
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 21 December 2022
Sec. Public Health Policy
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.979063
 Wenfeng Cai1†
Wenfeng Cai1† Zifeng Yang2,3,4,5†
Zifeng Yang2,3,4,5† Jingyi Liang2,3,6†
Jingyi Liang2,3,6† Zhengshi Lin7†
Zhengshi Lin7† Yu Ma1†
Yu Ma1† Chun Chen1†
Chun Chen1† Yan Li6†
Yan Li6† Yongming Li2,3†
Yongming Li2,3† Zhitong Mai2,3,4
Zhitong Mai2,3,4 Kailin Mai2,3
Kailin Mai2,3 Xuetao Kong2
Xuetao Kong2 Xingyi Liang8
Xingyi Liang8 Qianying Li2
Qianying Li2 Chuanmeizi Tu2,3
Chuanmeizi Tu2,3 Canxiong Chen2
Canxiong Chen2 Chitin Hon6
Chitin Hon6 Pengzhe Qin1
Pengzhe Qin1 Ke Li1
Ke Li1 Xiaoning Li1
Xiaoning Li1 Yutian Miao1
Yutian Miao1 Xuexing Liu1
Xuexing Liu1 Wenda Guan2,3
Wenda Guan2,3 Zhiqi Zeng2,3
Zhiqi Zeng2,3 Wanli Qiu1
Wanli Qiu1 Wei He6
Wei He6 Lin Zhang7*
Lin Zhang7* Zhicong Yang1*
Zhicong Yang1* Nanshan Zhong2,3*
Nanshan Zhong2,3*Introduction: SARS-CoV-2 has ravaged the world and undergone multiple mutations during the course of the COVID-19 pandemic. On 7 April 2022, an epidemic caused by SARS-CoV-2 Omicron (BA.2) variant broke out in Guangzhou, China, one of the largest transportation and logistical hubs of the country.
Methods: To fast curtained the Omicron epidemic, based on the routine surveillance on the risk population of SARS-CoV-2 infection, we identify key places of the epidemic and implement enhanced control measures against Omicron.
Results: Transmission characteristics of the Omicron variant were analyzed for 273 confirmed cases, and key places involved in this epidemic were fully presented. The median incubation time and the generation time were 3 days, and the reproduction number Rt was sharply increased with a peak of 4.20 within 2 days. We tried an all-out effort to tackle the epidemic in key places, and the proportion of confirmed cases increased from 61.17% at Stage 2 to 88.89% at Stage 4. Through delimited risk area management, 99 cases were found, and the cases were isolated in advance for 2.61 ± 2.76 days in a lockdown zone, 0.44 ± 1.08 days in a controlled zone, and 0.27 ± 0.62 days in a precautionary zone. People assigned with yellow code accounted for 30.32% (84/277) of confirmed COVID-19 cases, and 83.33% of them were detected positive over 3 days since code assignment. For the districts outside the epicenter, the implementation duration of NPIs was much shorter compared with the Delta epidemic last year.
Conclusion: By blocking out transmission risks and adjusting measures to local epidemic conditions through the all-out effort to tackle the epidemic in key places, by delimiting risk area management, and by conducting health code management of the at-risk population, the Omicron epidemic could be contained quickly.
SARS-CoV-2 has ravaged the world and undergone multiple mutations during the course of the COVID-19 pandemic (1). The latest Omicron variant B.1.1.529.1, a variant of concern (VOC), was first identified in South Africa in November 2021; it rapidly replaced the Delta variant and predominantly circulates worldwide at present with an R0 of >7.0 (2, 3). The World Health Organization's (WHO) COVID-19 Weekly Epidemiological Update on 5 April 2022 (4) reports over 9 million new cases and over 26,000 new deaths during the week of 28 March to 3 April 2022 across the six WHO regions. Among the 417,147 sequences uploaded to GISAID with specimens collected in March 2022, 416,175 (99.8%) were Omicron, the relative proportion of Omicron lineage BA.2 has increased from 85.38% at Week 11 to 93.6% at Week 13 in 2022.
Compared to other VOCs (especially the Delta variant), a marked degree of mutations, enhanced transmissibility, and immune evasion have been apparently observed (5). It can cause reinfection in a person who has recovered from a previous infection, as well as breakthrough infections in vaccinated populations. In fact, the highly transmissible Omicron has caused widespread infections within a short period of time somewhere in the world, resulting in a sudden increase in large numbers of cases and case fatalities (6). These characteristics bring new difficulties and challenges to the prevention and control of the outbreak. It is evident that if the epidemic was not contained at the initial stage, it is likely to cause the extension of the epidemic, ultimately paying a much higher price to control, such as requiring excessive manpower and material resources, overwhelming medical and health systems, and even losing more lives tragically.
On the other hand, the COVID-19 pandemic has been lingering for more than 2 years, and a return to normal life has become a strong desire. Thus, implementation of epidemic prevention and control measures must be scientifically and timely adjusted according to current epidemiology and specific conditions of different countries, as such, managing to strike a balance between strict prevention and control measures and minimizing the impact on people's normal life is an important issue of the moment (7, 8). Since the clinical symptoms of Omicron are milder than those of Delta (predominantly with upper respiratory tract infection symptoms) (9, 10), some countries/areas have loosened their control measures based on the high infection rate and vaccination rate (11). China is the world's second most populous developing country; up to 19 April 2022, the nationwide vaccination rate (three doses) is approximately 51% (12), therefore, precise and strict preventive and control measures are necessary to buy more time for people at high risk to be vaccinated.
