
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 13 March 2023
Sec. Infectious Diseases: Epidemiology and Prevention
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1018983
This article is part of the Research TopicWorld AIDS Day 2022: Putting ourselves to the test: achieving equity to end HIVView all 30 articles
 Megan Ung1
Megan Ung1 Sarah Martin2,3
Sarah Martin2,3 Fern Terris-Prestholt4
Fern Terris-Prestholt4 Matthew Quaife4
Matthew Quaife4 Warittha Tieosapjaroen5,6
Warittha Tieosapjaroen5,6 Tiffany Phillips5,6
Tiffany Phillips5,6 David Lee5
David Lee5 Eric P. F. Chow5,6
Eric P. F. Chow5,6 Nick Medland5,7
Nick Medland5,7 Benjamin R. Bavinton7
Benjamin R. Bavinton7 Stephen W. Pan8,9
Stephen W. Pan8,9 Limin Mao10
Limin Mao10 Jason J. Ong4,5,6*
Jason J. Ong4,5,6*The HIV epidemic in Australia is changing with higher risk for HIV among newly-arrived Asian-born men who have sex with men (MSM) compared to Australian-born MSM. We evaluated the preferences for HIV prevention strategies among 286 Asian-born MSM living in Australia for <5 years. A latent class analysis uncovered three classes of respondents who were defined by their preferences: “PrEP” (52%), “Consistent condoms” (31%), and “No strategy” (17%). Compared to the “No strategy” class, men in the “PrEP” class were less likely to be a student or ask their partner for their HIV status. Men in the “Consistent condoms” class were more likely to get information about HIV from online, and less likely to ask their partner for their HIV status. Overall, PrEP was the preferred HIV prevention strategy for newly arrived migrants. Removing structural barriers to access PrEP can accelerate progress toward ending HIV transmission.
Australia has a concentrated HIV epidemic as is the case in many high-income countries. The majority of HIV diagnoses are in men (90%), with the highest acquisition risk in men who have sex with men (MSM) (1). Australia has upheld a successful and sustained approach to reducing the incidence of new HIV diagnoses each year (2). The highest annual cases recorded in Australia were 2,890 cases in 1984 (3). Since then, there has been a steep decline in the number of HIV notifications with 633 new diagnoses in 2020 (1). Australia has supported sequential approaches to HIV prevention, which in turn has contributed to the decline in HIV notifications in the last decade. These preventative methods have ranged from condom use and safer injecting practices to treatment as prevention (TasP), increased frequency of testing and most recently, pre-exposure prophylaxis (PrEP) (4, 5). Australia's healthcare system is such that those who are eligible for Medicare (anyone who is an Australian citizen, permanent resident, or a temporary resident covered by a ministerial order), are able to obtain HIV anti-retroviral therapy and HIV PrEP at a subsidized cost (6). However, people living with HIV who are Medicare-ineligible usually obtain HIV anti-retroviral therapy via compassionate access (i.e., provided by pharmaceutical companies), or import from their country of origin or from online pharmacies. Similarly, people who are Medicare-ineligible and desire PrEP at an affordable price often rely on personal importation from international online pharmacies, which is legal in Australia (5).
A greater focus on Asian-born MSM is crucial to end the HIV epidemic in Australia. The number of HIV diagnoses amongst Australian-born MSM has declined by over 44% in the past 5 years, while the number of new HIV diagnoses among overseas-born MSM remained steady between 2016 and 2019 (1). The prevalence of HIV in gay, bisexual and other men who have sex with men living in Australia is 7.3% (7). The prevalence of HIV in Asian born MSM who have recently migrated to Australia is not known. In 2017, research from Melbourne Sexual Health Center (MSHC) indicated that overall, incident HIV infections (infections that occurred within the last year) declined in MSM between 2008 and 2018, but had not declined in newly-arrived (< 5 years) Asian-born MSM (8). Newly-arrived Asian-born MSM are now four times more likely to be diagnosed with incident HIV infection at MSHC, compared to other MSM (9). It is not clear why newly-arrived Asian-born MSM are at a higher risk of incident HIV infection compared to Australian-born MSM despite reporting higher levels of condom use and fewer sexual partners, and being less likely to be diagnosed with other sexually transmitted infections (10). Reduced access to PrEP and HIV testing may explain this divergent trend among newly-arrived Asian-born MSM (11). Another hypothesis is that newly-arrived Asian-born MSM are at higher risk as their sexual networks may be other newly-arrived Asian-born MSM who have a higher rate of undiagnosed infection acquired in countries with lower coverage of HIV testing, treatment and virological suppression than Australia.
