
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Public Health , 15 September 2022
Sec. Disaster and Emergency Medicine
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.975667
This article is part of the Research Topic International Borders and Health: An Emerging Topic View all 7 articles
 Markus Ries1,2,3*†
Markus Ries1,2,3*†Background: In the context of a holistic and comprehensive disaster response effort to the COVID-19 pandemic, many countries across the globe mobilized their military forces in order to cope with sudden and exponential surges of critically ill patients with COVID-19 in stretched healthcare systems.
Objective: The purpose of this work is to identify, map, and render world-wide key concepts of civil-military cooperation (CIMIC) in disaster management during the COVID-19 crisis visible.
Material and methods: Literature was systematically searched in three databases (PubMed, Web of Science, Cochrane Library) on 26 January 2022, and analyzed with qualitative, mixed narrative-phenomenological methods in compliance with PRISM-ScR and SRQR.
Results: Forty-five publications were included in the analysis; pertinent authors were from 22 countries covering five continents. We identified three key thematic clusters in the published literature: Cluster (1) Medico-scientific contributions with the participation of military medical personnel or institutions: members of the military acted as subject matter experts, clinical and experimental (co-) investigators as well as co-founders for enabling COVID-19 relevant research. Areas covered were relevant to the COVID-19 patient's clinical journey from prevention, exposure, diagnostics, and treatment and included pertinent fields such as digital health and telemedicine, global and public health, critical care, emergency and disaster medicine, radiology, neurology, as well as other medical specialties, i.e., respiratory care, pulmonology, burn medicine, and transfusion medicine, in addition to environmental and occupational sciences as well as materials science. Cluster (2) CIMIC field experiences or analyses included areas such as political framework, strategy, structure, nature of civil-military interaction, and concrete mission reports in selected countries. Themes covered a broad spectrum of pandemic disaster management subjects such as capacity and surge capacity building, medical and pharmaceutical logistics, patient care under austere circumstances, SARS-CoV-2 testing support, intelligent and innovative information management, vaccination support, and disaster communication. Cluster (3) The military as a role model for crisis management.
Conclusion: Civil-military cooperation made a significant contribution to the level of resilience in crisis management on a global scale, positively impacting a broad spectrum of core abilities during the COVID-19 pandemic.
Coronavirus disease 2019 (COVID-19) is a rapidly spreading, pandemic, multisystemic infectious disease caused by the novel coronavirus (also known as SARS-CoV-2, i.e., severe acute respiratory syndrome coronavirus 2). First cases of a “viral pneumonia” that would later be known as COVID-19 were reported in Wuhan, China, in December 2019, on 30 January the World Health Organization (WHO) declared the rapidly spreading outbreak a “Public Health Emergency of International Concern,” and finally considered the situation a pandemic on 11 March 2020 (1). By 09 June 2022, 533.766.156 cases, 6.305.234 deaths, and 11.529.693.882 SARS-CoV-2 vaccine doses administered were reported globally (2). Transmitted through aerosols from person-to-person including still asymptomatic, but yet infectious individuals, the condition spread rapidly around the globe, impacting a large geographic area in a dramatic time dynamic that was considered a VUCA (volatile, uncertain, complex, and ambiguous) public health situation for the global disaster response community (3, 4). In the context of a holistic and comprehensive disaster response effort, many countries across the globe mobilized their military forces in order to cope with sudden and exponential surges of critically ill patients with COVID-19 in stretched healthcare systems.
Mutual challenges within the global disaster response community were intense (5). In the author's personal experience, this led to extremely close long-term cooperation between civil and military partners, providing excellent mutual learning opportunities. In contrast, the currently available range of material in the research literature on this emerging and multi-faceted topic has not yet been well-defined in detail, which renders it difficult to obtain a clear picture on global key concepts within civil-military cooperation (CIMIC) for COVID-19 disaster relief. Strengthening global societal resilience toward crises and disaster becomes increasingly important for now and the future ahead of us. Therefore, the purpose of this work is to identify, map, and render world-wide key concepts of civil-military cooperation in disaster management during the COVID-19 crisis visible (6). We therefore focused our research efforts on the macro-level question “what was the range, extent, and nature of civil-military cooperation during the SARS-CoV-2 pandemic worldwide?,” and investigated this important issue through a broad, comprehensive scoping literature review based on three, mainly medical literature databases.
