBW). For example, responses such as not wanting to receive the vaccine were coded as attitudinal barriers. Each barrier (i.e., cost, transportation, information, attitudinal) was defined as a binary indicator of whether one or more barriers in each domain was reported.
We assessed the prevalence of each barrier to vaccination, both overall and by self-reported vaccination status (at least one COVID-19 vaccine dose vs. no doses). For all barrier domains with sufficient prevalence in the sample (>10%), we then used logistic regression models to assess unadjusted and adjusted differences between respondent characteristics hypothesized to influence COVID-19 vaccine uptake (25). P-values were calculated using Chi-squared tests or Fisher-Freeman Halton tests [for covariates with more than 2 categories and cell sizes smaller than 5 (26)]. Model fit was assessed based on the Pseudo R2 and using the Hosmer and Lemeshow's goodness-of-fit test (27–29). Covariates included in analyses were based on Andersen's model of health care utilization (30, 31) and previous literature examining covariates associated with COVID-19 vaccine uptake acceptance and uptake (6, 32–34). Sociodemographic characteristics included self-reported age, sex, race/ethnicity, and household income. Geographic characteristics included rurality [dichotomized based on the Rural-Urban Commuting Area codes (35): Rural (≥4), Non-rural (<4)] and region of residence. Characteristics related to healthcare access included health insurance coverage and usual source of care. We detected no collinearity in the final models.
Using logistic regression results, we calculated the average marginal effect for each covariate, which can be interpreted as the average difference in the predicted probability of each outcome, holding all other covariates constant, across all observations in the analytic sample. Standard errors and confidence intervals (CIs) for all marginal effects were estimated by applying the Delta method using the “margins” command in STATA 16.1 (StataCorp, College Station, TX).
Results
Of the 1,342 participants in the analytic sample, the majority were female (58%) and Non-Hispanic White (61%). Though only five percent of participants were between the ages of 19 and 35 years, participant ages were evenly distributed between 36–55 years (31%), 56–65 years (30%), and over 65 years (34%). The majority of respondents were insured by Medicare (64%), had an annual household income less than $48,000 (75%), and reported having a general practitioner as their usual source of care (84%) (Table 1). Overall, 86% of participants self-reported receiving one or more doses of the COVID-19 vaccine, with a higher prevalence among participants over 65 years of age vs. ≤65 (96 vs. 82%) and among Non-Hispanic White participants vs. Black and Hispanic or Latinx (89 vs. 83% vs. 83%) (Supplemental Table 2).
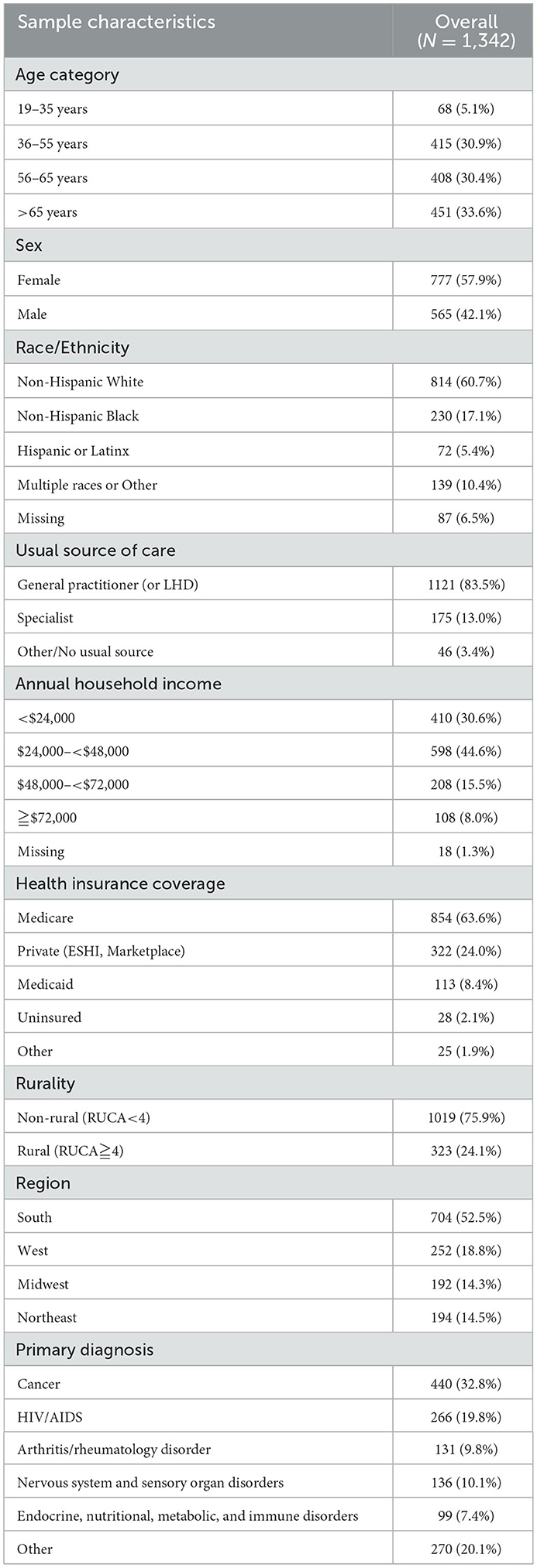
Table 1. Descriptive statistics from a sample of patients with chronic or life-threatening illness who received assistance from a national non-profit.
