- 1Department of Public Health Science, Indian Institute of Public Health Gandhinagar (IIPHG), Gandhinagar, India
- 2School of Epidemiology and Public Health, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences (Deemed to be University), Wardha, India
- 3World Health Partners (WHP), Noida, India
Tuberculosis (TB) is the second leading cause of death due to infectious diseases globally, and delay in the TB care cascade is reported as one of the major challenges in achieving the goals of the TB control programs. The main aim of this study was to investigate the delay and responsible factors for the delay in the various phases of care cascade among TB patients in two Indian states, Jharkhand and Gujarat. This cross-sectional study was conducted among 990 TB patients from the selected tuberculosis units (TUs) of two states. This study adopted a mixed-method approach for the data collection. The study targeted a diverse profile of TB patients, such as drug-sensitive TB (DSTB), drug resistance TB (DRTB), pediatric TB, and extra-pulmonary TB. It included both public and private sector patients. The study findings suggested that about 41% of pulmonary and 51% of extra-pulmonary patients reported total delay. Delay in initial formal consultation is most common, followed by a delay in diagnosis and treatment initiation in pulmonary patients. While in extra-pulmonary patients, delay in treatment initiation is most common, followed by the diagnosis and first formal consultation. DR-TB patients are more prone to total delay and delay in the treatment initiation among pulmonary patients. Addiction, co-morbidity and awareness regarding monetary benefits available for TB patients contribute significantly to the total delay among pulmonary TB patients. There were system-side factors like inadequacy in active case findings, poor infrastructure, improper adverse drug reaction management and follow-up, resulting in delays in the TB care cascade in different phases. Thus, the multi-disciplinary strategies covering the gambit of both system and demand side attributes are recommended to minimize the delays in the TB care cascade.
1. Introduction
Tuberculosis (TB) is one of the global public health concerns as TB is the second leading cause of death due to infectious diseases (1). In 2020, 1.5 million people lost their lives due to TB worldwide, and India accounted for almost 34% of the total deaths (2). Early care-seeking, accurate and timely diagnosis and prompt treatment initiation are foremost for breaking the transmission chain and effectively controlling TB (3, 4). Delay in care-seeking at any stage of the care cascade among TB patients remains one of the challenges in achieving the intended outcomes of the TB control programs (5–7).
Delays in various phases of the TB care cascade, like the first formal consultation, diagnosis, and treatment, could increase the risk of unfavorable outcomes (including aggravation of the illness and infection, leading to complications, and raising the risk of mortality). And also result in the spreading of TB infection at the community level (8, 9). Reducing the time interval between the onset of symptoms and care-seeking can reduce the incidence of TB as it reduces the window during which infected people with symptoms can spread the disease to others. Evidence suggests that if the average care-seeking delay was reduced by 25% amongst TB patients, TB mortality would be reduced by nearly 6%, and the incidence would decline comparably (10). Therefore, to reduce the overall disease burden and for the significant effect of TB control programs, it is necessary to address the delays amongst TB patients on priority.
The interval for diagnosis and initiation of treatment is higher in high-burden countries and is attributed to both patient and health system-related factors (11, 12). In India, estimated patient, diagnostic, and treatment delays were 18.4 (14.3–27.0), 31.0 (24.5–35.4), and 2.5 days (1.9-3.6), respectively, for TB and chest symptomatic patients combined and the median total delay was 55.3 days (46.5–61.5) (13). The socio-economic condition, disease knowledge and awareness, myths/beliefs, family and social support, and addictions among the patients were reflected in many studies as the prime patient side factors responsible for delay at various phases of the care cascade (14–19).
There are numerous studies on predictors of delay amongst TB patients in India in various phases of the care cascade (13). However, there is a dearth of literature available for these two selected states. The results from other states have been mixed and are more context-specific or study-setting specific (13). Therefore, this study aims to investigate the delay and responsible factors for the delay in the various phases of care cascade among TB patients in two Indian states, Jharkhand and Gujarat. Hence, this study provides a better understanding of the reasons for delays in various phases of care cascade among TB patients for this selected study site. The study findings may aid in designing effective and sustainable interventions to fulfill the gaps in the TB care cascade under the national elimination programme (NTEP).
2. Methods
The cross-sectional assessment was carried out from Jan-July 2021 in the two Indian states, Jharkhand and Gujarat.
2.1. Study setting
The assessment was done in 10 out of 25 Tuberculosis Units (TUs) in the Purbi Singhbhum and Ranchi districts (Jharkhand state) and 22 out of the 32 TUs in Gandhinagar and Surat districts (Gujarat state). The two states and two districts from each state were selected purposively based on the consultation with the state officials. TU was considered the sampling unit in the demand side, where the probability proportional to size (PPS) sampling follow the simple random sampling. The PPS sampling strategy was used to select the sampling units concerning the patient load and the distribution of the functional TU. A total of 32 TUs were sampled out of 57 TUs based on a random selection with the principle of PPS.
2.2. Study design
This study adopts an embedded mixed-method design (Quantitative assessment followed by qualitative interviews) (20) for data collection. The quantitative (cross-sectional survey of TB patients) was carried out, followed by the qualitative [in-depth interview (IDI) both from the system-side actors and demand-side TB patients]. The qualitative interviews were aimed to supplement the larger quantitative TB patient survey.
2.3. Study samples and sampling
2.3.1. Quantitative assessment
The quantitative assessment targeted a diverse profile of TB patients, such as drug-sensitive TB (DSTB), drug resistance TB (DRTB), pediatric TB, and extra-pulmonary TB. It included both public and private sector patients. A multistage cluster sampling was used to recruit the patients. A PPS was used to identify the primary sampling unit, TU. From each TU, patients were recruited randomly depending on their availability and willingness to participate. The assessment was intended to cover all stages of the TB care cascade and the delays in the respective phases. Notified TB patients were recruited from 1Q-2019 to 4Q-2020 for DS-TB. Similarly, for DRTB, patients were recruited from 3Q-2018 to 4Q-2020. Patients were interviewed at their convenience, either at the hospital or at their residences. About 990 patients with different categories were recruited for the quantitative assessment. Based on the limited evidence from India on the proportion of delay in the TB care cascade (21) and based on the formative research experiences in the selected study sites, it has been averaged out that 50% of the TB patients delayed seeking care. Therefore, with 95% CI, 90% power, 50% delay, the estimated sample size for the one-sample proportion test (Wald z test) was 778. Adding a non-response rate of an average of 10%, the final sample size for the study was 856.
2.3.2. Qualitative assessment
IDIs were conducted both among the actors from the system side and selected TB patients. About 40 system side actors and 10 TB patients were interviewed to supplement the quantitative findings. The patients and system side actors were interviewed based on their availability and consent for participation. Among the system-side actors, there were healthcare staff from the NTEP programs and the general health system working at the State TB cell, District TB Center, TB Unit, PHI. These actors who were involved in direct contact with TB patient care and decision-making were purposively selected. For the demand side, conveniently, 10 patients were selected at the end of the quantitative assessment to supplement the findings. It was limited to only 10 diverse cases of TB patients and didn't extend beyond till the saturation of the responses due to the project timeline.
