- 1Department of Health Policy and Management, Tabriz Health Services Management Research Center, School of Management and Medical Informatics, Tabriz University of Medical Sciences, Tabriz, Iran
- 2Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran
- 3Social Determinants of Health Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
- 4Wolfson Institute of Population Health, Queen Mary University of London, London, United Kingdom
- 5Department of Infectious Disease Epidemiology, London School of Hygiene and Tropical Medicine, London, United Kingdom
Background: Delivering essential health services through non-governmental organizations (NGOs) could facilitate moving toward universal health coverage (UHC), especially in low- and middle-income countries. This study investigates the viewpoints of Iranian health system experts and executive stakeholders on the role of NGOs in moving toward UHC.
Method: We conducted 33 semi-structured interviews with health policymakers, NGO representatives at the national and provincial level, and other key informants and analyzed using content analyses methods, using MAXQDA 12. The inductive-deductive approach was used for qualitative data analyses.
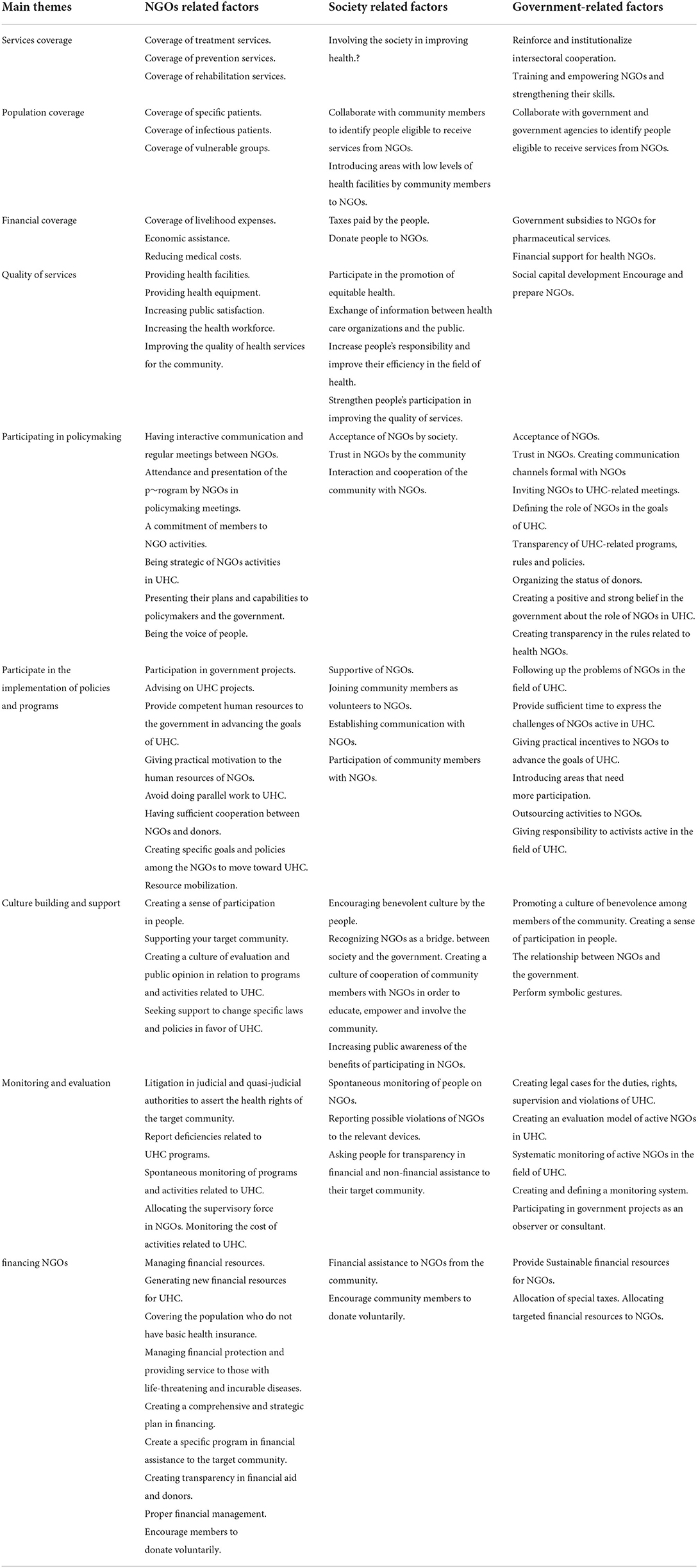
Result: Based on the thematic analysis of interviews and document reviews, nine main themes and one hundred and five sub-themes were identified. Each theme was categorized based on NGO-, society-, and government-related factors.
Conclusion: Recognizing the critical role of NGOs and their contribution in moving toward UHC is essential, particularly in the local context. Collaboration between NGO stakeholders and the government could facilitate moving toward UHC.
Introduction
Universal health coverage (UHC) is essential to achieve optimal health and justice in every country (1), and all community members should have access to all aspects of health services, including prevention, treatment, and rehabilitation (2). Health systems need to be sufficiently efficient in population, service, and financial coverage to achieve sustainable UHC (3). However, despite injecting financial and human resources into the health systems, many countries still have difficulties achieving UHC (4, 5), as allocating funding for healthcare priorities alone is insufficient (6).
Like many other countries, Iran has made additional efforts to move toward UHC during the last decades. Recent reforms aimed to improve the situation by increasing the number and variety of services provided to patients (especially to the poor) and increasing access to primary healthcare in remote parts of the country (4). However, providing adequate and fair services to all populations remains one of the main challenges in Iran's UHC goals (7). As UHC has become a priority for the global health community, understanding the role of various groups and organizations in the country and how they contribute to reaching this goal is critical. Non-governmental organizations (NGOs) can help achieve the goals of UHC (5). NGOs have grown significantly since the mid-1970s, and through creative activities and increased public participation, they have increased population coverage, especially in disadvantaged and rural communities (8–10). The term “NGO” usually refers to any non-profit voluntary group of global citizens who work locally, nationally, and internationally for various cultural, social, charitable, and professional purposes (11).
