- 1Department of Nursing, Fourth Military Medical University, Shaanxi, China
- 2Department of Health Statistics, Fourth Military Medical University, Shaanxi, China
- 3Department of Endocrinology, Tangdu Hospital, Fourth Military Medical University, Shaanxi, China
Aim: COVID-19 patients' security is related to their mental health. However, the classification of this group's sense of security is still unclear. The aim of our research is to clarify the subtypes of security of patients infected with COVID-19, explore the factors affecting profile membership, and examine the relationship between security and psychological capital for the purpose of providing a reference for improving patients' sense of security and mental health.
Methods: A total of 650 COVID-19 patients in a mobile cabin hospital were selected for a cross-sectional survey from April to May 2022. They completed online self-report questionnaires that included a demographic questionnaire, security scale, and psychological capital scale. Data analysis included latent profile analysis, variance analysis, the Chi-square test, multiple comparisons, multivariate logistical regression, and hierarchical regression analysis.
Results: Three latent profiles were identified—low security (Class 1), moderate security (Class 2), and high security (Class 3)—accounting for 12.00, 49.51, and 38.49% of the total surveyed patients, respectively. In terms of the score of security and its two dimensions, Class 3 was higher than Class 2, and Class 2 was higher than Class 1 (all P < 0.001). Patients with difficulty falling asleep, sleep quality as usual, and lower tenacity were more likely to be grouped into Class 1 rather than Class 3; Patients from families with a per capita monthly household income <3,000 and lower self-efficacy and hope were more likely to be grouped into Classes 1 and 2 than into Class 3. Psychological capital was an important predictor of security, which could independently explain 18.70% of the variation in the patients' security.
Conclusions: Security has different classification features among patients with COVID-19 infection in mobile cabin hospitals. The security of over half of the patients surveyed is at the lower or middle level, and psychological capital is an important predictor of the patients' security. Medical staff should actively pay attention to patients with low security and help them to improve their security level and psychological capital.
Introduction
At present, the COVID-19 pandemic continues to spread among countries and regions, and there is no specific antiviral therapy so far (1, 2). It has greatly changed the global political and economic development model, the trend of international relations, and even people's daily lives (3). The scope, scale, destructive power, and consequences of COVID-19 are unprecedented in history (4, 5). It has a strong transmission capacity, and once human beings are infected with the novel coronavirus, they can develop chest pain, cough, expectoration, fever, and other infection symptoms (6, 7). Severe infections can lead to respiratory failure or even multiple organ failure (8). To some extent, COVID-19 has created panic and fear among people.
Now in China, the COVID-19 pandemic is still existing, and the fight against the pandemic is ongoing. In March 2022, COVID-19 broke out on a large scale in Shanghai, China. By the end of May, there had been more than 600,000 confirmed cases of COVID-19 and asymptomatic infections in Shanghai. As an effective epidemic control measure for COVID-19 pandemic, the mobile cabin hospital is an effective way to cut off the potential route of infection in society (9). Medical staff are dispatched to mobile cabin hospitals to take care of patients who test positive for the virus but show no severe symptoms. This can relieve the pressure of hospital reception and achieve the goal of zero transmission in communities outside quarantine (10, 11). The mobile cabin hospital has many advantages, such as its rapid deployment, good mobility, and strong environmental adaptability, and can apply well to emergency medical rescue tasks, so it has been highly valued by various countries (12, 13). In this round of the pandemic in Shanghai, a great number of cabin hospitals were needed to curb the COVID-19 pandemic, and exhibition halls, gymnasiums, and other buildings were transformed into mobile cabin hospitals.
As a kind of stressor, the outbreak of an epidemic can easily lead to individual psychological stress (14, 15). Research shows that the psychological status of patients with diagnosed COVID-19 is not optimistic, and they have varying degrees of anxiety and panic due to their worrying about the prognosis of the disease (16, 17). Patients who entered mobile cabin hospitals for centralized isolation treatment were highly concentrated in a relatively narrow but open space. Such an unfamiliar environment can easily induce mental health problems and hinder the rehabilitation of the disease (18). Furthermore, with the virus becoming less and less aggressive, most patients will have mild or moderate symptoms, to whom more attention should be paid. The source of their negative emotions and mental health problems is mainly their uncertainty and lack of security (19, 20).
Sense of security refers to the individual's feeling of confidence and freedom when faced with fear and danger (21), as well as the psychological feeling when dealing with these risks (22). It is one of the important factors affecting mental health and is mainly manifested as a sense of certainty and control (23). In recent years, because security is a basic psychological need, it has received a lot of attention and been widely studied. When individuals' security is threatened, they will be nervous and afraid, and their normal life and work will even be affected (24). Since COVID-19 pandemic is a public health emergency and is highly contagious, it threatens people's security (25). When the confirmed cases enter the mobile cabin hospital for centralized isolation, facing the unfamiliar environment and uncertain conditions, their security is threatened. This will cause them to have negative emotions such as anxiety and fear and affect the treatment of the disease (26). Therefore, patients' security in mobile cabin hospitals needs attention.
Psychological capital refers to a positive psychological state that individuals show in the process of growth and development, including self-efficacy, hope, optimism, and tenacity (27). Research shows that psychological capital is positively correlated with a sense of security; that is, individuals with good psychological capital will have a strong sense of security (28). In the face of threats, psychological capital has a good buffer effect to counter fear and anxiety (29). Under the same situation, the security of individuals with high psychological capital is higher than that of those with low psychological capital (30, 31).
However, currently there are few investigations into the security of patients with COVID-19 infection in mobile cabin hospitals, and their security levels are not clear. Moreover, there are rare researches on the relationship between the security and psychological capital of patients with COVID-19 infection in mobile cabin hospitals. Therefore, the purpose of our study is to take the COVID-19 patients in mobile cabin hospitals during the outbreak of COVID-19 in Shanghai as the research objects and to investigate their sense of security and related influencing factors to provide a reference for further optimizing the management of mobile cabin hospitals and improving the patients' sense of security.