Discrete choice experiments (DCEs) have been widely utilized in economics and marketing to assess how much participants value the attributes of a good or service (12). DCE methodology has evolved over time and now is used internationally to measure individual preferences in a wide range of settings, including HIV-related research (13, 14). This preference elicitation method is used to understand which attributes are preferred by observing how participants trade-off between attributes in their decision-making (15). The advantage of using the DCE methodology is by presenting a variety of hypothetical scenarios to participants, the analyst can quantify the relative importance of each attribute or attribute during the decision-making process (16). This study aims to use a DCE methodology to examine preferences for HIV prevention strategies among newly arrived Asian-born MSM.
For the formative step of the DCE, we conducted semi-structured in-depth interviews with 24 newly-arrived Asian-born MSM between May to December 2019 to understand their experience of HIV testing and type of prevention strategies (17, 18). We found most men relied on condoms for HIV prevention but many indicated an interest in accessing PrEP. Using data from the first 14 interviews, we presented an example choice set for the DCE survey to the final 10 interviewees to obtain their feedback on the comprehensibility of the choice scenarios and choice sets and whether there were any missing HIV prevention strategies. Final DCE survey attributes and levels were determined (Table 1). The participants were asked to choose between two unlabeled alternatives or an opt-out alternative (Figure 1). The choice scenario was presented to all participants: “Imagine you are going to have sex with someone where you are not completely certain he is HIV-negative. What strategy would you prefer to protect yourself against HIV?”
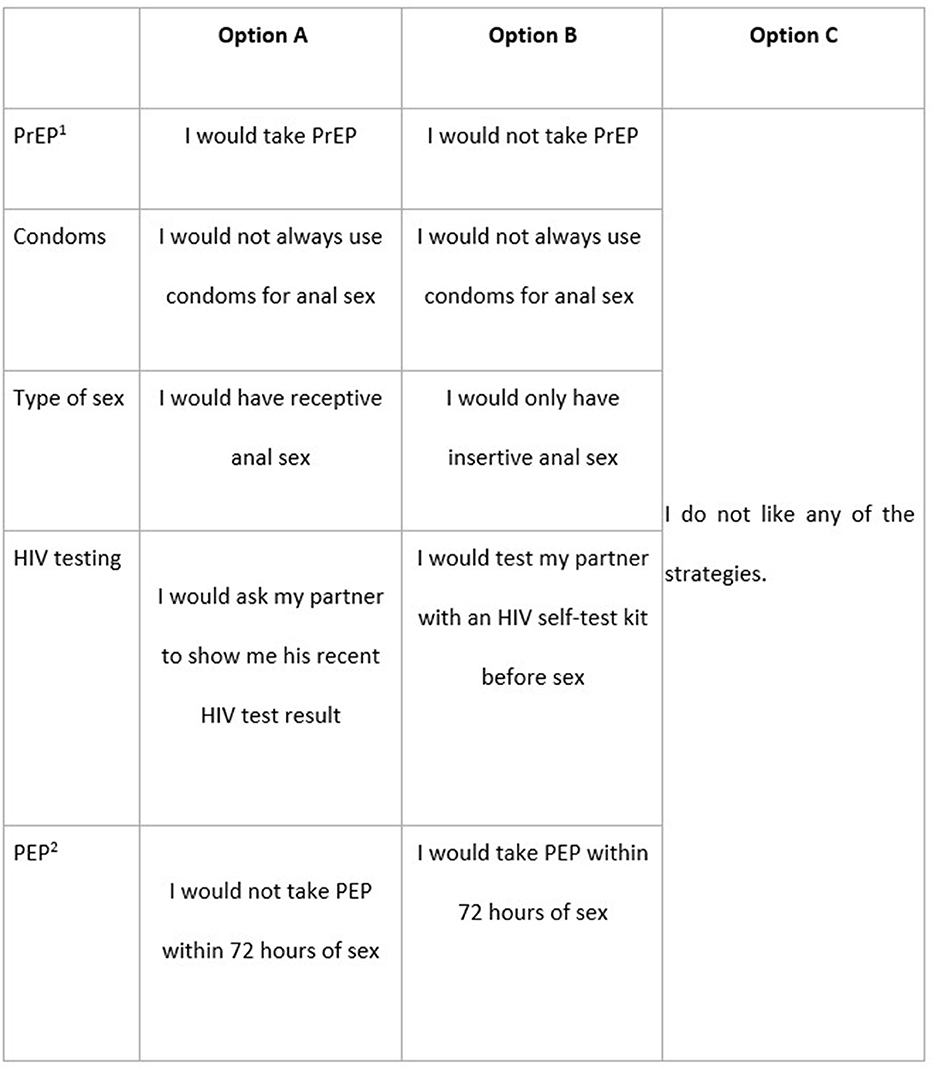
Figure 1. Example choice set. Imagine you are going to have sex with someone where you are not completely certain he is HIV-negative. What strategy would you prefer to protect yourself against HIV? 1PrEP, Pre-exposure prophylaxis; 2PEP, Post-exposure prophylaxis.
