- 1School of Medicine, Chongqing University, Chongqing, China
- 2Chongqing Cancer Multi-omics Big Data Application Engineering Research Center, Chongqing University Cancer Hospital, Chongqing, China
- 3Radiation Oncology Center, Chongqing University Cancer Hospital, Chongqing, China
Objective: Health insurance programs are effective in preventing financial hardship in patients with cancer. However, not much is known about how health insurance policies, especially in Southwest China with a high incidence of nasopharyngeal carcinoma (NPC), influence patients’ prognosis. Here, we investigated the association of NPC-specific mortality with health insurance types and self-paying rate, and the joint effect of insurance types and self-paying rate.
Materials and methods: This prospective cohort study was conducted at a regional medical center for cancer in Southwest China and included 1,635 patients with pathologically confirmed NPC from 2017 to 2019. All patients were followed up until May 31, 2022. We determine the cumulative hazard ratio of all-cause and NPC-specific mortality in the groups of various insurance kinds and the self-paying rate using Cox proportional hazard.
Results: During a median follow-up period of 3.7 years, 249 deaths were recorded, of which 195 deaths were due to NPC. Higher self-paying rate were associated with a 46.6% reduced risk of NPC-specific mortality compared to patients with insufficient self-paying rate (HR: 0.534, 95% CI: 0.339–0.839, p = 0.007). For patients covered by Urban and Rural Residents Basic Medical Insurance (URRMBI), and for patients covered by Urban Employee Basic Medical Insurance, each 10% increase in the self-paying rate reduced the probability of NPC-specific death by 28.3 and 25%, respectively (UEBMI).
Conclusion: Results of this study showed that, despite China’s medical security administration improved health insurance coverage, NPC patients need to afford the high out-of-pocket medical costs in order to prolong their survival time.
Introduction
Nasopharyngeal carcinoma (NPC) has a notable ethnic and geographic distribution, with a predominance in southern China and southeast Asia (1). Although NPC is fairly uncommon in several jurisdictions, it remains a significant public health problem in South China, which accounted for more than 40% of the approximate 130,000 patients worldwide in 2020 (2, 3). Radiotherapy or chemoradiotherapy is considered the primary radical treatment for non-metastatic NPC and the 3-year failure-free survival rate for non-metastatic patients exceeds 80% (4–6). Cancer survival now means living with a chronic and complex condition. Thus, the long-term management and care for cancer survivors bring severe financial stress to individuals and their families, particularly in the great majority of less developed countries where the public healthcare system is inadequate to lessen the burden on citizens (7, 8).
The presence of medical insurance system is considered a means of reducing the financial burden of cancer prevention and treatment, which seems essential for a country to achieve universal healthcare coverage and health equity. The majority of studies on the correlation between medical insurance and cancers have focused on geographical variations in health insurance coverage for cancer patients (9, 10), differences in the financial burden of cancer patients by type of health insurance (11–15), and the coverage of new types of anti-cancer treatments by health insurance policies (16–19). Fewer shreds of evidence have shown the influence of current medical insurance policies on cancer prognosis. So far, only studies on liver (20), lung (21), and breast cancers (22, 23) have suggested that underinsured patients have an increased risk of death and patients require higher out-of-pocket costs to reduce this risk. However, it is unknown whether the medical insurance policies, especially in high incidence areas of NPC, where the patients may afford higher self-paying rate, influence cancer prognosis. Therefore, we sought to investigate the association between health insurance types and self-paying rate and the incidence of NPC-specific death, as well as the joint effect of insurance types and self-paying rate, using a prospective cohort of patients diagnosed with NPC from 2017 to 2019.
Materials and methods
Patients selection
The medical database of Chongqing University Cancer Hospital covers almost all patients with nasopharyngeal carcinoma diagnosed in Chongqing since 2017, which is the foundation of this prospective cohort study. We enrolled 1,635 patients between May 31, 2017 and May 31, 2019. Clinical records were independently reviewed through the hospital’s electronic medical record database to prospectively gather data on demographic and clinical traits, lab tests, and treatments. In addition, patients with the following characteristics were excluded: (1) Non-primary NPC, (2) Pathologically confirmed non-squamous cell carcinoma, (3) Most of the treatment was not performed at our institution, (4) Missing data information collected, (5) Minors (17 years old and younger), and (6) No follow-up records.
Health insurance
China’s basic medical insurance is a national, provincial, municipal, and county-level system. The Urban Employee Basic Medical Insurance Scheme (UEBMI), which covers only unit employees, was implemented in 1998. The New Rural Cooperative Medical Scheme (NRCMS), which covers rural residents, was implemented in 2003. The Urban Residents Basic Medical Insurance Scheme (URBMI), which covers urban non-workers (students, children and youth, non-working urban residents, etc.), was implemented in 2007. URBMI and NRCMS merged in 2016 to create a basic medical insurance plan for urban and rural residents (URRBMI). Both types of medical insurance cover the same services, but their reimbursement ratios differ. As of 2019, the UEBMI reimbursement ratio in Chongqing is 83% and the URRBMI ratio is 75%. This difference is due to different insurance contributions. Chongqing’s 2020 URRBMI contribution rate is 220 or 550 RMB/person-years, but UEBMI requires a minimum health insurance contribution of 4,189 RMB/person-years, 20% of which is paid by the individual and the remainder is paid by the employer. Due to different contribution methods, reimbursement comes from different places. Individual contributions and government subsidies fund URRBMI, while UEBMI has individual accounts (individual contribution plus a small portion of unit contribution) and coordinated funds (the majority of the unit portion of the contribution plus government subsidies, funding, etc.). Geography (inside and outside the city), contribution status (contribution interruption, contribution years), and hospital level also affect reimbursement rate (Level I, II, III). The municipal government coordinates the regional implementation of health insurance reimbursement’s complex calculation. During treatment, patients must pay for medications, treatment items, and medical services that are not covered by their basic medical insurance, and the self-paying rate is the proportion of this cost to the patient’s total treatment cost.