An epidemic caused by the Omicron variant broke out on 8 April 2022 in Guangzhou, China. Guangzhou has a resident population of over 18 million; it is the transportation hub of southern China and is one of the largest logistical hubs in the country. Based on our experience in controlling Delta's outbreak in the midyear of 2021 (13) and the epidemiological characteristics of Omicron, we quickly adopted precise control measures to contain the outbreak within 18 days and minimized the impact on society. Here, we present the Omicron epidemiological characteristics and share our experience in implementing control measures to contain the epidemic.
Data of demographics and epidemiological investigation of confirmed cases from 8–26 April 2022 were extracted from the collection of the Guangzhou Center for Disease Control and Prevention on 1 May, including patients' age, sex, vaccination status, residential district, history of close contact with confirmed cases, the number of risk population being tested, total infected cases diagnosed by real-time reverse transcriptase-polymerase chain reaction (RT-PCR) assay, health code assignment, confirmed cases in isolation, and the laboratory confirmation date.
Since the outbreak of the Delta variant, we set up the routine surveillance on the risk population for nucleic acid testing, which was divided into three groups: (A) compulsive nucleic acid testing group; (B) high-risk industries and population group; and (C) potential risk groups and risk areas. The definitions and detailed nucleic acid testing requirements of these groups are described in Supplementary Table S1. Taking potential risk groups and risk areas as an example, a screening nucleic acid test (NAT) was taken once a week on 25% of the population in the group, and the entire population was tested once a month.
With the joint effort of Guangzhou government departments, a “24-h” epidemiological survey protocol (Figure 1) was compiled to identify the risk populations and key places rapidly. According to this protocol, key places were defined based on where the confirmed cases stayed 2 days prior to the onset of illness. Subsequently, based on the information on the length of stay and frequency of confirmed cases visited, the completeness of close contact personal information, and the environmental ventilation of the premises, we further divided certain areas into high-, middle- and low-risk key places (Supplementary Table S2). Management of high-risk key places was one of the critical tactics in the overall anti-epidemic work, which included risk assessment, temporary closure, nucleic acid testing and registration information of stranded persons, risk assessment of personnel exposure, and environmental sampling and disinfection (Figure 2).
According to the judgment on the epidemic trend, we literally divided the whole epidemic into four stages (8–9 April, 10–12 April, 13–15 April, and 16–18 April 2022). Due to the higher transmissibility of Omicron, we thus modified and improved our previous prevention and control measures for the Delta variant (Table 1). The following three points were made:
1) In terms of the management of regional control, we divided Baiyun District (the epicenter of the outbreak) into the following three areas: lockdown zone, controlled zone, and precautionary zone. In the lockdown zone, people were quarantined at home and living with the help of volunteers; in the controlled zone, a number of grids had been set up, with no movement between grids permitted; and in the precautionary zone, people who entered and left the area must have the certificate of negative nucleic acid testing within 48 h. Classification of the three areas was based on the confirmed cases' trajectory and is summarized in Table 1.
2) People with yellow health code were required to have three NATs taken within 7 days (each test taken at least 24 h apart). When a negative result is obtained, the person's health code would turn green, but if the test was not taken as required, the yellow code would be assigned again. To avoid cross-infection, people with green and yellow codes had to be tested separately.
3) In addition to the regular NATs, we also introduced antigen testing in the precautionary zone.
Normal distribution data, such as the interval between control and testing positive in the delimited risk area, were presented as mean (±standard deviation). Qualitative information, such as the source of case findings, was presented as percentage or frequency. The Spearman rank test was performed in the comparison of interval calculation between two epidemics. All of the tests were two-tailed, and a value of P < 0.05 represented statistical significance. The statistical analysis was conducted using statistical R version 4.0.2. We applied a Bayesian framework to estimate the Rt value of the Omicron strain, which used a Gamma distributed prior, conjugated to the Poisson likelihood, and obtained an analytical formulation of the posterior distribution of Rt. To maintain the accuracy of the prediction and without hiding the underlying time trend, Rt values were estimated over a 7-day moving window.
A total of 277 cases were diagnosed in this epidemic. Among the mentioned cases, 251 (90.6%) were identified as confirmed cases, whereas 26 (9.39%) were as asymptomatic cases. Demographic characteristics of the confirmed cases are summarized in Table 2. The median incubation time and generation time were also 3 days, which means that the transmission is quick and insidious. The median age was 33 years (IQR:23.5, 43), and the male patients accounted for 45.78%. Infectious cases aged 15–44 years accounted for the majority of (69.96%) of the total cases. A total of 239 (87.55%) cases had received 2 or 3 doses of inactivated vaccine, and a total of 25 cases (9.15%) had not been vaccinated. Compared to the cases discovered from mass testing (1.10%), risk population (3.66%), and fever clinic (1.83%), most infectious cases were found among close contacts (56.41%) and in the delimited risk areas (36.26%) (Table 2).
