
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 04 July 2023
Sec. Public Health Policy
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1025399
This article is part of the Research TopicWomen in Science: Public Health Policy 2022View all 6 articles
Objective: This study examined the effect of Medicaid expansion in Oregon on duration of Medicaid enrollment and outpatient care utilization for low-income individuals during the postpartum period.
Methods: We linked Oregon birth certificates, Medicaid enrollment files, and claims to identify postpartum individuals (N = 73,669) who gave birth between 2011 and 2015. We created one pre-Medicaid expansion (2011–2012) and two post-expansion (2014–2015) cohorts (i.e., previously covered and newly covered by Medicaid). We used ordinary least squares and negative binomial regression models to examine changes in postpartum coverage duration and number of outpatient visits within a year of delivery for the post-expansion cohorts compared to the pre-expansion cohort. We examined monthly and overall changes in outpatient utilization during 0–2 months, 3–6 months, and 7–12 months after delivery.
Results: Postpartum coverage duration increased by 3.14 months and 2.78 months for the post-Medicaid expansion previously enrolled and newly enrolled cohorts (p < 0.001), respectively. Overall outpatient care utilization increased by 0.06, 0.19, and 0.34 visits per person for the previously covered cohort and 0.12, 0.13, and 0.26 visits per person for newly covered cohort during 0–2 months, 3–6 months, and 7–12 months, respectively. Monthly change in utilization increased by 0.006 (0–2 months) and 0.004 (3–6 months) visits per person for post-Medicaid previously enrolled cohort and decreased by 0.003 (0–2 months) and 0.02 (7–12 months) visits per person among newly enrolled cohort.
Conclusion: Medicaid expansion increased insurance coverage duration and outpatient care utilization during postpartum period in Oregon, potentially contributing to reductions in pregnancy-related mortality and morbidities among birthing individuals.
The United States has one of the highest rates of deaths among birthing individuals due to complications from pregnancy and childbirth among developed nations (1). The postpartum period from delivery through 6 months after delivery (2–4) is a critical time in the lives of birthing individuals and their newborns. Appropriate healthcare during this period can reduce mortality and morbidities such as urinary incontinence, depression, diabetes, and cardiac diseases among others (5–7) in the birthing individuals. Importantly, morbidity and mortality occur at higher rates among low-income birthing individuals in minority racial/ethnic groups, who also disproportionately receive maternity care through the Medicaid program.
The guidelines for postpartum care from the American College of Obstetrics and Gynecologists (2018) recommended comprehensive postpartum visits through 12 weeks postpartum (2). However, Medicaid only provides postpartum coverage from conception to 60 days after childbirth (2) for those low-income postpartum individuals who obtained pregnancy-related Medicaid coverage. After 60 days, these individuals can remain enrolled in Medicaid only if they are eligible for parental Medicaid or Child Health Insurance Program (CHIP) coverage based on income levels. This gap in coverage can render some birthing individuals without health insurance, affecting their access to postpartum care (8). Lack of health insurance may also contribute to these individuals and their families suffering from negative financial impact due to high out-of-pocket expenses related to healthcare needs (9).
Birthing individuals who do not receive appropriate postpartum care are at higher risk for undiagnosed complications of pregnancy, delayed initiation of contraception, and unaddressed infant care issues (10). In spite of the importance of postpartum care, only 40% of birthing individuals enrolled in Medicaid received postpartum care (2). This low utilization of care may be reflective of general barriers to healthcare access and utilization, as documented in previous literature (11–13).
In an effort to reduce health disparities and gaps in coverage for low-income people, the Affordable Care Act (ACA) provides the opportunity for states to expand Medicaid eligibility to adults with incomes up to 138% of the federal poverty level (FPL) through an optional Medicaid expansion (14). As of March 2021, 39 states and the District of Columbia had expanded Medicaid eligibility (15). Estimates indicated that by 2016 more than 20 million adults were enrolled through the ACA Medicaid expansion; 9.5 millions of these enrollees were individuals who could potentially give birth (16). Increased enrollment in Medicaid potentially improves postpartum insurance coverage and access to care.
Despite the importance of postpartum care and the far reaching social and individual impacts of such care on birthing individuals and their families, the effect of Medicaid expansion on postpartum coverage and use of postpartum care remains an understudied area. Although the ACA is associated with a decrease of up to 21% in the uninsurance rate for the general population (17), Marchi et al. (18) reported almost a 10% reduction in uninsurance rates during the postpartum period following the implementation of Medicaid expansion. In recent studies that examined the impact of Medicaid expansion on continuous enrollment in postpartum care, researchers found increased probabilities of having Medicaid coverage and postpartum care utilization (19–22). In addition, the ACA Medicaid expansion in Colorado and Arkansas were associated with greater use of outpatient care in the postpartum period compared to Utah, a non-expansion state (7, 21). Medicaid expansion was also found to have a significant association with a reduction in the mortality ratio among individuals who gave birth (23).
In 2014, under the ACA, Oregon expanded Medicaid eligibility to all individuals with incomes between 100 and 138% of the FPL. During the same period, Oregon also raised the income limit for Medicaid eligibility for pregnancy-related eligibility from 185 to 190% FPL. These extensions potentially increased postpartum duration of coverage and outpatient healthcare utilization for women who were previously enrolled and newly enrolled in Medicaid. Previous research suggested that it takes time for those newly enrolled in Medicaid to utilize healthcare services at the same rate as those who were previously enrolled (24).
By 2018 Oregon had enrolled 490,700 newly eligible beneficiaries under the expansion criteria (24). The aims of this study were, therefore, to (1) evaluate the impact of Medicaid expansion on the duration of Medicaid enrollment during the postpartum period, and (2) examine the effect of Medicaid expansion on utilization of outpatient care, among low-income birthing individuals in Oregon.