The Chongqing University Cancer Hospital’s information system (HIS) provides data on the types of medical insurance and hospitalization expenses. Due to the time window of medical insurance policy implementation, URRBMI in this study refers to both URMBI and URRBMI medical insurance types, which differ in terms of administration and reimbursement rate insignificantly. During the statistical analysis, there were only 44 NRCMS, so they were excluded from the study; additionally, 393 patients were publicly funded, self-funded, covered by commercial insurance, or had blank registration information, so they were excluded from the study; 11 patients with unclear costs were also excluded. For further analysis of health insurance efficacy, by referring to the literature of similar studies (21, 22) in conjunction with our study, we calculated median values for health self-paying rate (56.8% for URRBMI and 46.8% for UEBMI), and we divided the self-paying rate into a low (0–50%) and a high (> 50%) group for inclusion in the analysis.
Outcome and follow-up
The primary outcome in this study was NPC-specific death, and the secondary outcome was all-cause death. Patients were followed up from the day they were diagnosed with NPC until the event (death) occurred or the follow-up cut-off time passed (May 31, 2022). The follow-up data were obtained from the records of patients’ voluntary follow-up visits to our hospital and telephone follow-ups received from our hospital at 3–6 months intervals by patients or their immediate family members. Multiple relatives were sought in cases of death, and medical records were thoroughly examined to adequately define the type of death and reduce research error.
Statistical analysis
First, we ran descriptive statistics on patient demographic and clinical baseline data, reporting count data as frequencies and percentages. Demographic and clinical baseline characteristics were counted for each insurance type and self-paying rate grouping, and differences were examined using chi-square tests. After controlling for demographic and clinical factors, we used logistic regression to investigate the relationship between health insurance type, out-of-pocket costs, and several NPC treatment modalities (radiotherapy, chemotherapy, and targeted therapy). Subsequently, we used Cox regression models to compare the hazard ratios (HRs) and 95% confidence intervals for cancer-specific and all-cause mortality for patients with URRMBI and UEMBI, as well as for NPC patients with less than 50% and greater than or equal to 50% self-paying rate. Finally, the impacts of medical insurance type and self-paying rate on mortality risk were examined for joint effects, as well as the link between each 10% rise in deductible and the probability of death from any cause as well as from NPC-specific causes was examined.
We built three models in analysis to reduce the possibility of confounding bias from other factors. We adjusted for demographic factors and tumor characteristics such as age, gender, ethnic group, marital status, occupation, tumor stage, and tumor histopathological classification in model A. Model B was based on model A, with additional adjustments for potential clinical indicators affecting the prognosis of NPC patients including such plasma EBV viral DNA load, serum albumin to globulin ratio(A/G) (24), lactate dehydrogenase to albumin ratio(LAR) (25), peripheral blood neutrophil count to lymphocyte count ratio(NLR) (26), and peripheral blood platelet count to lymphocyte count ratio(PLR) (25). Similar to model B, model C was based on it and controls for different treatment modalities, like radiotherapy, chemotherapy, and targeted therapy. Before including the data on clinical continuous variables in the analysis, we categorized them by reviewing the literature or using X-tile software to find truncation values.
Software R (version 4.0.2; R Foundation for Statistical Computing, Vienna, Austria) and SAS9.4 statistical software (version 9.4; SAS Institute Inc., Cary, North Carolina) were used to analyze all of the data. p < 0.05 indicates a statistically significant difference.
Results
Patients’ characteristics
Applying the inclusion and exclusion standards, there were 1,635 patients with NPC of which 446 (27.28%) were females and 1,189 (72.72%) were males in the final cohort. They were almost Han and only 221 were minorities, with a median age of 51 years old. Their tumors were more likely to be non-metastatic (91.31%), undifferentiated (40.37%), and to have the locally advanced stage. Among the included study subjects, 1,055 (64.5%) patients were insured by URBMI, and the remaining 580 (35.5%) patients were insured by UEBMI. The median self-paying rate in URRBMI was 56.8%, whereas it was 46.8% in UEBMI. When categorized at a 50% deductible, 667 patients were below 50%, while the remaining 968 patients were above or just 50%. Most of the younger patients were covered by UEBMI, and there were no differences in marital status and gender between the different insurance types. Clinical stage and EBV copy number were statistically significant in the self-paying rate group. Table 1 shows the full study results.
Health insurance type, self-paying rate, and NPC treatment
We investigated the association of the groups of different health insurance types and self-paying rate, with treatment options for NPC, using the grouping of insurance type and self-paying rate as independent variables, treatment regimens as the outcome, and other adjustment variables in the model. As shown in Table 2, after adjusting gender, occupation, marital status, ethnicity, age at diagnosis, cancer stage, histopathological diagnosis and clinical laboratory indicators, patients insured by UEBMI are more likely to choose radiotherapy, chemotherapy, targeted therapy when compared with patients who were insured by URRBM. Moreover, choosing these treatment regimens (including radiotherapy, chemotherapy, and targeted therapy) could obviously lead to higher out-pocket costs for NPC patients.
