- 1College of Medicine, Mohammed Bin Rashid University of Medicine and Health Sciences, Dubai, United Arab Emirates
- 2Green Life Medical College and Hospital, Dhaka, Bangladesh
- 3West Bengal University of Health Sciences, Kolkata, India
- 4Faculty of Medicine, Dow Medical College, Dow University of Health Sciences, Karachi, Pakistan
- 5Institute for Excellence in Health Professions Education, Mohammed Bin Rashid University of Medicine and Health Sciences, Dubai, United Arab Emirates
Objectives: Vaccine hesitancy remains a global issue, especially within poverty-stricken countries where there's an interplay of financial and non-financial barriers. This narrative review aims to understand attitudes and behaviors toward COVID-19 vaccination in four South Asian countries and make context-specific recommendations to vaccine program drivers and decision-makers.
Methods: A search was conducted using PubMed and Science Direct, and CINHAL from January 2020 up to May 2022 restricted to the English language for terms: “Afghanistan” OR “Pakistan” OR “India” OR “Bangladesh” in combination with “COVID-19 vaccine” and other related terms. All articles were initially included, and those with relevance were included in the synthesis of this paper.
Results: A narrative review was performed for this study. Our narrative review included a total of eighteen studies with a sample size (n = 223–5,237) averaging about 1,325 participants per study conducted. The studies included revealed public hesitancy to receive the COVID-19 vaccine ranging from 6.3 to 56.2% with an average of 31.63% across all eighteen studies. Several reasons were linked to this observation in these four South Asian countries, and the predominant ones included: Insufficient information provided to the general public about the side effects of the vaccines, concerns regarding vaccine safety, and skepticism of vaccine efficacy.
Conclusion: Vaccine hesitancy is a global problem within the context of COVID-19, and issues regarding equity, misinformation, and poverty in South Asian countries makes it difficult to meet goals for herd immunity. Policymakers and governments should aim toward financial and non-financial incentives to drive the public toward vaccination.
Introduction
Vaccines are considered to be one of the most efficacious public health intercessions in preventing further disease progression and reducing mortality rates worldwide. Over the recent years, they have been increasingly employed in various successful outbreak-related response strategies proving their essential role in the abatement of communicable diseases (1, 2). Despite the paramount evidence provided by experts in this field, there still remains a prevailing public concern globally over the safety of these therapeutic agents (3). Vaccine hesitancy, as stated by the World Health Organization (WHO) is defined as a “delay in acceptance or refusal of vaccines despite availability of vaccination services” (4). This phenomenon is being observed in many communities and especially in the South Asian region where imputable causes are plenty.
Vaccine hesitancy poses a substantial threat to tackling pandemics and most notably, the current COVID-19 pandemic which relies heavily on vaccination rings and public uptake in creating herd immunity. The causes behind this alarming phenomenon vary but can be attributed to the shaken public trust in the services provided by the healthcare systems in these countries, various doubts and mistrust of the efficacy of such interventions, and the circulated false social media claims as well as a plethora of non-factual medical statements made by religious figures in these countries (5). Additionally, socio-demographic factors have been widely studied and have shown that people residing in urban areas, those with a lower education level and a lower family economic status are more likely to be hesitant to receive the vaccine (6).
The COVID-19 situation in South Asia, in particular in Afghanistan, Pakistan, India, and Bangladesh is highly critical as these countries are among the most poverty-stricken regions of the world, accounting for a substantial portion of COVID-19 cases globally with a total count of 47,580,486 cases to date (7). By understanding the public's behaviors and attitudes toward vaccinations, we can suggest key recommendations for expanding the coverage and help correct any vaccine-related misinformation that could relate itself to the denial or active rejection of this effective tool. Furthermore, the involvement of key health policymakers in improving the containment strategies in these countries could reflect an enhanced approach to vaccination implementation. Our narrative review aims to bring national attention to an already existing problem that has been further exacerbated by the COVID-19 pandemic and to consequently use the mentioned studies' findings to help deliver context-specific recommendations to vaccine program drivers and decision-makers, thereby increasing public confidence and trust in the accessible vaccines.
Materials and methods
A narrative review was performed using PubMed and ScienceDirect, and CINHAL from January 2020 up to May 2022. The search was restricted to the English language, in order to identify COVID-19 vaccine hesitancy in the included countries. The last search was performed on the 9th of May 2022. We included the following search terms: “Afghanistan” OR “Pakistan” OR “India” OR “Bangladesh” in combination with “COVID-19 vaccine” and “vaccine hesitancy” with any other relevant and identified synonyms. We included only survey-based studies with a primary outcome of COVID-19 vaccine hesitancy, which were conducted in South Asian countries. These studies investigated the perception, vaccine confidence, and vaccine hesitancy in these populations Following this initial literature review, we only included the articles which were pertinent to our research aims. The final database of studies included one of the four aforementioned countries with a clear focus on COVID-19 vaccine hesitancy amongst the public (Figure 1).