The study population included all birthing individuals aged 18–44 in Oregon who had at least one delivery funded by Medicaid between 2011 and 2015. We divided our sample into three delivery cohorts, one pre-Medicaid expansion and two post-Medicaid expansion cohorts. Pre-Medicaid expansion deliveries occurred during 2011–2012 and were not impacted by Medicaid expansion. We excluded deliveries in 2013 because a portion of the 12-months postpartum period occurred in 2014 when Medicaid expansion was implemented. Post-Medicaid expansion cohorts included deliveries in 2014 and 2015. Deliveries during the 2014–2015 period to individuals who ever had Medicaid coverage prior to 2014 were categorized as the post-Medicaid expansion previously enrolled cohort. We assumed that individuals who had never been enrolled in Medicaid before 2014 were new enrollees who gained coverage due to Medicaid expansion. Therefore, deliveries during the 2014–2015 period by these birthing individuals were defined as the post-Medicaid expansion newly enrolled cohort (Appendix Figure 1).
We linked person-level datasets acquired from different sections or programs within the Oregon Health Authority (OHA) and included Oregon Medicaid eligibility and claims, birth certificates, death certificates and hospital discharge data of individuals who gave birth during the study period. The linkage was completed by the Integrated Client Service data warehouse maintained by the Oregon Health Authority (OHA) and the Oregon Department of Human Services (ODHS). The linked dataset captures all Medicaid funded births in the state of Oregon. Medicaid enrollment files were used to calculate the duration of postpartum coverage and to track historical coverage status for the cohort creation. Claims data were used to identify utilization of outpatient care services by birthing individuals after delivery. Individuals’ socio-demographic and birth characteristics were obtained from Medicaid enrollment files and birth certificates. The study was approved by institutional review boards at the [blinded for review].
A count variable was created that indicated the total number of months of Medicaid coverage from delivery date to the last day of the 12-months follow-up period or the last month of Medicaid enrollment. An individual was counted as having coverage for the entire month if they were enrolled for at least 1 day in the month.
Centers for Medicare and Medicaid Services define outpatient care as medical or surgical care received from a clinic or hospital but not admitted as an inpatient. Outpatient care may include emergency department services, observation services, outpatient surgery, lab tests, or X-rays (25). We defined outpatient care as all medical services with the exception of inpatient and emergency care. We examined total number of outpatient visits that occurred in three postpartum periods: 0–2 months, 3–6 months, and 7–12 months and used Current Procedural Terminology (CPT) codes (see Supplementary Material) in Medicaid claims file to identify these visits.
We included an indicator for post-Medicaid expansion delivery that took a value of 1 if the delivery occurred during 2014 or 2015. The coefficient of this variable estimated the average difference in each outcome between the pre-Medicaid expansion and the post-Medicaid expansion cohorts. We created binary indicators for the three delivery cohorts: pre-Medicaid expansion, post-Medicaid expansion previously enrolled, and post-Medicaid expansion newly enrolled. We also created a time trend variable to investigate how the impact of Medicaid expansion on the outcomes changed over the post-Medicaid expansion timeline. This variable took the value of 0 for all deliveries during the pre-Medicaid expansion period and January 2014 when Medicaid expansion started, and increased by 1 for each month thereafter till December of 2015. We also included the interaction terms of the time trend variable and indicators of post-Medicaid expansion cohorts to estimate the monthly change of the impact of Medicaid expansion on the outcomes during the Medicaid expansion period, compared to the pre-Medicaid expansion period.
Our statistical models examining the impact of Medicaid expansion on the outcomes controlled for individual level characteristics were collected from birth certificate data including age, race/ethnicity, educational status, marital status, rurality, type of delivery, parity, number of prenatal care visits, and morbidities among infants and birthing individuals. Birthing individual’s age was a continuous variable that denoted the age of the individual during delivery and ranged from 18 to 44 years. Binary variables for the individuals’ race-ethnicity included Non-Hispanic (NH) white, NH Black, NH American Indian and Alaskan Native (AIAN), NH Asian, Native Hawaiian and Pacific Islander, and Hispanic ethnicity. The educational status of the individual during delivery was denoted by binary variables and included less than high school education, high school and some college education, bachelor’s degree, and graduate degree. Type of delivery was denoted by binary variables and included spontaneous delivery, assisted vaginal delivery, and cesarean delivery. Binary variables for parity included zero, one, two, and three or more deliveries. A count variable for total prenatal visits for the delivery was also used and ranged from 0 to 55 visits.
Morbidities among birthing individuals included diabetes, hypertension during pregnancy, and eclampsia. Infant morbidities included premature birth, congenital infections, and low birth weight. A three-level rurality variable which included urban, large rural town, small and isolated rural towns was created from ZIP code of residence using the Rural Urban Commuting Area Categorization B (RUCA) criteria (26). Cases with missing data were excluded from our analysis. However, because the proportion of missing data was relatively low, this exclusion did not significantly impact the results of our study.
We estimated descriptive statistics for dependent and independent variables by cohorts and compared characteristics between pre-Medicaid expansion group and each of post-Medicaid expansion groups using unadjusted bivariable regression models. We used multivariate ordinary least squares regression to estimate the impact of Medicaid expansion on the duration of postpartum coverage during the first 12 months following delivery.
We used negative binomial regression models to estimate the impact of Medicaid expansion on service utilization in the post-Medicaid expansion period compared to the pre-Medicaid period, adjusting for full list of covariates. We estimated two sets of models, including models comparing the pre-Medicaid expansion cohort and the post-Medicaid expansion previously enrolled cohort, and models comparing the pre-Medicaid expansion cohort and the post-Medicaid expansion newly enrolled cohort. Because coefficients from nonlinear models could be misleading and do not capture magnitude, we computed the average marginal effect (via a finite difference method) that measured an average change in outpatient utilization associated with Medicaid expansion. Because the mathematical structure of the standard error of the average marginal effect is unknown, we used bootstrapped standard errors (300 repetitions) for statistical significance tests.
Model robustness was confirmed after conducting sensitivity analysis with zero inflated negative binomial (ZINB) models. While the results were very similar, the negative binomial models exhibited better Akaike information criterion, Bayesian information criterion, and log-likelihood values when compared with ZINB models. We also conducted sensitivity analysis for the impact of Medicaid expansion on postpartum outpatient care utilization by excluding individuals who had multiple births during the study period.
