
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 13 December 2022
Sec. Health Economics
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.986776
This article is part of the Research TopicHealth Economics Disparities, Inequality and Inequity In Healthcare Services: Today's Reality and Tomorrow's ChallengesView all 19 articles
Background: Whenever vaccines for a new pandemic or widespread epidemic are developed, demand greatly exceeds the available supply of vaccine doses in the crucial, initial phases of vaccination. Rationing protocols must then fulfill a number of ethical principles balancing equal treatment of individuals and prioritization of at-risk and instrumental subpopulations. For COVID-19, actual rationing methods used a territory-based first allocation stage based on proportionality to population size, followed by locally-implemented prioritization rules. The results of this procedure have been argued to be ethically problematic.
Methods: We use a formal-analytical approach arising from the mathematical social sciences which allows to investigate whether any allocation methods (known or unknown) fulfill a combination of (ethical) desiderata and, if so, how they are formulated algorithmically.
Results: Strikingly, we find that there exists one and only one method that allows to treat people equally while giving priority to those who are worse off. We identify this method down to the algorithmic level and show that it is easily implementable and it exhibits additional, desirable properties. In contrast, we show that the procedures used during the COVID-19 pandemic violate both principles.
Conclusions: Our research delivers an actual algorithm that is readily applicable and improves upon previous ones. Since our axiomatic approach shows that any other algorithm would either fail to treat people equally or fail to prioritize those who are worse off, we conclude that ethical principles dictate the adoption of this algorithm as a standard for the COVID-19 or any other comparable vaccination campaigns.
When vaccines for the COVID-19 pandemic first became available, countries around the world rushed to secure as many doses as possible, with little or no attempt at coordination (1–5). To mitigate the ensuing chaos, and to provide global, equitable access to vaccines, the World Health Organization (WHO), the Coalition for Epidemic Preparedness Innovations (CEPI), and the Vaccine Alliance (Gavi) proposed the multilateral initiative Covax Facility (COVAX). The European Union also acted on behalf of all its member states (6), and the U.S. allocated vaccines among jurisdictions (7). In those and many other cases, vaccines were centrally acquired and had to be distributed among the territories.
The allocation of a centrally-acquired stock of (scarce) medical resources to individual territories is, however, a complex problem which is encountered in different environments. In the case of COVID-19, the various organizations referred above implemented different procedures on the basis of their political support rather than objective, scientific criteria (8). As a result, an ethical debate erupted, pointing out a number of serious flaws in the implemented procedures (9, 10). For example, some territories received enough vaccines to start inoculating lower-priority groups while other territories were not able to fully immunize higher-priority ones (11, 12). Further, individuals noticed that they would in practice receive higher priority if they simply moved from one territory to the next (13, 14).
According to a prominent strain of the medical ethics literature (15–18), the key ethical desiderata (or “fundamental values”) to take into account when facing the rationing of scarce medical resources are four: “(i) maximizing the benefits produced by scarce resources, (ii) treating people equally, (iii) promoting and rewarding instrumental value, and (iv) giving priority to the worst off” [(17), p. 2051]. If we restrict our attention to the allocation of scarce vaccines, the first and the third fundamental values are relevant to establish the different priority classes. In other words, priority classes should be defined to reflect medical and scientific evidence as, for example, the different effects of treatments on individuals in different health states (12), and practical considerations as those dictating preferential treatment of medical personnel. In contrast, the challenges arising from the distributional aspects of vaccine allocation involve the second and the fourth fundamental values above.
In this contribution, we shed light on these distributional aspects of the allocation of scarce vaccines. In other words, we assume that the priority classes have already been decided (e.g., by experts in medical ethics and organizations like the WHO). The remaining key ethical desiderata are two. First, priority should be given to worse-off groups (as the elderly or otherwise at-risk) and to those with instrumental value (as, e.g., medical personnel). Second, equal people, that is, those with the same priority, should be treated equally, meaning that they should have the same likelihood of being vaccinated.