Informational barriers were reported most commonly by 20% (264/1,342) of the sample, followed by attitudinal barriers (9%, 126/1,342). Transportation and cost barriers were reported much less commonly, by only 1.1% (15/1,342) and 0.7% (10/1,342) of the sample, respectively. Only attitudinal barriers were associated with COVID-19 vaccine uptake (p < 0.001); compared to only 4% (41/1160) of the vaccinated sample, 47% of unvaccinated respondents (85/182) reported attitudinal barriers (Figure 1).
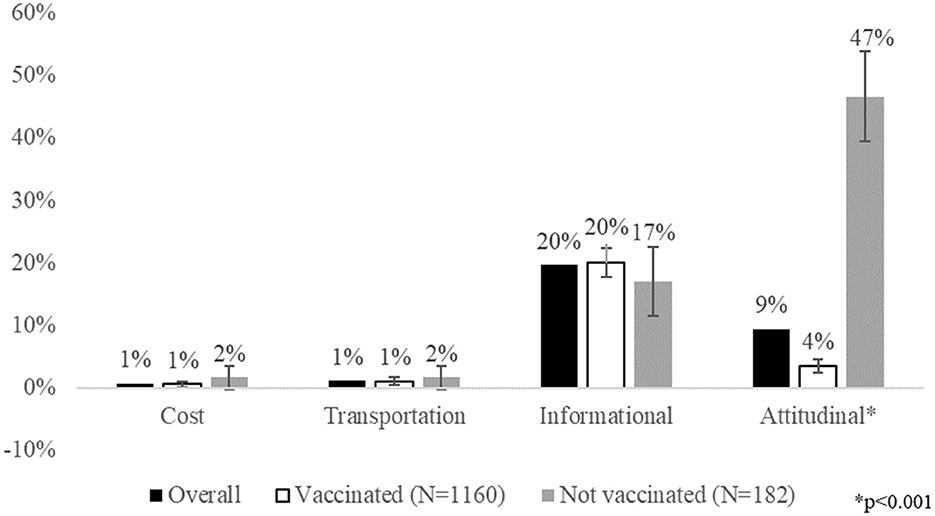
Figure 1. Patient-reported barriers to COVID-19 vaccination by vaccination status (N = 1,342). It shows the prevalence of patient-reported barriers to COVID-19 vaccination, both overall and by vaccination status. Cost barriers include concerns about cost of the vaccine itself and not having insurance. Transportation barriers refer to concerns about getting to a vaccine appointment. Informational barriers include not being able to find an available appointment, not being sure how to make an appointment or where to get vaccinated, and questions about eligibility for the vaccine. Attitudinal barriers include being afraid or nervous about the vaccine, not having time to get the vaccine, or not wanting the vaccine. Attitudinal barriers were statistically significantly associated with vaccine uptake (*p < 0.001).
In unadjusted analysis, only race/ethnicity and usual source of care were associated with reporting informational barriers. Informational barriers were more commonly reported by Non-Hispanic White respondents (24%) compared to Non-Hispanic Black (6%) and Hispanic or Latinx (8%) respondents. Whereas informational barriers were reported by only 18% of respondents with a general practitioner as their usual source of care, informational barriers were reported more commonly by respondents with a specialist as their usual source of care (28%) and respondents with no usual source of care (37%) (Table 2). These differences remained in multivariable analysis. Controlling for all other respondent characteristics, Non-Hispanic Black respondents, compared to Non-Hispanic White respondents, had a 17.7% point (95% CI: 13.3–22.1) lower predicted probability of reporting informational barriers, and Hispanic or Latinx respondents had a 15.0% point (95% CI: 7.7–22.4) lower predicted probability compared to Non-Hispanic Whites. Compared to respondents with a general practitioner as their usual source of care, respondents with a specialist had an 8.4% point (95% CI: 1.7–15.1) higher predicted probability of reporting informational barriers, and respondents without a usual source of care had an 18.1 (95% CI: 4.3–32.0) higher predicted probability (Table 2). Additionally, the Pseudo R2 was 0.0585, and the Hosmer and Lemeshow's goodness-of-fit test was insignificant (p = 0.4926), indicating good model fit.