The sample included 73,669 deliveries, 35,513 deliveries (48.21%) in 2011–2012 prior to Medicaid expansion and 38,155 deliveries (51.79%) in the post-Medicaid expansion period 2014–2015 (Table 1). Among post-Medicaid expansion deliveries, 29,514 (40.06%) were post-Medicaid expansion previously enrolled and 8,642 (11.73%) deliveries were post-Medicaid expansion newly enrolled.
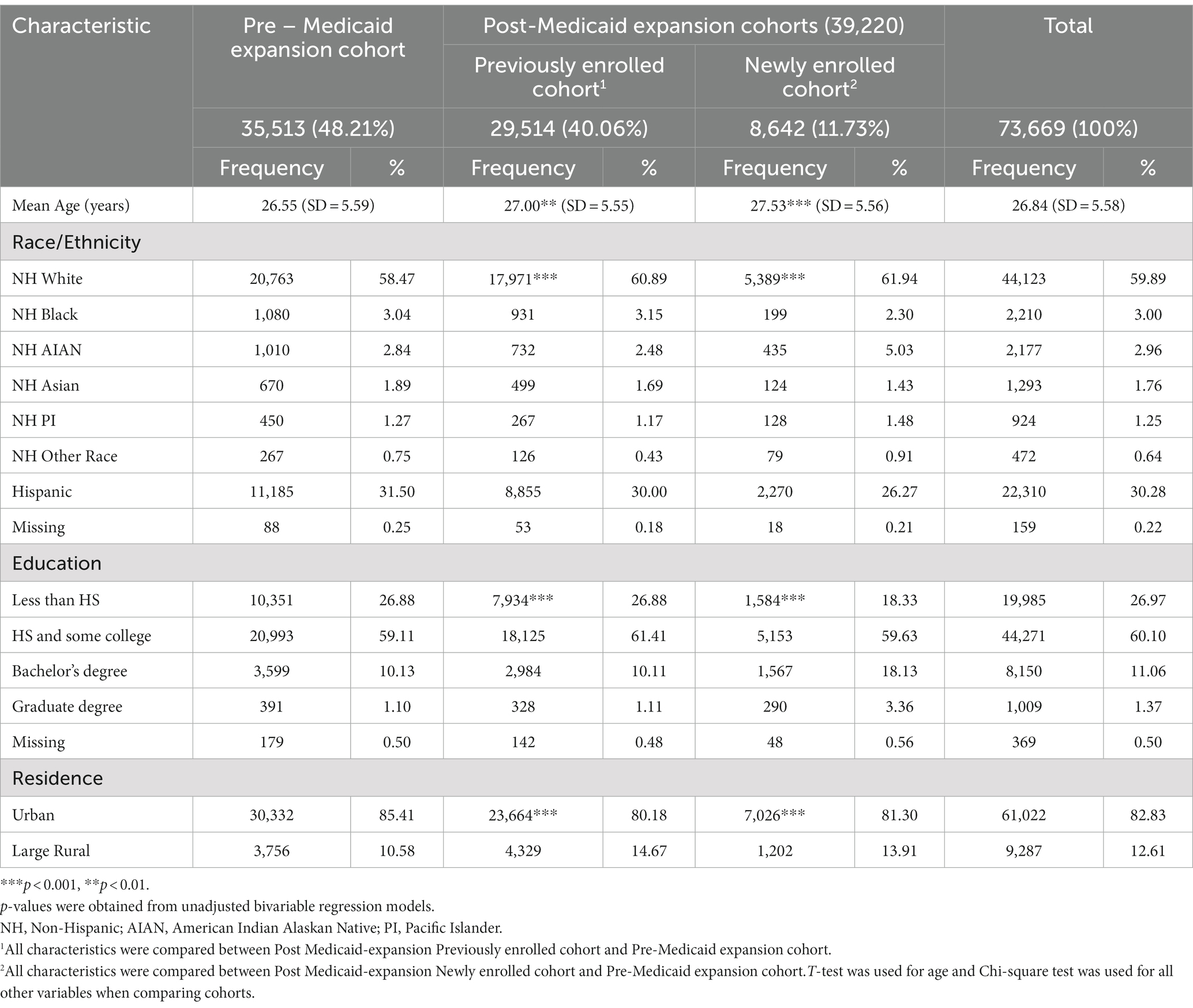
Table 1. Characteristics of Medicaid-enrolled birthing individuals in Oregon by expansion cohort, 2011–2015.
The mean age of birthing individuals at the time of delivery was 26.84 years (standard deviation [SD] = 5.58). Compared to the pre-Medicaid expansion cohort (mean = 26.55; [SD] = 5.59), birthing individuals in both post-Medicaid expansion previously enrolled cohort (mean = 27.00; [SD] = 5.55) and post-Medicaid expansion newly enrolled cohort (mean = 27.53; [SD] = 5.56) were older (p < 0.001). Racial/ethnic composition was similar among the three delivery cohorts. Non-Hispanic (NH) White birthing individuals formed the majority racial and ethnic group, followed by birthing individuals who identified as Hispanic. Less than 10% of the birthing individuals identified as NH Black, NH American Indian and Alaskan Native, NH Pacific Islander and Other NH races. Birthing individuals in post-Medicaid expansion newly enrolled cohort were more likely to have bachelors’ degree and post-graduate degree compared to both the pre-Medicaid expansion and post-Medicaid expansion previously enrolled cohorts (p < 0.001). The proportion of birthing individuals living in rural areas was higher for the post-Medicaid expansion previously enrolled (18.99%) and the post-Medicaid expansion newly enrolled cohorts (17.84%), compared to the pre-Medicaid expansion cohort (17.68%) (p < 0.001).
