- Faculty of Psychology and Education Sciences, Alexandru Ioan Cuza University, Iaşi, Romania
Introduction: The present study investigated psychological distress and coping strategies among infertile women during the COVID-19 pandemic using a multi-dimensional model of infertility-related stress. We explored the associations between individual (i.e., age) and situational characteristics related to infertility (i.e., duration of infertility, cause of infertility, number of lost pregnancies, and assisted reproductive techniques [ART] status), and perceived-infertility-related factors (i.e., the perceived importance of motherhood).
Methods: Our total sample consisted of 193 women aged 20 to 46 (M= 33.23, SD = 4.58), out of which 102 were undergoing ART procedures (M = 33.60, SD = 4.23), and 91 were not (M= 32.81, SD = 4.94). Participants filled in questionnaires measuring psychological distress, coping strategies, and the importance of motherhood.
Results: Correlation analyses suggested that the importance of motherhood was positively associated with psychological distress and negative coping strategies. Mediation analysis results indicated that both in the overall sample and in the sample of women undergoing ART procedures, the negative self-perception fully mediated the link between the importance of motherhood on psychological distress. In the non-ART sample, we found a significant mediation effect of denial on the link between the importance of motherhood and psychological distress.
Discussion: We discuss the theoretical and practical implications of the present findings, focusing on the mental health-related consequences of the social stigma of infertility heightened by the pressure of parenthood.
Introduction
The problem of infertility [i.e., the inability to conceive after 12 months of unprotected intercourse or after 6 months if a woman is 35 years or older] (1, 2) has been a constant concern over the years among researchers due to its complex implications at various personal and social levels (3, 4). It is generally estimated that infertility affects around 25 million people in the European Union alone (5). The Romanian Association for Human Reproduction (6) suggested that around 17% of the examined fertile population (4,680 participants) were in an infertility situation, and 38% of these couples sought infertility treatment.
Treating infertility is a common practice, although it is influenced by factors such as genetics, social expectations about motherhood, and public opinions and attitudes toward infertility and assisted reproductive techniques (ART), such as in-vitro fertilization (IVF) procedures (7). However, the choice of treatment relies on the exact cause of infertility, with approaches ranging from ovulation induction using a variety of medicines to more technically advanced procedures like IVF (8). Ovulatory disorders, for example, are among the most common medical causes of reduced reproduction, and a considerable percentage of couples worldwide are affected. Blocked fallopian tubes, endometriosis, or uterine anomalies are among the conditions that can reflect female infertility.
Infertility and psychological distress
The link between stress and infertility has generally been studied using a bidirectional approach, i.e., exploring the impact of stress on fertility and the impact of infertility on stress and overall psychological wellbeing. If the answers to the question “Does stress affect fertility?” might seem contradictory, according to the previous studies (9–12), the answer to the question “Does infertility affect stress?” seems significantly more straightforward (13).
Even if it is not a life-threatening diagnosis, infertility is still a highly stressful experience. Infertility has been linked to decreased marital wellbeing (14) and sexual functioning (15). Additionally, infertility can lead to feelings of failure, anxiety, depression, remorse, grief, and guilt (16, 17). This diagnosis can also negatively affect self-esteem (18, 19), with low levels leading to anxiety and depression (20).
Stress, anxiety, and depression are specific forms of psychological distress, generally more common among females than males (21). Previous research addressing the link between psychological distress and infertility (20, 22–30) generally highlighted the positive link between these variables. A systematic review and meta-analysis study concluded that the prevalence of depression was higher among infertile women than in the general population of a given country (25).
It was also suggested that infertile women experience significantly higher levels of depression, anxiety, and stress compared to their spouses (18, 22, 31), especially since women are considered complete only when they become mothers (26). Furthermore, depression is often followed by social isolation and low self-esteem because of gender discrimination (16) and the fact that motherhood is considered a highly desirable achievement (32). At the same time, Kiani et al. (33) suggested that infertile women report high anxiety levels due to the unpredictability of fertility treatment outcomes and the long-term nature of ART procedures.
Furthermore, among infertile women, higher depression was positively associated with low self-esteem (20, 34), high levels of shame (27, 35), stress (36), social concern, sexual concern and maternal relationship stress (37). Finally, the importance of parenthood was indirectly associated with depression, throughout the association of experiential avoidance, as a coping strategy and the perceived impact of infertility (38).
ART, age, and duration of infertility
Regarding the impact of assisted reproductive technologies, most previous studies suggested that repeated ART might be linked to higher distress in anxiety and depression (39, 40), though the findings in this area are mixed (41). Furthermore, previous studies (42–44) also suggested that the number of lost pregnancies and the duration of infertility (45–48) might be significantly related to infertile women's psychological distress. A review study (42) concluded that infertility and perinatal loss are associated with major depressive disorder, anxiety, posttraumatic stress disorder, complicated grief, marital discord, and low quality of life. The authors also highlighted the importance of treating anxiety and depression because infertility and perinatal loss may be caused or perpetuated by these symptoms. Along with high levels of depression and anxiety following the loss, infertile women also experience feelings of shame, self-blame, social awkwardness, fear, profound loss and grief, feelings of personal responsibility for what had happened, injustice or lack of fairness and inadequacy (44).
Regarding the duration of infertility, previous studies suggested that as the duration of infertility increases, depression may also increase (39, 46–48). Some studies have concluded that the long duration of infertility is positively associated with stress and anxiety (45). However, other studies suggested that the duration of infertility might not be directly associated with anxiety (39, 49) but rather mediated by the importance of motherhood (41).
Finally, when it comes to age, studies suggested that it might be negatively associated with infertile women's anxiety (34) and might not correlate with depression (34, 50). On the other hand, other studies found a positive correlation between age and distress, anxiety, and depression (37, 51). Thus, the results in this area are mixed and call for further research.
A multi-dimensional model of infertility-related stress
Based on the Transactional Theory of Stress (TTS); (52), Zurlo et al. (49) proposed a multi-dimensional model of infertility-related stress. The TTS emphasizes that several risk (individual and situational characteristics) and protective factors (e.g., coping strategies) must be considered when predicting psychological health. Based on this conceptual approach, Zurlo et al. (49) expanded it and added a series of demographic characteristics and coping strategies as part of individual characteristics. In addition, infertility-related parameters (i.e., type of diagnosis and duration of infertility), perceived sources of stress in infertility (i.e., social concern; couple's relationship concern; the need for parenthood; rejection of childfree lifestyle), and the perceived dyadic adjustment dimensions (i.e., dyadic consensus; affectional expression; dyadic cohesion; and dyadic satisfaction) were also added as situational characteristics.
The model proposed by Zurlo et al. (49) aimed to explore the predictive role of these factors when discussing psychological distress (i.e., anxiety and depression) among both partners of couples undergoing infertility treatments. In the present study, we used this theoretical approach, which we extended by adding some specific variables related to ART status and the number of lost pregnancies.
Coping with infertility
Coping strategies, considered individual characteristics, include cognitive, emotional, and behavioral efforts to manage internal or external sources of stress and are the major factor in adaptational outcomes (52, 53). Folkman and Moskowitz (54) classify coping strategies into four categories: problem-focused (behavioral strategies that address the problem that causes distress), emotion-focused (aimed to reduce negative emotions associated with the problem), meaning-focused (cognitive strategies that help the person to understand the problem), support seeking (reducing stress by reaching out to the community for emotional support).
These strategies are the subject of various studies related to the level of psychological distress among infertile individuals (49, 55), which investigated them as a mediator (56) and as a moderator (49) in the relationship between the sources and the outcomes of psychological distress. On the other hand, the relationship between coping strategies and anxiety and depression has been shown to be moderated by the duration of infertility (57) and mediated by the quality of life (58).
Among infertile women, active coping strategies (e.g., problem-solving, seeking social support) have been associated with low levels of distress (49, 59), while passive strategies (e.g., avoidance, denial, disengagement, social withdrawal) have been associated with increased levels of distress (35, 60). Regarding the potential gender differences, previous studies suggested that females, compared to males, seem to resort more often to social support (49, 61), which is associated both positively with anxiety (62), as well as negatively (22), in addition to being negatively related to infertility-related stress (63).
Coping strategies can be subject to cultural specificities (64), which can also influence the acceptance or denial of an infertility diagnosis and the option and adherence to treatment (65, 66). Furthermore, in countries with a collectivist culture, as is also the case in Romania, where family and religion are mainstream values (67), turning to divinity in the event of an illness is a strategy that many people might use to reduce the level of associated stress (68). For example, some studies have shown that women facing infertility turn to religious coping (69), which might help them reduce their stress, anxiety, and depression (70, 71). However, the literature also distinguishes between positive religious coping (which refers to the perceived help/support that the divinity can provide) and negative coping (infertility is considered a divine punishment). In the case of negative religious coping, these strategies seem to have increased infertility-related psychological distress (69).
Cousineau and Domar (72) suggested that one's self-perception can be affected when the only goal is motherhood, which might be hard to achieve. Previous studies have concluded that the inability to have a child leads to numerous psychological problems, including associated stress, anxiety, and negative self-perception (64), and social support might decrease them (73). Karaca and Unsal (74) concluded that infertility harms self-perception due to the perceived social pressure and infertility-related stigma, and similar findings were reported by Coşkuner Potur et al. (75).
