- 1Centre for Addiction and Mental Health (CAMH) and Department of Psychiatry, Campbell Family Mental Health Research Institute, University of Toronto, Toronto, ON, Canada
- 2Institute of Medical Science, University of Toronto, Toronto, ON, Canada
- 3Institute for Mental Health Policy Research, CAMH, Toronto, ON, Canada
- 4Dalla Lana School of Public Health, University of Toronto, Toronto, ON, Canada
- 5Krembil Centre for Neuroinformatics, CAMH, Toronto, ON, Canada
- 6Provincial System Support Program (PSSP), CAMH, Toronto, ON, Canada
Introduction: Governments and public health authorities across many jurisdictions implemented social (physical) distancing measures to contain the spread of the 2019 novel coronavirus disease (COVID-19). Adherence to these measures is variable and likely influenced by various factors. This study aimed to 1) identify the individual sociodemographic, COVID-19 and social distancing related, and psychological determinants of social distancing adherence, and 2) explore regional differences in social distancing adherence in the United States (U.S.) and English-speaking Canada based on each region's discrepant response to social distancing restrictions.
Methods: A web-based repeated cross-sectional survey was conducted in 4,942 English-speaking participants from the four most populous U.S. states, specifically New York, California, Texas, and Florida, and Canada (www.covid19-database.com). The study was conducted at two timepoints, from May 1 to 5, 2020 (n = 1,019, Canadian participants only) and from July 6 to 10, 2020 (n = 3,923). Separate univariate models were computed for individual sociodemographic, COVID-19 and social distancing related, and psychological determinants of social distancing adherence. To determine the total variance explained, a univariate analysis including all of the determinants was performed. Regional differences in social distancing were compared between the four U.S. states and Canada, and between the U.S. as a whole and Canada.
Results: Adherence to social distancing was higher in May (mean = 4.4/5.0±0.7) compared to July (mean = 4.3/5.0±0.7) [t(4940) = 6.96, p < 0.001], likely a reflection of relaxing restrictions. There were no regional differences in adherence. Sociodemographic, COVID-19 and social distancing related, and psychological determinants explained 10, 36, and 23% of the variance of social distancing adherence, respectively. Higher perceived seriousness of COVID-19 [β (SE) = 0.39 (0.01), p < 0.001, partial η2 = 0.22], lower risk propensity [β (SE) = −0.15 (0.01), p < 0.001, partial η2 = 0.06], germ aversion [β (SE) = 0.12 (0.01), p < 0.001, partial η2 = 0.03], age [β (SE) = 0.01 (0.00), p < 0.001, partial η2 = 0.02], and greater social support [β (SE) = 0.03 (0.00), p < 0.001, partial η2 = 0.02] had the largest effects on social distancing adherence.
Conclusion: Public service initiatives to emphasize the serious consequences of infection and targeted interventions toward certain sociodemographic groups, such as younger adults and vulnerable individuals in greater need of social support, may help enhance the public's adherence to social distancing measures during subsequent waves of COVID-19 and future pandemics.
Introduction
The 2019 novel coronavirus disease (COVID-19) was first identified at the end of 2019 in stallholders working at the South China Seafood Market in Wuhan, a city in the Hubei Province of China. On December 31, 2019, Chinese authorities alerted the World Health Organization (WHO) of an outbreak of a novel coronavirus. The first confirmed cases of COVID-19 were reported in the United States (U.S.) and Canada in January 2020 (1, 2). In March, the WHO characterized the COVID-19 outbreak as a pandemic. As of May 1, 2020, there were 3 million cases of COVID-19 and 224,172 deaths attributable to COVID-19 globally. Two months later, as of July 1, 2020, the global number of cases and deaths increased to 10 million and 508,055, respectively (3).
Government agencies around the world had advised social (physical) distancing and other infection prevention and control measures to prevent the transmission of COVID-19 (4, 5). These included public gathering bans, school and nonessential business closures, and advisements to maintain physical distance from non-household contacts. These interventions are considered essential to ‘flatten the curve’ (6). The aim of flattening the curve is to avoid overwhelming the healthcare system (7), as occurred in Lombardy, Italy and New York City, U.S. If enacted early, through a coordinated response among public agencies, and with cooperation of the population, mortality attributable to the pandemic can be reduced (6, 8). By pushing cases into the future, social distancing measures allow more time for the creation of additional healthcare infrastructure and the development and testing of antiviral drugs and vaccines.
There is evidence that social distancing measures have been effective in countries that enacted epidemic control measures in a timely manner (Supplementary Figure 1) (9). Prolonged or intermittent social distancing is required to mitigate further transmission of COVID-19 until the adequate dissemination of vaccines (10, 11). Lessons from past pandemics indicate that relaxing social distancing leads to an increase in cases of infection, and that the rate and number of cases is proportional to implementation delays in social distancing restrictions. Communities that enacted prolonged social distancing fared better than those that withdrew social distancing prematurely (6, 12).
Although these measures are advised by the leading health authorities around the world, including the WHO and U.S. Center for Disease Control and Prevention (CDC), other potent factors influence the political decision to maintain or relax social distancing restrictions. Specifically, the economic impact of “nonessential” business closures weighs heavily on the minds of policy decision-makers and is the rationale for loosening restrictions (13, 14). Many jurisdictions have made allowances for some businesses to be reopened and small gatherings permitted. A resurgence of cases may halt or reverse the phased relaxation of government mandated restrictions (15). Additionally, some members of society may oppose social distancing restrictions, for example, by minimizing the seriousness of COVID-19, and in turn, not adhere to infection prevention measures (16), which may undermine the public health response.