We visually examined monthly trends in duration of enrollment by cohort and observed an increase for both the post-expansion cohorts with birthing individuals in the post-Medicaid expansion previously enrolled cohort having longer coverage duration by the end of 2016 (Appendix Figure 2). In adjusted analysis, we observed that duration of postpartum coverage increased for the post-Medicaid expansion previously enrolled and the post-Medicaid expansion newly enrolled cohorts (Table 2). Coverage duration for deliveries of the post-Medicaid expansion previously enrolled cohort increased by 3.14 months (p < 0.001; 95% CI: 2.92, 3.09) compared to the pre-Medicaid expansion cohort. This change represented a 37.66% increase compared to the baseline mean coverage duration of 8.31 months (Table 3) among pre-Medicaid expansion deliveries. Medicaid expansion was associated with an increase of 2.78 months (p < 0.001; 95% CI: 3.05, 3.35) or 33.4% increase in coverage duration for the post-Medicaid expansion newly enrolled deliveries, compared to pre-Medicaid expansion deliveries.
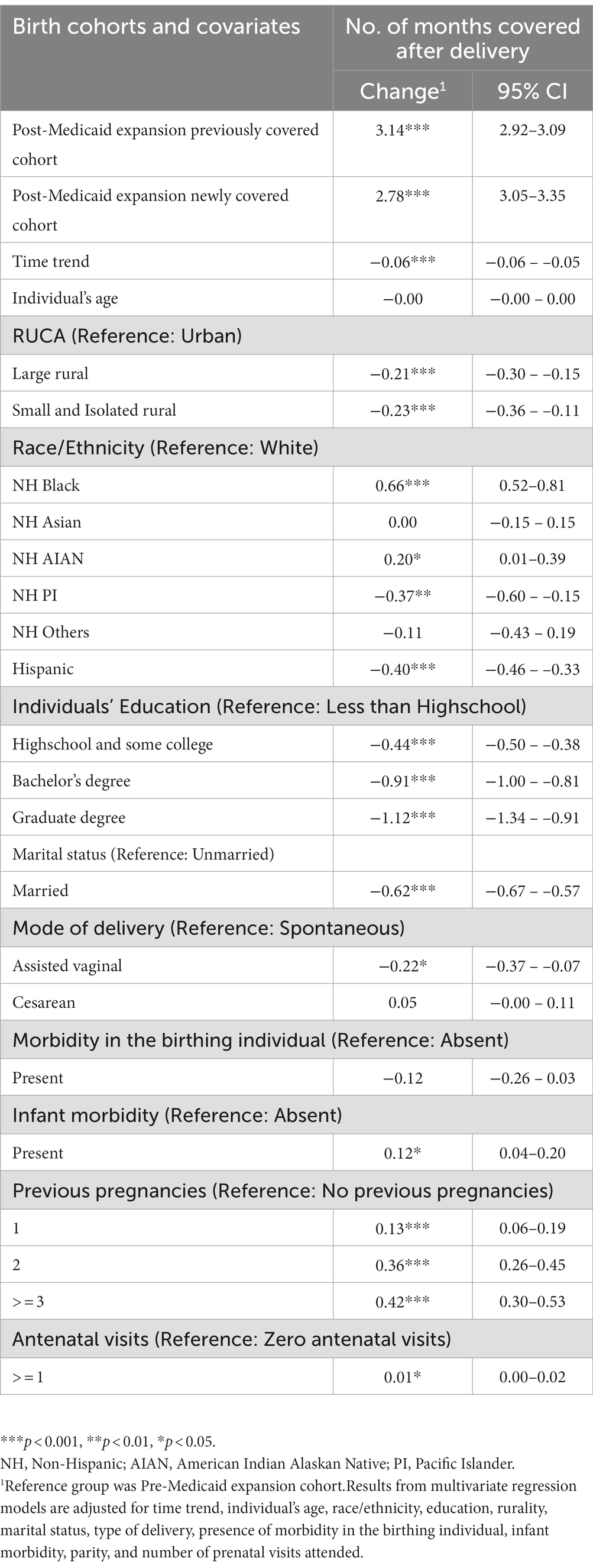
Table 2. Impact of Medicaid expansion on duration of enrollment during the 12-month postpartum period for Medicaid-enrolled birthing individuals of Oregon in 2011–2015.
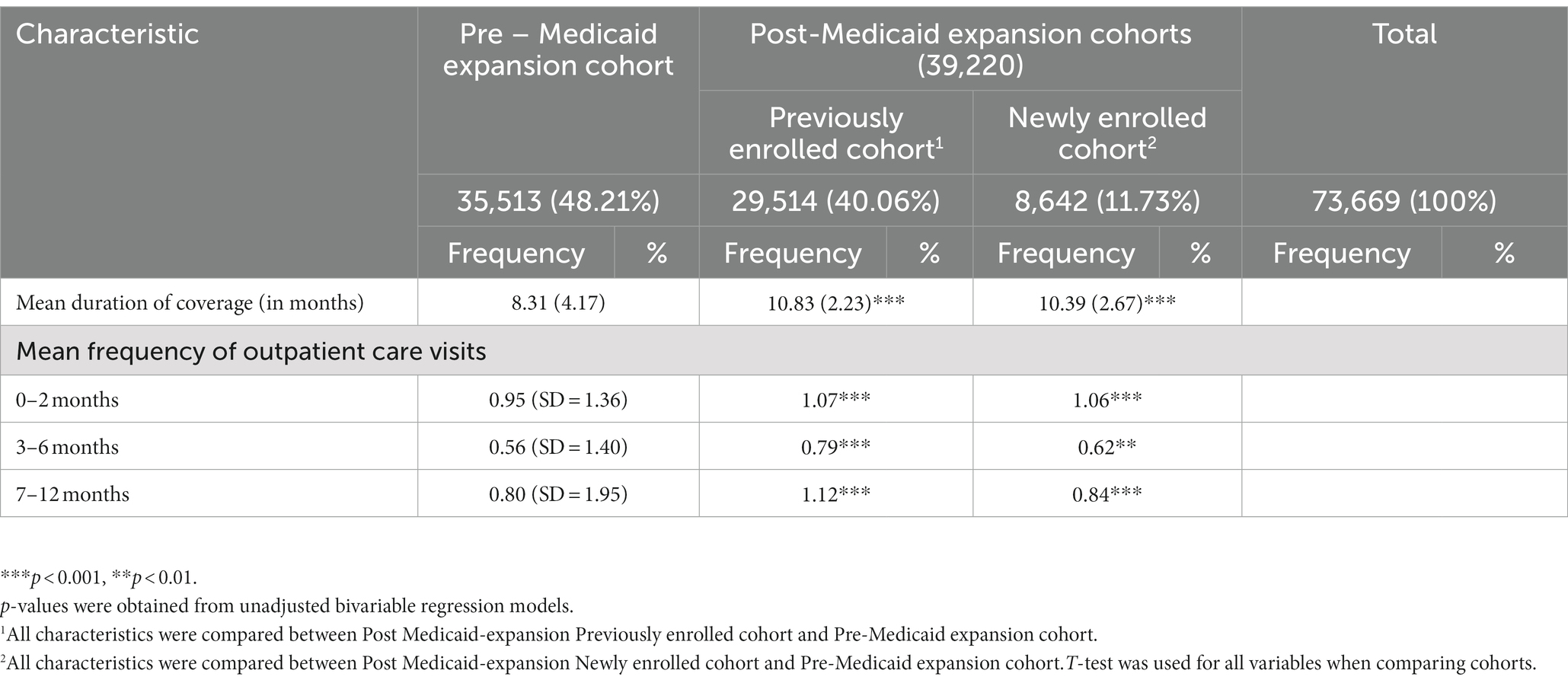
Table 3. Baseline characteristics of Medicaid access and utilization for Medicaid-enrolled birthing individuals in Oregon by expansion cohort, 2011–2015.