Preoccupation with infertility-related thoughts can become obsessive, affecting the daily activities of women who want to become mothers and fail (74). Moreover, as the years pass and the number of failed treatments increases, the constant thinking about infertility [e.g., about the effectiveness of treatments, causes of infertility, efforts to find ways to avoid explanations to family/friends, uncertainty about the future – who they would be and how would their life will look like if they cannot conceive; (76)] becomes a common coping strategy in infertile couples (77). Additionally, interacting with potentially stressful stimuli (e.g., seeing a pregnant woman) triggers significantly more intrusive thoughts in females than in males (78).
Finally, infertility-related stress might also occur because of society-related and cultural factors and norms, i.e., the idea that having a child is mandatory. Thus, the related social pressure might lead to emotional imbalance and the need for social withdrawal or keep the diagnosis a secret (13, 79).
The importance of motherhood
Though voluntary childlessness (i.e., the option of fertile couples not to have children) - as an alternative to parenthood - appears to be gaining popularity globally (80), in many parts of the world (especially in countries with pronatalist policies), motherhood is associated with a higher social status (81), since children are an important source of social desirability (82). At the same time, cultural norms and beliefs favor reproduction, resulting in a predominantly negative opinion of childless women (83). People believe that a life without children cannot be fully satisfying (84). Adults who choose not to have children are stigmatized, viewed as aberrant, egocentric, or lacking in a feeling of responsibility (85). Women without children are typically seen more perceived more negatively than those having children (86). In Romania, according to the Barometer of Public Opinion (87), 83% of Romanian adults ranked family and children as the most important component of their lives, followed by religion.
Other studies concluded that motherhood represents a woman's most important goal and source of ultimate satisfaction (32, 88), but this aspect is also associated with high anxiety (49). Furthermore, studies investigating infertility suggest that infertile women struggle to cope with the stigma and powerlessness associated with not fulfilling this prescribed social norm [i.e., motherhood; (89)].
The implications of the importance of motherhood in the mental health of infertile women have been the subject of several studies (38, 90, 91). Most of them suggested that socially-prescribed motherhood (which is also associated with high social pressure) seems to predict infertility-related distress (91). It has also been suggested that the desire to become a parent is associated with one's wellbeing, life satisfaction, stress, and depression (90, 92). On the other hand, some studies suggested that infertility and, consequently, the inability to fulfill this role doesn't directly lead to depression but somewhat indirectly, through feelings of inadequacy and unfulfillment (38, 93).
Furthermore, according to recent data (94, 95), Romania is one of the most religious countries in Europe [with 86.6% Orthodox population, according to the (96)], and this also reflects on the importance of motherhood and the various pathways to parenthood, in general (2). Furthermore, when it comes to motherhood and the general perception regarding the pathway to becoming a parent in the case of women affected by infertility, according to Maftei and Holman (2), adoption seems to be the most preferred option among Romanian women, followed by IVF and surrogacy.
The present study
The present study was built on the multi-dimensional model of infertility-related stress proposed by Zurlo et al. (49). We aimed to explore the associations between individual characteristics such as sociodemographic factors (i.e., age) and coping strategies, and situational characteristics related to infertility-related parameters, i.e., duration of infertility, cause of infertility, number of lost pregnancies, ART status (i.e., whether the participants were undergoing ART procedures at the time of the research), and perceived-infertility-related factors, such as the perceived importance of motherhood (see Figure 1).
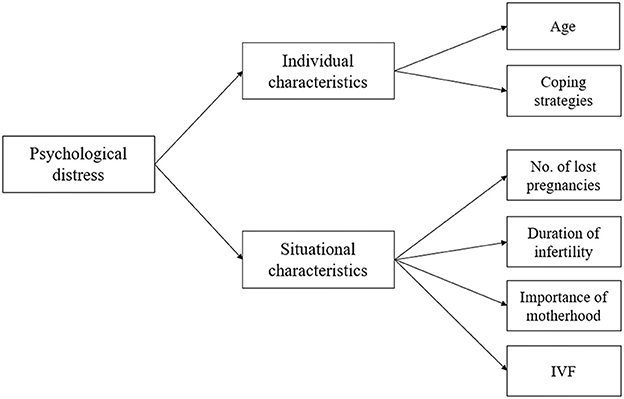
Figure 1. The proposed conceptual framework, based on Zurlo et al. (49).
The novelty of our study lies in (1) the addition of the variable concerning the number of lost pregnancies as an infertility-related parameter, in line with previous studies (42, 44, 47) that suggested its importance when examining the emotional outcomes related to infertility, (2) the addition of the ART-status variable, since previous studies documented its important role, as well, when discussing infertility-related distress (39, 40), (3) the moment of our research, i.e., during the COVID-19 pandemic.
Based on this theoretical model and the previous related literature, the general assumptions were the following: H1. There would be significant differences concerning psychological distress and maladaptive coping strategies, depending on women's ART status (i.e., participants who were undergoing ART procedures at the time of the research and women who were not). More specifically, according to previous literature, we assumed that women who were not undergoing ART would report higher psychological distress and more maladaptive coping strategies (41); H2. Regardless of the ART status, the importance of motherhood would be positively associated with maladaptive coping strategies. Next, as we added to Zurlo's model (49) the number of lost pregnancies as an infertility-related parameter, we assumed that H3. The number of lost pregnancies would be significantly associated with infertile women's psychological distress and maladaptive coping strategies; more specifically, we assumed that the higher the number of lost pregnancies, the higher the psychological distress and maladaptive coping strategies. Finally, we also assumed that H4. Maladaptive coping strategies would have a significant indirect effect on the link between the importance of motherhood and participants' psychological distress.
Method
Participants and procedure
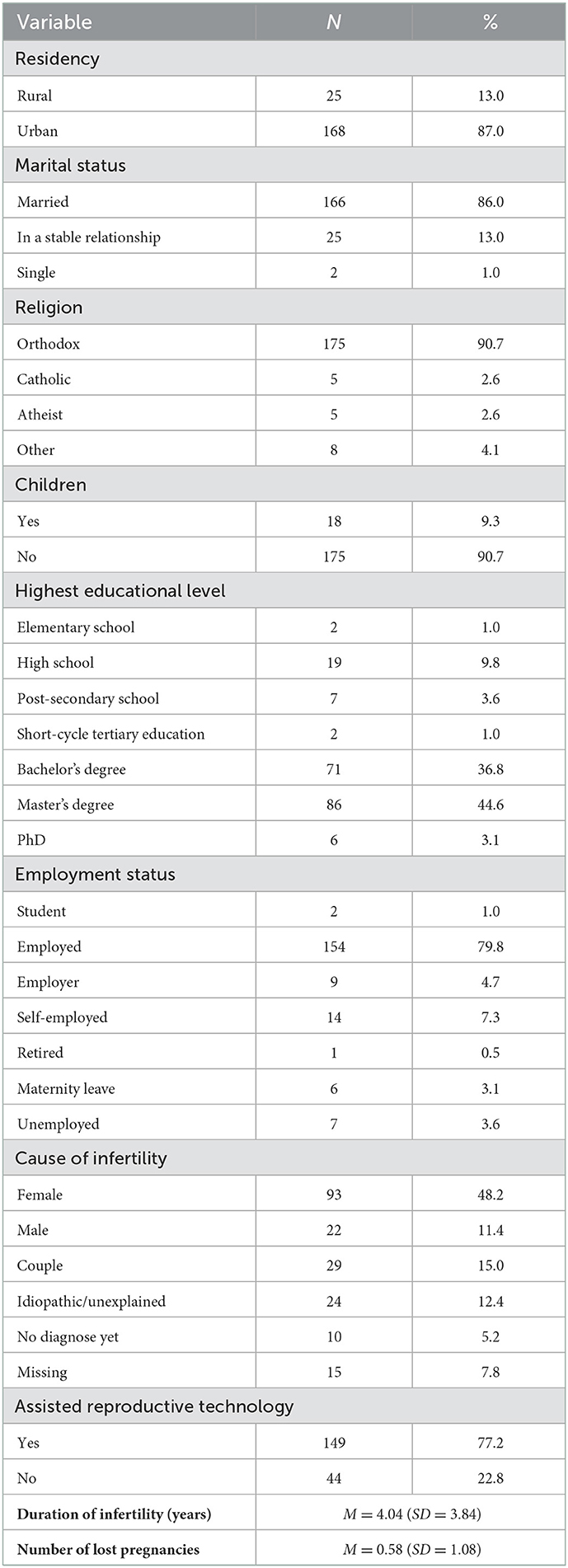
One hundred ninety-three women aged 20 to 46 (M = 33.23, SD = 4.58) participated in our study. Most of them were married (86%), employed (around 80%), and had a Bachelor's or a Master's degree. The demographic scale we used also included details related to the number of children and residency (rural or urban). The inclusion criteria that we used were the following: women aged at least 18, with an infertility diagnosis, who wanted children. Though the medical diagnosis of female infertility was a condition to participate in our study, we also asked participants to state the perceived cause of their infertility. Additionally, the participants also reported the number of lost pregnancies and whether they used assisted reproductive techniques (intracytoplasmatic sperm injection, artificial insemination, gamete intrafallopian transfer, IVF). All these details are presented in Table 1.