The DCE survey contained questions about participants' sociodemographic characteristics, including their age, education level, English fluency, sexual identity, connectedness to the gay community in Australia and their home country, use of HIV prevention strategies and sexual behaviors in the preceding 6 months. We used NGENE Software (Version 1.2.1, Choicemetrics, USA) to construct a D-efficient experimental design to maximize the information from each choice set. The experimental design contained 18 choice sets which we blocked into two so each participant would only see nine choice sets. We translated the survey into Thai, Simplified Chinese and Vietnamese with a professional translation service. The translated versions were sent to at least five MSM fluent in these languages to check the appropriateness of terminologies and comprehensibility of the survey.
The online survey was constructed using SurveyEngine. We recruited participants through online advertisements to users of the gay dating apps (Blued and Grindr), postcards (with QR code) of clients attending Melbourne Sexual Health Centre and Canberra Sexual Health Centre, social media (Facebook groups, Twitter), community-based organization email lists and the University of Melbourne student online portal from February 2020 to February 2021. Potential participants were shown an advertisement that links to an online survey for those interested in the survey. Those who were eligible to participate were MSM, not diagnosed with HIV, over 18 years old, born in Asia (South Asia, East Asia, South-East Asia), and arrived in Australia <5 years prior. Each participant read an online consent form and consented to participate by opening the survey. The minimum sample size was calculated using a standard of at least 100 respondents needed to model preference data (19).
We used descriptive statistics to summarize the sociodemographic characteristics of study participants. We used random parameters logit (RPL) models to analyze the choice data. The models were estimated using a maximum likelihood approach with 1000 Halton draws. All parameters were set to have an underlying normal distribution. We calculated the log-likelihood and Akaike information criteria to assess model fit. Qualitative variables were effect coded (20). The coefficients represent the relative strength of preference for the attribute level (higher magnitude of a positive coefficient represents an attribute that is more preferred whilst a higher magnitude of a negative coefficient represents an attribute that is less preferred). If the standard deviation (SD) for an attribute level is statistically significant, this indicates an unobserved heterogeneous spread of preferences for this attribute level. The attribute with the largest range in its coefficients indicates the relative importance of that attribute (21). To explore the heterogeneity of preferences and the popularity of various HIV prevention strategies, we conducted a latent class analysis (LCA) to identify clustering of similar preferences for HIV prevention strategies among recently-arrived Asian-born MSM. The LCA is a statistical procedure that allows the identification of underlying and unobservable latent variables using observed indicators, in order to determine subgroups for targeting interventions (22). All model estimations were performed using NLOGIT 6 (version 6, Econometric Software Inc., USA). We conducted a supplementary analysis in STATA (version 17.0, Statacorp) using logistic regression models to compare the sociodemographic characteristics of men who had the highest probability of being classified as having “no strategy”.
In total, 1,475 individuals clicked on the initial survey, and 286 (19%) completed the survey. Their mean age was 29.2 (SD 6.8) and mean duration living in Australia was 2.8 years (SD 1.4). The mean number of regular male sex partners in the last 6 months was 2.0 (SD 4.0) and the average number of casual male sex partners in the last 6 months was 6.0 (SD 11.5). Most (94%) had tested for HIV within 1 year and a quarter were taking PrEP (Table 2).
Generally, when faced with the possibility of having sex with a partner of unknown HIV status, men preferred using PrEP themselves or ensuring their partner took PrEP, and disliked the option with no PrEP (Table 3). Men preferred always using condoms compared to inconsistent condom use. Men preferred checking their partner's HIV test results and disliked no discussion about HIV status. The most important to least important HIV prevention strategy was PrEP (34.8%), condom use (32.3%), post-exposure prophylaxis (PEP) (20.1%), asking their sexual partners for their latest HIV test result (10.0%), and seropositioning (i.e., selectively practicing the type of sex based on partner's HIV status) (2.7%). There was significant preference heterogeneity noted for PrEP strategies, condoms, seropositioning and PEP.