There exist many frameworks addressing distributional fairness in healthcare (4, 16–22), but they typically remain unspecified, that is, they discuss desiderata but stop short of identifying actual distribution mechanisms. For the case of vaccine allocation, at this point, society needs an allocation procedure or vaccine rationing protocol fulfilling the two key requirements discussed above. That is, higher-priority classes should receive vaccinations before lower-priority ones, and people within the same priority class should be treated equally.
The rationing protocols used to distribute vaccines in the case of COVID-19 failed on all accounts. Indeed, the dispersion in vaccination rates for given priority classes in EU countries was remarkable. In the 12th week of 2021, 99.6% of all healthcare workers were vaccinated (primary course) in Hungary,1 71.5% in Romania, and 66.9% in Estonia, while the rates of fully-vaccinated health care workers were much lower in Denmark (36.8%), Czechia (42.7%), Ireland (54%), or Iceland (21.5%) (Figure 1A). Note that the vaccination rates for the healthcare workers in these countries were near 100% in January 2022, demonstrating that healthcare workers of those countries had a clear preference for being vaccinated, and hence that equal people were far from being treated equally.2
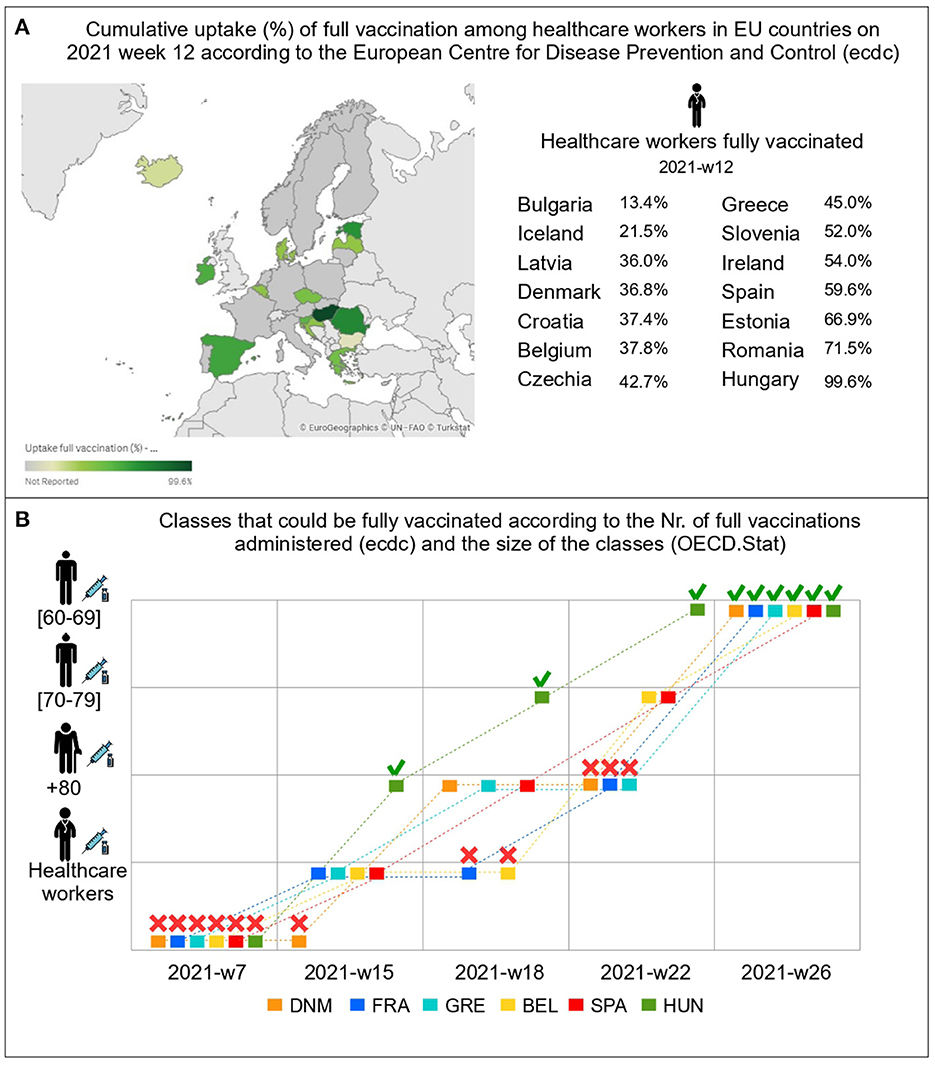
Figure 1. Data and map from the European Center for Disease Prevention and Control (ecdc) and OECD.Stat. (A) shows a high dispersion in the vaccination rates of healthcare workers within the EU in week 12/2021, showing that Prioritizing According To Needs was violated. (B) uses OECD data (Table 1) and shows which priority classes could have been fully immunized at different points in time (2021) according to ecdc data on full vaccinations administered (primary course) in each territory. This exercise shows that Treating Equal People Equally was violated. For example, on week 22nd, beyond the case of Hungary (which decided to buy vaccines from third countries on top of the agreement with the EU), we observe that Belgium and Spain could have started immunizing citizens from 60 to 69 years while France, Greece, or Denmark did not have enough vaccines to have immunized all citizens above 70 years. Icons made by Freepik from Flaticon.
It is also clear that prioritization was violated. Figure 1B reports a simple exercise performed using publicly-available vaccination numbers from the European Center for Disease Prevention and Control and the size of population groups (healthcare workers and age groups) from the OECD (Table 1). Respecting priority means that, say, all healthcare workers in the entire EU should have been vaccinated (or it should have been possible to vaccinate them if willing) before immunization of other classes started, that no 70-year old should be vaccinated before all those aged above 80 were vaccinated in the entire EU, etc. In reality, in week 22, Spain and Belgium had received enough vaccines to vaccinate all healthcare workers and those aged 70 or older, while Denmark, France, and Greece only had received enough to immunize those older than 80, and Hungary already had enough to immunize all above 60. Even ignoring the case of Hungary (which had bought additional vaccines), this illustrates that the allocation protocol did not respect priority classes, as within the same vaccination alliance (the EU) people from lower-priority classes were being immunized while higher-priority classes had still not been fully vaccinated.
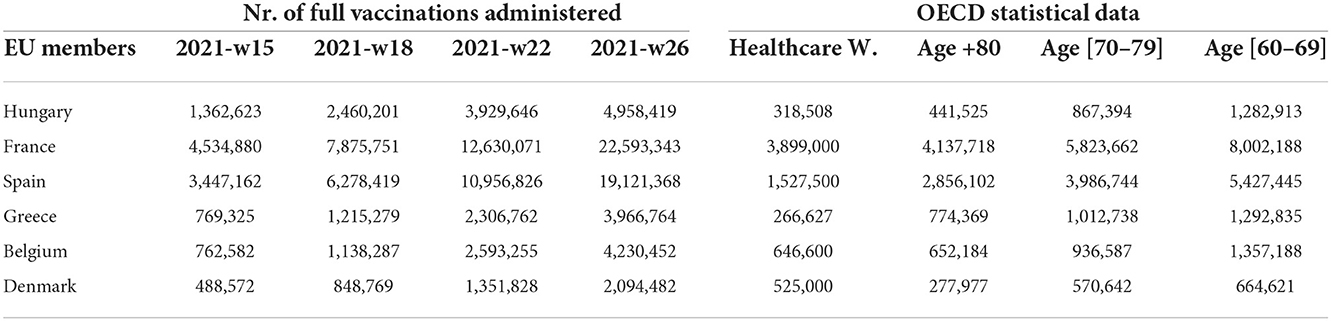
Table 1. Table reporting actual data about full vaccinations administered (primary course) at weeks 15, 18, 22, 26 of 2021 and the population by priority class according to the OECD.Stat.
We make use of the axiomatic approach proper of the mathematical social sciences. Formally, one translates ethical desiderata into analytical properties to be satisfied by protocols (themselves defined as mathematical functions), and then reverse-engineers the protocols fulfilling those properties. Very often, when using this methodology, one ends up with an impossibility theorem which reveals that the desiderata are mutually incompatible or too exacting. In this contribution, we demonstrate that the problem to find a vaccine allocation protocol fulfilling prioritization and equal treatment can be solved analytically. The failures illustrated above were not borne out of lack of competence at any level, or of inefficiency in administering a protocol. Rather, they are inherent failures of the protocols that were used. We show analytically that those protocols cannot fulfill the requirements of prioritization and equal treatment. We go even further and show that there exists one and only one protocol that satisfies both requirements. This means that any other protocol, already-existing or yet-to-be-designed, will either fail to respect priority classes or treat people within the same priority class unequally. This includes all protocols that have been used to distribute vaccinations for the COVID-19 pandemic. We pin down the new protocol to the algorithmic, ready-to-use level, and offer it for use by any vaccine alliance.