All participation was voluntary. We used convenience sampling using the snowballing technique. We distributed the participation link via specialized online support groups (e.g., Facebook groups associated with the medical clinics that treated infertile women) and, with the help of three physicians (obstetricians who worked in those clinics), the link was also directly distributed to the patients who agreed to be informed of such research opportunities (e.g., via e-mail or WhatsApp messages).
The instruments were administered at the end of 2021 (October-December). The participants were informed of the participation requirements, incentives, and their right to withdraw from the study at any time. We also informed all participants that their answers would remain confidential and anonymous and would only be used for the present research. The research protocol was developed following the ethical guidelines from the university with whom the authors are affiliated and the 2013 Helsinki Declaration. The average time needed to answer the items was around 35 min.
Measures
Psychological distress
We measured psychological distress using the 21-item Depression, Anxiety, and Stress Scale [DASS-21, (97)]. We selected this scale because of its documented dependability and efficacy (i.e., a relatively small number of items measuring three psychological dimensions). Using a scale ranging from 0 (did not apply at all) to 3 (very applicable), participants rated the applicability of each item (7 items for each subscale) considering the preceding week. Example items included “I couldn't seem to experience any positive feeling at all” (depression); “I was aware of dryness of my mouth” (anxiety); and “I found it hard to wind down” (stress). Cronbach's alpha-s for all three scales indicated good reliability, i.e., α = 0.89 for depression, α = 0.90 for anxiety, and α = 0.89 for stress. Higher scores indicated higher depression, anxiety, and stress. In the present study, we also computed an overall score for the scale (i.e., Psychological distress).
Coping strategies
We used the Coping Scale for Infertile Women [CSIW; (64)] to explore the coping strategies used by the participants in our sample in dealing with infertility-related problems. The items are scored on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). The scale comprises ten dimensions, i.e., Preoccupation with thoughts (e.g., I have physical problems like insomnia and loss of appetite because of my thoughts), Spiritual coping (e.g., I believe that God will reward me for dealing with this problem), Denial (e.g., I prefer to talk about this problem), Social withdrawal (e.g., I prefer to contact with my relatives less often), Negative self-perception (e.g., I feel weak and incomplete), Hope (e.g., I am dreaming about children), Social support seeking (e.g., I ask a relative or a friend, whom I respect or trust, for advice regarding this problem), Accept (e.g., I learn to live with this problem), Investigating in Self (e.g., I pay more attention to my appearance compared to the past), and Spousal relations (e.g., I am trying to involve my partner in each step of the problem/treatment). In the present study, following internal reliability analyses, we used a 34-item version of the scale, comprising six dimensions, i.e., Preoccupation with thoughts (α = 0.88), Spiritual coping (α = 0.72), Negative self-perception (α = 0.83), Social withdrawal (α = 0.80), Denial (α = 0.70), and Social support seeking (α = 0.76). A high score indicated that the person uses more of that way of coping.
The importance of motherhood
We asked participants to evaluate on a scale ranging from 1 (not at all) to 100 (extremely important) how important it was for them to have (another) child.
We used the International Test Commission (98) cross-cultural adaption approaches before using the instruments (99, 100). First, two independent translators transcribed the instrument from English to Romanian. We examined the two translated versions and assessed the potential ambiguities with a third translator. There were no major contradictions, and the consensus allowed the initial translation scales. We then blindly back-translated the initial tentative translation of the instruments and compared the two back-translated scales to create the final instruments.
Results
Overview of the statistical analysis
We first conducted preliminary analyses; then, we computed zero-order correlations among the variables and tested for differences depending on the ART status using independent T-tests. Finally, we conducted mediation analyses based on these results.
Preliminary analyses
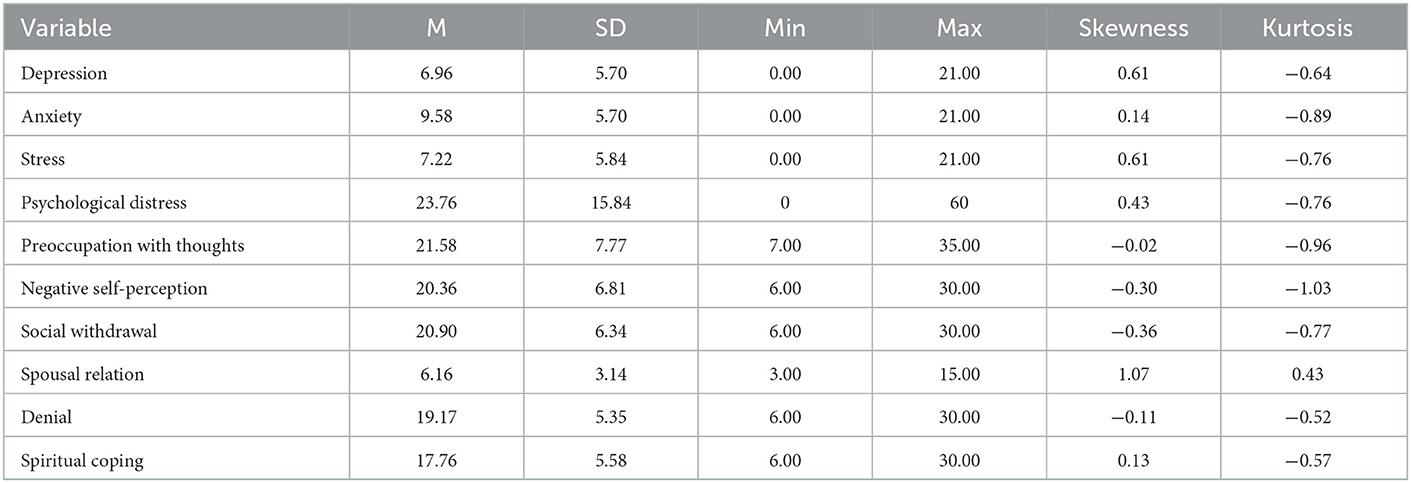
We used the IBM SPSS 26 statistical software for the analyses. Data cleaning steps and normality checks were performed preliminary to any analyses. Out of the 201 participants who initially formed our sample, eight were eliminated because they stated they did not want children anymore. We then computed the Skewness and Kurtosis values to assess the normality of the distributions, and all the values were in the 2/-2 limit suggested by George and Mallery (101) (see Table 2 for the descriptive statistics of the main variables).
Associations among the main variables
Independent T-tests further suggested marginally significant differences between the participants who were undergoing ART procedures at the time of the research, and women who were not, concerning psychological distress, t(191) = 1.96, p = 0.052, preoccupation with thoughts, t(191) = 2.48, p = 0.01, and spiritual coping, t(191) = 2.08, p = 0.03, with higher rates (in all cases) among women who were not undergoing ART.