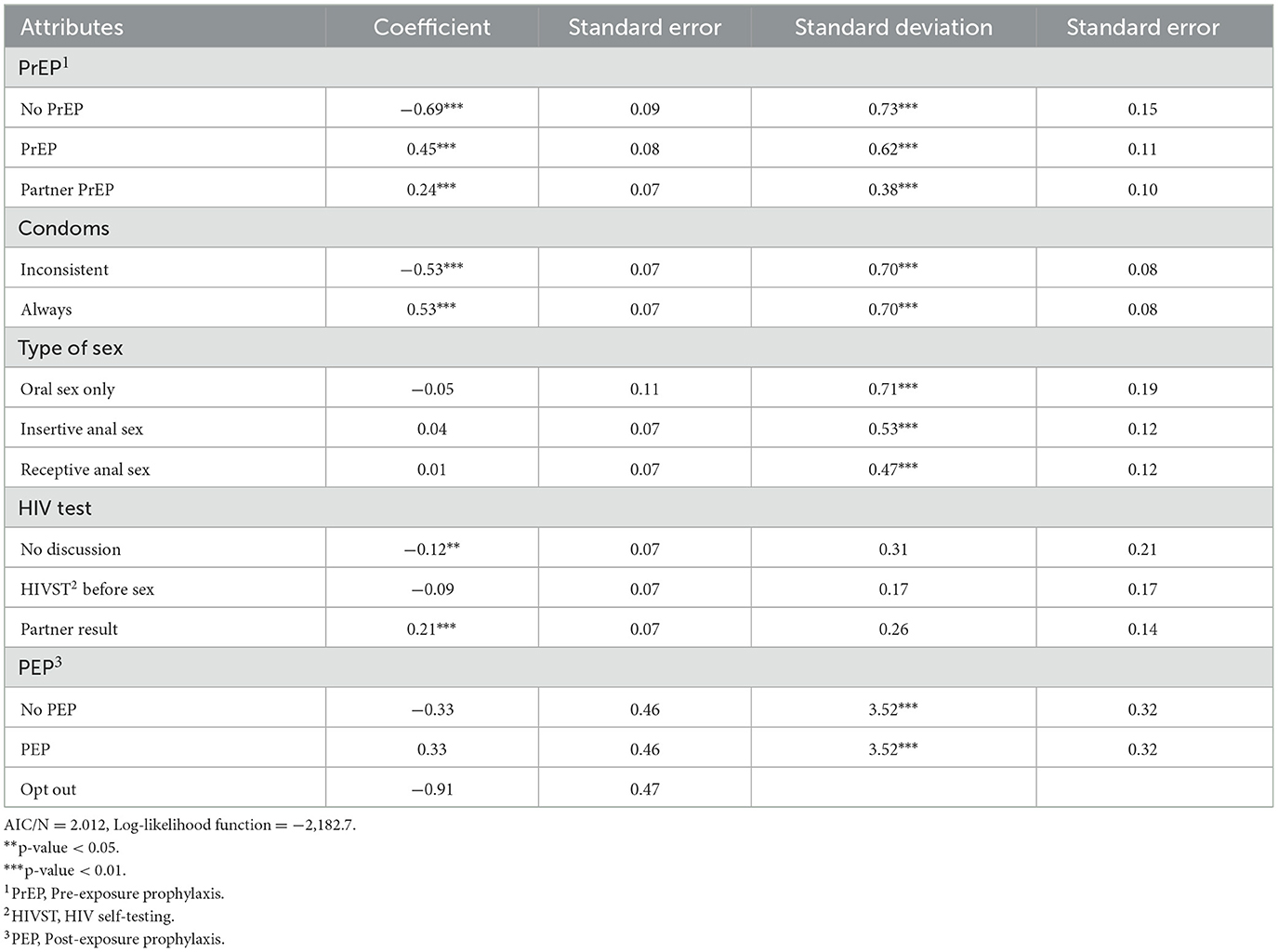
Table 3. Preferences for HIV prevention strategies among overseas born MSM (N = 286), random parameters logit model.
For the latent class analysis (Table 4), we found three classes. The largest class (PrEP, 52%) was characterized by men who preferred PrEP (ß = 0.38) more than twice as much as consistent condom use (ß = 0.15). Asking partner's latest HIV test result (ß = 0.15) was equally preferred to consistent condom use. People in this class were less likely to be students or to ask partner's latest HIV test result. The next largest class (Condoms, 31%) preferred consistent condom use (ß = 0.91) five times more than taking PrEP themselves (ß = 0.18). They had a greater preference for their partner to be on PrEP (ß = 0.29) rather than themselves (ß = 0.18). They equally preferred asking about their partner's latest HIV test result (ß = 0.28) as the partner taking PrEP (ß = 0.29). People in this class were more likely to be seek HIV information online, used condoms at their last sex, and less likely to ask partners about their latest HIV test result. The smallest class (No strategy, 17%) were most likely to opt out (ß = 3.00), i.e., they did not prefer the strategies presented in the choice set. They were more likely to ask their partners about their latest HIV test. To further unpack the characteristics of this class for whom HIV prevention did not appear a highly salient issue, we analyzed their characteristics. Besides having greater odds of being a student (OR 1.84, 95% CI: 0.99–3.45), we did not find any other statistically significant factors associated with the “No strategy” class (Supplementary Table 1).