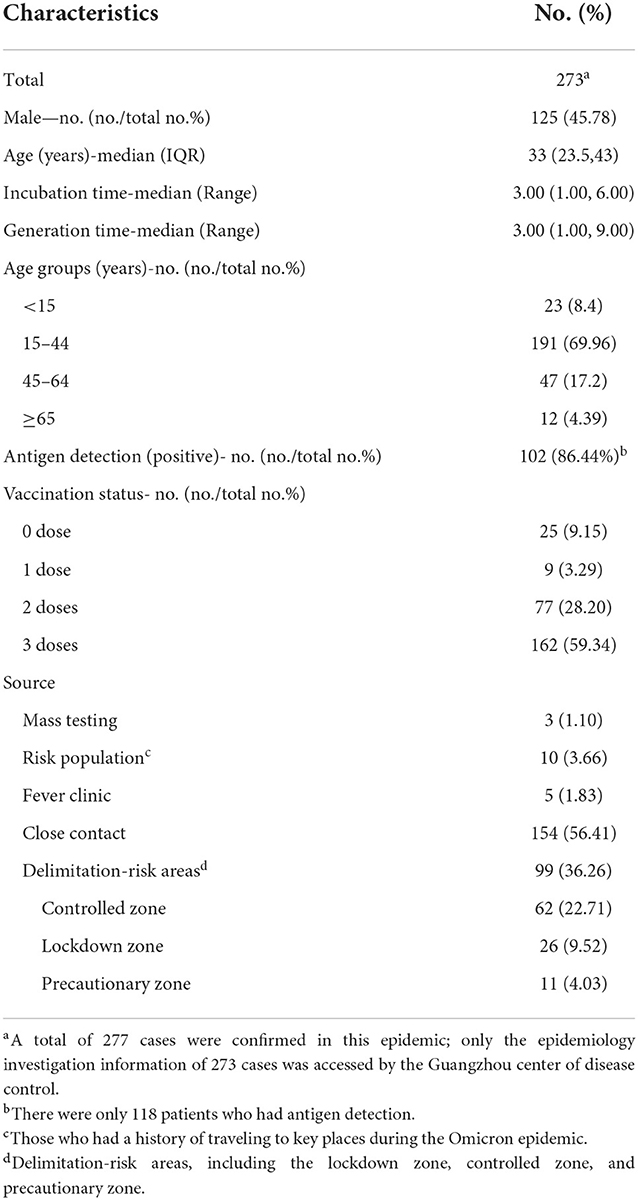
Table 2. Demographic characteristics of the subjects infected with the SARS-CoV-2 Omicron variant in Guangzhou, 2022.
The first case was a 7-year-old student who was identified during a routine back-to-school screening. Subsequently, the government rapidly launched mass testing in each district of Guangzhou, followed by epidemic investigations in key places, dynamic delimitation, and management of at-risk areas. According to the results of the epidemiological survey, this epidemic originated in the YY garment factory and spread to several social entertainment places and subsequently to family members (Figure 3).
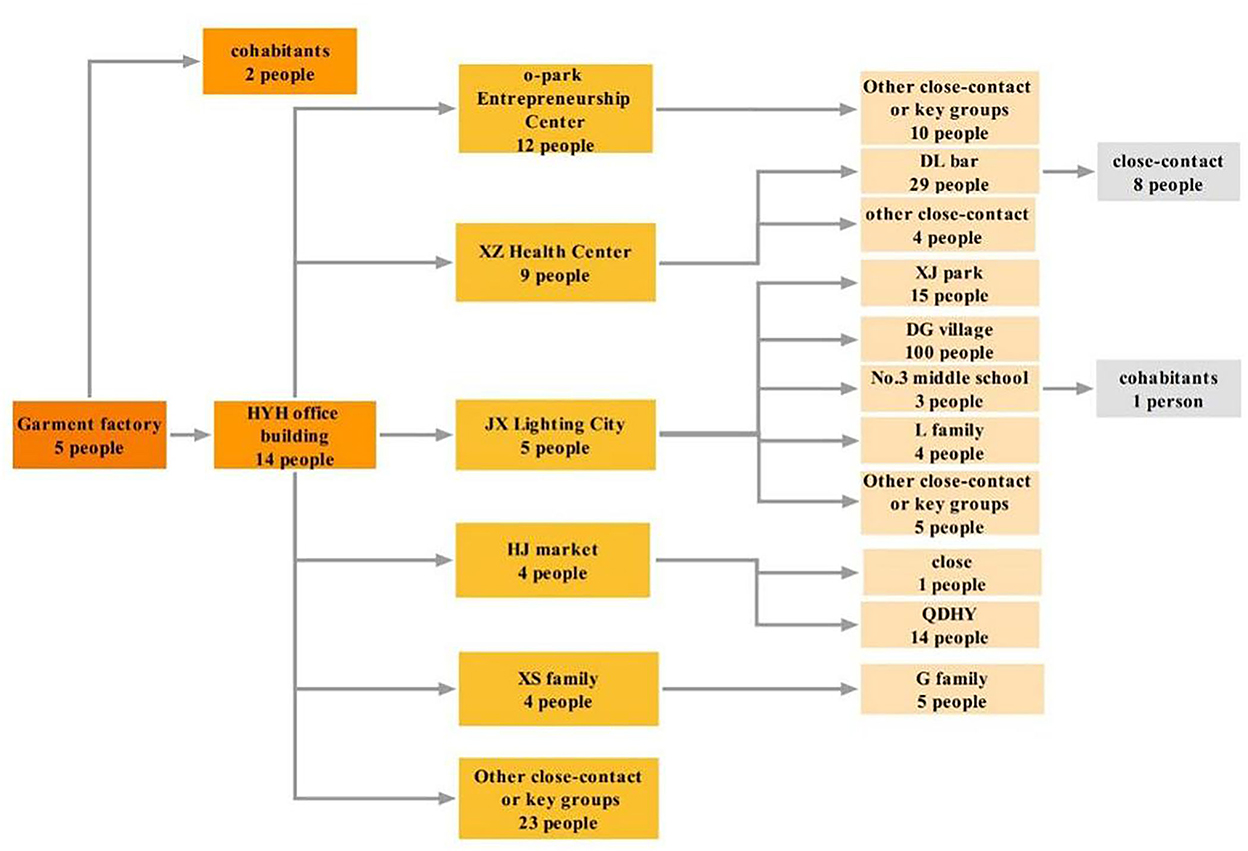
Figure 3. Transmission profile of Omicron epidemic in Guangzhou. Numbers in the figure are based on the results of epidemiology investigation and gene sequencing; the transmission chain was identified with each key place as a single unit, and the different colors represented different generations.