With the increase in new COVID-19 cases and deaths around the world, and given the evidence in favor of extended social distancing measures to reduce morality (6), it is important to identify the determinants of social distancing adherence. A scoping review carried out in 2021 that incorporated 84 studies investigating the determinants of social distancing adherence found that “Environmental Context and Resources” and the “Person X Environment Interaction” were the two most coded constructs identified (17). The former refers to a broad category that depicts a person's situation, such as their economic status, their demographic characteristics, the severity of the pandemic in their locality, and the specific public health policies, while the latter represents the interaction between participants' demographic characteristics or personality traits and their environment. Other frequently coded constructs include “Beliefs about Consequences,” “Emotion,” and “Social influence” (17). Another systematic review that included 28 studies about the barriers to social distancing adherence identified several individual and community level factors. Individual level factors included lacking trust in government and authority, knowledge or misconceptions about the disease, and perceived lack of threat of COVID-19 (18). Additional influences identified by this review that might hinder social distancing adherence included financial hardship, dependence on social networks and support systems, and social-cultural norms (18). Both reviews highlighted the influence of individual sociodemographic and psychological factors on adherence to social distancing restrictions.
This study aimed to add to the literature investigating the determinants of social distancing adherence. Specifically, the study intended to: (1) identify the individual sociodemographic, COVID-19 and social distancing related, and psychological determinants of social distancing adherence, and (2) explore regional differences in social distancing adherence in the U.S. and English-speaking Canada. We hypothesized a higher degree of adherence to social distancing in New York, California, and Canada compared to Florida and Texas based on each region's discrepant response to the public health recommendations at the time of the study (19).
Methods
Data collection
Responses from a web-based repeated cross-sectional survey were collected from 4,942 participants 18 years of age or older from the most populous U.S. states, including California, New York, Texas, and Florida, and English-speaking Canada (www.covid19-database.com). The survey was conducted from May 1 to 5 (n = 1,019) and from July 6 to 10, 2020 (n = 3,923) (Figure 1). Responses from the U.S. were collected in July only. Our target sample was quota controlled for age. All participants provided written informed consent. Information regarding survey development and quality-control can be found in Supplementary material 1. All participants provided written informed consent prior to starting the survey. The study was approved by the Centre for Addiction and Mental Health's Research Ethics Board.

Figure 1. Weekly number of new confirmed COVID-19 cases per million people in the United States and Canada. The survey data was collected from May 1 to 4, 2020 (n = 1,019) and from July 6 to 10 (n = 3,923). Source: COVID-19 Data Repository by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (20) via Our World in Data.
Measures
We developed the Social Distancing Adherence Scale based on recommendations from the WHO, CDC, and Public Health Agency of Canada (5, 21, 22). The scale consists of 6 items each assessed using a Likert scale, from “1, Never” to “5, Always” (Supplementary material 2). A summary score was calculated to assess the degree of social distancing adherence. The scale items had high internal consistency (Cronbach's alpha = 0.90).
Participants provided sociodemographic information and completed a battery of measures including: Citizen Trust in Government Organizations' Scale (CTGO) (23), Risk Propensity Scale (RPS) (24), Perceived Vulnerability to Disease Questionnaire (PVD) (25), Multidimensional Iowa Suggestibility Scale (MISS) (26), Duke University Religion Index (DRI), religiosity/spirituality subscale (27), Ten-Item Personality Inventory (TIPI) (28), Vaccine Attitude Examination (VAX) (29), Holistic Complementary and Alternative Medicine Questionnaire (HCAM) (30), Brief Locus-of-Control Scale (LOC) (31), General Trust Scale (GTS) (32), Authority Behavior Index (ABI) (33), Positive and Negative Affect Schedule (PANAS) (34), and Experiences in Close Relationships Scale (ECR) (35). A detailed description of each of the above measures and their internal reliability can be found in Supplementary material 3. All variables were categorized as a sociodemographic, COVID-19 and social distancing related, or psychological determinant.
Statistical analyses
Univariate analyses were performed to identify the main determinants of social distancing adherence. A separate model was created for: (1) sociodemographic, (2) COVID-19 and social distancing related, and (3) psychological determinants. Beta (β) and partial eta squared (η2) values were generated and a threshold of p < 0.01 (0.05/3 models) was used to determine significance. Partial η2 values were used to define small (η2 = 0.01), medium (η2 = 0.06), and large (η2 = 0.14) effect sizes (36, 37). The above analyses were repeated with timepoint as a covariate (i.e., responses collected in May or July). To determine the total variance explained, a univariate analysis including all of the determinants in a single model was performed.
For exploratory purposes, the associations between the determinants and social distancing adherence were examined using spearman correlations and one-way analysis of variance (ANOVA) tests for continuous and categorical determinants, respectively. Correlation coefficients and VIF values were inspected for multicollinearity as defined by correlation coefficients ≥0.7 and VIF values ≥10.
Regional differences in social distancing adherence were compared between New York, California, Florida, Texas, and Canada, and between the U.S. as a whole and Canada using ANOVA. As no data from the U.S. was collected in May, only the responses from July were used to compare regional differences. A threshold of p < 0.05 was used to determine significance.