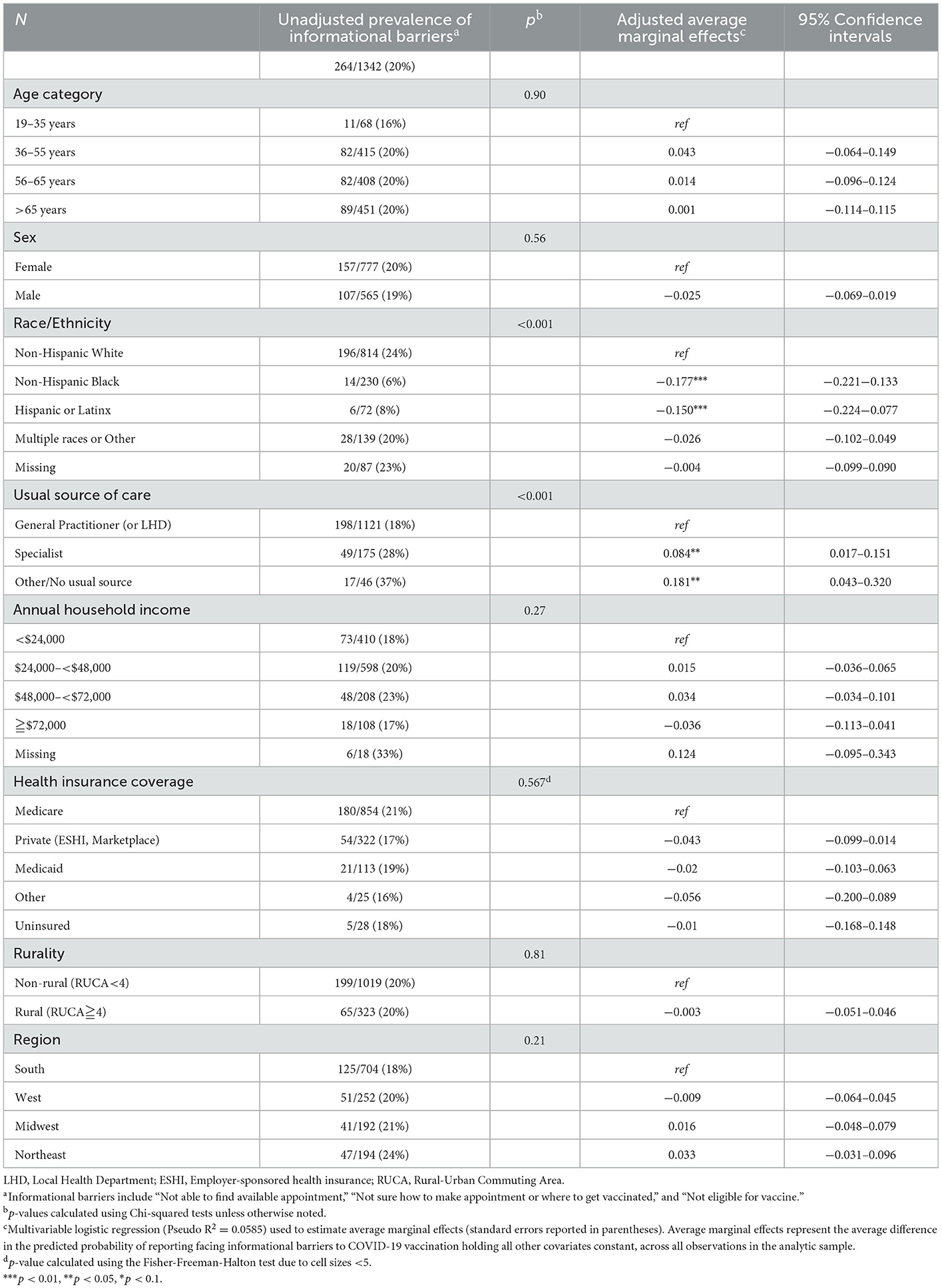
Table 2. Unadjusted and adjusted associations between socio-demographic characteristics and informational barriers to COVID-19 vaccination (N = 1,342).
In unadjusted analysis, attitudinal barriers were associated with age, sex, race/ethnicity, and health insurance coverage (Table 3). However, after controlling for all sociodemographic and healthcare access characteristics, most associations were attenuated. Compared to females, males had an 8.4% point (95% CI: 5.5–11.4) lower predicted probability of reporting attitudinal barriers. Additionally, respondents reporting multiple races or other race/ethnicity had a 6.6% point (95% CI: 0.6–12.5) higher predicted probability of reporting attitudinal barriers compared to Non-Hispanic White respondents. Though only borderline significant, respondents over 65 years of age (compared to respondents between 19–35 years of age) had a 7.0% point (95% CI: 1.3–15.3) lower predicted probability of reporting attitudinal barriers, and uninsured respondents (compared to Medicare-insured) had a 10.9% point (95% CI: −1.9–23.7) higher predicted probability of reporting attitudinal barriers (Table 3). For this multivariable analysis, the Pseudo R2 was 0.1083, and the Hosmer and Lemeshow's goodness-of-fit test was insignificant (p = 0.338), indicating good model fit.
