- 1Department of Medicine, Ziauddin University, Karachi, Pakistan
- 2Kabir Medical College, Gandhara University, Peshawar, Pakistan
- 3Institute of Public Health and Social Science (IPH&SS), Khyber Medical University, Peshawar, Pakistan
- 4Hamad Medical Corporation, Doha, Qatar
With over 500 million confirmed cases and 6.2 million deaths worldwide, the novel coronavirus has highlighted the underlying disparities in healthcare, unpreparedness to deal with a new disease and the need for monitoring and surveillance for a post-infectious syndrome as well as complicated diseases. Initially, children were thought to be spared but reports of a new phenomenon manifesting as Kawasaki-like disease, toxic shock syndrome, and multi-system inflammatory syndrome, which developed after a few weeks of severe COVID-19 infection, emerged in the pediatric population. As the pandemic progressed, increased prevalence of multi-system inflammatory syndrome in children (MIS-C) related to COVID-19 was seen in non-Hispanic blacks, Asians, and Latinos as compared to the white population drawing attention to a possible role of ethnicity and socio-economic disparities. The CDC currently reports that 31% of MIS-C cases were seen in Black Non-Hispanics and 26% in Latinos, who were historically more affected in previous pandemics. Furthermore, MIS-C cases in developing countries showed higher mortality as compared to high-income countries, which points toward the role of social determinants of health and limitations in a low-resource set up in increasing the disease burden of MIS-C, which should be treated as a public health emergency. Our review highlights the role of ethnicity, socio-economic factors, comorbidities, and differences in populations affected by MIS-C in high-income vs. low- and middle-income countries.
Introduction
What started as a mere flu in December 2020, the Coronavirus (COVID-19) pandemic caused by the SARS-CoV-2 virus resulted in over 6.2 million deaths from nearly 500 million confirmed cases (1). Early reports showed that children were mostly spared from severe forms of illnesses associated with COVID-19, with only 2% of cases diagnosed in the pediatric population up till February 2020 (2). Epidemiological studies further suggested that compared with adult patients' the clinical manifestations of COVID-19 in children were mostly mild and showed minimum mortality (3). However, this judgment was revised in April 2020 when several countries in Europe and North America reported cases of young patients with “Multi-System Inflammatory Syndrome in Children (MIS-C)” associated with SARS-CoV-2 also known as Kawasaki-like syndrome and toxic shock syndrome (4). Reports of clusters of children and adolescents affected by MIS-C admitted to ICU or requiring mechanical ventilation emerged from the UK, Italy, and New York, followed by other parts of the US (5, 6). It was further found that Black and Hispanic children formed an overwhelming majority (66%) of those who developed the life-threatening MIS-C (7).
Although rare, this condition needs extensive surveillance in areas with a high burden of COVID-19, which have shown consistent patterns of racial/ethnic differences (8, 9). The exact role of race and ethnicity on clinical outcomes of COVID-19 is unknown, but given the general consensus, there is a greater need to examine the factors behind disproportionate levels of adverse clinical outcomes (10). Particularly in pediatric populations where reports of severe disease have been limited owing to incomplete public health data worldwide (11). The current studies lack data on race and ethnicity-specific presentations of the syndrome, the mechanism of genetic predisposition to MIS-C, and further research into its' worldwide distribution, given that it should be treated as a public health emergency that requires intensive care and surveillance. Literature regarding disparities in COVID-19 has largely addressed the adult population while the extent of racial and ethnic disparities in children is relatively unknown. While MIS-C initially emerged in the US and Europe, soon after cases were reported in the developing countries which was a source of immediate concern and attention for communities worldwide. It is also imperative to understand the variation in clinical features and severity of this disease in affected countries and to assess the potential role played by social determinants of health. Given the scarcity of data in the current literature, in this review we compare the distribution of MIS-C in High-Income Countries (HICs) and Low-Income Countries (LMICs) and explore the role of social and living conditions, comorbidities, and ethnicity in the development of MIS-C as well as the extent of severe forms of the disease in certain populations.
