
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 26 January 2023
Sec. Public Health Education and Promotion
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1038062
This article is part of the Research Topic Strengthening the Community Health Worker Practice View all 12 articles
 Whenayon Simeon Ajisegiri1*‡
Whenayon Simeon Ajisegiri1*‡ Seye Abimbola1,2‡
Seye Abimbola1,2‡ Azeb Gebresilassie Tesema1,3‡
Azeb Gebresilassie Tesema1,3‡ Olumuyiwa O. Odusanya4‡
Olumuyiwa O. Odusanya4‡ David Peiris1†‡
David Peiris1†‡ Rohina Joshi5,6†‡
Rohina Joshi5,6†‡Introduction: Nigeria's skilled health professional health workforce density is insufficient to achieve its national targets for non-communicable diseases (NCD) which include 25% reduction in the prevalence of diabetes and hypertension, particularly at the primary health care (PHC) level. This places a great demand on community health workers (CHWs) who constitute the majority of PHC workers. Traditionally, CHWs are mainly involved in infectious diseases programmes, and maternal and child health services. Their involvement with prevention and control of NCDs has been minimal. With government prioritization of PHC for combating the rising NCD burden, strengthening CHWs' skills and competencies for NCD care delivery is crucial.
Methods: We conducted a mixed methods study to explore the roles and practices of CHWs in the delivery of hypertension and diabetes care at PHC facilities in four states (two each in northern and southern regions) in Nigeria. We reviewed the National Standing Orders that guide CHWs' practices at the PHC facilities and administered a survey to 76 CHWs and conducted 13 focus groups (90 participants), and in-depth individual interviews with 13 CHWs and 7 other local and state government stakeholders.
Results: Overall, we found that despite capacity constraints, CHWs frequently delivered services beyond the scope of practice stipulated in the National Standing Orders. Such informal task-shifting practices were primarily motivated by a need to serve the community.
Discussion: While these practices may partially support health system functions and address unmet need, they may also lead to variable care quality and safety. Several factors could mitigate these adverse impacts and strengthen CHW roles in the health system. These include a stronger enabling policy environment to support NCD task-sharing, investment in continuous capacity building for CHWs, improved guidelines that can be implemented at the point of care, and improved coordination processes between PHC and higher-level facilities.
Most countries have a critical shortage of skilled health workers, in particular doctors and nurses (1, 2). The World Health Organization (WHO) recommends a skilled health professional density of at least 4.45/1,000 population to achieve the sustainable development goals (SDGs) (3). The majority of countries in Africa have densities <2.28/1,000 population (4). Despite having one of the largest health workforces on the continent, Nigeria's skilled health workforce density is only 1.95/1,000 population, well below the recommended benchmark (5). Health system weaknesses due to inadequate number and skills of health workers is most pronounced at the primary health care (PHC) level in Nigeria. These weaknesses threaten the achievement of Universal Health Coverage and national NCD targets which includes about 25% reduction in the premature death from NCDs, prevalence of diabetes, hypertension and obesity (6);—and the ability to address the growing burden of non-communicable diseases (NCDs) in Nigeria.
The deployment of community health workers CHWs to deliver essential health services has proven to be a well-established strategy to address critical skilled health workforce (7, 8). The term CHW is a broad category comprising and although there are over 30 designations different types of health cadres globally, they share the common role of working at the frontline in community (9). The WHO considers CHWs to be members of the community with varying levels of formal education who are trained to address the health problems of individuals and the community (10). They usually share similar life experiences, socio-economic status and ethnicity with the communities they serve (11). CHWs often form the backbone of most health systems (11) at the PHC level and provide a linkage between communities and health systems (12).
The diversity in CHW roles is driven by a wide variation in the duration, content, and level of their training. While some CHWs are formally trained according to structured curricula and have a specified duration in government-recognized institutions, others are informally trained with access to variable content and may work in unregulated settings (13). Although CHW is a generic term used in most countries, each country usually has specific terms and scope of practice appropriate for their CHW cadre. For instance, CHWs are called Accredited Social Health Activists and auxiliary nurse midwives in India (14), Health Extension Workers (HEW) in Ethiopia (15), and Family Welfare Assistants or health assistants in Bangladesh (16).
In Nigeria, CHW titles include Community Health Officers (CHOs), Community Health Extension Workers (CHEW) and Junior Community Health Extension Workers (JCHEW) who have received various degrees of training at government-recognized institutions (6). JCHEWs and CHEWs hold Certificates and Diplomas in community health after completing 2- and 3-year training programmes respectively at Schools of Health Technology. CHOs are CHEWs who possess a higher national diploma obtained through an additional 1-year training programme in PHC at a teaching hospital (17).
The roles and responsibilities of CHWs in Nigeria depend on factors that include (but are not limited to) the level of education, type of training received, health care setting, size of population serviced and geographical coverage (18). These roles may be general or specialized (19) and span health promotion, prevention and treatment of diseases as well as management of data (8). The practice of CHWs is regulated by National Standing Orders which are the primary guidelines for CHW training and delivery of services to the community. They typically describe clinical features of common disease conditions and how they should be managed and define the scope of CHW practice under the instruction and supervision of physicians (20). Apart from ensuring normative guidance in the quality of care, adherence to the National Standing Orders also offer legal protection to CHWs in the course of service provision (21, 22).
CHWs have been traditionally involved in programmes that target infectious diseases and maternal and child services. Their involvement in the prevention and control of NCDs is relatively new and tends to be less well-documented (23). Although some studies have assessed the effectiveness of CHWs in the prevention and management of NCDs elsewhere (24, 25), there is a dearth of studies on CHWs' engagement in NCD care in Nigeria. One study on CHW management of hypertension and diabetes identified substantial knowledge gaps in the diagnosis and treatment of these NCDs (26). A pilot study to assess CHW support and self-home blood pressure (BP) monitoring found that such CHW support had potential to be successfully implemented in PHC settings in Nigeria (27). A study that explored stakeholders' perspectives on the adaptation of a hypertension treatment program for PHC facilities in Nigeria suggested empowering CHWs through training to participate in team-based care was a major enabler to hypertension treatment in those facilities (28).