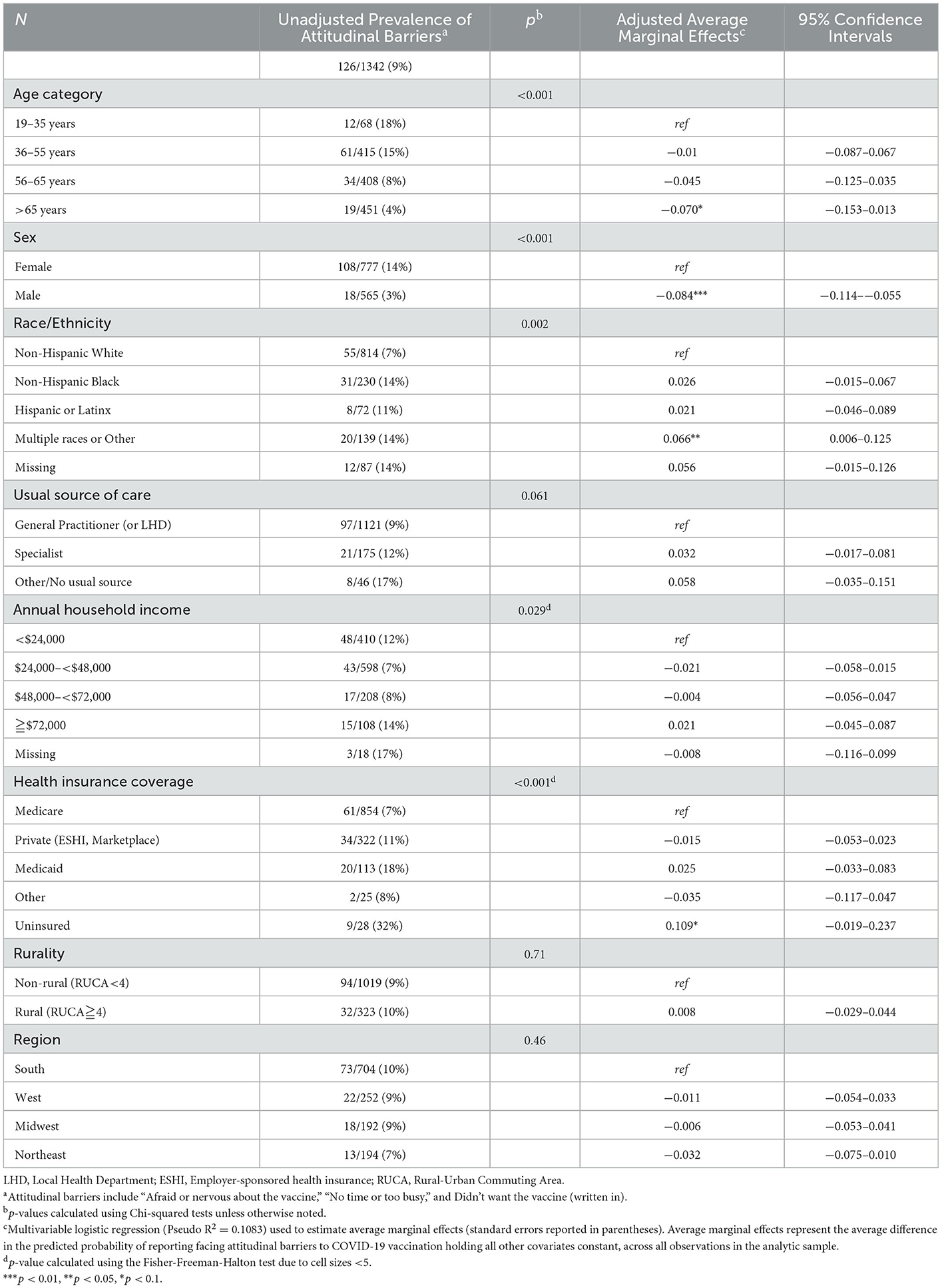
Table 3. Unadjusted and adjusted associations between socio-demographic characteristics and attitudinal barriers to COVID-19 vaccination (N = 1,342).
In sensitivity analyses, we explored the effect of adding Covid-19 vaccine uptake as a covariate in the multivariable models for both informational and attitudinal barriers. On the whole, adding vaccination status did not change the results of the associations between patient characteristics and vaccine barriers. As shown in Figure 1 as well, vaccination status was statistically significantly associated with reporting attitudinal barriers but not informational barriers (Supplemental Table 3).
Discussion
Among a sample of resource-limited adults with chronic illnesses, informational and attitudinal barriers were more commonly reported than structural access barriers (i.e., transportation and cost barriers). Attitudinal barriers were associated with lower vaccine uptake. In particular, attitudinal barriers were more prevalent among females (compared to males) and uninsured (compared to insured individuals). Interestingly, Black and Latinx or Hispanic individuals were less likely to face informational barriers than their White counterparts. Participants with either a specialist as their usual source of care or no usual source of care were more likely to report informational barriers compared to those whose usual source of care was a general practitioner. As ongoing COVID-19 vaccination continues to be a primary defense against the pandemic, our findings aim to inform efforts to develop interventions that are needed to overcome vaccine hesitancy and improve access to vaccine uptake in the national response to COVID-19 (36).
Even prior to the COVID-19 pandemic, having a usual source of care has been considered essential to improving or maintaining individual's health, especially among individuals with chronic illness. Having a usual source of care facilitates timely receipt of preventative services, including immunizations (37–42), as well as fewer emergency department visits and hospital admissions (43). Among a nationally representative population, older, adult men (ages 50–64) and women (ages 40–64) with a usual source of care had, respectively, almost 10 times higher odds of receiving a Prostate Specific Antigen test and 5 times higher odds of receiving a mammogram compared with to those without a usual source of care (44). During the COVID-19 pandemic, having a usual source of care facilitated access to COVID-19 testing and treatment services (45). For example, primary care providers could directly contact patients to encourage them to vaccinate; a randomized controlled trial found that outreach via electronic secure messages and mailings from an individual's regular primary care physician increased COVID-19 vaccination rates among older Black and Latinx/Hispanic adults (46).
The rate of COVID-19 vaccination is significantly lower among Black and Hispanic or Latinx populations (5–8). Several studies suggest that this is due to vaccine hesitancy among these historically marginalized populations (32, 47, 48). Even in our study, the proportion of individuals of color reporting attitudinal barriers was higher than those reporting informational barriers; in fact, the percent Black participants reporting attitudinal barriers was more than twice the percent reporting informational barriers. While we found that Black and Hispanic/Latinx respondents were significantly less likely to report informational barriers than White respondents, this is potentially because these individuals have experienced systemic racism and consequently are less likely to receive the vaccine or to seek out information on the vaccine; in other words, they avoided facing informational barriers altogether due to mistrust of healthcare systems. Indeed, even among individuals with chronic conditions that need regular medical care, Black individuals have demonstrated high vaccine hesitancy (49). Alternatively, however, this could also be due to the success of outreach programs that specifically targeted Black and Latinx/Hispanic individuals; programs focused on equity-based vaccine allocation and community engagement have been shown to almost double vaccination rates (50). Furthermore, a recent study found that, over the course of the pandemic, the rate of vaccine hesitancy has been decreasing more rapidly among Black individuals than White individuals (29). Future research on strategies to increase COVID-19 vaccination among people of color should continue to explore the barriers faced be these populations and develop tailored, and potentially multicomponent, interventions to address the identified barriers.