NGO activities in Iran
In Iran, NGO is an organization that is legal, non-profitable, independent from the government or any political or religious organization, and voluntary and is known as “SAMAN,” a short version of the Persian phrase “Sazmanha-ye Mardom Nahad,” translated as “community-based organizations” or “people's organizations.” NGOs have similar functions to Charites. According to the NGO functions, government institutions such as Ministry of Interior, Governor and Governorates, Ministry of Sports and Youth, Law Enforcement Command, and Welfare Organization monitor the activities of NGOs in Iran (12). In 2017, National Health Assembly was funded consisting representatives from different policy and management levels and health-related NGOs (13). In addition, three national assembly participate in the process of health-related policies including the National Assembly of Youth NGO, the National Assembly of People's organizations, and the Assembly of Marriage Donors. Also, there are foreign NGOs that do not have an impact on Iranian health policy, and their main focus is on the immigrants who enter Iran. The Iranian Diabetes NGO, which provides disease-related services, or the Iranian AIDS NGO, which is responsible for organizing and coordinating all public activities in the field of HIV/AIDS, are the popular NGOs in Iran. Following the last official report based on 2004 Census, there were 6,914 active NGOs in Iran. According to unofficial statistics (Deputy Minister of Social Participation), the number of NGOs was about twenty thousand in 2020. Since the beginning of NGOs' establishment in Iran, they have had a role in healthcare provision, treatment and pharmaceutical activities, financial support, education and prevention, social health, consulting role, and technical information, as well as in monitoring individuals' communities' access to healthcare (14, 15). Furthermore, new adopted policies and regulations support public organizations and NGOs (i.e., articles 95, 97, 104, 140, and 163 of the Law of the Iran Fourth Economic, Social, and Cultural Five-Year Development Plan the Horizon of Iran 1404). NGO contributions to universities of medical sciences in Iran were around 357 to 405 million USD in 2016–2017 (16). Until 2015, about 6 billion USD channeled through NGOs' donations supported the construction of hospitals, equipment purchasing, and expanded healthcare service delivery infrastructure. Overall, some NGOs have a pivotal role in providing financial assistance for the construction and equipment of the hospitals.
UHC in Iran
The framework Iranian health system has a clear cut three-level design, containing primary, secondary, and tertiary facilities, whose financial resources include government funds, general taxation, health insurance, out-of-pocket, and individual donations. After the revolution, Iran has made many changes in its health system to achieve health for all, and since UHC was considered as the main priority, its components were included in the national upstream policy documents such as Five-Year Development Plans and 20-year vision plan (17, 18). To translate national policy documents to implementation plans, major reforms toward achieving UHC including the Family Physician Program (2004), merging all existing health insurance funds into MSIO (2012) and the Health Transformation Plan(HTP) (2014), were developed in Iran (19, 20). One of the aims of the HTP that the then government emphasized on it was socialization of health. In this regard, civil societies, especially NGOs, were considered as key factor in the health sector functions. In 2017, the National Health Assembly was formed and NGOs officially entered the policymaking processes in Iran's health system (21). Implementing HTP along with other policy interventions led to an impact on the three dimensions of UHC, including providing primary healthcare, promoting health indexes, controlling epidemics, preventing and eradicating some diseases, extending healthcare insurance, improving health resources both qualitatively and quantitatively, improving the quality of healthcare and services, and developing pharmaceutical industry (7). Also, out-of-pocket expenditures have decreased from 80.5 (1995) to 38.8% (2016) of current health expenditure (22).
To develop working policies to engage NGOs in a movement toward UHC effectively, it is essential to understand the potential and roles of NGOs activities in facilitating progress toward UHC goals. This study aimed to explore the views of NGOs' participants, policymakers, and planners on the activities performed by NGOs, examine to what extent they could play a role in progress toward UHC in Iran, and how their function can be maximized in services provision in the long run.
Materials and methods
Design and setting
This qualitative case study was carried out using semi-structured interviews and documentary reviews. The study's design and the presentation of findings follow the Consolidated Criteria for Reporting Qualitative Research (COREQ) 32-item checklist (23).
Participants
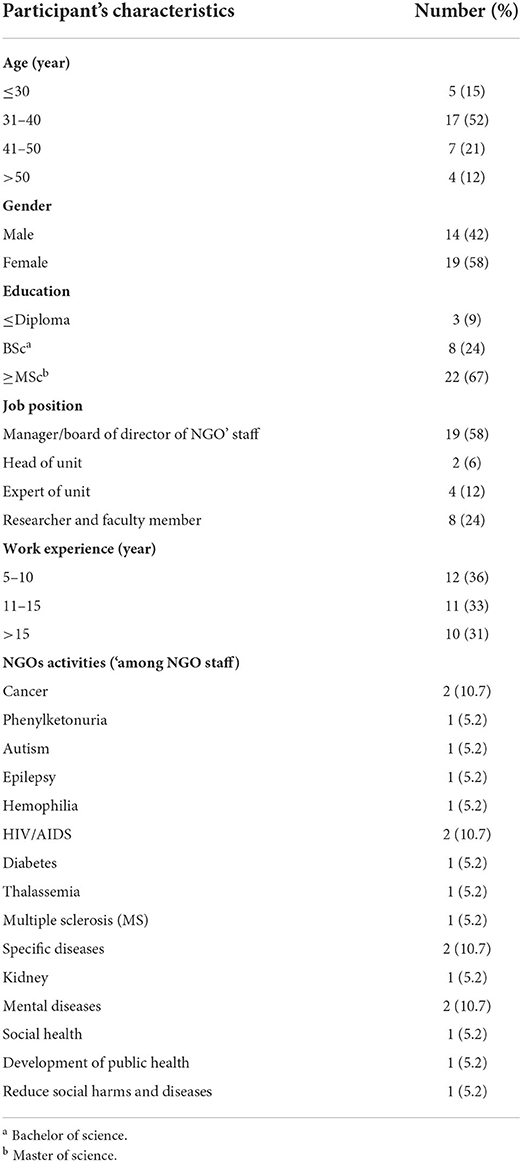
Semi-structured interviews were conducted with NGO managers, board of directors and technical experts, faculty members, researchers, scholars, heads of NGOs, and experts of government agencies that issue licenses to NGOs' establishments. Considering the scope and role of NGOs and the geographical extent of Iran, purposeful sampling with maximum variation was used to select participants. In addition to practice backgrounds and experience, for NGOs, criteria such as the level of activity (provincial, national, and international), the number of years of activity, and their willingness to participate were considered. For the rest of the participants, individuals' educational and professional background was also considered when selecting interviewees. People with experience in collaboration with health organizations and involvement in related activities were preferred. Before participation, the prospective participants were contacted and invited to participate in the study via email or telephone, and the interview was conducted face to face. Data saturation was considered as the basis for the number of study participants. Interviewee characteristics are presented in Table 1.