Our study measured preferences for HIV prevention strategies amongst Asian-born MSM living in Australia. We add to the sparse literature for newly-arrived Asian-born MSM who have a higher risk for HIV compared with their Australian-born counterparts (9). We found that Asian-born MSM strongly preferred PrEP as a HIV preventive strategy, followed closely by consistent use of condoms. There was heterogeneity in preferences for HIV prevention strategies according to where people sought information about HIV, strategy used at last sex and whether they were students.
Overall, PrEP was a strongly preferred HIV preventative method in our study. It was noted that those who prefer PrEP strongly were also less likely to consistently use condoms. This finding is similar to a latent class analysis of MSM living in Montreal, whereby MSM who were PrEP users also had a low probability of using condoms consistently (23). However, in the Australian context, there is a discrepancy between the preference to use PrEP and the ease of accessing PrEP services for those who are newly-arrived in Australia. Newly-arrived MSM who are not familiar with navigating the Australian health system may not be aware of current, more affordable options to access PrEP and may be unable to pay for accumulative costs for a doctor's consultation (~$70), HIV and sexually transmitted infections (STIs) testing (~$200) and buying an unsubsidized PrEP script (30 pills cost ~$70) (24, 25). These structural barriers can deter newly-arrived MSM from seeking services including HIV testing and PrEP (26). Other existing barriers for newly-arrived MSM in Australia to access PrEP also include social and cultural barriers. Asian-born MSM may have originated from countries where stigma and discrimination surrounding same-sex attraction and HIV is highly prevalent (27). This may be in part why our study also found newly arrived MSM who were students were less likely to prefer using PrEP and more likely to be in the “no strategy” latent class. Approximately 350,000 international students from Asia come to Australia each year for higher education (28). International students living in Australia report concerns about hidden costs for accessing health services (27). In addition, a recent Australian study found most of the 111 recently arrived Asian MSM diagnosed with HIV did not have access to Medicare and were international students holding temporary visas (10). Currently, HIV testing is not mandatory for people applying for a temporary visa to stay in Australia (29). A possible solution to mitigate the incidence of HIV in Australia is to offer free HIV testing to people applying for temporary visas in Australia and affordable treatment where necessary. Furthermore, a focus on eliminating the barriers to preventative healthcare for recently arrived Asian-born MSM (particularly students) is a critical factor in reducing the incidence of HIV in this subpopulation.
About a third of men strongly preferred consistent use of condoms as a HIV preventive method but were less likely to prefer PrEP. Consistent condom use is a key HIV prevention strategy, as well as for reducing STIs acquisition. Lack of consistent condom use places at-risk groups at a higher risk of acquiring HIV if they are not relying on PrEP or undetectable viral load (30). Nonetheless, consistent condom use may be difficult to sustain, particularly given the falling rates of consistent use among MSM with the increasing uptake of PrEP in the recent years. Condomless anal sex with casual partners amongst MSM living in Australia has increased substantially from 53.7% in 2017 to 65.2% in 2021 (31). We found that those who sought information about HIV online were more likely to choose condom use as their HIV prevention strategy. Thus, there may be an opportunity to increase awareness about PrEP using eHealth platforms. eHealth platforms could eliminate fears of judgment and non-confidential clinical settings and allow for more convenient access to PrEP (32). For example, in Thailand, “Adam's Love” is a leading online outreach platform for PrEP awareness and counseling among the Thai MSM and transgender population and has facilitated recruitment and enrolment into PrEP studies (33). However, there is limited evidence on available eHealth platforms for PrEP access in other Asia-Pacific countries. Offering an online health service with telemedicine, counseling, prevention information, HIV testing and PrEP delivery may be worth exploring to target the newly arrived Asian MSM in Australia who find it difficult to navigate the Australian health system.