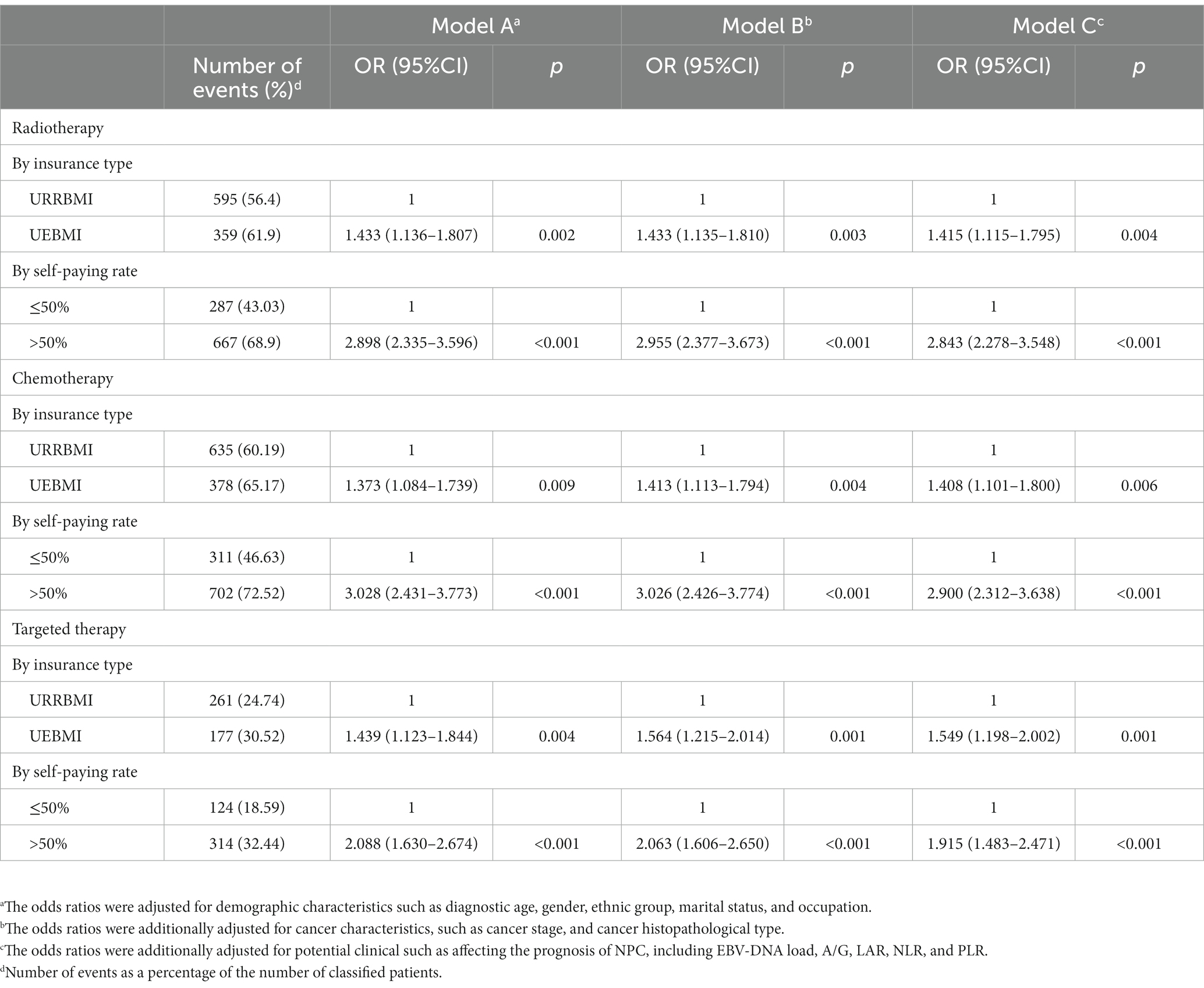
Table 2. Associations between treatment kind and insurance type and self-paying rate, according to demographic and clinical traits.
NPC-specific mortality and health insurance type and self-paying rate
During a median follow-up period of 3.7 years, 249 deaths were recorded, of which 195 died of NPC. As shown in Figure 1, Patients with a lower self-paying rate had a greater cumulative hazard overall and NPC-specific mortality than patients with a higher self-paying rate. The overall and NPC-specific mortality rate were not different between patients receiving UEBMI and those with URRBMI. After adjusting for demographic and tumor characteristics, patients with higher out-of-pocket costs compared to those with insufficient out-of-pocket costs experienced a risk reduction of overall mortality of 56.7% (HR: 0.433, 95% CI: 0.322–0.583, p < 0.001) and a risk reduction of NPC-specific mortality of 61.4% (HR: 0.386, 95% CI: 0.253–0.588, p < 0.001) (Table 3). When additionally adjusting the clinical characteristics and NPC treatment regimens, the risk of overall mortality was reduced by 47.5% (HR: 0.525, 95% CI: 0.380–0.727, p < 0.001) for patients with higher self-paying rate in comparison to patients with insufficient self-paying rate, and the risk of NPC-specific mortality was reduced by 46.6% (HR: 0.534, 95% CI: 0.339–0.839, p = 0.007).