The results of our analyses examining the effect of the Medicaid expansion on number of outpatient care visits by postpartum periods are presented in Table 4. During the 0–2 months postpartum period, on average, the utilization of outpatient care by the post-Medicaid expansion previously enrolled birthing individuals was higher by 0.06 visits per person (p < 0.001; 95% CI: 0.03, 0.09) compared to that of pre-Medicaid expansion birthing individuals. The mean frequency of outpatient care visits for the post-Medicaid expansion previously enrolled cohort was, thus, higher at 1.02 visits per person, when compared to the baseline of 0.95 visits per person (Table 3) in the pre-Medicaid expansion cohort. For every month further from the start of Medicaid expansion, the monthly change in average number of visits during 0–2 months postpartum for previously enrolled birthing individuals was higher by 0.006 visits per person (p < 0.001; 95% CI: 0.004, 0.009) compared to that of the pre-Medicaid expansion birthing individuals. Overall, the post-Medicaid expansion newly enrolled cohort had more outpatient visits during the 0–2 months postpartum by 0.12 visits per person (p < 0.001; 95% CI: 0.06, 0.17) compared to the pre-Medicaid expansion birthing individuals. Compared to the pre-Medicaid expansion period, monthly change in utilization of outpatient care during 0–2 month postpartum for newly enrolled birthing individuals was lower by 0.003 visits per person (p < 0.001; 95% CI: −0.007, 0.002).
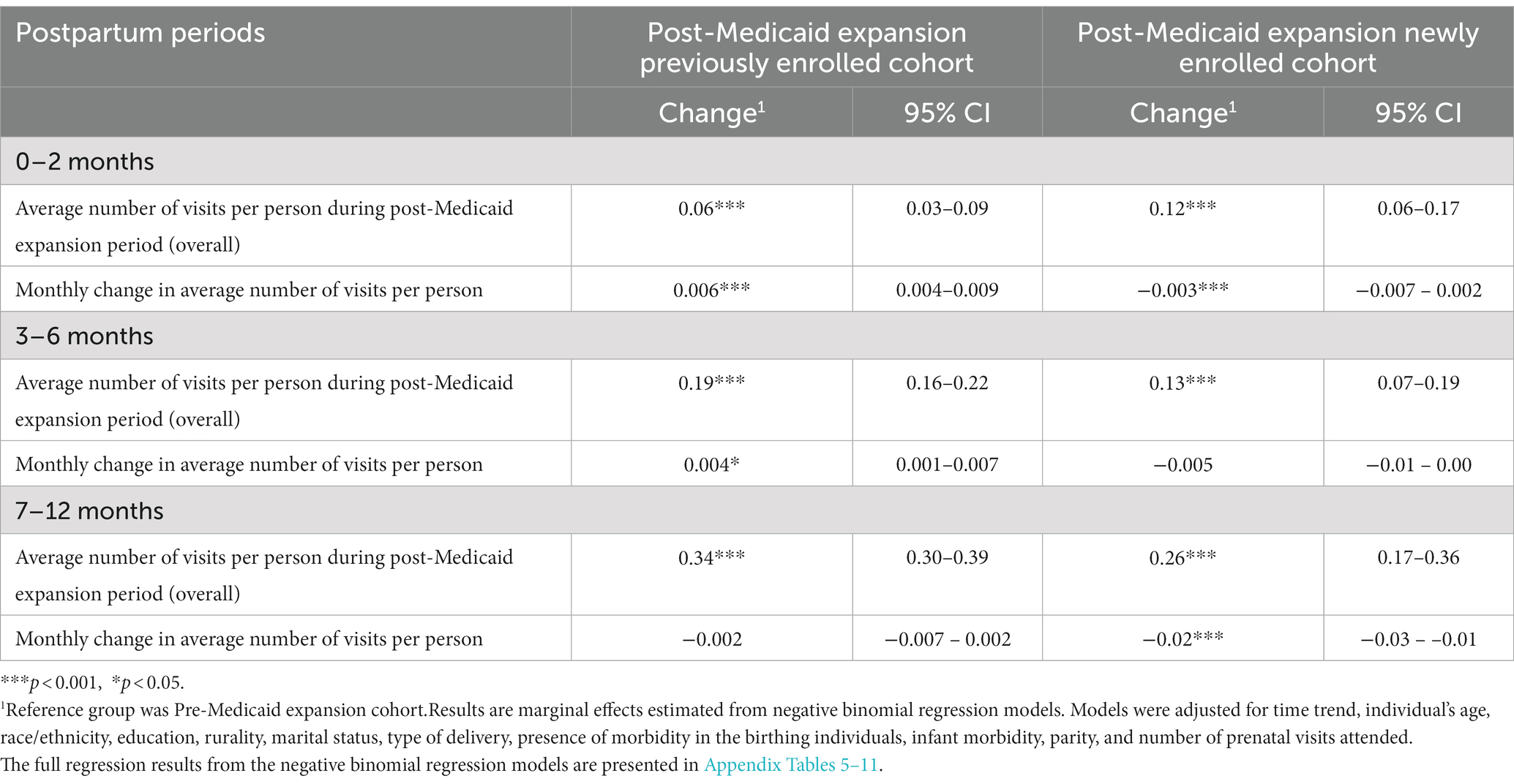
Table 4. Negative binomial regression models on number of outpatient care visits by postpartum periods for Medicaid-enrolled Oregon birthing individuals in 2011–2015.