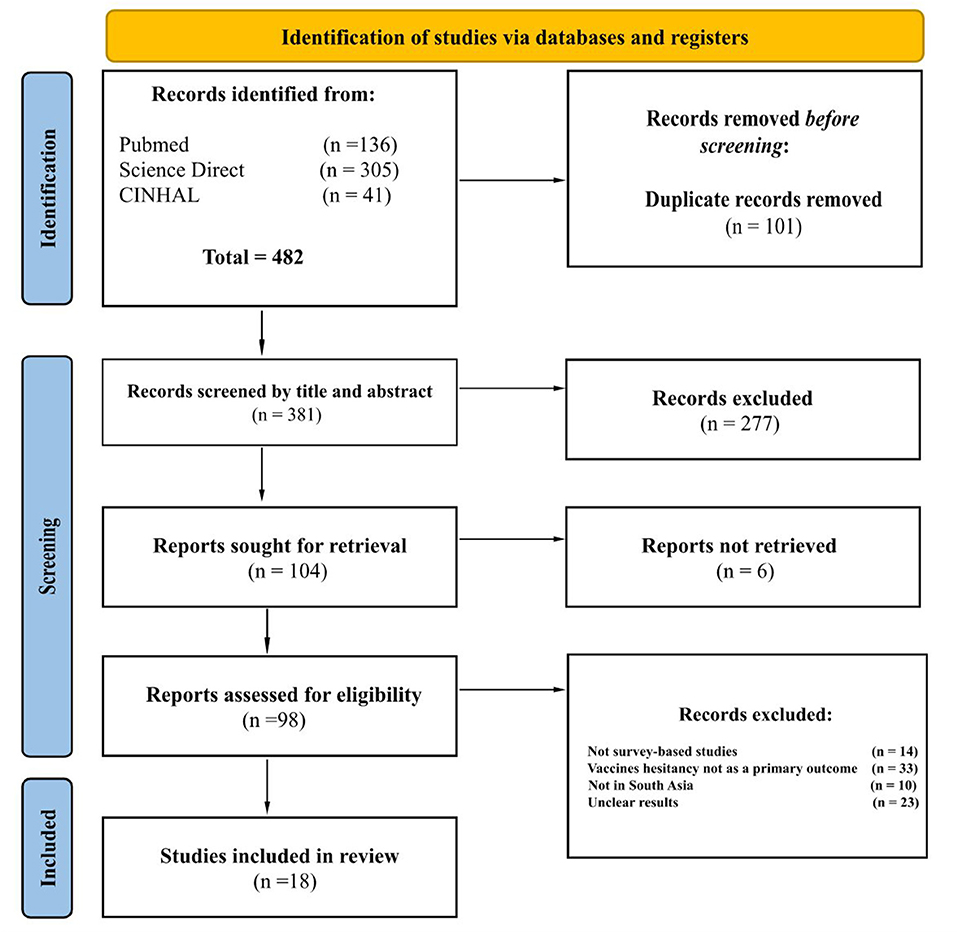
Figure 1. PRISMA flow diagram highlighting the selection process of the final studies included in this narrative review.
Results
The final pool of the studies comprised a sample size ranging from 223 to 5,237 participants with an average study sample of 1,325 and a total of 23,854 participants across all eighteen studies included (8–25). Our review included a total of one study from Afghanistan, five from Bangladesh, eight from India and four from Pakistan. Amongst the studies that explored reasons for vaccine hesitancy, it was noted that insufficient information provided to the public and increased concerns about vaccine safety and efficacy were identified as being the major arguments for COVID-19 vaccine refusal and hesitancy. Additionally, other reported reasons included the public perception that the COVID-19 vaccines might low-quality. Another common argument made was that people did not anticipate being infected with the virus hence, they did not feel the urge to seek the vaccines. From these four South Asian countries, we concluded that the prevalence of vaccine hesitancy for COVID-19 varied from 6.3 to 56.2% with an average rate of 31.63%.
Study participants included in this narrative literature review differed in age, gender, ethnicity, profession, the highest level of education attained, financial income, and marital status (Table 1).
