- 1The Second Affiliated Hospital, China Medical University, Shenyang, China
- 2School of Public Health, Shandong University, Jinan, China
- 3School of Pharmaceutical Sciences, Jiangxi University of Traditional Chinese Medicine, Nanchang, China
- 4The Fourth Affiliated Hospital, Harbin Medical University, Harbin, China
- 5The Third Clinical Department, China Medical University, Shenyang, China
- 6School for Policy Studies, University of Bristol, Bristol, United Kingdom
- 7Affiliated Hospital of Integrated Traditional Chinese and Western Medicine, Nanjing University of Traditional Chinese Medicine, Nanjing, China
- 8School of Basic Medical Sciences, Shandong University, Jinan, China
- 9Department of Health Communication, Chinese Center for Health Education, Beijing, China
- 10School of Public Health, Peking University, Beijing, China
Objective: Cigarettes have become the the biggest killer of contemporary female's health and beauty. What kind of health information is suitable for the general public is an important issue to be discussed globally. The purpose of this study is to generate systematic, rigorous, public-demand-oriented and appropriate core information relevant to tobacco control based on the best available evidence, combined with audience preferences and pre-dissemination content review from multidisciplinary expertise in order to improve the effectiveness of health communication of tobacco control.
Methods: Relevant systematic reviews meta-analysis that reported smoking on risks of female disease were identified by searching PubMed, Embase, the Cochrane Library, Web of Science, Clinical Trials.gov, and the International Clinical Trial Registry Platform. The Grading of Recommendations Assessment, Development and Evaluation (GRADE) process was applied to assess the evidence in order to make rigorous core information. The audience prevalence survey was conducted to ensure that core information was targeted and tailored. Finally, the expert assessment was used for a pre-dissemination content review and to evaluate whether the core information was appropriate or not.
Results: The final core information consisted of eight parts concerning the effects of smoking and female cardiovascular disease, diabetes, rheumatoid arthritis, respiratory disease, digestive system disease, mental disease, non-pregnant female reproductive system disease, as well as pregnant women and their fetuses. A total of 35 items of core information suitable for dissemination was included and the quality of evidence, the degree of public demand and the outcome of pre-dissemination content review were reported.
Conclusion: The core information related to female cardiovascular system diseases, as well as liver cancer and upper gastrointestinal cancer is the preferred content for health communication of tobacco control. The quality of evidence for core information related to pregnant women and their infants, as well as diseases of reproductive system, respiratory system, and diabetes needs to be improved to meet high public demand. The core information related to mental disease is more suitable for dissemination to patients with mental illness than to the general public. Besides, dissemination of core information should be individualized. Evidence-based Core Information for Health Communication of Tobacco Control would be helpful to provide evidence support for health communication related to tobacco control and enhance public health literacy for international communities that have high smoking prevalence and related disease burden.
Introduction
The sheer number of dieases and deaths caused by tobacco underscores the importance of tobacco control as an urgent global health priority (1–5), especially for women, with their special physiological conditions which are different from males, the harm of smoking to them deserves more attention (6–14). The nicotine in tobacco can reduce the production of estrogen in women, which can lead to disorders in the body and the development of tumors (10, 11). And smoking can significantly reduce activated immune cells and lymphocytes, thereby reducing the immunity of the reproductive tract, increasing the risk of female gynecological diseases, and adversely affecting reproduction (12). The magnitude of change in trends in female smoking prevalence over the past 20 years signifies that female prevalence has not changed significantly since 2000 in most countries, or declined by < 10 percentage points (6, 7). Recently, a global smoking epidemic data shows that female smoking prevalence was 34–40% in Pacific Island countries (Nauru, Micronesia, Kiribati), 10–19% in several OECD (the Organization for Economic Co-operation and Development) countries (Canada, the USA, the UK, Australia and New Zealand) as well as many countries in Western Europe, and < 2–3% in several countries in Africa, as well as Tajikistan and Sri Lanka (6, 7).
Substantial global effort was devoted to curtailing the tobacco epidemic over the past two decade (15), including health communication for tobacco control which is an important part of tobacco control measures (e.g., tobacco pictorial health warnings, point-of-sale health communication campaigns, tobacco prevention education campaigns in university, media campaigns for tobacco control, interpersonal communication in tobacco control campaigns) (16–20), the pace of progress in reducing smoking prevalence has been with little success due to heterogeneous across development status, public literacy and age (21) as well as complicated evidence (7).
As demonstrated by GBD 2015 Tobacco Collaborators (21), countries with higher SDI (Socio-demographic Index) have higher prevalence of daily smoking and age patterns varied more by SDI. Female smoking prevalence typically peaked around age 25 years for high and high-middle SDI countries, while prevalence generally increased until age 60 years in low to middle SDI countries (21). This reminds us that tailored tobacco control health communication strategies (22–24) need to be adopted for different development status, public literacy and age pattern. Furthermore, health communication of tobacco control requires systematic, rigorous, targeted and appropriate evidence on smoking level. To meet this demand in the context of health communication, we propose “core information,” an unprecedented concept. Core information is condensed and suitable health information to be provided to health workers for dissemination to the public. Its development refers to the methods of evidence formation from WHO handbook, based not only on the best available evidence, but also on audience preferences and pre-dissemination content review from multidisciplinary expertise.
Therefore, the Evidence-based Core Information for Health Communication of Tobacco Control is formed in order to improve the effectiveness of health communication of tobacco control and subsequently reduced smoking prevalence, risks of related disease. It will also be helpful to enhance public health literacy for international communities that have high smoking prevalence and related disease burden.
Methods
Preliminary research basis for core information
This study was supposed to develop according to the methods of evidence formation from WHO handbook (25). The study followed the latest definition of evidence formation of Institute of Medicine(IOM) (26, 27) and conformed to the requirements for evidence in Reporting Items 2.0 for Practice Guidelines in Healthcare(RIGHT) (28), the RIGHT statement (29) and Appraisal Of Guidelines For Research & EvaluationII(AGREE II) (30). The technical route for development of Evidence-based Core Information for Health Communication of Tobacco Control is shown in Figure 1.
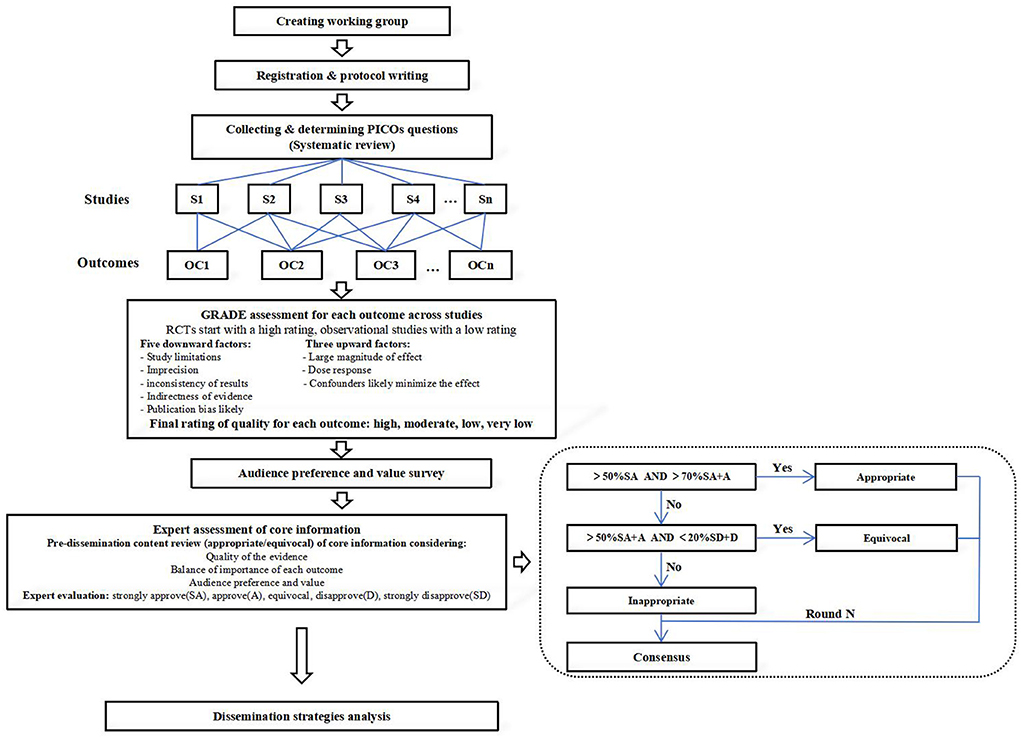
Figure 1. The technical route for development of Evidence-based Core Information for Health Communication of Tobacco Control.
