
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 21 November 2022
Sec. Occupational Health and Safety
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.981592
This article is part of the Research Topic Employee Experience, Occupational Health, and Organizational Supportive Factors: From an Integrated Perspective View all 40 articles
A correction has been applied to this article in:
Corrigendum: Limited social support is associated with depression, anxiety, and insomnia in a Japanese working population
 Chie Omichi1,2†
Chie Omichi1,2† Yuki Kaminishi1†
Yuki Kaminishi1† Hiroshi Kadotani1*†
Hiroshi Kadotani1*† Yukiyoshi Sumi1†
Yukiyoshi Sumi1† Ayaka Ubara1,3†
Ayaka Ubara1,3† Kohei Nishikawa1,4†
Kohei Nishikawa1,4† Arichika Matsuda1
Arichika Matsuda1 Yuji Ozeki1† on behalf of NinJaSleep Study Group1
Yuji Ozeki1† on behalf of NinJaSleep Study Group1Background: Lack of social support is associated with depression, anxiety, and insomnia. This study aimed to determine the source of support related to depression, anxiety, and insomnia among Japanese workers.
Methods: As part of a cohort study, we conducted a questionnaire survey among city government employees in Koka City, Shiga Prefecture, Japan, from September 2021 to March 2022. We used the Patient Health Questionnaire-9 (PHQ-9), Generalized Anxiety Disorder−7 (GAD-7), and Insomnia Severity Index (ISI) to assess depressive symptoms, anxiety symptoms, and insomnia, respectively. We used the Brief Job Stress Questionnaire (BJSQ) to assess job stressors and social support (from supervisors, colleagues, and family).
Results: A total of 1,852 Japanese employees (38.4% male, 45.9 ± 12.9 years) participated in the survey, with 15.5, 10.8, and 8.2% of the participants having depressive symptoms (PHQ-9 ≥ 10), anxiety symptoms (GAD-7 ≥ 10), and insomnia (ISI ≥ 15), respectively. The logistic regression analysis suggested that job stressors were associated with depressive symptoms (p < 0.001), anxiety symptoms (p < 0.001), and insomnia (p = 0.009). In contrast, support from co-workers (p = 0.016) and family members (p = 0.001) was associated with decreased depressive symptoms. Support from family members was associated with decreased insomnia (p = 0.005).
Conclusion: Social support from co-workers and family may be associated with reduced depressive symptoms, and family support may be associated with reduced insomnia in the Japanese working population.
Clinical trial registration: https://clinicaltrials.gov/ct2/show/NCT03276585.
Stress in individual workers and the work environment has been reported to be associated with chronic absenteeism, turnover, suicide, and family disruption (1–3). A previous study reported that 40% of U.S. workers rated their jobs as very or extremely stressful and that 26% were often or very often burned out or stressed by their work (4). The National Institute for Occupational Safety and Health (NIOSH) defines occupational stress as “the harmful physical and emotional responses that occur when the requirements of the job do not match the capabilities, resources, or needs of the worker (4).” In the NIOSH model of job stress, stressful job conditions may lead to the risk of injury and illness, and individual and situational factors can modify and protect workers from risk (4).
Job stressors (exposure to stressful working conditions) may cause negative outcomes such as depression, anxiety, and insomnia (5). Depression is a major global public health problem and is projected to greatly contribute to disease burden worldwide in the coming decades (6, 7). Insomnia commonly occurs as a principal component of depression (8) and causes presenteeism (low work productivity due to being present at work, but ill or experiencing medical conditions) (9). Depression and anxiety are the two most prevalent mental disorders in the Japanese population (10, 11).
Social support is defined as a perception leading a person to believe that they are cared for and loved, esteemed, and a member of a network of mutual obligations (12). A systemic review indicated that low co-worker support and low supervisor support predicted the incidence of stress-related diseases, together with high job demands, low job control, low procedural justice, low relational justice, and a high effort-reward imbalance (13). A meta-analysis indicated that a high level of job stress, effort-reward imbalance, high demand, heavy workload, and low social support are associated with insomnia (14). Social support includes received and perceived social support. Received social support refers to the amount of support received, while perceived social support refers to its adequacy and availability (15). Research has shown that perceived social support is more closely related to mental health than received social support (16). Bidirectional associations were found between depressive and anxiety symptoms and loneliness (17). Loneliness was a stronger predictor of depressive and anxiety symptoms relative to the reverse causal direction. High loneliness may be a key risk factor for the development of future anxiety or depressive symptoms (17), thus, perceived social support not only from the workplace but also from family/friends may be important to decrease depression and anxiety levels in workplaces. According to a systemic review on depression and work-related risk factors, previous studies mainly reported support from supervisors and co-workers, but studies reporting support from family/friends were very limited (18). In another review of job stress, anxiety, and depression, family support was not mentioned (19). In a systemic review on insomnia and job stress, three studies reported social support, one reported support from supervisors or co-workers, and two did not report the origin of support (14).