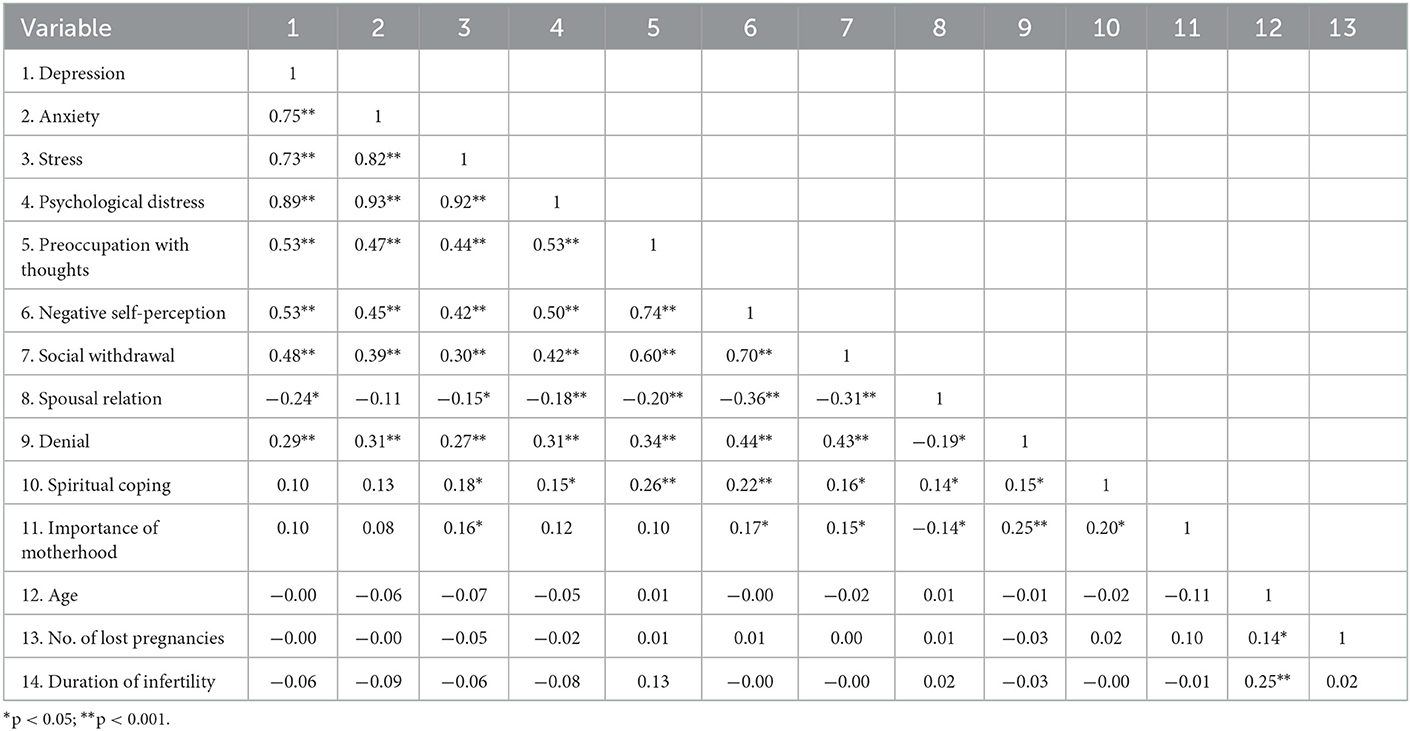
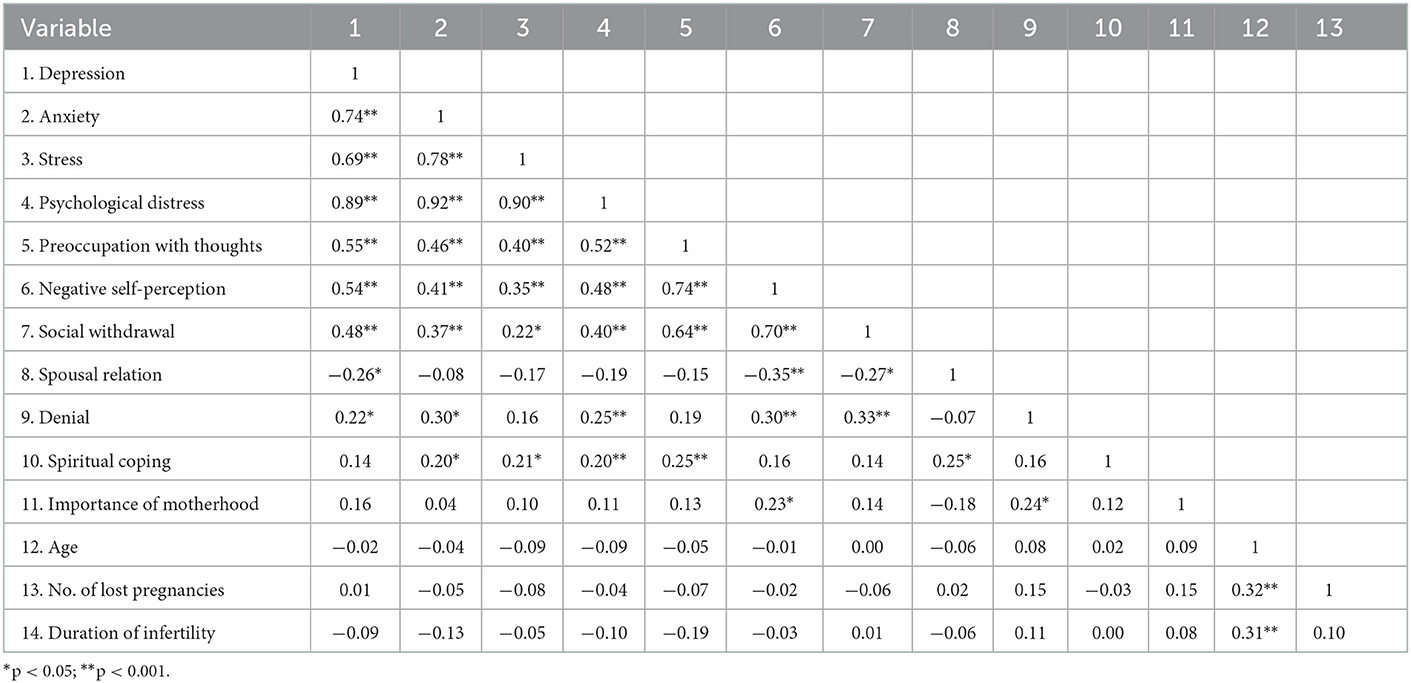
We further computed zero-order correlations to investigate the associations between the research variables and test for potential multicollinearity. Given the t-test results concerning the differences between ART and non-ART groups, and for a better understanding of emotional outcomes examined (i.e., psychological distress), we examined these links separately for the overall sample (Table 3A), participants who were involved in the time of the research in any ART procedures (Table 3B), and participants who were not involved at the time of the research such procedures (Table 3C).
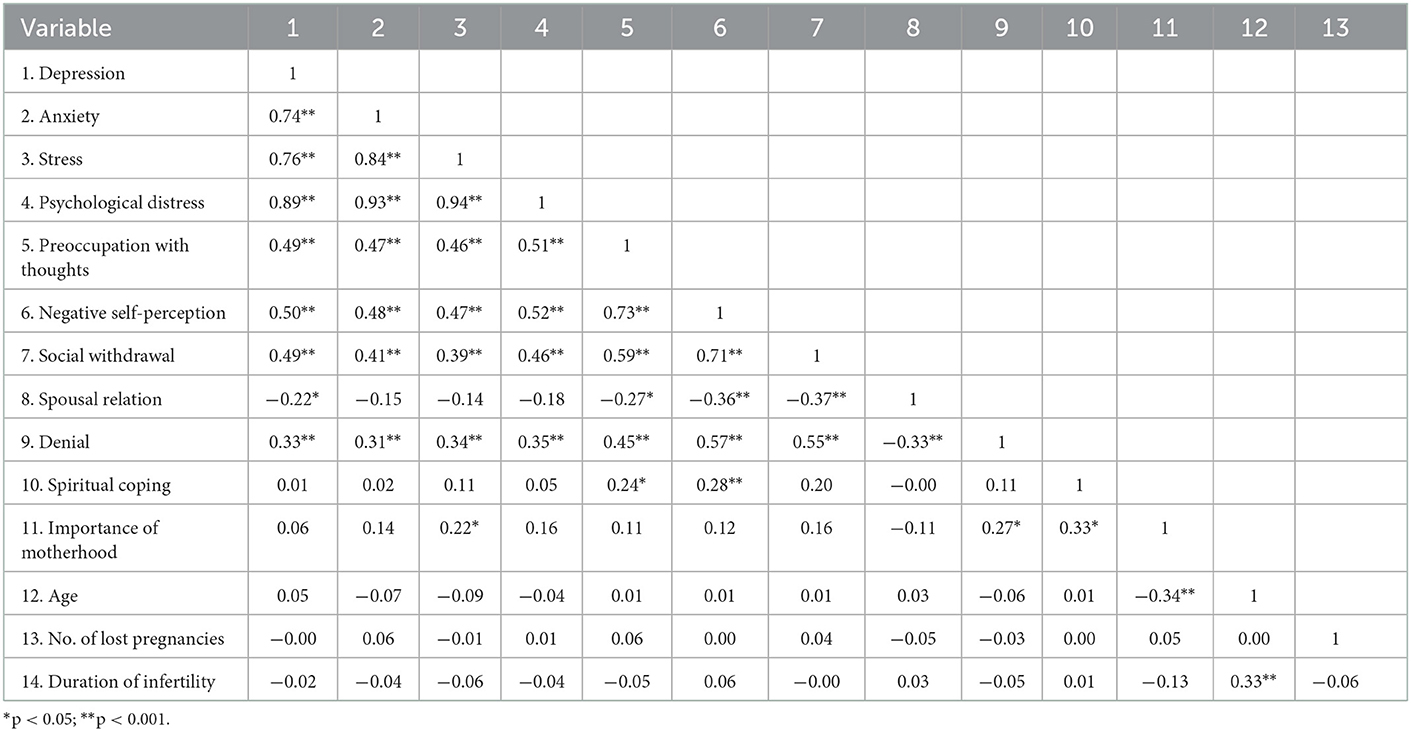
Table 3C. Zero-order correlations among the main variables — women who are not undergoing ART (N = 91).
In the overall sample, the results suggested significant associations between psychological distress and preoccupation with thoughts (r = 0.53, p < 0.001), negative self-perception (r = 0.50, p < 0.001), social withdrawal (r = 0.42, p < 0.001), spousal relations (r = −0.18, p = 0.01), denial (r = 0.31, p < 0.001), and spiritual coping (r = 0.15, p = 0.03). The importance of motherhood was significantly associated with stress (r = 0.16, p = 0.02), negative self-perception (r = 0.17, p = 0.01), social withdrawal (r = 0.15, p = 0.03), spousal relations (r = −0.14, p = 0.04), denial (r = 0.25, p < 0.001), and spiritual coping (r = 0.20, p < 0.001).
In the sample of participants who were not undergoing ART procedures at the time of the research (N = 91), the pattern of relations remained relatively similar. The results suggested significant associations between psychological distress and preoccupation with thoughts (r = 0.51, p < 0.001), negative self-perception (r = 0.52, p < 0.001), social withdrawal (r = 0.46, p < 0.001), and denial (r = 0.35, p < 0.001). The importance of motherhood was positively associated with stress (r = 0.22, p = 0.03), denial (r = 0.27, p = 0.008), and spiritual coping (r = 0.33, p = 0.001).