This study was initiated by the Health Communication Working Committee of the Chinese Medical Doctor Association, with methodological support provided by the Drug Evaluation Center of Peking University School of Medicine, and academic support provided by China Smoking Control Association, Beijing Smoking Control Association and other units. And this project was registered on the International Practice Guidelines Registry Platform (http://www.guidelines-registry.org/). The registration number was IPGRP-2020CN072.
Guideline evidence
Literature search and screening
PICOs (participants, female; interventions (equivalent to exposure), smoking; comparisons, smokers vs. non-smokers; outcomes, incidence and mortality of various diseases; study types, systematic reviews) questions (10) followed literature pre-retrieving, International guideline reference and consulting with clinicians, clinical pharmacists, nurses, behavioral epidemiologists and health communication workers. Then the search strategy was determined through the final PICOs questions. To ensure the comprehensiveness of the evidence, we searched PubMed, Embase, and Web of Science, which are recognized as authoritative medical databases worldwide. The Cochrane Library was searched for evidence-based medical literature. Considering unpublished studies and their study details, we also searched Clinical Trials.gov and the International Clinical Trial Registry Platform. The retrieval time was from database construction to February 2021. The search formula consisted of keywords related to smoking and related diseases. Taking smoking and cardiovascular disease in women as an example, the search terms included: (cigarette OR cigarettes OR tobacco OR smoking OR smoking) AND (hypertension OR blood pressure) OR cancer OR (CVD OR cardiovascular disease OR coronary cardiovascular disease OR coronary heart disease). The language of the publication was Chinese or English and systematic reviews and meta-analysis were included. References and gray literature information (i.e., non-published literature, e.g., non-published government literature, dissertations, etc.) of the included literature were also manually searched and screened. The literature screening process was completed independently by two trained researchers. If there was a disagreement, a third researcher would join the discussion to reach a consensus.
GRADE accessment
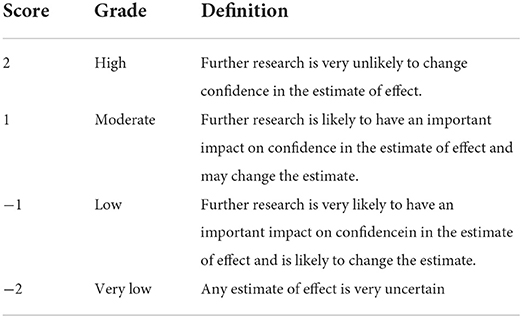
The GRADE (Grade Recommendations Assessment, Development, and Evaluation) tool (31) was used to evaluate the quality of evidence in order to make rigorous core information (For specific implementation content, see Supplementary material 1). The evidence quality was divided into four levels: high, medium, low and very low (Table 1), considering five downward factors (study limitations, imprecision, inconsistency of results, indirectness of evidence and publication bias likely) and three upward factors (large magnitude of effect, dose effect and confounders likely minimize the effect) (Figure 1 and Supplementary material 1).
Audience preference and value survey
The core information development group conducted an audience preference and value survey on the content of the core information (For specific implementation content, see Supplementary material 2). 670 participants was recruited, taking into account the distribution of age, gender, education level, occupation, smoking situation and chronic diseases in line with socio-demographic characteristics. Researchers of the development group explained the background and necessity of core information and discussed them with participants (32). Participants rated the core information using the Likert Level 5 scale: 5 for very necessary, 4 for necessary, 3 for equivocal, 2 for unnecessary, and 1 for very unnecessary. the mean ± standard deviation of each core information and the overall were calculate. The mean ± standard deviation of the overall was 3.10 ± 0.10, based on which, the degree of public demand was divided into four levels: low, medium, high and very high (Table 2). Finally, the results were formed and summarized and analyzed to provide reference for expert assessment group.
Expert assessment of core information
Expert assessment process: An expert assessment survey (For specific implementation content, see Supplementary material 3) was used for the pre-dissemination content review and to evaluate whether the core information was appropriate or not based on quality of evidence, audience preferences and values, balance of importance of each outcome, equity, feasibility, acceptability etc. After two rounds of evaluation and modification of core information, the final version of core information suitable for dissemination was reached (see Table 5 in Supplementary material 3) (33).
The experts participating in this survey were distributed across the country, including 32 multidisciplinary experts whose professional level was high (see Table 2 in Supplementary material 3). They voted anonymously through the Chinese online ‘Questionnaire Star' platform. This process was monitored by the guideline development group. If the voting ratio of “5” was more than 50% and the voting ratio of “5” + “4” was more than 70%, the item was appropriate; if the voting ratio of “5” + “4” was more than 50% and the voting ratio of “2” + “1” was < 20%, the item was equivocal (Figure 1) (29). In the remaining cases, it was deemed inappropriate.
Results
Summary of core information
The correlation between smoking and risks of non-pregnant female reproductive system disease
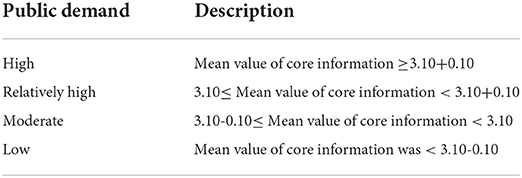
Female reproductive system diseases mainly include gynecological inflammation, gynecological tumors, menstrual disorders and infertility, which bring both physical and mental effects to women and seriously reduce their quality of life. According to WHO global report on trends in prevalence of tobacco use 2000-2025, there were as many as 244 million women using tobacco in 2018 (30). It has been shown that cigarette smoke contains a variety of toxins that affect reproductive function to varying degrees (10), and smoking is therefore considered to be an important factor in the increased prevalence and mortality of female reproductive disorders (31–38)(For summary of evidence, see Supplementary material 1). Our study found that the degree of public was concentrated in “Moderate” and “Relatively High,” but the quality of evidence needed to be improved to meet the general public demand (Table 3). The core information in this field can be used as the content of tobacco control health communication. The specific summary of core information of female reproductive system disease is shown in Table 3.
Effects of smoking on pregnant women and their fetuses
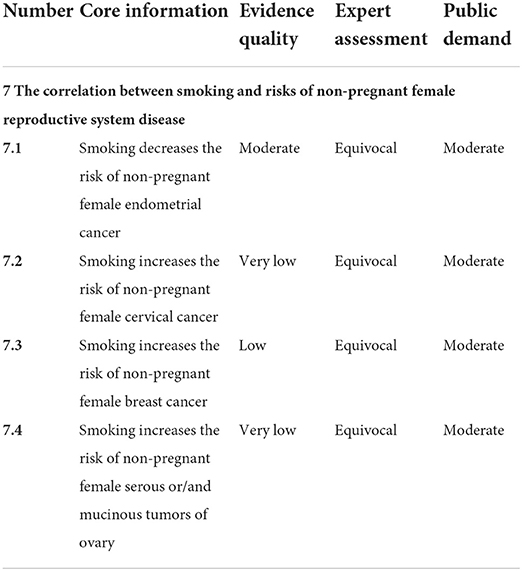
Considering that pregnancy is a special period for women, pregnant women and fetuses are more susceptible to external influences during this period. Studies have shown that prenatal exposure to maternal smoking during pregnancy is harmful to mothers and fetuses (10, 39–44), including congenital heart disease, schizophrenia, attention deficit and hyperactivity disorder in the fetus as well as postpartum depression, coronary heart disease, abnormal pregnancy and all stages of reproduction in pregnant women. Our study revealed that the public had the greatest demand for core information in this field, but the quality of evidence needed to be improved (Table 4). The core information in this field can be used as the content of tobacco control health communication.
