
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 16 November 2022
Sec. Occupational Health and Safety
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.994443
This article is part of the Research Topic The Public Health Problem of Burnout in Health Professionals View all 17 articles
Burnout is an epidemic, with deleterious effects on individuals, patient care, and healthcare systems. The Coronavirus Disease 2019 (COVID-19) pandemic may be exacerbating this problem. We aimed to explore socio-cultural and gender norms that modulate burnout development in physicians during the pandemic and analyze any disparities associated with gender, marital and immigration status and work-life balance. We conducted an online cross-sectional survey of physicians (August–November, 2021): The Maslach Burnout Inventory-Human Services Survey (MBI-HSS) was used to measure burnout, combined with a validated survey assessing work-life balance. Demographic data was obtained for each participant. MBI-HSS subscales were measured, along with work and home related changes due to COVID-19. The association between life changes due to COVID-19 and odds of burnout was estimated by logistic regression. Complementary analysis was performed to determine factors most associated with burnout. 352 respondents were analyzed. There was a high prevalence of burnout. Over half of individuals reported a high degree of emotional exhaustion (EE) (56%). 83% of individuals reported at least one life factor changed due to COVID-19. Home-related life changes due to COVID-19 were associated with 143% higher odds of emotional burnout [adjusted odds ratio (aOR) 2.43; 95% confidence interval (CI) 1.49, 3.98] after covariate adjusted analysis. High EE was most evident when there were three or more life changes, suggesting a cumulative effect. First-generation immigrants, older physicians, and trainees were identified as protective factors. Although female gender was identified as a factor related to EE through forward selection, this was not statistically significant (aOR 1.34; 95% CI 0.80, 2.24). Burnout remains pervasive among physicians. We highlight new risk factors for EE (home-life changes due to COVID-19), and protective factors (first-generation immigrants) not previously explored. Understanding burnout and its disparities allows for improved mitigation strategies, decreasing its deleterious effects.
Burnout among health care workers (HCW) is a public health crisis that has reached epidemic proportions (1). Originally described by Freudenberger in 1974 as emotional exhaustion associated with psychological and psychosomatic symptoms, the 11th Revision of the International Classification of Diseases (ICD-11) has since defined it as an occupational phenomenon resulting from chronic stress in the workplace that has not been successfully managed (2). It encompasses emotional exhaustion and energy depletion, depersonalization, and reduced professional efficacy (2–4).
Burnout not only has a negative impact on one's self but pervades many aspects of patient care. It has been associated with higher rates of patient morbidity and mortality, hospital length of stay, medical errors, employee attrition, and up to $6.3 billion dollars yearly in US healthcare costs (5, 6). Although efforts to evaluate and mitigate burnout are ongoing (7), HCW burnout rates at best appear to be stagnant (8) and at worst are increasing (4).
The current pandemic has only served to exacerbate the problem globally. A recent publication by The Washington Post/Kaiser Family Foundation Survey Project reported HCW burnout rates as high as 55% in the USA (9). Maunder et al. reported burnout in up to 62% in Canadian HCW (10), and Denning et al. reported burnout symptoms in 67% of HCW in the UK, Poland and Singapore (11). This is likely multifactorial. Increased work hours, fear of personal infection and transmission to family, high patient mortality, unpredictable infection surges, emergence of more virulent and transmissible viral strains, vaccine hesitancy and medical misinformation may be pushing the emotional and psychological wellbeing of HCW to a breaking point.
The pandemic has also brought to the forefront challenges specific to women in medicine. Although women in healthcare have consistently reported higher rates of burnout compared to men over the last few decades, a 2022 national report showed a greater disparity compared to normal: 56% of women reported burnout compared to 41% of men (8). Pre-existing gender-bias and pay inequality in the workplace likely continue to play a role, but factors specific to the pandemic such as increased household responsibilities and coordinating care for “at home children” may exacerbate work-life conflict. In fact, burnout may disproportionately affect HCW not only based on their gender, but also marital and immigration status and family dynamics (4, 8, 12). We hypothesized that immigration status and female gender are protective factors for burnout and sought to identify and analyze these and other possible disparities.
After obtaining IRB approval, an anonymous online cross-sectional survey consisting of two main components: the MBI-HSS and a gender-focused questionnaire developed and validated by Raffi et al. (13, 14) was administered through the Qualtrics survey platform to HCW who had worked during the COVID-19 pandemic, including but not limited to those who had direct contact with patients diagnosed with COVID-19.