Intuitively, the protocol identified by our approach proceeds as follows. First, one must consider the size of the different priority classes jointly across territories, and distribute (on paper) vaccines to classes according to their priorities. Second, for each priority class, one distributes the vaccines to the territories proportionally to the size of the class in each territory. This protocol can be applied to any multi-territory organization, ranging from current multi-jurisdiction countries and alliances to the ideal of a global vaccine distribution (19, 20, 28–30). In contrast, currently-used protocols have been essentially based on an approach where, first, vaccines are allocated to territories proportionally to population (7, 31, 32), and then allocated to classes following priority within each territory (33, 34). As we show below, these methods violate both desiderata described above, and hence are inherently flawed, both technically and ethically.
The formal-analytical proof of the existence and uniqueness result given below is in the Supplementary material.
There are T ≥ 2 territories, indexed by t = 1, …, T, and P priority classes, p = 1, …, P. A total of V > 0 vaccinations are available and must be allocated across territories and priority classes. For simplicity, a “vaccination” refers to a unit containing the number of doses required to immunize a single individual (e.g., two doses for most of the initial COVID-19 vaccinations, one for booster campaigns, etc.).
Territorial authorities report or request the number of vaccinations required for each class in each territory. Denote by the corresponding claim for class p in territory t. Let and be the total claims for class p and territory t, respectively. The total claim is . A Vaccine Rationing Problem appears when C>V, that is, the total claim exceeds the available number of vaccinations and hence the latter must be rationed and distributed across territories and priority classes.
Let be the number of individuals belonging to priority class p in territory t, which is observable through administrative records. Denote by the total population of territory t, and by N = n1 + … + nT the total population across all territories. Obviously, claims are constrained so that for each p and t. To simplify notation, write c and n to denote the matrices containing all and all , respectively.
The solution for Vaccine Rationing Problems is a Vaccine Rationing Protocol which takes as inputs the claims and the population sizes , and delivers as outputs the vaccinations allocated to each p and t, denoted by R(c, V). This is in itself a matrix, that is, given claims and total available vaccinations V, the protocol R allocates vaccinations to priority class p in territory t. The only requirement is that the sum up to V, i.e., all vaccinations are allocated. Formally, every protocol R is a mathematical mapping between well-defined spaces (see Supplementary material A.1). The key of our contribution is that ethical desiderata can be translated into formal properties which such protocols should fulfill, and the axiomatic approach from the mathematical social sciences (see Supplementary material A.3) allows to pin down an exact protocol as the only one which satisfies the desiderata.
Among the ethical desiderata discussed in the introduction, the technical aspects of the requirement to maximize the benefits of scarce vaccinations are already encompassed in the definition of Vaccine Rationing Protocol, and specifically into the condition that the add up to V, that is, no vaccinations are wasted. The requirement to promote and reward instrumental value means that priority classes should take into account professional groups as e.g., clinical or security personnel—since we take the priority classes as given, for our purposes this requirement is subsumed in the requirement to prioritize worse-off groups, which means that classes with higher priority (lower p) should receive vaccinations before the immunization of classes with worse priority starts.
Say that a class in a territory is rationed if it does not fully receive its claim, i.e., , and that it is excluded if it receives zero, i.e., . The requirement that priority classes are honored is the following.
Prioritizing According To Needs. If a class in a territory is rationed, then every class with worse priority (in any territory) is excluded.
Formally, this can be written as follows: If for some p and some t, then for all p′ = p + 1, …, P and for all t′. In other words, if there are not enough vaccinations to immunize all the individuals in a priority class for a given territory, then the protocol must not have allocated vaccinations to any lower-priority class in any territory. The requirement that this holds for any territory is crucial; as we will see below, standard allocation procedures during COVID-19 violated this desideratum.
The second desideratum is that (equal) people should be treated equally. Obviously, it is impossible to treat everybody equally while respecting priority of different classes, and what is actually meant by this desideratum is that two different people belonging to the same class should not face different constraints, and specifically should not be treated differently across territories. To formulate this principle, let the vaccination rate of a priority class be the proportion of people in the class that can be inoculated, given the number of allocated vaccinations, i.e., .
Treating Equal People Equally. The vaccination rates of priority classes do not differ across territories.
Formally, this means that, for every priority class p and any two territories t, t′,
provided and .
The ratios can also be interpreted as the probability of being vaccinated for priority class and territory. Thus, this desideratum implies that individuals cannot increase their vaccination chances by moving from one territory to another.
Generally speaking (as, e.g., in the case of COVAX or the EU), COVID-19 vaccinations were distributed in a two-stage fashion where first vaccinations were allocated to territories (31, 32), and then those allotments were redistributed across the priority classes in each territory (33, 34).
These naïve protocols violate both ethical principles, Prioritizing According To Needs and Treating Equal People Equally. To see this, we first define the procedure sketched above formally. This is a simplified procedure sharing the defining characteristics of the methods actually used in the case of COVID-19, and it suffices to see why such methods are problematic. For this purpose, we describe the procedure used by the European Union to allocate vaccines among their Member States proportionally to their population, with the simplifying assumption that in the second stage all Member States treat the priority classes the same way.
The Territorial Allocation protocol (TA). This protocol, which mimics those actually used for COVID-19 in a simplified way, proceeds as follows (Figure 2A). In the first stage, the available vaccinations V are distributed among the territories proportionally to the territories' population, unless the territorial claim can be fulfilled. Specifically, each territory t receives a total allotment of
where N = n1 + … + nT is the total population across all territories and λ is a constant computed to guarantee that the vaccinations are exhausted, i.e.,
In words, the procedure allocates V proportionally to the population of the territories, but reduces the allocation to the actual claim if that is exceeded, reallocating the excess vaccinations to other territories. Hence, λ is the proportion of the total population that can be vaccinated for those territories that are actually rationed.