The correlation between smoking and risks of female respiratory disease
Of all risk factors, Smoking is the leading risk factor for chronic respiratory diseases, For women, the leading cause of smoking-attributable DALYs is COPD (21). Evidences found that female current smokers had with increasing age (especially beyond age 45 to 50 years in the pre and post menopausal periods) a significantly faster annual decline in FEV1% (a golden indicator of COPD) predicted than male current smokers (linear regression analysis, R2 = 0.56; p = 0.008), and this trend was evident even in female smokers who smoked only a modest amount of cigarettes (<15 g/day) (45). (For summary of evidence, see Supplementary material 1). Besides, smoking may also have a greater negative impact on lung growth in female than male during childhood and adolescence (46, 47). This suggests that the relationship between gender, age and changes in FEV1% may be U-shaped. The mechanisms responsible for the increased susceptibility of women than men to cigarette smoke can be summarized as: (1) smoking-inflammation pathway in the pre and post-menopausal periods (48, 49); (2) bronchial hyperresponsiveness in women compared to men (50–52); (3) hormonal status (53); (4) differences in lung development between females and males (54–56). Our study showed that the public demand for core information in this area was high, but the quality of evidence was low (Table 5). The dangers of smoking on the respiratory system are obvious, but evidence for women is still lacking. This is because women smoke less than men, so most surveys focus on male groups. Therefore, it is of great urgency to explore high-quality and sufficient evidence in this area to meet public health needs, and pay more attention to health education for adolescent and menopausal female. The specific summary of core information of female respiratory disease is shown in Table 5.
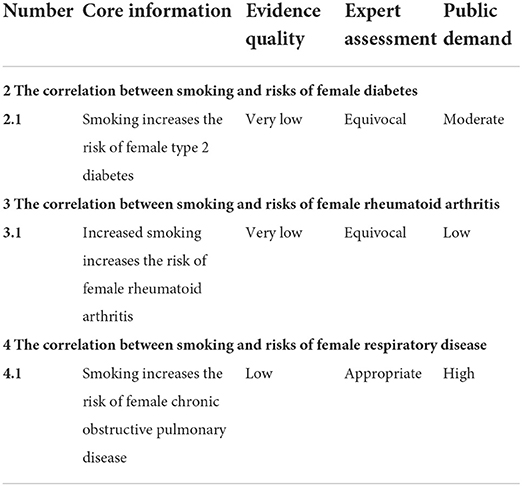
Table 5. The correlation between smoking and risks of female diabetes, rheumatoid arthritis and respiratory disease.
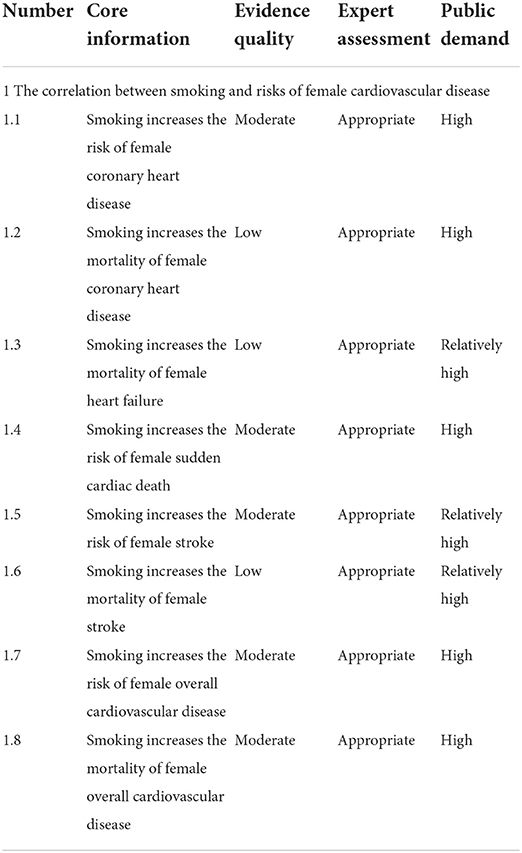
The correlation between smoking and risks of female cardiovascular disease
Several studies have shown that smoking is recognized as independent risk factors for cardiovascular diseases (21), which not only increases the oxidative stress, causing the oxidation of low-density lipoproteins (LDL), but also increases inflammation (57). It affects all stages of atherosclerosis, and eventually leads to cardiovascular diseases. In postmenopausal women, the estrogen, regarded as the guardian of blood vessels, is greatly reduced, which results in increased LDL and decreased high-density lipoproteins (HDL), thereby accelerating hardening of the arteries and leads to an increased risk of coronary heart disease, heart failure, sudden cardiac death, stroke and overall cardiovascular diseases (58–62) (For summary of evidence, see Supplementary material 1). Our research found that the quality of evidence, the degree of public demand and the results of expert assessments were relatively consistent and high in this area (Table 3). This is because cardiovascular diseases are closely related to people's lives and carry a high risk of death. Researches have found that the global mortality of cardiovascular diseases has increased by 12.5% over the past decade, and cardiovascular diseases currently account for about one-third of global deaths (63), so preventing cardiovascular diseases will greatly improve global health. This means that the core information in this field is the preferred content for health communication of tobacco control. Furthermore, It is worth noting that lifestyle and other factors are important control variables and should be considered in the health communication of tobacco control when discussing the impact of smoking on female cardiovascular disease. Smokers are more likely to have poor lifestyles like high-fat diet (increases triglyceride and cholesterol levels in the blood, causing hyperlipidemia and atherosclerosis), lack of exercise (leads to obesity and metabolic syndrome) and being sedentary (results in thrombosis), which jointly contribute to the development of cardiovascular diseases (64, 65). The specific summary of core information is shown in Table 6.
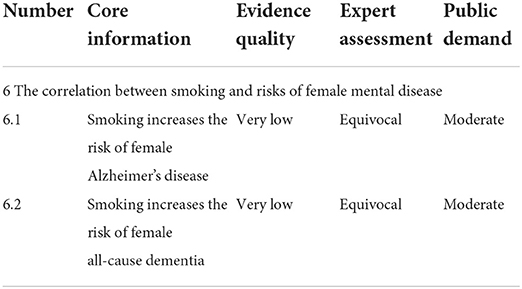
The correlation between smoking and risks of female mental disease
Mental illness have a huge burden on health in the world today. According to statistics, the global burden of mental illness accounts for 32·4% of years lived with disability (YLDs) and 13·0% of disability-adjusted life-years (DALYs) (66). Smoking rate was high in patients with mental illness, and it was estimated that more than 200,000 of 520,000 people suffer from mental illness who died mainly from chronic diseases caused by smoking in the United States (67). Especially for women, changes in their sex hormone levels (for example, the “recession” of sex hormones in menopausal women aged 45–55 years old, causing a series of physiological changes, imbalances in Nervous system activity and reduced adaptability to the outside world), as well as social stereotypes and low inclusion of women, lead to a higher prevalence of depression in this group, resulting in high smoking rates. Besides, female smoking groups are more likely to be discriminated against and stigmatized in social life (68), and they themselves are more sensitive and vulnerable to social impact (such as more passive to be exposed to smoking, more susceptible to negative emotions with smoking addiction) (69), causing further damage to their mental health. Our study found that the quality of evidence, the degree of public demand and the results of expert assessments are relatively consistent and low in this area (Table 7). This is because the effects of smoking on psychiatric disorders are mainly indirect (66–68) and unclear (70, 71) (For summary of evidence, see Supplementary material 1). In most cases, it is the mental illness itself that leads to the action of smoking. Therefore, this result suggests to health communicators that core information in this field is less appropriate for dissemination to the general public compared with other core information, but is more suitable for patients with mental illnesses. The specific summary of core information of female mental disease is shown in Table 7.