Given the current knowledge gaps and the central role played by CHWs in the PHC workforce, an assessment of their skills and competencies for carrying out NCD-related activities is crucial to develop and implement NCD policies and programmes in Nigeria. Because the National Standing Orders do not address service delivery for cancers and chronic respiratory illnesses, we focused on hypertension and diabetes care. Study aims were to: (1) describe the role of CHWs in the prevention and control hypertension and diabetes in PHC facilities in Nigeria; (2) identify the policies and practice gaps by comparing CHWs' actual practices with those stipulated in their guidelines; and (3) highlight opportunities for enhancing CHW support to address those gaps.
We conducted a cross-sectional study with mixed methods data collection approach that included the following: (1) analysis of policies and guidelines related to CHW practices for hypertension and diabetes service delivery; (2) a cross-sectional survey of CHWs to quantify actual NCD service delivery practices; and (3) key informant interviews (KII) and focus group discussions (FGDs) with CHWs and other stakeholders to understand the processes involved in the reported practices in the survey.
The study was conducted in 13 PHC facilities across four states in Nigeria (two states in each of the northern and southern regions) between July and September 2019. The PHC facilities were purposively selected to obtain a diverse sample based on available human resources and health-seeking behaviors across the northern and southern regions of the country. This resulted in three PHCs selected per state except in one state where four PHCs were selected.
We started by reviewing and summarizing the National Standing Orders for hypertension and diabetes control for JCHEWs, CHOs and CHEWs, and PHC guidelines in Nigeria (21, 22, 29).
An interviewer-administered survey was used for obtaining information from CHWs on their socio-demographic characteristics and service provision (overall and specific to NCD-related activities). The survey included elements adapted from the WHO Package of Essential NCDs (WHO PEN) intervention (30) and the United States Agency for International Development Community Health Workers Assessment and Improvement Matrix (CHWAIM) toolkit (31) (Supplementary Appendix 1). CHWAIM was developed in 2011 to help government and non-governmental organizations assess, improve and plan CHW programmes and address implementation gaps. Although it has a maternal, newborn and child health and infectious diseases focus, it is designed to be adaptable for other services (31). In 2018, the Programme Functionality Matrix of the CHWAIM toolkit was reviewed and updated through a systematic review and extensive stakeholder consultation, resulting in ten criteria (32). We adapted these ten criteria or domains to understand the role of CHWs in their workplace, particularly in providing NCD care (Box 1).
Box 1. CHWAIM survey domains.
i. Role and recruitment: How are CHWs recruited and how are their roles defined?
ii. Training: What pre-service and in-service training is provided to CHWs to provide quality care and how are they evaluated?
iii. Accreditation: How is knowledge assessed and accredited during pre-service and in-service?
iv. Equipment and supplies: What is the availability and access to the required equipment?
v. Supervision: How is supportive supervision conducted?
vi. Incentives: How are CHWs incentivized/remunerated (both financial and non-financial incentives)?
vii. Community involvement: What is the level of community involvement in the CHWs' programmes?
viii. Opportunity for advancement: Is career progression an option available to the CHWs?
ix. Data: How does data flow from and to the community?
x. Linkages to the national health system: What policies are in place that integrate and include CHWs in health system planning, budget, and logistical support?
We then used findings from the survey to develop CHW interview guides. All three cadres of CHWs across 13 PHC facilities were invited to participate (JCHEWs, CHEWs, and CHOs). Sampling of CHWs for interview participation was not stratified by category, rather an invitation was sent out to all CHWs. FGDs were conducted at each PHC facility, and KIIs were conducted with the head or most senior CHW in a facility. We also interviewed state and local governments stakeholders to understand their perspectives on CHWs' NCD-related work in PHC facilities. These stakeholders supervised CHWs and are involved with disease control (including NCDs) activities at the state and local government levels. Interviews were conducted by the lead author (WSA), who has worked with the Nigerian government at national and frontline level of the country's health system. He was supported by two other trained data collectors. Each FGD involved 5–10 participants, lasting 45–75 min. Each KII lasted 30–45 min. The interviews (KII and IDIs) and FGDs were conducted in English language, digitally recorded and transcribed verbatim.
Survey responses were tabulated using Microsoft Excel. Descriptive variables were illustrated as frequencies and proportions. Qualitative data were coded in NVivo Pro 12. Initial themes were guided by the survey findings and focused on understanding the gaps between policy, guidelines and practice. The research team met regularly to analyses and interpret the themes emerging from the interviews. These meetings helped to refine themes, make appropriate inferences and synthesize findings across study sites.
Ethical approval was granted by the National Health Research Ethics Committee of Nigeria (Approval no: NHREC/01/01/2007) and the University of New South Wales Human Research Ethics Committee (HC: 190051). Informed written consent was obtained from all participants that contributed data to the study. Anonymity and confidentiality of all respondents was maintained throughout, and participants names were replaced with codes during data analysis and reporting.
Figure 1 summarizes the National Standing Orders care pathways for CHWs in the delivery of care for hypertension and diabetes at PHC facilities. Management guidance is focused on acute care for people presenting either with elevated blood pressure or symptoms that may be associated with diabetes. There is minimal focus on preventive activities or ongoing chronic care once a diagnosis of hypertension or diabetes is made. This includes limited guidance on: (1) preventive screening of risk factors for diabetes or hypertension; (2) ongoing risk factor monitoring for prevention of complications in patients with established diabetes or hypertension, (3) assessment of cardiovascular disease risks by the CHWs; and (4) follow up treatment with feedback from referral centers (to ensure continuity of care).