2.4. Data collection
The quantitative data were collected through a structured delay assessment questionnaire, and the semi-structured interview guide was prepared for qualitative assessment in vernacular language. Trained researchers were administered the survey tools at the respective sites.
2.4.1. Quantitative data collection
The demand-side assessment collected quantitative information through a structured, pilot-tested questionnaire in vernacular language. The information such as socio-demographic details, history of addiction and co-morbidities, patient's basic knowledge about the TB symptoms, social perception of TB patients, drug acceptance and adverse drug reactions, perception about the availed health services and perception of the healthcare workers and financial expenses were collected. The social perception was measured through a self-reported likert scale of five, mentioning agree to disagree. The additional care-seeking pathway section captured the sketch of all the events, i.e., detection of symptoms, seeking healthcare, first formal consultation, diagnosis, and treatment initiation to completion within the time frame. The delay assessment was captured from the care-seeking pathway section. Trained research assistants administered the survey tool to the selected TB patients in their households or at a place convenient to the patients in the vernacular language.
2.4.2. Qualitative data collection
There were two sides to qualitative assessment. IDIs among TB patients aimed to explore the reasons for delay from the socio-cultural context, whereas among the system-side actors aimed to understand the delay reasons from the supply side. The trained researchers conducted the IDIs using the semi-structured interview guide in the vernacular language. The semi-structured interview guide for the system side actors was designed to capture barriers and challenges in implementing the NTEP, different aspects of the NTEP programs and the delays in the TB care cascade from the service provider's perspective. The semi-structured interview guide for the patients was designed with predecided themes of care-seeking pathways prior to the treatment initiation, delays within the care cascade and the challenges. Therefore, open-ended questions like details prior to the treatment initiation to treatment completion and different issues fronted during the various phase, TB medications, motivation, counseling details on drop-out, and reasons for the delay were included in the semi-structured interview guide.
2.5. Data analysis
The quantitative and qualitative data were handled independently. The below-mentioned procedures were followed for data analysis.
2.5.1. Quantitative data analysis
Once the data collection was completed, data sets were imported from the application and validated, followed by data cleaning and analysis performed using statistical software STATA version 14.1. For the care-seeking pathway, the duration of delays across each care level was measured in the days from the care-seeking pathways section and then analyzed further. For the detailed analysis of the delays, patients were grouped into two categories i.e., pulmonary and extra-pulmonary TB patients and analyzed accordingly. Three categories of delay were estimated: (i) Delay in first formal consultation that led to confirmed diagnosis (onset of symptoms to first formal consultation); (ii) Diagnostic delay (consultation to confirmatory diagnosis) and (iii) Treatment delay (diagnosed to treatment initiation). The continuous variable of various delays was dichotomized using the cut-off values mentioned in the definitions for each phase of TB care cascade. The multivariate analysis was conducted using binomial logistic regression with delay as the outcome variable to understand the determinants for the delay in various stages of the care cascade. For the delay in the different cascade of TB, only three important variables i.e., type of TB (DSTB/DRTB), Age group (Adults/Pediatric) & place of services received (Public/Private Healthcare Facility) were included in the final analysis; whereas all the variables including other sociodemographic factors irrespective of statistical significance level were included in the multivariate analysis for the total delay.
The agree and disagree responses were averaged and reported for all the indicators under the social perception.
2.5.2. Qualitative data analysis
The interviews were recorded, and verbatim notes were also taken during the interviews after the consent from the participants. The audios were transcribed and then translated into English. Manual descriptive content analysis was used to analyze the transcripts (22, 23). The decision on coding rules and quote generation were made by using standard procedures and in consensus with a specific focus on the phases of the delays (24). Both inductive and deductive codes were generated. To ensure that the results were a reflection of the data, the codes were related back to the quantitative data. The quotes were described as part of the qualitative findings and reported using Consolidated Criteria for Reporting Qualitative Research (25).
2.6. Definitions
Two sets of definitions were used, one for the delay in pulmonary and another for the delay in extra-pulmonary TB patients.
2.6.1. Definitions of delay for pulmonary TB patients
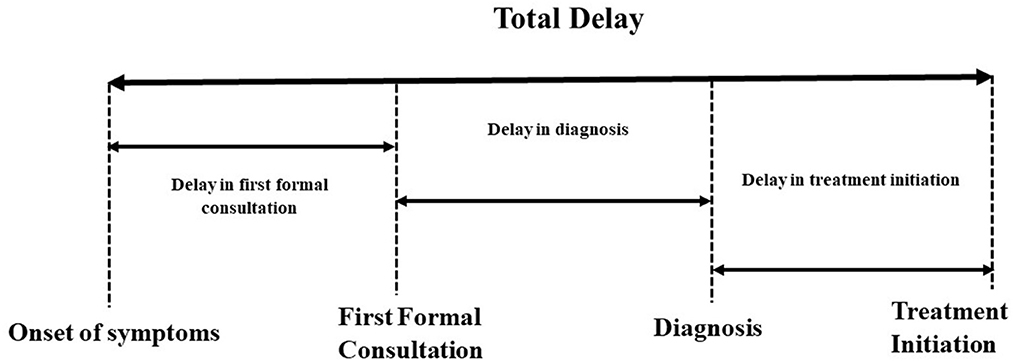
• Delay in first formal consultation: The time interval between the onset of symptoms and the first formal consultation in TB patients. This was considered as more than 14 days as symptoms more than 14 days suggestive of TB as per the Standard for TB Care in India (STCI) guidelines (26).
• Delay in diagnosis: The time interval between the first formal consultation and diagnosis. This was considered as more than seven days (27).
• Delay in treatment initiation: The time interval between the diagnosis and treatment initiation. This was considered as more than seven days, as treatment should be initiated within seven days of diagnosis as per the NTEP guidelines (14).
• Total delay: A collective estimate of >28 days was used to define a cut-off value from the time interval between the onset of symptoms to initiation of anti-TB treatment, as depicted in Figure 1.
2.6.2. Definition of delay for the extra-pulmonary TB patients
The median was considered as a cut-off value for the delay among the extra-pulmonary TB patients. Duration of days equal to or more than the median was considered the delay for the respective phases mentioned above. For the total delay also, a similar strategy was considered.