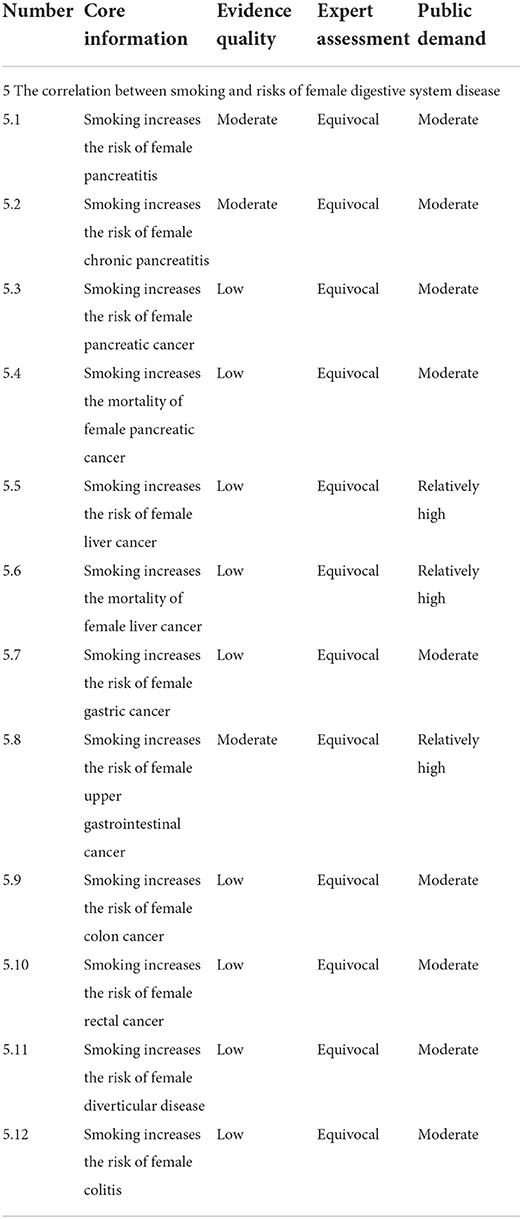
The correlation between smoking and risks of female digestive system disease
The chemicals in cigarette smoke including tobacco-specific nitrosamines, polycyclic aromatic hydrocarbons and aromatic amines play a major role in the development of digestive diseases by causing genetic mutations (72). Additionally, unhealthy diet like low fruit and vegetables intake (64), high fat eating (64), high salt consumption (73) and excessive alcohol ingestion (74, 75) (which itself has the effect of disease-promoting) and inappropriate daily habits like smoking after meals (which is harmful not only to the respiratory system, but also the digestive system) could be crucial reasons for an increased risk of digestive diseases, as these factors had synergistic effects with smoking. A total of 14 articles reported the effect of smoking on morbidity and mortality of female digestive diseases (76–89), including pancreatitis, pancreatic cancer, liver cancer, stomach cancer, upper gastrointestinal cancer, colon cancer, rectal cancer, diverticular disease, colitis (For summary of evidence, see Supplementary material 1). In this field, The quality of evidence and public demand for liver and upper gastrointestinal cancers were high, which might be related to the higher incidence of these cancers. For such diseases that are closely related to people's lives, these core information can be used as the first choice in the health communication of tobacco control, and the factors about the unhealthy diet and inappropriate daily habits mentioned above need to be paid enough attention to. The specific summary of core information of female digestive disease is shown in Table 8.
The correlation between smoking and risks of female diabetes
Two studies have shown that smoking increases the risk of diabetes in women, with results of 1.42 (95%: 1.19, 1.69) and 1.33 (95%: 1.26–1.41) relative risks of diabetes for current smokers respectively (90, 91) (For summary of evidence, see Supplementary material 1). The prevalence of type 2 diabetes (T2D) has gradually increased over the past three decades and has become a major global public health challenge. Given the high prevalence of smoking in many countries and the increasing burden of diabetes worldwide, reducing tobacco use should be prioritized as an important public health strategy that may contribute to the prevention and control of diabetes (90). This was also in line with a moderate public demand for core information in this area, but the quality and quantity of evidence was low (Table 4). This suggests that high-quality and sufficient evidence is urgently needed in this field to meet public health needs. The specific summary of core information of female diabetes is shown in Table 5.
The correlation between smoking and risks of female rheumatoid arthritis
Rheumatoid arthritis (RA) is a major autoimmune disease and is typically characterized by chronic inflammation of the articulations and bone destruction (92). As the most common form of inflammatory arthritis, its worldwide prevalence is approximately 1%, with women at two to three times the risk of developing rheumatoid arthritis compared to men due to the effect of estrogen on the immune system. The cumulative adult prevalence is 3.6% for women and 1.7% for men (93). Two systematic reviews have shown that smoking increases the risks of rheumatoid arthritis in women (94, 95), and male smokers are at greater risk than female smoker (95–97) (For summary of evidence, see Supplementary material 1). But the results of different original articles were inconsistent. Whether smoking habits caused RA was not clear. Our study found that the quality of evidence, the degree of public demand and the results of expert assessments were relatively consistent and low in this area (Table 5). This result suggests to health communicators that core information in this field is less suitable for tobacco control health communication. The specific summary of core information of female rheumatoid arthritis is shown in Table 5.
Dissemination analysis of core information
Dissemination of core information should be individualized. Based on audience preferences survey, we conducted a dissemination analysis of core information to guide health communicators how to spread the core information to audiences.
Different levels of education, gender and age had an effect on the degree of need for core information (Table 1 in Supplementary material 2). Among them, college students and undergraduates, women, and groups aged 26–45 were in greater demand. Most smokers were not only well educated but also aware of the dangers of smoking, however, they rarely received advice or help to quit (98). We suggest that middle-aged non-smoking women with higher education can be regarded as the main target for health communication workers to spread tobacco control core information. Because they can not only obtain more information about tobacco control for themselves and their families, but also play the role of supervision and persuasion.
Different occupations had different degrees of demand for core information, and the demand of medical workers was higher than that of non-medical workers, indicating that medical workers paid more attention to the impact of smoking on diseases (Table 1 in Supplementary material 2). Because of the particularity of their occupations, medical staff paid more attention to health-related information than other occupations, especially for the information needs of smoking hazards. Studies have shown that health education and health promotion can effectively improve medical staff's awareness of the dangers of smoking and their support for comprehensive smoking bans in medical and health institutions. This suggests that it is necessary to increase tobacco control education for medical personnel, and at the same time encourage and drive more medical personnel to contribute to medical education, scientific research, and international cooperation related to tobacco harm.
The public with chronic diseases had a higher demand for core information than the public without chronic diseases (Table 1 in Supplementary material 2). A large number of studies have shown that smoking is an important risk factor for the occurrence and death of various chronic non-communicable diseases, so people with these chronic diseases also paid more attention to the information on whether smoking control affected their health. In chronic disease management, the importance of smoking cessation-related health education was particularly important. It is recommended to increase the intensity of tobacco control health education among elderly patients with chronic diseases, which is of great significance for the effective management of chronic diseases, curbing the progress and adverse outcomes of the disease, and improving the quality of life of patients.
Compared with smokers, non-smokers had a higher degree of demand, indicating that non-smokers were more concerned about the information that smoking was harmful to health (Table 3 in Supplementary material 2). Our research also showed that the reason for the willingness to quit smoking among smokers was mainly “fear of getting sick.” Therefore, strengthening publicity and education about the harm of smoking can help smokers generate their willingness to quit (99).
Additionally, core information can be explained in a simple, science-based way that is more appropriate to the general public. This coincides with the importance of using visuals, telling real stories and using familiar language, as highlighted by the WHO Strategic Communication Framework for Effective Communications (100). Furthermore, attention should be paid to multi-culture group differences in health communication and tailored and targeted health communication strategies (22–24) are adopted for different groups. And different population groups based on the characteristics of the recipients (education, age and occupation) in the same culture context also need diversified communications to ensure effectiveness (101–103). A WHO scoping review noted that arts-based approaches are particularly useful in programming for multicultural groups and for building trust around sensitive health topics (104).