In the sample of participants who were undergoing ART procedures at the time of the research (N = 102), results suggested significant associations between psychological distress and preoccupation with thoughts (r = 0.52, p < 0.001), negative self-perception (r = 0.48, p < 0.001), social withdrawal (r = 0.40, p < 0.001), denial (r = 0.25, p < 0.001), and, in addition to the non-ART sample, we also found a significant association with spiritual coping (r = 20, p = 0.03). The importance of motherhood was positively associated with negative self-perception (r = 23, p = 0.01) and denial (r = 0.24, p = 0.01).
Mediation analyses
Based on the results from the correlation analyses, we further used the SPSS macro program PROCESS – Model 4 (30) [95% confidence interval (CI); 5,000 bootstrapped samples] to explore the potential mediating roles of the coping strategies on the link between the importance of motherhood and psychological distress. We examined these indirect effects separately (overall, ART, and non-ART samples).
a. The indirect effects of negative self-perception, social withdrawal, spousal relation, denial, and spiritual coping on the link between the importance of motherhood and psychological distress (overall sample, N = 193).
We ran the mediation analyses using all four mediators. The results suggested that the total effect of the importance of motherhood on psychological distress was not significant, b = 0.10, SE = 0.05, p = 0.07, 95% CI [−0.01; 0.2], and neither was the direct effect, b = 0.01, SE = 0.05, p = 0.07, 95% CI [−0.08; 0.12]. The only significant indirect effect was the one of negative-self-perception, b = 0.05, SE = 0.02, 95% CI [0.01; 0.11]. Thus, women's negative self-perception fully mediated the link between the importance of motherhood on psychological distress.
b. The indirect effects of negative self-perception and denial on the link between the importance of motherhood and psychological distress (ART sample, N = 102).
We ran the mediation analyses using both mediators. The results suggested that the total effect of the importance of motherhood on psychological distress was not significant, b = 0.09, SE = 0.08, p = 0.25, 95% CI [−0.07; 0.27], and neither was the direct effect, b = −0.01, SE = 0.07, p = 0.08, 95% CI [−0.17; 0.14]. The only significant indirect effect was the one of negative-self-perception, b = 0.09, SE = 0.05, 95% CI [0.01; 0.23]. Thus, as in the case of the overall sample, women's negative self-perception fully mediated the link between the importance of motherhood on psychological distress.
c. The indirect effects of denial and spiritual coping on the link between the importance of motherhood and psychological distress (non-ART sample, N = 91).
We ran the mediation analyses using both mediators. The results suggested that the total effect of the importance of motherhood on psychological distress was not significant, b = 0.12, SE = 0.08, p = 0.12, 95% CI [−0.03; 0.29], and neither was the direct effect, b = 0.06, SE = 0.08, p = 0.49, 95% CI [−0.11; 0.23]. The only significant indirect effect was the one of denial, b = 0.06, SE = 0.03, 95% CI [0.01; 0.14]. Thus, denial fully mediated the link between the importance of motherhood on psychological distress in the sample of women who were not undergoing ART procedures at the moment of research.
Discussion
The present study aimed to explore the associations between individual characteristics and coping strategies, situational characteristics related to infertility, and perceived-infertility-related factors, such as the perceived importance of motherhood. Our research was based on the multi-dimensional model of infertility-related stress proposed by Zurlo et al. (49).
In line with previous studies (90), our results suggested that the importance of motherhood was positively associated with psychological distress and coping strategies such as negative self-perception, social withdrawal, denial, and spiritual coping. This particular result might highlight the overwhelming role played by social norms that dictate the need to have children and consider motherhood a moral duty (32, 83, 88). Furthermore, mediation analysis results suggested that both in the overall sample and in the sample of women undergoing ART procedures, the negative self-perception fully mediated the link between the importance of motherhood on psychological distress. In the sample of participants who were not undergoing ART procedures at the time of the study, we found a significant indirect effect between the importance of motherhood on psychological distress. These results seem consistent with previous results suggesting that resorting to dysfunctional coping strategies such as avoidance or denial is usually associated with increased levels of psychological distress (35, 60).
Furthermore, these findings generally underline the similarities between the samples (overall, non-ART, and ART), with significant indirect effects of maladaptive coping strategies on the link between the value of motherhood and infertile women's depression, anxiety, and stress. The implications of these findings are both theoretical and practical: first, they add to the literature on psychological distress among infertile women by providing a comparative perspective between women undergoing ART procedures and those who are not. Second, these results highlight the need for psychological support and intervention strategies addressing maladaptive coping and its link with the value placed on motherhood and different social expectations regarding parenting roles (102).
Next, our results suggested marginally significant differences (which also underlines that we should interpret these results with caution) between the ART vs. non-ART samples concerning psychological distress, preoccupation with thoughts, and spiritual coping, with higher rates among non-ART women. In other words, though some studies suggested that ART procedures can be highly stressful for infertile couples (39, 40), our results seem to align with the ones suggested by Moura-Ramos et al. (41), suggesting that the infertile couples undergoing ART might be less stressed than the infertile couples who are not experiencing these procedures.
The low control over the desire to become a parent (i.e., infertility diagnosis) and the desire to achieve this goal might explain why, in the present study, the importance of motherhood was positively associated with stress, denial, and spiritual coping. Turning to religiosity might be a way to reduce infertility-related stress (68), as the desire for biological parenthood can also lead women to turn to religiosity before deciding to use ART (103). The idea is also supported by our results which suggested that, in the case of non-ART participants, the importance of motherhood was associated with religious coping, while in ART sample this association was not observed.
Our findings also suggested that participants' negative self-perception fully mediated the link between the importance of motherhood on psychological distress, both in the overall and in the ART samples. These results are in line with Cousineau and Domar (72), who suggested that one's self-perception can be affected by the value placed on motherhood. This result highlights the need for multidisciplinary teams (e.g., medical professionals and psychotherapists) to work with infertile women's psychological distress to help them overcome the social stigma of infertility.
Our results also suggested that in the case of the non-ART sample, denial fully mediated the link between the importance of motherhood on psychological distress. These results align with the idea that coping strategies can influence the acceptance or rejection of an infertility diagnosis and the option and adherence to treatment (65, 66). The desire to become a biological mother is so high sometimes that it causes infertile women to postpone turning to ART, hardly accepting the diagnosis. This result can be the basis of future psychoeducation interventions to facilitate decision-making among infertile women or couples and increase their wellbeing.
Regarding the current study, some limitations need to be addressed as well. First, our study is not as generalizable as it could have been because we employed a convenient sample size of participants that was relatively small (104). In subsequent research, it may be beneficial to investigate the correlations between the primary variables of our investigation in more comprehensive and diverse samples. We also used self-reported measurements, which enhanced the possibility of desirable answers. For future studies, it may be beneficial to use various assessment methods, such as experimental procedures, to address this limitation.
Another potential limitation might be related to the time of the study, i.e., the COVID-19 pandemic – at a time when the fear of COVID-19 challenged people worldwide. Thus, our findings should be interpreted cautiously, considering this specific factor in future ecological research perspectives. In this regard, the significant psychological impact of the COVID-19 pandemic on infertile women who had in-vitro treatment interrupted or postponed should be considered (105, 106).
Also, we did not assess the cultural particularities, even though we know that these aspects may play a significant part in discussing emotional repercussions connected to infertility. Furthermore, we used a cross-sectional approach, which does not allow us to draw any conclusions related to causal relationships between the variables, a limitation that future studies should address. Also, we focused only on heterosexual women, which might also limit the generalizability of our findings (107).
Also, we did not include several other variables that might account for significant changes in the relationships we examined. Out of these factors, we consider the partner's perspective on infertility, the importance of parenthood in men's lives, as well as men's psychological distress (41), might be considered in future studies that would further explore these links while also examining the role played by the COVID-19 pandemic in this regard (108). Also, in the demographic scale, we measured the perceived cause of infertility. Though our approach was not focused on this factor, future studies might want to account for the potential variabilities concerning this factor, especially in such religious contexts as the Romanian one. Next, while our research attempted to compare rural versus urban populations regarding the primary variables of our study, especially given the religious context, the two groups were too unbalanced for further analyses, an issue that might be addressed in further research. Finally, as we previously highlighted, the influence of cultural and religious factors on the value placed on motherhood and the choice to undergo ART is highly significant. However, the importance of these factors can also be regarded in terms of pregnancy termination decisions, and the perception (i.e., value) of motherhood (109, 110).
Our study was based on the multi-dimensional model of infertility-related stress proposed by Zurlo et al. (49). We added to this model the variables concerning the number of lost pregnancies as an infertility-related parameter and the ART-status variable since previous studies documented its important role when discussing infertility-related distress (39, 40). However, our findings did not suggest a significant link between psychological distress and the number of lost pregnancies. However, the differences we found between the ART and non-ART samples highlight the importance of the ART status when examining infertile women's emotional distress and coping strategies (a research path worth examining in future, more extended studies).