Some studies analyzed the association between depression, anxiety, and insomnia among Japanese workers (20–24). Honda et al. reported that having little conversation with co-workers and/or supervisors was a risk factor for psychological distress among Japanese workers (20). Nishitani and Sakakibara reported that insomnia was related to the psychological response of depression in Japanese male workers of a manufacturing plant (21). Toyoshima et al. reported that insomnia directly affected state anxiety among Tokyo Medical University employees (22). Deguchi et al. reported that anxious temperament and role conflict were associated with insomnia among Japanese local government employees (23). Saojyo et al. found a synergistic association of job control and social support at work with depression and insomnia among Japanese government employees (24). However, these are cross-sectional studies, and depression, anxiety, insomnia, and social support (both at work and at home) were not simultaneously analyzed.
We hypothesized that lack of social support is associated with depressive symptoms, anxiety symptoms, and insomnia in the Japanese working population. The purpose of this study was to test this hypothesis and determine the source of support related to depression, anxiety, and insomnia among cohort study (NinJaSleep Study) participants.
We have performed a cohort study on sleep and mental health in a Japanese working population, named the Night in Japan Home Sleep Monitoring Study (NinJaSleep Study) (8, 25, 26). We conducted questionnaire surveys on sleep, mental health, and job stress among local government employees of Koka City, a rural city in Shiga Prefecture, Japan, which is known as the home of the ninja. Employees (n = 2081) were recruited for the questionnaire survey, and 1,852 employees participated in the survey from September 2021 to March 2022 (Figure 1).
The Ethics Committee of the Shiga University of Medical Science approved the study protocol (R2017–111). The study was registered at UMIN-CTR (UMIN000028675, registered on 2017/8/15) and ClinicalTrials.gov (NCT03276585, registered on 2017/9/3). Informed consent was obtained from all the participants. The datasets analyzed in this study are available from the corresponding author upon reasonable request.
Job stress was assessed using the Brief Job Stress Questionnaire (BJSQ) (16), a 57-item multidimensional job stress questionnaire evaluated on a Likert scale of 1 to 4. The BJSQ contains 17, 29, 9, and 2 items that assess job stressors, stress reactions, social support, and work/life satisfaction, respectively. Job stressors have nine subscales (job demands, job control, meaningfulness of work, work environment, suitability for work, physical burden, skill utilization, required job quality, and interpersonal relationships), with scores ranging from 17 to 68 and higher scores suggesting higher job stress levels.
“Social Support” included three subscales (supervisors, co-workers, and family), with scores ranging from 3 to 12 for each subscale and lower scores suggesting better support. “How freely can you talk with the following people?,” “How reliable are the following people when you are troubled?,” and “How well will the following people listen to you when you ask for advice on personal matters?” were asked about superiors, co-workers, and family (spouse, family, friends, etc.) on a four-point scale (1 = extremely, 2 = very much, 3 = somewhat, and 4 = not at all). The sum of the scores for superiors, co-workers, and family were separately calculated to indicate social support, with a range of 3–12 for each category. Cronbach's alpha coefficients for job demand, job control, and social support from supervisors, coworkers, and family/friends were reported to be 0.77–0.83, 0.68–0.69, 0.79–0.89, 0.76–0.85, and 0.83–0.86, respectively (27, 28). All BJSQ scales have been proven to have acceptable or high levels of internal consistency reliability and factor-based validity (27, 29). Workers with high job stress levels were identified using the BJSQ scoring program ver. 3.5 (Ministry of Health, Labor, and Welfare, Tokyo, Japan).
The Patient Health Questionnaire-9 (PHQ-9) is a 9-item questionnaire designed to screen for depression/depressive symptoms in clinical and research settings (30). The PHQ-9 contains items derived from the DSM-IV classification system pertaining to (1) anhedonia, (2) depressed mood, (3) trouble sleeping, (4) feeling tired, (5) change in appetite, (6) guilt or worthlessness, (7) trouble concentrating, (8) feeling slowed down or restless, and (9) suicidal thoughts; each item is scored from “0” (not at all) to “3” (nearly every day) (30). The standard cutoff score for screening to identify possible major depression/depressive symptoms is ≥ 10. In previous studies, participants with a PHQ-9 score ≥ 10 were classified as having depression (30, 31). According to a meta-analysis comparing PHQ-9 with validated diagnostic interviews, PHQ-9 had a sensitivity and specificity of 0.85 (95% confidence interval (CI):0.79–0.89) and 0.85 (95% CI: 0.82–0.87) to detect major depression, respectively (32).
The 7-item Generalized Anxiety Disorder Scale (GAD-7) is a widely used tool for assessing the frequency of anxiety symptoms in the past 2 weeks on a scale of “0” (not at all) to “3” (nearly every day) (33). The sum of the scores ranges from 0 to 21. Participants with GAD-7 scores ≥ 10 were classified as having moderate anxiety symptoms, indicating a need for further diagnostic testing (34).