3. Results
3.1. Quantitative findings
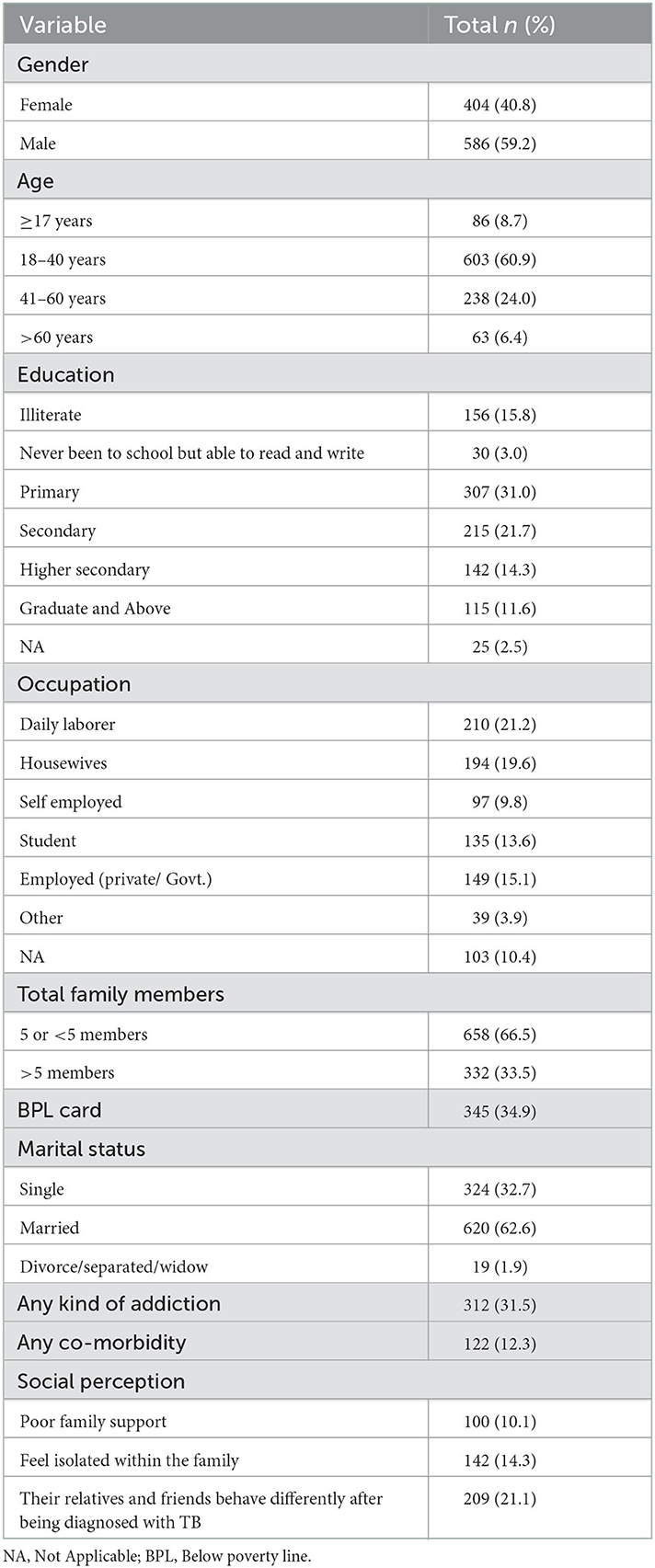
A total of 990 TB patients were interviewed, as shown in Table 1, more than half of the patients (59.2%) were males, and 60.9% of the patients were 18–40 years old. Of all the patients, 15.8 % were illiterate, and only 11.6 % were graduates or had higher education. Almost one-fifth (21.2%) of the participants were daily laborers, 19.6% were housewives, and 24.9% were employed either owing business or with the organization. 31.5% of the patients reported having any addiction, and 12.3% reported co-morbidities. Almost 21.1% of the patients said their relatives and family members behave differently after being diagnosed with TB, and 10.1% said they have poor support from their family members.
As documented in Table 2, the mean duration between the onset of symptoms and formal consultation among the pulmonary patient was 30.9 (± 69.2) days, and the median was 10 days, the highest amongst all the phases of the TB care cascade. While in the extra-pulmonary patients, the mean duration between the onset of symptoms and formal consultation among the pulmonary patient was 40.4 (± 112.4) days, and the median was 12 days. The duration between formal consultation and the diagnosis was reported as 12.7 (±56.2) days in pulmonary and 14.0 (±50.0) in extra-pulmonary patients. The treatment was initiated in the next 7.4 (± 33.7) days in pulmonary and 7.1 (±20.7) in extra-pulmonary patients after diagnosis.
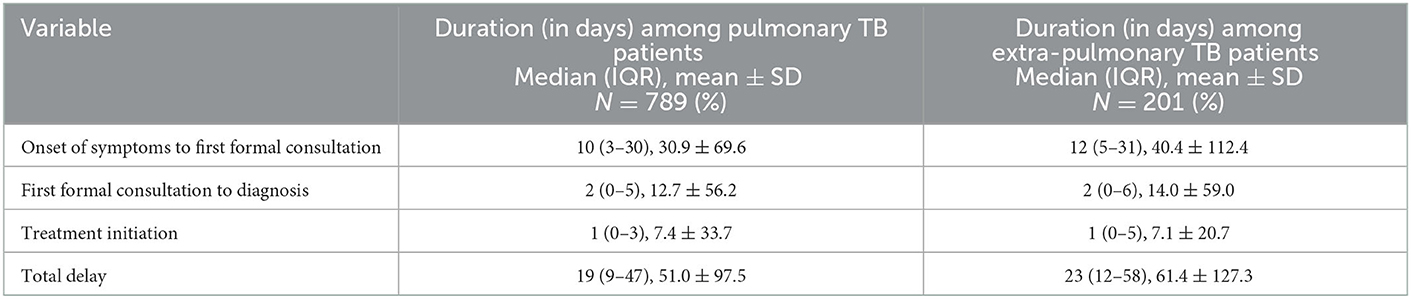
Table 2. Duration of the care-seeking at the various phase of the care cascade among surveyed TB patients in two Indian states Jharkhand, Gujarat during Jan–Jul 2021.
Of the 990 patients, 789 (79.7) were pulmonary TB patients, and the remaining were extra-pulmonary. Most of the pulmonary TB patients (40.2%) reported a delay in initial formal consultation after the onset of symptoms, followed by a delay in diagnosis and treatment initiation. Almost 41% of the pulmonary patients reported total delay in the care cascade. In contrast, most of the extra-pulmonary TB patients (70.2%) reported a delay in treatment initiation, followed by a delay in diagnosis and first formal consultation. About half of the extra-pulmonary patients reported total delay in the care cascade, as indicated in Table 3.