Methods
Sample size
The sample size was equal to 10 times the number of items being tested. There were 49 items in our questionnaire. Therefore, the calculation formula of sample size was n = (7 items + 16 items + 26 items) × 10 = 490, which meant that at least 490 subjects were required for this study. Considering an expected sample loss rate of 20%, the sample size needed be further expanded. Therefore, the final sample size required was n = 490 ÷ (1–20%) ≈612.5, and the final sample size required was 613 at least.
Participants
The study was conducted in accordance with the Declaration of Helsinki (32) and the guidelines of the Air Force Medical University. Participants were patients with confirmed COVID-19 recruited from a mobile cabin hospital during the outbreak of COVID-19 in Shanghai. All patients were informed that participation in this study was voluntary. They could withdraw from the study at any time for any reason, and the questionnaires were completed anonymously. The inclusion criteria were COVID-19 patients in a mobile cabin hospital. The exclusion criteria were those who had recently experienced major life events and those who were unwilling to participate in the survey. A total of 650 patients with COVID-19 were selected for the cross-sectional survey from April to May 2022. However, 18 subjects withdrew from the survey, 13 did not fill out the questionnaire completely, and 11 filled out the questionnaire with too much homogeneity, which was regarded as an invalid questionnaire. The final sample included 608 patients (270 men, 338 women) from the mobile cabin hospital, aged 11–76 years (Mage = 38.08, SD = 13.47).
Measures
Descriptive measures
Data on demographic variables (i.e., sex, age, place of residence, education background, marital status, monthly income per capita in family, sleep quality after diagnosis with COVID-19) were collected through a self-reported questionnaire.
Security
Participants' security levels were measured using the Security Scale (33). The Security Scale is applicable to Chinese cultural background and is widely used in China, as well as has good reliability and validity among Chinese people (34, 35). The Security Scale contains 16 items and two dimensions: interpersonal security and certainty in control. Among them, the interpersonal security dimension contains eight items, which mainly reflect the individual's security in the process of interpersonal communication. The certainty in control dimension contains eight items, which mainly reflect the individual's prediction of life and their sense of certainty and control. The scale adopts Likert's 5-level scoring method, with 1–5 points from very consistent to very inconsistent, respectively. The highest possible score is 80, with higher scores indicating more security. For example, “I always worry that something bad will happen.” The Cronbach's alpha for the interpersonal security dimension and the certainty in control dimension were 0.868 and 0.934, and for the total scale was 0.902.
Psychological capital
Participants' psychological capital was measured using the Psychological Capital Scale (36). The psychological capital Scale is widely used in China and has good reliability and validity among Chinese people (37, 38). The scale contains 26 items and four dimensions: self-efficacy, hope, optimism, and tenacity. The higher the score of the scale, the higher the positive tendency of psychological capital. The scale adopts Likert's 7-level scoring method, with 1–7 points from completely non-compliant to fully compliant, respectively. The Cronbach's alpha coefficient of the scale was 0.873 and ranged between 0.855 and 0.920 for the four dimensions.
Procedure and data analysis
Before beginning the formal investigation, we trained the researchers to ensure the quality of the research. With the consent of the mobile cabin hospital managers, researchers explained the purpose of the survey to the patients to obtain their approval and support prior to data collection, and the patients gave their consent to participate in the research. With the help of head nurses in the mobile cabin hospital, questionnaires were distributed to the patients. The questionnaire was collected on the spot. We eliminated invalid questionnaires that were not filled in completely and answered randomly. The method of double check was used to input the data of the valid questionnaires to ensure accuracy.
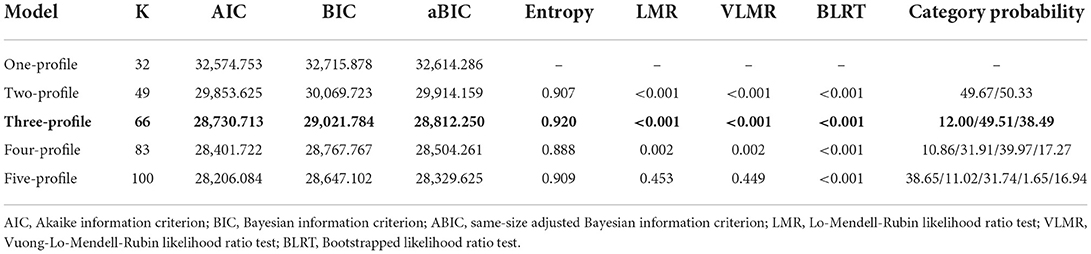
SPSS 26.0 statistical software and Mplus 8.3 were used for statistical analysis. Descriptive statistics (mean, standard deviation, frequency and percentage) were used to describe the sample's characteristics. The Chi-square test and variance analysis were used to screen statistically significant indicators. Logistic regression analysis was used to evaluate the influencing factors of potential categories. The data for security were entered into the latent profile analysis, with one class initially and additional classes added incrementally until a unique solution could not be determined with maximum likelihood methods. The latent profile analysis model evaluation indicators included the Akaike information criterion (AIC), Bayesian information criterion (BIC), sample-size-adjusted BIC (aBIC), bootstrapped likelihood ratio test (BLRT), Lo-Mendell-Rubin (LMR) adjusted likelihood ratio test, Vuong-Lo-Mendell-Rubin likelihood ratio test (VLMR), and entropy. A higher entropy value, which is an important indicator, indicates a more accurate classification of the model. The smaller the AIC, BIC, and aBIC values, the better the model fit. LMR, BLRT, and VLMR are often used in model comparison, and a significant P-value indicates that K model categories are better than K – 1 model categories. The best-fitting models were selected through comprehensive evaluation of the above indexes, and the security among patients infected with COVID-19 in the mobile cabin hospital was divided into different categories. Hierarchical regression analysis was used to explore the impact of psychological capital on the security of patients. All tests conducted were two-sided, with a significance level of 0.05.
Ethical considerations
Our research was in accordance with the ethical standards formulated in the Declaration of Helsinki (39) and was confirmed by the Fourth Military Medical University ethics committee approval (KY20224143-1). Informed consent was provided by the participants prior to their participation. The survey was anonymous, and the confidentiality of the information was assured.