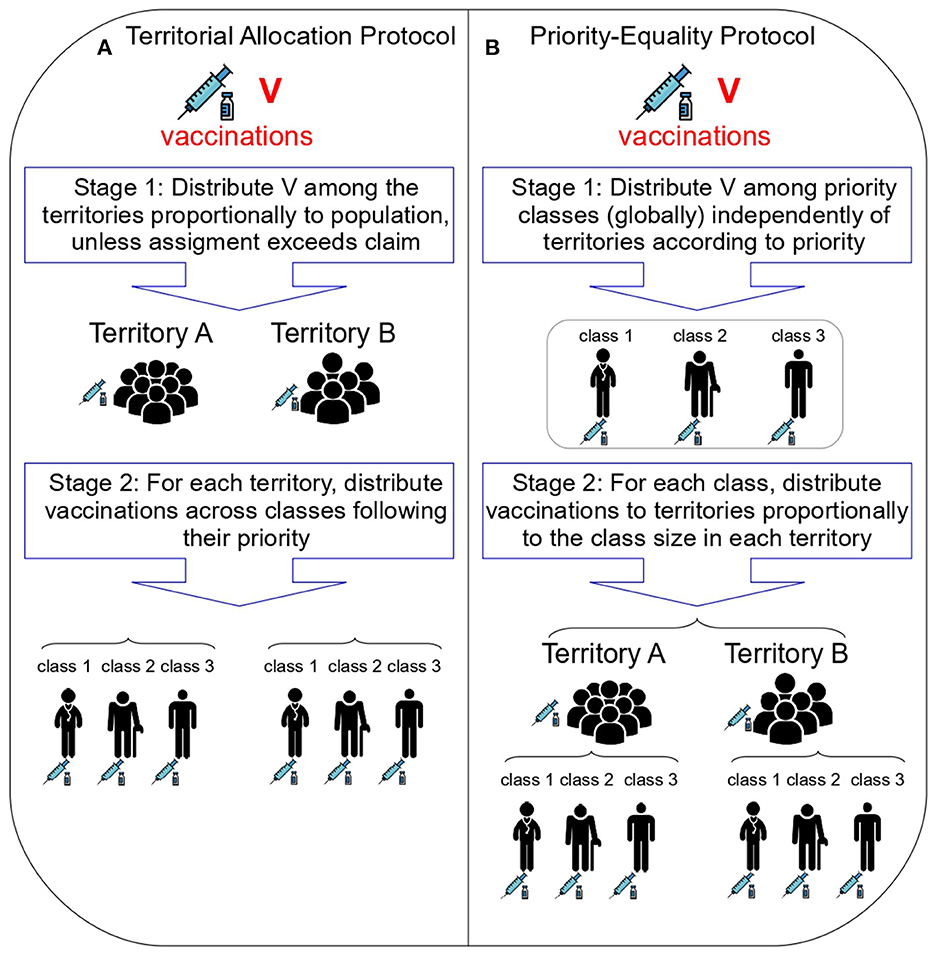
Figure 2. The Territorial Allocation and Priority-Equality protocols. (A) (left) shows the two stages of the Territorial Allocation protocol, which captures the essential features of those actually used for COVID-19. (B) (right) shows the two stages of the Priority-Equality protocol, which we identify in this work as the only one satisfying fundamental ethical principles. Icons made by Freepik from Flaticon.
In the second stage, the TA protocol distributes the allotment Rt(c, V) of each territory t among the priority classes in t following the order of the priority classes. That is, for each territory, the highest-priority class is vaccinated, with the remaining vaccinations (if any) going to the second class, and so on until the doses are exhausted. Formally, let p*(t) be the unique class such that but , i.e., the first class in order of decreasing priority such that available vaccinations in the territory do not allow for full coverage. Then,
This intuitive protocol violates not one but both of the ethical principles described above. To see this a counterexample suffices. Figure 3 shows an example of Vaccine Allocation Problem where the second priority class in a territory receives vaccinations while the first priority class in another territory is still rationed, hence violating Prioritizing According To Needs (Figure 3A). Further, vaccination rates per class are strictly better in the first territory, violating Treating Equal People Equally (Figure 3B).
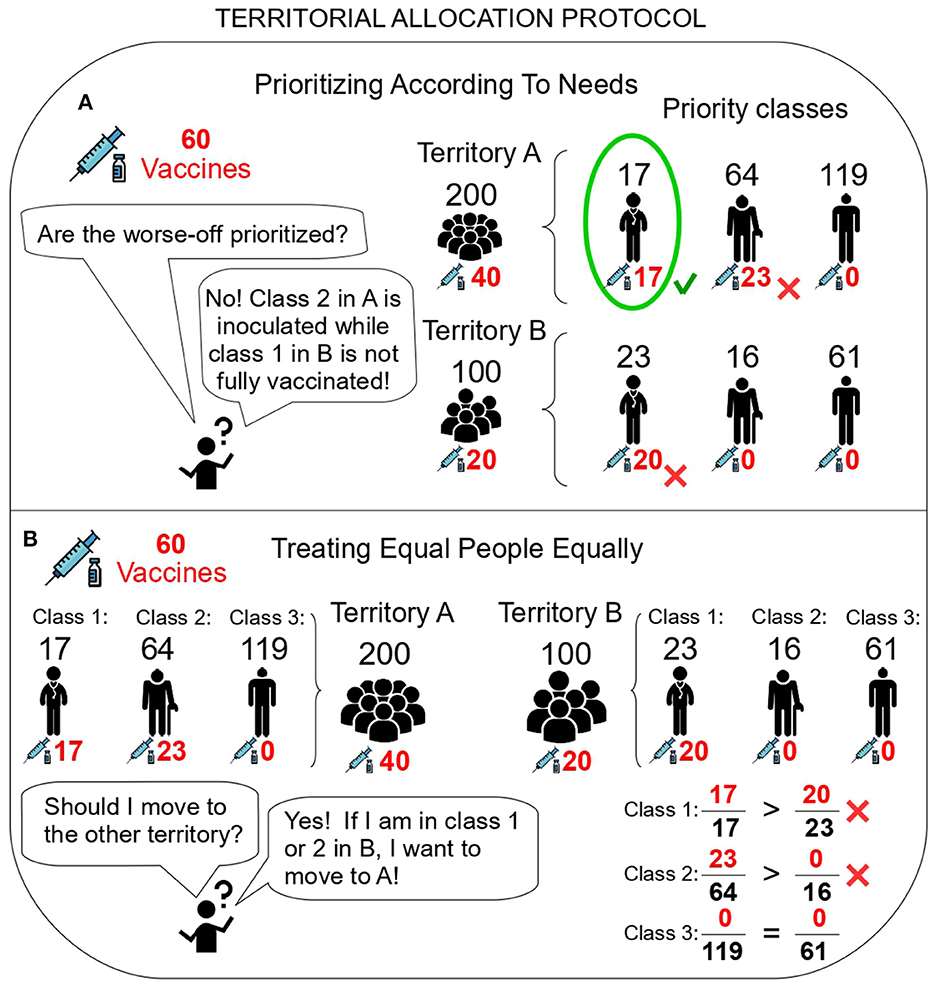
Figure 3. The Territorial Allocation protocol violates ethical principles. (A) The Territorial Allocation protocol violates Prioritizing According To Needs. Territory A receives two thirds of the vaccinations (40), which suffice to fully immunize the first class and partially inoculate the second (, ). Territory B receives one third of the vaccinations (20), which is insufficient to fully immunize the first class (). (B) The Territorial Allocation protocol violates Treating Equal People Equally. For the first and second priority classes, vaccination rates are worse in territory B than in territory A, and hence B-residents belonging to those classes would prefer to move to A. Icons made by Freepik from Flaticon.