Discussion
This study focused on women's health, with rigorous, public-demand-oriented and appropriate core information covering eight parts and proposing 35 core information to maximize coverage of the dangers of smoking on all systems in females and to provide guidance on the health communication for tobacco control. Of all the core information, the core information related to female cardiovascular system diseases, as well as liver cancer and upper gastrointestinal cancer is the preferred content for health communication of tobacco control. The quality of evidence for core information related to pregnant women and their infants, as well as diseases of reproductive system, respiratory system, and diabetes needs to be improved to meet high public demand. The core information related to mental disease is more suitable for dissemination to patients with mental illness than to the general public. Besides, dissemination of core information should be individualized.
Advantages of this study are as follows. Initially, it is the first systematic and comprehensive evidence-based core information for health communication in the field of tobacco control, which which will be of great significance to improve the reliability of evidence. In the past, tobacco control in health communication was primarily composed of the media communication channels (105, 106), whose reliability was often influenced by some large stakeholders, which led to frequent rumors in this field (7). Secondly, the formation of core information took into account the needs of the public with a reasonable distribution of age, gender, education level, occupation, smoking status and chronic disease status according to sociodemographic characteristics during the survey. This can ensure that the core information keeps “the common touch.” Thirdly, the expert assessment pre-dissemination content expert review from multidisciplinary expertise (29) was used and factors such as the quality of evidence, the degree of public demand, balance of importance of each evidence, equity, feasibility, acceptability were considered comprehensively so that core information is not only scientifically correct, but also suitable for dissemination.
However, this study has certain limitations. First, available evidences supporting this core information were actually weak due to ethical concerns (smoking is a detrimental factor and not suitable as an intervention), which contributed to a lack of large-scale randomized controlled trials (RCTs) and then led to scarcity of high quality evidence. Secondly, the public prevalence survey and expert assessment were mainly confined to the national conditions of China, which resulted in limitations in the scope of application. Thirdly, given that the overall number of smoking women was still less than that of men, related to specific diseases like rheumatoid arthritis, might be deviated from the objective reality.
For future perspectives, there are several important areas that need to be improved:
First, smoking and passive smoking are recognized as one of the main causes of cardiovascular diseases, and they are also independent risk factors for such diseases (21). Evidences show that the relationship between smoking and cardiovascular disease has received widespread attention and is of relatively high quality, recommendation and public need. Future investigations still require high-quality researches in this area.
Second, the relationship between smoking and respiratory disease is well known (21), as the respiratory system is the first system to be exposed to smoke and is susceptible to oxidative damage, resulting in chronic inflammatory responses and airway remodeling and, in severe cases, cancerous lesions. However, the available research lacks separate data on women and extensive empirical epidemiological evidence. Future development in this areas is of great value to assist tobacco control in women.
Third, future investigations on effects of smoking on pregnant women and their fetuses are of great importance to assist tobacco control in women due to greater susceptibility to tobacco among pregnant women and fetuses during pregnancy. At the same time, researches on the harm of second-hand smoke (in a passive way) to pregnant women and their fetuses are also worthy of attention. It suggests that future researches can form core information about the effects of passive smoking on pregnant women and their fetuses.
Fourth, the current study focuses less attention on the effect of smoking on female mental diseases which is a huge burden on health in the world today (66, 67). As large-scale, prospective studies are actually lacking in this areas, further studies are required for more convincing evidence.
Fifth, core information concerning smoking on female rheumatoid arthritis was controversial and with low evidence and public need and weak recommendation. Future investigation in this field need to be more comprehensive, accurate and rigorous.
Sixth, tobacco control health communication strategies of core information of this guideline are also needed for more tailored and targeted for different development status, public literacy and age pattern.
Finally, future development of evidence-based core information of tobacco control for health communication can focus on the effectiveness of positive interventions on tobacco control, such as mobile health interventions; and include more high-quality and large-scale RCTs.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
Draft writing: JL, Y-YH, X-LH, Y-BW, and X-ZJ. Draft revising and reviewing: Y-BW and X-ZJ. Conception and design: Y-BW, X-ZJ, JL, and C-XQ. Guideline registration and protocol writing: JL, C-XQ, and S-TW. Collecting and determining PICOs questions: JL, Y-YH, H-JM, M-LC, and S-TW. GRADE assessment: JL and Y-YH. Audience value survey: X-JS and JL. Delphi expert consensus survey: JL, H-JM, Y-YH, Y-BW, and X-ZJ. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Bloomberg Initiative to Reduce Tobacco Use(CHINA-25-07).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.986430/full#supplementary-material
References
1. GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1223–49. doi: 10.1016/S0140-6736(20)30752-2
2. GBD 2019 Tobacco Collaborators. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990-2019: a systematic analysis from the Global Burden of Disease Study 2019 [published correction appears in Lancet. Lancet. (2021) 397:2337–60. doi: 10.1016/S0140-6736(21)01169-7
3. Ezzati M, Lopez AD. Estimates of global mortality attributable to smoking in 2000. Lancet. (2003) 362:847–52. doi: 10.1016/S0140-6736(03)14338-3
4. Peto R, Lopez AD, Boreham J, Thun M, Heath C Jr, Doll R. Mortality from smoking worldwide. Br Med Bull. (1996) 52:12–21. doi: 10.1093/oxfordjournals.bmb.a011519
5. Peto R, Lopez AD, Boreham J. Health effects of tobacco use: global estimates and projections. In:Slama K, , editors. Tobacco and Health. Boston, MA: Springer. (1995). p. 109–20.
6. GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
7. Dai X, Gakidou E, Lopez AD. Evolution of the global smoking epidemic over the past half century: strengthening the evidence base for policy action. Tob Control. (2022) 31:129–37. doi: 10.1136/tobaccocontrol-2021-056535
8. Bolego C, Poli A, Paoletti R. Smoking and gender. Cardiovasc Res. (2002) 53:568–76. doi: 10.1016/S0008-6363(01)00520-X
9. Marom-Haham L, Shulman A. Cigarette smoking and hormones. Curr Opin Obstet Gynecol. (2016) 28:230–5. doi: 10.1097/GCO.0000000000000283
10. Hughes EG, Brennan BG. Does cigarette smoking impair natural or assisted fecundity? Fertil Steril. (1996) 66:679–89. doi: 10.1016/S0015-0282(16)58618-X
11. Mattison DR. The effects of smoking on fertility from gametogenesis to implantation. Environ Res. (1982) 28:410–33. doi: 10.1016/0013-9351(82)90139-6
12. Practice Committee of the American Society for Reproductive Medicine. Practice Committee of the American Society for Reproductive Medicine. Smoking and infertility: a committee opinion. Fertil Steril. (2018) 110:611–18. doi: 10.1016/j.fertnstert.2018.06.016
13. Malik A, Jeyaraj PA, Shankar A, Rath GK, Mukhopadhyay S, Kamal VK. Passive smoking and breast cancer—a suspicious link. Asian Pac J Cancer Prev. (2015) 16:5715–9. doi: 10.7314/APJCP.2015.16.14.5715
14. Tanaka K, Miyake Y, Hanioka T, Arakawa M. Active and passive smoking and prevalence of periodontal disease in young Japanese women. J Periodontal Res. (2013) 48:600–5. doi: 10.1111/jre.12044
15. Flor LS, Reitsma MB, Gupta V, Ng M, Gakidou E. The effects of tobacco control policies on global smoking prevalence. Nat Med. (2021) 27:239–43. doi: 10.1038/s41591-020-01210-8
16. van Mourik DA, Nagelhout GE, de Vries H, van den Putte B, Cummings KM, Borland R, et al. Quasi-experimentally examining the impact of introducing tobacco pictorial health warnings: Findings from the International Tobacco Control (ITC) 4C and Netherlands surveys in the Netherlands, Australia, Canada, United Kingdom, and the United States. Drug Alcohol Depend. (2020) 207:107818. doi: 10.1016/j.drugalcdep.2019.107818
17. Sutfin EL, Lazard AJ, Wagoner KG, King JL, Cornacchione Ross J, Wiseman KD, et al. Point-of-Sale health communication campaigns for cigarillos and waterpipe tobacco: effects and lessons learned from two cluster randomized trials. Health Commun. (2021) 15:1–12. doi: 10.1080/10410236.2021.1996910
18. Mackert M, Case K, Lazard A, Oh J, Hughes Wagner J, Hawk E, et al. Building a health communication brand for University of Texas System tobacco control. J Am Coll Health. (2019) 67:291–8. doi: 10.1080/07448481.2018.1469504
19. Duella CS. Communication is a determinant of public health: a media campaign for tobacco control in India. BMJ. (2013) 347:f6275. doi: 10.1136/bmj.f6275
20. Karletsos D, Hutchinson P, Leyton A, Meekers D. The effect of interpersonal communication in tobacco control campaigns: a longitudinal mediation analysis of a Ghanaian adolescent population. Prev Med. (2021) 142:106373. doi: 10.1016/j.ypmed.2020.106373
21. GBD 2015 Tobacco Collaborators. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990-2015: a systematic analysis from the Global Burden of Disease Study 2015. Lancet. (2017) 389:1885–906. doi: 10.1016/S0140-6736(17)30819-X
22. Agrawal PK, Aruldas K, Khan ME. Training Manual on Basic Monitoring and Evaluation of Social and Behavior Change Communication Health Programs. New Delhi: Population Council. (2014).