Case definition
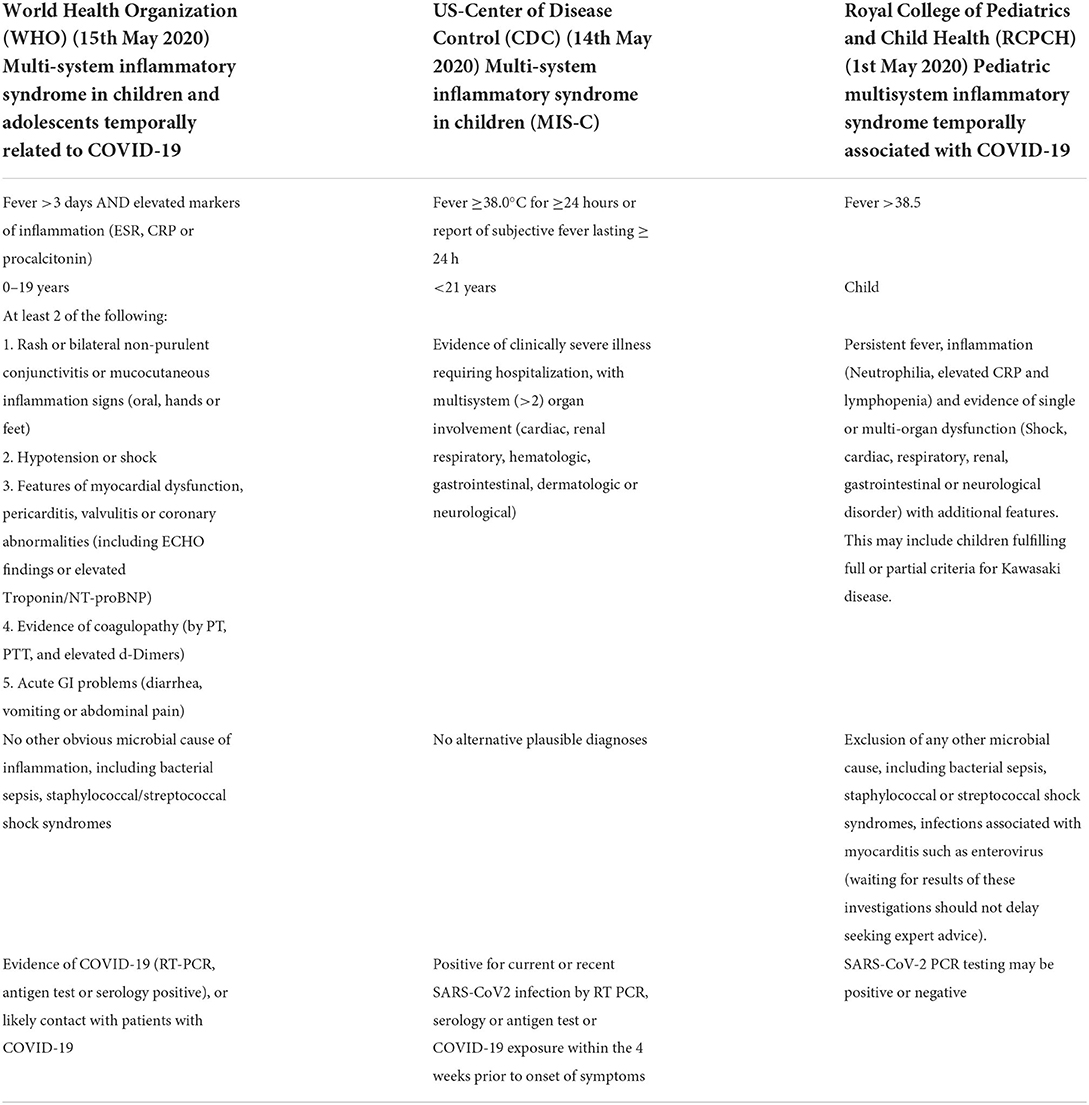
Variously termed as Kawasaki-like disease, pediatric multi system inflammatory syndrome temporally associated with COVIRD-19 (PIMS-TS) or MIS-C, case definitions have been produced by the World Health Organization, US Centers for Disease Control and Prevention and the UK Royal College of pediatrics (Table 1).
Difference between Kawasaki like disease and MIS-C (STING PATHWAY)
In a retrospective observational study from Japan Kawasaki-disease Shock Syndrome (KDSS) and MIS-C were seen to overlap in clinical symptoms however are 2 separate entities. Kawasaki disease is a medium-sized vessel vasculitis usually in children under 5 years of age preceded by fever for at least 5 days and generalized inflammation that involves lymph nodes and particularly the skin and mucous membranes (12). KD progresses to Kawasaki disease shock syndrome (KDSS) when there is a 20% decrease in systolic blood pressure (13). COVID-19 can also develop severe course characterized by acute respiratory distress syndrome (ARDS) with a hyperinflammatory response (14). Multi-system inflammatory response in COVID-19 is characterized by systemic inflammation involving multiple organs such as cardiac, renal and gastrointestinal. Entry of a foreign antigen in the body causes activation of simulator of interferon genes (STING) which leads to release of inflammatory cytokines, predominantly type 1 IFN. The STING pathway is shown to be activated in KD brining about an inflammatory response that consists of neutrophils, macrophages and cytotoxic T cells which are seen on the histology of coronary arteries affected in KD (12). It has been reported that type 1 IFNs drive the immune response in SARS-CoV-2 (15). It was when Domizio et al. (16) identified a H-151 STING inhibitor that served as a therapeutic agent in reducing severe inflammation in SARS-CoV-2 an important role of STING pathway in COVID-19 was found. CT angiogram can also play an important role in young patients with symptoms of KD overlapping with COVID-19 to identify coronary aneurysms in a timely manner so that the fatal risk of thromboses and lumen narrowing can be diagnosed initially.