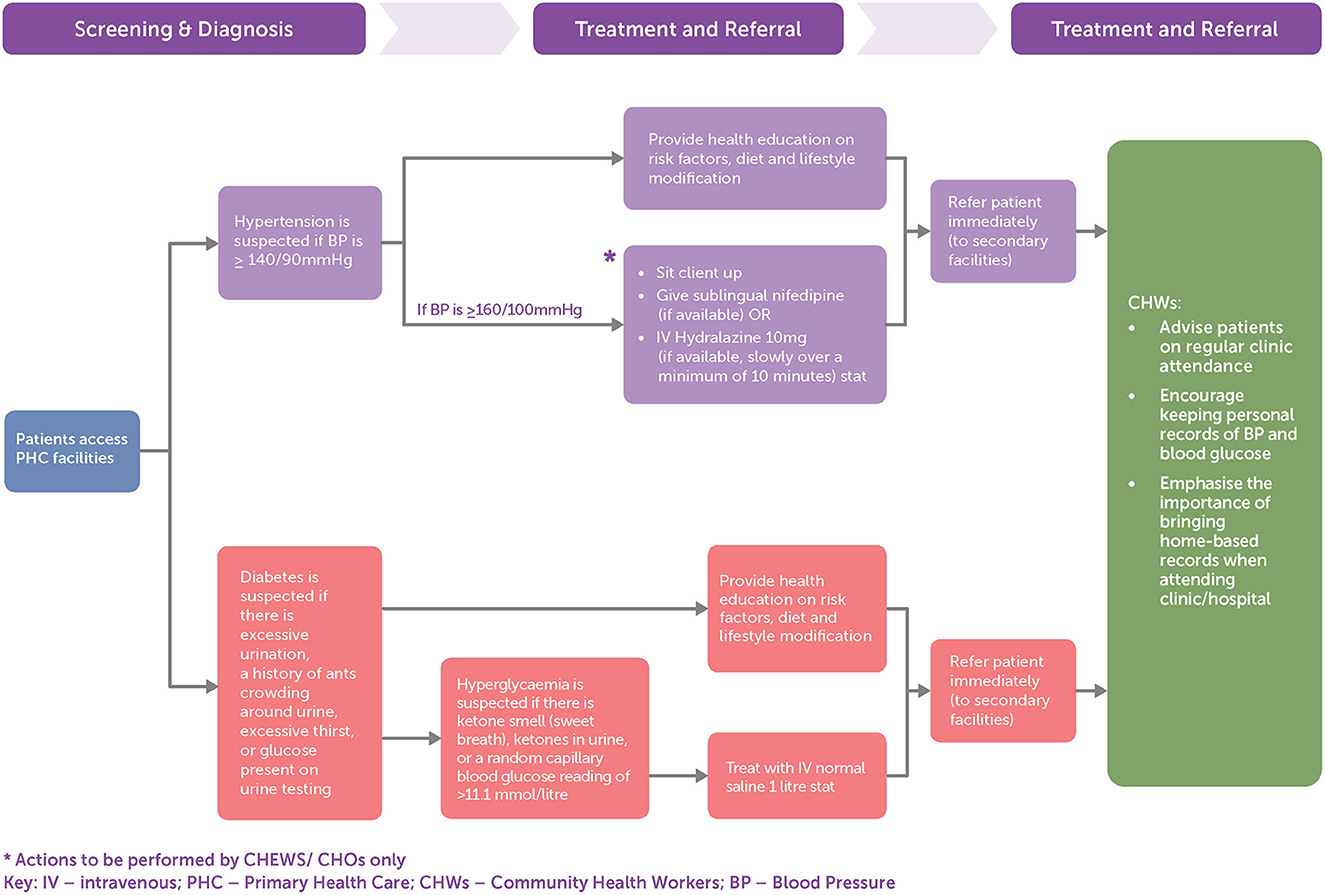
Figure 1. Care of patients with hypertension and diabetes according to National Standing Orders for Junior Community Health Extension Workers (JCHEWs), Community Health Extension Workers (CHEWs), and Community Health Officers (CHOs).
Among the 77 CHWs (CHO−9, CHEW−53, JCHEW−15) who participated in the survey on NCD care (representing a response rate of 85%), the vast majority were female, [70 (91%)] with a mix of full-time employment [36 (47%)] and volunteer contract [41 (53%)] workers. The majority worked in a facility with at least one nurse, however a minority worked with a doctor (Table 1). Although the majority reported receiving supervision in some areas, a substantial proportion reported receiving no supervisory support at all. Despite high levels of job satisfaction, many CHWs reported barriers to remaining in the job, particularly because of remuneration and in adequate administrative and health professional support.
Table 2 illustrates the self-reported services provided by CHWs compared with the in-service training received for conducting such activities. Blood pressure monitoring was the commonest activity conducted (88%) while cancer screening was the least (17%). CHWs engaged in more activities than they were formally trained for (except for awareness-raising activities for tobacco cessation), and the gap between conducting an activity and receiving formal training ranged from 8 to 31%.
CHWs identified inadequate training (84%), inadequate supplies of equipment (81%), poor infrastructure (71%) and inadequate supervision (52%) as the most frequent barriers to delivery of hypertension and diabetes care.
In total, 13 FGDs, 13 KII interviews with facility heads and 7 KIIs with other stakeholders were conducted (Table 3).
Three major themes were identified which influence how CHWs provide hypertension and diabetes care. These related to: (1) variable implementation of the National Standing Orders; (2) CHW role expansion and informal task-shifting; and (3) weak referral linkages.
Despite the National Standing Orders being the main guidance for management of hypertension and diabetes, the CHWs interviewed appeared to interpret them in varying ways. For instance, there was a wide interpretation both between and within facilities of what constituted hypertension “….If it is above normal, like 140/100 [mmHg]..” (KII7)……, or “…If somebody has, let's say, he has 170/100 [mmHg], or if he has [systolic of] 140 or 150 [mmHg]….”(FGD9 participants). and “....when we take their BP, when the BP is high, maybe its 150 over 90 [mmHg]…” (FGD7 participants.) Similarly for assessing diabetes, some CHWs were familiar with some clinical features but there was less familiarity with interpreting blood glucose values and criteria for diagnosing a patient with diabetes “…because we are meant to understand that [blood sugar] between 3.5 and 5.9 mmol/l is normal, then from this [value] upward is diabetes…” (FGD4 participants).
Another limitation to implementation of the National Standing Orders was medication and equipment availability. This led to CHWs having to “improvise” to assess blood pressure and blood glucose: “Under normal circumstances, different sections or units [are] supposed to have all those equipment, but [when] one section has to wait for the other to finish ….. we design a modality … where all patients that come in [check] their vital signs [centrally] before they go to wherever they are going to. So, [because] there is no equipment, we're just improvising” (FGD13 participants). This is particularly a problem for blood glucose testing where patients may be charged a fee for testing and not be able to pay, or glucometers are only available for part of the day: “….. the glucometer is stationed in the lab, and it doesn't run 24 h, so during the night shift, if you have such cases, … you can't help [the patient]….” (FGD4 participants).