23. Kreuter MW, Wray RJ. Tailored and targeted health communication: strategies for enhancing information relevance. Am J Health Behav. (2003) 27 (Suppl. 3):S227–32. doi: 10.5993/AJHB.27.1.s3.6
24. Noar S, Harrington N, Van Stee SK, Aldrich RS. Tailored health communication to change lifestyle behaviors. Am J Lifestyle Med. (2010) 5:112–22. doi: 10.1177/1559827610387255
25. World Health Organization. WHO Handbook for Guideline Development. World Health Organization. (2014).
26. Institute of Medicine (US) Committee to Advise the Public Health Service on Clinical Practice Guidelines. In: Field MJ, Lohr KN editors. Clinical Practice Guidelines: Directions for a New Program. Washington (DC): National Academies Press (US). (1990).
27. Institute of Medicine. Committee on Standards for Developing Trustworthy Clinical Practice Guidelines; Institute of Medicine. Clinical Practice Guidelines We Can Trust. (2011).
28. Schünemann HJ, Wiercioch W, Etxeandia I, Falavigna M, Santesso N, Mustafa R, et al. Guidelines 20: systematic development of a comprehensive checklist for a successful guideline enterprise. CMAJ. (2014) 186:E123–42. doi: 10.1503/cmaj.131237
29. Chen Y, Yang K, Marušic A, Qaseem A, Meerpohl JJ, Flottorp S, et al; RIGHT (Reporting Items for Practice Guidelines in Healthcare) Working Group. A reporting tool for practice guidelines in health care: the RIGHT statement. Ann Intern Med. (2017) 166:128–32. doi: 10.7326/M16-1565
30. WHO Global Report on Trends in Prevalence of Tobacco Use 2000-2025. Fourth Edition. Geneva: World Health Organization. (2021).
31. Sugawara Y, Tsuji I, Mizoue T, Inoue M, Sawada N, Matsuo K, et al. Research group for the development and evaluation of cancer prevention strategies in Japan. Cigarette smoking and cervical cancer risk: an evaluation based on a systematic review and meta-analysis among Japanese women. Jpn J Clin Oncol. (2019) 49:77–86. doi: 10.1093/jjco/hyy158
32. Kaderli R, Schnüriger B, Brügger LE. The impact of smoking on HPV infection and the development of anogenital warts. Int J Colorectal Dis. (2014) 29:899–908. doi: 10.1007/s00384-014-1922-y
33. Han YD, Wang XB, Cui NH, Zhang S, Wang C, Zheng F. Associations of P16INK4a promoter hypermethylation with squamous intra-epithelial lesion, cervical cancer and their clinicopathological features: a meta-analysis. Oncotarget. (2017) 8:1871–83. doi: 10.18632/oncotarget.12202
34. Macacu A, Autier P, Boniol M, Boyle P. Active and passive smoking and risk of breast cancer: a meta-analysis. Breast Cancer Res Treat. (2015) 154:213–24. doi: 10.1007/s10549-015-3628-4
35. Sollie M, Bille C. Smoking and mortality in women diagnosed with breast cancer-a systematic review with meta-analysis based on 400,944 breast cancer cases. Gland Surg. (2017) 6:385–93. doi: 10.21037/gs.2017.04.06
36. Jordan SJ, Whiteman DC, Purdie DM, Green AC, Webb PM. Does smoking increase risk of ovarian cancer? A systematic review. Gynecol Oncol. (2006) 103:1122–9. doi: 10.1016/j.ygyno.2006.08.012
37. Santucci C, Bosetti C, Peveri G, Liu X, Bagnardi V, Specchia C, et al. Dose-risk relationships between cigarette smoking and ovarian cancer histotypes: a comprehensive meta-analysis. Cancer Causes Control. (2019) 30:1023–32. doi: 10.1007/s10552-019-01198-8
38. Faber MT, Kjær SK, Dehlendorff C, Chang-Claude J, Andersen KK, Høgdall E, et al. Ovarian cancer association consortium. Cigarette smoking and risk of ovarian cancer: a pooled analysis of 21 case-control studies. Cancer Causes Control. (2013) 24:989–1004. doi: 10.1007/s10552-013-0174-4
39. Chen HL, Cai JY, Zha ML, Shen WQ. Prenatal smoking and postpartum depression: a meta-analysis. J Psychosom Obstet Gynaecol. (2019) 40:97–105. doi: 10.1080/0167482X.2017.1415881
40. Hunter A, Murray R, Asher L, Leonardi-Bee J. The effects of tobacco smoking, and prenatal tobacco smoke exposure, on risk of schizophrenia: a systematic review and meta-analysis. Nicotine Tob Res. (2020) 22:3–10. doi: 10.1093/ntr/nty160
41. Dong T, Hu W, Zhou X, Lin H, Lan L, Hang B, et al. Prenatal exposure to maternal smoking during pregnancy and attention-deficit/hyperactivity disorder in offspring: A meta-analysis. Reprod Toxicol. (2018) 76:63–70. doi: 10.1016/j.reprotox.2017.12.010
42. Lee LJ, Lupo PJ. Maternal smoking during pregnancy and the risk of congenital heart defects in offspring: a systematic review and metaanalysis. Pediatr Cardiol. (2013) 34:398–407. doi: 10.1007/s00246-012-0470-x
43. Dechanet C, Anahory T, Mathieu Daude JC, Quantin X, Reyftmann L, Hamamah S, et al. Effects of cigarette smoking on reproduction. Hum Reprod Update. (2011) 17:76–95. doi: 10.1093/humupd/dmq033
44. Shulman A, Ellenbogen A, Maymon R, Bahary C. Smoking out the oestrogens. Hum Reprod. (1990) 5:231–3. doi: 10.1093/oxfordjournals.humrep.a137077
45. Gan WQ, Man SF, Postma DS, Camp P, Sin DD. Female smokers beyond the perimenopausal period are at increased risk of chronic obstructive pulmonary disease: a systematic review and meta-analysis. Respir Res. (2006) 7:52. doi: 10.1186/1465-9921-7-52
46. Patel BD, Luben RN, Welch AA, Bingham SA, Khaw KT, Day NE, et al. Childhood smoking is an independent risk factor for obstructive airways disease in women. Thorax. (2004) 59:682–6. doi: 10.1136/thx.2003.010215
47. Gold DR, Wang X, Wypij D, Speizer FE, Ware JH, Dockery DW. Effects of cigarette smoking on lung function in adolescent boys and girls. N Engl J Med. (1996) 335:931–7. doi: 10.1056/NEJM199609263351304
48. Hutchinson WL, Koenig W, Fröhlich M, Sund M, Lowe GD, Pepys MB. Immunoradiometric assay of circulating C-reactive protein: age-related values in the adult general population. Clin Chem. (2000) 46:934–8. doi: 10.1093/clinchem/46.7.934