This works follows the principles and methodological framework for scoping review defined by Arksey and O'Malley, i.e., mapping range, extent, and nature of the topic investigated (6). The Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist was applied for design, execution, analysis, and reporting (7). The qualitative aspects of this work follow the Standards for Reporting Qualitative Research (SRQR) checklist (8). A review protocol was not registered.
We searched three literature databases on 26 January 2022: PubMed (9), Web of Science (10), and Cochrane Library (11). A combination of three databases was chosen, because the literature included in each individual database has a specific focus; the goal of the combination was to cover a broader spectrum. COVID-19 is mainly a medical issue, therefore the three databases were chosen, because they index predominantly medical literature in contrast to other databases that focus more on sociological research.
The search parameters in the advanced search functions in all three databases were: “civil” and “military” and “COVID” as well as “CIMIC” (which is the abbreviation for “civil-military cooperation”) and “COVID.” No filter was applied. The search was non-iterative and was not modified over time.
Literature search results were transferred to the citation manager Zotero (12). Duplicates were removed. Articles were retrieved and screened. Publications were considered eligible if their focus was centered on any aspect of civil-military cooperation in the COVID-19 pandemic. Articled not fulfilling this broad eligibility criterion were excluded during screening. In order to enhance trustworthiness, a critical appraisal of credibility was undertaken based on the professional judgment of the author. Languages considered a priori were English, German, French, and Spanish as the author is fluent in these. All levels of evidence were considered.
Identified publications were analyzed through a qualitative, mixed narrative-phenomenological approach as proposed by Creswell, and as applied in previous projects of similar scope published in the peer-reviewed literature (3, 4, 13, 14). This approach was considered best for providing the highest flexibility for identification of pertinent key topics rather than analyzing data automated with pre-specified terms which would potentially miss significant statements. Specifically, narrative-phenomenological qualitative information in the articles was identified by transcribing articles into a plain text format that were assessed for significant statements as the narrow unit of analysis (13, 14). These significant statements were then horizontalized and grouped into clusters of meaning (13, 14). The coding was conducted with the open source qualitative data analysis package RQDA 0.2–8 (15) in R (16) operated with Linux Mint 20 (17).
The following variables were qualitatively analyzed for significant statements, themes and clusters of meaning: title of publication, main subject, geographical focus, time (of the pandemic the report refers to), type of medical contribution of the military, medical specialty field of the overall work, methodology of the scientific work, and country of first author (for analytical perspective) or military (co-) author(s) (for medico-scientific context). For military context, the North Atlantic Treaty Organization (NATO) membership (for military context), membership of European Union (for political context), and continent (for wider geographical context) were considered contextual variables for country of first author. Continents were designated according to the nomenclature provided by the U.S. Geological Survey (18). In order to gain a visual insight into the literature's global distribution patterns, countries of first authors' or military (co-) authors affiliations were mapped with QGIS 3.10.4 (LTR)-A Coruña for Linux Ubuntu using Natural Earth vector map data (19, 20). For medico-scientific articles, military authors' affiliation countries were mapped in order to show where the military contributions- which were often large multinational multicenter studies—originated from. For CIMIC field experiences or analyses, the country of the first author of the publication identified was mapped, because the intention was to focus on the contextual national perspective of the contribution to the literature. The thematic mind map and bubble graph were drawn with MindMaster (21).
Qualitative data analysis can be influenced by the researcher's characteristics and reflexivity. The investigator of this work is a pediatric clinician-scientist practicing, researching, and teaching at the University Hospital Heidelberg, Germany, and the University of Heidelberg, Germany, with training or work experience in Germany, the United States, France, Spain, the UK, Chile, and at the NATO (North Atlantic Treaty Organization). He serves as a reserve medical staff officer in the rank of a Lt.-Colonel (OF-4) of the German Armed Forces in the local CIMIC command. Since March 2020, he has been involved directly in coordinating military-medical COVID-19 disaster management support for the city and healthcare system of Heidelberg, Germany, as well as for hospitals in the surrounding region.