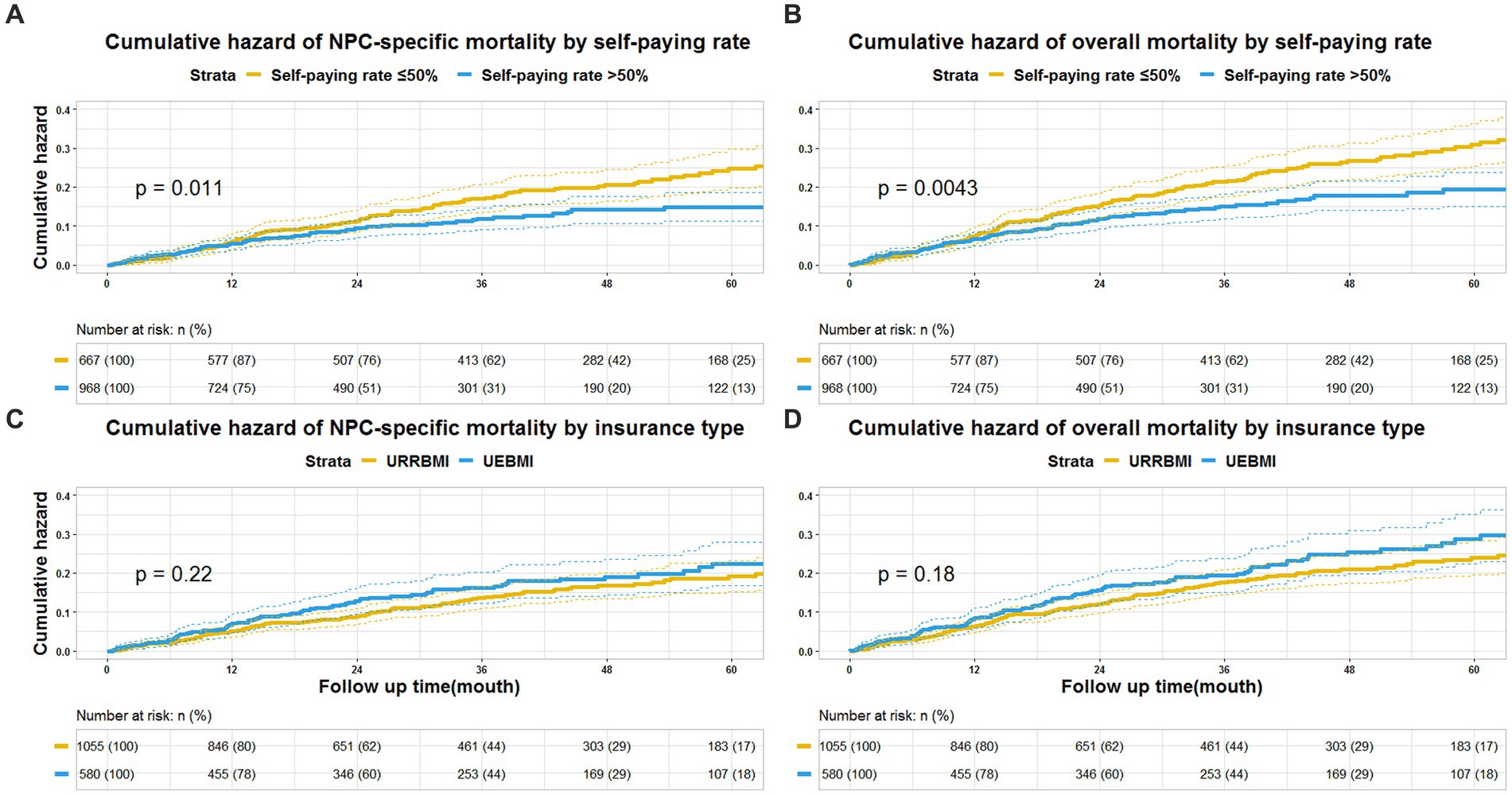
Figure 1. Cumulative hazard in patients with nasopharyngeal carcinoma. (A) Cumulative hazard of NPC-specific mortality by self-paying rate (self-paying rate). (B) Cumulative hazard of overall mortality self-paying rate (self-paying rate). (C) Cumulative hazard of NPC-specific mortality by insurance type. (D) Cumulative hazard of overall mortality by insurance type.
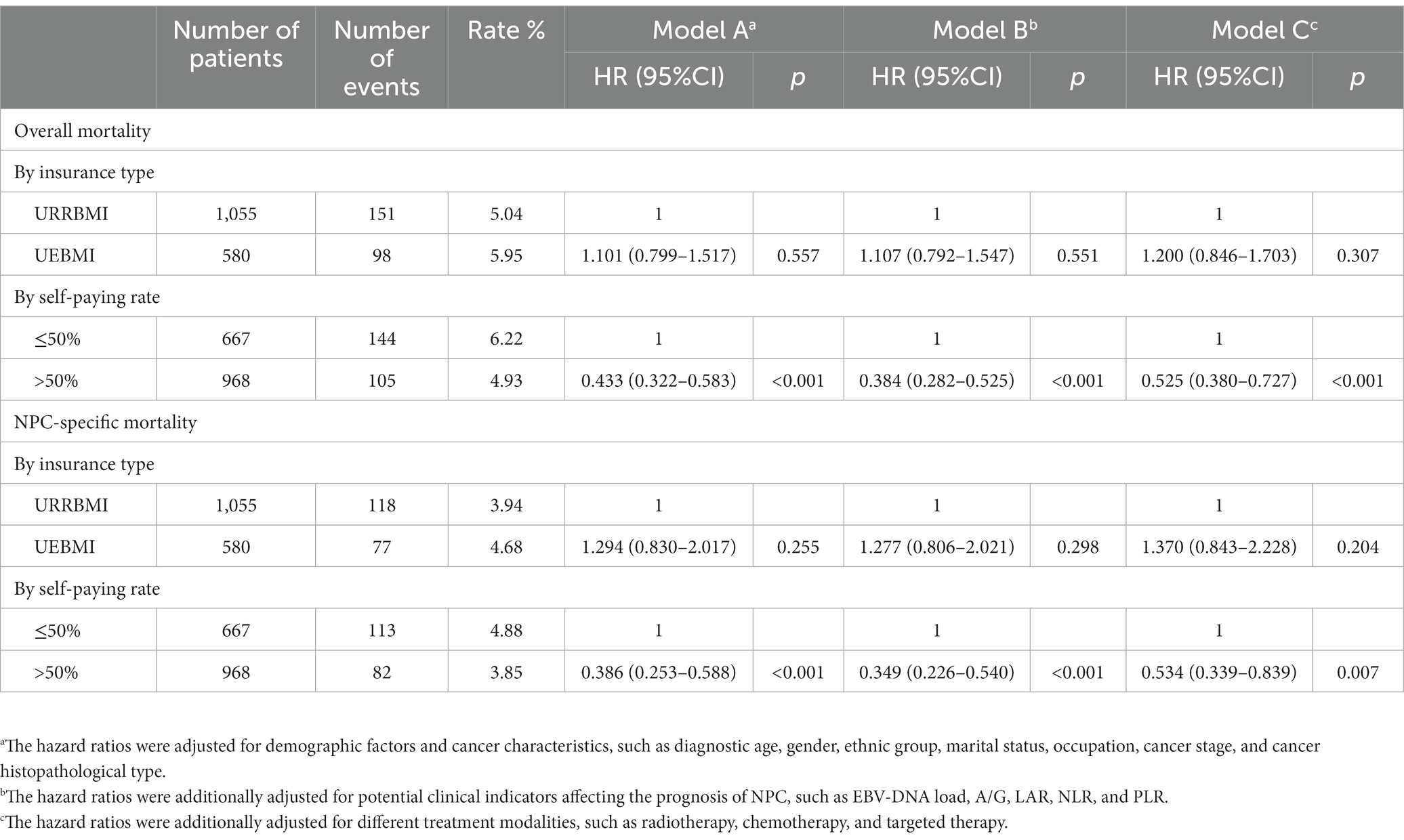
Table 3. Associations between insurance type and self-paying rate and NPC-specific or overall mortality risks.
The joint effect of insurance types and Self-paying rate