49. Gan WQ, Man SF, Sin DD. The interactions between cigarette smoking and reduced lung function on systemic inflammation. Chest. (2005) 127:558–64. doi: 10.1378/chest.127.2.558
50. Tashkin DP, Altose MD, Bleecker ER, Connett JE, Kanner RE, Lee WW, et al. The lung health study: airway responsiveness to inhaled methacholine in smokers with mild to moderate airflow limitation. The Lung Health Study Research Group. Am Rev Respir Dis. (1992) 145:301–10. doi: 10.1164/ajrccm/145.2_Pt_1.301
51. Leynaert B, Bousquet J, Henry C, Liard R, Neukirch F. Is bronchial hyperresponsiveness more frequent in women than in men? A population-based study. Am J Respir Crit Care Med. (1997) 156:1413–20. doi: 10.1164/ajrccm.156.5.9701060
52. Paoletti P, Carrozzi L, Viegi G, Modena P, Ballerin L, Di Pede F, et al. Distribution of bronchial responsiveness in a general population: effect of sex, age, smoking, and level of pulmonary function. Am J Respir Crit Care Med. (1995) 151:1770–7. doi: 10.1164/ajrccm.151.6.7767519
53. Baron JA, La Vecchia C, Levi F. The antiestrogenic effect of cigarette smoking in women. Am J Obstet Gynecol. (1990) 162:502–14. doi: 10.1016/0002-9378(90)90420-C
54. Skobeloff EM, Spivey WH, St Clair SS, Schoffstall JM. The influence of age and sex on asthma admissions. JAMA. (1992) 268:3437–40. doi: 10.1001/jama.1992.03490240045034
55. Hibbert ME, Couriel JM, Landau LI. Changes in lung, airway, and chest wall function in boys and girls between 8 and 12 yr. J Appl Physiol Respir Environ Exerc Physiol. (1984) 57:304–8. doi: 10.1152/jappl.1984.57.2.304
56. Merkus PJ, Borsboom GJ, Van Pelt W, Schrader PC, Van Houwelingen HC, Kerrebijn KF, et al. Growth of airways and air spaces in teenagers is related to sex but not to symptoms. J Appl Physiol. (1985). (1993) 75:2045–53. doi: 10.1152/jappl.1993.75.5.2045
57. Ambrose JA, Barua RS. The pathophysiology of cigarette smoking and cardiovascular disease: an update. J Am Coll Cardiol. (2004) 43:1731–7. doi: 10.1016/j.jacc.2003.12.047
58. Woodward M, Lam TH, Barzi F, Patel A, Gu D, Rodgers A, et al. Asia Pacific Cohort Studies Collaboration. Smoking, quitting, and the risk of cardiovascular disease among women and men in the Asia-Pacific region. Int J Epidemiol. (2005) 34:1036–45. doi: 10.1093/ije/dyi104
59. Hackshaw A, Morris JK, Boniface S, Tang JL, Milenković D. Low cigarette consumption and risk of coronary heart disease and stroke: meta-analysis of 141 cohort studies in 55 study reports. BMJ. (2018) 360:j5855. doi: 10.1136/bmj.j5855
60. Huxley RR, Woodward M. Cigarette smoking as a risk factor for coronary heart disease in women compared with men: a systematic review and meta-analysis of prospective cohort studies. Lancet. (2011) 378:1297–305. doi: 10.1016/S0140-6736(11)60781-2
61. Aune D, Schlesinger S, Norat T, Riboli E. Tobacco smoking and the risk of sudden cardiac death: a systematic review and meta-analysis of prospective studies. Eur J Epidemiol. (2018) 33:509–21. doi: 10.1007/s10654-017-0351-y
62. Peters SA, Huxley RR, Woodward M. Smoking as a risk factor for stroke in women compared with men: a systematic review and meta-analysis of 81 cohorts, including 3,980,359 individuals and 42,401 strokes. Stroke. (2013) 44:2821–8. doi: 10.1161/STROKEAHA.113.002342
63. Joseph P, Leong D, McKee M, Anand SS, Schwalm JD, Teo K, et al. Reducing the global burden of cardiovascular disease, part 1: the epidemiology and risk factors. Circ Res. (2017) 121:677–94. doi: 10.1161/CIRCRESAHA.117.308903
64. Thompson, Dewi H, Warburton DM. Lifestyle differences between smokers, ex-smokers and non-smokers, and implications for their health. Psychol Health. (1992) 7:311–21. doi: 10.1080/08870449208403160
65. Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol. (2012) 2:1143–211. doi: 10.1002/cphy.c110025
66. Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. (2016) 3:171–8. doi: 10.1016/S2215-0366(15)00505-2
67. Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis. (2006) 3:A42.
68. Brown-Johnson CG, Cataldo JK, Orozco N, Lisha NE, Hickman NJ. 3rd, Prochaska JJ. Validity and reliability of the internalized stigma of smoking inventory: an exploration of shame, isolation, and discrimination in smokers with mental health diagnoses. Am J Addict. (2015) 24:410–8. doi: 10.1111/ajad.12215
69. Helman TJ, Headrick JP, Vider J, Peart JN, Stapelberg NJC. Sex-specific behavioral, neurobiological, and cardiovascular responses to chronic social stress in mice. J Neurosci Res. (2022) 100:2004–27. doi: 10.1002/jnr.25115
70. Durazzo TC, Mattsson N, Weiner MW. Alzheimer's disease neuroimaging initiative. smoking and increased Alzheimer's disease risk: a review of potential mechanisms. Alzheimers Dement. (2014) 10:S122–45. doi: 10.1016/j.jalz.2014.04.009
71. Zhong G, Wang Y, Zhang Y, Guo JJ, Zhao Y. Smoking is associated with an increased risk of dementia: a meta-analysis of prospective cohort studies with investigation of potential effect modifiers. PLoS ONE. (2015) 10:e0118333. doi: 10.1371/journal.pone.0118333
72. Hecht SS. Tobacco carcinogens, their biomarkers and tobacco-induced cancer. Nat Rev Cancer. (2003) 3:733–44. doi: 10.1038/nrc1190
73. Gherasim A, Arhire LI, Ni?ă O, Popa AD, Graur M, Mihalache L. The relationship between lifestyle components and dietary patterns. Proc Nutr Soc. (2020) 79:311–23. doi: 10.1017/S0029665120006898
74. Zeka A, Gore R, Kriebel D. Effects of alcohol and tobacco on aerodigestive cancer risks: a meta-regression analysis. Cancer Causes Control. (2003) 14:897–906. doi: 10.1023/B:CACO.0000003854.34221.a8
75. Bagnardi V, Blangiardo M, La Vecchia C, Corrao G. Alcohol consumption and the risk of cancer: a meta-analysis. Alcohol Res Health. (2001) 25:263–70.