About half as many uninsured U.S. adults have received the COVID-19 vaccine as insured adults (51). The U.S. Department of Health and Human Services established the COVID-19 Uninsured Program, which reimburses providers at national Medicare rates, to help uninsured individuals access COVID-19 testing, vaccinations, and treatment (52). While this program addresses access barriers, our results suggest uninsured patients are more likely to face attitudinal barriers to COVID-19 uptake. Consequently, addressing vaccine hesitancy, in addition to addressing access barriers, is needed to improve vaccine uptake among the uninsured population.
While females are more likely to practice preventative behaviors such as wearing face masks to prevent COVID-19 infections (53, 54), COVID-19 vaccine refusal is significantly higher among females than males in the U.S (33, 47, 48). A large national study of adult Americans found the odds of expressing vaccine hesitancy were 44% higher in females than males (53). Even among adults with chronic diseases, sex differences persist. A study among immunocompromised individuals found that females were more likely to express vaccine hesitancy than males (55, 56); in particular, females expressed concerns about the safety of vaccinations and were more often worried about vaccine side effects (55). With the approval of the COVID-19 vaccine for children, these results are particularly troubling, as women are more often responsible for making medical decisions for their children than men (57). These differences in COVID-19 attitudes by sex, which we also found in this study, suggest that sex- and gender-specific concerns should be addressed and targeted when educating females about vaccinations or designing vaccination campaigns.
Several limitations of this study should be noted. First, results from this study may not be generalizable to the full US population of adults with chronic illness due to the relatively low response rate of 33% and that the sample was drawn from a surveyed population who sought financial assistance or social need navigation from a national non-profit. Given the resource constraints faced by these individuals, it is possible that our estimates may be biased as these individuals may have been more susceptible to experiencing vaccine-related barriers. In contrast, their prior experience accessing resources from a national non-profit may suggest a lower likelihood of facing access barriers to vaccination. Furthermore, while our analysis included several different types of barriers, we did not explore how these barriers may have interacted or influenced one another; for example, individuals may have not even tried to make a vaccine appointment (i.e., they altogether avoided facing informational barriers) if they believed they could not afford the vaccine or have the necessary transportation to attend a vaccine clinic appointment. Future qualitative research should further explore the nuances of the relationships between different types of barriers.
At the same time, our study has several strengths. First, because PAF is a nationally-recognized organization, the study sample includes individuals from across the US. Second, in contrast to previous studies that focused on describing barriers to vaccination, the present study quantitatively expresses different types of barriers. Finally, while the majority of the literature on barriers to COVID-19 vaccination have focused on the general population, this study is the first to examine barriers among those with chronic illness in the US.
Conclusion
Over 80% of the US population has received at least one dose of a COVID-19 vaccine (1). However, several rounds of booster vaccination shots have been recommended, depending on eligibility, and future booster vaccines are currently being developed. While a multitude of interventions and programs have been developed to improve vaccine uptake, in order to increase both effectiveness and efficiency of vaccine uptake, interventions should proactively tailor strategies to the most prevalent barriers encounters by target populations. In particular, our results among resource-limited individuals with chronic illness, campaigns providing information on finding and scheduling available vaccine appointments are needed for those without a usual source of care. Programs to address attitudinal barriers, particularly concerns about vaccine safety, should be targeted toward females and uninsured individuals.
Data availability statement
The datasets presented in this article are not readily available because this data is owned by Patient Advocate Foundation and is subject to a Data Use Agreement. Requests to access the datasets should be directed to Patient Advocate Foundation, https://www.patientadvocate.org/.
Author contributions
LS: conceptualization, methodology, formal analysis, and writing—original draft preparation. CB: conceptualization, methodology, writing—original draft preparation, and review and editing. RA and KG: investigation, conceptualization, and writing—review and editing. EA: data curation, conceptualization, and writing—review and editing. GR: writing—review and editing. SW: conceptualization, methodology, supervision, and writing—review and editing. All authors contributed to the article and approved the submitted version.
Funding
CB was supported by a NIH Cancer Care Quality Training Program grant, for which SW is mentor and PI, UNC-CH, Grant No. T32-CA-116339. NIH did not have any role in the study design, collection, management, analysis, interpretation of the data, writing of the manuscript, or the decision to submit the report for publication.
Conflict of interest
LS and SW have received financial support paid to their institution for unrelated work from AstraZeneca. SW has also received research grants from Pfizer paid to her institution for unrelated work.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1046515/full#supplementary-material
References
1. CDC COVID Data Tracker: Vaccinations in the US. Available online at: https://covid.cdc.gov/covid-data-tracker/#vaccinations_vacc-people-fully-percent-pop18 (accessed Jan 17, 2023).
2. COVID-19 Vaccination Strategies for Your Community|CDC. Available online at: https://www.cdc.gov/vaccines/covid-19/vaccinate-with-confidence/community.html (accessed May 19, 2022).