Worryingly, we found that a significant minority (17%) were categorized as having “no strategy”. It is not clear from our survey the reasons for not preferring any HIV prevention strategy. This might relate to factors not measured in our study such as low perception of risk, low health literacy, competing priorities in moving to a new country or genuine dislike of available HIV prevention strategies. Factors that have been associated with the non-uptake of PrEP in Australia among MSM (both Australian-born and Asian-born) include younger age, being less socially engaged with gay community, low perceived and/or actual risk of HIV and concerns of medication-related side effects of PrEP and taking daily medication (34, 35). A lack of Medicare coverage has also been independently associated with not using PrEP despite a willingness to use it (36). Qualitative research from 24 newly-arrived Asian-born MSM reported significant barriers including shame, stigma and fear related to HIV and their sexual identity remained despite living in a more liberal society (17, 18). More implementation research is needed to understand how to address the barriers of newly arrived Asian-born MSM to using effective HIV prevention strategies.
The strength of our study is that we quantitatively measured the preferences for HIV prevention strategies among Asian-born MSM to better understand their current preferences. We also uncovered subpopulations within this population with unique preferences to enable more targeted approaches to mitigate their risk of HIV acquisition. Our analysis has limitations. Firstly, there is potential for selection bias as we recruited mainly from sexual health clinics. These men may have higher health literacy than those not attending a sexual health clinic and may already be aware of HIV prevention strategies. Finding marginalized populations to ensure they have access to information and healthcare to inform their choice of HIV prevention strategies remains an ongoing challenge (37). Similarly, ensuring a representative sample of Asian-born MSM may not be possible, given the diversity of MSM from different countries in Asia. Future studies should explore the impact of diverse cultures and countries of origin on HIV prevention strategies. Secondly, there is potential for hypothetical bias inherent in stated choice surveys. However, recent reviews have demonstrated that health-related DCEs have adequate external validity (15, 38) and remain the best method to use when revealed preference data are not practical or possible to obtain. Third, our response rate was relatively low (19%), which may reflect the challenges in conducting research regarding sensitive issues such as HIV and sexual health.
In the context of higher risk of HIV acquisition among newly-arrived Asian-born MSM compared to Australian-born MSM, our study highlighted that overall, PrEP is strongly preferred as an HIV prevention strategy despite the current difficulties to access PrEP for this population.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics review and approval was granted by the Alfred Human Research Ethics Committee (222/19). Informed consent was obtained from the participants for the participation in this study.
JO, NM, FT-P, MQ, and SP contributed to the study conception and design. Material preparation, data collection, and analysis were performed by MU, SM, FT-P, MQ, DL, EC, SP, and JO. The first draft of the manuscript was written by MU and JO. All authors commented on previous versions of the manuscript and read and approved the final manuscript.
This study was funded by a Gilead fellowship. Besides providing funding to achieve our objectives, Gilead did not have any involvement with the analysis or dissemination of results from this project. The grant covered costs incurred through the advertising and online survey hosting.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1018983/full#supplementary-material
1. Kirby Institute. HIV Latest Data. (2021). Available online at: https://www.data.kirby.unsw.edu.au/hiv (accessed February 23, 2023).
2. Australian Government. Eight National HIV Strategy. Department of Health: Australian Government (2018).
3. ASHM. History of HIV Infection in Australia. Epidemiology and Natural History of HIV Infection. Australia: ASHM (2019).
4. Bavinton BR, Pinto AN, Phanuphak N, Grinsztejn B, Prestage GP, Zablotska-Manos IB, et al. Viral Suppression and HIV transmission in serodiscordant male couples: an international, prospective, observational, cohort study. Lancet HIV. (2018) 5:e438–47. doi: 10.1016/S2352-3018(18)30132-2
5. ASHM. National PrEP Guidelines Update, in Prevent HIV by Prescribing PrEP 2021: Australia. Australia: ASHM (2021).
6. Australian Government. Enrolling in Medicare, S. Australia, Editor (2021). Available online at: https://www.servicesaustralia.gov.au (accessed February 23, 2023).
7. Organisation A.F.o.A. HIV in Australia (2022). Available online at: https://www.afao.org.au/wp-content/uploads/2021/11/AFAO-HIV-in-Australia-2022.pdf (accessed February 23, 2023).