Insomnia severity was measured using the Japanese version of the Insomnia Severity Index (ISI) (35), a validated 7-item self-report questionnaire that assesses insomnia severity over the past 3 weeks. The total score ranges from 0 to 28, with lower scores indicating fewer insomnia symptoms. Severity levels were categorized as no insomnia (0–7 points), sub-threshold (mild) insomnia (8–14 points), moderate insomnia (15–21 points), or severe insomnia (≥ 22 points) (36).
All these questionnaires were self-administered. Participants with symptoms of insomnia, anxiety, and depression were defined as having ISI ≥ 15, GAD-7 ≥ 10, and PHQ-9 ≥ 10, respectively.
Demographic data, including birth year and month, height (cm), body weight (kg), sex, and history of chronic conditions such as hypertension, diabetes, and lipidemia were also collected. Age in September 2021 was calculated from birth year and month; BMI was calculated from height and body weight; and history of diagnosis (yes/no) of hypertension, diabetes, and lipidemia were asked.
We compared proportions between groups using the χ2 test and analyzed continuous data using the t-test.
We performed a logistic regression analysis with depressive symptoms (PHQ-9 ≥ 10), anxiety symptoms (GAD-7 ≥ 10), and insomnia (ISI ≥ 15) as dependent variables after adjusting for age, sex, BMI, job stressors, support from supervisors, support from co-workers, support from family, and high job stress. The results of high job stress analysis were assessed using the BJSQ in the previous year for two reasons. First, since the BJSQ determines high stress based on job stressor and social support, it may be not appropriate to analyze correlations using high stress determinations from the same year. Second, after high job stress was detected, workers who experienced this were expected to be cared for by their supervisors, co-workers, and family. Thus, the high job stress in the previous year may have affected their support.
We performed a linear regression analysis as a sensitivity analysis using the PHQ-9, GAD-7, or ISI scores as dependent values. All models included job stressors, and support from supervisors, co-workers, and family.
All data were analyzed using SPSS 25.0, statistical software (SPSS Inc., Chicago, IL), and MedCalc ver. 20.106 (MedCalc Software Ltd., Ostend, Belgium). Differences were considered statistically significant at p < 0.05.
The participation rate was 89.0% (1852/2081). Among the eligible participants, 38.4 and 61.6% were males and females, respectively (Table 1). Furthermore, 15.5, 10.8, and 8.2 of the participants had depression (PHQ-9 ≥ 10), anxiety (GAD-7 ≥ 10), and insomnia (ISI ≥ 15), respectively (Table 1). Of the participants, 41.8, 52.4, 5.7, and 0.1% classified their occupation as administrative/clerical, educational/teaching, medical/health support, or temporary/contracted, respectively. Of these jobs, 2.8% were night shifts.
Job stressors and support from supervisors, co-workers, and family members were significantly associated with depressive symptoms, anxiety symptoms, and insomnia (Table 2). We further analyzed the association between depressive symptoms, anxiety symptoms, insomnia, job stressors, and social support using logistic regression analysis (Table 3). Job stressors as well as lack of support from supervisors, co-workers, and family were associated with depressive symptoms, anxiety symptoms, and insomnia in the unadjusted model. In the adjusted model, job stressors were significantly associated with depressive and anxiety symptoms and insomnia. Support from co-workers and family members was associated with depressive symptoms, and family support was associated with insomnia. For sensitivity analysis, we performed a linear regression analysis. The results of the linear regression analysis were like those of the adjusted logistic regression analysis (Table 4).
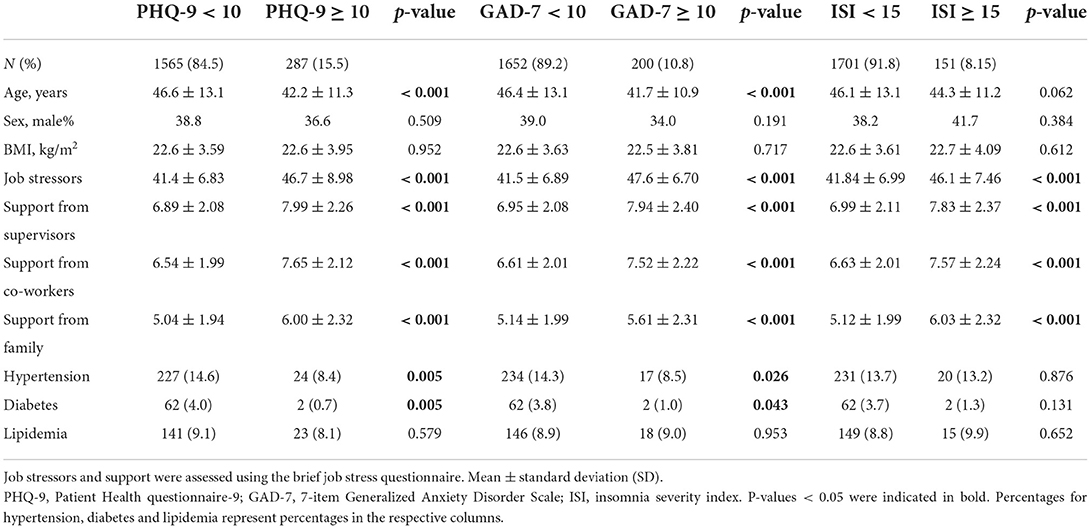
Table 2. Comparison between participants with and without depressive symptoms, anxiety symptoms, and insomnia.