Interview tool and data collection
A semi-structured interview tool was developed to guide all interviews and comprised five parts (i.e., participants' demographic data, current professional roles, study's objective, informed consent, and general opinion). The general interview questions focused more on the activities, performance, resources, and barriers to NGO participation in moving toward UHC. It was validated by three NGO representatives and two experts for face and content validation and piloted under intended interview conditions to confirm the validity and practice for the interviewer. The data on these pilot interviews were also used in the study analysis. An independent interviewer conducted all interviews. The research team consisted of four academic researchers, three male researchers and one female researcher. All four research team members have prior experience in qualitative research. All participants provided written informed consent before participating in interviews. With participants' consent, all conducted interviews were audio-recorded, each lasting on average 38 min. A total of 33 interviews were conducted with the research participants.
Document review
Document reviews were used as Supplementary Data. To conduct document reviews, relevant documents were collected from universities of medical sciences, MoHME, and local websites, such as registered documents in the “database for SAMANs.” Data on NGOs' activities, their population coverage, provided services and the costs from NGOs' financial records, strategic and operational plans, minutes of meeting between NGOs and authorities of vice-chancellors of social affairs, and other related documents were collected.
Data analysis
All interviews were transcribed verbatim. Analyses were performed simultaneously with transcription. If there were any inconsistencies or ambiguities, these were resolved by calling back interviewees for clarifications. To ensure the data were robust, we used strategies of member checking (in three stages of data collection, at the end of each interview, and after data analyses) and auditing (after extracting initial codes and development of initial themes). The interviews and policy documents were analyzed by the content analysis method. MAXQDA 12 (VERBI Software 2015, MAXQDA 12, computer program, VERBI Software, Berlin) was used for data analyses. Data coding process was done in three steps: generating and finalizing the initial codes, grouping codes denoting the same concepts into subcategories, and classifying subcategories indicating similar subjects into the main categories. Two authors read all documents and transcripts of the interviews to extract issues, themes, and sub-themes. During the data analysis phase, the two researchers had regular meetings to discuss any disagreements to reach a consensus openly. When consensus was not reached, the other two researchers resolved any disputes.
Results
Based on the thematic analyses of interviews and document reviews, nine main themes and one hundred and five sub-themes were identified. Each theme was categorized based on three factors: NGO-, society-, and government-related factors (Table 2). The strategies and challenges of each theme, if any, were stated in its sub-themes.
Based on the review of documents and the interviews, NGOs in Iran primarily had activities in ten health-related areas, including healthcare with five sub-sectors (public health development, environmental health, medicine, patient treatment and relief, and health infrastructure). The activity license of NGOs at national and provincial levels is issued through the Ministry of Interior, the Governor and Governorates and State Welfare Organization of Iran, the police force of the Islamic Republic of Iran, and the Ministry of Sports and Youth. Hence, NGOs can be differentiated based on their characteristics, that is, non-governmental, non-profit, non-political, and operating at national, regional, provincial, or international levels. In some Iranian national upstream documents, the importance of NGOs has been mentioned. NGOs working in the public health had six general programs, including training and empowerment of NGOs with the help of university or faculty of medical sciences through holding educational workshops, university and faculty of medical sciences' support of NGOs in line with the general health goals announced by the Minister of Health and Medical Education (MoHME), monitoring and evaluation of NGOs with the help of university and faculty of medical sciences, expanding the activities of national NGOs to the provinces and creating NGOs in provinces, and building networks in the provincial or national level in subjects such as AIDS or addiction.
NGOs' performance and UHC
There were conflicting views on the performance of NGOs in achieving the goals of moving toward UHC. NGO staff believed that their performance positively affected public health and health outcomes. Some participants mentioned that evaluation of the performance of NGOs and its effect on the health system is not possible. Lack of definition of NGOs' role and expectations of NGOs in line with UHC programs and the lack of an effective evaluation program of the activities of these organizations in achieving the goals of UHC were among the challenges mentioned by participants.
“When we can discuss the role of NGOs in universal health coverage and say it is good or bad, first of all, we should have a tool that would allow evaluating how they work and secondly what do we expect from NGOs in public health coverage.” [A NGOs researcher]
However, the establishment of the National Health Assembly with the slogan “All for health, health for all” in line with the Health Transformation Plan in Iran is a turning point in the participation of NGOs in UHC-related policies.
Service coverage
One of the factors influencing NGOs' participation in achieving UHC was service coverage. NGOs provided different services in three levels in this theme—prevention, treatment, and rehabilitation. Both NGO staff and experts agreed that the most NGO activity was in service coverage.