Although the National Standing Orders recommend that CHWs refer patients suspected or diagnosed with hypertension, many CHWs were comfortable to initiate treatment and provide ongoing medication management: “…some will have 130/80, or 140/80, we just give..and ask the person to have rest or come back the second day, to recheck. But, if it is more than that, we can give nifedipine or amlodipine. So, those are the drugs that we use to prescribe (KII9). Other CHWs would initiate management and then refer if there was a perceived failure to achieve control: “…Like if a patient comes in with BP<160/100[mmHg], we try to manage between 23 days, if it doesn't come down you have to refer because there might be something ….” (KII4). Similar care processes were described for patients with diabetes“…if the blood sugar is high,….. we may place the patient on daonil [glibenclamide], just for maybe 3 or 5 days. …..Then, and we advise the patient on diet…..” (FGD13 participants).
The criteria for initiating and continuing treatment varied across facilities, based on the attending CHW's discretion and medication availability within the PHC facility. One focus group participant referred to “mild” forms of medication to initiate treatment “.…It is the CHEW that will give the prescription, and in that aspect, we give the mild one, like nifedipine, amlodipine and diuretic…. we don't give the higher one because, you are trying to just initiate the patient……” (FGD1 participants).
Although CHWs exercise considerable discretion in how they implement the National Standing Orders, by contrast several government stakeholders held more rigid views that their role should be restricted to screening and referral. Many felt that the formal training provided to CHWs in the college of health technology is insufficient for taking on a treatment role: “….. the reason why they are training them is so that they can recognize (non-communicable diseases) …. if they see anyone with it they can refer…” (KII- Stakeholder). Another justification for restricting CHW scope of practice was related to limited medication supply. Although NCD drugs are on the list of essential drugs and should be available at PHC facilities, frequently such medications are not available: “… since they (CHWs) are not treating it, they don't need to buy..….. there are no drugs for NCDs in the PHC (KII- Stakeholder).
One motivator for extending their scope of practice beyond that stipulated in the National Standing Orders' is the sense of addressing unmet need: “….. where our “Standing Orders” say you should treat hypertension, most…will say “refer”, …(but) by initiating or starting them on medication, … we are just helping….” (FGD1 participants). Some government stakeholders felt an expanded scope of practice was needed to maintain patients' trust in the services provided at the PHC facility. Because referring patients to higher level facilities could negatively affect perceptions of PHC level care, participants believed that CHWs had to strike a balance “…so that it doesn't water down the respect they have for the [PHC] system…. If you refer, the person needs to understand that it's not because of the fact that you are not competent to care … In terms of NCDs also, if we don't manage that aspect carefully, it may also affect patronage…” (KII- Stakeholder).
Another important motivation was the sense of prestige derived from displaying similar skills to doctors. Some CHWs believed that they've worked long enough with physicians to acquire the experience needed to treat patients: …. “we have worked longed enough with doctors, so, we also have the experience [to treat hypertension]… (FGD5 participants).” This appears to be influenced by gender with one stakeholder commenting that male CHWs functioned like doctors at the PHC facility: “…in the past, there were no doctors at the PHC system…. Every male you see is “a doctor”… what doctors are doing now, were being handled by CHOs …. they do prescribe anti-hypertensive and anti-diabetics [but] the extent to which they can is something to debate” (KII- Stakeholder).
A related barrier to optimal care was the perception that referral processes are inadequate. CHWs use a two-way referral form which is intended to support communication between CHWs at PHC facilities and health workers at secondary health facilities. Implicit in this is the expectation that the secondary facility staff will refer patients back to PHC facilities with clear feedback to aid continuity of care. CHWs commented that this feedback provides a learning opportunity on “what to do next when there's another patient with a similar case…” (FGD13 participants). However, many participants said the feedback from secondary health facilities is often not given or ineffective: “…. after referring, most of these facilities don't give a response back. We are the only ones that attempt to call the patient to know their well-being.” (FGD13 participants). The lack of feedback may result in CHWs initiating a new treatment plan at their own discretion“…since I've been working here, I've not seen any feedback. …. That is why we do make calls to contact the patient…. It's very, very important [to get feedback].. we will know the health of that patient… but since we are not getting feedback, there's nothing we can do…” (KII13). As a strategy to overcome the challenges of feedback from secondary facilities, some CHWs employed workarounds such as directly telephoning or visiting secondary health facilities. Unfortunately, such a resource intensive effort such as this would not address the problem: “We normally go there to collect the feedback ourselves, and sometimes when we go there we do not even get the feedback….they will say the doctor is yet to sign it, the patient will be well, and the feedback is not yet signed (KII6).
This mixed methods study explored practices of CHWs in hypertension and diabetes care in two states in Nigeria. We found that CHWs flexibly implement national guidelines for hypertension and diabetes exercising considerable discretion in interpretation. Further, we identified considerable workforce capacity gaps, system barriers including inadequate medication and equipment supplies, and challenging referral processes characterized by limited communication between PHC facilities and higher-level facilities. The findings suggest the need for a re-appraisal for how NCDs are integrated into PHC care with consideration of the following four areas: (1) formalize task-sharing and task-shifting policies for NCDs among CHWs; (2) enhance the National Standing Orders with simplified NCD clinical algorithms/guidelines that can easily be used by CHWs at the point of care; (3) Provide continuous capacity building for CHWs to enhance their roles in NCD care; and (4) improve care coordination between PHC and higher-level facilities.
CHWs are central to shifting or sharing tasks traditionally undertaken by skilled health workers (33). Although task shifting models involving CHWs have been successfully implemented in Nigeria for maternal and child health programmes, infectious diseases management and provision of contraceptive implants (34, 35), such models have thus far been overlooked in NCD service delivery. Despite the lack of explicit policies in this area, we found abundant evidence of CHWs informally taking on the roles of physicians. Given the widespread nature of such informal task-sharing care models, it would be short-sighted and impractical to eliminate such practices. Rather, such practices may need to be explicitly endorsed, formalized into policy and supported by the health system—all requiring a substantial shift in what is currently stipulated in guidelines and policies.
In settings where health system pressures from NCDs are growing, task-shifting and task-sharing models of service delivery by non-physicians play a central role (36). There is mounting evidence that such strategies are feasible and cost-effective in LMICs (37, 38). However, this requires considerable strengthening and restructuring of the PHC system as task-shifting functions cannot occur in isolation and wider system reforms are required (38, 39). It requires appropriate remuneration structures, enhanced commitment to capacity building, provision of supportive supervision and active engagement with physicians, development of workforce policies that support team-based care, and the creation of the appropriate environment for its implementation, including addressing complex challenges such as role overlaps between different health worker cadres and community perceptions that might impact demand-side factors. Nigeria has considerable experience in implementing task-shifting structures for HIV and reproductive health and this should be leveraged for including reforms for NCD care (34, 35). In the absence of such reforms, informal practices will remain tacit, of variable quality and with high potential for unsafe care.