The MBI-HSS is a psychological assessment tool consisting of 22 items and is the most commonly used method to assess burnout in HCW. Its psychometric properties have been examined and well validated among numerous populations and professions (15, 16). It assesses the 3 main components of burnout scored on a seven-point scale, ranging from 0 (never) to 6 (every day). EE is evaluated over nine questions with a score range of 0–54 (>26 reflected high burnout, 17–26 reflected moderate burnout, and <17 reflected low burnout). Depersonalization is assessed over five questions with a score range of 0–30 points (>12 indicated high burnout, 7–12 reflected moderate burnout, and <7 reflected low burnout). Personal accomplishment is evaluated with eight items with a score range of 0–48 points (<32 reflected high burnout, 32–38 indicated moderate burnout and >38 reflected low burnout).
An established questionnaire by Rafii et al. was also used to characterize aspects of home and work life which have been previously associated with burnout. Evaluated attributes included clinical responsibilities such as time spent seeing patients, household responsibilities such as childcare, and sleep habits, as well as finances, substance/alcohol use and overall sense of wellbeing (14). For each individual attribute, participants reported if there was any change due to COVID-19.
Based on these answers, we determined if a participant had any life attribute, any home life attribute, and any work life attribute changed due to COVID-19. The total number of attributes changed due to COVID-19 was also calculated. The questionnaire also included other variables of interest including: age, female gender, trainee status, immigrant status (first- or second-generation immigrants) and specialty.
Various social media platforms restricted to HCW were used for global recruitment and questionnaire dissemination including: Worldwide Facebook groups: (Physicians Moms Group, Physicians for Patient Protection, The Physician Collective PMG COVID 19 subgroup, COVID-19 Texas Health care Professionals, Novel Coronavirus and COVID-19; Houston Women Physicians, Physician Women in Leadership) and WhatsApp (Pulmonary and Critical Care Fellows and Intensivists at Baylor College of Medicine, Houston, TX, Internal Medicine Residents in various programs in New Jersey, New York, Texas, Jamaica, India). The questionnaire was also sent via email (Baylor College of Medicine Alumni group, American University of Beirut and Andhra Medical College, Andhra Pradesh Medical graduates association, American association of Physicians of Indian Origin, Dow Medical school in Pakistan). The survey was only available in English and hence only sent to HCW with English proficiency. There was no randomization, group assignments or follow-up.
The analytic population were all physician respondents who provided complete data, including responses necessary to calculate scores on the MBI-HSS. Life changes due to COVID-19 which were not answered or not applicable for all respondents (such as who cared for children at home) were singly imputed as “no” and were categorized into work-related or home-related changes. Summary statistics were generated.
The association between life changes due to COVID-19 and odds of burnout in each MBI-HSS subscale was estimated by logistic regression. Unadjusted and adjusted estimates were performed. We conducted four separate analyses, parameterizing life changes due to COVID-19 as any life change, any work-related life change, any home-related life change, and a count variable of the total number of life changes. We adjusted a priori for age, gender, training status, and medical specialization, presuming these to be important covariates which may confound the relationship between life changes due to COVID-19 and burnout. A two-sided p < 0.05 was taken to infer statistical significance.
We next performed a complementary analysis to determine which factors most explained burnout, without forcing life changes due to COVID-19 into the model. Because of the exploratory objectives of the study, we relied on data agnostic techniques to identify these factors and no pre-specified power analysis was conducted. We did backward and forward stepwise techniques with the threshold p-value for variable removal or insertion, respectively, of p < 0.1, and best subset selection based on the model which produced the lowest Akiake Information Criterion (32148735).
All analyses were performed in Stata 15 (StataCorp; College Station, TX).
A total of 352 respondents were included in the analysis (Table 1). Mean age was 41 years, and approximately two-thirds were of female gender. Ninety-two (26%) of respondents self-identified as trainees. There was a high prevalence of burnout, with over half of individuals reporting a high degree of EE.
Table 2 summarizes the distribution of life changes that occurred due to COVID-19. Overall, most individuals (83%) reported at least one life factor changed due to COVID-19, with approximately equal proportions of these changes being in factors related to home or work.