After a careful identification and screening process as illustrated in the PRISMA flow diagram (Figure 1), forty-five publications were included in the analysis. Articles were published in English, French, or Spanish.

Figure 1. Literature search strategy PRISM flow chart. Three databases (PubMed, Web of Science, and Cochrane Library) were considered. Close of database was 26 January 2022.
Three thematic clusters were identified in the phenomenological analysis (Table 1).
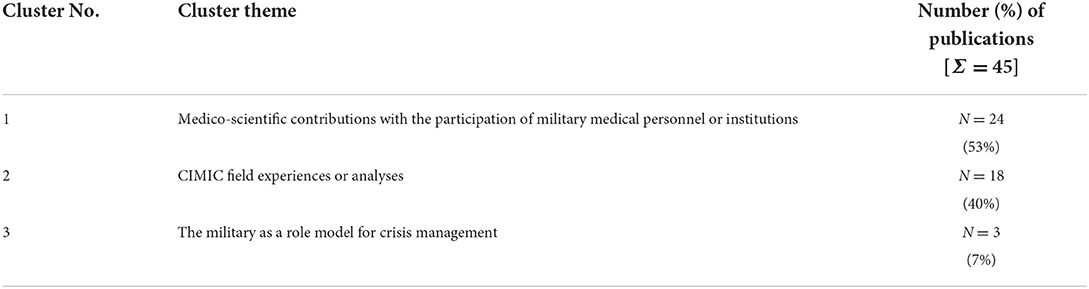
Table 1. Key concepts of civil-military interaction for disaster management during the COVID-19 pandemic: phenomenological clusters of meaning in the medical literature (searched in PubMed. Web of Science, Cochrane Library, close of database 26 January 2022).
Reports covered five continents: Asia, Europe, North America, South America, Oceania. First authors of CIMIC field reports, role model reports, and (co-) authors for medical studies included 22 different countries. Further details on thematic and geographic distribution will be presented and discussed below.
For medico-scientific contributions to the literature within CIMIC, the military acted in three distinct roles: (1) as subject matter experts, (2) as clinical or experimental investigators or co-investigators, and (3) as co-funders for research (22–45). Military subject matter expertise included telemedicine, digital health technology, critical care medicine, respiratory care, transfusion medicine, as well as global and public health. Military clinical investigators or co-investigators contributed to COVID-19 relevant topics such as critical care medicine, radiology, neurology, burn medicine, public health, emergency and disaster medicine, and pulmonology. One experimental military investigator worked within the field of environmental and occupational sciences. A synoptic overview of each contribution is provided in Figure 2, detailed information about each publication is listed in Table 2.
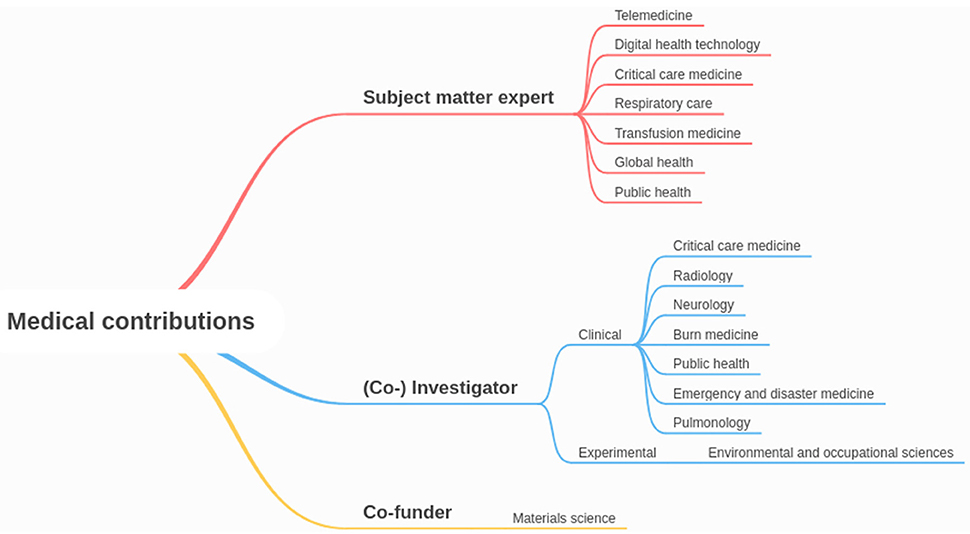
Figure 2. Mindmap of medical contributions with the participation of military medical personnel or institutions by role and specialty area covered.