Our main result shows that it is possible to satisfy both ethical desiderata. Strikingly, the axiomatic approach actually pins down the protocol (and the algorithm) which makes this possible. In other words, any other conceivable protocol, currently extant or not, will violate one of the principles.
Theorem 1. There exists one and only one Vaccine Rationing Protocol which satisfies Prioritizing According To Needs and Treating Equal People Equally. This is a two-stage procedure as follows:
• Stage 1: Allocate vaccinations to priority classes (globally) independently of territories according to priority.
• Stage 2: For each priority class, reallocate vaccinations across territories proportionally to the size of the class in them.
We refer to this two-stage procedure as the Priority-Equality protocol (PE; Figure 2B). Algorithmically, this protocol is as follows (see Figure 4 for an example). In Stage 1, the available vaccinations V are distributed following the order of the priority classes (without any distinction across territories). That is, the highest-priority class is vaccinated in all territories, with the remaining vaccinations (if any) going to the second class, and so on until the doses are exhausted. Formally, let p* be the unique class such that c1 + … + cp*−1 ≤ V but c1 + … + cp* > V, i.e., the first class in order of decreasing priority such that overall available vaccinations do not allow for full coverage. Then, each class p is allocated
In the second stage, the total allocation to class p, Rp(c, V), is distributed across territories (or, more properly, among their respective p-priority classes). This is done proportionally to the territorial claims for each priority class,
for the classes with cp > 0 [if for any class there were no claims, cp = 0, then for all t].
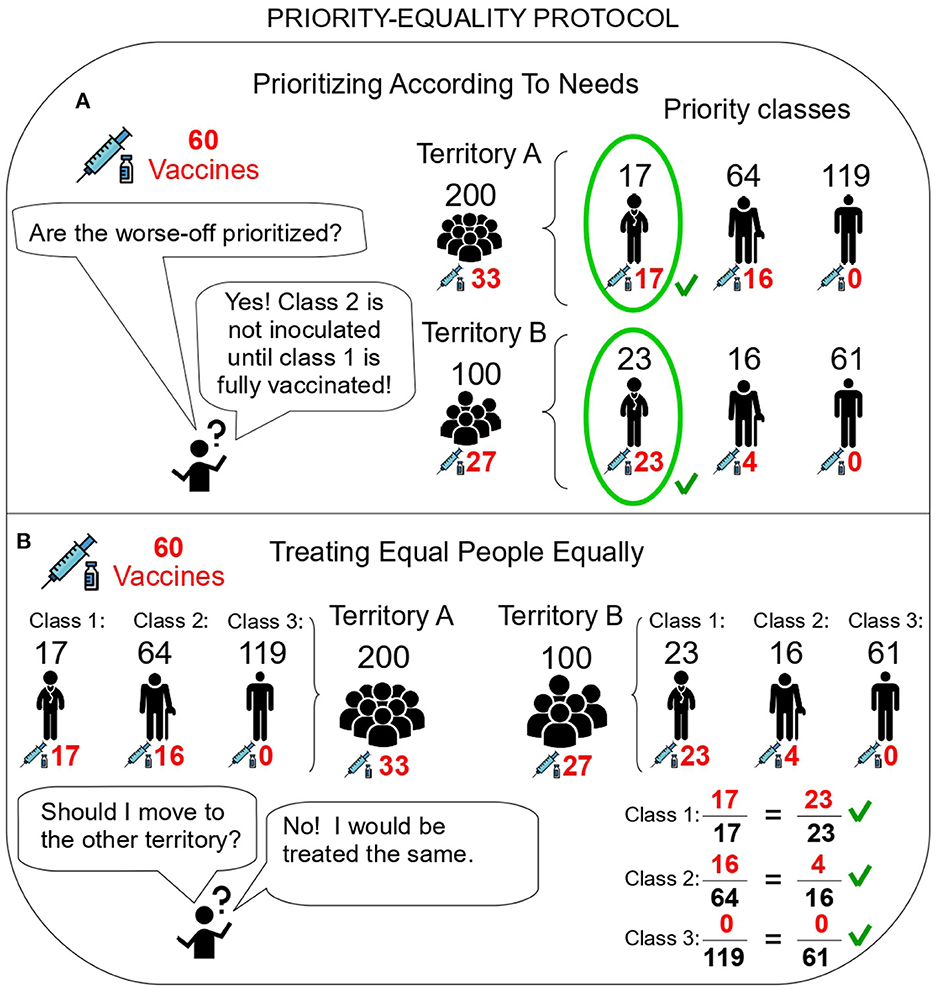
Figure 4. The Priority-Equality protocol satisfies ethical principles. (A) Prioritizing According To Needs. The highest priority class is fully covered in both territories. The remaining vaccinations (20) do not suffice to cover the second priority class, hence that class is rationed in both territories. Other classes are excluded. (B) Treating Equal People Equally. For the second class, vaccinations are allocated proportionally to the size of that class across the territories (, ). Hence, vaccination rates are identical. Icons made by Freepik from Flaticon.