“In general, NGOs work more in the field of service coverage than other dimensions because it is more tangible and has better facilities in this area.” [A manager at NGO]
NGO activities in the field of prevention services were related to education (such as obesity, overweight, high fat, high blood sugar, and high blood pressure and its effect on cardiovascular diseases, and healthy life) and awareness (adhering to a healthy diet, not smoking, and inactivity), empowerment, screening for communicable/non-communicable diseases, disseminating health-oriented information, and promoting community health. Also, other activities by NGOs were to cover services: the provision of curative services, which includes periodic visits by a general practitioner, the provision of dental services, and specialized services to patients according to their illness. Some NGOs performed activities in the coverage of rehabilitation services, including therapeutic counseling, occupational therapy, and speech therapy. The activities of NGOs in the field of treatment were mostly focused on providing medical services freely or with low cost to patients with special diseases such as diabetes, cancers, and blood diseases.
“NGOs have a variety of activities including education, community empowerment, dental services, chemotherapy services, counselling services...” [A head of Licensing Unit to NGOs]
On the contrary, one of the strategies that NGOs should consider and in which the community is involved is to involve the general public in improving health issues. Also, one of the challenges of the government in covering services is the issue of inter-sectoral cooperation, especially cooperation with NGOs, which the government should strengthen this area and adopt an appropriate strategy for it.
“NGOs can also count on people's capacity and ability in this field” [A manager at NGO]. Also, another participant stated, “In my opinion, the government is not fully utilising the capacity of NGOs and should increase its cooperation.” [An NGO staff]
Population coverage
One of the main foci of work NGOs was increasing population access to health services, particularly for vulnerable, poor, or people with a specific disease, using strategies and interventions such as community participation. Coverage of patients with particular conditions, infectious diseases, and coverage of vulnerable groups were among the main population covered by the NGOs. A review of documents showed that most of the NGOs in the public health field covered people with specific diseases such as kidney, cancer, hemophilia, thalassemia, and phenylketonuria. Another measure taken by NGOs to increase population coverage was to cover people with infectious diseases, such as leprosy, tuberculosis, and AIDS. Also, NGOs had a significant role in identifying vulnerable groups, such as marginalized, displaced, and informal populations, and providing health services to these populations.
“The role that NGOs can play in population coverage is to cover informal and marginalised populations such as immigrants, sex workers, etc. This population is not formally covered by insurance. We should consider that identifying this population is difficult. The role of NGOs is very prominent in identifying and introducing this population because they are located in the most peripheral part of the county.” [A senior health official]
The role of society is also significant, and since NGOs alone are not able to identify people and areas with poor health, people should aid NGOs and work with them. The government should also ask government agencies operating in health to cooperate with NGOs to identify people who are not in good health status.
“The people and the government can identify areas where NGOs need to cooperate so that they can go there and volunteer.” [A manager at NGO]
Financial coverage
According to the participants and document review, NGOs used various strategies to provide financial coverage to their populations. These strategies included coverage of livelihood expenses, economic assistance, and reducing medical costs. According to NGO mission, some tried to cover the living expenses of the people under their coverage by providing marriage, education, livelihood assistance, and travel allowances. The most critical action that NGOs took in UHC was reducing expenses by covering medical and pharmaceutical expenses in whole or in part. Also, another activity of NGOs in Iran was related to cooperation with local institutions that provide loans to people in the community to cover part of their health expenses.
“We provide aid in the form of a package or financial aid to people that might need any care or are in poverty or at risk of catastrophic health expenditure situation.” [A manager at NGO]
None of the NGOs had a strategy in line with the insurance coverage plans. They reduce the health costs of the covered people through direct payment of medical and pharmaceutical costs and also by making contracts with clinics and hospitals to provide services with low cost.
Quality of services
NGOs also worked toward improving the quality of services. In this regard, provision of health facilities, establishing medical centers or hospitals with donors' help, and equipping medical centers were among other activities mentioned by participants.
“Our NGO bought a new device for the hospital with the help of donors…. providing equipment such as condoms, wheelchairs and other medical needs of the population are some of the other activities that we do in our NGO.” [A manager at NGO]
Participant also stated that by recruiting volunteers and health workers, who are the official forces of the Ministry of Health, NGOs increased the number of services provided during non-operating hours in clinics and hospitals. By recruiting staff volunteers, they also increased the active workforce and improved the quality of services offered in health, which led to an increase in public satisfaction.
“NGOs can, with the help of specialist physicians and nurses, ask them to volunteer at NGO centres during the week.” [A NGOs researcher]
Factors affecting the participation of NGOs in the community in providing quality of services included involvement in the promotion of equitable health, exchange of information between healthcare organizations and the public people, increase people's responsibility, and improving their efficiency in the field of health and strengthening people's participation in improving the quality of services. On the contrary, the government promoted social capital and ultimately increased the quality of services by encouraging and preparing NGOs.
“I think people have a vital role to play in the quality of services provided by NGOs, and they should be involved in public health.” [A head of Licensing Unit to NGOs]
Participating in policymaking
According to NGO-related factors, having interactive communication and regular meetings between NGOs, attendance, and presentation of a program by NGOs in policymaking meetings, the commitment of members to NGO activities, being strategic of NGOs activities in UHC, presenting their plans and capabilities to policymakers and the government, and being the voice of people would lead to increased engagement of NGOs in the field of UHC.
“We must be active in policy-making meetings and be able to introduce ourselves properly.” [A manager at NGO]
In addition, acceptance of NGOs by society, trust in NGOs by the community, and interaction and cooperation of the community with NGOs were identified as crucial factors that can lead to active participation from NGOs in UHC. Finally, acceptance of NGOs, trust in NGOs, creating communication channels formal with NGOs, inviting NGOs to UHC-related meetings, defining the role of NGOs in the goals of UHC, transparency of UHC-related programs, rules, and policies, organizing the status of donors, creating a positive and strong belief in the government about the role of NGOs in UHC, and creating transparency in the rules related to health NGOs by the government led to increased engagement of NGOs.