When workers had high job stress levels, job stressors decreased and support from supervisors and co-workers improved in the following year (Table 5). However, support from the family did not change. When the distribution of participants with and without high job stress levels in 2020 was analyzed separately, apparent differences were observed in job stressors, support from supervisors, and support from co-workers (Figure 2).
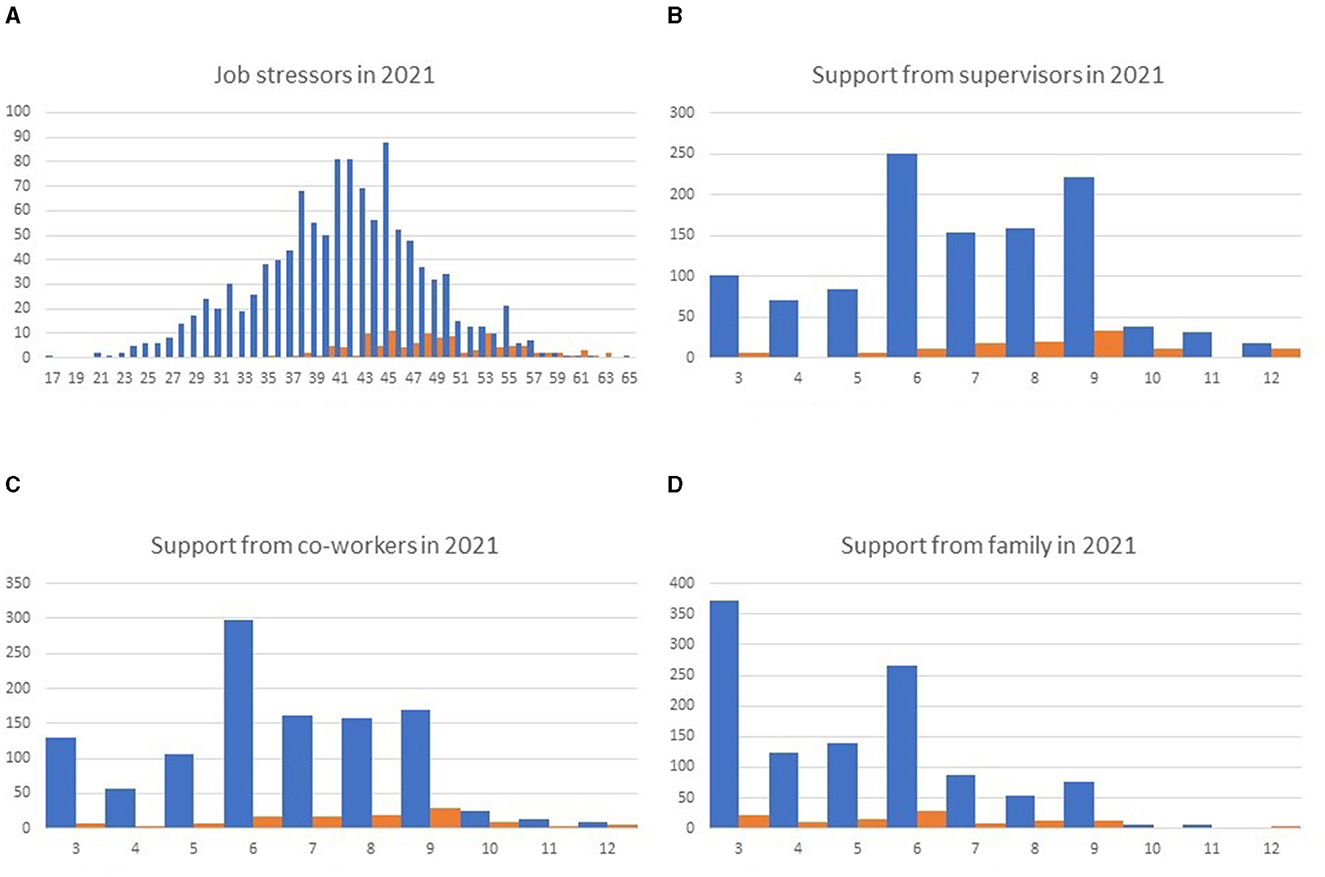
Figure 2. Histogram of stressors and support scores in 2021, classified according to the presence (orange) or absence (blue) of high stress levels in 2020. Job stressors (A) and support from supervisors (B), co–workers (C), and family (D) are presented. A smaller number of job stressors suggests less job stress. Smaller scores in the responses to the questions about support suggest a better support situation.