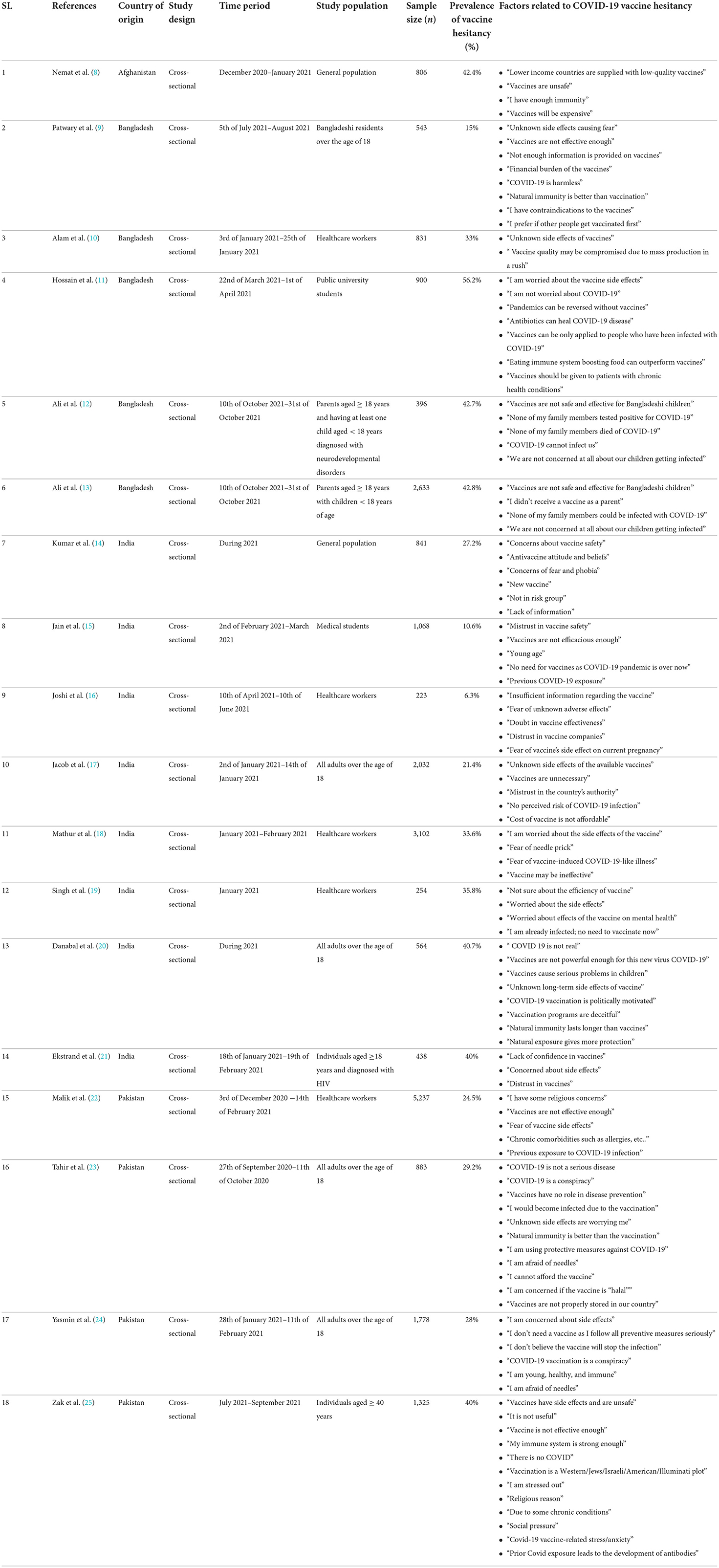
Table 1. Survey-based cross-sectional studies included in this narrative review relevant to COVID-19 vaccine hesitancy factors in Afghanistan, Pakistan, India, and Bangladesh.
Discussion
Vaccine hesitancy has been a prevailing concern reported by policymakers at varying levels, across as many as 90% of countries worldwide (26). Since the outbreak of the pandemic in 2020, a long journey of at least partially vaccinating 64.5% of the population across the globe, has been traversed (27). The issue of vaccine hesitancy remains a growing phenomenon, particularly during the COVID-19 pandemic. Unduly vaccine development efforts resulting in poor vaccine efficacy, and adverse reactions have been reported as some of the reasons behind the public's refusal to seek vaccines. Usually, the acceptability of a vaccine is said to have been influenced by the level of awareness about a disease, availability, and accessibility to a healthcare commodity (28).
Approximately, 49% of Pakistani citizens were reluctant to receive the COVID-19 vaccine (29). As of the 30th of April 2022, around 59.65% of the residents had been vaccinated (27). A literature review by Nemat et al. reported that about 88% of Afghanis were aware of the efforts being made to develop vaccines for COVID-19. They also observed a significantly higher number of females than males, eager to receive the COVID-19 vaccine, this comes in contrast to a European survey suggesting the opposite (8). Paterson et al. reported that vaccine hesitancy is also prevalent among healthcare workers and especially medical students (30, 31). Since January 2021, the COVID-19 vaccination programs in India had initially prioritized the frontline healthcare workers and then gradually, spread its programs to cover the rest of the population. It is noteworthy to mention that 61.98% of India's citizens are fully vaccinated (27). Abedin et al. observed that 74.5% of Bangladeshi citizens were keen to get the COVID-19 vaccination, resonating with France, Australia, Mexico, India, and Ireland, as confirmed by a population-based study conducted in these countries (32).