Although the National Standing Orders are intended to guide CHW practices, they lack sufficient clarity to ensure compliance. The structure and volume of the Standing Orders themselves may pose a challenge for adherence and there is a need to have more simplified, unambiguous, NCD-specific clinical algorithms that are easy to use at the point of care. The current National Standing Orders do not include cardiovascular risk assessment as recommended in WHO guidelines. By adopting such an approach, CHWs will have greater guidance on implementation of a total risk approach to care leading to improved identification of people most in need of referral and treatment (30). There is robust evidence that such an approach can be feasibly and effectively implemented in many LMICs (40, 41), especially when the services are being delivered by non-physicians (42). Digital clinical decision support tools have also been shown to support task sharing models for hypertension and diabetes care (43–46). Currently there is little work being undertaken in this area in Nigeria. Such algorithms also need to be accompanied by appropriate and regular supportive supervision and accountability to support their uptake. There is also a need to integrate such supervision into existing training processes for infectious and other diseases rather than establishing separate structures.
The wide discretion with which CHWs engage in care practices combined with minimal training opportunities was a key study finding. These practices are indications of system weakness and suggest high levels of unmet need that CHWs are attempting to address (47). While CHWs were motivated by multiple factors to act beyond their scope of practice in the delivery of care for NCDs, ensuring a functional PHC facility and the need to provide care for their communities appeared to be the dominant motivations. This sense of duty may be accompanied by an increase in perceived professional status. Some CHWs felt empowered when members of their community viewed them as integral members of the health system (48), comparable to other professionals such as nurses and doctors (49). As CHWs are strongly motivated to strengthen the health system for the communities they serve (50), there are major opportunities to further empower them, commensurate with their desired competencies. This would support them to provide an optimum quality of care and mitigate against feelings of being undervalued or undermined in their communities and facilities of practice. Empowerment of CHWs to strengthen NCD service delivery requires multi-level capacity building at substantially greater degree than what is currently being provided. Such capacity building needs to be implemented in training colleges and then continuously supported with pre-service and regular in-service training (41, 51).
To support follow up and long-term monitoring of patients with hypertension and diabetes by CHWs at the PHC facilities, this study identified the need to strengthen the referral and feedback processes and enhance care continuity and quality (52, 53). This can be partly achieved by making simplified referral guidelines available. As seen in this study and others, non-adherence to referral guidelines was common practice among CHWs (54, 55). It is therefore important to implement more effective mechanisms to support adherence to referral guidelines including supportive supervision and continuous CHW training (56). Although these findings are limited to NCDs (in particular hypertension and diabetes management), they are likely to be relevant to other areas of CHW practice.
However, there are also important discrepancies in perceptions of CHW roles, their scope of practice, and the functions of the PHC sectors more broadly that must also be addressed. These discrepancies may represent a deeper issue of how CHW roles and responsibilities are defined in policy, while they themselves do not have significant input into defining their own practice (57). The insights and skills that CHWs might have developed in the course of overcoming challenges in their practice are often not recognized when new policies and initiatives are developed (58). English and colleagues highlight that the tacit and contextual knowledge held by those in practice must be harnessed for implementing successful interventions (59). The omission of frontline worker perspectives could undermine success of health system reforms (60). These issues highlight the need to support PHC teams in which health workers of disparate training levels can work together to deliver accessible, high quality, coordinated care whether that be in PHC or higher-level care facilities (61).
The findings of this study may not hold across all PHC facilities in Nigeria, especially those PHC facilities with physicians fully on staff. However, the majority of the PHC facilities have no or limited physician presence. Another possible limitation of the study is that the findings could be influenced by courtesy bias, particularly given we relied on self-reported data to determine care practices. To minimize these biases, we assured the participants of strict confidentiality and the potential benefits to improving workforce support if the authentic situation was presented. We also were able to triangulate the findings across the quantitative and qualitative data sources. Lastly, our study did not directly explore community and patient perspectives with respect to NCDs care. This could provide a deeper understanding of demand-side barriers to NCD care including perceptions of the role of CHWs, and identify opportunities for greater community engagement to support improved implementation of NCD policies. We recommend that future studies should explore this aspect.
CHWs play key roles at the PHC level in addressing the growing burden of NCDs in Nigeria. However, these roles are at times beyond their allowed scope of practice and greatly limited by access to adequate training and supervision. This could compromise health care quality, raising the need to better equip this workforce for effective NCD service delivery at PHC facilities in Nigeria. Such considerations include formalizing task-sharing and task-shifting policies for NCDs among CHWs and fostering an enabling environment for their implementation; enhancing the National Standing Orders Development with point of care clinical algorithm/guidelines; continuous capacity building during working life; improved care coordination processes between PHC and higher-level facilities; and the promotion of multi-disciplinary team based approaches. Development of new policies in these areas should include substantial engagement with CHWs in their design. CHWs are highly motivated to deliver high quality NCD services and there are major opportunities to better support and leverage this workforce to strengthen Nigeria's health system response to NCDs.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by National Health Research Ethics Committee of Nigeria (Approval no: NHREC/01/01/2007) and University of New South Wales Human Research Ethics Committee (HC: 190051). The patients/participants provided their written informed consent to participate in this study.
The study was conceptualized by WA, RJ, and DP. Data collection was conducted by WA and supported by OO. WA, RJ, OO, DP, and SA were involved analysis of the qualitative data. All authors provided critical intellectual input during the analysis. Manuscript was drafted by WA. All authors reviewed the draft manuscript and approved the final version.
The project was supported by the George Institute for Global Health, Australia through the Seed Grant funds dedicated for under-served populations in LMICs for 2019/2020. The UNSW Scientia Scholarship program supports WA and AT. WA is also supported through the Australian Government Research Training Program Scholarship. SA was supported by the Australian National Health and Medical Research Council (NHMRC) through an Overseas Early Career Fellowship (APP1139631). RJ is supported by the Australian National Heart Foundation (APP 102059) and UNSW Scientia Fellowship. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
We express our sincere gratitude to all health agencies, study participants and research assistants who supported us through the data collection period.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1038062/full#supplementary-material
Supplementary Appendix 1. CHWs' survey questionnaire.