Statistical analyses were performed using SPSS Statistics (version 26 IBM Corp., Armonk, N.Y., USA).
Subgroup analyses
Univariate analyses using the same methodology described above were performed for the following groups: males and females, and participants >60 years of age.
Results
Sample characteristics
Participants were broadly representative of the U.S. and Canadian population with respect to age [mean (SD) = 44.7 (17.3)] and gender (50.8% woman). The majority of participants identified as White/Caucasian (66.8%). The majority of participants identified with a religion (63.4%), with the greatest representation from Christians (45.4%), the majority identifying as Roman Catholics (20.9%). A large proportion of the sample identified as “No religion” (39.5%). The most frequently reported political affiliation was center (35.6%), followed by liberal (29.4%) and conservative (27.4%). Although most of the participants were employed (55.3%), close to 12% of participants were unemployed. Students and retirees represented 5.7 and 22.1% of the sample, respectively. The most frequently reported household income was $60,000–$99,999. The majority of the participants reported drinking alcohol (63.7%). Close to 19, 13, and 18% of the participants endorsed smoking cigarettes, using electronic cigarettes/“vape,” and cannabis products in the past week, respectively.
Participants reported knowing someone personally close who is at higher risk of COVID-19, including a healthcare worker (37.5%), someone who is elderly or has an underlying health condition (63.4%), or lives in a senior's residence (20.6%) or a long-term care home (17.4%). At the time of the survey, the majority of participants did not know anyone personally close who is or was infected with COVID-19 (71.7%). Close to 15% of the survey participants indicated that they were tested for COVID-19 and 2.6% reported that they had tested positive. Although the majority of participants believed COVID-19 originated naturally from animals to humans (64.6%), a substantial proportion believed COVID-19 originated intentionally in a lab (19.2%), accidentally in a lab (8.4%), or does not exist (1.2%) (Table 1).
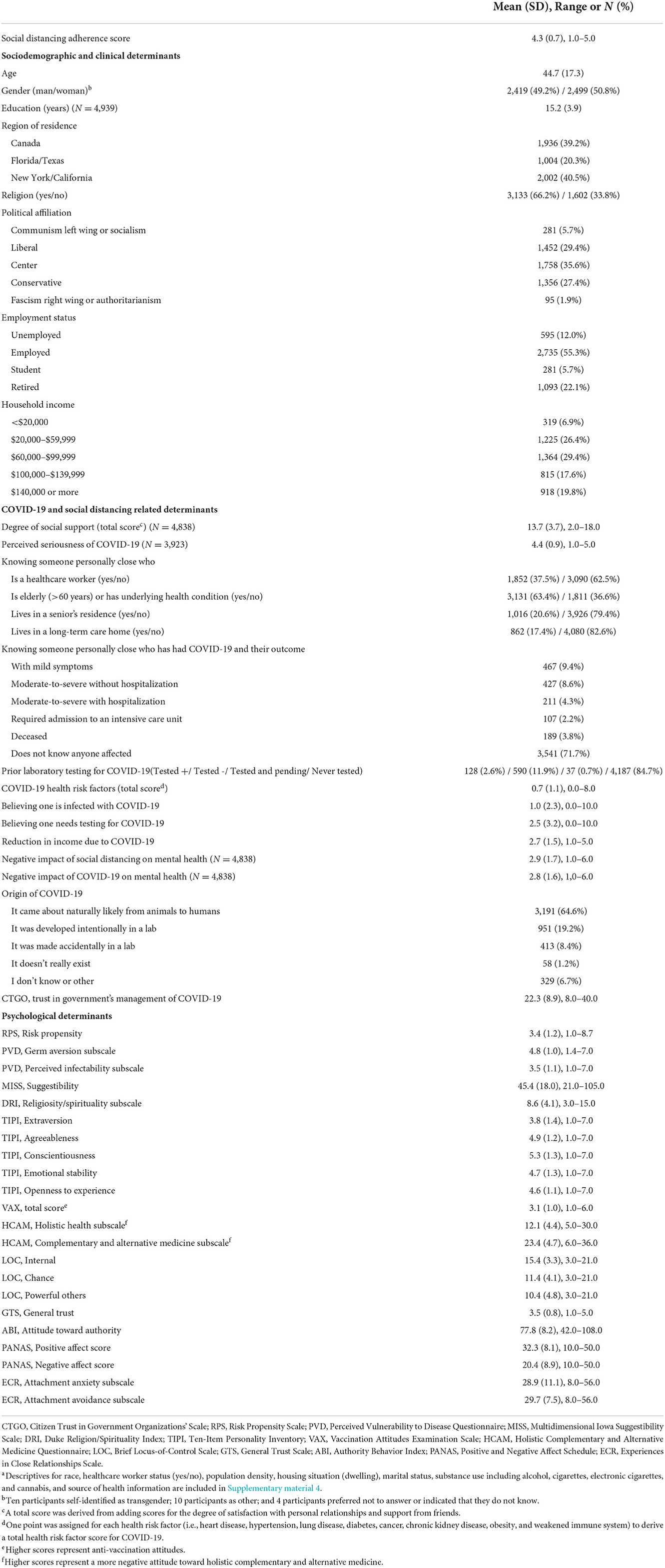
Table 1. Participant characteristics including sociodemographic and clinical, COVID-19 and social distancing related, and psychological determinantsa.