3. Saelee R, Zell E, Murthy BP, Castro-Roman P, Fast H, Meng L, et al. Disparities in COVID-19 vaccination coverage between urban and rural counties—United States, December 14, 2020–January 31, 2022. MMWR Morb Mortal Wkly Rep. (2022) 71:335–40. doi: 10.15585/mmwr.mm7109a2
4. Brown CC, Young SG, Pro GC. COVID-19 vaccination rates vary by community vulnerability: a county-level analysis. Vaccine. (2021) 39:4245–9. doi: 10.1016/j.vaccine.2021.06.038
5. Ndugga N, Hill L, Artiga S, Haldar S. Latest Data on COVID-19 Vaccinations by Race/Ethnicity|KFF. (2022). Available online at: https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-by-race-ethnicity/ (accessed Aug 10, 2022).
6. Baack BN, Abad N, Yankey D, Kahn KE, Razzaghi H, Brookmeyer K, et al. COVID-19 vaccination coverage and intent among adults aged 18–39 years—United States, March–May 2021. MMWR Morb Mortal Wkly Rep. (2021) 70:928–33. doi: 10.15585/mmwr.mm7025e2
7. Santibanez TA, Singleton J, Black C, Nguyen K, Hung MC, Masalovich S, et al. Sociodemographic factors associated with receipt of COVID-19 vaccination and intent to definitely get vaccinated, adults aged 18+ Years|CDC. (2021). Available online at: https://www.cdc.gov/vaccines/imz-managers/coverage/adultvaxview/pubs-resources/sociodemographic-factors-covid19-vaccination.html (accessed Aug 10, 2022).
8. Nguyen LH, Joshi AD, Drew DA, Merino J, Ma W, Lo CH, et al. Self-reported COVID-19 vaccine hesitancy and uptake among participants from different racial and ethnic groups in the United States and United Kingdom. Nat Commun. (2022) 13:1–9. doi: 10.1038/s41467-022-28200-3
9. Aw J, Seng JJB, Seah SSY, Low LL. COVID-19 vaccine hesitancy-a scoping review of literature in high-income countries. Vaccines. (2021) 9:900. doi: 10.3390/vaccines9080900
10. Abdul-Mutakabbir JC, Casey S, Jews V, King A, Simmons K, Hogue MD, et al. A three-tiered approach to address barriers to COVID-19 vaccine delivery in the Black community. Lancet Glob Heal. (2021) 9:e749. doi: 10.1016/S2214-109X(21)00099-1
11. Fisk RJ. Barriers to vaccination for coronavirus disease 2019 (COVID-19) control: experience from the United States. Glob Heal J. (2021) 5:51–5. doi: 10.1016/j.glohj.2021.02.005
12. OPERATION WARP SPEED Accelerated COVID-19 Vaccine Development Status and Efforts to Address Manufacturing Challenges Report to Congressional Addressees United States Government Accountability Office (2021).
13. Balasuriya L, Santilli A, Morone J, Ainooson J, Roy B, Njoku A, et al. COVID-19 vaccine acceptance and access among black and latinx communities. JAMA Netw Open. (2021) 4:e2128575–e212857. doi: 10.1001/jamanetworkopen.2021.28575
14. Chronic Diseases in America|CDC. Available online at: https://www.cdc.gov/chronicdisease/resources/infographic/chronic-diseases.htm (accessed Nov 15, 2022).
15. Buttorff C, Ruder T, Bauman M. Multiple Chronic Conditions in the United States. Mult Chronic Cond United States. (2017). Available online at: https://www.rand.org/pubs/tools/TL221.html doi: 10.7249/TL221 (accessed Nov 15, 2022).
16. People with Certain Medical Conditions|CDC. Available online at: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html (accessed Aug 15, 2022).
17. Tesoriero JM, Patterson W, Daskalakis D, Chicoine J, Morne J, Braunstein S, et al. Notes from the field: COVID-19 vaccination among persons living with diagnosed hiv infection—New York, October 2021. MMWR Morb Mortal Wkly Rep. (2022) 71:182–4. doi: 10.15585/mmwr.mm7105a4
18. Peng X, Gao P, Wang Q, Wu HG, Yan YL, Xia Y, et al. Prevalence and impact factors of COVID-19 vaccination hesitancy among breast cancer survivors: a multicenter cross-sectional study in China. Front Med. (2021) 8:1980. doi: 10.3389/fmed.2021.741204
19. Fu L, Wu S, Wang B, Zheng W, Sun Y, Tian T, et al. COVID-19 vaccination perception and uptake among cancer patients in Guangzhou, China. Hum Vaccin Immunother. (2022). Available online at: https://pubmed.ncbi.nlm.nih.gov/35976684/ (accessed Nov 15, 2022).
