
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 27 September 2022
Sec. Children and Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.979402
 Getu Engida Wake1*
Getu Engida Wake1* Kalkidan Chernet2
Kalkidan Chernet2 Almaz Aklilu3
Almaz Aklilu3 Fentahun Yenealem3
Fentahun Yenealem3 Girma Wogie Fitie1
Girma Wogie Fitie1 Michael Amera Tizazu1
Michael Amera Tizazu1 Yohannes Moges Mittiku1
Yohannes Moges Mittiku1 Moges Sisay Chekole1
Moges Sisay Chekole1 Geremew Kindie Behulu1
Geremew Kindie Behulu1Background: According to the World health organization, neonatal mortality is defined as the death of babies within the first 28 days of their lives. The newborn period is the most vulnerable period for a child's survival, with the bulk of neonatal deaths occurring on the first day and week. According to a recent study, about a third of all newborn deaths occur within the first day of life, and nearly three-quarters occur within the first week. This study aimed to assess the determinants of neonatal mortality among neonates admitted to the neonatal intensive care unit in Dessie comprehensive and specialized hospital, northeast Ethiopia.
Methodology: Health institution-based unmatched case-control study was conducted among neonates admitted to Dessie comprehensive and specialized hospital, Ethiopia from February 01 up to March 30, 2020. After keeping cases and controls in separate frames, study participants were chosen using a simple random sampling procedure until the sample size was met. Epi data version 7.0 and SPSS version 25 were used for data entry and analysis respectively. P ≤ 0.05 was used as a cut point of statistical significance in multivariable binary logistic regression.
Results: A total of 698 (233 cases and 465 controls) participated in the study. Pregnancy induced hypertension (AOR = 3.02; 95% CI; 1.47–6.17), public hospital delivery (AOR = 3.44; 95% CI; 1.84–6.42), prematurity (AOR = 2.06; 95% CI; 1.43–2.96), being referred (AOR = 4.71; 95% CI; 3.01–7.39), and hypothermia (AOR = 2.44; 95% CI; 1.56–3.82) were determinant factors of neonatal mortality.
Conclusion: Pregnancy-induced hypertension, public hospital delivery, prematurity, referral, and hypothermia were found to be the determinant factors of neonatal mortality. It would be important to give due attention to neonates delivered from mothers with a history of hypertensive disorder. Besides better to give due attention to neonates delivered in public health institutions, prematurely delivered, referred, and hypothermic neonates. Lastly, further research should be conducted to investigate the additional determinants of neonatal mortality.
According to the World Health Organization, neonatal mortality is defined as the death of babies within the first 28 days of their lives (WHO) (1). Very early, early, and late newborn mortality are the three types of neonatal mortality. The deaths that occur on the first day of life and within the first 7 days of life are referred to as very early and early neonatal mortalities. Late neonatal mortality is defined as deaths that occur after the seventh day but before the 28th day of life (1, 2). The newborn period is the most vulnerable period for a child's survival, with the bulk of neonatal deaths occurring on the first day and week, with around one million dying on the first day and over one million dying within the next 6 days (3). The number of neonatal deaths per 1,000 live births in a given year is known as the neonatal mortality rate (NMR), and it is one of the most sensitive indicators of a community's socioeconomic condition, as well as the availability and accessibility of health care services in the country (1, 4).
On a global scale, 2.4 million newborn deaths occurred in the first 28 days, with around 6,700 deaths every day in 2019 (3). According to a recent study, about a third of all newborn deaths occur within the first day of life, and nearly three-quarters occur within the first week (3).
Almost all newborn deaths occurred in developing nations, and the neonatal period is the most dangerous time for a child under the age of five (5). Six of the 12 nations that accounted for two-thirds of all live-born deaths worldwide were in sub-Saharan Africa, and they accounted for around 60% of all neonatal deaths (5, 6).In Ethiopia, over 87,000 newborns die within the first 28 days of life, making it one of the world's highest rates of neonatal mortality (7).
Similarly, neonatal death rates climbed from 29 per 1,000 live births in the Ethiopian demographic health survey (EDHS2016) to 30 per 1,000 live births in the Ethiopian mini demographic health survey (EMDHS 2019) report (8, 9). Goal three of the Sustainable Development Goals (SDG) to end unnecessary death and disability includes reducing newborn mortality (10).