Social distancing adherence
The mean (SD) social distancing adherence score was 4.3/5.0 (0.7). Adherence was higher in May [mean (SD) = 4.4/5.0 (0.7)] compared to July [mean (SD) = 4.3/5.0 (0.7) [t(4940) = 7.0, p < 0.001], likely a reflection of relaxing restrictions.
There was no regional difference between New York, California, Florida, Texas, and Canada. Social distancing adherence scores were higher in the U.S. compared to Canada [mean (SD) = 4.3 (0.7) and 4.2 (0.7), respectively, F(1, 3922) = 4.68, p = 0.031].
Sociodemographic determinants of social distancing adherence
Sociodemographic determinants explained 10% of the variance of social distancing adherence. Sociodemographic determinants of social distancing adherence with small effects were older age, women, and left-wing political affiliation (Table 2, Supplementary Figure 2). Controlling for timepoint (i.e., responses collected in May or July) did not change the results.
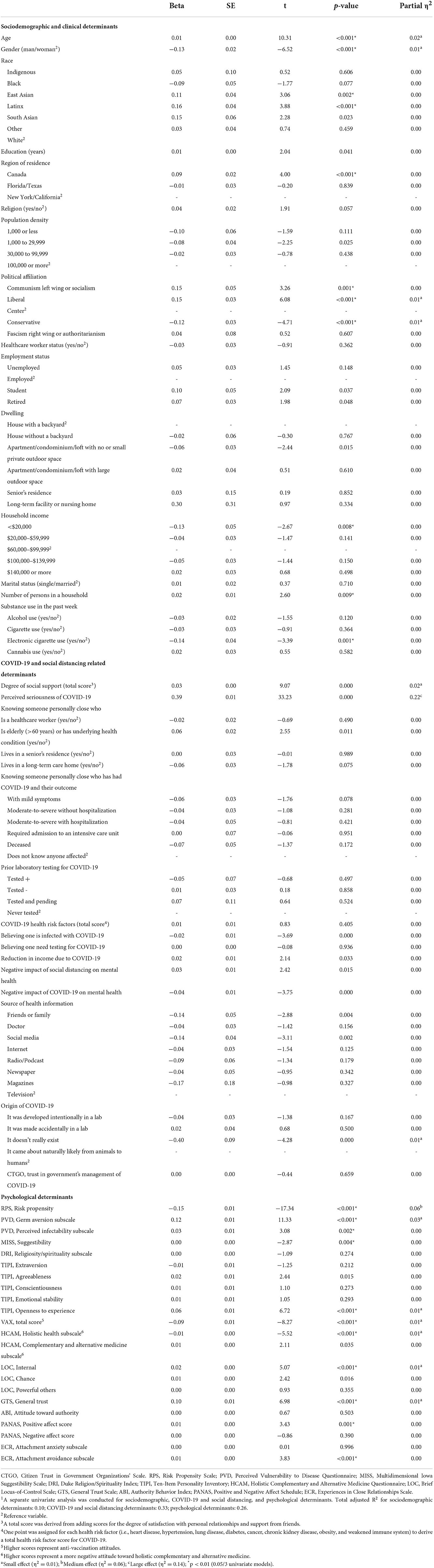
Table 2. Univariate analysis examining the association between sociodemographic, COVID-19 and social distancing related, and psychological determinants and social distancing adherence.1
COVID-19 and social distancing related determinants of social distancing adherence
COVID-19 and social distancing related determinants explained 33% of the variance in social distancing adherence. The main COVID-19 and social distancing related determinant with a large effect was higher perceived seriousness of COVID-19. Greater social support and believing that COVID-19 originated naturally rather than believing that it does not exist had small effects on social distancing adherence (Table 2). Controlling for timepoint did not change the results.
Psychological determinants of social distancing adherence
Psychological determinants explained 26% of the variance in social distancing adherence. The main psychological determinant of social distancing adherence with a medium effect was lower risk propensity. Other psychological determinants with small effects were germ aversion, the personality trait of openness to experience, positive attitudes toward vaccinations and holistic health approaches, higher internal locus-of-control, and general trust in others (Table 2). Controlling for timepoint did not change the results.
The total variance explained by sociodemographic, COVID-19 and social distancing related, and psychological determinants was 40% [F(96, 3861) = 27.58, p < 0.001] (Figure 2).
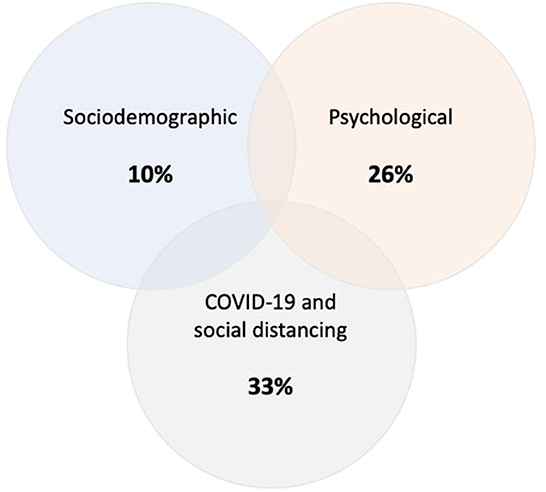
Figure 2. Variance of social distancing adherence explained by sociodemographic, COVID-19 and social distancing related, and psychological determinants. The percentages represent R2 that was derived from separate univariate models for each category. The total variance explained by sociodemographic, COVID-19 and social distancing related, and psychological determinants was 40%.