“There must be a strong will in the government to involve NGOs.” [A NGOs researcher] Also, another participant stated, “People need to trust NGOs and work together.” [A NGOs' staff]
Participate in the implementation of policies and programs
Participants mentioned that NGOs could assist the government in implementing programs and procedures by focusing and participating in government projects in UHC, providing qualified human resources and motivating volunteer forces, and mobilizing resources.
“We must have a competent force to carry out so that the government can trust us and give us some of its activities.” [A board of directors of NGO]
The community could implement UHC-related programs and policies by connecting and partnering with NGOs. In addition, the government could encourage NGOs to participate and address their problems by outsourcing some activities and creating more participation and enough time to implement programs and motivate NGOs.
“Our society has a lot of educated people, and when they see that they can help, they should come to work and help NGOs.” [A manager at NGO]
The participants stated that the country's health management system should give priority to delegation of authority and responsibility to the actors in the field of health, and in this regard, the National Health Assembly can be an effective consultative organization.
“… The formation of this assembly is emphasized as an effective advisory arm for the Supreme Council of Health and Food Safety.” [A manager at NGO]
Culture building and support
The study participants expected that NGOs would promote a culture of participation among the people, the government, and organizations to support their target community and support UHC-related laws and policies or seek to change them.
“The media can teach a culture of benevolence in the country and introduce NGOs to the people.” [A NGOs researcher]
In government and community-related factors, participants provided information about encouraging the community to help and understanding that NGOs are a bridge between community and government.
“Unfortunately, in the last 10, 15 years, they gave false information about NGOs to the people, but during these years, NGOs tried to show their true face to the people and the government, and we see that trust in them has increased.” [A manager at NGO]
Monitoring and evaluation
In this regard, participants stated that NGOs should cooperate with the relevant judiciary and executive bodies in UHC and report any violations in the case.
“This year, the judiciary has designed a platform on which NGOs can voluntarily register, which I think is a good activity.” [A board of directors of NGO]
In addition, society can help monitor and evaluate NGOs in UHC-related programs through voluntary monitoring, reporting of potential violations by NGOs, and transparency in funding. The government should strengthen the monitoring and evaluation system by establishing and defining a monitoring system, reviewing the principles of NGOs, and using NGOs as supervisors or consulting in UHC-related projects.
“One of the capabilities that I think has been overlooked by the government is that NGOs can supervisors' projects.” [A senior health official]
Financing NGOs
Participants stated that financing is one of the critical issues regarding the participation of NGOs in UHC programs and stressed that managing financial resources, generating new financial resources for UHC, covering the population who do not have basic health insurance, managing financial protection and providing service to those with life-threatening and incurable diseases, creating a comprehensive and strategic plan in the financing, creating a specific program in financial assistance to the target community, creating transparency in financial aid and donors, proper financial management, and encouraging members to donate voluntarily are essential. In addition, they acknowledged that the government could assist them by providing sustainable financial resources for NGOs, allocating special taxes, and providing targeted financial resources to NGOs.
“I have seldom noticed that NGOs or the government have a comprehensive funding program organisation, which I think can follow the example of successful countries like Italy, which levies part of the tax and allocates it to NGOs.” [An NGO member]
At the same time, due to Iran's economic conditions and external sanctions during the years, most of the funding sources of NGOs through foreign donors and international organizations were reduced.
“Due to the economic war with the world and sanctions, it is impossible to use the capacity of foreign aid, and unfortunately during last year's NGOs suffered a lot from this issue, and it affected their revenues and costs, and now NGOs are more focused on internal resources.” [A manager at NGO]
Discussion
This study examined the viewpoints of scientific experts and stakeholders on NGO UHC-related activities in Iran. Our results showed that NGOs work in all UHC dimensions in Iran, including quality service coverage, population coverage, and financial coverage. One of the significant issues raised was that the government has not appropriately used its full potential. Our findings also imply that lack of programs in this regard, lack of tools (including appropriate criteria for evaluating actions and activities of the NGOs), and ambiguity in the role and position of NGOs in the health system structure are among the main challenges of using NGOs potential in moving toward UHC in Iran to the fullest. For years, NGOs have tried to fill the gaps in health services provision by MoHME. They are increasingly stepping up along with healthcare providers and pursuing similar goals. This is confirmed by previous studies showing that the government's lack of a defined plan and resource constraints limits their participation in health system goals. Evidence shows that achieving social health is not possible without the participation of NGOs, especially in low-income countries (24). Nonetheless, NGO participation in healthcare is recognized as an effective strategy for promoting health, social development, and access to UHC.
NGOs can provide services directly through screening for communicable or non-communicable diseases, disseminating health information, equipping and developing infrastructure of healthcare centers, or indirectly through counseling and supporting services in prevention (24). They can also provide follow-ups and a wide range of pharmaceutical, outpatient and inpatient, and diagnostic services directly by covering drug and medical expenses or indirectly providing in-home support services (25–27). However, for better NGOs contribution and improving their motivation to participate in health system activities, the costs of NGOs need to be covered by supranational organizations such as the State Welfare Organization of Iran and the Relief Committee, or indirectly through contracts with medical centers. Studies conducted in other developing countries showed that NGOs could provide structural services such as building hospitals and providing medical equipment (15, 28–30). Other evidence showed that NGOs could improve and promote the health of their communities through the establishment of primary healthcare centers, providing laboratory services, training community health workers to screen for and manage chronic hypertension, providing maternal and new-born health services, providing medical services for children with cancers, providing mental health services through community-based rehabilitation, prevention and treatment groups received growth monitoring, referrals to public health facilities, home-based counseling, and providing mid-day meals for primary school students and adolescents (31–40).