Results
Common method deviation
The Harman single-factor method was used to test the common method deviation. The variance explained by the maximum factor variance was 27.8%, less than the critical value of 40% (40). The statistical test results showed that there was no significant common method bias in the measurement.
Exploratory latent profile analysis
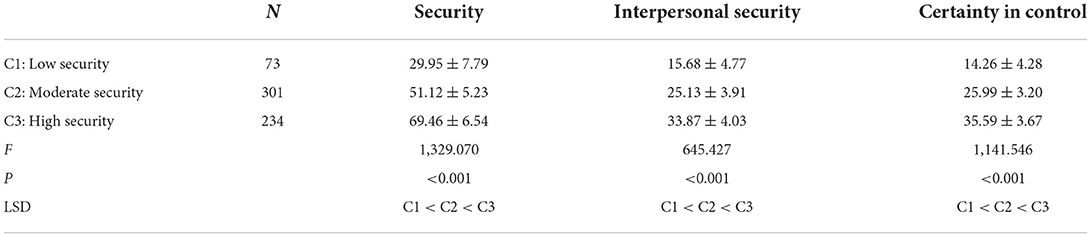
The best-fitting latent profile analysis was the three-class model (Table 1). The P-values of the LMR test (<0.001), VLMR test (<0.001), and BLRT test (<0.001) of the three-class model were the smallest, suggesting that this model was statistically significant at the α = 0.05 level. This model had the highest entropy value (0.920) and the lower AIC (28,730.713), BIC (29,021.784), and aBIC (28,812.250). Figure 1 shows the subtypes of patients' security (Classes 1, 2, and 3); the proportion of each type was 12.00, 49.51, and 38.49%. According to this model, they could be distinguished as having relatively low (Class 1), medium (Class 2), or high (Class 3) security. The correct classification probabilities mean the average latent class probabilities for the most likely latent class membership by latent class. The larger the proportion, the more accurate the result. In order to further verify the reliability of the classification results, the correct classification probabilities of the three categories of patients' safety were calculated to be 97.1, 96.6, and 95.7% respectively (Table 2).
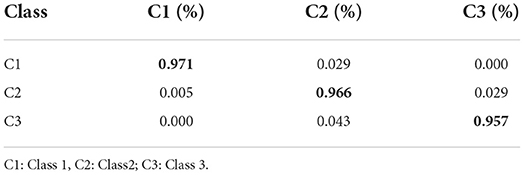
Table 2. Average latent class probabilities for most likely latent class membership (row) by latent class (column).
Security of patients with COVID-19 in different categories and characteristics of the different classes
Table 3 presents the security and its two dimensions of the three classes. The results of the analysis of variance of the total score and two dimensions of patient security in each group were statistically significant (F = 1,329.070, P < 0.001; F = 645.427, P < 0.001; F = 1,141.546, P < 0.001). Further least significant difference (LSD) analysis showed that Class 1 < Class 2 < Class 3 in terms of security and its two dimensions (P < 0.001). Univariate analysis showed that there were significant differences among the three groups in educational level (χ2 = 9.956, P = 0.007), family income (χ2 = 22.936, P = 0.001), psychological capital (F = 35.907, P < 0.001), and its four dimensions (F = 52.296, P < 0.001; F = 43.750, P < 0.001; F = 23.610, P < 0.001; F = 7.192, P = 0.001). There was no difference among the three groups in other demographic characteristics (Table 4).
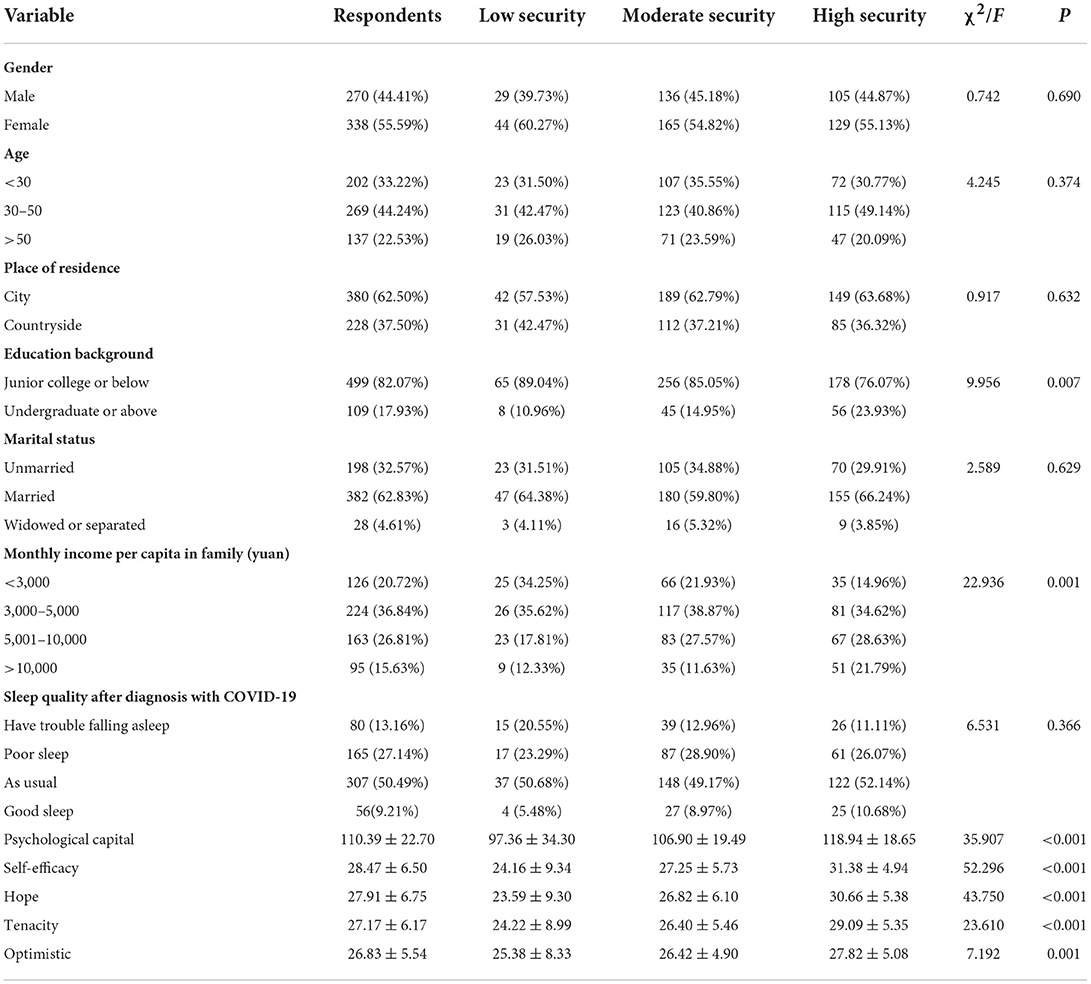
Table 4. The differences in the security types of COVID-19 patients in demography and psychological capital.