Exploratory analyses
Exploratory analyses examining the associations between the individual determinants and social distancing adherence are presented in Supplementary material 5.
Subgroup analyses
Descriptive analyses and results of univariate analyses in men, women, and participants 60 years of age or older can be found in Supplementary materials 4–14.
The principal determinants of social distancing adherence identified in the subgroup analyses are consistent with those found in the main analysis. Of note, in women, less negative mental health impact of COVID-19 and source of health information (i.e., preference for television over social media) had a small effect on social distancing adherence. In men, knowing someone personally close who is elderly was associated with a small effect on social distancing adherence. Also, in men, and in participants 60 years of age or older, an avoidant attachment style emerged as a determinant of social distancing adherence with a small effect.
Discussion
At the time of this study, perceptions of COVID-19 and the determinants of adherence to the recommended social distancing measures remained largely unknown. With the number of new cases of COVID-19 rising around much of the world, adherence with social distancing restrictions remained an active issue in relation to the containment and reduction of mortality attributable to COVID-19. While sustained social distancing strategies can save lives (6), prolonged social distancing may have considerable negative consequences, including loneliness, adverse mental health effects (38), and substantial social, educational, and economic disruption.
Our study found that adults in the U.S. and Canada were generally adherent to social distancing measures. At the time of the survey, messaging from the Government of the United States and Canada was to ‘Reopen’ (14, 39). As a whole, the U.S. states studied were modestly more adherent to social distancing restrictions than Canada. This may be due to reversal of reopening plans at that time due to the rising number of COVID-19 cases in some U.S. states, including California (see Figure 1, Timepoint 2, when regional differences were analyzed) (40).
Sociodemographic and psychological determinants explained 10% and 26% of the variance in social distancing adherence, respectively. COVID-19 and social distancing related factors explained 33% of the variance in social distancing adherence (Figure 2). The main determinant of social distancing adherence was higher perceived seriousness of COVID-19, followed by higher risk propensity. The principal finding that an individual's perception of the of seriousness of COVID-19 is consistent with the results of a systematic review that reported an individual's perception of COIVD-19 as a threat contributes to adherence to social distancing restrictions (18). Risk propensity refers to an individual's general tendency to take risks (24). Few studies have explored the role of risk propensity on social distancing behavior during COVID-19. All of these investigations, however, indicate that individuals with lower risk tolerance are more likely to adhere to social distancing restrictions, independent of the perceived seriousness or objective threat of COVID-19 (41). In contrary, people with higher risk propensity are more likely to engage in behaviors that are considered risky in the context of COVID-19 (42, 43).
In summary, our results describe individuals most likely to be nonadherent with social distancing restrictions as younger men with a right-wing political affiliation. They do not believe COVID-19 is serious or that it exists. They have a higher propensity for risk, negative attitudes toward vaccinations or holistic health approaches, a weak sense of self-agency (i.e., low internal locus of control), and are generally distrusting of others. Although there were minor differences in the determinants of social distancing adherence in men, women, and participants 60 years of age or older, the main determinants of social distancing adherence identified in these subgroups were consistent with those found in the main analysis. Other studies in varied countries have also supported our findings that age, gender, political affiliation, distrust, and perceived self-control are individual determinants that contribute to adherence to social distancing measures (44–48).
Of note, other studies have found that COVID-19 awareness of the COVID-19 pandemic and lack of concrete knowledge about the disease influence social distancing adherence, highlighting the importance of public education (18, 48, 49).
The results of our study are limited by the known biases associated with research participation, namely, individuals that consent to participate in research are often more conscientious and willing to sacrifice their time to support the greater good than are nonparticipants (50). Another limitation that is intrinsic to web-based surveys is that participants who are unfamiliar with using a computer or have no internet access are not represented. However, given the time sensitivity of the study, a web-based survey allowed for reaching a larger number participants within a short period of time without compromising validity and reliability (51). Further, we are unable to comment on the direction of the associations given the cross-sectional nature of the study.
Conclusions
The success of public health interventions, such as social distancing, depend on public support and adherence (6). Our study identified individual sociodemographic, COVID-19 and social distancing related, and psychological determinants that can inform public health and other authorities to develop public service interventions to improve social distancing adherence and contain the spread of COVID-19 and future infections more effectively. These may include public service initiatives to emphasize the seriousness of COVID-19 and future infectious diseases, and tackle false or misleading information about them. Targeted interventions toward certain sociodemographic groups, such as younger men and vulnerable individuals in greater need of social support, and health communications promoting a sense of control over COVID-19 and future infections and their consequences may also be beneficial.
Targeted recommendations
1) Seriousness of infection: Emphasize the seriousness of COVID-19, including increasing awareness of the risk of transmission, likelihood of serious illness, and the associated morbidity.
2) Risk propensity and germ aversion: Increase knowledge of the risk of transmission without infection prevention measures, including social distancing, and the elevated risk of mortality, particularly in the elderly. Influence perceptions by emphasizing the likelihood of a serious negative outcome with COVID-19 infection. Individuals may minimize the seriousness of COVID-19 after acquiring personal knowledge of individuals with mild cases of the infection.
3) Social support: Promote virtual social connection and support to address social isolation. Concerned, consistent, accessible others may alleviate one's sense of social isolation and attachment anxiety (52).