In addition, the assumed poor vaccine quality amongst the public, growing concerns over vaccine safety, and efficacy, rumors about clots during menstruation, and infertility have led to apprehensions regarding the COVID-19 vaccine. Few people even believed that the available vaccines may increase the mortality rate (6). Trust in the government due to inaccessible and inequitable distribution of economy and healthcare facilities among the communities, is also one of the major factors contributing to vaccine hesitancy. Furthermore, lack of technological literacy and poor refrigeration facilities adds to the dissimilar distribution of the COVID-19 vaccines across different regions in the same country.
Executing an effective mass vaccination drive demands the addressal of COVID-19 vaccine hesitancy. It is also essential to acknowledge various other factors which play an important role in these countries such as societal beliefs and literacy rates. Mass vaccination should be aimed at addressing the factors leading to vaccine hesitancy via interventions tailored to societal concerns and parameters, not restricted to any specific region.
The aim of the review is to illustrate the prevalence and describe the predictors of the COVID-19 vaccine hesitancy, in Pakistan, Afghanistan, India, and Bangladesh, with the latest available evidence, thereby, increasing the literature coverage in scoping. This will invaluably aid the various programs promoting vaccinations to raise awareness while addressing individual, economic, socio-cultural, political, and regional barriers. Specific proposals and recommendations formulated with the aid of public-private partnerships (PPP) would go a long way in combating this problem. The key to success in attaining herd immunity against COVID-19 mostly relies on the public uptake of the vaccines available. However, new emerging viral mutants, formed due to rapid antigenic shift and drift, are a constant challenge, which demands the attention of researchers worldwide.
Current efforts to combat COVID-19 vaccine hesitancy in these countries
In Pakistan, various efforts are being made at different levels to raise awareness about the efficacy of the COVID-19 vaccine, these include radio messages and large-scale video transmissions on TV and the internet providing the necessary adequate knowledge about vaccines and empowering the general public to accept the COVID-19 vaccine, as well as door-to-door vaccine administration and awareness drives similar to those used for Polio (33). Meanwhile, the government in India is not making any significant efforts to combat vaccine hesitancy; nevertheless, a “time-bound inquiry” into deaths that occurred soon after vaccination was ordered, and each mobile phone call in the country was automatically initiated by a national programmed message from the Indian government affirming the safety and effectiveness of vaccines (34). Several initiatives are being implemented in Afghanistan to prevent vaccination hesitancy, including routine immunization vaccinators and the deployment of 2,000 more new health professionals (teams of two people: one male and one female), raising societal awareness and educating them, and avoiding myths (35). Similarly, in Bangladesh, the most popular variables contributing to decreasing vaccination hesitancy include social media and awareness campaigns (36).
To lessen the impact of vaccine hesitancy, it is imperative to critically analyze the situation based on different countries. Each country has a unique context that should be taken into consideration. Hence, varied policies are need to be enacted so as to ensure that each country can impede the impact of vaccine hesitancy.
Effects and recommendations of COVID-19 vaccine hesitancy in Afghanistan
In Afghanistan, the presence of conflict, illiteracy, and poverty has favored the condition for COVID-19 to continue spreading. Despite the country's high trends of other problems, the virus has only become a normal disease for some people. The continued spread has also impacted the uptake of the vaccines. A study conducted in the capital of Afghanistan, Kabul, revealed that 37% of the population is hesitant to receive the vaccine. In order to improve the situation, community engagements to raise awareness about the harmful effects of COVID-19 and the positive effects of the vaccines are important to be conducted. Moreover, social media awareness is also considered essential to improve the public's perception. However, it must be monitored to detect any source of misinformation and immediately stifle it. Lastly, in a country like Afghanistan, people pay great attention to religion and religious figures. Therefore, religious figures' engagement is crucial to raise awareness about important aspects of the vaccines (8).
Effects and recommendations of COVID-19 vaccine hesitancy in India
The Republic of India is not strange in facing vaccine hesitancy. This longstanding problem has resulted in a deferment in achieving the vaccination target for COVID-19. However, the Indian government is firmly strengthening its vaccination drives, via mass, print as well as social media coverage to help burst the myths surrounding the COVID-19 vaccines. It is also imperative to encourage joint efforts between district-level administrations and political leaders to dispel the hoax around COVID-19 vaccines through awareness sessions using regional folk songs.