Conclusion
Infertility is a highly stressful life event with an even more significant impact on women's mental health if motherhood is considered a moral duty and a social imperative (91). At the same time, it might be even more stressful when dealing with unprecedented health crises, such as the COVID-19 pandemic. In addition to the theoretical insight added by our study, the practical implications are related to mental health professionals' awareness of the importance of motherhood on the mental health of infertile women, which may lead to a better therapeutic approach. The inclusion, in therapy, of techniques that can help to accept the unpredictability in reaching the proposed goal (e.g., fertility) and increasing the level of resilience can prevent the clinical pathology associated with infertility (primary prophylaxis) or can prevent complications and the unfavorable evolution of the mental health problems (secondary prevention).
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study's protocol was designed the following ethical requirements specific to the Faculty of Psychology and Educational Sciences, Alexandru Ioan Cuza University (Iasi, Romania) before beginning the study and supervised by Florentina-Larisa Foti. Ethical Approval No. 3058/28.09.2021. The patients/participants provided their written informed consent to participate in this study.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Funding
The authors are thankful to Romanian Ministry of Research, Innovation and Digitization, within Program 1 - Development of the National RD System, Subprogram 1.2 - Institutional Performance - RDI Excellence Funding Projects, Contract no.11PFE/30.12.2021 for financial support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Greil AL, Slauson-Blevins K, McQuillan J. The experience of infertility: a review of recent literature. Sociol Health Illness. (2010) 32:140–62. doi: 10.1111/j.1467-9566.2009.01213.x
2. Maftei A, Holman AC. Moral women, immoral technologies? Romanian women's perceptions of assisted reproductive technologies versus adoption. New Bioethics. (2020) 26:253–72. doi: 10.1080/20502877.2020.1796256
3. Greil AL, Schmidt L, Peterson BD. Understanding and treating the psychosocial consequences of infertility. In:Wenzel A., , editor. The Oxford Handbook of Perinatal Psychology. Oxford: Oxford University Press. (2016) p. 524–547.
4. Hazlina NHN, Norhayati MN, Bahari IS, Arif NANM. Worldwide prevalence, risk factors and psychological impact of infertility among women: a systematic review and meta-analysis. BMJ Open. (2022) 12:e057132. doi: 10.1136/bmjopen-2021-057132
5. Rautakallio-Hokkanen S (2018). Available online at: http://wwwfertilityeuropeeu/fertility-ed/ (accessed November 30, 2019).
6. The Romanian Association for Human Reproduction (2018). The first analysis study of infertility problems in Romania. Available online at: https://www.arur.ro/2018/06/18/855/ (accessed August 2, 2022).
7. Poote AE, van den Akker OB. British women's attitudes to surrogacy. Human Reprod. (2009) 24:139–45. doi: 10.1093/humrep/den338
8. Jain M, Singh M. Assisted Reproductive Technology (ART) techniques. In: StatPearls. StatPearls Publishing (2021).
9. Margan R, Margan MM, Fira-Mladinescu C, Putnoky S, Tuta-Sas I, Bagiu R, et al. Impact of stress and financials on Romanian infertile women accessing assisted reproductive treatment. Int J Environ Res Public Health. (2022) 19:3256. doi: 10.3390/ijerph19063256
10. Purewal S, Chapman S, van den Akker O. A systematic review and meta-analysis of psychological predictors of successful assisted reproductive technologies. BMC Res Notes. (2017) 10:711. doi: 10.1186/s13104-017-3049-z
11. Purewal S, Chapman S, van den Akker O. Depression and state anxiety scores during assisted reproductive treatment are associated with outcome: a meta-analysis. Reprod Biomed Online. (2018) 36:646–57. doi: 10.1016/j.rbmo.2018.03.010
12. Rooney KL, Domar AD. The relationship between stress and infertility. Dialog Clin Neurosci. (2022) 20:41–7. doi: 10.31887/DCNS.2018.20.1/klrooney
13. Nasim S, Bilal S, Qureshi M. Psycho-social aspects of infertility-a review of current trends. Professional Med J. (2019) 26:1537–41. doi: 10.29309/TPMJ/2019.26.09.4019
14. Steuber KR, Haunani Solomon D. Relational uncertainty, partner interference, and infertility: A qualitative study of discourse within online forums. J Soc Pers Relat. (2008) 25:831–55. doi: 10.1177/0265407508096698
15. Cudmore L. Becoming parents in the context of loss. Sexual Relation Ther. (2005) 20:299–308. doi: 10.1080/14681990500141204
16. Hasanpoor-Azghdy SB, Simbar M, Vedadhir A. The Social Consequences of Infertility among Iranian Women: A Qualitative Study. Int J Fertil Steril. (2015) 8:409–20. doi: 10.22074/ijfs.2015.4181
17. Zarif Golbar Yazdi H, Aghamohammadian Sharbaf H, Kareshki H, Amirian M. Infertility and psychological and social health of iranian infertile women: a systematic review. Iran J Psychiatry. (2020) 15:67–79. doi: 10.18502/ijps.v15i1.2441
18. El Kissi Y, Romdhane AB, Hidar S, Bannour S, Ayoubi Idrissi K, Khairi H, et al. General psychopathology, anxiety, depression and self-esteem in couples undergoing infertility treatment: a comparative study between men and women. Eur J Obstet Gynecol Reprod Biol. (2013) 167:185–9. doi: 10.1016/j.ejogrb.2012.12.014
19. Wischmann T, Schilling K, Toth B, Rösner S, Strowitzki T, Wohlfarth K, et al. Sexuality, self-esteem and partnership quality in infertile women and men. Geburtshilfe Frauenheilkd. (2014) 74:759–63. doi: 10.1055/s-0034-1368461
20. Porter AC, Zelkowitz RL, Gist DC, Cole DA. Self-evaluation and depressive symptoms: a latent variable analysis of self-esteem, shame-proneness, and self-criticism. J Psychopathol Behav Assess. (2019) 41:257–70. doi: 10.1007/s10862-019-09734-1
21. Viertiö S, Kiviruusu O, Piirtola M, Kaprio J, Korhonen T, Marttunen M, et al. Factors contributing to psychological distress in the working population, with a special reference to gender difference. BMC Public Health. (2021) 21:611. doi: 10.1186/s12889-021-10560-y
22. Faramarzi M, Pasha H, Esmaelzadeh S, Jorsarai G, Mir MR, Abedi S. Is coping strategies predictor of anxiety and depression in couple infertile? Health. (2013) 5:643–649. doi: 10.4236/health.2013.53A085
23. Iordăchescu DA, Paica CI, Boca AE, Gică C, Panaitescu AM, Peltecu G, et al. Anxiety, difficulties, and coping of infertile women. Healthcare (Basel, Switzerland). (2021) 9:466. doi: 10.3390/healthcare9040466
24. Iordăchescu DA, Gica C, Vladislav EO, Panaitescu AM, Peltecu G, Furtuna ME, et al. Emotional disorders, marital adaptation and the moderating role of social support for couples under treatment for infertility. Ginekol Pol. (2021) 92:98–104. doi: 10.5603/GP.a2020.0173
25. Kiani Z, Simbar M, Hajian S, Zayeri F. The prevalence of depression symptoms among infertile women: a systematic review and meta-analysis. Fertility Res Pract. (2021) 7:6. doi: 10.1186/s40738-021-00098-3
26. Hawkey AJ, Ussher JM, Perz J. “If you don't have a baby, you can't be in our culture”: Migrant and refugee women's experiences and constructions of fertility and fertility control. Women's Reprod Health. (2018) 5:75–98. doi: 10.1080/23293691.2018.1463728
27. Li H, Lei J, Xu F, Yan C, Guimerans M, Xing H, et al. A study of sociocultural factors on depression in Chinese infertile women from Hunan Province. J Psychosom Obstet Gynaecol. (2017) 38:12–20. doi: 10.1080/0167482X.2016.1265500
28. Yusuf L. Depression, anxiety and stress among female patients of infertility; A case control study. Pakistan J Med Sci. (2016) 32:1340–3. doi: 10.12669/pjms.326.10828
29. Raque-Bogdan TL, Hoffman MA. The relationship among infertility, self-compassion, and well-being for women with primary or secondary infertility. Psychol Women Q. (2015) 39:484–96. doi: 10.1177/0361684315576208
30. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: Guilford Press. (2013).
31. Ho TTT, Le MT, Truong QV, Nguyen VQH, Cao NT. Psychological burden in couples with infertility and its association with sexual dysfunction. Sex Disabil. (2020) 38:123–33. doi: 10.1007/s11195-019-09612-4
32. McQuillan J, Greil AL, Shreffler KM, Tichenor V. The Importance of Motherhood Among Women in the Contemporary United States. Gender Soc. (2008) 22:477–496. doi: 10.1177/0891243208319359
33. Kiani Z, Simbar M, Hajian S, Zayeri F, Shahidi M, Saei Ghare Naz M, et al. The prevalence of anxiety symptoms in infertile women: a systematic review and meta-analysis. Fertility Res Pract. (2020) 6:7. doi: 10.1186/s40738-020-00076-1
34. Cui C, Wang L, Wang X. Effects of self-esteem on the associations between infertility-related stress and psychological distress among infertile chinese women: a cross-sectional study. Psychol Res Behav Manag. (2021) 14:1245–55. doi: 10.2147/PRBM.S326994
35. Khalid A, Dawood S. Social support, self-efficacy, cognitive coping and psychological distress in infertile women. Arch Gynecol Obstet. (2020) 302:423–30. doi: 10.1007/s00404-020-05614-2
36. Upkong D, Orji E. Nijerya'daki Infertil Kadinlarda Ruh Sagligi [Mental health of infertile women in Nigeria]. Turk Psikiyatri Derg. (2006) 17:259–65.