4) Attitudes toward vaccinations: Enhance the public's confidence in safety and effectiveness of vaccines and the systems recommending and providing it. Increase awareness that vaccination is required to prevent infection and transmission of COVID-19, and that the benefits of any safe and effective vaccine outweigh the possible consequences.
5) Perception of holistic health: Promote a holistic attitude where individuals are mindful of the effects of emotional wellbeing on physical health, i.e. “Mental health is health” (53).
6) Internal locus-of-control: Promote individual agency or sense of control over COVID-19 and its consequences (e.g., the message “Conquering COVID-19 is in my hands! By adopting good hygiene and social distancing practices, I am keeping myself, family, friends, and my community safe,” may instill a sense of control over the impact of COVID-19 and enhance one's ability to practice protective behavior).
Data availability statement
The raw data supporting the conclusions of this article are available, without undue reservation, at: http://www.covid19-database.com/.
Ethics statement
All studies involving human participants are reviewed and approved by the Centre for Addiction and Mental Health. Participants provided their written informed consent to participate in this study.
Author contributions
PG, JK, and AG-G: agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors: substantial contributions to the conception or design of the work and/or the acquisition, analysis, or interpretation of data for the work, drafting of the manuscript and/or revising it critically for important intellectual content, final approval of the version to be published.
Funding
This study was funded by Center for Addiction and Mental Health Foundation and Canadian Institutes of Health Research. This work was also supported by the CAMH Foundation, an Academic Scholars Award from the Department of Psychiatry, University of Toronto, and Canadian Institute of Health Research (CIHR) (PJT-159807 to PG).
Conflict of interest
PG reports receiving research support from the Canadian Institute of Health Research (CIHR), Ontario Ministry of Health and Long-Term Care, Ontario Mental Health Foundation (OMHF), and the Center for Addiction and Mental Health (CAMH). FC has received funding from the CIHR Post-doctoral Fellowship Award and the CAMH Foundation. AG-G has received support from the United States National Institute of Health, CIHR, OMHF, Consejo Nacional de Ciencia y Tecnología, the Instituto de Ciencia y Tecnología del DF, the Brain & Behavior Research Foundation (Formerly NARSAD), the Ontario Ministry of Health and Long-Term Care, the Ontario Ministry of Research and Innovation Early Research Award, and Janssen.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.977857/full#supplementary-material
References
1. Centers for Disease Control and Prevention. First Travel-related Case of 2019 Novel Coronavirus Detected in United States. Centers for Disease Control and Prevention. (2020). Available online at: https://www.cdc.gov/media/releases/2020/p0121-novel-coronavirus-travel-case.html (accessed January 18, 2021).
2. Public Health Agency of Canada. Coronavirus Disease 2019 (COVID-19): Epidemiology Update. Government of Canada. (2021). Available online at: https://health-infobase.canada.ca/covid-19/epidemiological-summary-covid-19-cases.html (accessed January 18, 2021).
3. World Health Organization. Coronavirus Disease (COVID-19) Situation Report – 106. (2020). Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed January 21, 2021).
4. Centers for Disease Control and Prevention. COVID-19 and Your Health. Centers for Disease Control and Prevention. (2020). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html (accessed January 18, 2021).
5. Public Health Agency of Canada. Coronavirus Disease (COVID-19): Prevention and Risks. (2020). Available online at: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/prevention-risks.html (accessed May 3, 2020).
6. Markel H, Lipman HB, Navarro JA, Sloan A, Michalsen JR, Stern AM, et al. Nonpharmaceutical interventions implemented by US cities during the 1918-1919 influenza pandemic. JAMA. (2007) 298:644–54. doi: 10.1001/jama.298.6.644
7. Tuite AR, Fisman DN, Greer AL. Mathematical modelling of COVID-19 transmission and mitigation strategies in the population of Ontario, Canada. CMAJ. (2020) 192:E497–E505. doi: 10.1503/cmaj.200476
8. Markel H, Stern AM, Navarro JA, Michalsen JR, Monto AS, DiGiovanni C. Nonpharmaceutical influenza mitigation strategies, US communities, 1918-1920 pandemic. Emerg Infect Dis. (2006) 12:1961–4. doi: 10.3201/eid1212.060506
9. Lewnard JA, Lo NC. Scientific and ethical basis for social-distancing interventions against COVID-19. Lancet Infect Dis. (2020) 20:P631–633. doi: 10.1016/S1473-3099(20)30190-0
10. Kissler SM, Tedijanto C, Goldstein E, Grad YH, Lipsitch M. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. (2020) 368:860–8. doi: 10.1126/science.abb5793
11. Public Health Agency of Canada. COVID-19 in Canada: Using Data and Modelling to Inform Public Health Action. (2020). Available online at: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/covid-19-using-data-modelling-inform-public-health-action.html (accessed May 4, 2020).
12. Chowell G, Echevarría-Zuno S, Viboud C, Simonsen L, Tamerius J, Miller MA, et al. Characterizing the Epidemiology of the 2009 Influenza A/H1N1 Pandemic in Mexico. PLoS Med. (2011) 8:e1000436. doi: 10.1371/journal.pmed.1000436
13. Ontario. Ontario Unveils Guiding Principles to Reopen the Province. (2020). Available online at: https://news.ontario.ca/opo/en/2020/04/ontario-unveils-guiding-principles-to-reopen-the-province.html (accessed May 29, 2020).