In many countries, the poor still have limited access to primary healthcare, and NGOs can increase access to health services because of their ability to design population-based projects. NGOs are also able to implement prevention programs to reach vulnerable social populations. Innovative approaches such as the caregiver approach can be a promising alternative to existing strategies to provide critical healthcare to disadvantaged communities (41–44). UHC is a key priority set out by the WHO and the United Nations General Assembly (45, 46). Social health insurance schemes, one mechanism to achieve UHC, have become increasingly crucial in low- and middle-income countries as they work to achieve this goal. To ensure comprehensive health insurance coverage for a broad population at a reasonable cost, social health insurance schemes could be designed by NGOs so that individuals receive a set package of subsidized health services through accredited providers (45, 47, 48). NGOs can rightly play a vital role in moving toward UHC when their role is defined in UHC programs by the government and the Ministry of Health or other relevant entities. Therefore, health policymakers and planners should facilitate adequate and targeted services by NGOs by prioritizing important components of UHC and the goals required for medical and educational interventions (24).
In line with our findings, a recent study conducted in Iran showed that legal and managerial barriers are among challenges for NGOs to work with the government to move toward UHC (16). NGOs need to use appropriate strategies to achieve UHC goals. As noted in our study, building sustainable funding and developing strategies for the participation in legislative, planning, and decision-making levels are critical. For example, designing and implementing programs and policies related to health system goals and NGOs should be conducted with the support of the community and people who specialize in this field (9). The government should also create the right opportunities for NGOs to participate in public health and UHC activities, use them as advisors, and delegate responsibilities because these organizations have a very close relationship with the community. They are known as the voice of the people. In terms of the partnership of these organizations with the government and the capacity on both sides (both the government and the NGOs), the community and their participation are very effective. Previous studies in this area were also consistent with the findings of our study (49–55).
Collaboration with government and other government agencies is a key strategy for NGOs moving toward UHC, and this creates synergies and uses their capabilities. In other words, as it was shown in our study, NGOs need to formally communicate with all institutions involved in UHC to provide quality services to people in the community, especially vulnerable and marginalized groups (56, 57). At the same time, creating a human culture encouraging community members to help NGOs and encouraging a sense of participation in the community causes significant cooperation between the government, government agencies, and the community with NGOs (15).
Conclusion
NGOs could have a significant role in providing each UHC dimension and could have great potential in moving countries toward UHC. However, to use the NGOs potential, the government and MoHME must define the scope of NGOs activities and develop a comprehensive plan for engaging NGOs in UHC. Given the creation and expansion of health services and global attention to UHC, NGOs' participation can improve services provided to the populations, particularly the poor and marginalized areas. Despite the vital role of NGOs in health services delivery, relatively little is still known about how NGOs could be engaged to achieve UHC goals. NGOs' goals and expectations of public health coverage programs in Iran are not clear. Understanding NGOs' role and contributing to attaining UHC is critical, especially in the local context. Governments need to consider developing systematic and fundamental strategies for NGOs engagement in public health goals to move toward UHC.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study was approved by the Ethics Committee of Tabriz University of Medical Sciences (Approval No: IR.TBZMED.REC.1399.370). The patients/participants provided their written informed consent to participate in this study.
Author contributions
LD conceived the study. AS and LD contributed to designing, collecting, analyzing, drafting, and finalizing the paper. RK-Z and VS contributed to analyzing data. All authors read and approved the final version of the paper. All authors contributed to the study conception and design.
Funding
The study was funded by Tabriz University of Medical Sciences, Tabriz, Iran (Grant No: 64241).
Acknowledgments
This study is part of a Ph.D. thesis in the School of Management and Medical Informatics, Tabriz University of Medical Sciences, Tabriz, Iran. The authors express their gratitude to Tabriz University of Medical Sciences for supporting this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.985079/full#supplementary-material
Abbreviations
NGOs, non-governmental organizations; UHC, universal health coverage; MS, multiple sclerosis; PKU, phenylketonuria.
References
1. Etienne C, Asamoa-Baah A, Evans DB. Health Systems Financing: The Path to Universal Coverage. Geneva, Switzerland: World Health Organization (2010).
2. Schmidt H, Gostin LO, Emanuel EJ. Public health, universal health coverage, and Sustainable development goals: can they coexist? Lancet. (2015) 386:928–30. doi: 10.1016/S0140-6736(15)60244-6
3. Vega J. Universal health coverage: the post-2015 development agenda. Lancet. (2013) 381:179. doi: 10.1016/S0140-6736(13)60062-8
4. Letafat M, Beyranvand T, Aryankhesal A, Behzadifar M. Universal health coverage (UHC) in Iran. Iran J Public Health. (2018) 47:1061–2.
5. Sanadgol A, Doshmangir L, Majdzadeh R, Gordeev VS. Engagement of non-governmental organisations in moving towards universal health coverage: a scoping review. Global Health. (2021) 17:1–19. doi: 10.1186/s12992-021-00778-1
6. Mousavi SM, Sadeghifar J. Universal health coverage in Iran. Lancet Global Health. (2016) 4:e305–6.
7. Sajadi HS, Ehsani-Chimeh E, Majdzadeh R. Universal health coverage in Iran: Where we stand and how we can move forward. Med J Islam Repub Iran. (2019) 33:9. doi: 10.47176/mjiri.33.9
8. Das N, Kumar R. Role of Non-Governmental Organizations in Healthcare Sector of India. Germany: University Library of Munich (2016).
9. Khodayari-Zarnaq R, Kakemam E, Arab-Zozani M, Rasouli J, Sokhanvar M. Participation of Iranian non-governmental organizations in health policy-making; barriers and strategies for development. Int J Health Govern. (2020) 25:46–56. doi: 10.1108/IJHG-07-2019-0056
10. Piotrowicz, M, Cianciara, D. The role of non-governmental organizations in the social and the health system. Przeglad Epidemiol. (2013) 67:69–74.