We demonstrated that each 10% increase in the self-paying rate was related to a 24.3% decreased overall risk of NPC-specific mortality (HR: 0.757, 95% CI: 0.647–0.887, p < 0.001), and a 28.3% decreased risk of NPC-specific mortality for patients receiving URRBMI (HR: 0.717, 95% CI: 0.611–0.842, p < 0.001), and a 25% decreased risk of NPC-specific mortality for patients receiving UEBMI (HR: 0.750, 95% CI: 0.626–0.899, p = 0.002). Similar results in overall mortality were discovered (Table 4).
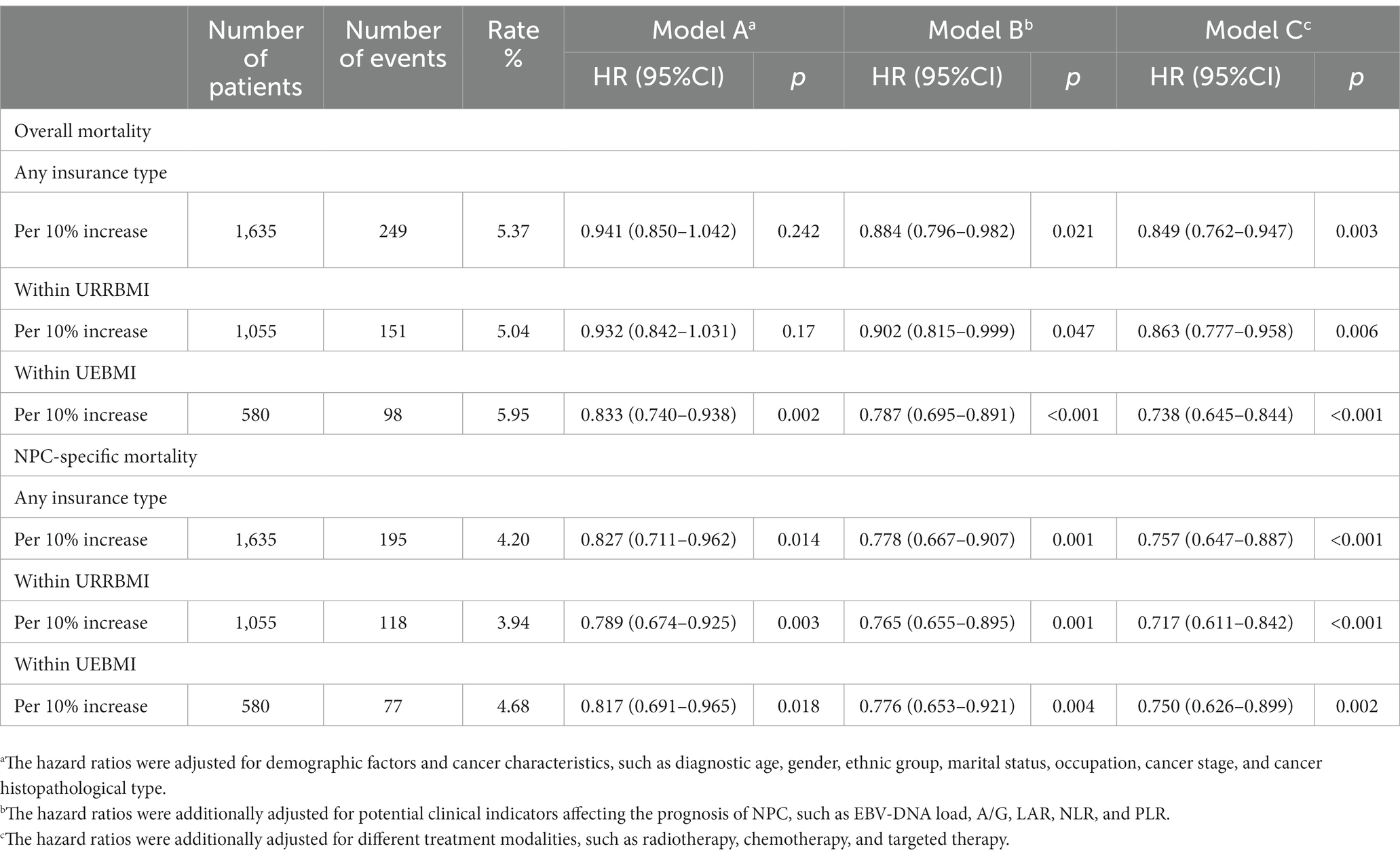
Table 4. Association between each 10% increase in insurance self-paying rate and risk of specific or overall mortality from NPC.