Influencing factors of security in different groups of patients with COVID-19
The security of patients with COVID-19 determined by latent profile analysis was used as the dependent variable, and Class 3 was used as the control group. Compared with Class 3, those with trouble falling asleep (OR = 6.572, P < 0.05), sleep quality as usual (OR = 3.693, P < 0.05), and lower tenacity (OR = 0.831, P < 0.05) were more likely to be grouped into Class 1. Those with a monthly per capita family income <3,000 (ORclass1 = 3.131, P < 0.05; ORclass2 = 2.383, P < 0.05), lower self-efficacy (ORclass1 =0.678, P < 0.001; ORclass2 = 0.783, P < 0.001), and lower hope (ORclass1 = 0.739, P < 0.001; ORclass2 = 0.868, P < 0.001) were more likely to be grouped into Classes 1 and 2 (Table 5).
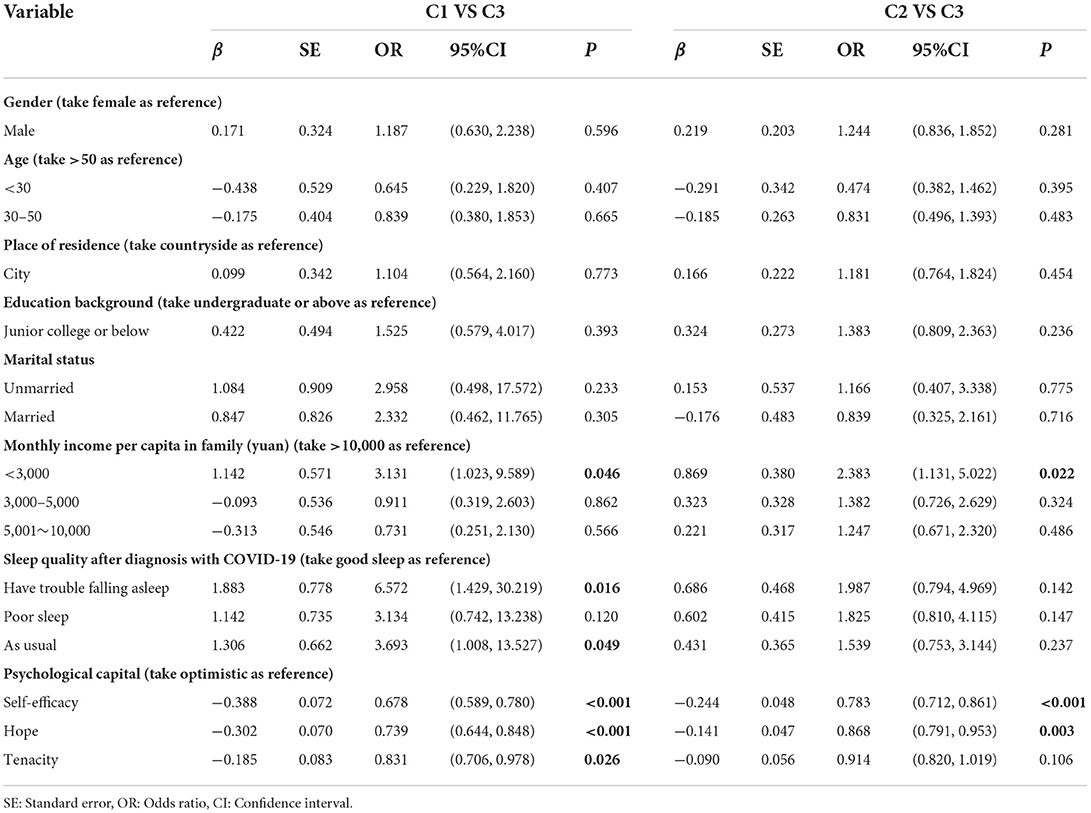
Table 5. The multifactor analysis of security of patients infected with COVID-19 by logistic regression.
Hierarchical regression analysis of COVID-19 patients' security
Table 6 shows the results of hierarchical regression analysis with security as the dependent variable. The results showed that family income and sleep quality had entered the regression equation of the security of COVID-19 patients (F = 3.182, R2 = 0.089, P < 0.001). On the basis of model 1, four dimensions of psychological capital were included in model 2 (F = 10.093, R2 = 0.275, P < 0.001). Variance expansion factors were <10, indicating that there was no obvious collinearity among variables. Psychological capital was an important predictor of patients' security that could independently explain 18.70% of its variation (ΔR2 = 0.187, P < 0.001).