37. Lakatos E, Szigeti JF, Ujma PP, Sexty R, Balog P. Anxiety and depression among infertile women: a cross-sectional survey from Hungary. BMC Women's Health. (2017) 17:48. doi: 10.1186/s12905-017-0410-2
38. Galhardo A, Alves J, Moura-Ramos M, Cunha M. Infertility-related stress and depressive symptoms - the role of experiential avoidance: a cross-sectional study. J Reprod Infant Psychol. (2020) 38:139–50. doi: 10.1080/02646838.2019.1612046
39. Maroufizadeh S, Karimi E, Vesali S, Omani Samani R. Anxiety and depression after failure of assisted reproductive treatment among patients experiencing infertility. Int J Gynaecol Obstetr. (2015) 130:253–6. doi: 10.1016/j.ijgo.2015.03.044
40. Reis S, Xavier MR, Coelho R, Montenegro N. Psychological impact of single and multiple courses of assisted reproductive treatments in couples: a comparative study. Eur J Obstet Gynecol Reprod Biol. (2013) 171:61–6. doi: 10.1016/j.ejogrb.2013.07.034
41. Moura-Ramos M, Gameiro S, Canavarro MC, Soares I, Almeida-Santos T. Does infertility history affect the emotional adjustment of couples undergoing assisted reproduction? the mediating role of the importance of parenthood. Br J Health Psychol. (2016) 21:302–17. doi: 10.1111/bjhp.12169
42. Bhat A, Byatt N. Infertility and perinatal loss: when the bough breaks. Curr Psychiatry Rep. (2016) 18:31. doi: 10.1007/s11920-016-0663-8
43. Wallis ELG. Women's narratives of miscarriage and their role in identity construction (Doctoral dissertation, University of Hertfordshire). (2021).
44. Wenzel A. Infertility, Miscarriage, and Neonatal Loss. In: The Wiley Encyclopedia of Health Psychology. (2020). p. 27–33. doi: 10.1002/9781119057840.ch136
45. Maroufizadeh S, Ghaheri A, Almasi-Hashiani A, Mohammadi M, Navid B, Ezabadi Z, et al. The prevalence of anxiety and depression among people with infertility referring to Royan Institute in Tehran, Iran: A cross-sectional questionnaire study. Middle East Fertil Soc J. (2018) 23:103–6. doi: 10.1016/j.mefs.2017.09.003
46. Negoi?ă V, Băban A. Depression, anxiety and self-esteem among infertile women: a systematic review of literature. Studia Univ Babes-Bolyai, Psychol Paedag. (2020) 65:87–112. doi: 10.24193/subbpsyped.2020.2.04
47. Simionescu G, Doroftei B, Maftei R, Obreja BE, Anton E, Grab D, et al. The complex relationship between infertility and psychological distress. Exp Ther Med. (2021) 21:1–1. doi: 10.3892/etm.2021.9737
48. Wu G, Yin T, Yang J, Xu W, Zou Y, Wang Y, et al. Depression and coping strategies of Chinese women undergoing in-vitro fertilization. Eur J Obstet Gynecol Reprod Biol. (2014) 183:155–8. doi: 10.1016/j.ejogrb.2014.10.019
49. Zurlo MC, Cattaneo Della Volta MF, Vallone F. Re-examining the role of coping strategies in the associations between infertility-related stress dimensions and state-anxiety: implications for clinical interventions with infertile couples. Front Psychol. (2020) 11:614887. doi: 10.3389/fpsyg.2020.614887
50. Abbasi S, Kousar R, Sadiq SS. Depression and anxiety in pakistani infertile women. J Surg Pakistan. (2016) 21:13–7. doi: 10.21699/jsp.21.1.4
51. Ogawa M, Takamatsu K, Horiguchi F. Evaluation of factors associated with the anxiety and depression of female infertility patients. Biopsychosoc Med. (2011) 5:15. doi: 10.1186/1751-0759-5-15
52. Lazarus RS, Folkman S. Transactional theory and research on emotions and coping. Eur J Person. (1987) 1:141–169. doi: 10.1002/per.2410010304
53. Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York NY: Springer Publishing Company. (1984).
54. Folkman S, Moskowitz JT. Coping: pitfalls and promise. Annu Rev Psychol. (2004) 55:745–74. doi: 10.1146/annurev.psych.55.090902.141456
55. Omani Samani R, Maroufizadeh S, Navid B, Amini P. Locus of control, anxiety, and depression in infertile patients. Psychol Health Med. (2017) 22:44–50. doi: 10.1080/13548506.2016.1231923
56. Mitrović M, Kostić JO, Ristić M. Intolerance of uncertainty and distress in women with delayed IVF treatment due to the COVID-19 pandemic: The mediating role of situation appraisal and coping strategies. J Health Psychol. (2021) 27:2515–28. doi: 10.1177/13591053211049950
57. Zurlo MC, Cattaneo Della Volta MF, Vallone F. Predictors of quality of life and psychological health in infertile couples: the moderating role of duration of infertility. Quality of Life Res. (2018) 27:945–54. doi: 10.1007/s11136-017-1781-4
58. Saif J, Rohail DI, Aqeel M. Quality of life, coping strategies, and psychological distress in women with primary and secondary infertility; a mediating model. Nat Nurture J Psychol. (2021) 1:8–17.
59. Sexton MB, Byrd MR, von Kluge S. Measuring resilience in women experiencing infertility using the CD-RISC: examining infertility-related stress, general distress, and coping styles. J Psychiatr Res. (2010) 44:236–41. doi: 10.1016/j.jpsychires.2009.06.007
60. Nagórska M, Obrzut B, Ulman D, Darmochwał-Kolarz D. The need of personalized medicine in coping with stress during infertility treatment. J Pers Med. (2021) 11:56. doi: 10.3390/jpm11010056
61. Mohammadi M, Samani RO, Navid B, Maroufizadeh S, Sabeti S. Coping strategy in infertile couples undergoing assisted reproduction treatment. Middle East Fertil Soc J. (2018) 23:482–5. doi: 10.1016/j.mefs.2018.07.004
62. Benyamini Y, Gefen-Bardarian Y, Gozlan M, Tabiv G, Shiloh S, Kokia E. Coping specificity: the case of women coping with infertility treatments. Psychol Health. (2008) 23:221–41. doi: 10.1080/14768320601154706
63. Nelson A, Gellar PA. Coping with fertility treatment: Infertility-related stress and social support among women receiving in vitro fertilization. Gend Med. (2011) 9:S100. doi: 10.1016/j.genm.2011.09.023
64. Karaca A, Ünsal G, Asik E, Keser I, Ankarali H, Merih YD. Development and assessment of a coping scale for infertile women in Turkey. Afr J Reprod Health. (2018) 22:13–23. doi: 10.29063/ajrh2018/v22i3.2
65. Dembińska A. Selected psychological and sociodemographic correlates of the acceptance of one's own infertility in women. Psychiatria i Psychologia Kliniczna. (2019) 19:308–14. doi: 10.15557/PiPK.2019.0032
66. Turabian JL. Doctor-patient relationship in the case of infertility: A vision from general medicine. Adv Reprod Sci Reprod Health Infert. (2019) 1:104. doi: 10.29011/ARRHI-104.100004
67. David D. Psihologia poporului român. Profilul psihologic al românilor într-o monografie cognitiv-experimentală [Psychology of the Romanian people. The psychological profile of Romanians in a cognitive-experimental monograph]. Romania, Iaşi: Polirom. (2015).
68. Pargament KI, Raiya HA. A decade of research on the psychology of religion and coping: Things we assumed and lessons we learned. Psyke Logos. (2007) 28:742–66. doi: 10.7146/pl.v28i2.8398
69. Oti-Boadi M, Asante KO. Psychological health and religious coping of Ghanaian women with infertility. Biopsychosoc Med. (2017) 11:1–7. doi: 10.1186/s13030-017-0105-9
70. Aflakseir A, Mahdiyar M. The role of religious coping strategies in predicting depression among a sample of women with fertility problems in Shiraz. J Reprod Infert. (2016) 17:117–22.