Discussion
To the extent that we are aware, this is the first study to comprehensively analyze the relationship between all-cause and NPC-specific death and insurance types or self-paying rate in NPC patients in China. In this large-scale cohort of 1,635 NPC patients treated at Chongqing University Cancer Hospital from 2017 to 2019, the sub-group analysis was conducted based on insurance types and self-paying rate. We found that the greater self-paying rate is associated with the lower incidence of NPC-specific death. Importantly, our results strongly suggest that the incidence of NPC-specific death was reduced by 25% per 10% rise in UEBMI’s self-paying rate, while the incidence of NPC-specific death was reduced by 28.3% per 10% rise in URRBMI’s self-paying rate. These associations are understood in part but not entirely by proven prognostic factors such as clinical features and NPC treatment regimens.
With the continuous development of precision radiotherapy technology and anti-cancer drugs, NPC patients have a great clinical curative effect and extended survival time, but meanwhile it also further increases the financial burden on individuals and their families (6). Since costly diagnostic screening (e.g., PET-CT), precise radiotherapy regimens (e.g., Helical Tomotherapy), and a part of anti-cancer targeted drugs and immune checkpoint inhibitors were not covered by medical insurance lists in China, NPC patients must afford the high out-of-pocket costs in order to prolong their survival time and improve their survival quality. In fact, our analysis shown that the association between high self-paying rate and NPC-specific mortality is somewhat attenuated by close to 15% after adjusting for treatment characteristics, suggesting a contribution from existing cancer treatments. Our data therefore provide a unique opportunity to uncover the underlying mechanisms of the relationship between health insurance and cancer prognosis, emphasizing the critical need to broaden the scope of reimbursement for diagnosis and treatment along with drugs in health insurance in order to dramatically enhance the prognosis of patients and minimize their financial hardship.
Patients with inadequate insurance would face a heavy economic burden and will not be able to pay for advanced therapy out-of-pocket (27). It is plausible that suboptimal medical services may lead to compromised prognosis after cancer diagnosis (28). Indeed, independent of clinical factors, our investigation showed that patients receiving URRBMI were more likely to have an advanced disease stage and that patients with low self-paying rate received less radiation, chemotherapy, and targeted treatment. For instance, Helical Tomotherapy was not covered by medical insurance lists during the study period, and the high out-of-pocket medical expenses may prevent financially vulnerable patients from such precise radiotherapy.
The increased prevalence of NPC-specific mortality in patients with insufficient out-of-pocket payments is not only due to differences in tumor features and treatment modalities. This is supported by our data that the increased risk of NPC-specific death remained robust in patients with low self-paying rate after exhaustive adjustment for clinical factors and treatment regimens. In addition, it is known that cancer patients face enormous psychological stress during cancer diagnosis and treatment (29). The high out-of-pocket costs, as a consequence of inadequate insurance, may aggravate patients’ emotional turmoil. It is no doubt that financial burden may impact patients’ prognosis via psychological disorders.
One significant feature of our study is that it is the first to investigate the relationship between NPC patients’ prognosis and medical expenses using a prospective cohort study design with comprehensive follow-up data. The abundance of data on the patient’s clinical and demographic traits helped us highlight how clearly health insurance policies influence NPC-specific mortality, which offers a fresh perspective for the development of our nation’s medical insurance. This study, however, has certain limitations. To begin with, because this cohort is based on a regional cancer center, the results can only provide a reference for generalization to the entire population. Second, our cohort only recorded the expenses incurred in the hospital for the treatment of NPC patients, but a small part of the costs incurred outside the hospital cannot be estimated. Third, we only discuss the association of NPC-specific mortality with insurance types and self-paying rate in the present study. Finally, the possible lack of patients who are most financially vulnerable may lead to information bias.
In conclusion, our findings suggest that patients with lower out-of-pocket costs face a higher risk of NPC-specific mortality in China, which may provide novel insights into the role of self-paying rate in cancer health disparities in China and likewise developing countries.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
YW, J-DS, and H-KL designed the protocol for the study. DL and H-KL performed statistical analysis and interpretation of the data. J-DS and DL composed the article, while YW, XZ, and X-LS revised it. H-LT, FW, and Y-WW participated in the data collection and cleaning. All authors participated in significant paper revisions and approved the final manuscript.