Figure 4 illustrates with an example how this protocol fulfills both desiderata. The mathematical proof of our result is provided in Supplementary material A.2. It first shows that the PE protocol fulfills both desiderata for all problems. Crucially, it then shows that any other hypothetical protocol that also fulfills those must be identical to PE.
It is easy to show that the two fundamental ethical desiderata considered here are logically independent (see Supplementary material A.4). Finally, we remark that the PE protocol also fulfills other appealing properties that the TA protocols violate, e.g., robustness to decentralization, equal treatment of territories with identical claims for a given class, or robustness to sequential vaccination campaigns (see Supplementary material A.5).
We offer a possible approach to the problem of allocating scarce vaccines from an ethical perspective. More concretely, we focus on the prominent work “Fair allocation of scarce medical resources in the time of COVID-19” (17). We restrict our attention to this ethical framework for two reasons. First, this is one of the most influential ethical frameworks in the literature. And second, this framework adapts existing, well-known paradigms for the ethical analysis of the allocation of scarce medical resources (16, 18) to the specific crisis of the COVID-19 pandemic. Our contribution consists in converting the ethical desiderata in this framework into formal axioms to analyze their potential compatibility. Our main result is that they are indeed compatible and single out one and only one protocol, which differs from the previously used ones.
The problem we analyze here is of course not limited to the allocation of vaccines during an epidemic. Rather, the protocol is applicable whenever scarce medical resources need to be allocated across different territories or organizations while respecting the ethical principles of prioritization and equal treatment of equals. More generally, the allocation of scarce medical resources is often decided ad hoc on the basis of heuristic approaches that often oversimplify the problem (35). The protocol we present here is derived from the formal analysis of the constraints arising from universally-appealing ethical principles, and hence provides a more nuanced approach. Of course, this protocol is not a universal recipe to be blindly applied to every ethical allocation dilemma. Our algorithm is well-suited for the normative allocation of scarce resources whenever three conditions are fulfilled. First, the demand exceeds the resources at hand. Second, administrative records of the patients or resource claimants are available. Third, there is an uncontroversial prioritization of the claimants (as decided by medical experts and the legitimate authority on the basis of scientific evidence). Note that these properties can be fulfilled at multiple levels, from allocations across countries in a supranational alliance or across states in a country to those across healthcare areas in a region or between hospitals in a local network.
The present work is complementary to an important strand of the literature that studies how to allocate priority depending on the societal objective function.3 For instance, other studies show that older groups should be vaccinated first if the target is minimizing deaths, but younger groups should be vaccinated earlier if the target is to minimize confirmed cases (37), that the allocation of vaccines among the different sociodemographic groups depends on the stated goal (38), or that infections and economic losses can be minimized combining the optimal vaccine prioritization and the optimal stay-at-home policy (39).
Our approach is, of course, not exempt of limitations. For instance, it has been noted that many rationing methods are too rigid to be applied in very-dynamic crises (40), and this criticism also applies to the protocol we identify. A more important limitation is that, necessarily, our formal approach takes the priority classes and their priority order as given. Our paper does not focus on vaccine prioritization, but rather on territorial and class allocation (fulfilling key ethical principles) given the priority classes. Ultimately, the consequences of the protocol might be judged in conjunction with a given definition of priority classes, which is beyond the scope of our contribution. For instance, one might argue that if healthcare workers are prioritized, the protocol implies allocating (relatively) more vaccines to countries that are already in the fortunate situation of having more healthcare workers per capita. This might be problematic from a deontological perspective, since these countries are already better placed to cope with a health crisis. On the contrary, one might counter that this very same fact makes engaging in a global, worldwide supra-national alliance more politically acceptable for the governments of these favored countries, since they are the ones paying the largest share of the bill at the end of the day. Obviously, the protocol we identify will prescribe different allocations depending on the final prioritization decided by the experts in the field. However, our result is orthogonal to these considerations. We only state that, given the priority classes (which are exogenously given and ideally determined by medical experts), there exists one and only one algorithm that allocates vaccines satisfying the ethical desiderata. If a given definition of priority classes is changed on the basis of ethical or political arguments, the ethical principles we discuss still pin down the same algorithm for vaccine allocation across the territories and the new classes.
A further limitation is that our work concentrates on the implications of specific ethical desiderata (17) for allocation procedures. Of course, a myriad of other dimensions are important in practice, ranging from logistic considerations to political constraints. However, it is important to understand that our result is a full characterization. Suppose that one considered some other, further desideratum to be crucial, e.g., arising from political or logistical considerations. Since there is one and only procedure satisfying the two key ethical desiderata, the question of whether there is a procedure satisfying those desiderata and also the additional one is immediately solved: if the PE protocol fulfills that desideratum, the answer is positive. If the PE protocol fails this further desideratum, the answer is negative.
Hence, our result can be seen as either good news or bad news. On the one hand, there exists a procedure fulfilling the fundamental ethical desiderata identified by a wide consensus. On the other hand, there exists only one such procedure, and hence adding any further constraints or wishes is likely to result in an impossibility theorem. We see our result mostly on the positive side. First, it shows that the allocation of scarce medical resources to multi-territorial areas (from medical districts to the whole planet) under priority constraints is feasible while respecting ethical principles. This does not mean that the implementation of such allocations will be logistically simple or politically uncontroversial. The result shows possibility, and hence hope that other difficulties can be overcome. Second, not all possible, additional desiderata will affect the allocation in itself. For example, logistical considerations might impose constraints on which specific vaccine batches can be allocated to which territories, or on the exact timing of delivery. However, if such difficulties can be overcome without affecting the allocation totals derived from the procedure, the properties of the allocation in itself are unaffected. That is, some additional (but of course important) dimensions of the allocation problem might concern implementation and be orthogonal to the properties considered here.
We show that elementary ethical desiderata can be fulfilled by Vaccine Rationing Protocols. This was by no means a given. The mathematical social sciences are ripe with examples where putting together a number of desiderata results in an impossibility theorem, as (to cite but one example) the celebrated Arrow's impossibility theorem (41) which shows that there exists no democratic voting method fulfilling a number of innocent-looking, ethically-appealing properties.