71. Casu G, Ulivi G, Zaia V, Fernandes Martins M, Parente Barbosa C, Gremigni P. Spirituality, infertility-related stress, and quality of life in Brazilian infertile couples: Analysis using the actor-partner interdependence mediation model. Res Nurs Health. (2018) 41:156–65. doi: 10.1002/nur.21860
72. Cousineau TM, Domar AD. Psychological impact of infertility. Best Pract Res Clin Obstetr Gynaecol. (2007) 21:293–308. doi: 10.1016/j.bpobgyn.2006.12.003
73. Avşar B, Emul TG. The relationship between social support perceived by infertile couples and their mental status. Res Square. (2021). doi: 10.21203/rs.3.rs-487754/v1
74. Karaca A, Unsal G. Psychosocial Problems and Coping Strategies among Turkish Women with Infertility. Asian Nurs Res. (2015) 9:243–50. doi: 10.1016/j.anr.2015.04.007
75. Coşkuner Potur D, Güngör Satilmiş I, Dogan Merih Y, Gün Kakaşçi Ç, Demirci N, Ersoy M. Does infertility affect the sexual function and sexual quality of life of women? A case control study. Int J Sexual Health. (2020) 32:22–32. doi: 10.1080/19317611.2019.1692983
76. Dube L, Nkosi-Mafutha N, Balsom AA, Gordon JL. Infertility-related distress and clinical targets for psychotherapy: a qualitative study. BMJ Open. (2021) 11:e050373. doi: 10.1136/bmjopen-2021-050373
77. Clark LF, Henry SM, Taylor DM. Cognitive examination of motivation for childbearing as a factor in adjustment to infertility. In:Stanton AL, Dunkel-Schetter C., , editors. Infertility: Perspectives from stress and coping research. New York, NY: Plenum Press. (1991). p. 157–180. doi: 10.1007/978-1-4899-0753-0_8
78. Poddar S, Sanyal N, Mukherjee U. Psychological profile of women with infertility: A comparative study. Ind Psychiatry J. (2014) 23:117–26. doi: 10.4103/0972-6748.151682
79. Hocaoglu C. The psychosocial aspect of infertility. Infertil Assist Reprod Technol Hormone Assays. (2019) 65:80713. doi: 10.5772/intechopen.80713
80. Ahmadi SE, Rafiey H, Sajjadi H, Nosratinejad F. Explanatory model of voluntary childlessness among iranian couples in tehran: a grounded theory approach. Iran J Med Sci. (2019) 44:449–56. doi: 10.30476/ijms.2019.44964
81. Ulrich M, Weatherall A. Motherhood and infertility: viewing motherhood through the lens of infertility. Feminism Psychol. (2000) 10:323–36. doi: 10.1177/0959353500010003003
82. Aflakseir A, Zarei M. Association between coping strategies and infertility stress among a group of women with fertility problem in Shiraz, Iran. J Reprod Infert. (2013) 14:202–6.
83. Maftei A, Holman A-C, Marchis M. Choosing a life with no children. The role of sexism on the relationship between religiosity and the attitudes toward voluntary childlessness. Curr Psychol. (2021). doi: 10.1007/s12144-021-02446-4
84. Ashburn-Nardo L. Parenthood as a moral imperative? Moral outrage and the stigmatization of voluntarily childfree women and men. Sex Roles. (2017) 76:393–401. doi: 10.1007/s11199-016-0606-1
85. Dever M, Saugeres L. I forgot to have children! Untangling links between feminism, careers and voluntary childlessness. J Assoc Res Mothering. (2004) 6:116–26.
86. Bays A. Perceptions, emotions, and behaviors toward women based on parental status. Sex Roles. (2017) 76:138–55. doi: 10.1007/s11199-016-0655-5
87. Bădescu G, Comşa M, Sandu D, Stănculescu M. Barometrul de Opinie Publică 1998–2007 [Barometer for Public Opinion 1998–2007]. SOROS Foundation. (2007).
88. Abbey A. Adjusting to infertility. In:Harvey JH, Miller ED, , editors. Loss and Trauma. New York, NY: Routledge. (2021). p. 331–344. doi: 10.4324/9781315783345-23
89. Taebi M, Kariman N, Montazeri A, Alavi Majd H. Infertility stigma: a qualitative study on feelings and experiences of infertile women. Int J Fertil Sterility. (2021) 15:189–96.
90. Li X, Ye L, Tian L, Huo Y, Zhou M. Infertility-Related stress and life satisfaction among chinese infertile women: a moderated mediation model of marital satisfaction and resilience. Sex Roles. (2020) 82:44–52. doi: 10.1007/s11199-019-01032-0
91. Miles LM, Keitel M, Jackson M, Harris A, Licciardi F. Predictors of distress in women being treated for infertility. J Reprod Infant Psychol. (2009) 27:238–57. doi: 10.1080/02646830802350880
92. McQuillan J, Torres Stone RA, Greil AL. Infertility and life satisfaction among women. J Fam Issues. (2007) 28:955–81. doi: 10.1177/0192513X07300710
93. Abbey A, Andrews FM, Halrnan LJ. Gender's role in responses to infertility. Psychol Women Q. (1991) 15:295–316. doi: 10.1111/j.1471-6402.1991.tb00798.x
94. Evans J, Baronavski C. How do European countries differ in religious commitment? Use our interactive map to find out. (2018). Available online at: https://www.pewresearch.org/religion/2018/10/29/eastern-and-western-europeans-differ-on-importance-of-religion-views-of-minorities-and-key-social-issues/ (accessed August 2, 2022).
95. Maftei A, Ghergu? A, Roca D, Dănilă O. Transitioning from decades of segregation: Religiosity and the attitudes towards intellectual disability in Romania. J Belief Value. (2020) 1–15. doi: 10.1080/13617672.2022.212567
96. European Commission (2019),. Romania: Population: Demographic situation, official language, and religions. Available online at: https://eacea.ec.europa.eu/national-policies/eurydice/content/population-demographic-situation-languages-and-religions-64_ro (accessed August 2, 2022).
97. Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. (2nd. Ed.) Sydney: Psychology Foundation. (1995). doi: 10.1037/t01004-000
98. International Test Commission. (2017). The ITC Guidelines for Translating and Adapting Tests (Second edition). Available online at: www.InTestCom.org (accessed August 2, 2022).
99. Sousa VD, Rojjanasrirat W. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: a clear and user-friendly guideline. J Eval Clin Pract. (2011) 17:268–274. doi: 10.1111/j.1365-2753.2010.01434.x
100. Tyupa S. A theoretical framework for back-translation as a quality assessment tool. New Voices Transl Stud. (2011) 7:35–46.
101. George D, Mallery P. SPSS for Windows Step by Step: A Simple Guide and Reference 17.0 Update. 10th Edition. Boston: Pearson. (2010).
102. Moura-Ramos M, Gameiro S, Canavarro MC, Soares I. Assessing infertility stress: re-examining the factor structure of the Fertility Problem Inventory. Hum Reprod. (2011) 27:496–505. doi: 10.1093/humrep/der388
103. Czarnecki D. Moral women, immoral technologies: how devout women negotiate gender, religion, and assisted reproductive technologies. Gender Soc. (2015) 29:716–42. doi: 10.1177/0891243215591504
104. Crossman A. Convenience samples for research. Thought Co. (2018). Available online at: http://www.thoughtco.com/convenience-sampling-3026726 (accessed August 2, 2022).
105. Barra F, La Rosa VL, Vitale SG, Commodari E, Altieri M, Scala C, et al. Psychological status of infertile patients who had in vitro fertilization treatment interrupted or postponed due to COVID-19 pandemic: a cross-sectional study. J Psychosom Obstet Gynaecol. (2022) 43:145–52. doi: 10.1080/0167482X.2020.1853095
106. Lablanche O, Salle B, Perie MA, Labrune E, Langlois-Jacques C, Fraison E. Psychological effect of COVID-19 pandemic among women undergoing infertility care, a French cohort - PsyCovART Psychological effect of COVID-19: PsyCovART. J Gynecol Obstetr Human Reprod. (2022) 51:102251. doi: 10.1016/j.jogoh.2021.102251
107. Walks M. Breaking the silence: Infertility, motherhood, and queer culture. J Assoc Res Mothering. (2007) 9:130–43.
108. Trinchant RM, Cruz M, Marqueta J, Requena A. Infertility and reproductive rights after the COVID-19 pandemic. Reprod Biomed Online. (2020) 41:151–3. doi: 10.1016/j.rbmo.2020.05.007
109. Zareba K, La Rosa VL, Ciebiera M, Makara-Studzińska M, Gierus J, Jakiel G. Psychosocial profile and reproductive decisions of women undergoing pregnancy termination for medical reasons-a cross-sectional study. Int J Environ Res Public Health. (2019) 16:3413. doi: 10.3390/ijerph16183413
Keywords: infertility, women, psychological distress, coping strategies, motherhood
Citation: Foti FL, Karner-Huţuleac A and Maftei A (2023) The value of motherhood and psychological distress among infertile women: The mediating role of coping strategies. Front. Public Health 11:1024438. doi: 10.3389/fpubh.2023.1024438
Received: 21 August 2022; Accepted: 06 January 2023;
Published: 02 February 2023.
Edited by:
Giulia Casu, University of Bologna, ItalyReviewed by:
Amanda Wilson, De Montfort University, United KingdomJean Marie Place, Ball State University, United States
Valentina Lucia La Rosa, University of Catania, Italy
Copyright © 2023 Foti, Karner-Huţuleac and Maftei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alexandra Maftei,  YWxleGFuZHJhLm1hZnRlaUB1YWljLnJv
YWxleGFuZHJhLm1hZnRlaUB1YWljLnJv
 Florentina Larisa Foti
Florentina Larisa Foti Adina Karner-Huţuleac
Adina Karner-Huţuleac Alexandra Maftei
Alexandra Maftei