20. Wang Y, Duan L, Li M, Wang J, Yang J, Song C, et al. COVID-19 vaccine hesitancy and associated factors among diabetes patients: a cross-sectional survey in Changzhi, Shanxi, China. Vaccines. (2022) 10:129. doi: 10.3390/vaccines10010129
21. Magee L, Knights F, Mckechnie DGJ. Al-bedaery R, Razai MS. Facilitators and barriers to COVID-19 vaccination uptake among ethnic minorities: A qualitative study in primary care Ebenso BE, editor. PLoS ONE. (2022) 17:e0270504. doi: 10.1371/journal.pone.0270504
22. Jacoby KB, Hall-Clifford R, Whitney CG, Collins MH. Vaccination and vacci-notions: Understanding the barriers and facilitators of COVID-19 vaccine uptake during the 2020–21 COVID-19 pandemic. Public Heal Pract. (2022) 3:100276. doi: 10.1016/j.puhip.2022.100276
23. Campochiaro C, Trignani G, Tomelleri A, Cascinu S, Dagna L. Potential acceptance of COVID-19 vaccine in rheumatological patients: a monocentric comparative survey. Ann Rheum Dis. (2021) 80:816–7. doi: 10.1136/annrheumdis-2020-219811
24. Puteikis K, Mameniškiene R. Factors associated with covid-19 vaccine hesitancy among people with epilepsy in lithuania. Int J Environ Res Public Health. (2021) 18:4374. doi: 10.3390/ijerph18084374
25. Andersen RM. National health surveys and the behavioral model of health services use. Med Care. (2008) 46:647–53. doi: 10.1097/MLR.0b013e31817a835d
26. Ruxton GD, Neuhäuser M. Good practice in testing for an association in contingency tables. Behav Ecol Sociobiol. (2010) 649:1505–13. doi: 10.1007/s00265-010-1014-0
27. Burke PF, Masters D, Massey G. Enablers and barriers to COVID-19 vaccine uptake: an international study of perceptions and intentions. Vaccine. (2021) 39:5116–28. doi: 10.1016/j.vaccine.2021.07.056
28. Hosmer DW, Lemeshow S. Goodness of fit tests for the multiple logistic regression model. Commun Stat Theory Methods. (1980) 9:1043–69. doi: 10.1080/03610928008827941
29. Kiran T, Junaid KP, Sharma D, Jain L, Vij J, Satapathy P, et al. Sociodemographic determinants of willingness and extent to pay for COVID-19 vaccine in India. Front Public Heal. (2022) 10:1220. doi: 10.3389/fpubh.2022.870880
30. Andersen R, Davidson P. “Improving access to care in America: individual and contextual indicators,” In R. Andersen, T. Rice, J. Kominski, eds. Changing the US Health Care System: Key Issues in Health Services Policy and Management. San Francisco, CA: Jossey-Bass (2007). p. 3–31.
31. Phillips KA, Morrison KR, Andersen R, Aday LA. Understanding the context of healthcare utilization: assessing environmental and provider-related variables in the behavioral model of utilization. Health Serv Res. (1998) 33:571.
32. Ruiz JB, Bell RA. Predictors of intention to vaccinate against COVID-19: results of a nationwide survey. Vaccine. (2021) 39:1080–6. doi: 10.1016/j.vaccine.2021.01.010
33. Malik AA, McFadden SAM, Elharake J, Omer SB. Determinants of COVID-19 vaccine acceptance in the US. EClin Med. (2020) 26:100495. doi: 10.1016/j.eclinm.2020.100495
34. Nguyen KH, Anneser E, Toppo A, Allen JD, Scott Parott J, Corlin L. Disparities in national and state estimates of COVID-19 vaccination receipt and intent to vaccinate by race/ethnicity, income, and age group among adults ≥ 18 years, United States. Vaccine. (2022) 40:107–13. doi: 10.1016/j.vaccine.2021.11.040
35. USDA ERS - Rural-Urban Commuting Area Codes. Available online at: https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx (accessed Mar 23, 2021).
36. McCabe SD, Hammershaimb EA, Cheng D, Shi A, Shyr D, Shen S, et al. Unraveling attributes of COVID-19 vaccine hesitancy and uptake in the U.S.: a large nationwide study. Serv Heal Sci. (2021). doi: 10.1101/2021.04.05.21254918
37. Flocke SA, Stange KC, Zyzanski SJ. The association of attributes of primary care with the delivery of clinical preventive services. Med Care. (1998) 36:AS21–AS30. doi: 10.1097/00005650-199808001-00004
38. Kagawa-Singer M, Pourat N. Asian American and Pacific Islander Breast and Cervical Carcinoma Screening Rates and Healthy People 2000 Objectives. Cancer. (2000) 89:696–705.
39. Zambrana RE, Breen N, Fox SA, Gutierrez-Mohamed M. Lou use of cancer screening practices by Hispanic women: analyses by subgroup. Prev Med. (1999) 29:466–77. doi: 10.1006/pmed.1999.0566
40. Xu KT. Usual source of care in preventive service use: a regular doctor versus a regular site. Health Serv Res. (2002) 37:1509. doi: 10.1111/1475-6773.10524
41. Smith PJ, Santoli JM, Chu SY, Ochoa DQ, Rodewald LE. The association between having a medical home and vaccination coverage among children eligible for the vaccines for children program. Pediatrics. (2005) 116:130–9. doi: 10.1542/peds.2004-1058
42. Shi L. The impact of primary care: a focused review. Scientifica. (2012) 2012:1–22. doi: 10.6064/2012/432892
43. Weiss LJ, Blustein J. Faithful patients: the effect of long-term physician-patient relationships on the costs and use of health care by older Americans. Am J Public Health. (1996) 86:1742–7. doi: 10.2105/AJPH.86.12.1742
44. Blewett LA, Johnson PJ, Lee B, Scal PB. When a Usual source of care and usual provider matter: adult prevention and screening services. J Gen Intern Med. (2008) 23:1354. doi: 10.1007/s11606-008-0659-0
45. Artiga S, Garfield R, Orgera K. Communities of Color at Higher Risk for Health and Economic Challenges due to COVID-19|KFF. (2020). Available online at: https://www.kff.org/coronavirus-covid-19/issue-brief/communities-of-color-at-higher-risk-for-health-and-economic-challenges-due-to-covid-19/?utm_campaign=KFF-2020-Uninsured&utm_source=hs_email&utm_medium=email&utm_content=2&_hsenc=p2ANqtz-_UqLIoowVMibewUsBF8kGfwkh4ndUc-Ng7RZ8if—KZNFdsVsWt8UG2un7FH2DxliVe3nEefuXSQR1155GRcIUWd7mg&_hsmi=2 (accessed Aug 10, 2022).