Over the last few decades, considerable progress has been made in reducing newborn death by adopting favorable health policies and allocating adequate resources to accelerate the accomplishment of neonatal survival goals (11–13). In Ethiopia, the integration of reproductive, maternal, newborn, and child health (RMNCH), policy formation, strong leadership, and cooperation, as well as evidence-based interventions, lowered infant death from 49 to 40% Worldwide in 2016 (14). Furthermore, since 2014, a standard neonatal care procedure has been implemented (15) and in Ethiopia, free maternity and neonatal health services were a huge help in lowering neonatal mortality (16). Even though those trials have lowered newborn mortality in several countries (17), Ethiopia's progress was slow, and it fell well short of the UN's ambitious aim of avoiding unnecessary infant deaths and lowering neonatal mortality to 12 per 1,000 live births in every nation by 2030 (8, 9, 18).
The majority of neonatal mortality is caused by preventable and treatable conditions such as diarrhea, pneumonia, sepsis, asphyxia, and preterm, all of which can be avoided by employing basic mother and child health care services (19, 20). Maternal variables such as antepartum hemorrhage, pregnancy-induced hypertension, and other medical/surgical disorders were linked to early infant death, according to another study (21). Low birth weight (LBW), very low birth weight (VLBW), extreme low birth weight (ELBW), and preterm birth are other neonatal and intrapartum concerns to consider (8, 9, 22, 23), prolonged rupture of membrane, mal-presentation (dystocia), home delivery, and instrument delivery (8, 24–26) were positively associated with neonatal mortality. The Amhara region in Ethiopia has the highest infant mortality rate (47/1,000 live births) (8) and the deaths in the NICU were found to be common (23.1%) (27). As a result, determining the determinant variables of newborn mortality is evidence for inventions and a necessary step in reducing the burden of neonatal deaths (4, 28). Despite the seriousness of the situation, there are inadequacies in research on newborn mortality that has been undertaken in Ethiopia, according to our understanding. As a result, we conducted a case-control study to determine the determinants of neonatal death among neonates hospitalized in the neonatal critical care unit at Dessie Comprehensive Specialized Hospital in Northeast Ethiopia.
From February 01 up to March 30, 2020, the research was carried out at Dessie Comprehensive and Specialized Hospital. Dessie is the capital city of the South Wollo Zone and is located 401 kilometers from Ethiopia's capital, Addis Ababa. The hospital is one of Ethiopia's Comprehensive Specialized Level Hospitals, serving more than 8 million people in Northeast Ethiopia. Since September 2012, it has provided neonatal intensive care unit (NICU) services and currently, the facility is divided into three sections: Kangaroo Mother Care (KMC), term, and preterm. The facility has 37 beds, five phototherapy machines, five incubators, 12 radiant warmers, four heaters, three mechanical ventilators, three oxygen concentrators, and 11 oxygen cylinders filled every 15 days. Continuous positive airway pressure (CPAP) was also made with locally available items such as a Ringer's lactated solution bag, tap water, and an oxygen cylinder.
All neonates, admitted to the NICU of Dessie Comprehensive and Specialized Hospital, were a source population.
All neonates, those were admitted to the NICU of Dessie comprehensive and specialized hospital and had a death summary from February 01 up to March 30, 2020.
All neonates admitted to NICU of Dessie comprehensive and specialized hospital, who were discharged alive from February 01 up to March 30, 2020.
The sample size for an unmatched case-control study was estimated using Epi data software version 7.0 under the assumption of a double population proportion formula, taking into account the following parameters: The maximum sample size was obtained by using low birth weight (LBW) as a determinant factor from a previous study conducted in Adama, Ethiopia, where the proportion of exposure among cases was 60% and among controls was 36% with an odds ratio of 1.6 and different sample sizes were produced from previously identified determinants of neonatal mortality (19). Based on the provided data, the maximum final sample size was 698 (233 cases and 465 controls).
A registration book from a neonatal intensive care unit (NICU) was used to select study participants. Then, after keeping cases and controls in separate frames, the final research participants were chosen using a simple random sampling procedure from a list of case and control groups received from the registration book until the sample size was met. Two controls were randomly selected from the frame of the register for each case using a computer-generated random sampling approach, and this procedure was repeated until the needed sample size was reached Figure 1.