In the 3–6 months postpartum period, on average, utilization of outpatient care by the post-Medicaid expansion previously enrolled birthing individuals was higher by 0.19 visits per person (p < 0.001; 95% CI: 0.16, 0.22) compared to that of pre-Medicaid expansion birthing individuals. Therefore, the average number of outpatient visits among the post-Medicaid expansion previously enrolled cohort was higher at 0.75 visits per person compared to the baseline service utilization of 0.56 visits per person (Table 3) by the pre-Medicaid expansion cohort. For each incremental month during the post-Medicaid expansion period, monthly change in service utilization during 3–6 month postpartum for previously enrolled birthing individuals was higher by 0.004 visits per person (p < 0.05; 95% CI: 0.001, 0.007) compared to that of pre-Medicaid expansion birthing individuals. We found that the post-Medicaid expansion newly enrolled cohort had an increase in outpatient visits during this postpartum period by 0.13 visits per person (p < 0.001; 95% CI: 0.08, 0.20) compared to that of pre-Medicaid expansion birthing individuals. Although not statistically significant, compared to the pre-Medicaid expansion period, monthly change in utilization of outpatient care during 3–6 month postpartum for newly enrolled birthing individuals was lower by 0.005 visits per person visits (p = 0.09; 95% CI: −0.01, 0.00).
Outpatient care utilization within 7–12 months postpartum due to Medicaid expansion increased on average by 0.34 visits per person (p < 0.001; 95% CI: 0.30, 0.39) and 0.26 visits per person (p < 0.001; 95% CI: 0.18, 0.37) for birthing individuals in post-Medicaid expansion previously enrolled and post-Medicaid expansion newly enrolled cohorts, respectively, compared to that of birthing individuals in pre-Medicaid expansion cohort. For every month since the Medicaid expansion in January 2014 up to the end of 2016, the average utilization of outpatient care within 7–12 months postpartum on average decreased by 0.002 visits per person (p = 0.29; 95% CI: −0.006, 0.002) and 0.02 visits per person (p < 0.001; 95% CI: −0.03, −0.01) for the post-Medicaid expansion previously enrolled cohort and post-Medicaid expansion newly enrolled cohorts, respectively, compared to that of pre-Medicaid expansion cohort. Sensitivity analysis conducted after excluding individuals with multiple deliveries yielded similar results, establishing the robustness of our results.
Our study is the first to explore the impact of Medicaid expansion on postpartum coverage and outpatient care among Medicaid-enrolled birthing individuals in Oregon. We found that the expansion of Medicaid in Oregon increased both duration of Medicaid coverage and utilization of outpatient care services in the postpartum period for low-income birthing individuals. We also found that birthing individuals who were previously enrolled in Medicaid had a larger increase in Medicaid coverage duration compared to newly enrolled birthing individuals.
After Medicaid expansion, birthing individuals who were previously enrolled in Medicaid experienced a larger increase in use of outpatient care compared to new enrollees during 3–6 months and 7–12 months after delivery. However, during the 0–2 months postpartum period, birthing individuals who were newly enrolled in Medicaid had more outpatient visits than those previously enrolled in the program.
Our findings are consistent with previous research that examined the effect of Medicaid expansion on use of services during the post-partum period (7, 19). These studies examined the impact of expansion for 6 months (7) or 300 days (19) post-delivery. We expanded the time frame to explore outpatient utilization trends over three time periods during the first 12 months post-delivery. This approach allowed us to better understand the trends in use during the postpartum period and the long-term impact of the policy on postpartum care utilization. Tracking access and utilization over 12 months after delivery also aligns with the provision under the American Rescue Plan which extended Medicaid coverage for pregnant people from 2 to 12 months after delivery (27).
Pent up demand could be one of many potential reasons for the increase in utilization in both post-expansion cohorts compared to the pre-expansion birthing individuals birthing individuals (28). Extension of pregnancy related medicaid eligibility from 185 to 190% FPL may also have contributed to some increase in utilization of services during the 0–2 months postpartum period. The largest increase in outpatient care utilization for both post-Medicaid expansion cohorts was during the 7–12 months postpartum period, followed by the increase in utilization in the 3–6 months postpartum. These periods coincide with the time frame when new birthing individuals would have lost coverage prior to Medicaid expansion. This finding could, in part, be due to delays in receiving services that newly enrolled birthing individuals may have experienced. Because of the surge of new members enrolled in Medicaid after expansion, appointments may have been unavailable and new enrollees could have experienced long waiting times (29, 30).
The trend of decreasing utilization of services over the time span of Medicaid expansion (monthly change in average number of visits per person), for both post-Medicaid expansion cohorts is consistent with other studies on Medicaid enrollees that examined the trends of expenditure on outpatient services (31, 32). This trend could be indicative of dissipated pent-up demand that was seen right after Medicaid expansion. This finding could also be due to other social, behavioral, and institutional barriers to access such as unawareness of the importance of postpartum care, lack of time, lack of transportation to service providers, difficulty in getting an appointment, and lack of caregiving support (33, 34).