Methods
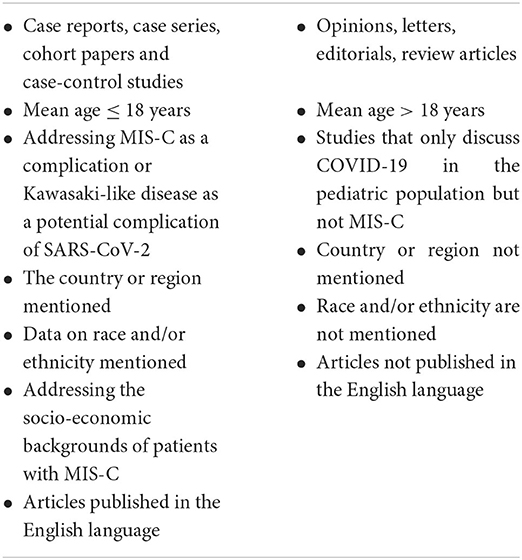
In this narrative review, a thorough literature search of all peer-reviewed articles published between 31st December' 2019 to 1st April' 2022 was undertaken using keywords “multi-system inflammatory syndrome”, “COVID-19”, “SARS COV-2”, “coronavirus”, “children”, “infant”, “Kawasaki/Kawasaki-like disease”, “pediatrics”, “pediatric multi-system inflammatory syndrome” and any other relevant keywords and supplementary concepts were identified. Reference lists of the identified studies were also screened to look for similar studies. Multiple electronic databases were searched, which included PubMed, Google Scholar, Elsevier, Wiley Online Library, ScienceDirect, and WHO COVID-19 database. To increase the scope of our search, pre-prints from Medxriv were also included. An inclusion and exclusion criteria were pre-decided to guide our search, which is as follows:
MIS-C and ethnicities
Previous studies published on COVID-19 in adults have highlighted racial/ethnic and socio-economic disparities and race discrimination continued in the provision of vaccines and treatments (17). A policy statement by American Academy of Pediatrics highlighted that the impact of racism starts from birth disparities which give rise to mental health problems and chronic stress conditions such as cortisol that predisposes children and adolescents to chronic disease (18). A study that enrolled 640 COVID-19 patients in the UK concluded that compared to white members, black individuals were at a 4 times higher risk of COVID-19, and it was twice higher in Asian and other non-white persons (19). However, there is limited data relevant to the pediatric population and if a certain ethnic group is at a higher risk of developing COVID-19, particularly MIS-C. Currently, the CDC website reports 7,880 MIS-C cases, 31% of which are Black Non-Hispanic and 26% are Hispanic/Latino, who are also disproportionately affected by COVID-19 (20). As seen in Kawasaki disease, which has shown a predominance in genetically susceptible children, similar patterns have been seen in MIS-C, in which higher prevalence was reported in Black, Hispanic, and South Asian populations (4, 21, 22). Dufort et al. reported a case series of 99 pediatric patients with confirmed and suspected MIS-C who belonged to New York. 31 out of 78 (40%) patients were black, and 31 out of 85 (36%) were Hispanic, compared to 29 out of 78 (37%) white patients (23). Adult deaths in New York showed a similar pattern. Compared to 22% African Americans and 29% Hispanic-Latinos in the overall population, the two groups accounted for 28 and 34% of deaths, respectively (24). Another study from New York reported that 45 and 39% of MIS-C patients were Hispanic/Latino and Black, respectively, compared to 9% White, 3% Asian, and 3% other ethnicities (25). In another cohort from NYC, among 223 patients meeting the MIS-C criteria, race/ethnicity data was available for 184 patients. 34.4% (75 patients) were Black, given the overall population of Black children 22.2 and 19.9% of patients under 20 years hospitalized due to COVID (26). From April to June 2020 the incidence of MIS-C in various states of America was 9.26, 8.92, and 2.94 times higher in Black, Hispanic or Latino, and Asians compared to white patients (27). Black and Hispanic populations also have the lowest rates of vaccination, and parents to date show hesitancy to vaccinate their children against COVID-19. Only 21% of children between 12 and 15 years were vaccinated, and 32% of those between 16 and 17 years of age among the racial/ethnic groups (28).
The racial disparities were not only confined to the United States of America (USA). Toubiana et al. reported 21 confirmed cases of Kawasaki Disease—like/MISC in the Paris region in France, where children of color were overrepresented, similar to what we saw in the USA. Twelve (57%) children had at least one parent from a sub-Saharan African or Caribbean Island, and 3 (14%) children were of Asian (Srilanka/China) descent (29). A study from the UK reported 15 cases of PIMS-TS (Pediatric Inflammatory Multisystem Syndrome-temporally associated with SARS-CoV-2) associated with COVID-19, and all children belonged to African/Afro-Caribbean, South Asian, mixed, or minority ethnic groups, which is relatively large given that only 3.3% of children are Black and 10% percent are Asian. In addition, these children showed severe cardiac symptoms, and 67% were admitted to the ICU (30). Another cluster of 8 children from the UK was reported with hyperinflammatory shock syndrome; all patients were Afro-Caribbean, Asian, and Middle Eastern, and all of them were admitted to the ICU and required mechanical ventilation, one child died, and the rest were discharged on surveillance (31). In Latin America, MISC was more widely reported compared to other developing countries, perhaps due to differing political opinions regarding the to approach the pandemic and lockdown policies making children more exposed to the infection during daily activities, which further support the point of view that children of Hispanic-Latino ethnicity are at a higher risk of developing MIS-C (32–34).
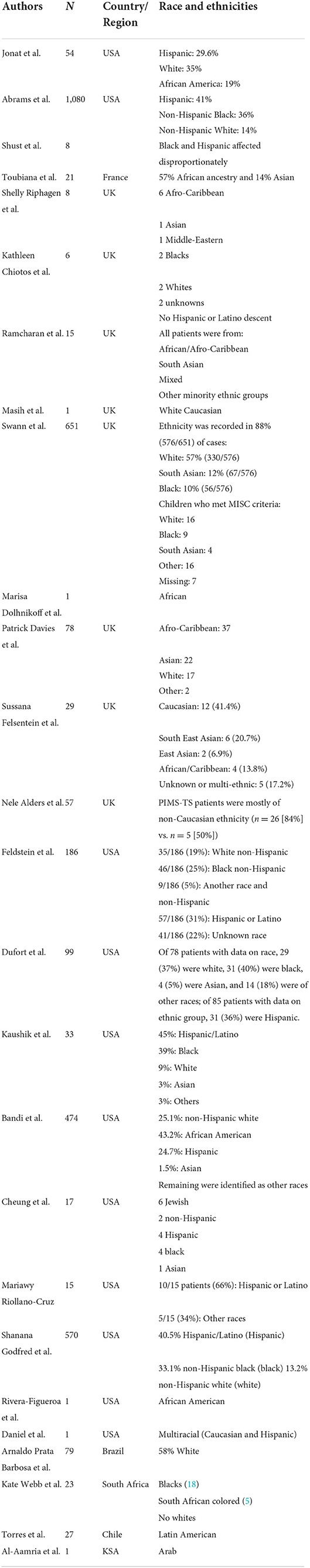
Table 2 summarizes the race and ethnicity findings of MIS-C.