Nevertheless, it is critical for the nation to develop an effectively sustainable campaign to tackle vaccine hesitancy. The government should invest in evidence-based research, as a public-private partnership, identify the population strata with distrust in vaccines with a resolute to resolve their hesitancy to expand wide immunization coverage. A versatile team comprising of experts from different fields such as immunology, pharmacology, microbiology, behavioral science, and sociology should be formulated at the national as well as, regional levels to conduct rigorous research and come up with solutions to help people accept the COVID-19 vaccines.
Communicating the advantages of vaccines in colloquial languages, backed by strong methodological proof of vaccine safety and efficacy, in addition to street plays to raise awareness, would pave the way in building the confidence of the masses in vaccines. Optimizing the support of mass media communications, and public posters to dismiss the hearsay and promote vaccines, besides, door-to-door campaigns conducted by social healthcare workers might be pivotal in instilling trust in vaccines (37).
Furthermore, rapid interventions are needed to accelerate the COVID-19 vaccination availability across the healthcare sectors and especially among individuals seeking the vaccines but facing inaccessibility to the vaccination centers. In order to encourage mass coverage, the administration should either make the vaccination available free of cost or provide reimbursement of the charges or tie up with the health insurance companies to cover the cost. Non-financial incentives, such as complimentary food items or a free health check-up, may also help out in the intention of combating vaccine hesitancy (38). Such sustained financial or non-financial incentives for vaccination coupled with public engagements would gauge the doubtfulness of the public and addresses their growing concerns.
Effects and recommendations of COVD-19 vaccine hesitancy in Bangladesh
According to many surveys conducted in Bangladesh, there has been significant vaccine hesitancy shown by the general public owing to personal beliefs, mistrust, religious factors, conspiracy theories, and concerns about vaccine safety - all of which have contributed to widespread misconceptions regarding vaccines. These incidents demand the immediate attention of Bangladesh's public health officials (9).
To clarify unfavorable public perceptions against the vaccination, an effective communication campaign engaging community members should be planned and conducted. Furthermore, it is paramount to ensure that accurate information on the COVID-19 vaccine procedure is constantly disseminated via effective media channels, such as the internet, TV news, and social media websites (39). Through these outlets, public health messages emphasizing faith in vaccination safety, efficacy, and benefits can be quite helpful. Public officials and national figures who have received the COVID-19 vaccination might also share their experiences in the media to urge others to become immunized. The authority should expand the number of community-based clinics and vaccination booths for online registration and immunization. With adequate administration, walk-in vaccination programs might be addressed. They can add extra personnel to properly handle the entire process. To combat this deadly disease, authorities must equip and teach their staff and other essential players. Furthermore, extensive coordination among academics, authorities, and societies is required to design a successful COVID-19 immunization program for all individuals (40).
All of these measures should be used by the authority to carry out its policy of broad COVID-19 immunization coverage. While it is challenging to manage misconceptions, it is essential to recognize inaccurate medical statements and circulated myths and work on rather promoting sound scientific facts regarding vaccination.
Effects and recommendations of vaccine hesitancy in Pakistan
Pakistan is also dealing with the rising issue of COVID-19 vaccination reluctance. It is one of the countries with the lowest vaccination rates. During these threatening times, COVID-19 vaccine hesitancy remains a significant barrier to Pakistan's public health. People from lower socioeconomic levels are less likely to be vaccinated. Fear of the vaccine's safety and efficacy, potential ill effects, lack of faith in vaccine-development institutions, and concern that the vaccination might cause autism, infertility, autoimmune diseases, and death are all factors impacting public adoption of the COVID-19 vaccine. As a result, Pakistan urgently needs to establish a stronger healthcare system to curb viral transmission (33, 41).
To urge people to get vaccinated against COVID-19, the Pakistani media must refrain from broadcasting anything that fuels conspiracy theories about the virus. An online telehealth programs should be established so that the any member of the public may direct their queries and concerns to specialists, who can reply and comment on vaccination safety. In the country, mass awareness campaigns should be conducted using various social media apps, TV channels, radio programs and newspapers as well. The priority should be placed on the importance of immunization by noting prior vaccine achievements (41). Consideration should be given to the provision of financial incentives for vaccination. Religious conspiracies and erroneous beliefs about vaccines containing pig or monkey derivatives should be reduced by incorporating the religious experts and have them educate the general public about the necessity of immunization in accordance with Islamic Sharia law (23).
The major cause of vaccine refusal in this country is the lack of scientific understanding about vaccination among the general people; hence, the WHO must step up its duties to effectively address public inquiries and provide the most up-to-date scientific information about the available vaccines.
Limitations
This paper has several limitations. Given the nature of narrative reviews, the articles included in our study were not systematically reviewed, hence there exists an area for selection bias. Moreover, articles in the English language were only included which may have prevented us from accessing literature in other native languages across South Asia. In addition, conference proceedings and other databases such as Scopus were not included in our search which limited our final results. Our review only included cross-sectional studies that were survey-based while other studies including ones that analyze threads on social media platforms may have provided more insights since the use of such platforms increased during the pandemic. Also, qualitative studies may have given more in-depth descriptions of individual experiences. Collectively, these different factors could potentially add bias, and varying views may reflect different findings suggesting the diversity of opinions and conclusions.