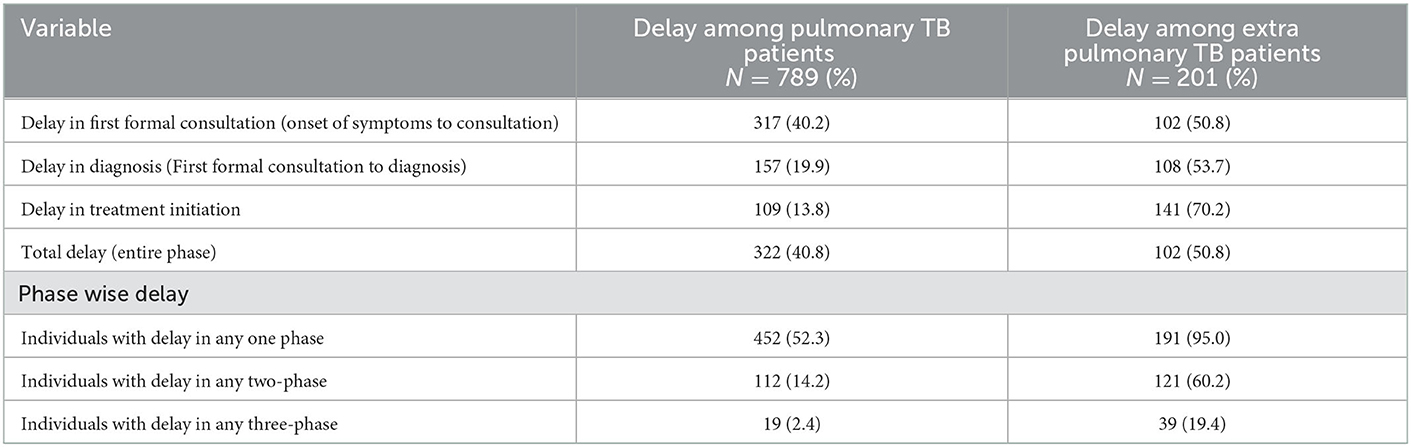
Table 3. Delay at the various phase of the care cascade among surveyed TB patients in two Indian states Jharkhand, Gujarat during Jan–Jul 2021.
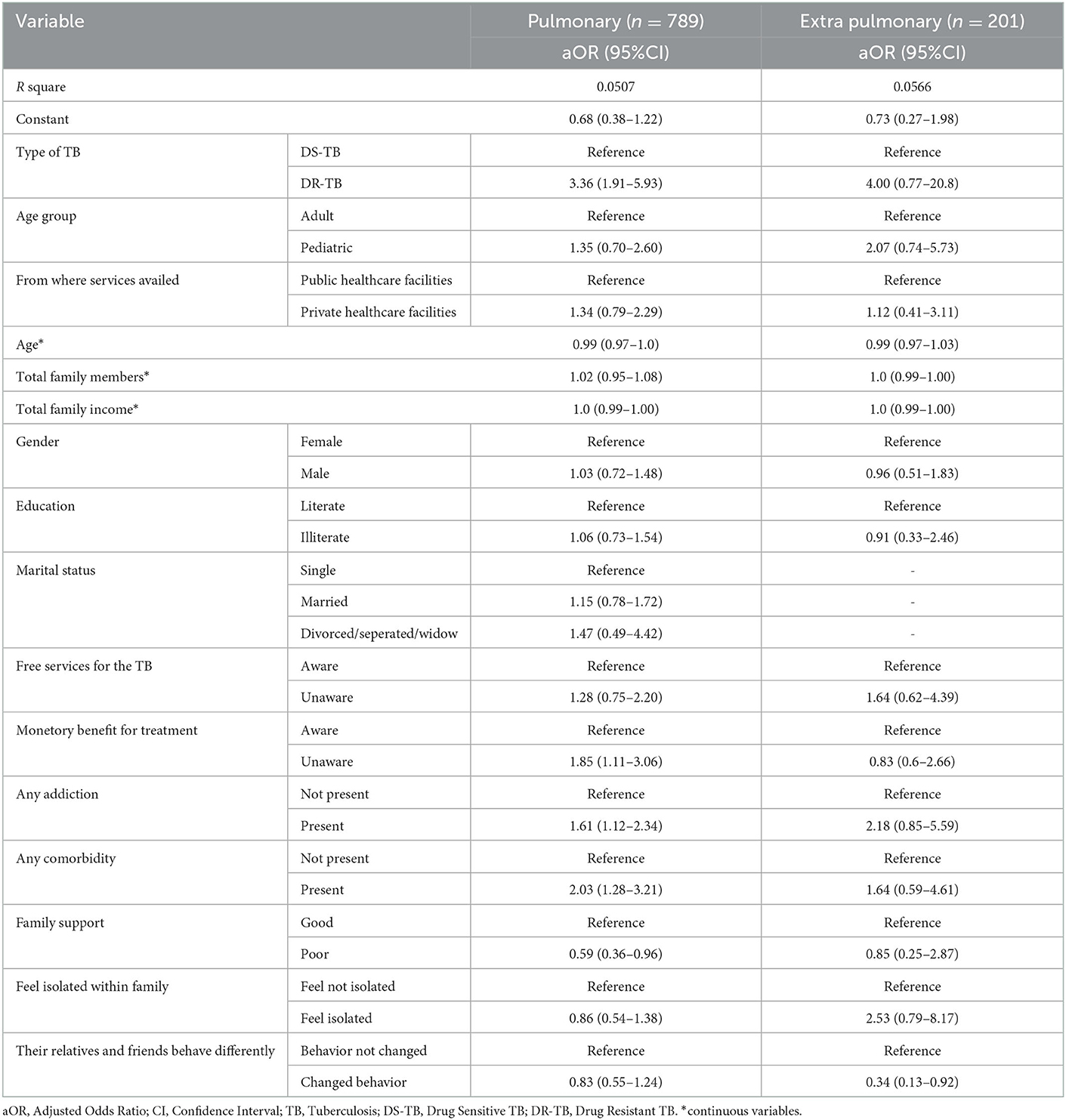
The multivariate logistic regression findings of the delays in different phases among pulmonary TB patients are depicted in Table 4. DR-TB patients were more likely to present with delay in treatment initiation (aOR = 3.49, 95%CI = 1.95–6.26) compared to DS-TB patients, found to be statistically significant. Pediatric patients were more likely to present with a delay in the diagnosis and treatment initiation (aOR = 1.71, 95%CI = 0.91–3.20; aOR = 1.46, 95%CI = 0.68–3.10) than the adults, while less likely to delay in the first formal consultation; however, found to be statistically non-significant. The patients availing services from the private health care facilities were more likely to have delay in first consultation (aOR = 1.07, 95%CI = 0.64–1.78) as compared to other phases and patients availing services from public health facilities (statistically non-significant). All the determinants for the extra-pulmonary TB were found to be statistically non-significant as indicated in Table 5. The pediatric patients were likelier to present delays in the first formal consultation and treatment initiation (aOR = 1.45, 95%CI = 0.68–3.10; aOR = 1.23, 95%CI = 0.53–2.84) than adults. DR-TB patients were more likely to present with delays in each phases i.e., first consultation (aOR = 2.14, 95%CI = 0.52–8.86), diagnosis (aOR = 7.51, 95%CI = 0.91–61.8) treatment initiation (aOR = 3.68, 95%CI = 0.45–30.23) compared to DS-TB patients.