MIS-C and comorbidities
The most common underlying condition in children with MIS-C was obesity (21, 23, 25, 26, 32, 35–38). The second most common comorbid highlighted in these cohorts was asthma (4, 22, 39–43). Hypothyroidism, non-alcoholic fatty liver disease, respiratory illness preceding 4 weeks of hospitalization, and glucose-6-phosphate-dehydrogenase deficiency were also seen in some cases (43, 44). Other comorbidities seen in severe COVID-19 cases were neurological problems, immunocompromised, premature births, and hematological problems, but only obesity was associated with MIS-C (40). Similar findings were seen in adult patients, where Black patients had higher prevalence of obesity, diabetes, hypertension, and chronic kidney disease compared to white patients (45). Black ethnicity was shown to be associated with comorbidities in a cohort where African American patients with 3 or more comorbidities formed a higher proportion of overall patients with severe COVID-19 (46). Particularly in the US, obesity was associated with factors such as age, race, Hispanic origin, and education of the household head which are directly related to ethnicity and one's socio-economic status (47). Furthermore, studies suggest that asthma is related to socio-economic factors, which are directly linked with ethnicity as well, such as environmental exposures, access to healthcare, stress, and psychological/cultural factors that have been associated with increased asthma morbidity (48).
MIS-C in the developing world
Compared to High-Income Countries (HIC's), studies from the developing world have reported higher rates of hospitalization and deaths from MIS-C (49). The first case to be reported in South Asia was from Pakistan, where a cluster of 8 children reported confirmed MISC at a university hospital in the city of Lahore, all of whom showed cardiovascular involvement, and one died due to myocardial infarction and subsequent organ failure (50). Involvement of coronary artery disease and the overall infectivity rate in Pakistan in children younger than 20 years was higher (>10%) compared to the rest of the world (50, 51). In India, neonates and infants were affected by MIS-C with various manifestations ranging from in-utero exposure to SARS-CoV-2 in a premature infant (52), fatal respiratory distress syndrome with hypotensive shock and meningoencephalitis (53), cavitary lung lesions (54), persistent neutropenia (55) to dermatological involvement (56). In Iran, a retrospective study that covered 3 hospitals in regions most severely hit by the pandemic reported 45 confirmed cases of MISC and a mortality of 11% (n = 5) (57). Another case report from Iran showed a 5-year-old girl with Kawasaki disease like inflammatory syndrome with severe symptoms consistent with MISC that improved with standard treatment consisting of IVIG and anti-biotics (58).
At the time of writing this review, studies from Low- and Middle-Income Countries (LMIC's) showed a lesser number of MISC patients compared to HICs but a higher proportion of deaths (49). This is alarming due to a number of factors. Firstly, many physicians working on the front lines were stretched to not allocate enough time for clinical research and data collection. Secondly, lack of testing capacity overwhelmed in-patient facilities, and limited pediatric ICU and ventilator resources can cause many patients to return undiagnosed. Thirdly, children make up a large part of the population in LMICs compared to HICs and have more exposure to risk factors of lower respiratory diseases such as air pollution, incomplete immunization, malnutrition, greater prevalence of infectious diseases like TB and HIV, and overcrowded conditions with water and sanitation problems (59). Therefore, the number of cases of MISC can be largely underestimated.
It is essential to consider practical prevention strategies according to the limitations of populations in low-income countries. In communities with widespread transmission mass awareness and advocacy campaigns regarding the spread of the disease can be carried out with focus on limiting healthy children from visiting healthcare facilities, regular well-child visits for newborns and infants for preventive care and timely vaccinations, local availability of telephone triage system, immediate closure of schools and public places or at least restricting entrance for children as well as nutritional education for parents as diet plays a huge role in the development of immune system (60).
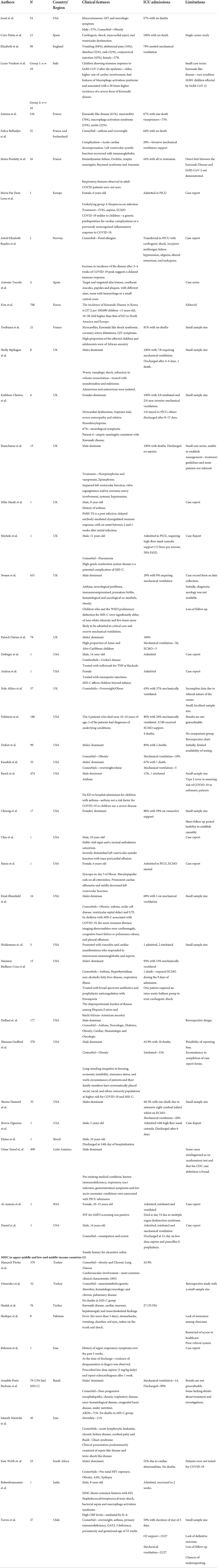
Table 3 summarizes findings from High-Income and Low-and Middle-Income countries based on the recent World Bank Classification (61).