Table 3 reports the adjusted relationship between any life change, any work-related life change, and any home-related life change due to COVID-19 with odds of burnout in each of the three MBI-HSS subscales. Unadjusted analysis is available in Table 4. In adjusted analysis, we did not find a statistically significant relationship between any life change due to COVID-19 with burnout in all scales. However, when examining home vs. work-related changes, we found that any home-related life change due to COVID-19 was associated with 143% higher odds of emotional burnout [adjusted odds ratio (aOR) 2.43; 95% confidence interval (CI) 1.49, 3.98]. There were no relationships between work-related life change due to COVID-19 and burnout. When the total number of COVID-19-related life changes were separated into equal sextiles, we found that high EE was most evident when there were three or more life changes, suggesting that the effect is cumulative (Figure 1).
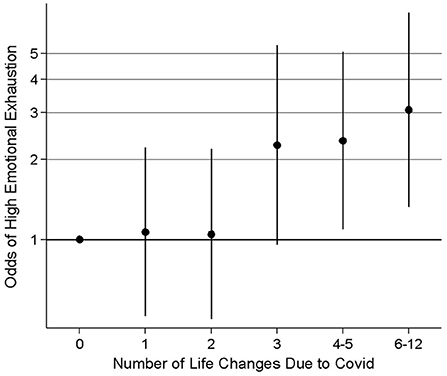
Figure 1. Odds ratios and 95% confidence intervals for emotional burnout associated with number of life changes due to COVID.
Because we found that life changes due to COVID-19 most impacted the EE dimension of the MBI-HSS, we next investigated if such life changes remained predictive of EE when taken together with all other factors assessed by the survey. All three variable selection methods found that home-related life changes due to COVID-19 retained a substantial relationship with high emotional burnout but work-related life changes did not.
In addition, high emotional burnout was also more likely with a greater number of hours spent seeing patients and greater household responsibility. Conversely, being a first-generation immigrant, being older, and being a trainee were identified as protective factors (Table 5). Both backward selection and best subset selection identified the same factors. Forward selection identified that female gender was related to emotional burnout, but this comparison was not statistically significant (aOR 1.34; 95% CI 0.80, 2.24).
Burnout as an entity remains pervasive among HCW. 81% of respondents in this present study self-reported at minimum moderate EE among respondents, with 56% reporting high EE. This correlates with previously published reports examining burnout (1, 9). While burnout is still a subjectively defined phenomenon, the effects of developing burnout can manifest as interpersonal difficulties, increased medical errors, patient morbidity and mortality and ultimately job burnout and attrition (5, 6). Burnout effects are cumulative. Repeated and prolonged EE may precipitate the movement of HCW to different institutions, or to leave medicine altogether. Indeed, The Washington Post/Kaiser Family Foundation Survey Project reports that 29% of HCW have considered leaving the medical field, in part due to burnout (9). Moreover, a recent AAMC report projects a shortfall of up to 124,000 physicians by 2034, with burnout contributing to accelerated rather than delayed retirement (17). There is scant research exploring the socio-cultural and gender norms that may modulate burnout development. In this study we sought to understand the effects, if any, gender and immigrant status had on self-reported burnout in our selected sample, as well the effects of the COVID-19 pandemic on work-life balance and its association with burnout.
In this study, 66.5% of our respondents identified as female. Women have historically reported and continue to report higher rates of burnout than men, and the reasons are not fully understood. A recent 2022 survey of over 13,000 physicians reported burnout rates of 56% in women vs. 41% in men (8). Although not statistically significant, forward selection in this present study also identifies a trend toward increased emotional burnout in women (aOR 1.34; 95% CI 0.80, 2.24). Although women may be more likely to report burnout than men, traditionally gender specific roles of childrearing and household responsibilities may be a contributing factor in working women who had increased home responsibilities due to COVID-19, or who had arranged for help and support prior to the pandemic, but lost it with virus-related restrictions. In fact, in both genders, life changes due to COVID-19 most impacted self-reported EE. Specifically, home changes were associated with 143% higher odds of emotional burnout, with apparent cumulative effects, with increasing likelihood of burnout per additional reported home change. This is particularly significant as the prevailing culture of medicine stigmatizes and discourages help-seeking. Many physicians do not seek care when depressed or anxious and are often expected to function impeccably at work despite personal life changes. The COVID-19 pandemic continues to highlight needed systemic changes in supporting faculty and trainees through personal difficulties as a way to counter the development/worsening of burnout.