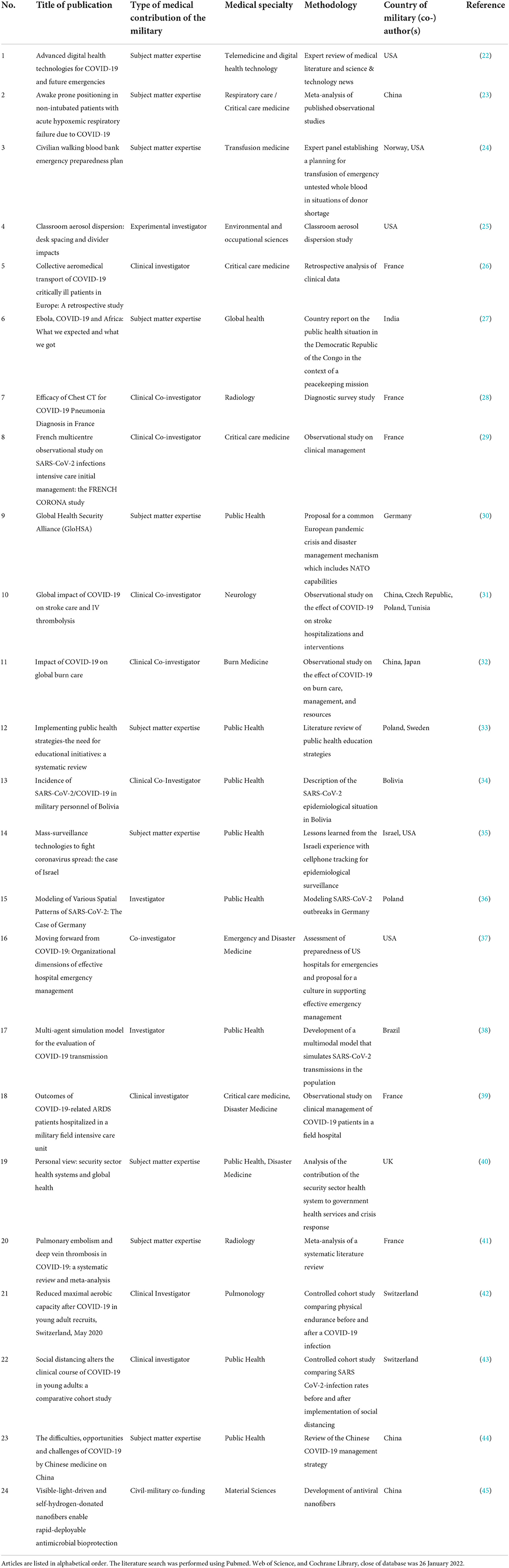
Table 2. Synopsis of medical publications that included the participation of military medical personal or institutions.
The map in Figure 3 shows countries of military (co-) authors in medico-scientific publications with military contributions during the COVID-19 pandemic.
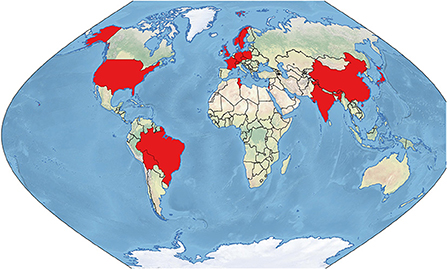
Figure 3. Countries of military (co-) authors' affiliation in medico-scientific civil-military publications during the COVID-19 pandemic (in red).