A questionnaire survey was conducted to analyze the association between social support and mental health outcomes in the Japanese working population. Higher scores on social support in the BJSQ (suggesting poorer support) were associated with higher PHQ-9, GAD-7, and ISI scores (suggesting severe symptoms of depression, anxiety, and insomnia, respectively) (Tables 2, 3). High job demand (increased workload/time pressure), low job control (minimal decision-making), and low social support have been reported to be associated with poorer employee mental health (37) and insomnia (38). Thus, social support may be important for preventing mental health problems in the working population.
The development of the BJSQ was based on the NIOSH job stress model (39). In the BJSQ, job stressors may include stressful job conditions, and social support may suggest individual and situational factors in the model (40). Job stressors were significantly associated with depression, anxiety, and insomnia in all analyses. Higher social support scores, which suggest poorer support, were associated with worse outcomes (higher PHQ-9, GAD-7, and ISI scores). These results may fit well with the NIOSH job stress model (4).
We found that lack of support from co-workers and family was associated with depressive symptoms and that lack of support from family was associated with insomnia. Support from closer groups seems to work protectively against depression and insomnia.
Comparing the presence of high stress levels in the previous year with changes in workplace stressors and social support in that year and the following year, the high stress level group showed a decrease in workplace stressors and improved support from supervisors and coworkers. This suggests that the high stress level-related decisions led to an improvement in the work environment in the following year.
In the previous year's high stress level group, the degree of family support did not change between that year and the following year. On the other hand, a logistic regression analysis of the relationship between family support and outcomes such as depression and insomnia in the same year showed a significant correlation. It is possible that family support may have already been provided sufficiently when the patient was determined to be highly stressed in the previous year.
Stressors and social support were compared in histograms stratified by the presence or absence of high stress levels in the previous year. The distribution of family support showed no clear relationship with the presence or absence of high stress levels in the previous year. On the other hand, the distribution of stressors and support from supervisors and co-workers apparently differed depending on the presence or absence of high stress levels in the previous year. These results suggest that family members may have already provided sufficient support to those in the high stress level group in the previous year and that although support from supervisors and co-workers improved after the high stress level rating, there may be still room for further improvement.
A systematic review of human resource management training programs aimed at teaching supervisors how to reduce employees' psychosocial stress reported only poor quality and inconsistent results (39). Some studies have suggested that supervisor training may be beneficial, but others have shown no improvement when compared with the absence of intervention (39). Both in-person (face-to-face) (41) and computer-based (web- and mobile-based) stress-management interventions (42) have reportedly been effective in reducing job stress levels. In this study, support from supervisors improved between the first and second years of the study but was not significantly associated with employee outcomes. However, a reduction in job stress levels was associated with decreased depression, anxiety, and insomnia. Stress-management interventions and reduction in job stressors may be more effective strategies than supervisor education to reduce workplace stress. We found that family support protects against depression and insomnia.
This study had some limitations. Our target population was government employees in a rural city in Japan. Our results cannot be generalized to other parts of Japan or other countries without further investigations. We plan to use the results of this study in our activities as occupational physicians to provide interventions aimed at reducing long-term absence and turnover through improved social support in multiple workplaces. This was a questionnaire survey, and structured interviews were not performed to diagnose depression, anxiety, insomnia, or other mental disorders. Social support was also assessed using a questionnaire asking how the participants recognized support but did not ask how much support was provided. However, perceived social support has been reported to have significantly higher effects than actual social support on promoting mental health (43).
The results of this cohort study have been displayed as posters in the cafeteria of the City Hall and lectures have been held to publicize the results to the participants (25). We plan to publicize the results of the present study in the same manner. We believe that incorporating into workplace training programs the usefulness of social support from supervisors and coworkers in improving depression, anxiety disorders, and insomnia will be useful in preventing these problems in the workplace.
In conclusion, social support from co-workers and family may be associated with decreased depressive symptoms, and family support may be associated with decreased insomnia in the Japanese working population. Anxiety symptoms were mainly associated with job stressors.
The datasets analyzed in this study are available from the corresponding author upon reasonable request.
The studies involving human participants were reviewed and approved by the Ethics Committee of the Shiga University of Medical Science. The patients/participants provided their written informed consent to participate in this study.