On the basis of a rapid 24-h epidemic investigation protocol, we had initially designated more than 1,000 key places. Having considered the duration of stay, frequency of activity, information completeness of contacts, and venue ventilation conditions, 15 high-risk key places were identified at last. With the effective management of the key places, the proportion of cases detected increased from 61.17% at Stage 2 to 88.89% at Stage 4 (Figure 4). In addition, parts of key places were located in urban villages (such as the Dagang area), and we adopted the double-cross search pattern (shape of the Union Jack) to screen the neighboring buildings. A total of 26 cases were found in Stage 4, 81% of them in the Dagang area.
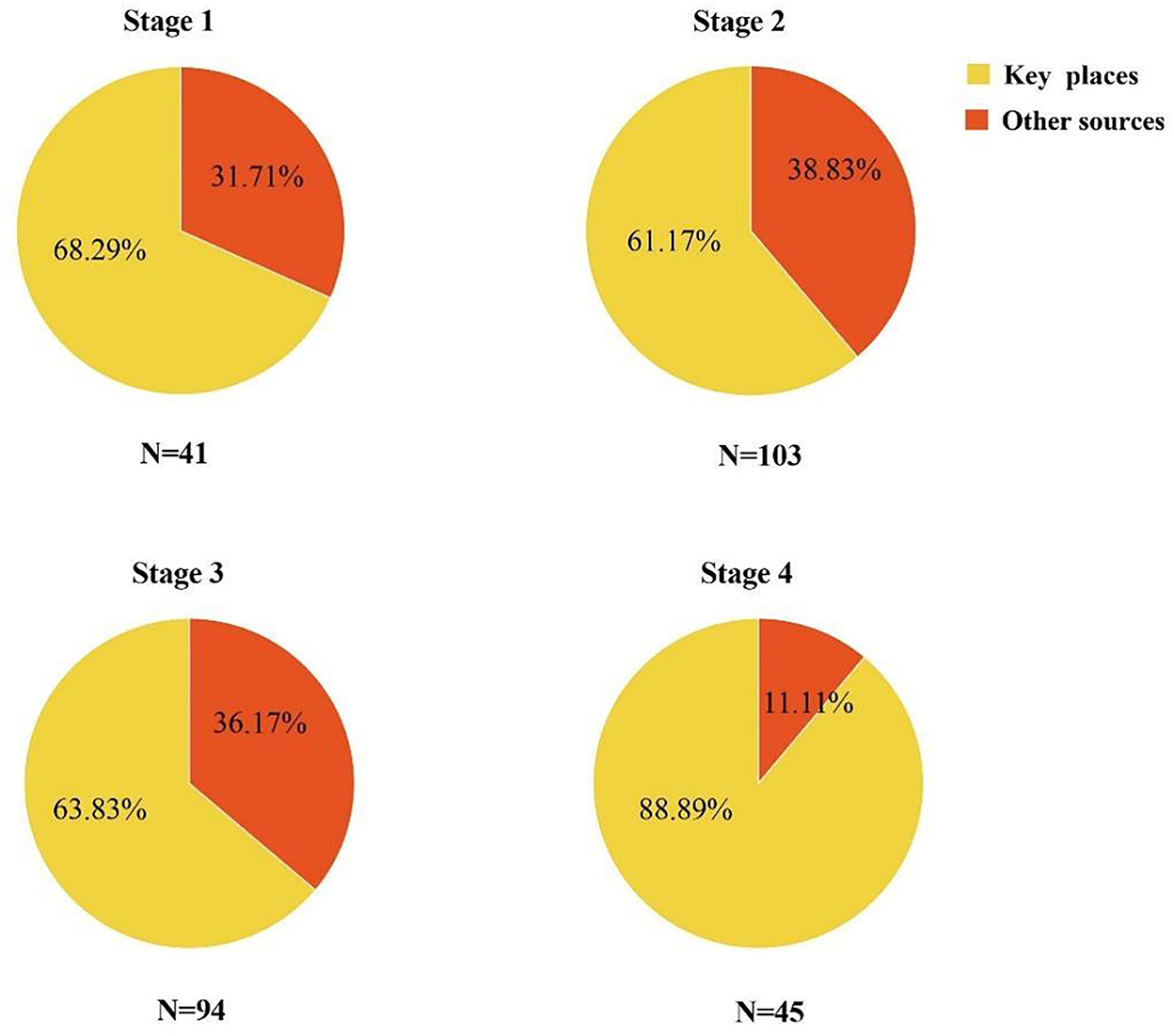
Figure 4. The case-finding source at each stage. Other case-finding sources include mass testing, fever clinic, and close contact.
To block out the transmission chain in a timely manner, we partitioned the at-risk areas from others in the city. Take Baiyun district, for instance, 155 lockdown zones, 71 control zones, and six precautionary zones were delimited throughout the four stages of the epidemic. With the implementation of delimited risk area management (Figure 5), 99 cases were found, and the average interval between a case testing positive and isolation was −2.61 ± 2.76 days in the lockdown zone, −0.44 ± 1.08 days in the controlled zone, and−0.27 ± 0.62 days in the precautionary zone, indicating the transmission risk had been under control in advance since the delimitation of at-risk areas. Also, as illustrated in Figure 5, the range of the lockdown zone and the control zone was dynamically adjusted immediately following the changes in the epidemic situation.
In order to screen for transmission chains that might have been overlooked, people having spatial–temporal intersections with the cases or absent from nucleic acid screening were assigned yellow health code (Table 1, Figure 6). To eliminate potential risks as quickly as possible, people with yellow code were required to complete the NAT within 24 h after receiving the notification; the staff of community service centers would help to supervise the process. Considering the increased transmissibility of the Omicron variant, the length of NAT monitoring for yellow-coded individuals in this outbreak was extended from 3 to 7 days. People with yellow code were requested to take the NAT on the first, third, and 7th days after receiving the notification. After taking the first NAT, the yellow health code was changed to a green one with a negative result or changed to a red one if a positive result was obtained. However, if people, for some reason, did not take the next detection as requested, the health code would automatically turn back to yellow, urging them to conduct self-health management and take the NAT.