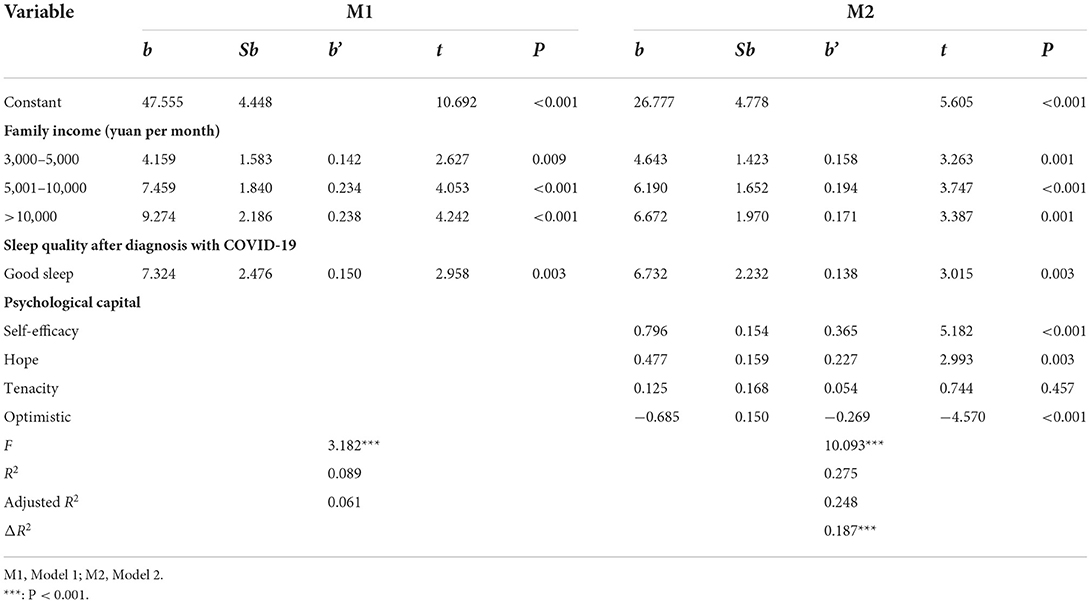
Table 6. Hierarchical regression analysis of psychological capital on the security of COVID-19 patients.
Discussion
Necessity of the study on the security of patients with COVID-19 infection in mobile cabin hospitals
The establishment of mobile cabin hospitals to treat a large number of patients with mild or moderate COVID-19 is an effective way to deal with the outbreak of the pandemic and block its spread at the social level (41). In the face of the special isolation environment in these hospitals, patients' security is threatened, which has an impact on their psychological health and disease treatment. However, there is a lack of research on the sense of security of this group, and limited studies have examined whether psychological capital might impact the sense of security of patients with COVID-19 infection in mobile cabin hospitals. Therefore, the purpose of this study was to clarify the subtypes of security of patients infected with COVID-19, to explore the influencing factors of different types of security, and to examine the relationship between patients' security and psychological capital. To our knowledge, this is the first research to study the security of patients with COVID-19 infection in mobile cabin hospitals.
More attention should be paid to patients with low sense of security
Our study used latent profile analysis to classify patients' sense of security into three categories: low security (Class 1), moderate security (Class 2), and high security (Class 3). Among them, Class 2 had the largest number, accounting for 49.51%, which indicates that nearly half of the patients had moderate security. Although the number of patients in Class 1 was the lowest, accounting for 12%, this group needs the most attention.
More and more attentions have been paid to patients' sense of security in recent years, and it is an important aspect of patient-centered care (42). Previous studies have shown that patients with low sense of security were more worried about their economic situation (43). A longitudinal study showed that patients with high security always had good psychological health (44). The patient's sense of security includes many influencing factors, such as external environmental factors and self-related factors, such as economic and psychological conditions (45, 46). In our study, we explored the sense of security of patients with COVID-19 from different perspectives, which were showed in Tables 4, 5. However, the results in Tables 4, 5 were not consistent because that a multivariable logistic regression model was performed to include all independent variables.
Those whose per capita family income was <3,000 tend to have a low or medium sense of security. This is because under COVID-19, people in controlled zones are restricted from going to work, which has a great impact on people's income, especially in low-income families (47, 48). Such people have to worry about disease, but also their living expenses and loan repayment, so they are more likely to have a low sense of security. Furthermore, our results showed that the sleep quality of patients after diagnosed with COVID-19 also affected their security, and that the two are closely related. Our results are consistent with Hoyniak et al.'s (49) finding that emotional security is conducive to sleep. A cross-sectional study showed that COVID-19 is associated with changes in sleep schedule and in the quantity and quality of nighttime sleep because of the new stressors, altered roles, and uncertainties about health and economic security (50). Therefore, in the management and nursing of COVID-19 patients in mobile cabin hospitals, from the perspective of improving their security, we should focus on patients with low income and poor sleep quality.
The important role of psychological capital in patients' safety
Psychological capital belongs to the category of positive psychology, which emphasizes individual strength and enthusiasm (51, 52). Our study shows that COVID-19 patients with good psychological capital tend to have a high sense of security, and it is an important predictor of patients' security that can independently explain 18.70% of the variation in security, which is consistent with the results of Eweida et al. (28). In the hierarchical regression analysis of this study, tenacity was not significant in model 2. The reason for this may be that tenacity is a persistent quality that has few impacts on the sense of security. Research shows that individuals with low psychological capital have a low sense of security (53, 54). Psychological capital can buffer the uncertainty, stress, and anxiety of patients in mobile cabin hospitals, which can easily lead to an increase in security (55, 56). Therefore, managers of shelter hospitals can improve patients' security by improving their psychological capital level (28). Medical staff can guide patients to adjust their mentality and help them to adjust their negative emotions, which is conducive to the acquisition of a sense of security. According to Bandura's social cognitive theory, people who have subjective initiative can actively adapt to and change the environment (57). Research shows that mindfulness can improve the level of individual psychological capital (58). Therefore, mindfulness-based cognitive therapy can be conducted for patients in shelters to treat and alleviate their emotional and psychological problems, such as anxiety, depression, and impulsiveness, so as to improve their self-efficacy, hope, and optimism (59, 60). Individuals with a high level of psychological capital are more willing to take initiative and face difficulties and turning points, are more optimistic, confident, and hopeful, and can recover quickly even if they encounter setbacks (61).
Limitations
There are some limitations to our study. Firstly, because of the impact of the pandemic, our research group only conducted a questionnaire survey on COVID-19 patients in the shelter unit within our own management, and we did not investigate the patients in the whole mobile cabin hospital. Secondly, our study was conducted in the form of self-report questionnaires, and the results tended to be subjective. Third, we only preliminarily explored the relationship between the psychological capital and the security of patients, without combining the clusters of security. In future research, we will further explore the relationship between security and psychological capital in combination with the type of security.