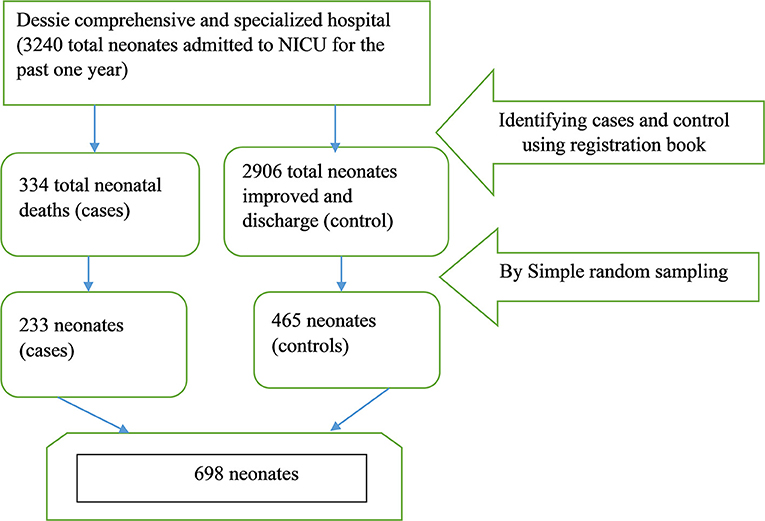
Figure 1. A diagram of the sampling technique among NICU admitted newborns in Dessie Comprehensive and Specialized Hospital was presented from February 1/2020 to March 30/2020.
Neonatal mortality.
Maternal characteristics: Age, parity, antenatal care visit, pregnancy and delivery complications such as pregnancy-induced hypertension, antepartum hemorrhage, preterm rupture membrane, and site and mode of delivery are all factors to consider.
Neonatal characteristics include gestational age at birth, weight, birth type, breastfeeding within 1 h of birth, referred neonate, referral location, the temperature at admission time, and cause for NICU hospitalization [congenital anomaly, asphyxia, sepsis, jaundice, respiratory distress syndrome (RDS), meconium aspiration syndrome (MAS)].
Data were collected through chart reviews using a pre-tested checklist adapted from kinds of literature (29–32). The checklist includes three sections; maternal-related characteristics, and neonatal-related variables. The data were collected by a five-degree pharmacy using an English version checklist under strict daily supervision. The supervision was done by the Principal investigator and one M.Sc. Midwife Supervisor.
Before being utilized to collect the real data, the checklist was converted to English language and pretested on 35 neonates at Dessie comprehensive and specialized hospital. Data collectors and supervisors received a 1-day training session on the data collection tool and procedure. During data collection, the questionnaires were given codes. The principal investigator and supervisor kept a close eye on the data to ensure that it was complete and consistent during the data collection period.
Data were cleaned, coded, and put into Epi data version 7.0 before being exported to SPSS version 25. For the cases and controls, summary statistics such as median and Interquartile Range (IQR) were calculated. The independent variables were compared between cases and controls in a cross-tabulation. Then, to analyze the crude relationship between the independent and outcome variables, bivariable binary logistic regression was used. To analyze the net effect by controlling confounders, factors having a P < 0.25 in bivariable binary logistic regression were put into a multivariable binary logistic regression. In multivariable binary logistic regression, factors with a p < 0.05 were considered statistically significant determinants of Neonatal Mortality.
A total of 233 cases and 465 controls were included in this investigation. Approximately (84.1%) of cases and (85.6%) of controls were delivered by women aged 20–34. The majority of mothers in both cases (98.3%) and controls (97.2%) had an antenatal care (ANC) visit. Premature rupture of membrane occurred in about (11.6%) of cases and (7.5%) of controls. More than half of the cases (53.6%) and controls (57.8%) were delivered naturally through the vaginal canal. Preterm newborns made up around half of the cases (51%) and roughly (27.5%) of the controls. Low birth weight was seen in more than half of the cases (54.9%) and 151 (32.5%) of the controls. The majority of cases (85.4%) and controls (82.6%) were singleton births. Hypothermia affected more than half of the cases (77.3%) and 270 (58.1%) of the controls. About (16.7%) of cases and (13.3%) of controls had asphyxia. Respiratory distress syndromes (RDS) were found in less than half of the cases (33.5%) and 103 (22.2%) of the controls (Table 1).

Table 1. Maternal and neonatal related factors for neonates admitted to neonatal intensive care unit of Dessie comprehensive and specialized hospital, Northeast Ethiopia, 2020 (n = 698).