Our result actually pins down a protocol. If several protocols fulfilled the ethical desiderata, we would have opened Pandora's box and started a discussion about the relative virtues of one or another protocol. On the contrary, there exists only one protocol fulfilling the targeted properties. Using any other protocol, or any variant of PE (no matter how seemingly small the deviation) will result in a procedure which violates either Prioritizing According to Needs or Treating Equal People Equally. Hence, as long as those principles are deemed desirable, the protocol we identify shows the only way to implement them. It is important to note that the protocol is algorithmic and readily implementable. Our analysis provides not a discussion of a framework, but an actual method, down to the specific computations, ready to be implemented out of the box.
Our results lead to immediate recommendations. If decision makers wish to implement the ethical principles reflected by Prioritizing According to Needs and Treating Equal People Equally, currently-used allocation protocols as the Territorial Allocation protocol need to be replaced by the Priority-Equality protocol. This creates the need for territorial authorities to formally agree to the protocol and its implementation. Of course, this will be easier for certain territorial alliances (states within a single country) than others (heavily decentralized multinational entities).
We conclude by remarking that our algorithm is a general tool to allocate any scarce medical resources, including of course vaccines but also newly-developed, expensive treatments, or preventive treatments from a national stockpile (e.g., iodine pills in the face of nuclear threats).
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
CA-F, JG-S, and MG-V conceptualized the project, proposed the formal model, and drafted the paper. CA-F and JG-S revised the manuscript and added examples based on real data. All authors contributed to the article and approved the submitted version.
JG-S received financial support from Universitat Jaume I and Generalitat Valenciana under the Grants UJI-B2020-16 and AICO/2021/005.
We thank Eurogeographics, FAO, and TurStat for the permission for using the map included in Figure 1.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.986776/full#supplementary-material
1. ^Starting in February 2021, Hungary decided to buy Sputnik V and Sinopharm vaccines from Russia and China, respectively (23, 24), considering that the EU scheme was too slow. This helps explain both the high rate of vaccinated healthcare workers on the 12th week of 2021 as well as Hungary's high performance, in Figure 1B, in terms of the classes that each country could have immunized at every point in time along the year 2021. We thank an anonymous referee for this insightful comment.
2. ^In the 12th week of 2021, Bulgaria had a rate of only 13.4% fully-vaccinated healthcare workers. However, this rate was still 28.7% in early March 2022, suggesting that Bulgaria's issue is orthogonal to these considerations, and most likely related to the widespread vaccine hesitancy in this country (25–27).
3. ^Other works look at more operational aspects of vaccine distribution. For example, the optimal number of doses to hold in an inventory (36).
1. Kupferschmidt K. Vaccine nationalism' threatens global plan to distribute COVID-19 shots fairly. Science. (2020) 28. doi: 10.1126/science.abe0601
2. Moon S, Alonso Ruiz A, Vieira M. Averting future vaccine injustice. N Engl J Med. (2021) 385:193–6. doi: 10.1056/NEJMp2107528
3. Bollyky TJ, Bown CP. The tragedy of vaccine nationalism: only cooperation can end the pandemic. Foreign Affairs. (2020) 99:96.
4. Ranabhat CL, Jakovljevic MM, Kim CB. COVID-19 pandemic: an opportunity for Universal Health Coverage? Front Public Health. (2021) 9:673542. doi: 10.3389/fpubh.2021.673542
5. Hinnant L, Cheng M, Ghosal A. Vaccine Inequity: Inside the Cutthroat Race to Secure Doses. AP News (2021). Available online at: https://apnews.com/article/coronavirus-vaccine-inequality-dac9c07b324e29d3597037b8dc1d908a.html (accessed April 22, 2022).
6. European Commission. Commission Decision C(2020) 4192 of 18.6.2020 on Approving the Agreement with Member States on Procuring COVID-19 Vaccines on Behalf of the Member States and Related Procedures. (2020).
7. Center for Disease Control Prevention. How COVID-19 Vaccines Get to You. (2021). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/distributing.html (accessed April 18, 2022).
8. Emanuel EJ, Persad G, Kern A, Buchanan A, Fabre C, Halliday D, et al. An ethical framework for global vaccine allocation. Science. (2020) 369:1309–12. doi: 10.1126/science.abe2803
9. Herzog LM, Norheim OF, Emanuel EJ, McCoy MS. Covax must go beyond proportional allocation of COVID vaccines to ensure fair and equitable access. BMJ. (2021) 372:m4853. doi: 10.1136/bmj.m4853
10. Pak A, Adegboye OA, Adekunle AI, Rahman KM, McBryde ES, Eisen DP. Economic consequences of the COVID-19 outbreak: the need for epidemic preparedness. Front Public Health. (2020) 8:241. doi: 10.3389/fpubh.2020.00241
11. Holder J, Schoenfeld Walker A. Many Older Americans Still Aren't Vaccinated, Making the Delta Wave Deadlier. The New York Times (2021). Available online at: https://www.nytimes.com/interactive/2021/08/24/world/vaccines-seniors.html (accessed April 29, 2022).
12. Schmidt H, Weintraub R, Williams MA, Miller K, Buttenheim A, Sadecki E, et al. Equitable allocation of COVID-19 vaccines in the United States. Nat Med. (2021) 27, 1–10. doi: 10.1038/s41591-021-01379-6
13. Business Insider. Vaccine Tourists are Traversing the US to Get a COVID-19 Shot. Here Are 4 States Treating Visitors. (2021). Available online at: https://www.businessinsider.com/4-states-vaccinating-out-of-staters-and-part-time-residents-2021-2.html (accessed April 22, 2022).
14. El Diario. Pasar a Francia para vacunarse antes: “Asítenemos un verano más tranquilo”. (2021). Available online at: https://www.eldiario.es/euskadi/pasar-francia-vacunarse-verano-tranquilo_1_8064305.html (accessed October 8, 2022).