14. U.S. Department of Health and Human Services, Center for Disease Control and Prevention. CDC Activities and Initiatives Supporting the COVID-19 Response and the President's Plan for Opening America Up Again. (2020). Available online at: https://www.whitehouse.gov/openingamerica/ (accessed January 18, 2021).
15. Leung K, Wu JT, Liu D, Leung GM. First-wave COVID-19 transmissibility and severity in China outside Hubei after control measures, and second-wave scenario planning: a modelling impact assessment. Lancet. (2020) 395:1382–93. doi: 10.1016/S0140-6736(20)30746-7
16. Draaisma M. “Bunch of Yahoos”: Ontario Premier Slams Anti-lockdown Protesters at Queen's Park | CBC News. CBC. (2020). Available online at: https://www.cbc.ca/news/canada/toronto/ontario-shutdown-protesters-queens-park-yahoos-1.5545253 (accessed May 18, 2020).
17. Noone C, Warner NZs, Byrne M, Durand H, Lavoie KL, McGuire BE, et al. A scoping review of research on the determinants of adherence to social distancing measures during the COVID-19 pandemic. Health Psychol Rev. (2021) 15:350–70. doi: 10.1080/17437199.2021.1934062
18. Sadjadi M, Mörschel KS, Petticrew M. Social distancing measures: barriers to their implementation and how they can be overcome - a systematic review. Eur J Public Health. (2021) 31:1249–58. doi: 10.1093/eurpub/ckab103
19. Thompson SA, Serkez Y, Kelley L. Opinion | How Has Your State Reacted to Social Distancing? The New York Times. (2020). Available online at: https://www.nytimes.com/interactive/2020/03/23/opinion/coronavirus-economy-recession.html (accessed September 22, 2020).
20. Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. (2020) 20:533–4. doi: 10.1016/S1473-3099(20)30120-1
21. Centers for Disease Control and Prevention. How to Protect Yourself & Others. Centers for Disease Control and Prevention. (2020). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html (accessed January 21, 2021).
22. World Health Organization (WHO). Coronavirus Disease (COVID-19) Advice for the Public. (2021). Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (accessed January 21, 2021).
23. Grimmelikhuijsen S, Knies E. Validating a scale for citizen trust in government organizations. Int Rev Adm Sci. (2015) 83. doi: 10.1177/0020852315585950
24. Meertens RM, Lion R. Measuring an individual's tendency to take risks: the risk propensity scale. J Appl Soc Psychol. (2008) 38:1506–20. doi: 10.1111/j.1559-1816.2008.00357.x
25. Duncan LA, Schaller M, Park JH. Perceived vulnerability to disease: development and validation of a 15-item self-report instrument. Pers Individ Dif. (2009) 47:541–6. doi: 10.1016/j.paid.2009.05.001
26. Kotov RI, Bellman SB, Watson DB. Multidimensional IOWA Suggestibility Scale (MISS) Brief Manual. (2004). Available online at: https://dspace.sunyconnect.suny.edu/handle/1951/60894 (accessed January 21, 2021).
27. Koenig H, Parkerson GR, Meador KG. Religion index for psychiatric research. Am J Psychiatry. (1997) 154:885–6. doi: 10.1176/ajp.154.6.885b
28. Gosling SD, Rentfrow PJ, Swann WB. A very brief measure of the Big-Five personality domains. J Res Pers. (2003) 37:504–28. doi: 10.1016/S0092-6566(03)00046-1
29. Martin LR, Petrie KJ. Understanding the dimensions of anti-vaccination attitudes: the vaccination attitudes examination (VAX) scale. Ann Behav Med. (2017) 51:652–60. doi: 10.1007/s12160-017-9888-y
30. Hyland ME, Lewith GT, Westoby C. Developing a measure of attitudes: the holistic complementary and alternative medicine questionnaire. Complement Ther Med. (2003) 11:33–8. doi: 10.1016/S0965-2299(02)00113-9
31. Sapp SG, Harrod WJ. Reliability and validity of a brief version of Levenson's Locus of Control Scale. Psychol Rep. (1993) 72:539–50. doi: 10.2466/pr0.1993.72.2.539
32. Yamagishi T, Yamagishi M. Trust and commitment in the United States and Japan. Motiv Emot. (1994) 18:129–66. doi: 10.1007/BF02249397
33. Rigby K. An authority behavior inventory. J Pers Assess. (1987) 51:615–25. doi: 10.1207/s15327752jpa5104_14
34. Crawford JR, Henry JD. The positive and negative affect schedule (PANAS): construct validity, measurement properties and normative data in a large non-clinical sample. Br J Clin Psychol. (2004) 43:245–65. doi: 10.1348/0144665031752934
35. Brennan KA, Clark CL, Shaver PR. Self-report measurement of adult attachment: An integrative overview. (1998).
36. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. New York: Routledge. (1988).
37. Richardson JTE. Eta squared and partial eta squared as measures of effect size in educational research. Educ Res Rev. (2011) 6:135–47. doi: 10.1016/j.edurev.2010.12.001
38. Galea S, Merchant RM, Lurie N. The Mental Health Consequences of COVID-19 and Physical Distancing: The Need for Prevention and Early Intervention. JAMA Intern Med. (2020) 180:817–8. doi: 10.1001/jamainternmed.2020.1562
39. CPAC. Federal ministers and health officials provide COVID-19 update – May 4, 2020. The Cable Public Affairs Channel. (2020). Available online at: https://www.youtube.com/watch?v=77NLZ403Qvo (1:20 min; 48:38 min) (accessed May 4, 2020).