8. Gunaratnam P, Heywood AE, McGregor S, Jamil MS, McManus H, Mao L, et al. HIV diagnoses in migrant populations in Australia - A changing epidemiology. PLoS ONE. (2019) 14:e0212268. doi: 10.1371/journal.pone.0212268
9. Medland NA, Chow EP, Read TH, Ong JJ, Chen M, Denham I, et al. Fairley. Incident HIV infection has fallen rapidly in men who have sex with men in Melbourne, Australia (2013-2017) but not in the newly-arrived Asian-born. BMC Infect Dis. (2018) 18:1. doi: 10.1186/s12879-018-3325-0
10. Blackshaw LC, Chow EP, Varma R, Healey L, Templeton DJ, Basu A, et al. Characteristics of recently arrived Asian men who have sex with men diagnosed with HIV through sexual health services in Melbourne and Sydney. Austr N Zeal J Public Health. (2019) 43:12926. doi: 10.1111/1753-6405.12926
11. University of New South Wales Kirby, Institute. Qualitative Interviews with Overseas-Born Gay and Bisexual Men Recently Diagnosed with HIV from Non-English Speaking Countries: Report of Results. (2022). Available online at: https://kirby.unsw.edu.au/sites/default/files/kirby/report/Qualitative-Interviews-with-OSB-GBM-Report.pdf (accessed February 23, 2023).
12. Emily Lancsar JL. Conducting discrete choice experiments to inform healthcare decision making: a user's guide. PharmacoEconomics. (2008) 26:4. doi: 10.2165/00019053-200826080-00004
13. Soekhai V, de Bekker-Grob EW, Ellis AR, Vass CM. Discrete choice experiments in health economics: past, present and future. Pharmacoeconomics. (2019) 37:201–26. doi: 10.1007/s40273-018-0734-2
14. Sharma M, Ong JJ, Celum C, Terris-Prestholt F. Heterogeneity in individual preferences for HIV testing: a systematic literature review of discrete choice experiments. EClinicalMedicine. (2020) 29–30:100653. doi: 10.1016/j.eclinm.2020.100653
15. Merlo G, van Driel M, Hall L. Systematic review and validity assessment of methods used in discrete choice experiments of primary healthcare professionals. Health Econ Rev. (2020) 10:39. doi: 10.1186/s13561-020-00295-8
16. de Bekker-Grob EW, Ryan M, Gerard K. Discrete choice experiments in health economics: a review of the literature. Health Econ. (2012) 21:145–72. doi: 10.1002/hec.1697
17. Phillips TR, Medland N, Chow EP, Maddaford K, Wigan R, Fairley CK, et al. Moving from one environment to another, it doesn't automatically change everything. Exploring the transnational experience of Asian-born gay and bisexual men who have sex with men newly arrived in Australia. PLoS ONE. (2020) 15:e0242788. doi: 10.1371/journal.pone.0242788
18. Phillips TR, Medland N, Chow EP, Maddaford K, Wigan R, Fairley CK, et al. Newly arrived Asian-born gay men in Australia: exploring men's HIV knowledge, attitudes, prevention strategies and facilitators toward safer sexual practices. BMC Infect Dis. (2022) 22:209. doi: 10.1186/s12879-022-07174-z
19. de Bekker-Grob EW, Donkers B, Jonker MF, Stolk EA. Sample size requirements for discrete-choice experiments in healthcare: a practical guide. Patient. (2015) 8:373–84. doi: 10.1007/s40271-015-0118-z
20. Bech M, Gyrd-Hansen D. Effects coding in discrete choice experiments. Health Econ. (2005) 14:1079–83. doi: 10.1002/hec.984
21. Hauber AB, González JM, Groothuis-Oudshoorn CG, Prior T, Marshall DA, Cunningham C, et al. Statistical methods for the analysis of discrete choice experiments: a report of the ISPOR conjoint analysis good research practices task force. Value Health. (2016) 19:300–15. doi: 10.1016/j.jval.2016.04.004
22. Lanza ST, Rhoades BL. Latent class analysis: an alternative perspective on subgroup analysis in prevention and treatment. Prev Sci. (2013) 14:157–68. doi: 10.1007/s11121-011-0201-1
23. Doyle CM, Maheu-Giroux M, Lambert G, Mishra S, Apelian H, Messier-Peet M, et al. Combination HIV prevention strategies among montreal gay, bisexual, and other men who have sex with men in the PrEP era: a latent class analysis. AIDS Behav. (2020) 25:269–83. doi: 10.1007/s10461-020-02965-4
24. Murphy D. Factors Influencing Coverage of PrEP in Australia. Australian Federation of AIDS Organisations (2021).
25. Scheme PB. Tenofovir Disoproxil + Emtricitabine. D.o. Health, Editor (2022). Available online at: https://www.pbs.gov.au/medicine/item/10347N-11146P-11149T-11276L-11296M-11306C-12506F-12542D (accessed February 23, 2023).