These findings should be interpreted within the study limitations. Inconsistencies in coding for the type and setting of services used could have resulted in lower numbers compared to the actual numbers of services utilized (35). However, Medicaid data is a more reliable source of data for access and utilization of health care compared to self-reported data (35). We did not explore the potential effect of other ACA provisions intended to increase access to private insurance, such as the health insurance mandate, exchange, changes in payment methods to providers, all of which could have contributed to increased duration of enrollment and utilization of services. Furthermore, we utilized only 2 years of post-Medicaid expansion data which is a relatively short duration to capture the full impact of the policy. Future research should examine the long-term impacts of Medicaid expansion on healthcare service utilization during the postpartum. Because our findings reflect one state’s experience with Medicaid expansion, they may not be generalizable to other states that differ in terms of demographics, population health, political climate, and how Medicaid is managed. The results can, however, provide valuable insights for other states with similar characteristics that have not expanded Medicaid. Finally, in this study, identification of the effect of Medicaid expansion came from single interrupted time series (SITS) estimation and our findings remain robust to different time trends (e.g., quadratic and cubic functional forms). Further, we are unaware of any other important policy or system changes that occurred during the study period and therefore might serve as potential threats to the internal validity of our SITS analysis. Nonetheless, our findings should be interpreted with caution that ITS is subject to potential misspecification bias, especially bias from functional form misspecifications in the absence of an appropriate comparison group.
Medicaid expansion in Oregon was significantly associated with enrollment duration and utilization of outpatient care by low-income birthing individuals during the postpartum period. These improvement could potentially contribute to reducing mortality and morbidity among birthing individuals in the United States (36). In addition to studying the impact of expanding Medicaid coverage on the use of postpartum services, future research is also needed to examine other social, behavioral, and infrastructural barriers that may limit utilization of services for low-income birthing individuals.
The data analyzed in this study is subject to the following licenses/restrictions: The datasets presented in this article are not readily available because the current Data Use Agreement between Oregon State University (OSU) and Oregon Health Authority (OHA) does not allow public release of any data files including original data from OHA and analytic data files constructed by OSU. Requests to access these datasets should be directed to bWFyaWUuaGFydmV5QG9yZWdvbnN0YXRlLmVkdQ==.
SP and SH conceived and designed the manuscript. SP performed statistical analysis in consultation with LB and JY. SP drafted the manuscript. SP, SH, LB, and JY revised the manuscript for important intellectual content. All authors have made substantial contribution to the manuscript, read, and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1025399/full#supplementary-material
1. Gunja, MZ, Tikkanen, R, Seervai, S, and Collins, SR. What is the status of women’s health and health care in the U.S. compared to ten other countries? [Internet]. The Commonwealth Fund. (2018). Available at: https://www.commonwealthfund.org/publications/issue-briefs/2018/dec/womens-health-us-compared-ten-other-countries (Accessed April 5, 2021).
2. ACOG Committee Opinion No. 736: Optimizing Postpartum Care. Obstet Gynecol. (2018) 131:e140–e150. doi: 10.1097/AOG.0000000000002633
3. Romano, M, Cacciatore, A, Giordano, R, and La Rosa, B. Postpartum period: three distinct but continuous phases. J Prenat Med. (2010) 4:22–5.
4. Trends in Maternal Mortality. Trends in maternal mortality 2000-2017 [Internet]. UNICEF Data. (2019). Available at: https://data.unicef.org/resources/trends-maternal-mortality-2000-2017/ (Accessed February 1, 2021).
5. Borders, N. After the afterbirth: a critical review of postpartum health relative to method of delivery. J Midwifery Womens Health. (2006) 51:242–8. doi: 10.1016/j.jmwh.2005.10.014
6. CDC. Prevent pregnancy-related deaths [Internet]. Ctr Dis Control Prev. (2019). Available at: https://www.cdc.gov/vitalsigns/maternal-deaths/index.html (Accessed January 11, 2021).
7. Gordon, SH, Sommers, BD, Wilson, IB, and Trivedi, AN. Effects of Medicaid expansion on postpartum coverage and outpatient utilization. Health Aff. (2020) 39:77–84. doi: 10.1377/hlthaff.2019.00547
8. Daw, JR, Hatfield, LA, Swartz, K, and Sommers, BD. Women in the United States experience high rates of coverage “churn” in months before and after childbirth. Health Aff. (2017) 36:598–606. doi: 10.1377/hlthaff.2016.1241
9. Daw, JR, and Sommers, BD. The affordable care act and access to care for reproductive-aged and pregnant women in the United States, 2010–2016. Am J Public Health. (2019) 109:565–71. doi: 10.2105/AJPH.2018.304928
10. Conde-Agudelo, A, Rosas-Bermúdez, A, and Kafury-Goeta, AC. Birth spacing and risk of adverse perinatal outcomes a meta-analysis. JAMA. (2006) 295:1809–23. doi: 10.1001/jama.295.15.1809
11. Chen, J, Vargas-Bustamante, A, Mortensen, K, and Ortega, AN. Racial and ethnic disparities in health care access and utilization under the affordable care act. Med Care. (2016) 54:140–6. doi: 10.1097/MLR.0000000000000467
12. Lee, H, and Porell, FW. The effect of the affordable care act Medicaid expansion on disparities in access to care and health status. Med Care Res Rev. (2020) 77:461–73. doi: 10.1177/1077558718808709
13. Weir, S, Posner, HE, Zhang, J, Willis, G, Baxter, JD, and Clark, RE. Predictors of prenatal and postpartum care adequacy in a Medicaid managed care population. Womens Health Issues. (2011) 21:277–85. doi: 10.1016/j.whi.2011.03.001
14. MACPAC. Overview of the affordable care act and Medicaid [Internet]. MACPAC. (2021). Available at: https://www.macpac.gov/subtopic/overview-of-the-affordable-care-act-and-medicaid/ (Accessed January 11, 2021).
15. Kaiser Family Foundation. Status of state Medicaid expansion decisions: interactive map [Internet]. Status of State Medicaid Expansion Decisions: Interactive Map. (2021). Available at: https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/ (Accessed December 8, 2020).