To our knowledge, this is the first study of its kind to examine the effect of first and second-generation immigrant status on trainee and non-trainee physician burnout. Immigrant status appears to be protective from EE in our survey. Compared to non-immigrants, first generation immigrants were 49% less likely to report burnout symptoms, and there was a non-statistically significant trend toward less exhaustion among second generation immigrants. The reasons for this are unknown. Although there is a paucity of data regarding burnout among immigrant physicians, West et al. attempted to explore differences in burnout between U.S. and international medical graduates (IMGs) in Internal Medicine residency. They hypothesized that IMGs trainees in US residency programs may be less prone to burnout due to their successful navigation through the complex and highly competitive residency selection process (18). Onge et al. suggested that differences in medical school curricula and emphasis on USMLE scores may play a role (19). We further theorize this may be due to cultural differences as it relates to moral value systems and increased emphasis on labor in many developing countries and under resourced settings. Nevertheless, this finding is in line with the perspective that burnout development is a fairly personal experience with intricate socio-cultural effects that need further investigation. Burnout in immigrant physicians, who constitute 28% of the United States physician workforce, and who train and work in the U.S., appears to be poorly understood, and further study is needed in this population.
Of the three subdivisions of burnout, 81% of respondents reported moderate to high EE compared to 63.3% reporting depersonalization and 30.4% reporting low personal achievement. EE is likely the first manifestation of burnout. We hypothesize that repeated and prolonged EE has a direct temporal relationship to eventual depersonalization and low professional achievement. Future study is needed on this.
We do recognize limitations in this study. Recruitment strategies involved use of various social media platforms for questionnaire dissemination and may have targeted particular groups including but not limited to physicians in Lebanon, India, and Pakistan, acknowledging that various cultures may have alternate views on the responsibilities of men and women at home and at work. Survey completion was also limited to English-speaking participants meaning the sample was not globally representative. Moreover, there was no randomization within the study of participants which potentially affects the generalizability of results.
The survey design also inquired less about work-related changes than home-related changes, taking into account only hours spent working and time spent obtaining CME and subspecialty education. Future assessments of burnout may need to assess other work-related aspects of work-life balance in order to have a more comprehensive understanding of physician burnout. Most studies about physician burnout identify key workplace factors such as dealing with patient death and illness, a loss of autonomy at work, decreased sense of control over work due to administrative requirements, clerical stressors related to utilization of electronic health record usage, and frequent call duties (5). It is possible that such factors may compromise the delivery of health care services and lead to increased rates of medical errors and decreased job satisfaction. The implications of work-related changes could be far-reaching and should be a topic of future study.
Another consideration in this study was that a significant sector of the study population was excluded due to incomplete survey answers, particularly to questions about gender expectation, a core area our group was interested in studying.
Burnout remains a global epidemic affecting the healthcare sector with significant impact on medical workers' individual lives and on patient care. The COVID-19 pandemic, still ongoing after 2 years and with no clear signs of remitting, has had unprecedented implications for HCW work-life balance. This worldwide cross-sectional survey brings to light unique risk factors for emotional exhaustion and burnout during the pandemic as well as unique protective factors. First and second-generation immigrant status, a factor not known to be previously explored in this manner, appears to be protective from EE in our survey. Only by understanding high risk workers who may develop high levels of EE, depersonalization and decreased personal accomplishment, can we enact effective mitigation strategies to prevent end-stage burnout and subsequent exodus from the field of medicine.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Institutional Review Board for Human Subject Research for Baylor College of Medicine and Affiliated Hospitals (BCM IRB). The patients/participants provided their written informed consent to participate in this study.
GO: literature review, chart review, data and results analysis, and grammatical composition. NS: data review, discussion, and conclusion drafts. TW: statistical analysis. NM and KG: hypothesis and methods outline, questionnaire formulation, IRB applications, overall guidance, and review of project including suggestions for discussion. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. The Lancet Editorial. Physician burnout: a global crisis. Lancet. (2019) 394:93. doi: 10.1016/S0140-6736(19)31573-9
2. Freudenberger, H. Staff burn-out. J Social Issues. (1974) 30:159–65. doi: 10.1111/j.1540-4560.1974.tb00706.x
3. World Health Organization. ICD-11 for Mortality and Morbidity Statistics. (2022). https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/129180281 (accessed August 1, 2022).