In bivariable binary logistic regression analyses variables such as neonates delivered from mothers who had a history of the premature rupture of membrane and pregnancy-induced hypertension, place of delivery, mode of delivery, gestational age, birth weight, referred neonates, Breastfeeding initiation time, presence of hypothermia, asphyxia and respiratory distress syndrome (RDS) were significantly associated with neonatal mortality. After controlling for potential confounders on multivariable binary logistic regression analysis; neonates delivered from mothers who had pregnancy-induced hypertension, Place of delivery, prematurity, referred neonates, and presence of hypothermia were identified as determinant factors of neonatal mortality. Accordingly, neonates delivered from mothers who had pregnancy-induced hypertension were almost 3 times more likely to face neonatal mortality compared to neonates who were delivered from mothers who had no pregnancy-induced hypertension (AOR = 3.02; 95% CI; 1.47–6.17). Neonates delivered at the public hospital were almost 3 times higher odds of neonatal mortality as compared to neonates who were delivered at private hospitals (AOR = 3.44; 95% CI; 1.84–6.42). Preterm babies were 2 times more prone to neonatal mortality than those term babies (AOR = 2.06; 95% CI; 1.43–2.96). Referred neonates were almost 5 times at higher odds of neonatal mortality as compared to neonates who were not referred (AOR = 4.71; 95% CI; 3.01–7.39). The odds of neonatal mortality among hypothermic newborns were 2 times higher as compared to non-hypothermic newborns (AOR = 2.44; 95% CI; 1.56–3.82) (Table 2).
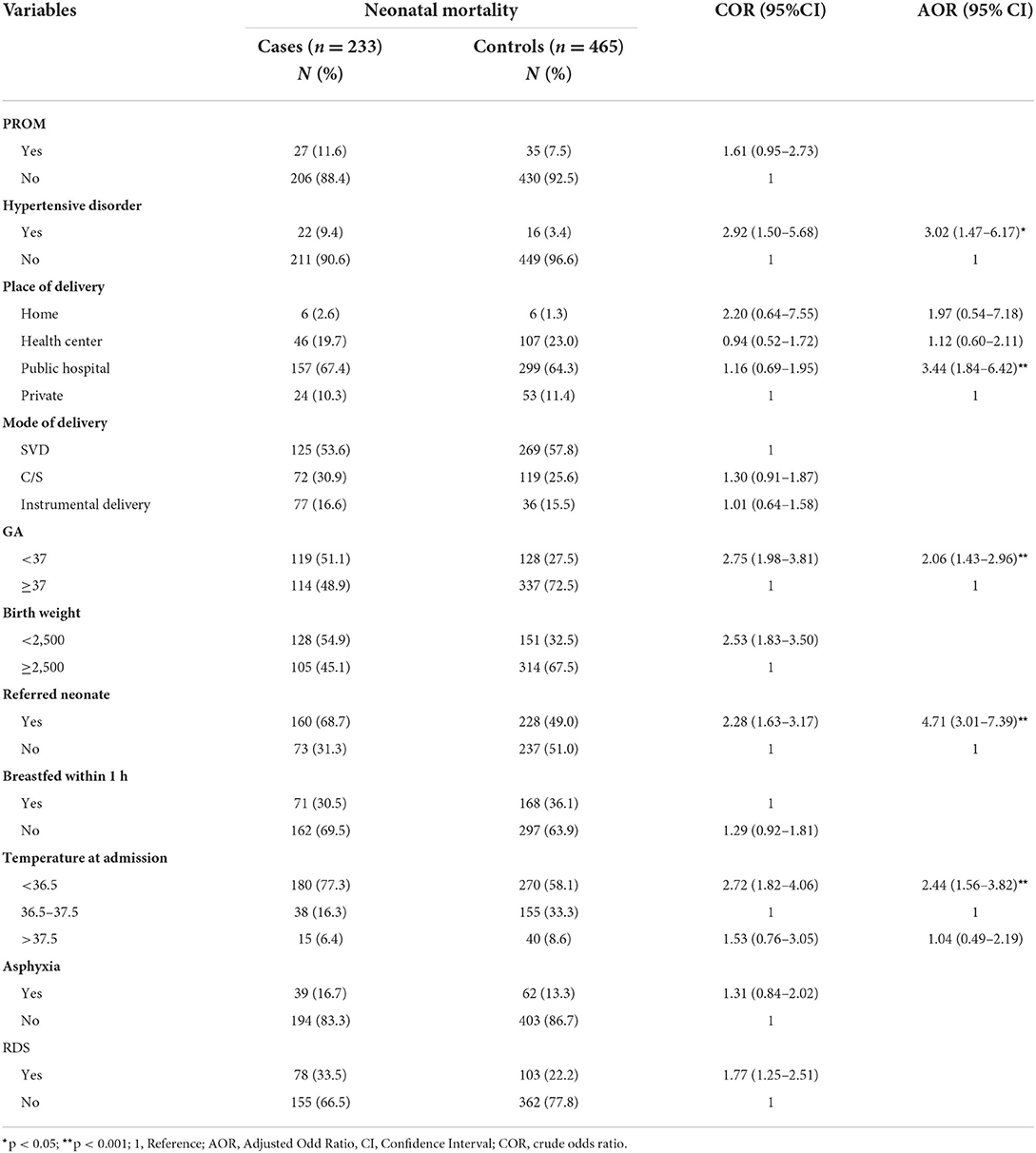
Table 2. Determinants of neonatal mortality among neonates admitted to neonatal intensive care unit of Dessie comprehensive and specialized hospital, northeast Ethiopia, 2020 (n = 698).