MIS-C and socio-economic factors
Given the ethnically diverse nature of the aforementioned HICs, the high number of cases suggests a relationship between socio-economic factors and MIS-C. Higher COVID-19 infection rates have been associated with lack of insurance, overcrowded neighborhoods where social distancing is ineffective, and high exposure jobs within the service industry, transport, and healthcare sectors which are dominated by people of color (62). Especially Hispanic families who mostly live in metropolitan areas in apartment buildings, bigger families, and mainly use public transport (63). This can lead to adults exposing more children to coronavirus at home and serve as a possible explanation for the increased number of COVID-19 cases progressing to MIS-C. Discrimination within the healthcare system, limited healthcare access because of lack of transportation to take their children to the hospital on time, cultural and linguistic barriers, inability to take time off work, possible distrust in the system due to inherent biases and fears of deportation for symptomatic adults also play a role in acquiring timely access to healthcare (64, 65). A retrospective case-control study in Massachusetts conducted on 44 patients with MIS-C (Hispanic = 44%, Black = 26%) concluded that a higher social vulnerability index (SVI), lower socio-economic status (SES), Hispanic ethnicity, and Black race were independently associated with developing MIS-C (66). Mitigating social determinants of health is important as future winter waves of SARS-CoV-2 are anticipated. Improved housing decreases in overcrowding, and improved nutrition has for years proven to be effective interventions for controlling respiratory infections such as tuberculosis (67). Factors such as reducing smoke exposure, financial support to low-income households, improving access to healthcare, free and accessible testing, and provision of shelter to those in need have great potential to improve future pandemic morbidity and mortality (68).
Conclusion
This review highlights the need for high-quality data on ethnicities and socio-economic positions of patients affected by MISC, especially in regions severely impacted by COVID-19. Social determinants of health should be routinely considered in clinical assessments the same way as age and sex, as they can play an important role by aiding in the creation of tailor-made policies for risk mitigation. It is important to note the equitable distribution of resources, such as critical care and hospital beds for pediatric patients with MISC, is essential for reducing mortality because most of the resources were allocated to adult COVID-19 patients. In LMICs, where lockdown policies put vulnerable populations such as the elderly and children at a higher risk of exposure as most people live in overcrowded conditions, there should be strict surveillance. Good standard healthcare is not free in most LMICs, hospitals funded by the government are found to be stretched, and the cost associated with prolonged hospital admissions and critical care can be a factor that holds back families from seeking hospital care until an emergency arises. In addition to social determinants of health, comorbidities were another driving factor leading to the overrepresentation of ethnic minorities getting affected by MISC. Further genetic studies are also needed to warrant the role of genetic susceptibility to MISC in children. This review can form the basis of larger cohort studies investigating the role of ethnicity and social determinants of health in developing MISC that pose a serious public health concern. Our review also elucidates the importance of cross-cultural prospective cohorts to correctly assess the wide clinical variability of this syndrome and help us solidify common socio-economic and racial/ethnic factors driving the severity of MIS-C. Including data from LMICs helped in gaining a new perspective for the occurrence of this syndrome as we saw how delays in attaining appropriate treatment, unavailability of critical care and a lack of timely diagnosis led to severe forms of disease. In conclusion our review identified similar patterns of racial findings, socio-economic strata and limitations of health set ups across different countries of the same economic classification which can aid policy makers in making effective strategies to mitigate the development of MIS-C therefore further studies in the same area should be focused on.
Author contributions
ZA conceived the idea, developed the methodology for the study, and wrote the first draft. ZA, KS, FB, OS, and MS were equally involved in literature review, synthesizing results from the literature, and writing and editing of the manuscript. AW contributed to editing. IU and AN contributed in the overall structure and editing of the manuscript. All authors read, critically analyzed, edited, and approved the final manuscript.
Conflict of interest
Author AN is employed by Hamad Medical Corporation.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. WHO. WHO Coronavirus (COVID-19) Dashboard. Geneva: WHO (2022). Available online at: https://covid19.who.int/ (accessed May 19, 2022).
2. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72,314 cases from the Chinese center for disease control and prevention. JAMA. (2020) 323:1239–42. doi: 10.1001/jama.2020.2648
3. Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, et al. Epidemiology of COVID-19 among children in China. Pediatrics. (2020) 145:e0702. doi: 10.1542/peds.2020-0702
4. Hoste L, Van Paemel R, Haerynck F. Multisystem inflammatory syndrome in children related to COVID-19: a systematic review. Eur J Pediatrics. (2021) 180:2019–34. doi: 10.1007/s00431-021-03993-5
5. WHO. Multi-System Inflammatory Syndrome in Children and Adolescents Temporally Related to COVID-19. Geneva: WHO (2020). Available online at: https://www.who.int/news-room/commentaries/detail/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19 (accessed May 20, 2022).