40. AJMC. A Timeline of COVID-19 Developments in 2020. (2021). Available online at: https://www.ajmc.com/view/a-timeline-of-covid19-developments-in-2020 (accessed January 27, 2021).
41. Shou Y, Smithson M, Gulliver A, Murray K, Banfield M, Rodney Harris RM, et al. Risk tolerance and changes in coronavirus disease (COVID) related health behaviors: a longitudinal study. Health Psychol. (2022) 41:507. doi: 10.1037/hea0001197
42. Diaconu (Maxim) L. The Behaviour of Airlines' Passengers in the Context of COVID-19 Pandemic. CES Work Papers. (2021) 13:230–242. Available online at: https://ceswp.uaic.ro/articles/CESWP2021_XIII2_DIA.pdf
43. Leung XY, Cai R. How pandemic severity moderates digital food ordering risks during COVID-19: An application of prospect theory and risk perception framework. J Hosp Tour Manag. (2021) 47:497–505. doi: 10.1016/j.jhtm.2021.05.002
44. Gualda E, Krouwel A, Palacios-Gálvez M, Morales-Marente E, Rodríguez-Pascual I, García-Navarro EB. Social Distancing and COVID-19: Factors Associated With Compliance With Social Distancing Norms in Spain. Front Psychol. (2021) 12:727225. doi: 10.3389/fpsyg.2021.727225
45. Farias ST, Mungas D, Reed BR, Cahn-Weiner D, Jagust W, Baynes K, et al. The Measurement of Everyday Cognition (ECog): scale development and psychometric properties. Neuropsychology. (2008) 22:531–44. doi: 10.1037/0894-4105.22.4.531
46. Barbieri PN, Bonini B. Political orientation and adherence to social distancing during the COVID-19 pandemic in Italy. Econ Polit. (2021) 38:483–504. doi: 10.1007/s40888-021-00224-w
47. Sewpaul R, Mabaso M, Cloete A, Dukhi N, Naidoo I, Davids AS, et al. Social distancing behaviour: avoidance of physical contact and related determinants among South Africans: twelve days into the COVID-19 lockdown. Psychol Health Med. (2022) 0:1–19. doi: 10.1080/13548506.2022.2075020
48. Hadizadeh-Talasaz F, Delshad Noghabi A, Mohammadzadeh F. Relationship between socio-demographic factors and adherence to social distancing recommendations during COVID-19 pandemic in Gonabad, Iran: a cross-sectional study. Int J Community Based Nurs Midwifery. (2022) 10:134–45. doi: 10.30476/IJCBNM.2021.90930.1747
49. Wolff W, Martarelli CS, Schüler J, Bieleke M. High boredom proneness and low trait self-control impair adherence to social distancing guidelines during the COVID-19 pandemic. Int J Environ Res Public Health. (2020) 17:5420. doi: 10.3390/ijerph17155420
50. Lönnqvist JE, Paunonen S, Verkasalo M, Leikas S, Tuulio-Henriksson A, Lönnqvist J. Personality characteristics of research volunteers. Eur J Pers. (2007) 21:1017–30. doi: 10.1002/per.655
51. Risko EF, Quilty LC, Oakman JM. Socially Desirable Responding on the Web: Investigating the Candor Hypothesis. J Pers Assess. (2006) 87:269–76. doi: 10.1207/s15327752jpa8703_08
52. Pietromonaco PR, Uchino B, Dunkel Schetter C. Close relationship processes and health: implications of attachment theory for health and disease. Health Psychol. (2013) 32:499–513. doi: 10.1037/a0029349
53. CAMH. Mental Health is Health. CAMH. (2020). Available online at: https://www.camh.ca/en/driving-change/mental-health-is-health (accessed May 20, 2020).
Keywords: COVID-19, pandemic, social distancing adherence, disease prevention, survey, infection prevention and control, sociodemographic determinants, psychological determinants
Citation: Gerretsen P, Kim J, Brown EE, Quilty LC, Wells S, Caravaggio F, Song J, Sanches M, Agic B, Pollock BG and Graff-Guerrero A (2023) Determinants of social distancing adherence. Front. Public Health 10:977857. doi: 10.3389/fpubh.2022.977857
Received: 25 June 2022; Accepted: 23 November 2022;
Published: 12 January 2023.
Edited by:
Zhiwen Hu, Zhejiang Gongshang University, ChinaReviewed by:
Jeffrey Harris, Massachusetts Institute of Technology, United StatesIvana Hromatko, University of Zagreb, Croatia
Copyright © 2023 Gerretsen, Kim, Brown, Quilty, Wells, Caravaggio, Song, Sanches, Agic, Pollock and Graff-Guerrero. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Philip Gerretsen, cGhpbGdlcnJldHNlbkB5YWhvby5jb20=; cGhpbGlwLmdlcnJldHNlbkBjYW1oLmNh
 Philip Gerretsen1,2*
Philip Gerretsen1,2* Julia Kim
Julia Kim Eric E. Brown
Eric E. Brown Lena C. Quilty
Lena C. Quilty Samantha Wells
Samantha Wells Jianmeng Song
Jianmeng Song Marcos Sanches
Marcos Sanches Branka Agic
Branka Agic Bruce G. Pollock
Bruce G. Pollock Ariel Graff-Guerrero
Ariel Graff-Guerrero