Conclusion
With the rise in COVID-19 cases amidst new variants on a global scale, there is a strong need to tackle socio-economic challenges to vaccine uptake in developing countries, including vaccine hesitancy in the general population. Lower-and-middle income countries such as Afghanistan, Bangladesh, India, and Pakistan have shown the unique challenges to vaccinations along with lessons on successful implementation of cost-effective strategies in these regions. Further research is warranted on the role of vaccine misinformation and recommendations for unified health governance on this crucial matter.
Author contributions
FE contributed to the conceptualization of this manuscript, writing of the original draft, and review and editing. RQ contributed to the methodology, analysis of the data, and literature review. UU, PP, KQ, FN, and ZI contributed to the writing of the original draft. NZ contributed to the review and editing of the original draft. All authors contributed to the article and approved the submitted version.
Funding
This study received funding in part from Al Jalila Foundation in addition to a Pfizer Independent Medical Education Grant (Agreement No. 67504787). The funders were not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Acknowledgments
The authors would like to thank the College of Medicine at Mohammed Bin Rashid University of Medicine and Health Sciences for their support and mentorship in promoting active research on COVID-19 vaccine hesitancy. This work was partly supported by the Al Jalila Foundation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Harris KM, Maurer J, Kellermann AL. Influenza vaccine — safe, effective, and mistrusted. N Engl J Med. (2010) 363:2183–5. doi: 10.1056/NEJMp1012333
2. Vetter V, Denizer G, Friedland LR, Krishnan J, Shapiro M. Understanding modern-day vaccines: what you need to know. Ann Med. (2018) 50:110–20. doi: 10.1080/07853890.2017.1407035
3. Fridman A, Gershon R, Gneezy A. COVID-19 and vaccine hesitancy: a longitudinal study. PLoS ONE. (2021) 16:e0250123. doi: 10.1371/journal.pone.0250123
4. The Lancet Child & Adolescent Health. Vaccine hesitancy: a generation at risk. Lancet Child Adolesc Health. (2019) 3:281. doi: 10.1016/S2352-4642(19)30092-6
5. Hawlader MDH, Rahman ML, Nazir A, Ara T, Haque MM, Saha S, et al. COVID-19 vaccine acceptance in South Asia: a multi-country study. Int J Infect Dis. (2022) 114:1–10. doi: 10.1016/j.ijid.2021.09.056
6. Marzo RR, Sami W, Alam MZ, Acharya S, Jermsittiparsert K, Songwathana K, et al. Hesitancy in COVID-19 vaccine uptake and its associated factors among the general adult population: a cross-sectional study in six Southeast Asian countries. Trop Med Health. (2022) 50:4. doi: 10.1186/s41182-021-00393-1
7. COVID-19 | SAARC Region. (2022). Available online at: http://www.covid19-sdmc.org/ (accessed July 1, 2022).
8. Nemat A, Bahez A, Salih M, Raufi N, Noor NAS, Essar MY, et al. Public willingness and hesitancy to take the COVID-19 vaccine in Afghanistan. Am J Trop Med Hyg. (2021) 105:713–7. doi: 10.4269/ajtmh.21-0231
9. Patwary MM, Bardhan M, Disha AS, Hasan M, Haque MdZ, Sultana R, et al. Determinants of COVID-19 vaccine acceptance among the adult population of Bangladesh using the health belief model and the theory of planned behavior model. Vaccines. (2021) 9:1393. doi: 10.3390/vaccines9121393
10. Alam ABMM, Azim Majumder MA, Haque M, Ashraf F, Khondoker MU, Mashreky SR, et al. Disproportionate COVID-19 vaccine acceptance rate among healthcare professionals on the eve of nationwide vaccine distribution in Bangladesh. Expert Rev Vaccines. (2021) 20:1167–75. doi: 10.1080/14760584.2021.1951248
11. Hossain ME, Islam MS, Ghose TK, Jahan H, Chakrobortty S, Hossen MS, et al. COVID-19 vaccine acceptability among public university students in Bangladesh: Highlighting knowledge, perceptions, and attitude. Human Vacc Immunother. (2021) 17:5089–98. doi: 10.1080/21645515.2021.2010426
12. Ali M, Proma TS, Tasnim Z, Islam MdA, Urmi TA, Ahmed S, et al. Parental COVID-19 vaccine hesitancy for children with neurodevelopmental disorders: a cross-sectional survey. Trop Med Health. (2022) 50:24. doi: 10.1186/s41182-022-00415-6