Funding
The current study was supported by grants from the National Natural Science Foundation of China (no 81802740 to J-DS; no. 81972857 to YW), Science-Health Joint Medical Scientific Research Project of Chongqing (no 2022ZDXM028 to J-DS), Natural Science Foundation Project of Chongqing (no cstc2018jcyjAX0741 to J-DS).
Acknowledgments
We thank all the members of the Radiation Oncology Translational Research Group who participated in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
NPC, nasopharyngeal carcinoma; URRBMI, Urban and Rural Residents Basic Medical Insurance; UEBMI, Urban Employee Basic Medical Insurance; EBV-DNA, plasma Epstein–Barr virus DNA load; A/G, serum albumin to globulin ratio; LAR, lactate dehydrogenase to albumin ratio; NLR, peripheral blood neutrophil count to lymphocyte count ratio; PLR, peripheral blood platelet count to lymphocyte count ratio; CI, confidence interval; OR, odds ratio; HR, hazard ratio.
References
1. Mimi, CY, and Yuan, JM. Epidemiology of nasopharyngeal carcinoma. Semin Cancer Biol. (2002) 12:421–9. doi: 10.1016/s1044579x02000858
2. Ferlay, J., Ervik, M., Lam, F., Colombet, M., Mery, L., Piñeros, M., et al., (2020) Global Cancer Observatory: Cancer Today. International Agency for Research on Cancer. Available at: https://gco.iarc.fr/today. Accessed June 10, 2022.
3. Sung, H, Ferlay, J, Siegel, RL, Laversanne, M, Soerjomataram, I, Jemal, A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660. Epub 2021 Feb 4
4. Zhang, Y, Chen, L, Hu, GQ, Zhang, N, Zhu, XD, Yang, KY, et al. Gemcitabine and Cisplatin Induction Chemotherapy in Nasopharyngeal Carcinoma. N Engl J Med. (2019) 381:1124–35. doi: 10.1056/NEJMoa1905287
5. Blanchard, P, Lee, A, Marguet, S, Leclercq, J, Ng, WT, Ma, J, et al. Chemotherapy and radiotherapy in nasopharyngeal carcinoma: an update of the MAC-NPC meta-analysis. Lancet Oncol. (2015) 16:645–55. doi: 10.1016/S1470-2045(15)70126-9
6. Wong, K.C., Hui, E.P., Lo, K.W., Lam, W.K.J., Johnson, D., Li, L., and Tao, Q., K.C.A. Chan, King, A.D., and Ma, B.B, Nasopharyngeal carcinoma: an evolving paradigm. Nat Rev Clin Oncol (2021), 18, 679–695. doi: 10.1038/s41571-021-00524-x
7. Global Burden of Disease Cancer. Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life Years for 29 Cancer Groups From 2010 to 2019: A Systematic Analysis for the Global Burden of Disease Study 2019. JAMA. Oncologia. (2022) 8:420–44. doi: 10.1001/jamaoncol.2021.6987
8. de Souza, JA, Hunt, B, Asirwa, FC, Adebamowo, C, and Lopes, G. Global Health Equity: Cancer Care Outcome Disparities in High-, Middle-, and Low-Income Countries. J Clin Oncol. (2016) 34:6–13. doi: 10.1200/JCO.2015.62.2860
9. Du, X. Racial disparities in health insurance, triple-negative breast cancer diagnosis, tumor stage, treatment and survival in a large nationwide SEER cohort in the United States. Mol Clin Oncol. (2022) 16:95. doi: 10.3892/mco.2022.2528
10. Wang, H, Hua, X, Yao, N, Zhang, N, Wang, J, Anderson, R, et al. The Urban-Rural Disparities and Associated Factors of Health Care Utilization Among Cancer Patients in China. Front Public Health. (2022) 10:842837. doi: 10.3389/fpubh.2022.842837
11. Zhao, Y, Tang, S, Mao, W, and Akinyemiju, T. Socio-Economic and Rural-Urban Differences in Healthcare and Catastrophic Health Expenditure Among Cancer Patients in China: Analysis of the China Health and Retirement Longitudinal Study. Front Public Health. (2021) 9:779285. doi: 10.3389/fpubh.2021.779285
12. Zhan, C, Wu, Z, Yang, L, Yu, L, Deng, J, Luk, K, et al. Disparities in economic burden for children with leukemia insured by resident basic medical insurance: evidence from real-world data 2015-2019 in Guangdong, China. BMC Health Serv Res. (2022) 22:229. doi: 10.1186/s12913-022-07564-8
13. Mao, W, Tang, S, Zhu, Y, Xie, Z, and Chen, W. Financial burden of healthcare for cancer patients with social medical insurance: a multi-centered study in urban China. Int J Equity Health. (2017) 16:180. doi: 10.1186/s12939-017-0675-y
14. Li, Y, Yang, Y, Yuan, J, Huang, L, Ma, Y, and Shi, X. Differences in medical costs among urban lung cancer patients with different health insurance schemes: a retrospective study. BMC Health Serv Res. (2022) 22:612. doi: 10.1186/s12913-022-07957-9
15. Han, X, Yabroff, KR, Ward, E, Brawley, OW, and Jemal, A. Comparison of Insurance Status and Diagnosis Stage Among Patients With Newly Diagnosed Cancer Before vs After Implementation of the Patient Protection and Affordable Care Act. JAMA Oncol. (2018) 4:1713–20. doi: 10.1001/jamaoncol.2018.3467