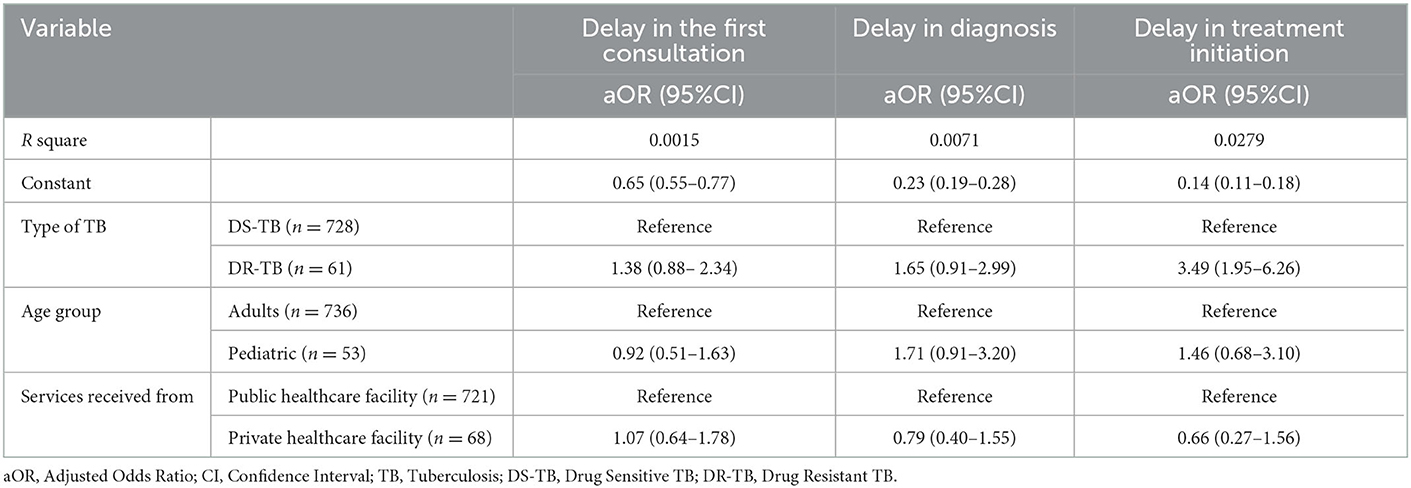
Table 4. Analysis of the delay in the various care cascade phases amongst the various pulmonary TB patients (N = 789).
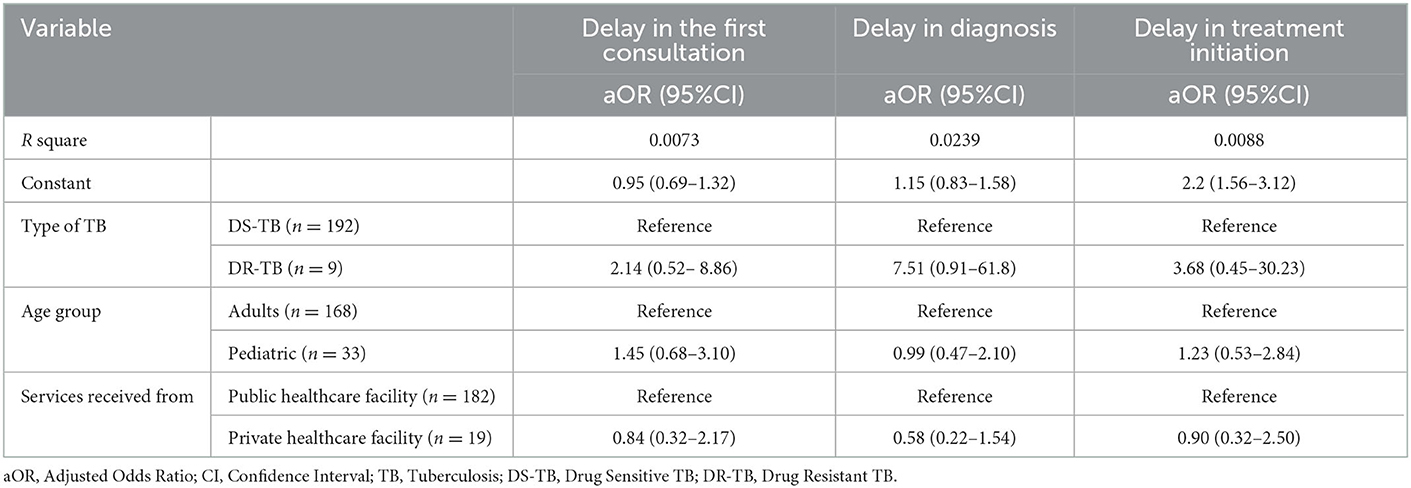
Table 5. Analysis of the delay in the various care cascade phases amongst the various extra-pulmonary TB patients (N = 201).
It was observed that DR-TB patients were more likely to present with total delay in both pulmonary and extra-pulmonary patients, which was found to be statistically non-significant among the extra-pulmonary patients. In the pulmonary patients, addiction to any substance (aOR = 1.61, 95%CI = 1.12–2.34) and the presence of co-morbidity (aOR = 2.03, 95%CI = 1.28–3.21) were the common factors responsible for the total delay. Similarly, addiction (OR = 2.18, 95%CI = 0.85–5.59) and co-morbidity (aOR = 1.64, 95%CI = 0.59–4.61) were also identified as risk factors for delay in extra-pulmonary patients, however, found to be statistically non-significant. Unaware of monetary benefits (aOR = 1.85, 95%CI = 1.11–3.06) was also one of the contributing factors to the total delay among the pulmonary patients. As presented in detail in Table 6. Unawareness of free services for TB was also one of the risk factors in both categories, while illiteracy was only in pulmonary patients.
3.2. Qualitative findings
3.2.1. System side actors' perception
The respondents reported that the unawareness among the community and stigma as one of the important factors responsible for the delay in the first formal consultation. Both system and demand side factors emerged as the reasons for the delay in the diagnosis. The overburden of the staff with work and negligence from the providers were reasons for the delay in the diagnosis. The stigma, addiction, lack of awareness and financial constraints contribute to the delay in the diagnosis. While for the treatment initiation, mainly the patients' behavior and lack of knowledge on the importance of treatment emerged as one of the factors responsible for the delay. Moreover, the delay in the first formal consultation was directly attributed to the missing TB cases by the system, the active case findings were not qualitatively assured or supervised and monitored, and a few gaps in contact tracing because of the migrant population. In the diagnostic cascade, the delay was attributed majorly to the poor infrastructure, quality of sputum samples submitted by patients, sample collection to transportation, and neglected referrals of TB comorbid cases. In the treatment cascade, the delay was attributed to the adverse drug reaction and its management and inadequate counseling by the healthcare staff. The major quotes are indicated below-
“There are few cases of the same (diagnosed but not put on treatment). Many are transfer outs and not recorded. Self-denial and doctor- hopping are common reasons.” (State TB Training & Demonstration Center Director).
“It is a fact that wherever we go(national level or local level) patients go for multiple consultations. If the person is educated, he will go for investigation but here it is a tribal area, so less awareness about TB…..” (Senior Treatment Supervisor).
“……Social stigma, Unawareness among the community, Financial constrain are among other prime factors in this rural part of the state.” (Medical Officer).
“delay in diagnosis is from the system side, due to workload not able to perform CBNAAT on time.” (Senior TB Laboratory Supervisor).
“…….2–3 days delay in turnaround time for CBNAAT, due to higher workload” (Senior TB Laboratory Supervisor).