12. Academy IC. The Role of Non-Governmental Organizations in Solving the Country's Problems. (2020). Available online at: https://ac.kheir.ir/people-instituterole-s-in-country (accessed August 2, 2022).
13. Assembly NH. Statement of the First National Health Assembly. (2017). Available online at: https://social.nkums.ac.ir/Category/25937 (accessed September 6, 2022).
14. Bidar Z, Ghasemi G. Role of NGOs in developing the right of health. Iran J Med Law. (2020) 14:7–26. Available online at: http://ijmedicallaw.ir/article-1-964-en.html
15. Damari B, Heidarnia MA, Bonab MR. Role and Performance of IRANIAN NGOs in Community. Available online: https://payeshjournal.ir/article-1-275-en.pdf
16. Bahabadi ZG, Amiresmaili M, NekoeiMoghadam M, Amiryousefi S. Role of charities in the health system: A qualitative study. J Qual Res Health Sci. (2013) 2:1–10. Available online at: https://jqr1.kmu.ac.ir/article_90736_ce4040030b08813b84a4cb5f41a4cbd4.pdf
17. Moghaddam AV, Damari B, Alikhani S, Salarianzedeh M, Rostamigooran N, Delavari A, et al. Health in the 5th 5-years Development Plan of Iran: main challenges, general policies and strategies. Iran J Public Health. (2013) 42:42–9.
18. Rashidian A, Damari B, Larijani B, Moghadda AV, Alikhani S, Shadpour K, et al. Health observatories in Iran. Iran J Public Health. (2013) 42:84–7.
19. Doshmangir L, Moshiri E, Mostafavi H, Sakha MA, Assan A. Policy analysis of the Iranian Health Transformation Plan in primary healthcare. BMC Health Serv Res. (2019) 19:1–8. doi: 10.1186/s12913-019-4505-3
20. Harirchi I, Hajiaghajani M, Sayari A, Dinarvand R, Sajadi HS, Mahdavi M, et al. How health transformation plan was designed and implemented in the Islamic Republic of Iran? Int J Prev Med. (2020) 11. doi: 10.4103/ijpvm.IJPVM_430_19
21. Ashoorkhani M, Rajabi F, Majdzadeh R. The meaning of “socialization of health” to Iranian policymakers and how it can be implemented. Med J Islam Repub Iran. (2019) 33:6. doi: 10.47176/mjiri.33.6
22. Doshmangir L, Bazyar M, Najafi B, Haghparast-Bidgoli H. Health financing consequences of implementing health transformation plan in Iran: achievements and challenges. Int J Health Policy Manage. (2019) 8:384. doi: 10.15171/ijhpm.2019.18
23. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting Qual research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. (2007) 19:349–57. doi: 10.1093/intqhc/mzm042
24. Nikjoo RG, Partovi Y, Joudyian N. Involvement of charities in Iran's health care system: a quality study on problems and executive/legal/supportive requirements. BMC Health Serv Res. (2021) 21:1–13. doi: 10.1186/s12913-021-06187-9
25. Roland AB, Yenshu VE, Ndoh IM, Ndzifon KJ. Rural development NGOs and service delivery to the very poor: an empirical analysis of a training center in rural Cameroon. Asian J Agric Rural Dev. (2015) 5:103–15. Available online at: https://archive.aessweb.com/index.php/5005/article/view/1387
26. Batley R, Mcloughlin C. Engagement with non-state service providers in fragile states: reconciling state-building and service delivery. Dev Pol Rev. (2010) 28:131–54. doi: 10.1111/j.1467-7679.2010.00478.x
27. Henderson K. Alternative service delivery in developing countries: NGOs and other non-profits in urban areas. Public Organ Rev. (2002) 2:99–116. doi: 10.1023/A:1016051211179
28. Gooding K. The role of NGOs' service delivery experience in developing relevant research agendas: experience and challenges among NGOs in Malawi. Health Res Pol syst. (2017) 15:1–14. doi: 10.1186/s12961-017-0199-3
29. Opoku RA. Examining the motivational factors behind charitable giving among young people in a prominent Islamic country. Int J Nonprofit Volunt Sector Market. (2013) 18:172–86. doi: 10.1002/nvsm.1457
30. Zaidi S, Mayhew SH, Cleland J, Green AT. Context matters in NGO–government contracting for health service delivery: a case study from Pakistan. Health Policy Plan. (2012) 27:570–81. doi: 10.1093/heapol/czr081
31. Baig M, Panda B, Das JK, Chauhan AS. Is public private partnership an effective alternative to government in the provision of primary health care? A case study in Odisha. J Health Manag. (2014) 16:41–52. doi: 10.1177/0972063413518679
32. Baqui AH, Rosecrans AM, Williams EK, Agrawal PK, Ahmed S, Darmstadt GL, et al. NGO facilitation of a government community-based maternal and neonatal health programme in rural India: improvements in equity. Health Policy Plan. (2008) 23:234–43. doi: 10.1093/heapol/czn012
33. Chanani S, Waingankar A, Shah More N, Pantvaidya S, Fernandez A, Jayaraman A, et al. Effectiveness of NGO-government partnership to prevent and treat child wasting in urban India. Matern Child Nutr. (2019) 15:e12706. doi: 10.1111/mcn.12706
34. Mehta P, Sharma S, Manglani M. Improvement in pediatric cancer survival in a developing country through collaboration with nongovernmental organization.: PUB-0165. Pediatr Blood Cancer. (2013) 60:889–91. doi: 10.1002/pbc.24476
35. Sankaran S, Ravi PS, Wu YE, Shanabogue S, Ashok S, Agnew K, et al. An NGO-implemented community–clinic health worker approach to providing long-term care for hypertension in a remote region of Southern India. Global Health Sci Pract. (2017) 5:668–77. doi: 10.9745/GHSP-D-17-00192
36. Sharma A, Singh S, Meena S, Kannan A. Impact of NGO run mid day meal program on nutrition status and growth of primary school children. Indian J Pediatr. (2010) 77:763–9. doi: 10.1007/s12098-010-0116-z
37. Singh V, Ahmed S, Dreyfuss ML, Kiran U, Chaudhery DN, Srivastava VK, et al. Non-governmental organization facilitation of a community-based nutrition and health program: effect on program exposure and associated infant feeding practices in rural India. PLoS ONE. (2017) 12:e0183316. doi: 10.1371/journal.pone.0183316
38. Sivakumar T, James JW, Basavarajappa C, Parthasarathy R, Kumar CN, Thirthalli J, et al. Impact of community-based rehabilitation for mental illness on “out of pocket” expenditure in rural South India. Asian J Psychiatr. (2019) 44:138–42. doi: 10.1016/j.ajp.2019.07.029
39. Thomas R, Srinivasan R, Sudarshan H. Nutritional status of tribal children and adolescents in rural south India: the effect of an NGO delivered nutritional programme. Indian J Pediatr. (2013) 80:821–5. doi: 10.1007/s12098-013-1098-4
40. Wamai RG. Reforming Health Systems: The Role of NGOs in Decentralization—Lessons from Kenya and Ethiopia. Baltimore: International Society for Thirdsector Research (2008).