16. Diao, Y, Lin, M, Xu, K, Huang, J, Wu, X, Li, M, et al. How government health insurance coverage of novel anti-cancer medicines benefited patients in China -a retrospective analysis of hospital clinical data. BMC Health Serv Res. (2021) 21:856. doi: 10.1186/s12913-021-06840-3
17. Diao, Y, Lin, M, Xu, K, Huang, J, Wu, X, Li, M, et al. Impact of public health insurance coverage of novel anticancer medication on medical expenditure and patient affordability in a provincial medical centre of China: a propensity score-matching analysis with the quasi-experimental design. BMJ Open. (2022) 12:e054713. doi: 10.1136/bmjopen-2021-054713
18. Diao, Y, Qian, J, Liu, Y, Zhou, Y, Wang, Y, Ma, H, et al. How government insurance coverage changed the utilization and affordability of expensive targeted anti-cancer medicines in China: an interrupted time-series study. J Glob Health. (2019) 9:020702. doi: 10.7189/jogh.09.020702
19. Fang, W, Xu, X, Zhu, Y, Dai, H, Shang, L, and Li, X. Impact of the National Health Insurance Coverage Policy on the Utilisation and Accessibility of Innovative Anti-cancer Medicines in China: An Interrupted Time-Series Study. Front Public Health. (2021) 9:714127. doi: 10.3389/fpubh.2021.714127. eCollection 2021
20. Wu, J, Liu, C, and Wang, F. Disparities in Hepatocellular Carcinoma Survival by Insurance Status: A Population-Based Study in China. Front Public Health. (2021) 9:742355. doi: 10.3389/fpubh.2021.742355
21. Wang, Y, Lei, H, Li, X, Zhou, W, Wang, G, Sun, A, et al. Lung Cancer-Specific Mortality Risk and Public Health Insurance: a Prospective Cohort Study in Chongqing. Front Public Health. (2022) 10:842844. doi: 10.3389/fpubh.2022.842844
22. Xie, Y, Valdimarsdóttir, UA, Wang, C, Zhong, X, Gou, Q, Zheng, H, et al. Public health insurance and cancer-specific mortality risk among patients with breast cancer: A prospective cohort study in China. Int J Cancer. (2021) 148:28–37. doi: 10.1002/ijc.33183
23. Hsu, CD, Wang, X, Habif, DV Jr, Ma, CX, and Johnson, KJ. Breast cancer stage variation and survival in association with insurance status and sociodemographic factors in US women 18 to 64 years old. Cancer. (2017) 123:3125–31. doi: 10.1002/cncr.30722
24. Du, XJ, Tang, LL, Mao, YP, Sun, Y, Zeng, MS, Kang, TB, et al. The pretreatment albumin to globulin ratio has predictive value for long-term mortality in nasopharyngeal carcinoma. PLoS One. (2014) 9:e94473. doi: 10.1371/journal.pone.0094473
25. Peng, RR, Liang, ZG, Chen, KH, Li, L, Qu, S, and Zhu, XD. Nomogram Based on Lactate Dehydrogenase-to-Albumin Ratio (LAR) and Platelet-to-Lymphocyte Ratio (PLR) for Predicting Survival in Nasopharyngeal Carcinoma. J Inflamm Res. (2021) 14:4019–33. doi: 10.2147/JIR.S322475
26. Ma, SJ, Yu, H, Khan, M, Gill, J, Santhosh, S, Chatterjee, U, et al. Evaluation of Optimal Threshold of Neutrophil-Lymphocyte Ratio and Its Association With Survival Outcomes Among Patients With Head and Neck Cancer. JAMA Netw Open. (2022) 5:e227567. doi: 10.1001/jamanetworkopen.2022.7567
27. Fu, R, Wang, Y, Bao, H, Wang, Z, Li, Y, Su, S, et al. Trend of urban-rural disparities in hospital admissions and medical expenditure in China from 2003 to 2011. PLoS One. (2014) 9:e108571. doi: 10.1371/journal.pone.0108571
28. Meng, Q, Fang, H, Liu, X, Yuan, B, and Xu, J. Consolidating the social health insurance schemes in China: towards an equitable and efficient health system. Lancet. (2015) 386:1484–92. doi: 10.1016/S0140-6736(15)00342-6
Keywords: health insurance, nasopharyngeal carcinoma, NPC-specific mortality, self-paying rate, NPC prognosis
Citation: Li D, Lei H-K, Shu X-L, Zhang X, Tu H-L, Wang F, Wang Y-W, Wang Y and Sui J-D (2023) Association of public health insurance with cancer-specific mortality risk among patients with nasopharyngeal carcinoma: a prospective cohort study in China. Front. Public Health 11:1020828. doi: 10.3389/fpubh.2023.1020828
Edited by:
Vivek Kumar, Brigham and Women's Hospital and Harvard Medical School, United StatesReviewed by:
Suma Sri Chennapragada, Louisiana State University Health Shreveport, United StatesDawei Chen, Shandong Cancer Hospital, China
Qingzhu Jia, Army Medical University, China
Copyright © 2023 Li, Lei, Shu, Zhang, Tu, Wang, Wang, Wang and Sui. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiang-Dong Sui, amlhbmdkb25nLnN1aUBjcXUuZWR1LmNu; Ying Wang, eWluZ3dhbmcxOTcwMTFAMTYzLmNvbQ==
†These authors have contributed equally to this work
 Dan Li
Dan Li Hai-Ke Lei
Hai-Ke Lei Xiao-Lei Shu3
Xiao-Lei Shu3 Hong-Lei Tu
Hong-Lei Tu Feng Wang
Feng Wang Jiang-Dong Sui
Jiang-Dong Sui