6. Nakra NA, Blumberg DA, Herrera-Guerra A, Lakshminrusimha S. Multi-system inflammatory syndrome in children (MIS-C) following SARS-CoV-2 infection: review of clinical presentation, hypothetical pathogenesis, and proposed management. Children. (2020) 7:69. doi: 10.3390/children7070069
7. Dennis-Heyward EA. Disparities in susceptibility to multisystem inflammatory syndrome in children. JAMA Pediatrics. (2021) 175:892–3. doi: 10.1001/jamapediatrics.2021.1115
8. Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. (2020) 323:2466–7. doi: 10.1001/jama.2020.8598
10. Pan D, Sze S, Minhas JS, Bangash MN, Pareek N, Divall P, et al. The impact of ethnicity on clinical outcomes in COVID-19: a systematic review. Eur Clin Med. (2020) 23:100404. doi: 10.1016/j.eclinm.2020.100404
11. DeBiasi RL, Song X, Delaney M, Bell M, Smith K, Pershad J, et al. Severe coronavirus disease-2019 in children and young adults in the Washington, DC, metropolitan region. J Pediatrics. (2020) 223:199–203.e1. doi: 10.1016/j.jpeds.2020.05.007
12. Fang Y, Aravamudan VM, Sridharan GK, Mehta KK, Sekhar R, Senguttuvan NB, et al. Kawasaki like illness due to COVID-19: a review of the literature. J Infect Dev Ctries. (2021) 15:630–8. doi: 10.3855/jidc.14185
13. Zhang MM, Shi L, Li XH, Lin Y, Liu Y. Clinical analysis of kawasaki disease shock syndrome. Chin Med J. (2017) 130:2891–2. doi: 10.4103/0366-6999.219151
14. Vogel TP, Top KA, Karatzios C, Hilmers DC, Tapia LI, Moceri P, et al. Multisystem inflammatory syndrome in children and adults (MIS-C/A): case definition and guidelines for data collection, analysis, and presentation of immunization safety data. Vaccine. (2021) 39:3037–49. doi: 10.1016/j.vaccine.2021.01.054
15. Li H, Zhou F, Zhang L. STING a critical contributor to SARS-CoV-2 immunopathology. Sig Transduct Target Ther. (2022) 7:106. doi: 10.1038/s41392-022-00967-3
16. Domizio JD, Gulen MF, Saidoune F, Thacker VV, Yatim A, Sharma K, et al. The cGAS–STING pathway drives type I IFN immunopathology in COVID-19. Nature. (2022) 603:145–51. doi: 10.1038/s41586-022-04421-w
17. Kasapçopur Ö. Anti-racist pediatric research against discrimination in science with diversity, equity, and inclusion. Turk Arch Pediatrics. (2022) 57:116–7. doi: 10.5152/TurkArchPediatr.2022.180222
18. Trent M, Dooley DG, Dougé J, Cavanaugh RM, Lacroix AE, Fanburg J, et al. The impact of racism on child and adolescent health. Pediatrics. (2019) 144:e20191765. doi: 10.1542/peds.2019-1765
19. Lassale C, Gaye B, Hamer M, Gale CR, Batty GD. Ethnic disparities in hospitalisation for COVID-19 in England: The role of socio-economic factors, mental health, and inflammatory and pro-inflammatory factors in a community-based cohort study. Brain Behav Immun. (2020) 88:44–9. doi: 10.1016/j.bbi.2020.05.074
20. CDC. Health Department-Reported Cases of Multisystem Inflammatory Syndrome in Children (MIS-C) in the United States. Atlanta, GA: CDC (2022). Available online at: https://covid.cdc.gov/covid-data-tracker/#mis-national-surveillance
21. Esposito S, Principi N. Multisystem inflammatory syndrome in children related to SARS-CoV-2. Pediatric Drugs. (2021) 23:119–29. doi: 10.1007/s40272-020-00435-x
22. Toraih EA, Hussein MH, Elshazli RM, Kline A, Munshi R, Sultana N, et al. Multisystem inflammatory syndrome in pediatric COVID-19 patients: a meta-analysis. World J Pediatrics. (2021) 17:141–51. doi: 10.1007/s12519-021-00419-y
23. Dufort EM, Koumans EH, Chow EJ, Rosenthal EM, Muse A, Rowlands J, et al. Multisystem inflammatory syndrome in children in New York State. N Engl J Med. (2020) 383:347–58. doi: 10.1056/NEJMoa2021756
24. Alcendor DJ. Racial disparities-associated COVID-19 mortality among minority populations in the US. J Clin Med. (2020) 9:2442. doi: 10.3390/jcm9082442
25. Kaushik S, Aydin SI, Derespina KR, Bansal PB, Kowalsky S, Trachtman R, et al. Multisystem inflammatory syndrome in children associated with severe acute respiratory syndrome coronavirus 2 infection (MIS-C): a multi-institutional study from New York City. J Pediatrics. (2020) 224:24–9. doi: 10.1016/j.jpeds.2020.06.045
26. Lee EH, Kepler KL, Geevarughese A, Paneth-Pollak R, Dorsinville MS, Ngai S, et al. Race/ethnicity among children with COVID-19: associated multisystem inflammatory syndrome. JAMA Netw Open. (2020) 3:e2030280-e. doi: 10.1001/jamanetworkopen.2020.30280
27. Payne AB, Gilani Z, Godfred-Cato S, Belay ED, Feldstein LR, Patel MM, et al. Incidence of multisystem inflammatory syndrome in children among US persons infected with SARS-CoV-2. JAMA Netw Open. (2021) 4:e2116420-e. doi: 10.1001/jamanetworkopen.2021.16420
28. Martin AA, Harris CE, Ang JY. RE racial and ethnic disparities in multisystem inflammatory syndrome in children. Pediatrics. (2021) 148:e053907A. doi: 10.1542/peds.2021-053907A
29. Toubiana J, Poirault C, Corsia A, Bajolle F, Fourgeaud J, Angoulvant F, et al. Kawasaki-like multi-system inflammatory syndrome in children during the covid-19 pandemic in Paris, France: prospective observational study. BMJ. (2020) 369:m2094. doi: 10.1136/bmj.m2094