Conceptualization: YK and HK. Methodology, software, formal analysis, writing original draft preparation, visualization, supervision, and funding acquisition: HK. Validation: YS. Investigation: CO and HK. Resources: KN and HK. Data acquisition: the NinJaSleep Study Group. Data curation: CO. Writing review and editing: YK, CO, YS, AU, KN, AM, and YO. Project administration: YO. All authors have read and agreed to the published version of the manuscript.
This work was supported in part by a research grant from the Investigator-Initiated Studies Program of Merck Sharp & Dohme LLC/MSD K.K. HK received grants from Eisai Co., Ltd., (HHCS20210930005) and SECOM Science and Technology Foundation. HK reported consulting fees from Takeda Pharmaceutical Co. Ltd. HK, AU, and AM were associated with a laboratory that was supported by donations from Fukuda Lifetech Co., Ltd., and Fukuda Life Tech Keiji Co., Ltd., to the Shiga University of Medical Science. JSPS KAKENHI grant number 22K18384.
We express our gratitude to the participants of Koka city. We thank T. Toyoda, R. Matsumoto, A. Toguchi, S. Sawada, H. Nakayama, M. Kawasaki, K. Konishi, K. Awazu, and A. Sagara for their assistance with the data collection. The complete list of collaborators in the Nin JaSleep Study is as follows: Hiroshi Kadotani, Chie Omichi, Yukiyoshi Sumi, Ayaka Ubara, Kohei Nishikawa, Arichika Matsuda, Aiko Sagara, Taeko Toyoda, Yuji Ozeki (Department of Psychiatry, Shiga University of Medical Science), Hitoshi Yamanaka, Keitaro Miyaji, and Isao Kikuchi (Koka City).
This work was supported in part by a research grant from the Investigator-Initiated Studies Program of Merck Sharp & Dohme LLC/MSD K.K. The opinions expressed in this paper are those of the authors and do not necessarily represent those of Merck Sharp & Dohme LLC / MSD K.K. HK received grants from Eisai Co., Ltd., and the SECOM Science and Technology Foundation. HK reports consulting fees from Takeda Pharmaceutical Co., Ltd., HK, AU, and AM were associated with a laboratory that was supported by donations from Fukuda Lifetech Co., Ltd., and Fukuda Life Tech Keiji Co., Ltd., to Shiga University of Medical Science. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results. JSPS KAKENHI grant number 22K18384.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Inoue A, Tsutsumi A, Kachi Y, Eguchi H, Shimazu A, Kawakami N. Psychosocial work environment explains the association of job Dissatisfaction with long-term sickness absence: a one-year prospect study of Japanese employees. J Epidemiol. (2020) 30:390–5. doi: 10.2188/jea.JE20190050
2. Kachi Y, Inoue A, Eguchi H, Kawakami N, Shimazu A, Tsutsumi A. Occupational stress and the risk of turnover: a large prospective cohort study of employees in Japan. BMC Public Health. (2020) 20:174. doi: 10.1186/s12889-020-8289-5
3. Bhui KS, Dinos S, Stansfeld SA, White PD, A. synthesis of the evidence for managing stress at work: a review of the reviews reporting on anxiety, depression, and absenteeism. J Environ Public Health. (2012) 2012:515874. doi: 10.1155/2012/515874
4. Sauter S, Murphy L, Colligan M, Swanson N, Hurrell J Jr., Scharf F Jr. Stress at work: U.S. Department of Health Human Services. Public Health Service Centers for Disease Control Prevention, National Institute for Occupational Safety Health.. (1999) DHHS (NIOSH) Publication No. 99-101:1-26. Available online at: https://www.cdc.gov/niosh/docs/99-101/ (accessed May 30, 2022).
5. Kato M. Final development of the brief job stress questionnaire mainly used for assessment of the individuals. In: The Ministry of Labour Sponsored Grant for The Prevention Of Work-Related Illness. Tokyo: Tokyo Medical University (2000). p. 126–64.
6. Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. (2012) 380:2197–223. doi: 10.1016/S0140-6736(12)61690-0
7. Baglioni C, Spiegelhalder K, Nissen C, Riemann D. Clinical implications of the causal relationship between insomnia and depression: how individually tailored treatment of sleeping difficulties could prevent the onset of depression. EPMA J. (2011) 2:287–93. doi: 10.1007/s13167-011-0079-9
8. Takami M, Kadotani H, Nishikawa K, Sumi Y, Nakabayashi T, Fujii Y, et al. Quality of life, depression, and productivity of city government employees in Japan: a comparison study using the Athens insomnia scale and insomnia severity index. Sleep Sci Pract. (2018) 2:1–8. doi: 10.1186/s41606-018-0024-0
9. Itani O, Kaneita Y, Otsuka Y, Tokiya M, Jike M, Matsumoto Y, et al. A cross-sectional epidemiological study of the relationship between sleep duration, quality, and rhythm and presenteeism in workers. Sleep Biol Rhythms. (2022) 20:53–63. doi: 10.1007/s41105-021-00339-4
10. Kadotani T, Kadotani H, Arai H, Takami M, Ito H, Matsuo M, et al. Comparison of self-reported scales and structured interviews for the assessment of depression in an urban male working population in Japan: a cross-sectional survey. Sleep Sci Pract. (2017) 1:1–7. doi: 10.1186/s41606-017-0010-y
11. Kawakami N, Takeshima T, Ono Y, Uda H, Hata Y, Nakane Y, et al. Twelve-month prevalence, severity, and treatment of common mental disorders in communities in Japan: preliminary finding from the world mental health Japan survey 2002–2003. Psychiatry Clin Neurosci. (2005) 59:441–52. doi: 10.1111/j.1440-1819.2005.01397.x
12. Cobb S. Social support as a moderator of life stress. Psychosom Med. (1976) 38:300–14. doi: 10.1097/00006842-197609000-00003
13. Nieuwenhuijsen K, Bruinvels D, Frings-Dresen M. Psychosocial work environment and stress-related disorders, a systematic review. Occup Med (Lond). (2010) 60:277–86. doi: 10.1093/occmed/kqq081
14. Yang B, Wang Y, Cui F, Huang T, Sheng P, Shi T, et al. Association between insomnia and job stress: a meta-analysis. Sleep Breath. (2018) 22:1221–31. doi: 10.1007/s11325-018-1682-y
15. Haber MG, Cohen JL, Lucas T, Baltes BB. The relationship between self-reported received and perceived social support: a meta-analytic review. Am J Community Psychol. (2007) 39:133–44. doi: 10.1007/s10464-007-9100-9
16. Eagle DE, Hybels CF, Proeschold-Bell RJ. Perceived social support, received social support, and depression among clergy. J Soc Pers Relatsh. (2019) 36:2055–73. doi: 10.1177/0265407518776134
17. McDowell CP, Meyer JD, Russell DW, Sue Brower C, Lansing J, Herring MP. Bidirectional associations between depressive and anxiety symptoms and loneliness during the COVID-19 pandemic: dynamic panel models with fixed effects. Front Psychiatry. (2021) 12:738892. doi: 10.3389/fpsyt.2021.738892
18. Saade S, Parent-Lamarche A, Bazarbachi Z, Ezzeddine R, Ariss R. Depressive symptoms in helping professions: a systematic review of prevalence rates and work-related risk factors. Int Arch Occup Environ Health. (2022) 95:67–116. doi: 10.1007/s00420-021-01783-y
19. Bhui KS, Dinos S, Stansfeld SA, White PD. A synthesis of the evidence for managing stress at work: a review of the reviews reporting on anxiety, depression, and absenteeism. J Environ Public Health. (2012) 2012:515874.
20. Honda A, Date Y, Abe Y, Aoyagi K, Honda S. Work-related stress, caregiver role, and depressive symptoms among Japanese workers. Saf Health Work. (2014) 5:7–12. doi: 10.1016/j.shaw.2013.11.002
21. Nishitani N, Sakakibara H. Job stress factors, stress response, and social support in association with insomnia of Japanese male workers. Ind Health. (2010) 48:178–84. doi: 10.2486/indhealth.48.178
22. Toyoshima K, Inoue T, Shimura A, Uchida Y, Masuya J, Fujimura Y, et al. Mediating roles of cognitive complaints on relationships between insomnia, state anxiety, and presenteeism in Japanese adult workers. Int J Environ Res Public Health. (2021) 18:4516. doi: 10.3390/ijerph18094516
23. Deguchi Y, Iwasaki S, Ishimoto H, Ogawa K, Fukuda Y, Nitta T, et al. Relationships between temperaments, occupational stress, and insomnia among Japanese workers. PLoS ONE. (2017) 12:e0175346. doi: 10.1371/journal.pone.0175346
24. Saijo Y, Chiba S, Yoshioka E, Nakagi Y, Ito T, Kitaoka-Higashiguchi K, et al. Synergistic interaction between job control and social support at work on depression, burnout, and insomnia among Japanese civil servants. Int Arch Occup Environ Health. (2015) 88:143–52. doi: 10.1007/s00420-014-0945-6
25. Omichi C, Kadotani H, Sumi Y, Ubara A, Nishikawa K, Matsuda A, et al. Prolonged sleep latency and reduced REM latency are associated with depressive symptoms in a Japanese working population. Int J Environ Res Public Health. (2022) 19:2112. doi: 10.3390/ijerph19042112
26. Fujiwara K, Goto Y, Sumi Y, Kano M, Kadotani H. Sleep-EEG-based parameters for discriminating fatigue and sleepiness. Front Sleep. (2022) 1:975415. doi: 10.3389/frsle.2022.975415
27. Shimomitsu T, Haratani T, Nakamura K, Kawakami N, Hayashi T, Hiro H, et al. The final development of the brief job stress questionnaire mainly used for assessment of the individuals. In:Kato M, , editor. The Ministry of Labour Sponsored Grant for the Prevention of Work-Related Illness: the 1999 report. Tokyo: Tokyo Medical College (2000). p. 126–64.