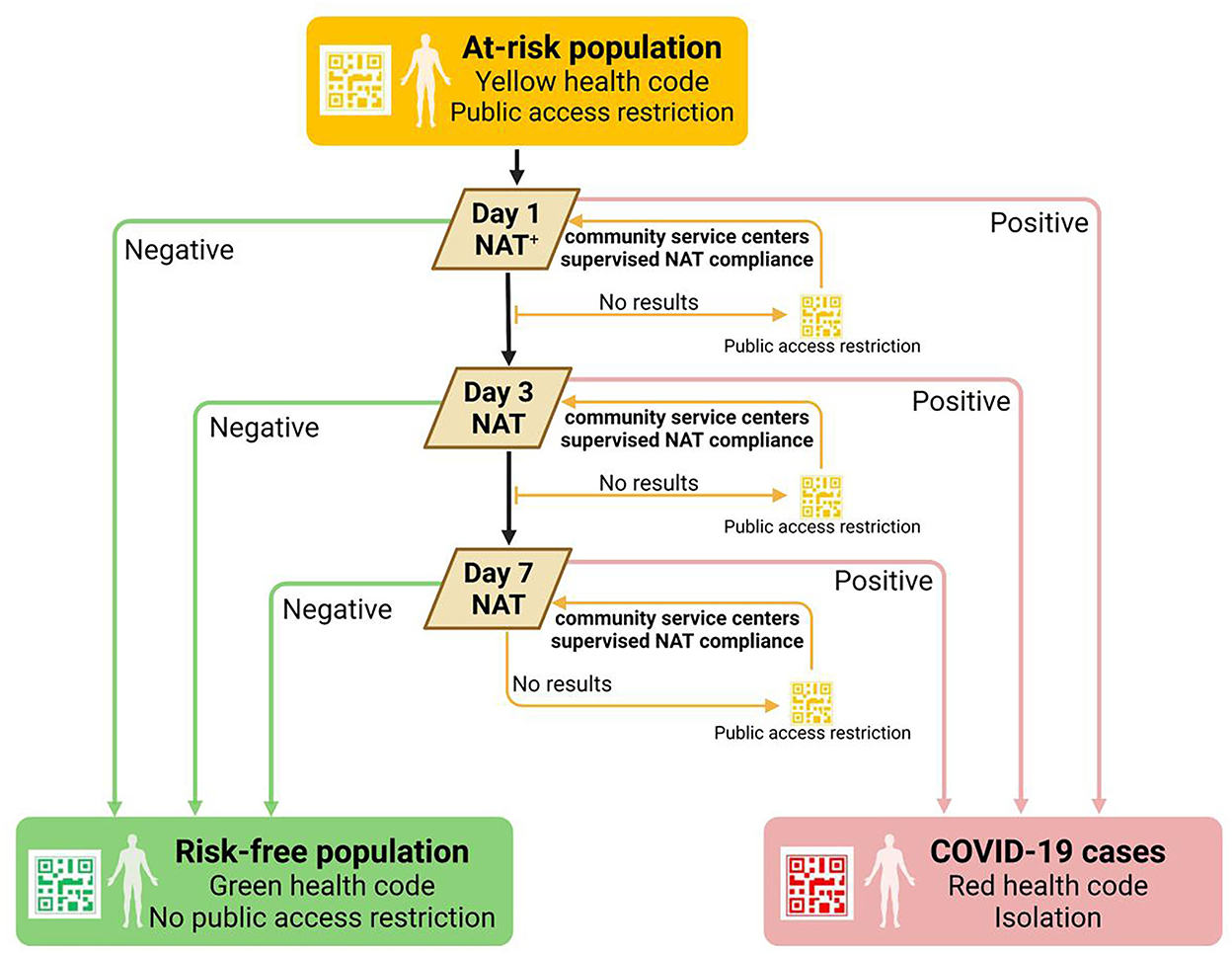
Figure 6. Health code management of the at-risk population. +Public access included public transportation usage and public places entrance. NAT, nucleic acid test.
A total of 2,944,484 yellow codes were assigned, of which 84 were eventually confirmed as COVID-19 cases, accounting for 30.32% (84/277). The longest interval between the yellow-code assignment and the date for NAT positive was 9 days; 16.67% (14/84) cases only took 3 days since the yellow code was assigned.
The effective reproduction number (Rt) rose rapidly at the beginning of this Omicron epidemic, and it reached the peak value (4.20) on the third day since the epidemic began and fell below 1 on the 9th day (6 days later). All COVID-19 transmission chains in communities outside the quarantined areas were cut off after 9 days (Figure 7A).