Although the reason for neonatal mortality is unknown, it is a multifaceted issue. This study looked at some of the key factors that influence neonatal mortality in neonates admitted to Dessie's comprehensive and specialized hospital's NICU. According to the findings, neonates born to women with pregnancy-induced hypertension, place of delivery, preterm, referral, and hypothermia were all factors that contributed to neonatal mortality. The odds of neonatal death were three times more likely among neonates delivered from mothers who had pregnancy-induced hypertension in comparison to their counterparts. This finding was consistent with the results of a study conducted in the Netherlands and two studies in Ethiopia (33–35). Maternal hypertensive disorders during the pregnancy increase the risk of low birth weight, low 1st minute Apgar score, respiratory distress syndrome, and preterm birth which were the leading cause of neonatal mortality (33). Another piece of evidence indicated that small size neonates were highly susceptible to different infections due to having low immunity defense (33).
Neonates delivered at public health institutions had three times higher odds of neonatal mortality as compared to neonates who were delivered at private health institutions. This result was in line with the results of the study conducted in Australia (36). This might be because of the high coverage of birth in public health institutions as compared to private health institutions. On and another hand delay in the decision to seek care, delay in reaching care, and delay in receiving adequate health care for new babies by the doctor in governmental health institutions since they are engaged with various private institutions for pecuniary benefits and hand over the duty to new untrained doctors and other health care professionals. The odds of neonatal death were two times higher among preterm-delivered neonates as compared to term-delivered neonates. This finding is consistent with a study conducted in Brazil, Kenya, and four studies in Ethiopia (24, 31, 32, 34, 37–39). Prematurity is related to difficulty in extra uterine adaptation due to the immaturity of different organ systems (39). The supply of oxygen through the placenta increases with the course of gestation according to the fetal needs (40, 41). Premature birth interrupts this process, exposing the newborn to oxygen deprivation, which can be harmful to the tissues, especially the nervous system, increasing the risk of cerebral palsy, visual disturbances, and chronic disease in adulthood (42). Another piece of evidence indicated that preterm and low birth weight babies were more likely to be prone to complications such as hypothermia, infections, and birth asphyxia (resulting in tissue hypoxia and multi-organ failure) (31).
The odds of neonatal mortality among referred neonates were almost five times higher compared to neonates who were not referred. This finding was similar to the results of a study done in India, a low resource setting, and Ethiopia (43–45). This might be due to delays in deciding to seek care, delay in reaching a first referral level facility, and delay in actually receiving care after arriving at the facility. Another piece of evidence indicated that lack of well-equipped infrastructure to respond to a crisis, non-availability of obstetric emergency care, and lack of transportation facilities to deal with emergency cases add to the loss of lives (46). The odds of neonatal death among hypothermia neonates were almost five times higher compared to neonates who had normal body temperature. This finding was similar to the results of a study conducted in India, Ethiopia south Nepal (43, 47, 48). This can be justified by neonates who are in a hypothermic state may be more prone to different infections and are more likely to become septic and die when compared to neonates with normal body temperatures (49).
Our study didn't include other maternal socio-demographic characteristics such as the number of prenatal care received, the history of preterm birth before the delivery of the current newborn, and type of birth attendant (Physician, Midwife, and Nurse) and social determinants except for maternal age. Besides, professional-related factors were not incorporated in this study due to the COVID-19 endemic.
Neonates delivered from mothers who had a history of pregnancy-induced hypertension, neonates delivered in Public hospitals, being prematurity, being referred and Hypothermia was found to be the determinant factors of neonatal mortality among NICU admitted neonates. It would be important to give due attention to neonates delivered from mothers with a history of hypertensive disorder. Besides better to give due attention to neonates delivered in public health institutions, prematurely delivered, referred, and hypothermic neonates. Lastly, further research should be conducted to investigate the additional determinants of neonatal mortality.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Helsinki's declaration for medical research involving human subjects was followed. Ethical clearance was obtained from the institutional health research review committee board (Ref. No. IRB-014/02/2020) of the College of Medicine and Health Sciences of Bahir Dar University. Permission was obtained from all responsible bodies at Dessie Comprehensive and Specialized Hospital, NICU, and client registration (card room).