Conclusion
Our study explored the characteristics of security among patients with COVID-19 infection in mobile cabin hospitals and its relationship with psychological capital. Based on latent profile analysis, we identified their security as low security (Class 1), moderate security (Class 2), or high security (Class 3), accounting for 12.00, 49.51, and 38.49%, respectively, of the total number of patients. The predictors of COVID-19 patients' security were monthly income per capita in the family, sleep quality, and psychological capital. Psychological capital was an important predictor of security that could independently explain 18.70% of the variation in the patients' security. All these predictive factors are of great significance to improve COVID-19 patients' security, which managers of shelter hospitals should pay attention to.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
CW, J-rY, and C-yH wrote the main manuscript text. H-jL, JW, and C-nH distributed questionnaires. Y-jZ and JD contributed to the writing and revision of articles. Y-wL and Y-hZ contributed to the analysis and processing of data. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Aleem A, Akbar Samad AB, Slenker AK. Emerging Variants of SARS-CoV-2 and Novel Therapeutics Against Coronavirus (COVID-19). StatPearls. Treasure Island, FL: StatPearls Publishing Copyright © (2022).
2. Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet. (2020) 395:1225–8. doi: 10.1016/S0140-6736(20)30627-9
3. El Keshky MES, Basyouni SS, Al Sabban AM. Getting Through COVID-19: the pandemic's impact on the psychology of sustainability, quality of life, and the global economy - a systematic review. Front Psychol. (2020) 11:585897. doi: 10.3389/fpsyg.2020.585897
4. Doraiswamy S, Abraham A, Mamtani R, Cheema S. Use of telehealth during the COVID-19 pandemic: scoping review. J Med Internet Res. (2020) 22:e24087. doi: 10.2196/24087
5. Søreide K, Hallet J, Matthews JB, Schnitzbauer AA, Line PD, Lai PBS, et al. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. Br J Surg. (2020) 107:1250–61. doi: 10.1002/bjs.11670
6. Alizadehsani R, Alizadeh Sani Z, Behjati M, Roshanzamir Z, Hussain S, Abedini N, et al. Risk factors prediction, clinical outcomes, and mortality in COVID-19 patients. J Med Virol. (2021) 93:2307–20. doi: 10.1002/jmv.26699
7. Qin W, Hu BZ, Zhang Z, Chen S, Li FJ, Zhu ZY, et al. Clinical characteristics and death risk factors of severe COVID-19. Zhonghua Jie He He Hu Xi Za Zhi. (2020) 43:648–53. doi: 10.3760/cma.j.cn112147-20200320-00380
8. Sousa Neto AR, Carvalho ARB, Oliveira EMN, Magalhães RLB, Moura MEB, Freitas DRJ. Symptomatic manifestations of the disease caused by coronavirus (COVID-19) in adults: systematic review. Rev Gaucha Enferm. (2021) 42:e20200205. doi: 10.1590/1983-1447.2021.20200205
9. Dong L, Chen L, Ding S. Illness uncertainty among patients with COVID-19 in the Mobile Cabin Hospital. Nurs Open. (2022) 9:1456–64. doi: 10.1002/nop2.924
10. Li H, Lian H, Lin J, Chen K, Lyu Y, Chen Y, et al. Mobile cabin hospital compulsory quarantine for mild patients can serve as an alternative treatment for COVID-19: the Chinese experience. Am J Transl Res. (2022) 14:3132–42.
11. Pan L, Xu Q, Kuang X, Zhang X, Fang F, Gui L, et al. Prevalence and factors associated with post-traumatic stress disorder in healthcare workers exposed to COVID-19 in Wuhan, China: a cross-sectional survey. BMC Psychiatry. (2021) 21:572. doi: 10.1186/s12888-021-03589-1
12. He J, Yang L, Pang J, Dai L, Zhu J, Deng Y, et al. Efficacy of simplified-cognitive behavioral therapy for insomnia(S-CBTI) among female COVID-19 patients with insomnia symptom in Wuhan mobile cabin hospital. Sleep Breath. (2021) 25:2213–9. doi: 10.1007/s11325-021-02350-y
13. Shi F, Li H, Liu R, Liu Y, Liu X, Wen H, et al. Emergency preparedness and management of mobile cabin hospitals in China during the COVID-19 pandemic. Front Public Health. (2021) 9:763723. doi: 10.3389/fpubh.2021.763723
14. Galanti T, Guidetti G, Mazzei E, Zappal, à S, Toscano F. Work from home during the COVID-19 outbreak: the impact on employees' remote work productivity, engagement, and stress. J Occup Environ Med. (2021) 63:e426–32. doi: 10.1097/JOM.0000000000002236
15. Labrague LJ. Psychological resilience, coping behaviours and social support among health care workers during the COVID-19 pandemic: a systematic review of quantitative studies. J Nurs Manag. (2021) 29:1893–905. doi: 10.1111/jonm.13336
16. Putri DU, Tsai YS, Chen JH, Tsai CW, Ou CY, Chang CR, et al. Psychological distress assessment among patients with suspected and confirmed COVID-19: a cohort study. J Formos Med Assoc. (2021) 120:1602–10. doi: 10.1016/j.jfma.2021.02.014
17. Tashakori-Miyanroudi M, Souresrafil A, Hashemi P, Jafar Ehsanzadeh S, Farrahizadeh M, Behroozi Z. Prevalence of depression, anxiety, and psychological distress in patients with epilepsy during COVID-19: a systematic review. Epilepsy Behav. (2021) 125:108410. doi: 10.1016/j.yebeh.2021.108410
18. Zhang XB, Xiao W, Lei J, Li MX, Wang X, Hong YJ, et al. Prevalence and influencing factors of anxiety and depression symptoms among the first-line medical staff in Wuhan mobile cabin hospital during the COVID-19 epidemic: a cross-sectional survey. Medicine. (2021) 100:e25945. doi: 10.1097/MD.0000000000025945