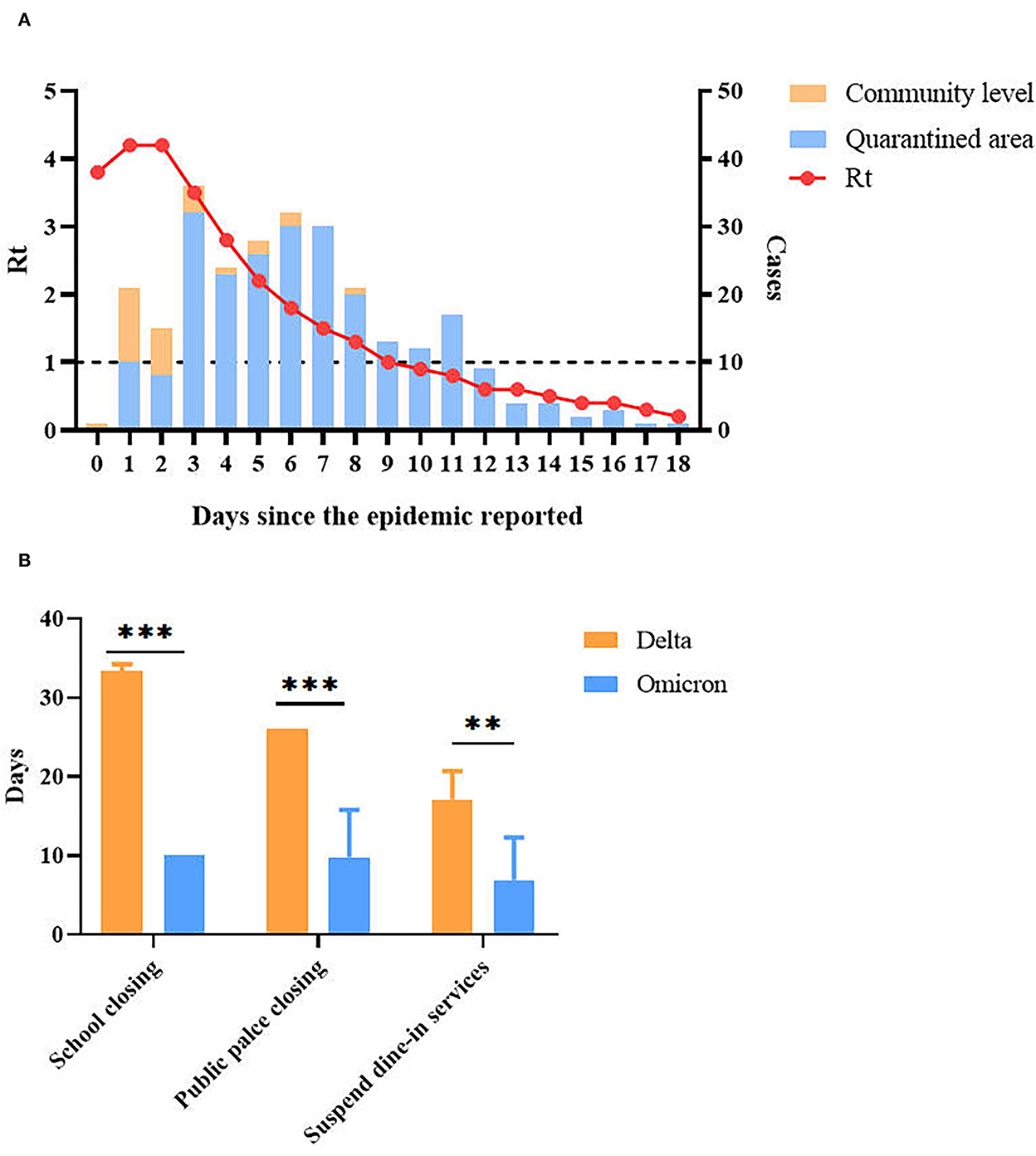
Figure 7. Effectiveness of epidemic control (Omicron vs. Delta). (A) Rt throughout the epidemic. The epidemic started date is 8 April 2022. (B) The duration of non-pharmaceutical interventions (NPIs) implemented by the government. The ** and *** symbols indicate the P values < 0.01 and < 0.001 with the difference between groups are significant respectively.
In addition to evaluating the effectiveness of intervention measures through calculation of Rt, we also compared the duration of non-pharmaceutical intervention policies (NPIs) implemented by the government between the Omicron epidemic and the last year's Delta epidemic, which included school closing, public place closing, and suspended dine-in service, to evaluate the impact on life. As shown in Figure 7B, for the districts outside the epicenter of Guangzhou, the implementation duration of NPIs was much shorter compared with the Delta epidemic last year.
The SARS-CoV-2 Omicron variant has rapidly spread worldwide since November 2021 and become the dominant epidemic strain at present. It is characterized by more mutations, quicker transmissibility, and enhanced immune evasion. Although weakened virulence can be observed in Omicron, the fatalities remained high, especially for the elderly (14, 15). Besides, for older persons, the protective efficacy of two doses of inactivated vaccine immunization is not ideal. It is reported that the effectiveness of the inactivated vaccine (two doses) in preventing serious illness is only 60.7% in those older than 80 years, while an additional booster shot could get a 98% improvement (16). Currently, the percentage of older adults in Guangzhou who have received two doses of the SARS-CoV-2 vaccine is 92.2%, but the percentage of those who received booster shots is only 60.7% (17). Therefore, if the local outbreak of Omicron had not been contained at the beginning, an unpredictable epidemic size would have overwhelmed our medical capacity and disrupted social stability.
In response to this Omicron epidemic in Guangzhou, fast, strict and precise control strategies were implemented. With an all-out effort to tackle the epidemic in key places, dynamic delimitation and management of at-risk areas, and health code management of at-risk populations, the effective reproduction number (Rt) sharply declined, and the implementation of NPIs in non-epicenter was minimized. Remarkably, the Omicron epidemic was contained within 18 days.
In terms of epidemiological characteristics, we observed that the Guangzhou epidemic has the characteristics of rapid spread, strong concealment, and a large number of places involved. First, the median incubation time and generation time were 3 days, which means that the community transmission is quick; second, the first case we found was confirmed to be the third generation or above after tracing the source; and third, the positive cases had obviously clustered in places such as working places, daily living places, and so on. The epidemic mainly originated in the YY garment factory, spread to several social entertainment places, and then spread to homes. More than 87% of the cases had completed two or more doses of inactivated vaccine, which confirmed that Omicron did have the ability to escape immunity to the virus (18, 19).