GEW, KC, AA, FY, GW, YM, MA, MS, and GB: conceptualization. GEW, GW, KC, FY, and GB: methodology. GW, AA, FY, YM, and MS: software and supervision. GEW, MA, KC, GW, and GB: formal analysis. GW, MA, AA, YM, MS, and GB: data curation. GEW, GW, FY, and GB: writing—original draft preparation. GEW, GW, KC, and MA: writing—review and editing. GEW, AA, and FY: visualization. GEW, GW, YM, MA, MS, and GB: funding acquisition. All authors have read and approved the final version of the manuscript to be published.
Bahir Dar University had covered the costs for data collection instruments, data collectors, and supervisors, but the funder had no role in the decision to publish.
We would like to thank Bahir Dar University, college of medicine and health science for providing us with ethical clearance. Our special thanks go to all study participants, data collectors, supervisors, and all health workers of Dessie comprehensive and specialized hospital for their cooperation.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ANC, Antenatal Care; AOR, Adjusted odds ratio; CI, Confidence interval; EDHS, Ethiopian Demographic and Health Survey; LBW, Low birth weight; MAS, Meconium aspiration syndrome; NICU, Neonatal intensive care unit; NM, Neonatal mortality; NMR, Neonatal mortality rate; OR, Odds ratio; RDS, Respiratory distress syndrome; SDG, Sustainable development goal; SPSS, Statistical package for social science; WHO, World health organization.
1. World health Organization. Neonatal and Perinatal Mortality,Country, Regional and Global Estimates. (2006). p. 433–43.
2. Barfield WD. Standard terminology for fetal, infant, and perinatal deaths. Pediatrics. (2016) 137:e20160551. doi: 10.1542/peds.2016-0551
3. UNICEF, WHO, WBO. Levels & Trends in Child Mortality Report. (2020). Un Igme. (2020). p. 48. Available online at: https://www.unicef.org/media/79371/file/UN-IGME-child-mortality-report-2020.pdf.pdf
4. World Health Organisation (WHO). Making Every Baby Count: Audit and Review of Stillbirths and Neonatal Deaths. WHO Libr Cat Data (2016). p. 144.
5. UN IGME. Levels & Trends in Child Mortality: Estimates: Report (2018). Who/Unicef/World Bank/Un. (2018). 1–48.
6. World Health Organization. Every newborn: An action plan to end Preventable deaths. Who, Unicef. (2014). 58. Available online at: https://www.who.int/initiatives/every-newborn-action-plan
9. Ethiopian Public Health Institute (EPHI) ICF. Ethiopia Mini Demographic and Health Survey 2019: Final Report. (2019). Available online at: https://dhsprogram.com/pubs/pdf/FR363/FR363. p. 1–207
10. Bora JK, Saikia N. Neonatal and under-five mortality rate in Indian districts with reference to Sustainable Development Goal 3: an analysis of the National Family Health Survey of India (NFHS), 2015–2016. PLoS ONE. (2018) 13:e0201125. doi: 10.1371/journal.pone.0201125
12. WHO UNICEF. Reaching the Every Newborn National. (2020). Milestones Country Progress, Plans and Moving Forward (2017). p. 2015–2018. Available online at: http://apps.who.int/iris/bitstream/10665/255719/1/9789241512619-eng.pdf?ua=1
13. IEG World Bank ICF MIGA. Delivering the Millennium Development Goals to Reduce Maternal and Child Mortality: A Sytematic Review of Impact Evaluation Evidence. (2012). p. 149. Available online at: https://www.oecd.org/derec/norway/WORLDBANKDeliveringtheMDGtoreducematernalandchildmortality.pdf
14. UNICEF, WHO, The World Bank Group UN Population Division. Levels and Trends in Child Mortality: Report. (2017). United Nations Inter-gr Child Mortal Estim (2017). p. 40. Available online at: https://childmortality.org/wp-content/uploads/2018/10/UN-IGME-Child-Mortality-Report-2017.pdf
15. Sava DI. Neonatal intensi (NICU) Training Management Protocolve care unit. OT Pract. (2014) 13:8. Available online at: http://repository.iifphc.org/bitstream/handle/123456789/709/NICU%20Training%20Management%20Protocol_08April%202014%20.pdf?sequence=1&isAllowed=y
16. Ministry of Health Ethiopia, PMNCH, World Health Organization, World Bank AHPSR. Success Factors for Women's and Children's Health Ethiopia. (2015). p. 28.