1. Islam SMS, Purnat TD, Phuong NTA, Mwingira U, Schacht K, Fröschl G. Non-Communicable diseases (NCDs) in developing countries: a symposium report. Glob Health. (2014) 10:81. doi: 10.1186/s12992-014-0081-9
2. Maher D, Ford N, Unwin N. Priorities for developing countries in the global response to non-communicable diseases. Glob Health. (2012) 8:14. doi: 10.1186/1744-8603-8-14
3. World Health Organization. Health Workforce Requirements for Universal Health Coverage to Achieve Millennium Development Goals. Geneva: World Health Organization (2016).
4. World Health Organization. Global Health Workforce Crisis Key Messages-−2013. Geneva: World Health Organization (2013). Available online at: https://www.who.int/workforcealliance/media/key_messages_2014.pdf (accessed October 22, 2021).
5. World Health Organization. “Nigeria,” in >Global Health Workforce Alliance. Geneva: World Health Organization (2016). Available online at: https://www.who.int/workforcealliance/countries/nga/en/ (accessed October 22, 2021).
6. Federal Federal Ministry of Health, Nigeria. National Strategic Health Development Plan II: 2018–2022. Abuja: Federal Ministry of Nigeria (2018).
7. Lewin S, Dick J, Pond P, Zwarenstein M, Aja GN, Wyk BE, et al. Lay health workers in primary and community health care. Cochrane Database Syst Rev. (2005) 1:CD004015. doi: 10.1002/14651858.CD004015.pub2
8. Olaniran A, Smith H, Unkels R, Bar-Zeev S, van den Broek N. Who is a community health worker? A systematic review of definitions. Glob Health Action. (2017) 10:1272223. doi: 10.1080/16549716.2017.1272223
9. Bhattacharyya K, Winch P, LeBan K, Tien M. Community Health Worker Incentives and Disincentives: How They Affect Motivation, Retention, and Sustainability. Arlington: Basic Support for Institutionalizing Child Survival Project (BASICS II) for the United States Agency for International Development (2001).
10. World Health Organization. WHO Guideline on Health Policy and System Support to Optimize Community Health Worker Programmes. Geneva: World Health Organization (2018). p. 1–116. Available online at: http://www.ncbi.nlm.nih.gov/books/NBK533329/ (accessed May 27, 2020).
11. U.S. Department of Health and Human Services. Role of Community Health Workers. New York, NY: U.S. Department of Health and Human Services (2014). Available online at: https://www.nhlbi.nih.gov/health/educational/healthdisp/role-of-community-health-workers.htm (accessed October 18, 2021).
12. Mishra SR, Neupane D, Preen D, Kallestrup P, Perry HB. Mitigation of non-communicable diseases in developing countries with community health workers. Glob Health. (2015) 11:43. doi: 10.1186/s12992-015-0129-5
13. O'Brien MJ, Squires AP, Bixby RA, Larson SC. Role development of community health workers: an examination of selection and training processes in the intervention literature. Am J Prev Med. (2009) 37:S262–9. doi: 10.1016/j.amepre.2009.08.011
14. Abdel-All M, Abimbola S, Praveen D, Joshi R. What do Accredited Social Health Activists need to provide comprehensive care that incorporates non-communicable diseases? Findings from a qualitative study in Andhra Pradesh, India. Hum Resour Health. (2019) 17:73. doi: 10.1186/s12960-019-0418-9
15. Liu A, Sullivan S, Khan M, Sachs S, Singh P. Community health workers in global health: scale and scalability. Mt Sinai J Med J Transl Pers Med. (2011) 78:419–35. doi: 10.1002/msj.20260
16. Olaniran A, Madaj B, Bar-Zev S, van den Broek N. The roles of community health workers who provide maternal and newborn health services: case studies from Africa and Asia. BMJ Glob Health. (2019) 4:e001388. doi: 10.1136/bmjgh-2019-001388
17. Adepoju AA, Vidler M, Akadri AA, Jaiyesimi E, Nwankpa CC, Odubena OO, et al. The ability and safety of community-based health workers to safely initiate lifesaving therapies for pre-eclampsia in Ogun State, Nigeria: an analysis of 260 community treatments with MgSO4 and/or methyldopa. Pregn Hypertens. (2021) 25:179–84. doi: 10.1016/j.preghy.2021.05.005
18. Mishra SR, Lygidakis C, Neupane D, Gyawali B, Uwizihiwe JP, Virani SS, et al. Combating non-communicable diseases: potentials and challenges for community health workers in a digital age, a narrative review of the literature. Health Policy Plan. (2019) 34:55–66. doi: 10.1093/heapol/czy099
19. Lehmann U, Sanders D. Community Health Workers: What Do We Know About Them? Geneva: World Health Organization, Evidence Information for Policy, Department of Human Resources for Health (2007). p. 42. Available online at: https://www.who.int/hrh/documents/community_health_workers.pdf (accessed October 23, 2021).
20. Ibrahim DO. Assessment of the use of national standing orders in the treatment of minor ailments among community health practitioners in Ibadan municipality. Int J Sci Res Publ. (2016) 6:50–4.
21. National Primary Health Care Development Agency. National Standing Orders for Community Health Officers (CHO) and Community Health Extension Workers (CHEW). Abuja: National Primary Health Care Development Agency (2015). Available online at: https://nphcdang.com/publications (accessed November 22, 2021).
22. National Primary Health Care Development Agency. National Standing Orders for Junior Community Health Extension Workers (JCHEW). Abuja: National Primary Health Care Development Agency (2015). Available online at: https://nphcdang.com/publications (accessed November 22, 2021).