26. Walia AM, Fairley CK, Bradshaw CS, Chen MY, Chow EP. Disparities in characteristics in accessing public Australian sexual health services between Medicare-eligible and Medicare-ineligible men who have sex with men. Austr N Zeal J Public Health. (2020) 44:e13029. doi: 10.1111/1753-6405.13029
27. Gray C, Lobo R, Narciso L, Oudih E, Gunaratnam P, Thorpe R, Crawford G. Why I can't, Won't or Don't test for HIV: insights from Australian Migrants Born in Sub-Saharan Africa, Southeast Asia and Northeast Asia. Int J Environ Res Public Health. (2019) 16:1034. doi: 10.3390/ijerph16061034
28. Hazel Ferguson HS. Overseas Students in Australian Higher Education: A Quick Guide. C.o. Australia, Editor (2021). Available online at: https://www.aph.gov.au/About_Parliament/Parliamentary_Departments/Parliamentary_Library/pubs/rp/rp2021/Quick_Guides/OverseasStudents (accessed February 23, 2023).
29. Affairs A,.G.D.o.H. Threats to Public Health. Immigration Citizenship (2022). Available online at: https://immi.homeaffairs.gov.au/help-support/meeting-our-requirements/health/threats-to-public-health (accessed August 2, 2023).
30. Siegler AJ, Rosenthal EM, Sullivan PS, Mehta CC, Moore RH, Ahlschlager L. Cecil. Levels of clinical condom failure for anal sex: a randomized cross-over trial. EClinicalMedicine. (2019) 17:12. doi: 10.1016/j.eclinm.2019.10.012
31. Timothy Broady CC, Bavinton B, Mao L, Molyneux A, Delhomme F, Power C, et al. Gay Community Periodic Survey Sydney. C.f.S.R.i. Health, Editor. UNSW Sydney (2021).
32. Rousseau E, Julies RF, Madubela N, Kassim S. Novel platforms for biomedical HIV prevention delivery to key populations - community mobile clinics, peer-supported, pharmacy-led PrEP delivery, and the use of telemedicine. Nat Public Health Emerg Coll. (2021) 18:1–8. doi: 10.1007/s11904-021-00578-7
33. Anand T, Nitpolprasert C, Ananworanich J, Pakam C, Nonenoy S, Jantarapakde J, et al. Innovative strategies using communications technologies to engage gay men and other men who have sex with men into early HIV testing and treatment in Thailand. J Virus Eradic. (2015) 1:111–5. doi: 10.1016/S2055-6640(20)30483-0
34. Hammoud MA, Vaccher S, Jin F, Bourne A, Maher L, Holt M. HIV pre-exposure prophylaxis (PrEP) uptake among gay and bisexual men in Australia and factors associated with the nonuse of PrEP among eligible men: results from a prospective cohort study. JAIDS. (2019) 81:2047. doi: 10.1097/QAI.0000000000002047
35. Health C.f.S.R.i. Attitudes to Biomedical HIV Prevention Among Australian Gay and Bisexual Men: Key Findings from the PrEPARE Project 2019. U. Sydney, Editor. Australia: Health C.f.S.R.i (2019).
36. MacGibbon J, Lea T, Ellard J, Murphy D, Kolstee J, Power C. Access to subsidized health care affects HIV pre-exposure prophylaxis (PrEP) uptake among gay and bisexual men in Australia: results of national surveys 2013-2019. JAIDS. (2021) 86:2572. doi: 10.1097/QAI.0000000000002572
37. De Abreu Lourenço R, Devlin N, Howard K, Ong JJ, Ratcliffe J, Watson J, et al. Giving a voice to marginalised groups for health care decision making. Patient. (2021) 14:5–10. doi: 10.1007/s40271-020-00456-1
Keywords: HIV, men who have sex with men, migrants, pre-exposure prophylaxis, Australia, health preference research, discrete choice experiment
Citation: Ung M, Martin S, Terris-Prestholt F, Quaife M, Tieosapjaroen W, Phillips T, Lee D, Chow EPF, Medland N, Bavinton BR, Pan SW, Mao L and Ong JJ (2023) Preferences for HIV prevention strategies among newly arrived Asian-born men who have sex with men living in Australia: A discrete choice experiment. Front. Public Health 11:1018983. doi: 10.3389/fpubh.2023.1018983
Received: 14 August 2022; Accepted: 16 February 2023;
Published: 13 March 2023.
Edited by:
Francisco Antunes, Universidade de Lisboa, PortugalReviewed by:
Yuhua Ruan, Chinese Center for Disease Control and Prevention, ChinaCopyright © 2023 Ung, Martin, Terris-Prestholt, Quaife, Tieosapjaroen, Phillips, Lee, Chow, Medland, Bavinton, Pan, Mao and Ong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jason J. Ong, amFzb24ub25nQG1vbmFzaC5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.