4. Prasad K, McLoughlin C, Stillman M, Poplau S, Goelz E, Taylor S, et al. Prevalence and correlates of stress and burnout among U.S. healthcare workers during the COVID-19 pandemic: a national cross sectional survey study. EClin Med. (2021) 35:1, 3, 5–8. doi: 10.1016/j.eclinm.2021.100879
5. Patel R, Bachu R, Adikey A, Malik M, Shah M. Factors related to physician burnout and its consequences: a review. Behav Sci. (2018) 8:98. doi: 10.3390/bs8110098
6. Han S, Shanafelt T, Sinsky C, Awad K, Dyrbye L, Fiscus L, et al. Estimating the Attributable Cost of Physician Burnout in the United States. Ann Intern Med. (2019) 170:784. doi: 10.7326/M18-1422
7. Aryankhesal A, Mohammadibakhsh R, Hamidi Y, Alidoost S, Behzadifar M, Sohrabi R, et al. Interventions on reducing burnout in physicians and nurses: A systematic review. Med J Islam Repub Iran. (2019) 33:77. doi: 10.34171/mjiri.33.77
8. Kane L. Physician Burnout & Depression Report 2022: Stress, Anxiety, and Anger. Medscape.com 2022. Available online at: https://www.medscape.com/slideshow/2022-lifestyle-burnout-6014664 (accessed July 6, 2022).
9. Kirzinger A, Kearney A, Hamel L, Brodie M. KFF/The Washington Post Frontline Health Care Workers Survey. KFF.org (2021). Available online at: https://www.kff.org/coronavirus-covid-19/poll-finding/kff-washington-post-health-care-workers/ (accessed July 2, 2022).
10. Maunder RG, Heeney ND, Strudwick G, Shin H, O'Neill B, Young N, et al. Burnout in hospital-based healthcare workers during COVID-19. Sci Briefs. (2021) 2:1–24. doi: 10.47326/ocsat.2021.02.46.1.0
11. Denning M, Goh E, Tan B, Kanneganti A, Almonte M, Scott A, et al. Determinants of burnout and other aspects of psychological well-being in healthcare workers during the COVID-19 pandemic: a multinational cross-sectional study. PLoS ONE. (2021) 16:e0238666. doi: 10.1371/journal.pone.0238666
12. Leo C, Sabina S, Tumolo M, Bodini A, Ponzini G, Sabato E, et al. Burnout among healthcare workers in the COVID 19 era: a review of the existing literature. Front Public Health. (2021) 9:750529. doi: 10.3389/fpubh.2021.750529
14. Raffi J, Trivedi M, White L, Murase J. Work–life balance among female dermatologists. Int J Women's Dermatol. (2020) 6:13–9. doi: 10.1016/j.ijwd.2019.07.001
15. Pisanti R, Lombardo C, Lucidi F, Violani C, Lazzari D. Psychometric properties of the Maslach Burnout Inventory for Human Services among Italian nurses: a test of alternative models. J Adv Nurs. (2013) 69:697–707. doi: 10.1111/j.1365-2648.2012.06114.x
16. Lin C, Alimoradi Z, Griffiths M, Pakpour A. Psychometric properties of the Maslach Burnout Inventory for Medical Personnel (MBI-HSS-MP). Heliyon. (2022) 8:e08868. doi: 10.1016/j.heliyon.2022.e08868
17. IHS Markit Ltd. The Complexities of Physician Supply and Demand: Projections From 2019 to 2034. Washington, DC: AAMC (2021).
18. West C, Shanafelt T, Kolars J. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. (2011) 306:952–60. doi: 10.1001/jama.2011.1247
Keywords: burnout, COVID-19, immigrants, gender, women
Citation: Otuonye GC, Shenoi N, Wu TD, Guntupalli K and Moukaddam N (2022) “I have nothing more to give”: Disparities in burnout and the protective role of immigrant status during the COVID-19 pandemic. Front. Public Health 10:994443. doi: 10.3389/fpubh.2022.994443
Received: 14 July 2022; Accepted: 17 October 2022;
Published: 16 November 2022.
Edited by:
Oriol Yuguero, Lleida Institute for Biomedical Research (IRBLleida), SpainReviewed by:
Vera Martins, University of Porto, PortugalCopyright © 2022 Otuonye, Shenoi, Wu, Guntupalli and Moukaddam. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gene Chibuchim Otuonye, R2VuZS5vdHVvbnllQGJjbS5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.