30. Ramcharan T, Nolan O, Lai CY, Prabhu N, Krishnamurthy R, Richter AG, et al. Paediatric inflammatory multisystem syndrome: temporally associated with SARS-CoV-2 (PIMS-TS): cardiac features, management and short-term outcomes at a UK tertiary paediatric hospital. Pediatric Cardiol. (2020) 41:1391–401. doi: 10.1007/s00246-020-02391-2
31. Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. (2020) 395:1607–8. doi: 10.1016/S0140-6736(20)31094-1
32. Torres JP, Izquierdo G, Acuña M, Pavez D, Reyes F, Fritis A, et al. Multisystem inflammatory syndrome in children (MIS-C): report of the clinical and epidemiological characteristics of cases in Santiago de Chile during the SARS-CoV-2 pandemic. Int J Infect Dis. (2020) 100:75–81. doi: 10.1016/j.ijid.2020.08.062
33. Matsuda EM, Santos SAD, Castejon MJ, Ahagon CM, Campos IB, Brígido LFM. COVID-19 in children: a case report of Multisystem Inflammatory Syndrome (MIS-C) in São Paulo, Brazil. Brazil J Infect Dis Off Publ Brazil Soc Infect Dis. (2020) 24:580–2. doi: 10.1016/j.bjid.2020.09.002
34. Antúnez-Montes OY, Escamilla MI, Figueroa-Uribe AF, Arteaga-Menchaca E, Lavariega-Saráchaga M, Salcedo-Lozada P, et al. COVID-19 and multisystem inflammatory syndrome in latin American children: a multinational study. Pediatric Infect Dis J. (2021) 40:e1–6. doi: 10.1097/INF.0000000000002949
35. Jonat B, Gorelik M, Boneparth A, Geneslaw AS, Zachariah P, Shah A, et al. Multisystem inflammatory syndrome in children associated with coronavirus disease 2019 in a children's hospital in New York City: patient characteristics and an institutional protocol for evaluation, management, and follow-up. Pediatrics Crit Care Med. (2021) 22:e178–e91. doi: 10.1097/PCC.0000000000002598
36. Abrams JY, Oster ME, Godfred-Cato SE, Bryant B, Datta SD, Campbell AP, et al. Factors linked to severe outcomes in multi-system inflammatory syndrome in children (MIS-C) in the USA: a retrospective surveillance study. Lancet Child Adolesc Health. (2021) 5:323–31. doi: 10.1016/S2352-4642(21)00050-X
37. Alders N, Penner J, Grant K, Patterson C, Hassell J, MacDermott N, et al. COVID-19 pandemic preparedness in a United Kingdom tertiary and quaternary children's hospital: tales of the unexpected. J Pediatric Infect Dis Soc. (2020) 9:772–776. doi: 10.1101/2020.08.20.20178541
38. Godfred-Cato S, Bryant B, Leung J, Oster ME, Conklin L, Abrams J, et al. COVID-19-associated multisystem inflammatory syndrome in children—United States, March–July 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:1074–80. doi: 10.15585/mmwr.mm6932e2
39. Masih M, Moll S, Raza N. Paediatric case of prolonged COVID-19 manifesting as PMIS-TS and atypical Kawasaki. BMJ Case Rep. (2020) 13:e237194. doi: 10.1136/bcr-2020-237194
40. Swann OV, Holden KA, Turtle L, Pollock L, Fairfield CJ, Drake TM, et al. Clinical characteristics of children and young people admitted to hospital with covid-19 in United Kingdom: prospective multicentre observational cohort study. BMJ. (2020) 370:m3249. doi: 10.1136/bmj.m3249
41. Bandi S, Nevid MZ, Mahdavinia M. African American children are at higher risk of COVID-19 infection. Pediatric Allergy Immunol. (2020) 31:861–4. doi: 10.1111/pai.13298
42. Cheung EW, Zachariah P, Gorelik M, Boneparth A, Kernie SG, Orange JS, et al. Multisystem inflammatory syndrome related to COVID-19 in previously healthy children and adolescents in New York City. JAMA. (2020) 324:294–6. doi: 10.1001/jama.2020.10374
43. Riollano-Cruz M, Akkoyun E, Briceno-Brito E, Kowalsky S, Reed J, Posada R, et al. Multisystem inflammatory syndrome in children related to COVID-19: a New York City experience. J Med Virol. (2021) 93:424–33. doi: 10.1002/jmv.26224
44. Al-Aamri MA, Al-Khars FT, Alkhwaitem SJ, AlHassan AK, Aithan AMA, Alkhalifa FH, et al. A Saudi G6PD deficient girl died with pediatric multisystem inflammatory syndrome-COVID-19. medRxiv. (2020). doi: 10.7759/cureus.10589
45. Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and mortality among black patients and white patients with Covid-19. N Engl J Med. (2020) 382:2534–43. doi: 10.1056/NEJMsa2011686
46. Muñoz-Price LS, Nattinger AB, Rivera F, Hanson R, Gmehlin CG, Perez A, et al. Racial disparities in incidence and outcomes among patients with COVID-19. JAMA Netw Open. (2020) 3:e2021892. doi: 10.1001/jamanetworkopen.2020.21892
47. Ogden CL, Fryar CD, Hales CM, Carroll MD, Aoki Y, Freedman DS. Differences in obesity prevalence by demographics and urbanization in US children and adolescents, 2013–2016. JAMA. (2018) 319:2410–8. doi: 10.1001/jama.2018.5158
48. Forno E, Celedon JC. Asthma and ethnic minorities: socio-economic status and beyond. Curr Opin Allergy Clin Immunol. (2009) 9:154–60. doi: 10.1097/ACI.0b013e3283292207
49. Irfan O, Muttalib F, Tang K, Jiang L, Lassi ZS, Bhutta Z. Clinical characteristics, treatment and outcomes of paediatric COVID-19: a systematic review and meta-analysis. Arch Dis Child. (2021) 106:440–8. doi: 10.1136/archdischild-2020-321385