17. World Health Organization (WHO). World Health Statics. Vol. 3, Khatulistiwa Informatika. (2015). p. 124–133.
19. Jehan I, Harris H, Salat S, Zeb A, Mobeen N, Pasha O, et al. Neonatal mortality, risk factors and causes: a prospective population-based cohort study in urban Pakistan. Bull World Health Organ. (2009) 87:130–8. doi: 10.2471/BLT.08.050963
20. Debelew GT, Afework MF, Yalew AW. Determinants and causes of neonatal mortality in jimma Zone, Southwest Ethiopia: a multilevel analysis of prospective follow up study. PLoS ONE. (2014) 9:e107184. doi: 10.1371/journal.pone.0107184
21. Vogel JP, Souza JP, Mori R, Morisaki N, Lumbiganon P, Laopaiboon M, et al. Maternal complications and perinatal mortality. Obstet Anesth Dig. (2015) 35:73. doi: 10.1097/01.aoa.0000463817.02019.7d
22. Abdallah Y, Namiiro F, Mugalu J, Nankunda J, Vaucher Y, McMillan D. Is facility based neonatal care in low resource setting keeping pace? A glance at Uganda's National Referral Hospital. Afr Health Sci. (2016) 16:347–55. doi: 10.4314/ahs.v16i2.2
23. Reyesa JCL, Ramírez ROP, Ramosa LL, Ruiz LMG, Vázquez EAB, Patinõ VR. Neonatal mortality and associated factors in newborn infants admitted to a Neonatal Care Unit. Arch Argent Pediatr. (2018) 116:42–8. doi: 10.5546/aap.2018.eng.42
24. Yego F, D'Este C, Byles J, Nyongesa P, Williams JS. A case-control study of risk factors for fetal and early neonatal deaths in a tertiary hospital in Kenya. BMC Pregnancy Childbirth. (2014) 14:389. doi: 10.1186/s12884-014-0389-8
25. Abdullah A, Hort K, Butu Y, Simpson L. Risk factors associated with neonatal deaths: a matched case-control study in Indonesia. Glob Health Action. (2016) 9:30445. doi: 10.3402/gha.v9.30445
26. Demisse AG, Alemu F, Gizaw MA, Tigabu Z. Patterns of admission and factors associated with neonatal mortality among neonates admitted to the neonatal intensive care unit of University of Gondar Hospital, Northwest Ethiopia. Pediatr Health Med Ther. (2017) 8:57–64. doi: 10.2147/PHMT.S130309
27. Mehretie K. Institution Based Prospective Cross-Sectional Study on Patterns of Neonatal Morbidity at Gondar University Hospital Neonatal Unit. (2011). p. 73–9.
28. Mengesha HG, Sahle BW. Cause of neonatal deaths in Northern Ethiopia: a prospective cohort study. BMC Public Health. (2017) 17:1–8. doi: 10.1186/s12889-016-3979-8
29. Kolobo H, Chaka T, Kassa R. Determinants of neonatal mortality among newborns admitted to neonatal intensive care unit Adama, Ethiopia: A case–control study. J Clin Neonatol. (2019) 8:232. doi: 10.4103/jcn.JCN_23_19
30. Alebel A, Wagnew F, Petrucka P, Tesema C, Moges NA, Ketema DB, et al. Neonatal mortality in the neonatal intensive care unit of Debre Markos referral hospital, Northwest Ethiopia: A prospective cohort study. BMC Pediatr. (2020) 20:1–11. doi: 10.1186/s12887-020-1963-z
31. Desalew A, Sintayehu Y, Teferi N, Amare F, Geda B, Worku T, et al. Cause and predictors of neonatal mortality among neonates admitted to neonatal intensive care units of public hospitals in eastern Ethiopia: a facility-based prospective follow-up study. BMC Pediatr. (2020) 20:1–11. doi: 10.1186/s12887-020-02051-7
32. Seid SS, Ibro SA, Ahmed AA, Olani Akuma A, Reta EY, Haso TK, et al. Causes and factors associated with neonatal mortality in Neonatal Intensive Care Unit (NICU) of Jimma University Medical Center, Jimma, South West Ethiopia. Pediatr Heal Med Ther. (2019) 10:39–48. doi: 10.2147/PHMT.S197280
33. van Esch JJA, van Heijst AF, de Haan AFJ, van der Heijden OWH. Early-onset preeclampsia is associated with perinatal mortality and severe neonatal morbidity. J Matern Neonatal Med. (2017) 30:2789–94. Available from: doi: 10.1080/14767058.2016.1263295
34. Kidus F, Woldemichael K, Hiko D. Predictors of neonatal mortality in Assosa zone, Western Ethiopia. BMC Pregnancy Childbirth. (2019) 19:1–13. doi: 10.1186/s12884-019-2243-5