“(Maximum delay) in diagnosis sir… due to poor infrastructure... there is no lacking on the part of patients…patients are coming at right place only but because of poor infrastructure, we are able to provide timely services…” (Senior Treatment Supervisor)
“There is delay. There is huge negligence in private sectors. Private doctors initiate general treatment and they do not keep TB in their differential diagnosis……”. (Medical Officer).
“A bit of delay in diagnosis is the from system side issues. Secondly due to lack of awareness patient could not reach to us… there are the two main reason in TB” (Medical Officer).
“Patient does not feel the importance of getting diagnosed, so they refuse sometimes. Social stigma. Alcoholism.” (Laboratory Technician).
“Main reason for the delay in diagnosis is that people are alcoholic, financial constraint (transportation) and lack of awareness and importance of the disease.” (TB health visitor).
“Some patients (TB confirmed) refuse to take medicine because of addiction (smoking/alcohol). Takes time to convince them.” (Laboratory Technician).
“Patient having no knowledge on importance of treatment. Even patients having MDR TB along with comorbid condition refuses for treatment management at DTC.” (Medical Officer).
3.2.2. Demand side perception
The patients shared that the lack of knowledge regarding the TB symptoms and addiction were the major reasons responsible for the delay in care seeking at various phases of the care cascade. The fear of isolation, health-seeking behavior and the perceived severity of the symptoms also contribute to the delay. Moreover, the delays in the first formal consultation phase were attributed to the ease of access to the traditional healers, patient literacy about TB care, and health-seeking behavior and attitude of the respective patients. During the diagnostic cascade, the delay was attributed to the stigma related to the TB diagnosis and fear, patients were from remote areas and traveled only for consultation. In the treatment care cascade, the delay was attributed to the potential discrimination for taking TB drugs for a long duration by family/ community, poverty leading to an inability for physical access to the services, migration as part of the livelihood, adverse drug reactions potentially prolong use of substance abuse and addictions and multiple reasons for treatment interruptions.
“I thought there was some delay in treatment initiation because at that time I was not aware regarding TB symptoms…..” (DS-TB patient).
“…..Who take medicines, it is better to have alcohol rather than medicines” (DR-TB patient).
“Few people forced (indicated surrounded neighbors) that if my symptoms are TB, then they will not mingle with me…….So, I was afraid” (DS TB patient).
“Initially, I thought the symptoms are seasonal, so brough a few medicines from one of the nearest doctor (informal provider). It was good for few days. When symptoms again aggravated, I went to the Govt. hospital and there they said it's TB……” (EP TB patients).
“I took medicines for cough and cold over 3 months, but symptoms didn't subside” (Extra-pulmonary TB patient).
“…and chemist also said that this is the normal cough, and having cough in this season is quite normal so, it will be fine after few days of medication” (DS-TB patient).
“What does a layman do, when (s)he develops cold/cough, then simply go to a chemist and take medicines; I did the same” (DS TB patient)“…almost 5 months taken for proper treatment initiation. Initially went to the informal provider where almost Rs. 2,000 spent then went to private doctors where tests were done and medicine given but not got relief…….” (MDR-TB patient).
4. Discussion
This study aimed to assess the delay among TB patients, which is an important factor contributing to the successful treatment outcome. The findings of this study revealed a substantial delay in care-seeking at the various phases of the care cascade in TB patients. Our study found that the delay in the first formal consultation of 41% is the highest among all three delays across the phases of the care cascade in pulmonary patients. This prevalence rate of delay in care-seeking is quite similar to what was found in studies from Ethiopia and South Africa (28, 29). However, studies from various states of India reported a delay in care-seeking ranging from 27 to 74% (14, 21, 27, 30). In contrast, delay in treatment initiation is highest in extra-pulmonary patients, and almost half of the patients reported total delay. Patients with DR-TB are more prone to report the total delay in the care cascade among the pulmonary patiets. One of the Indian studies also reports that the median onset of symptoms to first consultation and first consultation to diagnosis was higher in multidrug-resistant (MDR) patients than the non-MDR (31).
The findings from the systematic review from India states the median patient delay (i.e., delay in first formal consultation), diagnostic delay and treatment delay of 18.4, 31.0, and 2.5 days, respectively (13); this median duration is higher than the duration we found in this study. One of the possible reasons for these variations in median and prevalence could be that delay is defined differently in each study.
The addiction to any substance among TB patients emerged as one of the contributing factors to total delay in pulmonary TB patients. This was also found in other studies (14, 17, 21, 32) conducted in various categories of TB patients. Various studies from different parts of the country stated that literacy level (32), financial constraints (14, 15, 17, 30, 33, 34), myths / wrong beliefs (14, 15, 17, 21, 30, 33–36), knowledge regarding availability of the services (15, 32), contribute to the delay at various phases of the care cascade. This study also reports the unawareness among the patients regarding the services available as one of the risk factors for total delay among pulmonary patients. This highlights the importance of creating awareness among the community regarding the disease and the services and benefits available. Another finding is that illiteracy is one of the risk factors for delay in pulmonary patients (although statistically non-significant, this was evident in qualitative findings).
In a few studies, social stigma, discrimination (34, 36, 37) and lack of family support (17) were identified as the contributing factors to delay in care-seeking. However, in particular, in this study, we did not find any significant difference in family support, discrimination and stigma as risk factors for the delay; however, in qualitative, it was prompted.
Understanding delay and its factors will minimize patient loss across the TB care cascade, as evidenced in the literature (38, 39). Future research on a similar topic with various TB patients across India is recommended to understand the divergent delay and its associated contextual factors. There is a lack of evidence in extra-pulmonary TB patients; however, few international studies are available (40). Hence, the delayed assessment should comprise extra-pulmonary TB patients distinctly different from the pulmonary TB care-seeking pathways recommended for contextual understanding. Documenting the delay attributes across the different geographical contexts is important, as both the system and demand side factors vary significantly. A comprehensive strategy addressing all these factors is recommended within the national TB elimination program to minimize the delays in the TB care cascade and ultimately achieve the larger goal of End TB strategy.
One of the limitations of this study is that all the data was collected retrospectively, so patients may fail to remember the exact date for the events of the care cascade. Therefore, there is a chance of recall bias. However, all the research teams involved in the data collection process trained thoroughly to get the most accurate details from the patients. Secondly, we could not include the missing cases that were not notified under the nikshay. Third, there were no such thumb rules to include minimum number of TB patients per each categories such as DR-TB and pediatric TB. We have intended to capture minimum of 30 patients and a diverse representation to run the statistical analysis. Fourth, we were able to recruit only 10 TB patients as part of the qualitative enquiry. In an ideal scenario for qualitative data collection, data should be collected till saturation; however, due to the project timeline, we were not in a position to continue the data collection, which is considered one of the limitations of the demand side qualitative assessment.