19. Botha E, Gwin T, Purpora C. The effectiveness of mindfulness based programs in reducing stress experienced by nurses in adult hospital settings: a systematic review of quantitative evidence protocol. JBI Database System. Rev Implement Rep. (2015) 13:21–9. doi: 10.11124/jbisrir-2015-2380
20. Liu JJ, Dalton AN, Lee J. The “Self” under COVID-19: Social role disruptions, self-authenticity and present-focused coping. PLoS ONE. (2021) 16:e0256939. doi: 10.1371/journal.pone.0256939
21. Cucoranu IC, Parwani AV, West AJ, Romero-Lauro G, Nauman K, Carter AB, et al. Privacy and security of patient data in the pathology laboratory. J Pathol Inform. (2013) 4:4. doi: 10.4103/2153-3539.108542
22. Freitas M, Rahioui H. Late-life attachment. Geriatr Psychol Neuropsychiatr Vieil. (2017) 15:56–64. doi: 10.1684/pnv.2017.0651
23. Khamisa N, Oldenburg B, Peltzer K, Ilic D. Work related stress, burnout, job satisfaction and general health of nurses. Int J Environ Res Public Health. (2015) 12:652–66. doi: 10.3390/ijerph120100652
24. Awang H, Mansor N, Nai Peng T, Nik Osman NA. Understanding ageing: fear of chronic diseases later in life. J Int Med Res. (2018) 46:175–84. doi: 10.1177/0300060517710857
25. Malik SM, Barlow A, Johnson B. Reconceptualising health security in post-COVID-19 world. BMJ Glob Health. (2021) 6:1675–83. doi: 10.1136/bmjgh-2021-006520
26. Zhang H, Qin S, Zhang L, Feng Z, Fan C. A psychological investigation of coronavirus disease 2019 (COVID-19) patients in mobile cabin hospitals in Wuhan. Ann Transl Med. (2020) 8:941. doi: 10.21037/atm-20-4907
27. Zhao J, Wei G, Chen KH, Yien JM. Psychological capital and university students' entrepreneurial intention in China: mediation effect of entrepreneurial capitals. Front Psychol. (2019) 10:2984. doi: 10.3389/fpsyg.2019.02984
28. Eweida RS, Hamad NI, Abdo R, Rashwan ZI. Cyberbullying among adolescents in Egypt: a call for correlates with sense of emotional security and psychological capital profile. J Pediatr Nurs. (2021) 61:e99–105. doi: 10.1016/j.pedn.2021.05.008
29. Laurence J, Kim HH. Individual and community social capital, mobility restrictions, and psychological distress during the COVID-19 pandemic: a multilevel analysis of a representative US survey. Soc Sci Med. (2021) 287:114361. doi: 10.1016/j.socscimed.2021.114361
30. Alat P, Das SS, Arora A, Jha AK. Mental health during COVID-19 lockdown in India: role of psychological capital and internal locus of control. Curr Psychol. (2021) 1–13. doi: 10.1007/s12144-021-01516-x
31. Valdersnes KB, Eid J, Hystad SW, Nielsen MB. Does psychological capital moderate the relationship between worries about accidents and sleepiness? Int Marit Health. (2017) 68:245–51. doi: 10.5603/IMH.2017.0043
32. Snaedal J. The Helsinki Declaration. Laeknabladid. (2014) 100:135. doi: 10.17992/lbl.2014.03.533
33. Testoni I, Palazzo L, Ronconi L, Rossi G, Ferizoviku J, Morales JRP. The experience of children with a parent suffering from Amyotrophic Lateral Sclerosis during the COVID-19 pandemic. Sci Rep. (2021) 11:16046. doi: 10.1038/s41598-021-95338-3
34. Dai BZ, Zhou LL, Mei YJ. Old age security in rural China: there is a long way to go. Chin Med J. (2013) 126:4348–53.
35. Wang W, Luo X, Zhang C, Song J, Xu D. Can land transfer alleviate the poverty of the elderly? Evidence from Rural China. Int J Environ Res Public Health. (2021) 18:1–15. doi: 10.3390/ijerph182111288
36. Wu S, Xu Z, Zhang Y, Liu X. Relationship among psychological capital, coping style and anxiety of Chinese college students. Riv Psichiatr. (2019) 54:264–8. doi: 10.1708/3281.32545
37. Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. (2020) 287:112934. doi: 10.1016/j.psychres.2020.112934
38. Zhao S, Li Y, Su Y, Sun L. Reliability and validity of the Chinese general social capital scale and its effect on physical disease and psychological distress among Chinese medical professionals. Int J Environ Res Public Health. (2021) 18:6635–48. doi: 10.3390/ijerph18126635
39. Halonen JI, Erhola M, Furman E, Haahtela T, Jousilahti P, Barouki R, et al. The Helsinki Declaration 2020: Europe that protects. Lancet Planet Health. (2020) 4:e503–5. doi: 10.1016/S2542-5196(20)30242-4
40. Jin HR, Kim DW, Jung HJ. Common sites, etiology, and solutions of persistent septal deviation in revision septoplasty. Clin Exp Otorhinolaryngol. (2018) 11:288–92. doi: 10.21053/ceo.2017.01788
41. Shen J, Duan H, Zhang B, Wang J, Ji JS, Wang J, et al. Prevention and control of COVID-19 in public transportation: experience from China. Environ Pollut. (2020) 266(Pt 2):115291. doi: 10.1016/j.envpol.2020.115291
42. Newell S, Jordan Z. The patient experience of patient-centered communication with nurses in the hospital setting: a qualitative systematic review protocol. JBI Database System. Rev Implement Rep. (2015) 13:76–87. doi: 10.11124/jbisrir-2015-1072
43. Milberg A, Friedrichsen M, Jakobsson M, Nilsson EC, Niskala B, Olsson M, et al. Patients' sense of security during palliative care-what are the influencing factors? J Pain Symptom Manage. (2014) 48:45–55. doi: 10.1016/j.jpainsymman.2013.08.021