After the first case was found, we carried out a rapid epidemiological investigation, so as to determine the trajectory of the case in a timely manner, and to delineate key places with a higher risk of the epidemic. Some key places would later be released from control and isolation in time if it was proved that a positive case had not been there within the latent infection period. In order to quickly extinguish the epidemic in key places, we established a work arrangement of “one place, one special group,” which means that police officers, professionals from disease control departments, and staff of community service centers worked on-site together for 24 h a day. Such workflow arrangement guaranteed all the tasks, such as epidemiology investigation, case management and control, transshipment, and isolation in key places run smoothly, thus reducing communication costs, increasing work efficiency, and eventually outpacing the virus transmission.
We defined and divided certain areas with different epidemic risks into three levels (lockdown, control, and precautionary), and each partition had corresponding prevention and control policies with respect to the frequency of NAT and personnel mobility, thus enabling us to better concentrate our efforts and resources on outbreak control. In addition, we subdivided the control zone into 14 control grids according to the specific geographical features (demarcated by adjacent rivers, highways, large buildings, etc.), which was beneficial for the management and delivery of living materials. What is worth mentioning is that the government dispatched staff through the “1 + 5 + 3 + 9 + N” working mechanism to ensure manpower supplement and the normal life of residents in the grids.
Implementation of the yellow health code policy in this Omicron epidemic showed its advantage; it facilitated the identification of at-risk individuals faster and more accurately than that in the Delta outbreak, with approximately 30.32% of COVID-19 cases found among people with yellow health code. The yellow health code daily clearance policy stressed the timely management of the at-risk population. By clearing people holding yellow health code every 24 h, they were urged to complete NAT as soon as possible, thus having CDC professionals work on screening cases in high-risk places. On the other hand, the negative NAT results can be used to redefine a risk-free population and reduce the impact on people's normal life and work. However, in the initial stage of the epidemic, the yellow health code assignment relies heavily on the epidemiological investigation result, which needs several hours to complete. To control the spread as soon as possible, yellow health code management could not take the place of community screening to find out the underlying transmission chain. We suggest NAT screening can be gradually narrowed down to the key population marked with yellow health codes after the community transmission risk is eliminated, reducing its impact brought social and economic development (20).
In total, we summarize the experience in controlling this Omicron epidemic. First, to avoid large-scale outbreaks in the community, routine surveillance of high-risk populations is an indispensable measure for the early discovery of infectious cases; only early initiation of the epidemiological investigation, soon after positive cases are found, can put transmission under control in time. Therefore, it is recommended to establish a routine surveillance workflow on people with high exposure risk. It is evident that fast and accurate epidemiological investigation necessitates key place and population identification, so digital and artificial intelligence tools can be applied to speed up the investigation (21). Moreover, it is extremely important for municipal authorities and professionals from public health institutions to work together to establish and unify all epidemic control measures to conquer the disaster.
What we know about SARS-CoV-2 is only the tip of the iceberg, and its mutation is still ongoing and unpredictable (22). Before the development of more effective drugs and vaccines, in the face of local outbreaks, fast and accurate epidemic prevention and control measures are necessary; the main goal is to reduce the number of infected people for early diagnosis and adequate treatment of confirmed cases, so as to reduce the fatality rate maximally and to guarantee more time for full vaccination of the entire population. However, the way to achieve a balance between epidemic prevention and people living a normal life is an issue that we need to constantly explore.
In the face of the highly infectious Omicron strain, rapid and comprehensive epidemiological investigation provides assurance of early control of the transmission. Reasonable delimitation of at-risk areas and dynamic refinement of control areas can reduce the impact of epidemic prevention measures on people's lives.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements.
ZiY, LZ, NZ conceived the idea of the study. ZM, KM, XK, XL, YaL, QL, CT, CC, CH, PQ, KL, XLi, YM, XLiu, WG, ZZ, WQ, WH contributed to the design of the study and contributing the design of study and data collection. ZiY, NZ, ZhY interpreted the data. WC, ZiY, JL, ZL, YM, CC, YoL contributed to the preparation of the manuscript. All authors contributed to the article and approved the submitted version.
This work was funded by National Key Research and Development Program of China (Grant Nos. 2022YFC2600705 and 2021YFF0306006), Science and Technology Development Fund of Macau SAR (0045/2021/A), Key Project of Medicine Discipline of Guangzhou (Grant No. 2021-2023-11), Key Research and Development Program of Guangdong Province (Grant No. 2021A1111120009), Science and Technology Project of Guangzhou (Grant No. 202102100003), and Emergency Key Program of Guangzhou Laboratory (Grant No. EKPG21-06).
The authors thank Xuanran Tao for his advice on this article. The authors are sincerely grateful to all epidemiology investigators, staffs of local community office, medical workers, and volunteers for their hard work in helping to control the epidemic outbreak. Thanks to all patients and Guangzhou citizens for their collaboration.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.979063/full#supplementary-material
1. World Health Organization. Tracking SARS-CoV-2 variants (2022). Available online at: https://www.who.int/activities/tracking-SARS-CoV-2-variants (accessed June 24, 2022).
2. Boarman A. Omicron is the Dominant COVID Variant for Two Reasons (2021). Available online at: https://vitals.sutterhealth.org/omicron-is-the-us-dominant-covid-variant-for-two-reasons/ (accessed June 24, 2022).