5. Conclusion
In this cross-sectional study, more than half (52.3%) of pulmonary TB patients reported a delay in care-seeking during any phase of the care cascade. While in the extra-pulmonary patients, it is even higher than that. Almost 41% of the pulmonary and 51% of the extra-pulmonary patients had reported total delay in the care cascade. Out of all three delays at the various phases of the care cascade, delay in initial formal consultation after the onset of the symptoms is most common, followed by a delay in diagnosis and treatment initiation in pulmonary patients. While in extra-pulmonary patients, delay in treatment initiation is most common, followed by the diagnosis and first formal consultation. DR-TB patients are more prone to total delay and delay in the treatment initiation among pulmonary patients; however, a similar observation was statistically non-significant among the extra-pulmonary patients. Factors like awareness regarding monetary benefits available for TB patients, addiction, and co-morbidity contribute significantly to the total delay among pulmonary TB patients. There were a few systems-side factors, such as inadequate case findings in the first formal consultation, poor infrastructure in the diagnostic cascade and inadequate adverse drug reaction management in the treatment cascade, among other attributes to the delay. The TB care cascade delay is multi-dimensional, as indicated by both the system and demand side attributes having their own contribution. Therefore, the balance between service delivery and socio-cultural context needs strategies to address the delays in the TB care cascade.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Institutional Ethics Committee (IEC) of the Indian Institute of Public Health Gandhinagar (IIPHG), India. The patients/participants provided their written informed consent to participate in this study.
Author contributions
SY, HS, SS, and DS participated in the conception and design of the study protocol. SS, AS, TP, YP, and DS involved in project administration. SY, HS, PB, and JP collected the field data and conducted the interviews. SY and PB analyzed the data. PB drafted the first draft of the paper. SY, HS, SS, AS, TP, YP, and DS critically reviewed the paper. All authors contributed equally to the development of this study and read and approved the final manuscript.
Funding
This study was made possible by the generous support of the American people through the United States Agency for International Development (USAID). The work described in this article was implemented under the USAID Closing the gaps in TB Care Cascade Project, managed by World Health Partners under the terms of Cooperative Agreement Number 72038620CA00012. Staff of the funding agency critically reviewed the draft and offered comments to improve the paper.
Acknowledgments
We wish to extend our gratitude to the Health and Family Welfare, the Government of Gujarat & Jharkhand, and State TB Training and Demonstration Center (STDC) team and National Tuberculosis Elimination Programm (NTEP) staff for their kind support during the project activities. We are thankful to the State TB Officers, District TB Officers, all the NTEP staff and all the participants of Gujarat and Jharkhand for providing the necessary information for this study. We are also thankful to the research team of the Indian Institute of Public Health Gandhinagar (IIPHG) for their support during the field activities. We would like to thank the World Health Partners (WHP) for their continuous support in the Closing the gaps in TB Care Cascade (CGC) project. We express our sincere thanks to USAID New Delhi, India, for funding this study as a part of the larger project, namely, Closing the gaps in the TB care cascade.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The US Agency for International Development administers the US foreign assistance program providing economic and humanitarian assistance in more than 80 countries worldwide. This study is made possible by the generous support of the American people through the United States Agency for International Development (USAID). The contents are the responsibility of the authors and do not necessarily reflect the views of USAID or the United States Government.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1015024/full#supplementary-material
References
1. World Health Organization (WHO). Tuberculosis. (2022). Available online at: https://www.who.int/news-room/fact-sheets/detail/tuberculosis (accessed May 29, 2022).
2. World Health Organization (WHO). Global Tuberculosis Report 2021. Geneva: World Health Organization (2021).
3. World Health Organization (WHO). Treatment of Tuberculosis: Guidelines. 4th ed. World Health Organization (2010).
4. Sreeramareddy CT, Panduru KV, Menten J, van den Ende J. Time delays in diagnosis of pulmonary tuberculosis: a systematic review of literature. BMC Infect Dis. (2009) 9:1–10. doi: 10.1186/1471-2334-9-91
5. Alema HB, Hailemariam SA, Misgina KH, Weldu MG, Gebregergis YS, Mekonen GK, et al. Health care seeking delay among pulmonary tuberculosis patients in North West zone of Tigrai region, North Ethiopia. BMC Infect Dis. (2019) 19:1–8. doi: 10.1186/s12879-019-3893-7
6. Yoshikawa R, Kawatsu L, Uchimura K, Ohkado A. Delay in health-care-seeking treatment among tuberculosis patients in Japan: what are the implications for control in the era of universal health coverage? Western Pac Surveill Response J. (2020) 11:37–47. doi: 10.5365/wpsar.2019.10.1.010
7. Gopinath R, Bhatia R, Khetrapal S, Ra S, Babu GR. Tuberculosis Control Measures in Urban India. Strenthening delivery of comprehensive primary health services ADB South Asia. Working Paper Ser. (2020) 80:1–102. doi: 10.22617/WPS200409-2
8. Gebreegziabher SB, Bjune GA, Yimer SA. Total delay is associated with unfavorable treatment outcome among pulmonary tuberculosis patients in West Gojjam Zone, Northwest Ethiopia: A prospective cohort study. PLoS ONE. (2016) 11:1–16. doi: 10.1371/journal.pone.0159579
9. Virenfeldt J, Rudolf F, Camara C, Furtado A, Gomes V, Aaby P, et al. Treatment delay affects clinical severity of tuberculosis: a longitudinal cohort study. BMJ Open. (2014) 4:4818. doi: 10.1136/bmjopen-2014-004818
10. Vesga JF, Hallett TB, Reid MJA, Sachdeva KS, Rao R, Khaparde S, et al. Assessing tuberculosis control priorities in high-burden settings: a modelling approach. Lancet Glob Health. (2019) 7:e585–95. doi: 10.1016/S2214-109X(19)30037-3
11. World Health Organization; Regional Office for the Eastern Mediterranean. Diagnostic and Treatment Delay in Tuberculosis. World Health Organization (2006). Available online at: https://apps.who.int/iris/handle/10665/116501
12. Yimer S, Bjune G, Alene G. Diagnostic and treatment delay among pulmonary tuberculosis patients in Ethiopia: a cross sectional study. BMC Infect Dis. (2005) 5:1–7. doi: 10.1186/1471-2334-5-112
13. Sreeramareddy CT, Qin ZZ, Satyanarayana S, Subbaraman R, Pai M. Delays in diagnosis and treatment of pulmonary tuberculosis in India: a systematic review. Int J Tubercul Lung Dis. (2014) 18:255–66. doi: 10.5588/ijtld.13.0585
14. Mistry N, Rangan S, Dholakia Y, Lobo E, Shah S, Patil A. Durations and delays in care seeking, diagnosis and treatment initiation in uncomplicated pulmonary tuberculosis patients in Mumbai, India. PLoS ONE. (2016) 11:1–17. doi: 10.1371/journal.pone.0160796
15. Valvi C, Chandanwale A, Khadse S, Kulkarni R, Kadam D, Kinikar A, et al. Delays and barriers to early treatment initiation for childhood tuberculosis in India. HHS Public Access. (2020) 23:1090–9. doi: 10.5588/ijtld.18.0439
16. Shewade HD, Govindarajan S, Thekkur P, Palanivel C, Muthaiah M, Kumar AM, et al. MDR-TB screening in a setting with molecular diagnostic techniques: who got tested, who didn't and why? Pubic Health action. (2015) 5:132–9. doi: 10.5588/pha.14.0098
17. Velavan A, Purty AJ, Shringarpure K, Sagili KD, Mishra AK, Selvaraj KS, et al. Tuberculosis retreatment outcomes and associated factors: a mixed-methods study from Puducherry, India. Public Health Action. (2018) 8:187–93. doi: 10.5588/pha.18.0038
18. Yasobant S, Bhavsar P, Kalpana P, Memon F, Trivedi P, Saxena D. Contributing factors in the tuberculosis care cascade in India : a systematic literature review. Risk Manag Healthc Policy. (2021) 3275–86. doi: 10.2147/RMHP.S322143
19. Samal J. Health seeking behaviour among tuberculosis patients in India: a systematic review. J Clin Diag Res. (2016) 10:LE01. doi: 10.7860/JCDR/2016/19678.8598
21. van Ness SE, Chandra A, Sarkar S, Pleskunas J, Ellner JJ, Roy G, et al. Predictors of delayed care seeking for tuberculosis in southern India: an observational study. BMC Infect Dis. (2017) 17:1–9. doi: 10.1186/s12879-017-2629-9
22. Creswell JW, Clark VLP. Designing and Conducting Mixed Methods Research. 3rd ed. Thousand Oaks, CA: SAGE (2018). 849 p.