44. Milberg A, Liljeroos M, Krevers B. Can a single question about family members' sense of security during palliative care predict their well-being during bereavement? A longitudinal study during ongoing care and one year after the patient's death. BMC Palliat Care. (2019) 18:63. doi: 10.1186/s12904-019-0446-1
45. Blenkinsopp J, Snowden N, Mannion R, Powell M, Davies H, Millar R, et al. Whistleblowing over patient safety and care quality: a review of the literature. J Health Organ Manag. (2019) 33:737–56. doi: 10.1108/JHOM-12-2018-0363
46. Millar R, Mannion R, Freeman T, Davies HT. Hospital board oversight of quality and patient safety: a narrative review and synthesis of recent empirical research. Milbank Q. (2013) 91:738–70. doi: 10.1111/1468-0009.12032
47. Azeez TA, Lakoh S, Adeleke AA, Balogun OT, Olanipekun BJ, Olusola FI. Chemoprophylaxis against COVID-19 among health-care workers using Ivermectin in low- and middle-income countries: a systematic review and meta-analysis. Indian J Pharmacol. (2021) 53:493–8. doi: 10.4103/ijp.ijp_117_21
48. Lau LL, Hung N, Go DJ, Ferma J, Choi M, Dodd W, et al. Knowledge, attitudes and practices of COVID-19 among income-poor households in the Philippines: a cross-sectional study. J Glob Health. (2020) 10:011007. doi: 10.7189/jogh.10.011007
49. Hoyniak CP, Bates JE, McQuillan ME, Albert LE, Staples AD, Molfese VJ, et al. The family context of toddler sleep: routines, sleep environment, and emotional security induction in the hour before bedtime. Behav Sleep Med. (2021) 19:795–813. doi: 10.1080/15402002.2020.1865356
50. Gupta R, Grover S, Basu A, Krishnan V, Tripathi A, Subramanyam A, et al. Changes in sleep pattern and sleep quality during COVID-19 lockdown. Indian J Psychiatry. (2020) 62:370–8. doi: 10.4103/psychiatry.IndianJPsychiatry_523_20
51. Corbu A, Peláez Zuberbühler MJ, Salanova M. Corrigendum: positive psychology micro-coaching intervention: effects on psychological capital and goal-related self-efficacy. Front Psychol. (2021) 12:669283. doi: 10.3389/fpsyg.2021.669283
52. Corbu A, Peláez Zuberbühler MJ, Salanova M. Positive psychology micro-coaching intervention: effects on psychological capital and goal-related self-efficacy. Front Psychol. (2021) 12:566293. doi: 10.3389/fpsyg.2021.566293
53. Wu M, Long R, Chen H. Public psychological distance and spatial distribution characteristics during the COVID-19 pandemic: a Chinese context. Curr Psychol. (2022) 41:1065–84. doi: 10.1007/s12144-021-01861-x
54. Ye X, Ren S, Li X, Wang Z. The mediating role of psychological capital between perceived management commitment and safety behavior. J Safety Res. (2020) 72:29–40. doi: 10.1016/j.jsr.2019.12.004
55. Kan D, Yu X. Occupational stress, work-family conflict and depressive symptoms among Chinese bank employees: the role of psychological capital. Int J Environ Res Public Health. (2016) 13:134–45. doi: 10.3390/ijerph13010134
56. Li X, Kan D, Liu L, Shi M, Wang Y, Yang X, et al. The mediating role of psychological capital on the association between occupational stress and job burnout among bank employees in China. Int J Environ Res Public Health. (2015) 12:2984–3001. doi: 10.3390/ijerph120302984
57. Akbari M, Taheri M, Tabaeian SP, Karimi M, Fayazi H, Fayazi N. The effect of E-learning on self-efficacy and sense of coherence of cancer caregivers: application of the bandura and antonovsky social cognitive theory. Curr Health Sci J. (2021) 47:539–46. doi: 10.12865/CHSJ.47.04.09
58. Decuypere A, Audenaert M, Decramer A. When mindfulness interacts with neuroticism to enhance transformational leadership: the role of psychological need satisfaction. Front Psychol. (2018) 9:2588. doi: 10.3389/fpsyg.2018.02588
59. Apolinário-Hagen J, Drüge M, Fritsche L. Cognitive behavioral therapy, mindfulness-based cognitive therapy and acceptance commitment therapy for anxiety disorders: integrating traditional with digital treatment approaches. Adv Exp Med Biol. (2020) 1191:291–329. doi: 10.1007/978-981-32-9705-0_17
60. Hofmann SG, Gómez AF. Mindfulness-based interventions for anxiety and depression. Psychiatr Clin N Am. (2017) 40:739–49. doi: 10.1016/j.psc.2017.08.008
Keywords: latent profile analysis, mobile cabin hospital, patients with COVID-19 infection, security, psychological capital
Citation: Wu C, Yan J-r, He C-y, Wu J, Zhang Y-j, Du J, Lin Y-w, Zhang Y-h, Heng C-n and Lang H-j (2022) Latent profile analysis of security among patients with COVID-19 infection in mobile cabin hospitals and its relationship with psychological capital. Front. Public Health 10:993831. doi: 10.3389/fpubh.2022.993831
Received: 14 July 2022; Accepted: 28 October 2022;
Published: 16 November 2022.
Edited by:
Xue Yang, The Chinese University of Hong Kong, ChinaReviewed by:
Gang Sun, Bloomberg School of Public Health, Johns Hopkins University, United StatesGuohua Zhang, Wenzhou Medical University, China
Copyright © 2022 Wu, Yan, He, Wu, Zhang, Du, Lin, Zhang, Heng and Lang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yu-hai Zhang, emh5aEBmbW11LmVkdS5jbg==; Chun-ni Heng, THZjaGVueWV5ZUAxMjYuY29t; Hong-juan Lang, TGFuZ2hqQGZtbXUuZWR1LmNu
†These authors have contributed equally to this work
 Chao Wu
Chao Wu Jia-ran Yan
Jia-ran Yan Chun-yan He
Chun-yan He Jing Wu
Jing Wu Yin-juan Zhang
Yin-juan Zhang Juan Du
Juan Du Ya-wei Lin
Ya-wei Lin Yu-hai Zhang2*
Yu-hai Zhang2* Chun-ni Heng
Chun-ni Heng Hong-juan Lang
Hong-juan Lang