50. Sadiq M, Aziz OA, Kazmi U, Hyder N, Sarwar M, Sultana N, et al. Multisystem inflammatory syndrome associated with COVID-19 in children in Pakistan. Lancet Child Adolesc Health. (2020) 4:e36–e7. doi: 10.1016/S2352-4642(20)30256-X
51. Khan KS, Ullah I. SARS-CoV-2 causes Kawasaki-like disease in children: cases reported in Pakistan. J Med Virol. (2021) 93:20–1. doi: 10.1002/jmv.26340
52. Kappanayil M, Balan S, Alawani S, Mohanty S, Leeladharan SP, Gangadharan S, et al. Multisystem inflammatory syndrome in a neonate, temporally associated with prenatal exposure to SARS-CoV-2: a case report. Lancet Child Adolesc Health. (2021) 5:304–8. doi: 10.1016/S2352-4642(21)00055-9
53. Didel S, Khera D, Kumar P, Goyal JP. COVID-19 in a young infant: a fatal multisystem inflammatory disorder. Indian J Pediatrics. (2021) 88:395. doi: 10.1007/s12098-020-03647-8
54. Bakhle A, Sreekumar K, Baracho B, Sardessai S, Silveira MP. Cavitary lung lesions in a neonate: potential manifestation of COVID-19 related multi-system inflammatory syndrome. Pediatrics Pulmonol. (2022) 57:311–4. doi: 10.1002/ppul.25732
55. Diwakar K, Gupta BK, Uddin MW, Sharma A, Jhajra S. Multisystem inflammatory syndrome with persistent neutropenia in neonate exposed to SARS-CoV-2 virus: a case report and review of literature. J Neonatal Perinatal Med. (2022) 15:373–7. doi: 10.3233/NPM-210839
56. Khan HQ, Srinivas SM, Sanjeeva GN, Swamynathan S, Shivappa SK. Scrotal ulcers in an infant with multi-system inflammatory syndrome in children associated with severe acute respiratory syndrome coronavirus 2 infection. Pediatrics Dermatol. (2022) 39:141–2. doi: 10.1111/pde.14871
57. Mamishi S, Movahedi Z, Mohammadi M, Ziaee V, Khodabandeh M, Abdolsalehi MR, et al. Multisystem inflammatory syndrome associated with SARS-CoV-2 infection in 45 children: a first report from Iran. Epidemiol Infect. (2020) 148:e196. doi: 10.1017/S095026882000196X
58. Bahrami A, Vafapour M, Moazzami B, Rezaei N. Hyperinflammatory shock related to COVID-19 in a patient presenting with multi-system inflammatory syndrome in children: First case from Iran. J Paediatr Child Health. (2021) 57:922–5. doi: 10.1111/jpc.15048
59. Zar HJ, Dawa J, Fischer GB, Castro-Rodriguez JA. Challenges of COVID-19 in children in low- and middle-income countries. Paediatric Resp Rev. (2020) 35:70–4. doi: 10.1016/j.prrv.2020.06.016
60. Rajabkhah K, Soodejani MT, Mahmudimanesh M, Gheshlaghi LA, Tabatabaei SM. Prevention of COVID-19 in children and neonates: a review. Arch Prevent Med. (2020) 5:026–30. doi: 10.17352/apm.000015
61. Groups Bank, TW,. World Bank Country Lending Country Classification. Nepal: Groups, Bank TW (2022). Available online at: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed May 20, 2022).
62. Millett GA, Jones AT, Benkeser D, Baral S, Mercer L, Beyrer C, et al. Assessing differential impacts of COVID-19 on black communities. Ann Epidemiol. (2020) 47:37–44. doi: 10.1016/j.annepidem.2020.05.003
63. Rodriguez RM, Torres JR, Sun J, Alter H, Ornelas C, Cruz M, et al. Declared impact of the US President's statements and campaign statements on Latino populations' perceptions of safety and emergency care access. PLoS ONE. (2019) 14:e0222837. doi: 10.1371/journal.pone.0222837
64. CDC. Health Equity Considerations and Racial and Ethnic Minority Groups. Atlanta, GA: CDC (2019). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html (accessed May 20, 2022).
65. Maldonado CZ, Rodriguez RM, Torres JR, Flores YS, Lovato LM. Fear of discovery among Latino immigrants presenting to the emergency department. Acad Emerg Med. (2013) 20:155–61. doi: 10.1111/acem.12079
66. Javalkar K, Robson VK, Gaffney L, Bohling AM, Arya P, Servattalab S, et al. Socio-economic and racial and/or ethnic disparities in multisystem inflammatory syndrome. Pediatrics. (2021) 147:e2020039933. doi: 10.1542/peds.2020-039933
67. Abrams EM, Szefler SJ. COVID-19 and the impact of social determinants of health. Lancet Respir Med. (2020) 8:659–61. doi: 10.1016/S2213-2600(20)30234-4
Keywords: multi-system inflammatory syndrome, COVID-19, SARS CoV-2, children, infant, pediatric multi-system inflammatory syndrome, Kawasaki disease, health disparities
Citation: Asghar Z, Sharaf K, Butt FA, Shaikh OA, Shekha M, Waris A, Ullah I and Nashwan AJ (2022) A global review of racial, ethnic and socio-economic disparities in multisystem inflammatory syndrome in children related to COVID-19. Front. Public Health 10:996311. doi: 10.3389/fpubh.2022.996311
Received: 17 July 2022; Accepted: 30 September 2022;
Published: 20 October 2022.
Edited by:
Orna Tal, Yitzhak Shamir Medical Center, IsraelReviewed by:
Ozgur Kasapcopur, Istanbul University-Cerrahpasa, TurkeyAmra Adrovic, Koç University Hospital, Turkey
Meyyur Aravamudan Veeraraghavan, Khoo Teck Puat Hospital, Singapore
Copyright © 2022 Asghar, Sharaf, Butt, Shaikh, Shekha, Waris, Ullah and Nashwan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abdulqadir J. Nashwan, YW5hc2h3YW5AaGFtYWQucWE=
 Zoha Asghar
Zoha Asghar Kanza Sharaf
Kanza Sharaf Faran Ahmed Butt1
Faran Ahmed Butt1 Omer Ahmed Shaikh
Omer Ahmed Shaikh Irfan Ullah
Irfan Ullah Abdulqadir J. Nashwan
Abdulqadir J. Nashwan