41. Albis MLF, Bhadra SK, Chin B. Impact evaluation of contracting primary health care services in urban Bangladesh. BMC Health Serv Res. (2019) 19:1–12. doi: 10.1186/s12913-019-4406-5
42. Amirkhanian YA, Kelly J, Benotsch EG, Somlai AM, Brown KD, Opgenorth K, et al. HIV prevention nongovernmental organizations in Central and Eastern Europe: programs, resources and challenges. Cent Eur J Public Health. (2004) 12:12–8. Available online at: http://cejph.szu.cz/pdfs/cjp/2004/01/03.pdf
43. Ejaz I, Shaikh BT, Rizvi N. NGOs and government partnership for health systems strengthening: a Qual study presenting viewpoints of government, NGOs and donors in Pakistan. BMC Health Serv Res. (2011) 11:1–7. doi: 10.1186/1472-6963-11-122
44. Perry H, Morrow M, Borger S, Weiss J, DeCoster M, Davis T, et al. Care groups I: an innovative community-based strategy for improving maternal, neonatal, and child health in resource-constrained settings. Global Health Sci Pract. (2015) 3:358–69. doi: 10.9745/GHSP-D-15-00051
45. World Health Organization. Sustainable health financing, universal coverage and social health insurance. World Health Assembly Resolut. (2005) 58:139–40. Available online at: https://apps.who.int/iris/handle/10665/20302
46. Organization WH. World Health Report (The): Health Systems Financing: The Path to UNIVERSAL COVERAGE (Arabic). Geneva, Switzerland: World Health Organization (2010).
47. Carrin G, James C. Reaching Universal Coverage Via Social Health Insurance: Key Design Features in the Transition Period, vol. 13. Geneva, Switzerland: World Health Organization (2004).
48. Savedoff WD, de Ferranti D, Smith AL, Fan V. Political and economic aspects of the transition to universal health coverage. Lancet. (2012) 380:924–32. doi: 10.1016/S0140-6736(12)61083-6
49. Banks N, Hulme D, Edwards M. NGOs, states, and donors revisited: Still too close for comfort? World Dev. (2015) 66:707–18. doi: 10.1016/j.worlddev.2014.09.028
50. Boris ET. Philanthropic Foundations in the United States: An Introduction. Washington, DC: Council on Foundations. (1992).
51. Hassan M, Wedig GJ, Morrisey MA. Charity care by non-profit hospitals: the price of tax-exempt debt. Int J Econ Bus. (2000) 7:47–62. doi: 10.1080/13571510084050
52. Mosadeghrad AM, Tajvar M, Ehteshami F. Donors' Participation in Financing Health System of Iran. Hakim Res. J. (2019) 22:26–42. Available online at: https://www.sid.ir/paper/411316/en
53. Namazi B. Volunteer's Community Organizations in Iran. (2002). Tehran: Municipalities Organization.
54. Shadpour K. Health sector reform in Islamic Republic of Iran. J Inflamm Dis. (2006) 10:7–20. Available online at: http://journal.qums.ac.ir/article-1-110-en.html
55. Yagub AI. Collaboration between government and non-governmental organizations (NGOs) in delivering curative health Services in North Darfur State, Sudan-a National Report. Iran J Public Health. (2014) 43:561–71.
56. Hushie M. Public-non-governmental organisation partnerships for health: an exploratory study with case studies from recent Ghanaian experience. BMC Public Health. (2016) 16:1–13. doi: 10.1186/s12889-016-3636-2
Keywords: non-governmental organizations, universal health coverage, services coverage, population coverage, financial coverage, health system research and policy
Citation: Sanadgol A, Doshmangir L, Khodayari-Zarnaq R and Sergeevich Gordeev V (2022) Role of non-governmental organizations in moving toward universal health coverage: A case study in Iran. Front. Public Health 10:985079. doi: 10.3389/fpubh.2022.985079
Received: 03 July 2022; Accepted: 28 September 2022;
Published: 20 October 2022.
Edited by:
Hongping Yuan, Guangzhou University, ChinaReviewed by:
Michael Thiede, IU International University of Applied Sciences, GermanyJolanta Wierzba, Medical University of Gdansk, Poland
Copyright © 2022 Sanadgol, Doshmangir, Khodayari-Zarnaq and Sergeevich Gordeev. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Leila Doshmangir, leiladoshmangir.tbzmed@gmail.com
 Arman Sanadgol
Arman Sanadgol