46. Lieu TA, Elkin EP, Escobar PR, Finn L, Klein NP, Durojaiye C, et al. Effect of electronic and mail outreach from primary care physicians for COVID-19 vaccination of black and latino older adults: a randomized clinical trial. JAMA Netw Open. (2022) 5:e2217004. doi: 10.1001/jamanetworkopen.2022.17004
47. Callaghan T, Moghtaderi A, Lueck JA, Hotez P, Strych U, Dor A, et al. Correlates and disparities of intention to vaccinate against COVID-19. Soc Sci Med. (2021) 272:113638. doi: 10.1016/j.socscimed.2020.113638
48. Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine. Ann Internal Med. (2020) 173:964–73. doi: 10.7326/M20-3569
49. Arvanitis M, Opsasnick L, O'Conor R, Curtis LM, Vuyyuru C, Yoshino Benavente J, et al. Factors associated with COVID-19 vaccine trust and hesitancy among adults with chronic conditions. Prev Med Rep. (2021) 24:101484. doi: 10.1016/j.pmedr.2021.101484
50. Wong CA, Dowler S, Moore AF, Sosne EF, Young H, Tenenbaum JD, et al. COVID-19 vaccine administration, by race and ethnicity—North Carolina, December 14, 2020–April 6, 2021. MMWR Morb Mortal Wkly Rep. (2021) 70:991–6. doi: 10.15585/mmwr.mm7028a2
51. Sparks G, Kirzinger A, Brodie M. KFF COVID-19 Vaccine Monitor: Profile of The Unvaccinated|KFF. (2021). Available online at: https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-profile-of-the-unvaccinated/ (accessed Aug 10, 2022).
52. COVID-19 Claims Reimbursement to Health Care Providers and Facilities for Testing, Treatment, and Vaccine Administration for the Uninsured|Official web site of the U.S. Health Resources & Services Administration. Available online at: https://www.hrsa.gov/CovidUninsuredClaim (accessed Aug 10, 2022).
53. Khubchandani J, Saiki D, Kandiah J. Masks, Gloves, and the COVID-19 pandemic: rapid assessment of public behaviors in the United States. Epidemiol. (2020) 1:16–22. doi: 10.3390/epidemiologia1010004
54. Griffith DM, Sharma G, Holliday CS, Enyia OK, Valliere M, Semlow AR, et al. Men and COVID-19: a biopsychosocial approach to understanding sex differences in mortality and recommendations for practice and policy interventions. Prev Chronic Dis. (2020) 17:E63. doi: 10.5888/pcd17.200247
55. Müller F, Heinemann S, Hummers E, Noack EM, Heesen G, Dopfer-Jablonka A, et al. Immunosuppressed people's beliefs, expectations, and experiences with COVID-19 vaccinations : Results of a longitudinal study. Z Rheumatol. (2022) 1–11.
56. Shrestha R, Meyer JP, Shenoi S, Khati A, Altice FL, Mistler C, et al. COVID-19 Vaccine hesitancy and associated factors among people with HIV in the United States: findings from a national survey. Vaccines. (2022) 10:424. doi: 10.3390/vaccines10030424
57. Walker KK, Head KJ, Owens H, Zimet GD. A qualitative study exploring the relationship between mothers' vaccine hesitancy and health beliefs with COVID-19 vaccination intention and prevention during the early pandemic months. Hum Vaccin Immunother. (2021) 17:3355. doi: 10.1080/21645515.2021.1942713
Keywords: COVID-19, barriers, chronic illness, vaccine hesitancy, vaccine uptake
Citation: Spees LP, Biddell CB, Angove RSM, Gallagher KD, Anderson E, Christenbury A, Rocque G and Wheeler SB (2023) Barriers to COVID-19 vaccine uptake among resource-limited adults diagnosed with chronic illness. Front. Public Health 11:1046515. doi: 10.3389/fpubh.2023.1046515
Received: 16 September 2022; Accepted: 20 January 2023;
Published: 09 February 2023.
Edited by:
Emily E. Ricotta, National Institute of Allergy and Infectious Diseases (NIH), United StatesReviewed by:
Tanvi Kiran, Post Graduate Institute of Medical Education and Research (PGIMER), IndiaHolipah Holipah, University of Brawijaya, Indonesia
Copyright © 2023 Spees, Biddell, Angove, Gallagher, Anderson, Christenbury, Rocque and Wheeler. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lisa P. Spees,  THNwZWVzMjFAbGl2ZS51bmMuZWR1
THNwZWVzMjFAbGl2ZS51bmMuZWR1
 Lisa P. Spees
Lisa P. Spees Caitlin B. Biddell1,2
Caitlin B. Biddell1,2 Rebekah S. M. Angove
Rebekah S. M. Angove Kathleen D. Gallagher
Kathleen D. Gallagher Gabrielle Rocque
Gabrielle Rocque Stephanie B. Wheeler
Stephanie B. Wheeler