13. Ali M, Ahmed S, Bonna AS, Sarkar A, Islam MA, Urmi TA, et al. Parental coronavirus disease vaccine hesitancy for children in Bangladesh: a cross-sectional study. F1000Res. (2022) 11:90. doi: 10.12688/f1000research.76181.1
14. Kumar R, Bairwa M, Beniwal K, Kant R. COVID-19 vaccine acceptability, determinants of potential vaccination, and hesitancy in public: a call for effective health communication. J Educ Health Promot. (2021) 10:392. doi: 10.4103/jehp.jehp_327_21
15. Jain J, Saurabh S, Kumar P, Verma MK, Goel AD, Gupta MK, et al. COVID-19 vaccine hesitancy among medical students in India. Epidemiol Infect. (2021) 149:e132. doi: 10.1017/S0950268821001205
16. Joshi A, Sridhar M, Tenneti VJD, Devi V, K T S, Nallaperumal AB. COVID-19 vaccine hesitancy in healthcare workers amidst the second wave of the pandemic in India: A single centre study. Cureus. (2021) 13:e17370. doi: 10.7759/cureus.17370
17. Jacob J, Stephen S, Issac A, Krishnan N, Radhakrishnan RV, R VV, et al. Determinants of Willingness for COVID-19 vaccine: Implications for enhancing the proportion of vaccination among indians. Cureus. (2021) 13:e15271. doi: 10.7759/cureus.15271
18. Mathur M, Verma A, Mathur N, Singhal Y, Dixit M, Patyal A, et al. Predictors and Perceptions of Healthcare workers regarding vaccines safety in the initial phase of covid-19 vaccination drive in western part of India: A regression analysis. Cureus. (2022) 14:e21267. doi: 10.7759/cureus.21267
19. Singh AK, Kumari R, Singh S, Kandpal SD, Kaushik A. The dilemma of COVID-19 vaccination among Health Care Workers (HCWs) of Uttar Pradesh. Indian J Community Health. (2021) 33:319–24. doi: 10.47203/IJCH.2021.v33i02.017
20. Danabal KGM, Magesh SS, Saravanan S, Gopichandran V. Attitude towards COVID 19 vaccines and vaccine hesitancy in urban and rural communities in Tamil Nadu, India – a community based survey. BMC Health Serv Res. (2021) 21:994. doi: 10.1186/s12913-021-07037-4
21. Ekstrand ML, Heylen E, Gandhi M, Steward WT, Pereira M, Srinivasan K. COVID-19 vaccine hesitancy among PLWH in South India: implications for vaccination campaigns. J Acq Immune Def Syndromes. (2021) 88:421–5. doi: 10.1097/QAI.0000000000002803
22. Malik A, Malik J, Ishaq U. Acceptance of COVID-19 vaccine in Pakistan among health care workers. PLoS ONE. (2021) 16:e0257237. doi: 10.1371/journal.pone.0257237
23. Tahir MJ, Saqlain M, Tariq W, Waheed S, Tan SHS, Nasir SI, et al. Population preferences and attitudes towards COVID-19 vaccination: a cross-sectional study from Pakistan. BMC Public Health. (2021) 21:1759. doi: 10.1186/s12889-021-11814-5
24. Yasmin F, Asghar W, Babar MS, Khan H, Ahmad S, Hameed Z, et al. Acceptance rates and beliefs toward COVID-19 vaccination among the general population of Pakistan: a cross-sectional survey. Am J Trop Med Hyg. (2021) 105:1230–9. doi: 10.4269/ajtmh.21-0297
25. Zakar R, Momina A, Shahzad S, Hayee M, Shahzad R, Zakar MZ. COVID-19 vaccination hesitancy or acceptance and its associated factors: findings from post-vaccination cross-sectional survey from Punjab Pakistan. Int J Environ Res Public Health. (2022) 19:1305. doi: 10.3390/ijerph19031305
26. Khattak FA, Rehman K, Shahzad M, Arif N, Ullah N, Kibria Z, et al. Prevalence of Parental refusal rate and its associated factors in routine immunization by using WHO Vaccine Hesitancy tool: A Cross sectional study at district Bannu, KP, Pakistan. Int J Infect Dis. (2021) 104:117–24. doi: 10.1016/j.ijid.2020.12.029
27. Coronavirus (COVID-19) Vaccinations - Our World in Data. Available from: https://ourworldindata.org/covid-vaccinations (accessed July 3, 2022).
28. Feleszko W, Lewulis P, Czarnecki A, Waszkiewicz P. Flattening the curve of COVID-19 vaccine rejection—An International Overview. Vaccines. (2021) 9:44. doi: 10.3390/vaccines9010044
29. Gallup Pakistan,. Coronavirus Attitude Tracker Survey Pakistan. (2020). Available from: https://gallup.com.pk/wp/wp-content/uploads/2021/01/Gallup-Covid-Opinion-Tracker-Wave-9-pdf.pdf (accessed July 3, 2022).