23. Tsolekile LP, Puoane T, Schneider H, Levitt NS, Steyn K. The roles of community health workers in management of non-communicable diseases in an urban township. Afr J Prim Health Care Fam Med. (2014) 6:48. doi: 10.4102/phcfm.v6i1.693
24. Khetan AK, Purushothaman R, Chami T, Hejjaji V, Madan Mohan SK, Josephson RA, et al. The effectiveness of community health workers for CVD prevention in LMIC. Glob Heart. (2017) 12:233–43.e6. doi: 10.1016/j.gheart.2016.07.001
25. Joshi R, Thrift AG, Smith C, Praveen D, Vedanthan R, Gyamfi J, et al. Task-shifting for cardiovascular risk factor management: lessons from the Global Alliance for Chronic Diseases. BMJ Glob Health. (2018) 3:e001092. doi: 10.1136/bmjgh-2018-001092
26. Anyanti J, Akuiyibo S, Idogho O, Amoo B, Aizobu D. Hypertension and diabetes management practices among healthcare workers in Imo and Kaduna States, Nigeria: an exploratory study. Risk Manag Healthc Policy. (2020) 13:2535–43. doi: 10.2147/RMHP.S271668
27. Ojji DB, Baldridge AS, Capital TN, Orji AI, Shedul LG, Ojji OI, et al. Feasibility and effect of community health worker support and home monitoring for blood pressure control in Nigeria: a randomised pilot trial. Cardiovasc J Afr. (2020) 31:e4–6. doi: 10.5830/CVJA-2019-066
28. Okoli RCB, Shedul G, Hirschhorn LR, Orji IA, Ojo TM, Egenti N, et al. Stakeholder perspectives to inform adaptation of a hypertension treatment program in primary healthcare centers in the Federal Capital Territory, Nigeria: a qualitative study. Implement Sci Commun. (2021) 2:97. doi: 10.1186/s43058-021-00197-8
29. National Primary Health Care Development Agency. Primary Health Care (PHC) Guideline in Nigeria. Abuja: National Primary Health Care Development Agency (2011). Available online at: https://nphcdang.com/publications (accessed November 22, 2021).
30. World Health Organization. Package of Essential Non-communicable (PEN) Disease Interventions for Primary Health Care in Low-Resource Settings. Geneva: World Health Organization (2016). p. 66.
31. Crigler L, Hill K, Furth R, Bjerregaard D. Community Health Worker Assessment and Improvement Matrix (CHW AIM): A Toolkit for Improving Community Health Worker Programs and Services. Revised Version. Bethesda, MD: University Research Co., LLC (URC).: USAID Health Care Improvement Project (2013). p. 118.
32. Ballard M, Bonds M, Burey JA, Foth J, Fiori K, Holeman I, et al. Community Health Worker Assessment and Improvement Matrix (CHW AIM): Updated Program Functionality Matrix for Optimizing Community Health Programs. Washington, DC: USAID (2018).
33. World Health Organization PEPFAR UNAIDS. Task Shifting: Rational Redistribution of Tasks Among Health Workforce Teams : Global Recommendations And Guidelines. Geneva: World Health Organization (2007). Available online at: https://apps.who.int/iris/handle/10665/43821 (accessed March 11, 2022).
34. Charyeva Z, Oguntunde O, Orobaton N, Otolorin E, Inuwa F, Alalade O, et al. Task shifting provision of contraceptive implants to community health extension workers: results of operations research in Northern Nigeria. Glob Health Sci Pract. (2015) 3:382–94. doi: 10.9745/GHSP-D-15-00129
35. Federal Ministry of Health. Task-Shifting and Task-Sharing Policy for Essential Health Care Services in Nigeria. Bonn: Federal Ministry of Health (2014).
36. Jeet G, Thakur JS, Prinja S, Singh M. Community health workers for non-communicable diseases prevention and control in developing countries: evidence and implications. PLoS ONE. (2017) 12:e0180640. doi: 10.1371/journal.pone.0180640
37. Gaziano T, Abrahams-Gessel S, Surka S, Sy S, Pandya A, Denman CA, et al. Cardiovascular disease screening by community health workers can be cost-effective in low-resource countries. Health Aff. (2015) 34:1538–45. doi: 10.1377/hlthaff.2015.0349
38. Anand TN, Joseph LM, Geetha AV, Prabhakaran D, Jeemon P. Task sharing with non-physician health-care workers for management of blood pressure in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Glob Health. (2019) 7:e761–71. doi: 10.1016/S2214-109X(19)30077-4
39. Joshi R, Peiris D. Task-sharing for the prevention and control of non-communicable diseases. Lancet Glob Health. (2019) 7:e686–7. doi: 10.1016/S2214-109X(19)30161-5
40. Harries AD, Zachariah R, Jahn A, Schouten EJ, Kamoto K. Scaling up antiretroviral therapy in Malawi-implications for managing other chronic diseases in resource-limited countries. JAIDS J Acquir Immune Defic Syndr. (2009) 52:S14. doi: 10.1097/QAI.0b013e3181bbc99e
41. Kengne AP, Awah PK, Fezeu LL, Sobngwi E, Mbanya JC. Primary health care for hypertension by nurses in rural and urban sub-Saharan Africa. J Clin Hypertens Greenwich Conn. (2009) 11:564–72. doi: 10.1111/j.1751-7176.2009.00165.x
42. Anand TN, Joseph LM, Geetha AV, Chowdhury J, Prabhakaran D, Jeemon P. Task-sharing interventions for cardiovascular risk reduction and lipid outcomes in low- and middle-income countries: a systematic review and meta-analysis. J Clin Lipidol. (2018) 12:626–42. doi: 10.1016/j.jacl.2018.02.008
43. Prabhakaran D, Jha D, Prieto-Merino D, Roy A, Singh K, Ajay VS, et al. Effectiveness of an mHealth-based electronic decision support system for integrated management of chronic conditions in primary care. Circulation. (2019) 139:380–91. doi: 10.1161/CIRCULATIONAHA.119.040782
44. Schwalm JD, McCready T, Lopez-Jaramillo P, Yusoff K, Attaran A, Lamelas P, et al. A community-based comprehensive intervention to reduce cardiovascular risk in hypertension (HOPE 4): a cluster-randomised controlled trial. Lancet Lond Engl. (2019) 394:1231–42. doi: 10.1016/S0140-6736(19)31949-X
45. Patel A, Praveen D, Maharani A, Oceandy D, Pilard Q, Kohli MPS, et al. Association of multifaceted mobile technology–enabled primary care intervention with cardiovascular disease risk management in rural Indonesia. JAMA Cardiol. (2019) 4:978–86. doi: 10.1001/jamacardio.2019.2974