28. Otsuka T, Kawada T, Ibuki C, Kusama Y. Relationship between job strain and radial arterial wave reflection in middle-aged male workers. Prev Med. (2009) 49:260–4. doi: 10.1016/j.ypmed.2009.07.005
29. Ito S, Fujita S, Matumoto K, Kitazawa T, Seto K, Hasegawa Y. Factorial structure for the Breaf Job Stress Questionnaire in Japanese health care workers. J Med Soc Toho Univ (2013) 60(1):15–23. doi: 10.14994/tohoigaku.60.15
30. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
31. Gilbody S, Richards D, Brealey S, Hewitt C. Screening for depression in medical settings with the patient health questionnaire (PHQ): a diagnostic meta-analysis. J Gen Intern Med. (2007) 22:1596–602. doi: 10.1007/s11606-007-0333-y
32. Levis B, Benedetti A, Thombs BD. DEPRESsion Screening Data (DEPRESSD) Collaboration. Accuracy of patient health Questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ. (2019) 365:l1476. doi: 10.1136/bmj.l1476
33. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
34. Plummer F, Manea L, Trepel D, McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. (2016) 39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005
35. Munezawa T, Inoue Y, Morin CM, Nedate K. Development of the Japanese version of the Insomnia Severity Index (ISI-J). Jpn J Psychiatr Treat. (2009) 24:219–25.
36. Bastien CH, Vallières A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. (2001) 2:297–307. doi: 10.1016/S1389-9457(00)00065-4
37. Harvey SB, Modini M, Joyce S, Milligan-Saville JS, Tan L, Mykletun A, et al. Can work make you mentally ill? A systematic meta-review of work-related risk factors for common mental health problems. Occup Environ Med. (2017) 74:301–10. doi: 10.1136/oemed-2016-104015
38. Portela LF, Kröning Luna CK, Rotenberg L, Silva-Costa A, Toivanen S, Araújo T, et al. Job strain and self-reported insomnia symptoms among nurses: what about the influence of emotional demands and social support? BioMed Res Int. (2015) 2015:820610. doi: 10.1155/2015/820610
39. Kuehnl A, Seubert C, Rehfuess E, von Elm E, Nowak D, Glaser J. Human resource management training of supervisors for improving health and well-being of employees. Cochrane Database Syst Rev. (2019) 9:CD010905. doi: 10.1002/14651858.CD010905.pub2
40. Ministry Ministry of Health Labour Welfare Labour Standards Bureau Health Safety Department. Stress Check System Implementation Manual Based on the Occupational Health and Safety Law. (2015). Available online at: https://www.mhlw.go.jp/content/000533925.pdf (accessed May 30, 2022).
41. Ruotsalainen JH, Verbeek JH, Mariné A, Serra C. Preventing occupational stress in healthcare workers. Cochrane Database Syst Rev. (2015) 13:CD002892. doi: 10.1002/14651858.CD002892.pub5
42. Phillips EA, Gordeev VS, Schreyögg J. Effectiveness of occupational e-mental health interventions: a systematic review and meta-analysis of randomized controlled trials. Scand J Work Environ Health. (2019) 45:560–76. doi: 10.5271/sjweh.3839
Keywords: social support, job stress, depression, anxiety, insomnia, occupational health
Citation: Omichi C, Kaminishi Y, Kadotani H, Sumi Y, Ubara A, Nishikawa K, Matsuda A and Ozeki Y (2022) Limited social support is associated with depression, anxiety, and insomnia in a Japanese working population. Front. Public Health 10:981592. doi: 10.3389/fpubh.2022.981592
Received: 05 August 2022; Accepted: 31 October 2022;
Published: 21 November 2022.
Edited by:
Yongxin Li, Henan University, ChinaReviewed by:
Adam Hege, Appalachian State University, United StatesCopyright © 2022 Omichi, Kaminishi, Kadotani, Sumi, Ubara, Nishikawa, Matsuda and Ozeki. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hiroshi Kadotani, a2Fkb3RhbmlzbGVlcEBnbWFpbC5jb20=
†ORCID: Chie Omichi orcid.org/0000-0003-4851-0301
Yuki Kaminishi orcid.org/0000-0003-2679-2838
Hiroshi Kadotani orcid.org/0000-0001-7474-3315
Yukiyoshi Sumi orcid.org/0000-0001-6775-0883
Ayaka Ubara orcid.org/0000-0003-4966-6703
Kohei Nishikawa orcid.org/0000-0002-7081-4232
Arichika Matsuda orcid.org/0000-0002-3014-9565
Yuji Ozeki orcid.org/0000-0002-9516-0941
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.