15. Biddison LD, Berkowitz KA, Courtney B, De Jong CMJ, Devereaux AV, Kissoon N, et al. Ethical considerations: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. (2014) 146:e145S–55S. doi: 10.1378/chest.14-0742
16. Emanuel EJ, Wertheimer A. Who should get Influenza vaccine when not all can? Science. (2006) 312:854–5. doi: 10.1126/science.1125347
17. Emanuel EJ, Persad G, Upshur R, Thome B, Parker M, Glickman A, et al. Fair allocation of scarce medical resources in the time of COVID-19. N Engl J Med. (2020) 382:2049–55. doi: 10.1056/NEJMsb2005114
18. Persad G, Wertheimer A, Emanuel EJ. Principles for allocation of scarce medical interventions. Lancet. (2009) 373:423–31. doi: 10.1016/S0140-6736(09)60137-9
19. Jecker NS, Wightman AG, Diekema DS. Vaccine ethics: an ethical framework for global distribution of COVID-19 vaccines. J Med Ethics. (2021) 47:308–17. doi: 10.1136/medethics-2020-107036
20. Jecker NS, Atuire CA, Bull SD. Towards a new model of global health justice: the case of COVID-19 vaccines. J Med Ethics. (2022). doi: 10.1136/medethics-2022-108165. [Epub ahead of print].
21. Lavazza A, Garasic MD. What if some patients are more “important” than others? A possible framework for COVID-19 and other emergency care situations. BMC Med Ethics. (2022) 23:24. doi: 10.1186/s12910-022-00763-2
22. Pilkington V, Keestra SM, Hill A. Global COVID-19 vaccine inequity: failures in the first year of distribution and potential solutions for the future. Front Public Health. (2022) 10:821117. doi: 10.3389/fpubh.2022.821117
23. Vokó Z, Kiss Z, Surján G, Surján O, Barcza Z, Pályi B, et al. Nationwide effectiveness of five SARS-CoV-2 vaccines in Hungary—the HUN-VE study. Clin Microbiol Infect. (2022) 28:398–404. doi: 10.1016/j.cmi.2021.11.011
24. Bíró-Nagy A, Szászi ÁJ. The roots of COVID-19 vaccine hesitancy: evidence from Hungary. J Behav Med. (2022). doi: 10.1007/s10865-022-00314-5. [Epub ahead of print].
25. Boytchev H. Covid-19: Why the Balkans' vaccine rollout lags behind most of Europe. BMJ. (2021) 375:n2412. doi: 10.1136/bmj.n2412
26. Gomez J. COVID in Europe: Bulgaria's Vaccination Rate is the Lowest in the EU. Euronews (2022). Available online at: https://www.euronews.com/2021/12/10/covid-in-europe-bulgaria-s-vaccination-rate-is-the-lowest-in-the-eu (accessed March 1, 2022).
27. Rankin J. Putting Lives at Risk: Bulgaria Referred to Rights Body Over COVID Vaccine Rollout. The Guardian (2022). Available online at: https://www.theguardian.com/world/2022/jan/25/putting-lives-at-riskbulgaria-referred-to-rights-body-over-covid-vaccine-rollout (accessed March 1, 2022).
28. Herlitz A, Lederman Z, Miller J, Fleurbaey M, Venkatapuram S, Atuire C, et al. Just allocation of COVID-19 vaccines. BMJ Global Health. (2021) 6:e004812. doi: 10.1136/bmjgh-2020-004812
29. Bassi LL. Allocating COVID-19 vaccines globally: an urgent need. JAMA Health Forum. (2021) 2:e210105. doi: 10.1001/jamahealthforum.2021.0105
30. Mamani H, Chick SE, Simchi-Levi D. A game-theoretic model of international influenza vaccination coordination. Manage Sci. (2013) 59:1650–70. doi: 10.1287/mnsc.1120.1661
31. GAVI The The Vaccine Alliance. COVAX Explained. (2021). Available online at: https://www.gavi.org/vaccineswork/covax-explained (accessed May 3, 2022).
32. European Commission. Questions & Answers on Vaccine Negotiations. (2021). Available online at: https://ec.europa.eu/commission/presscorner/detail/en/QANDA_21_48 (accessed April 19, 2022).
33. World Health Organization. Guidance on Developing a National Deployment and Vaccination Plan for COVID-19 Vaccines: Interim Guidance.
34. European Commission. Questions Answers on COVID-19 Vaccination in the EU. (2021). Available online at: https://ec.europa.eu/info/live-work-travel-eu/coronavirus-response/safe-covid-19-vaccines-europeans/questions-and-answers-covid-19-vaccination-eu_en (accessed April 11, 2022).
35. Baltussen R, Niessen L. Priority setting of health interventions: The need for multi-criteria decision analysis. Cost Effect Resource Allocat. (2006) 4:1–9. doi: 10.2139/ssrn.943814
36. Shumsky RA, Smith J, Hoen A, Gilbert M. Allocating COVID-19 vaccines: save one for the second dose? (2021) 3816200. doi: 10.2139/ssrn.3816200
37. Chen X, Li M, Simchi-Levi D, Zhao T. Allocation of COVID-19 vaccines under limited supply. (2020) 3678986. doi: 10.2139/ssrn.3678986
38. Ferranna M, Cadarette D, Bloom DE. COVID-19 vaccine allocation: Modeling health outcomes and equity implications of alternative strategies. Engineering. (2021) 7:924–935. doi: 10.1016/j.eng.2021.03.014
39. Babus A, Das S, Lee S. The Optimal Allocation of COVID-19 Vaccines. CEPR Discussion Paper No. DP15329. (2020). doi: 10.1101/2020.07.22.20160143
40. White DB, Lo B. A framework for rationing ventilators and critical care beds during the COVID-19 pandemic. JAMA. (2020) 323:1773–4. doi: 10.1001/jama.2020.5046
Keywords: rationing, vaccines, COVID-19, pandemics, medical ethics
Citation: Alós-Ferrer C, García-Segarra J and Ginés-Vilar M (2022) Ethical allocation of scarce vaccine doses: The Priority-Equality protocol. Front. Public Health 10:986776. doi: 10.3389/fpubh.2022.986776
Received: 01 August 2022; Accepted: 17 November 2022;
Published: 13 December 2022.
Edited by:
Aviad Tur-Sinai, Max Stern Academic College of Emek Yezreel, IsraelReviewed by:
Luca Valera, University of Valladolid, SpainCopyright © 2022 Alós-Ferrer, García-Segarra and Ginés-Vilar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Carlos Alós-Ferrer, Y2FybG9zLmFsb3MtZmVycmVyQGVjb24udXpoLmNo
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.