35. Berhan Y, Endeshaw G. Maternal mortality predictors in women with hypertensive disorders of pregnancy: a retrospective cohort study. Ethiop J Health Sci. (2015) 25:89–98. doi: 10.4314/ejhs.v25i1.12
36. Jang W, Flatley C, Greer RM, Kumar S. Comparison between public and private sectors of care and disparities in adverse neonatal outcomes following emergency intrapartum cesarean at term – a retrospective cohort study. PLoS ONE. (2017) 12:187040. doi: 10.1371/journal.pone.0187040
37. De Souza S, Duim E, Nampo FK. Determinants of neonatal mortality in the largest international border of Brazil: a case-control study. BMC Public Health. (2019) 19:1–9. doi: 10.1186/s12889-019-7638-8
38. Roro EM, Sisay MM, Sibley LM. Determinants of perinatal mortality among cohorts of pregnant women in three districts of North Showa zone, Oromia Region, Ethiopia: Community based nested case control study. BMC Public Health. (2018) 18:1–11. doi: 10.1186/s12889-018-5757-2
40. de Oliveira TG, Freire PV, Moreira FT, de Moraes J da SB, Arrelaro RC, Ricardi SRVA, et al. Apgar score and neonatal mortality in a hospital located in the southern area of São Paulo City, Brazil. Einstein. (2012) 10:22–8. doi: 10.1590/S1679-45082012000100006
41. Iliodromiti S, MacKay DF, Smith GCS, Pell JP, Nelson SM. Apgar score and the risk of cause-specific infant mortality: a population-based cohort study. Lancet. (2014) 384:1749–55. doi: 10.1016/S0140-6736(14)61135-1
42. Mwaniki MK, Atieno M, Lawn JE, Newton CRJC. Long-term neurodevelopmental outcomes after intrauterine and neonatal insults: a systematic review. Lancet. (2012) 379:445–52. doi: 10.1016/S0140-6736(11)61577-8
43. Aggarwal K, Gupta R, Sharma S, Sehgal R, Roy M. Mortality in newborns referred to tertiary hospital: an introspection. J Fam Med Prim Care. (2015) 4:435. doi: 10.4103/2249-4863.161348
44. Cavallin F, Bonasia T, Yimer DA, Manenti F, Putoto G, Trevisanuto D. Risk factors for mortality among neonates admitted to a special care unit in a low-resource setting. BMC Pregnancy Childbirth. (2020) 20:1–8. doi: 10.1186/s12884-020-03429-2
45. Mihiretu A, Negash T, Elazar T. Perinatal death and associated factors in wolaita sodo referral hospital, Southern Ethiopia: a Facility based cross-sectional study. Prim Heal Care Open Access. (2017) 7, 1–5. doi: 10.4172/2167-1079.1000269
46. Arokiasamy P, Gautam A. Neonatal mortality in the empowered action group states of India: trends and determinants. J Biosoc Sci. (2008) 40:183–201. doi: 10.1017/S0021932007002623
47. Orsido TT, Asseffa NA, Berheto TM. Predictors of Neonatal mortality in Neonatal intensive care unit at referral Hospital in Southern Ethiopia: A retrospective cohort study. BMC Pregnancy Childbirth. (2019) 19:1–9. doi: 10.1186/s12884-019-2227-5
48. Mullany LC, Katz J, Khatry SK, LeClerq SC, Darmstadt GL, Tielsch JM. Neonatal hypothermia and associated risk factors among newborns of southern Nepal. BMC Med. (2010) 8:43. doi: 10.1186/1741-7015-8-43
Keywords: neonatal mortality, determinants, unmatched case-control, Dessie, Ethiopia
Citation: Wake GE, Chernet K, Aklilu A, Yenealem F, Wogie Fitie G, Amera Tizazu M, Mittiku YM, Sisay Chekole M and Behulu GK (2022) Determinants of neonatal mortality among neonates admitted to neonatal intensive care unit of Dessie comprehensive and specialized hospital, Northeast Ethiopia; An unmatched case-control study. Front. Public Health 10:979402. doi: 10.3389/fpubh.2022.979402
Received: 27 June 2022; Accepted: 26 August 2022;
Published: 27 September 2022.
Edited by:
Anand Krishnan, All India Institute of Medical Sciences, IndiaReviewed by:
Anthony Pascual Calibo, St. Luke's Medical Center, PhilippinesCopyright © 2022 Wake, Chernet, Aklilu, Yenealem, Wogie Fitie, Amera Tizazu, Mittiku, Sisay Chekole and Behulu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Getu Engida Wake, Z2V0dWVuZ2lkYTMwMzBAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.