24. Jhonny Saldana. The Coding Manual for Qualitative Research. (2nd ed. SAGE Publications) (2013). Available online at: https://emotrab.ufba.br/wp-content/uploads/2020/09/Saldana-2013-TheCodingManualforQualitativeResearchers.pdf (accessed September 12, 2022).
25. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. (2007) 19:349–57. doi: 10.1093/intqhc/mzm042
26. Central TB Division Ministry of Health & Family Welfare Government Government of India and World Health Organization Country Office for India. Standards of TB Care in India. (2014).
27. Das S, Basu M, Mandal A, Roy N, Chatterjee S, Dasgupta A. Prevalence and determinants of delay in diagnosis of pulmonary tuberculosis in Darjeeling district of West Bengal. J Family Med Prim Care. (2017) 6:627. doi: 10.4103/2249-4863.214432
28. Wondawek TM, Ali MM. Delay in treatment seeking and associated factors among suspected pulmonary tuberculosis patients in public health facilities of Adama town, eastern Ethiopia. BMC Public Health. (2019) 19:1–7. doi: 10.1186/s12889-019-7886-7
29. Chiposi L, Cele LP, Mokgatle M. Prevalence of delay in seeking tuberculosis care and the health care seeking behaviour profile of tuberculous patients in a rural district of Kwazulu Natal, South Africa. Pan Af Med J. (2021) 39. doi: 10.11604/pamj.2021.39.27.26717
30. Mistry N, Lobo E, Shah S, Rangan S, Dholakia Y. Pulmonary tuberculosis in Patna, India: durations, delays, and health care seeking behavior among patients identified through household surveys. J Epidemiol Glob Health. (2017) 7:241–8. doi: 10.1016/j.jegh.2017.08.001
31. Atre SR, Jagtap JD, Faqih MI, Dumbare YK, Sawant TU, Ambike SL, et al. Tuberculosis pathways to care and transmission of multidrug resistance in India. Am J Respir Crit Care Med. (2022) 205:233–41. doi: 10.1164/rccm.202012-4333OC
32. Vijay S, Kumar P, Chauhan LS, Vollepore BH, Kizhakkethil UP, Rao SG. Risk factors associated with default among new smear positive TB patients treated under DOTS in India. PLoS ONE. (2010) 5:43. doi: 10.1371/journal.pone.0010043
33. Jaggarajamma K, Sudha G, Chandrasekaran V, Nirupa C, Thomas A, Santha T, et al. Reasons for non-compliance among patients treated under revised national tuberculosis control programme (RNTCP), Tiruvallur district, south India. Indian J Tuberc. (2007) 54:130–5.
34. Yerramilli A, Narreddy S, Anisetti R, Grace A, Rakuditti S. Patient's perceptions of barriers to tuberculosis care in private sector in India. InOpen Forum Infect Dis. (2019) 6:2019. doi: 10.1093/ofid/ofz360.1236
35. Bagchi S, Ambe G, Sathiakumar N. Determinants of poor adherence to anti-tuberculosis treatment in Mumbai, India. Int J Prev Med. (2010) 1:223–32.
36. Shewade HD, Kokane AM, Singh AR, Parmar M, Verma M, Desikan P, et al. Provider reported barriers and solutions to improve testing among tuberculosis patients “eligible for drug susceptibility test”: a qualitative study from programmatic setting in India. PLoS One. (2018) 13:1–18. doi: 10.1371/journal.pone.0196162
37. McArthur E, Bali S, Khan AA. Socio-cultural and knowledge-based barriers to tuberculosis diagnosis for women in Bhopal, India. Indian J Commun Med. (2016) 41:62–4. doi: 10.4103/0970-0218.170990
38. Padayatchi N, Daftary A, Naidu N, Naidoo K, Pai M. Tuberculosis: treatment failure, or failure to treat? Lessons from India and South Africa. BMJ Glob Health. (2019) 4:e001097. doi: 10.1136/bmjgh-2018-001097
39. Subbaraman R, Nathavitharana RR, Mayer KH, Satyanarayana S, Chadha VK, Arinaminpathy N, et al. Constructing care cascades for active tuberculosis: a strategy for program monitoring and identifying gaps in quality of care. PLoS Med. (2019) 16:2754. doi: 10.1371/journal.pmed.1002754
Keywords: delay, care cascade, tuberculosis, factors for delay, India
Citation: Yasobant S, Shah H, Bhavsar P, Patel J, Saha S, Sinha A, Puwar T, Patel Y and Saxena D (2023) Why and where?—Delay in Tuberculosis care cascade: A cross-sectional assessment in two Indian states, Jharkhand, Gujarat. Front. Public Health 11:1015024. doi: 10.3389/fpubh.2023.1015024
Received: 09 August 2022; Accepted: 02 January 2023;
Published: 27 January 2023.
Edited by:
Belaineh Girma Belaineh, International Training and Education Center for Health (I-TECH), United StatesReviewed by:
Ankita Kankaria, All India Institute of Medical Sciences, Bathinda (AIIMS Bathinda), IndiaMing Luo, Chongqing Public Health Medical Center, China
Kuldeep Singh Sachdeva, International Union Against Tuberculosis and Lung Disease (The Union), France
Copyright © 2023 Yasobant, Shah, Bhavsar, Patel, Saha, Sinha, Puwar, Patel and Saxena. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Deepak Saxena,  ZGRlZXBhazcyQGlpcGhnLm9yZw==
ZGRlZXBhazcyQGlpcGhnLm9yZw==
 Sandul Yasobant
Sandul Yasobant Harsh Shah
Harsh Shah Priya Bhavsar
Priya Bhavsar Jay Patel1
Jay Patel1 Somen Saha
Somen Saha Deepak Saxena
Deepak Saxena