3. Burki TK. Omicron variant and booster COVID-19 vaccines. Lancet Respir Med. (2022) 10:e17. doi: 10.1016/S2213-2600(21)00559-2
4. World Health Organization. COVID-19 Weekly Epidemiological Update. Geneva: World Health Organization (2022).
5. Brandal LT, MacDonald E, Veneti L, Ravlo T, Lange H, Naseer U, et al. Outbreak caused by the SARS-CoV-2 Omicron variant in Norway, November to December 2021. Euro Surveill. (2021) 26:2101147. doi: 10.2807/1560-7917.ES.2021.26.50.2101147
6. Mefsin Y, Chen D, Bond HS, Lin Y, Cheung JK, Wong JY, et al. Epidemiology of infections with SARS-CoV-2 Omicron BA.2 variant in Hong Kong, January-March 2022. medRxiv. (2022). doi: 10.1101/2022.04.07.22273595
7. Ling C-Q. Complementary and alternative medicine during COVID-19 pandemic: What we have done. J Integr Med. (2022) 20:1–3. doi: 10.1016/j.joim.2021.11.008
8. Liu J, Liu M, Liang W. The Dynamic COVID-Zero Strategy in China. China CDC Wkly. (2022) 4:74–5. doi: 10.46234/ccdcw2022.015
9. Nealon J, Cowling BJ. Omicron severity: milder but not mild. Lancet. (2022) 399:412–3. doi: 10.1016/S0140-6736(22)00056-3
10. Peacock TP, Brown JC, Zhou J, Thakur N, Newman J, Kugathasan R, et al. The SARS-CoV-2 variant, Omicron, shows rapid replication in human primary nasal epithelial cultures and efficiently uses the endosomal route of entry. bioRxiv. (2022). doi: 10.1101/2021.12.31.474653
11. GOV.UK. COVID-19 Response: Living with COVID-19 (2022). Available online at: https://www.gov.uk/government/publications/covid-19-response-living-with-covid-19/covid-19-response-living-with-covid-19 (accessed June 24, 2022).
12. Office, TSCI. P.R.C. Press conference held on situation regarding strict prevetion and control of COVID-19 epidemic 2022 Available online at: http://www.gov.cn/xinwen/gwylflkjz193/index.htm (accessed June 24, 2022).
13. Luo L, Yang Z, Liang J, Ma Y, Wang H, Hon C, et al. Crucial control measures to contain China's first Delta variant outbreak. Natl Sci Rev. (2022) 9:nwac004. doi: 10.1093/nsr/nwac004
14. Modes ME, Directo MP, Melgar M, Johnson LR, Yang H, Chaudhary P, et al. Clinical characteristics and outcomes among adults hospitalized with laboratory-confirmed SARS-CoV-2 infection during periods of B. 1.617. 2 (Delta) and B. 1.1. 529 (Omicron) variant predominance—one hospital, California, July 15–September 23, 2021, and December 21, 2021–January 27, 2022. Morb Mort Weekly Rep. (2022) 71:217–23. doi: 10.15585/mmwr.mm7106e2
15. Faust JS, Du C, Liang C, Mayes KD, Renton B, Panthagani K, et al. Excess mortality in Massachusetts during the delta and omicron waves of COVID-19. JAMA. (2022) 328:74–76. doi: 10.1001/jama.2022.8045
16. McMenamin ME, Nealon J, Lin Y, Wong JY, Cheung JK, Lau EHY, et al. Vaccine effectiveness of two and three doses of BNT162b2 and CoronaVac against COVID-19 in Hong Kong. medRxiv. (2022). doi: 10.2139/ssrn.4064649
17. Commission GMH. Guangzhou had received 54.33 million doses of COVID-19 vaccine as of May 1 (2022). Available online at: https://www.163.com/dy/article/H6COFB6F055004XG.html (accessed June 24, 2022).
18. Dejnirattisai W, Huo J, Zhou D, Zahradnik J, Supasa P, Liu C, et al. SARS-CoV-2 Omicron-B.1.1.529 leads to widespread escape from neutralizing antibody responses. Cell. (2022) 185:467–84 e15.
19. VanBlargan LA, Errico JM, Halfmann PJ, Zost SJ, Crowe JE, Purcell LA, et al. An infectious SARS-CoV-2 B11529 Omicron virus escapes neutralization by therapeutic monoclonal antibodies. Nat Med. (2022) 28:490–5. doi: 10.1038/s41591-021-01678-y
20. Raffle AE, Pollock AM, Harding-Edgar L. Covid-19 mass testing programmes. BMJ. (2020) 370:m3262. doi: 10.1136/bmj.m3262
21. Tarkoma S, Alghnam S, Howell MD. Fighting pandemics with digital epidemiology. EClinicalMedicine. (2020) 26:100512. doi: 10.1016/j.eclinm.2020.100512
Keywords: COVID-19, public health, control measure, epidemiological investigation, health code
Citation: Cai W, Yang Z, Liang J, Lin Z, Ma Y, Chen C, Li Y, Li Y, Mai Z, Mai K, Kong X, Liang X, Li Q, Tu C, Chen C, Hon C, Qin P, Li K, Li X, Miao Y, Liu X, Guan W, Zeng Z, Qiu W, He W, Zhang L, Yang Z and Zhong N (2022) How fast and how well the Omicron epidemic was curtailed. A Guangzhou experience to share. Front. Public Health 10:979063. doi: 10.3389/fpubh.2022.979063
Received: 27 June 2022; Accepted: 03 November 2022;
Published: 21 December 2022.
Edited by:
Hongping Yuan, Guangzhou University, ChinaReviewed by:
Jianhui Nie, National Institutes for Food and Drug Control, ChinaCopyright © 2022 Cai, Yang, Liang, Lin, Ma, Chen, Li, Li, Mai, Mai, Kong, Liang, Li, Tu, Chen, Hon, Qin, Li, Li, Miao, Liu, Guan, Zeng, Qiu, He, Zhang, Yang and Zhong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lin Zhang, emhfbEAyMWNuLmNvbQ==; Zhicong Yang, Z2RnemNkY0AxNjMuY29t; Nanshan Zhong, bmFuc2hhbkB2aXAuMTYzLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.