76. Andriulli A, Botteri E, Almasio PL, Vantini I, Uomo G, Maisonneuve P. Ad Hoc Committee of the Italian Association for the Study of the Pancreas. Smoking as a cofactor for causation of chronic pancreatitis: a meta-analysis. Pancreas. (2010) 39:1205–10. doi: 10.1097/MPA.0b013e3181df27c0
77. Ye X, Lu G, Huai J, Ding J. Impact of smoking on the risk of pancreatitis: a systematic review and meta-analysis. PLoS ONE. (2015) 10:e0124075. doi: 10.1371/journal.pone.0124075
78. Iodice S, Gandini S, Maisonneuve P, Lowenfels AB. Tobacco and the risk of pancreatic cancer: a review and meta-analysis. Langenbecks Arch Surg. (2008) 393:535–45. doi: 10.1007/s00423-007-0266-2
79. Lugo A, Peveri G, Bosetti C, Bagnardi V, Crippa A, Orsini N, et al. Strong excess risk of pancreatic cancer for low frequency and duration of cigarette smoking: a comprehensive review and meta-analysis. Eur J Cancer. (2018) 104:117–26. doi: 10.1016/j.ejca.2018.09.007
80. Ben QW, Liu J, Sun YW, Wang LF, Zou DW, Yuan YZ. Cigarette smoking and mortality in patients with pancreatic cancer: a systematic review and meta-analysis. Pancreas. (2019) 48:985–95. doi: 10.1097/MPA.0000000000001383
81. Lee YC, Cohet C, Yang YC, Stayner L, Hashibe M, Straif K. Meta-analysis of epidemiologic studies on cigarette smoking and liver cancer. Int J Epidemiol. (2009) 38:1497–511. doi: 10.1093/ije/dyp280
82. Pang Q, Qu K, Zhang J, Xu X, Liu S, Song S, et al. Cigarette smoking increases the risk of mortality from liver cancer: a clinical-based cohort and meta-analysis. J Gastroenterol Hepatol. (2015) 30:1450–60. doi: 10.1111/jgh.12990
83. Botteri E, Iodice S, Bagnardi V, Raimondi S, Lowenfels AB, Maisonneuve P. Smoking and colorectal cancer: a meta-analysis. JAMA. (2008) 300:2765–78. doi: 10.1001/jama.2008.839
84. Tsoi KK, Pau CY, Wu WK, Chan FK, Griffiths S, Sung JJ. Cigarette smoking and the risk of colorectal cancer: a meta-analysis of prospective cohort studies. Clin Gastroenterol Hepatol. (2009) 7:682–88.e6885. doi: 10.1016/j.cgh.2009.02.016
85. Cheng J, Chen Y, Wang X, Wang J, Yan Z, Gong G, et al. Meta-analysis of prospective cohort studies of cigarette smoking and the incidence of colon and rectal cancers. Eur J Cancer Prev. (2015) 24:6–15. doi: 10.1097/CEJ.0000000000000011
86. Aune D, Sen A, Leitzmann MF, Tonstad S, Norat T, Vatten LJ. Tobacco smoking and the risk of diverticular disease - a systematic review and meta-analysis of prospective studies. Colorectal Dis. (2017) 19:621–33. doi: 10.1111/codi.13748
87. Ladeiras-Lopes R, Pereira AK, Nogueira A, Pinheiro-Torres T, Pinto I, Santos-Pereira R, et al. Smoking and gastric cancer: systematic review and meta-analysis of cohort studies. Cancer Causes Control. (2008) 19:689–701. doi: 10.1007/s10552-008-9132-y
88. Ansary-Moghaddam A, Huxley RR, Lam TH, Woodward M. The risk of upper aero digestive tract cancer associated with smoking, with and without concurrent alcohol consumption. Mt Sinai J Med. (2009) 76:392–403. doi: 10.1002/msj.20125
89. Al Momani L, Balagoni H, Alomari M, Gaddam S, Boonpherg B, Aasen T, et al. The association between smoking and both types of microscopic colitis: a systematic review and meta-analysis. Arab J Gastroenterol. (2020) 21:9–18. doi: 10.1016/j.ajg.2020.01.004
90. Pan A, Wang Y, Talaei M, Hu FB, Wu T. Relation of active, passive, and quitting smoking with incident type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. (2015) 3:958–67. doi: 10.1016/S2213-8587(15)00316-2
91. Akter S, Goto A, Mizoue T. Smoking and the risk of type 2 diabetes in Japan: a systematic review and meta-analysis. J Epidemiol. (2017) 27:553–61. doi: 10.1016/j.je.2016.12.017
92. Scott DL, Wolfe F, Huizinga TW. Rheumatoid arthritis. Lancet. (2010) 376:1094–108. doi: 10.1016/S0140-6736(10)60826-4
93. Smolen JS, Aletaha D, Barton A, Burmester GR, Emery P, Firestein GS, et al. Rheumatoid arthritis. Nat Rev Dis Primers. (2018) 4:18001. doi: 10.1038/nrdp.2018.1
94. Sugiyama D, Nishimura K, Tamaki K, Tsuji G, Nakazawa T, Morinobu A, et al. Impact of smoking as a risk factor for developing rheumatoid arthritis: a meta-analysis of observational studies. Ann Rheum Dis. (2010) 69:70–81. doi: 10.1136/ard.2008.096487
95. Lahiri M, Morgan C, Symmons DP, Bruce IN. Modifiable risk factors for RA: prevention, better than cure? Rheumatology (Oxford). (2012) 51:499–512. doi: 10.1093/rheumatology/ker299
96. Rayman M, Callaghan A. Nutrition and Arthritis. Oxford, UK: Blackwell Publishing. (2006). doi: 10.1002/9780470775011
97. Stolt P, Källberg H, Lundberg I, Sjögren B, Klareskog L, Alfredsson L. EIRA study group. Silica exposure is associated with increased risk of developing rheumatoid arthritis: results from the Swedish EIRA study. Ann Rheum Dis. (2005) 62:582–6. doi: 10.1136/ard.2004.022053
98. Lee EH, Shin SH, Jeong GC. Smoking awareness and intention to quit smoking in smoking female workers: secondary data analysis. Int J Environ Res Public Health. (2022) 19:2841. doi: 10.3390/ijerph19052841
99. Eccles M, Mason J, Freemantle N. Developing valid cost effectiveness guidelines: a methodological report from the north of England evidence based guideline development project. Qual Health Care. (2000) 9:127–32. doi: 10.1136/qhc.9.2.127
100. World Health Organization. The Strategic Communications Framework for Effective Communications. (2019). https://www.who.int/mediacentre/communication-framework.pdfWebsite (accessed January 13, 2020).
101. Institute of Medicine (US) Committee on Communication for Behavior Change in the 21st Century: improving the health of diverse populations. Speaking of Health: Assessing Health Communication Strategies for Diverse Populations. Washington (DC): National Academies Press (US). (2002).
102. Parker RM, Gazmararian JA. Health literacy: essential for health communication. J Health Commun. (2003) 8 (Suppl 1):116–8. doi: 10.1080/713851963
103. Maibach EW, Maxfield A, Ladin K, Slater M. Translating health psychology into effective health communication: the American Healthstyles audience segmentation project. J Health Psychol. (1996) 1:261–77. doi: 10.1177/135910539600100302
104. Fancourt D, Finn S. What is the Evidence on the Role of the Arts in Improving Health and Well-Being? A Scoping Review. Copenhagen: WHO Regional Office for Europe. (2019).
105. Davis RM. The Role of the Media in Promoting and Reducing Tobacco Use: Executive Summary. US Department of Health and Human Services, National Institutes of Health, National Cancer Institute. (2008).
Keywords: tobacco control, smoking, smoking cessation, female diseases, health communication, core information
Citation: Liu J, Hao Y-Y, Mao H-J, Sun X-J, Huang X-L, Quan C-X, Cao M-L, Wei S-T, Jin X-Z and Wu Y-B (2022) Evidence-based core information for health communication of tobacco control: The effect of smoking on risks of female disease. Front. Public Health 10:986430. doi: 10.3389/fpubh.2022.986430
Received: 05 July 2022; Accepted: 15 September 2022;
Published: 18 October 2022.
Edited by:
Melody Goodman, New York University, United StatesReviewed by:
Lei Shi, Southern Medical University, ChinaFeiying He, Southern Medical University, China
Copyright © 2022 Liu, Hao, Mao, Sun, Huang, Quan, Cao, Wei, Jin and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xue-Zheng Jin, eWF5YTIybmRAaG90bWFpbC5jb20=; Yi-Bo Wu, YmptdXd1eWlib0BvdXRsb29rLmNvbQ==
 Jin Liu
Jin Liu Yun-Yi Hao
Yun-Yi Hao Hui-Jia Mao3
Hui-Jia Mao3 Shu-Ting Wei
Shu-Ting Wei Yi-Bo Wu
Yi-Bo Wu