46. Praveen D, Patel A, Raghu A, Clifford GD, Maulik PK, Abdul AM, et al. SMARTHealth India: development and field evaluation of a mobile clinical decision support system for cardiovascular diseases in Rural India. JMIR MHealth UHealth. (2014) 2:e3568. doi: 10.2196/mhealth.3568
47. Okpetu EI, Abimbola S, Koot JAR, Kane S. Implementing prevention interventions for non-communicable diseases within the Primary Health Care system in the Federal Capital Territory, Nigeria. J Commun Med Prim Health Care. (2018) 30:1–18. doi: 10.4314/jcmphc.v30i1
48. Kane S, Kok M, Ormel H, Otiso L, Sidat M, Namakhoma I, et al. Limits and opportunities to community health worker empowerment: a multi-country comparative study. Soc Sci Med. (2016) 164:27–34. doi: 10.1016/j.socscimed.2016.07.019
49. Sanou AK, Jegede AS, Nsungwa-Sabiiti J, Siribié M, Ajayi IO, Turinde A, et al. Motivation of community health workers in diagnosing, treating, and referring sick young children in a multicountry study. Clin Infect Dis Off Publ Infect Dis Soc Am. (2016) 63:S270–5. doi: 10.1093/cid/ciw625
50. Ajisegiri WS, Peiris D, Abimbola S, Odusanya OO, Tesema AG, Joshi R, et al. It is not all about salary: a discrete-choice experiment to determine community health workers' motivation for work in Nigeria. BMJ Glob Health. (2022) 7:e009718. doi: 10.1136/bmjgh-2022-009718
51. Mamo Y, Seid E, Adams S, Gardiner A, Parry E. A primary healthcare approach to the management of chronic disease in Ethiopia: an example for other countries. Clin Med. (2007) 7:228–31. doi: 10.7861/clinmedicine.7-3-228
52. Peck R, Mghamba J, Vanobberghen F, Kavishe B, Rugarabamu V, Smeeth L, et al. Preparedness of Tanzanian health facilities for outpatient primary care of hypertension and diabetes: a cross-sectional survey. Lancet Glob Health. (2014) 2:e285–292. doi: 10.1016/S2214-109X(14)70033-6
53. Katende D, Mutungi G, Baisley K, Biraro S, Ikoona E, Peck R, et al. Readiness of Ugandan health services for the management of outpatients with chronic diseases. Trop Med Int Health TM IH. (2015) 20:1385–95. doi: 10.1111/tmi.12560
54. Lal S, Ndyomugenyi R, Paintain L, Alexander ND, Hansen KS, Magnussen P, et al. Community health workers adherence to referral guidelines: evidence from studies introducing RDTs in two malaria transmission settings in Uganda. Malar J. (2016) 15:568. doi: 10.1186/s12936-016-1609-7
55. Chinbuah MA, Abbey M, Kager PA, Gyapong M, Nonvignon J, Ashitey P, et al. Assessment of the adherence of community health workers to dosing and referral guidelines for the management of fever in children under 5 years: a study in Dangme West District, Ghana. Int Health. (2013) 5:148–56. doi: 10.1093/inthealth/ihs008
56. Ajisegiri WS, Abimbola S, Tesema AG, Odusanya OO, Peiris D, Joshi R. The organisation of primary health care service delivery for non-communicable diseases in Nigeria: a case-study analysis. PLoS Glob Public Health. (2022) 2:e0000566. doi: 10.1371/journal.pgph.0000566
57. Oliver M, Geniets A, Winters N, Rega I, Mbae SM. What do community health workers have to say about their work, and how can this inform improved programme design? A case study with CHWs within Kenya. Glob Health Act. (2015) 8:27168. doi: 10.3402/gha.v8.27168
58. Theobald S, MacPherson E, McCollum R, Tolhurst R, REACHOUT. Close to community health providers post 2015: realising their role in responsive health systems and addressing gendered social determinants of health. BMC Proc. (2015) 9:S8. doi: 10.1186/1753-6561-9-S10-S8
59. English M, Nzinga J, Oliwa J, Maina M, Oluoch D, Barasa E, et al. Improving facility-based care: eliciting tacit knowledge to advance intervention design. BMJ Glob Health. (2022) 7:e009410. doi: 10.1136/bmjgh-2022-009410
60. MacKenzie NE, Chambers CT, Parker JA, Aubrey E, Jordan I, Richards DP, et al. Bridging the gap: Identifying diverse stakeholder needs and barriers to accessing evidence and resources for children's pain. Can J Pain. (2022) 6:48–64. doi: 10.1080/24740527.2022.2045192
61. Joshi R, Besigye I, Heredia-Pi I, Sharma M, Peiris D, Mash RJ, et al. How do diverse low-income and middle-income countries implement primary healthcare team integration to support the delivery of comprehensive primary health care? A mixed-methods study protocol from India, Mexico and Uganda. BMJ Open. (2022) 12:e055218. doi: 10.1136/bmjopen-2021-055218
Keywords: community health workers, primary health care, service delivery, hypertension, diabetes, non-communicable diseases, skills
Citation: Ajisegiri WS, Abimbola S, Tesema AG, Odusanya OO, Peiris D and Joshi R (2023) “We just have to help”: Community health workers' informal task-shifting and task-sharing practices for hypertension and diabetes care in Nigeria. Front. Public Health 11:1038062. doi: 10.3389/fpubh.2023.1038062
Received: 06 September 2022; Accepted: 09 January 2023;
Published: 26 January 2023.
Edited by:
Sunjoo Kang, Yonsei University, Republic of KoreaReviewed by:
Manoja Kumar Das, INCLEN Trust, IndiaCopyright © 2023 Ajisegiri, Abimbola, Tesema, Odusanya, Peiris and Joshi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Whenayon Simeon Ajisegiri,  d2FqaXNlZ2lyaUBnZW9yZ2VpbnN0aXR1dGUub3JnLmF1
d2FqaXNlZ2lyaUBnZW9yZ2VpbnN0aXR1dGUub3JnLmF1
†These authors have contributed equally to this work and share senior authorship
‡ORCID: Whenayon Simeon Ajisegiri orcid.org/0000-0002-8081-7058
Seye Abimbola orcid.org/0000-0003-1294-3850
Azeb Gebresilassie Tesema orcid.org/0000-0003-0618-4499
Olumuyiwa O. Odusanya orcid.org/0000-0003-4658-944X
David Peiris orcid.org/0000-0002-6898-3870
Rohina Joshi orcid.org/0000-0002-3374-401X
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.