30. Information Regarding COVID-19 Vaccine. Available from: https://www.mohfw.gov.in/covid_vaccination/vaccination/index.html (accessed July 3, 2022).
31. Paterson P, Meurice F, Stanberry LR, Glismann S, Rosenthal SL, Larson HJ. Vaccine hesitancy and healthcare providers. Vaccine. (2016) 34:6700–6. doi: 10.1016/j.vaccine.2016.10.042
32. Abedin M, Islam MA, Rahman FN, Reza HM, Hossain MZ, Hossain MA, et al. Willingness to vaccinate against COVID-19 among Bangladeshi adults: Understanding the strategies to optimize vaccination coverage. PLoS ONE. (2021) 16:e0250495. doi: 10.1371/journal.pone.0250495
33. Mehmood Q, Ullah I, Hasan MM, Kazmi SK, Ahmadi A, Lucero-Prisno DE. COVID-19 vaccine hesitancy: Pakistan struggles to vaccinate its way out of the pandemic. Ther Adv Vacc Immunother. (2022) 10:251513552210776. doi: 10.1177/25151355221077658
34. Sarkar MA, Ozair A, Singh KK, Subash NR, Bardhan M, Khulbe Y. SARS-CoV-2 vaccination in India: considerations of hesitancy and bioethics in global health. Ann Global Health. (2021) 87:124. doi: 10.5334/aogh.3530
35. Wardak MF, Rahimi A, Ahmadi A, Madadi S, Arif S, Nikbin AM, et al. COVID-19 vaccination efforts: is Afghanistan prepared? Am J Trop Med Hyg. (2021) 105:1137–40. doi: 10.4269/ajtmh.21-0448
36. Hossain MS, Islam MS, Pardhan S, Banik R, Ahmed A, Islam MZ, et al. Beliefs, barriers and hesitancy towards the COVID-19 vaccine among Bangladeshi residents: findings from a cross-sectional study. PLoS ONE. (2022) 17:e0269944. doi: 10.1371/journal.pone.0269944
37. Chandani S, Jani D, Sahu PK, Kataria U, Suryawanshi S, Khubchandani J, et al. COVID-19 vaccination hesitancy in India: state of the nation and priorities for research. Brain Behav Immunity Health. (2021) 18:100375. doi: 10.1016/j.bbih.2021.100375
38. Rosen B, Waitzberg R, Israeli A. Israel's rapid rollout of vaccinations for COVID-19. Isr J Health Policy Res. (2021) 10:6. doi: 10.1186/s13584-021-00440-6
39. Ahmad Rizal AR, Nordin SM, Ahmad WFW, Ahmad Khiri MJ, Hussin SH. How does social media influence people to get vaccinated? The elaboration likelihood model of a person's attitude and intention to get COVID-19 vaccines. Int J Environ Res Public Health. (2022) 19:2378. doi: 10.3390/ijerph19042378
40. OECD. Enhancing Public Trust in COVID-19 Vaccination: The Role of Governments. (2021). Available from: https://www.oecd.org/coronavirus/policy-responses/enhancing-public-trust-in-covid-19-vaccination-the-role-of-governments-eae0ec5a/ (accessed June 29, 2022).
Keywords: COVID-19, vaccine hesitancy, public perspectives, public opinion, South Asia
Citation: Ennab F, Qasba RK, Uday U, Priya P, Qamar K, Nawaz FA, Islam Z and Zary N (2022) COVID-19 vaccine hesitancy: A narrative review of four South Asian countries. Front. Public Health 10:997884. doi: 10.3389/fpubh.2022.997884
Received: 19 July 2022; Accepted: 16 September 2022;
Published: 10 October 2022.
Edited by:
Anat Gesser-Edelsburg, University of Haifa, IsraelReviewed by:
Atta Ur Rehman, Margalla Institute of Health Sciences, PakistanAhmed Hafez Mousa, Batterjee Medical College, Saudi Arabia
Afnan Jobran, Al-Quds University, Palestine
Copyright © 2022 Ennab, Qasba, Uday, Priya, Qamar, Nawaz, Islam and Zary. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Farah Ennab, RmFyYWguRW5uYWJAYWx1bW5pLm1icnUuYWMuYWU=
 Farah Ennab
Farah Ennab Rakhtan K. Qasba
Rakhtan K. Qasba Utkarsha Uday
Utkarsha Uday Priya Priya
Priya Priya Khulud Qamar4
Khulud Qamar4 Faisal A. Nawaz
Faisal A. Nawaz Zarmina Islam
Zarmina Islam Nabil Zary
Nabil Zary