16. Uberoi, N, Finegold, K, and Gee, E. Health insurance coverage and the affordable care act, 2010-2016 [Internet]. ASPE. (2016). Available at: https://aspe.hhs.gov/pdf-report/health-insurance-coverage-and-affordable-care-act-2010-2016 (Accessed April 14, 2021).
17. Gruber, J, and Sommers, BD. The affordable care act’s effects on patients, providers, and the economy: what we’ve learned so far. J Policy Anal Manage. (2019) 38:1028–52. doi: 10.1002/pam.22158
18. Marchi, KS, Dove, MS, Heck, KE, and Fan, C. The affordable care act and changes in women’s health insurance coverage before, during, and after pregnancy in California. Public Health Rep. (2021) 136:70–8. doi: 10.1177/0033354920962798
19. Patton, BP, Krans, EE, Kim, JY, and Jarlenski, M. The impact of Medicaid expansion on postpartum health care utilization among pregnant women with opioid use disorder. Subst Abus. (2019) 40:371–7. doi: 10.1080/08897077.2019.1573209
20. Dunlop, AL, Joski, P, Strahan, AE, Sierra, E, and Adams, EK. Postpartum Medicaid coverage and contraceptive use before and after Ohio’s Medicaid expansion under the affordable care act. Womens Health Issues. (2020) 30:426–35. doi: 10.1016/j.whi.2020.08.006
21. Steenland, M, Sinaiko, A, Glynn, A, Fitzgerald, T, and Cohen, J. The effect of the affordable care act on patient out-of-pocket cost and use of preventive cancer screenings in Massachusetts. Prev Med Rep. (2019) 15:100924. doi: 10.1016/j.pmedr.2019.100924
22. Eliason, EL, Daw, JR, and Allen, HL. Association of Medicaid vs marketplace eligibility on maternal coverage and access with prenatal and postpartum care. JAMA Netw Open. (2021) 4:e2137383. doi: 10.1001/jamanetworkopen.2021.37383
23. Eliason, EL. Adoption of Medicaid expansion is associated with lower maternal mortality. Womens Health Issues. (2020) 30:147–52. doi: 10.1016/j.whi.2020.01.005
24. Allen, H, Wright, BJ, and Baicker, K. New Medicaid enrollees in Oregon report health care successes and challenges. Health Aff. (2014) 33:292–9. doi: 10.1377/hlthaff.2013.1002
25. CMS. CMS data navigator glossary of terms. Baltimore, MD: Centers for Medicare and Medicaid Services (2021).
26. University of Washington. Rural-urban commuting area (RUCA) codes – WWAMI RHRC [Internet]. (2021). Available at: https://familymedicine.uw.edu/rhrc/ruca/ (Accessed November 8, 2021).
27. Yarmuth, JA. Text – H.R.1319-117th Congress (2021–2022): American Rescue Plan Act of 2021 [Internet]. (2021). Available at: https://www.congress.gov/bill/117th-congress/house-bill/1319/text (Accessed March 16, 2021).
28. Fertig, AR, Carlin, CS, Ode, S, and Long, SK. Evidence of pent-up demand for care after Medicaid expansion. Med Care Res Rev. (2018) 75:516–24. doi: 10.1177/1077558717697014
29. Biener, AI, Zuvekas, SH, and Hill, SC. Impact of recent Medicaid expansions on office-based primary care and specialty care among the newly eligible. Health Serv Res. (2018) 53:2426–45. doi: 10.1111/1475-6773.12793
30. Miller, S, and Wherry, LR. Health and access to care during the first 2 years of the ACA Medicaid expansions. N Engl J Med. (2017) 376:947–56. doi: 10.1056/NEJMsa1612890
31. Jacobs, PD, Kenney, GM, and Selden, TM. Newly eligible enrollees in Medicaid spend less and use less care than those previously eligible. Health Aff. (2017) 36:1637–42. doi: 10.1377/hlthaff.2017.0252
32. Springer, R, Marino, M, O’Malley, JP, Lindner, S, Huguet, N, and DeVoe, JE. Oregon Medicaid expenditures after the 2014 affordable care act Medicaid expansion: over-time differences among new, returning, and continuously insured enrollees. Med Care. (2018) 56:394–402. doi: 10.1097/MLR.0000000000000907
33. Ruderman, RS, Dahl, EC, Williams, BR, Davis, K, Feinglass, JM, Grobman, WA, et al. Provider perspectives on barriers and facilitators to postpartum care for low-income individuals. Women’s Health Reports. (2021) 2:254–62. doi: 10.1089/whr.2021.0009
34. Sakala, C, Declercq, ER, Turon, JM, and Corry, MP. Listening to mothers in California: a population based survey of women’s child bearing experiences [Internet]. National Partnership for Women and Families. (2018). Available at: http://www.nationalpartnership.org/our-work/health/listening-to-mothers-ca/report/chapter-5.html (Accessed May 20, 2022).
35. Virnig, B. Strengths and limitations of CMS administrative data in research|res DAC [Internet]. Res DAC. (2018). Available at: https://resdac.org/articles/strengths-and-limitations-cms-administrative-data-research (Accessed June 5, 2022).
Keywords: medicaid expansion, medicaid, coverage, postpartum, maternal health, affordable care act, outpatient, access and use
Citation: Pradhan S, Harvey SM, Bui LN and Yoon J (2023) Postpartum Medicaid coverage and outpatient care utilization among low-income birthing individuals in Oregon: impact of Medicaid expansion. Front. Public Health. 11:1025399. doi: 10.3389/fpubh.2023.1025399
Received: 22 August 2022; Accepted: 26 May 2023;
Published: 04 July 2023.
Edited by:
Li-Nien Chien, National Yang Ming Chiao Tung University, TaiwanReviewed by:
Erica Eliason, Brown University, United StatesCopyright © 2023 Pradhan, Harvey, Bui and Yoon. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Satyasandipani Pradhan, c2F0eWFzYW5kaXBhbmkucHJhZGhhbkBvcmVnb25zdGF0ZS5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.