The following section reviews concrete CIMIC field experiences or analyses of such (3, 46–62). Because disaster management during COVID-19 was generally guided by national frameworks and policies, pertinent reports in this section are reviewed grouped by country of first author in order to maintain this perspective (Figure 4), appearing geographically aggregated by continent and in descending order of overall numbers of reports per country. Further details, including time periods of reports covered, are provided in Table 3.
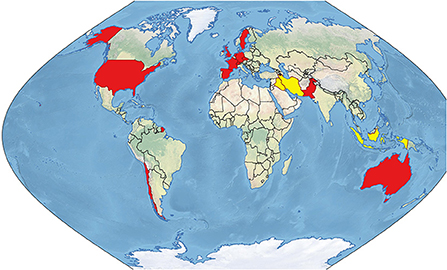
Figure 4. CIMIC field experiences and analyses during the COVID-19 pandemic. Red: first authors' countries of affiliation. Yellow: Countries in which CIMIC activities were analyzed by authors from other countries.
Gad et al. analyzed civil-military cooperation in six European countries, i.e., UK, France, Spain, Italy, Belgium and Sweden, in the early phase of the COVID-19 crisis (46). For this analysis, they identified seven main analytical themes, i.e., (1) Recognition of health security threat from coronavirus spread in Wuhan, (2) detection and announcement of first cases as reported through military health functions, (3) invocation or announcement of national crisis, plans and/or military involvement, (4) how military support was incorporated into national crisis response, (5) how the military modified its activities, (6) dealing with rumors/allegations related to COVID-19, and (7) other—military and COVID-19, and divided these themes into 19 categories of civil-military cooperation (46). The armed forces and the military medical service were key components of early disaster response and strengthened resilience, while Italy and Spain had the most intense and Sweden the least intense level of CIMIC within this group of countries (46). Gibson-Fall identified three different trends of national military involvement during the COVID-19 crisis worldwide: (1) minimal technical military support, (2) blended civil-military responses, and (3) military-led responses (47). An interesting example for enhancing crisis management capabilities in the public sector is the British stabilization unit, which facilitates cooperation between agencies, civilians and the military and could serve as a training and capacity building model (48). Ten military critical care transfer teams assisted the London Ambulance Service and transported 52 ventilated civilian patients during a COVID-19 patient surge in intensive care units in London, UK, during the last 2 weeks in April 2020 (49). Each two-member team was composed of (1) a consultant/registrar in emergency medicine and pre-hospital emergency medicine or anesthesia and (2) an emergency nurse or paramedic (49). Main lessons identified centered around overcoming technical issues with the ventilation and measures to avoid transmission SARS-CoV-2 to the staff (49).
Roßmann et al. focused on systems innovation, analyzing the dynamic challenges of the emerging COVID-19 pandemic through a Cynefin lens; very similar crisis management problems were found in different areas of the public health service in Germany (50). They identified four key areas that necessitated systems innovation to strengthen disaster resilience, i.e., (1) information-management including crisis communication, (2) data- and information-visualization (dashboard), (3) training and education of supporting staff, and (4) a framework and evaluation concept (“scoring-matrix”), and developed novel tools to adapt, change, and innovate the public disaster management system (38).
Schulze et al. described lessons learned during the SARS-CoV-2 emergency vaccination roll-out campaign in Heidelberg in the year 2020. The following five strategic elements were important for success: (1) robust mandate, (2) use of established networks, (3) fast on-boarding and securing of commitment of project partners, (4) informed planning of supply capacity, and (5) securing the availability of critical items (3). Planning tools included (1) analyses through a VUCA lens, (2) analyses of stakeholders and their management, (4) possible failures, and (5) management of main risks including mitigation strategies (3). Lessons learned identified ten tactical leadership priorities and ten major pitfalls. The authors proposed that these methods which comprised VUCA factors combined with analyses of possible failures, and management of stakeholders and risks could be adjusted to any public health care emergency anywhere across the globe in the future (3).
Barreau summarized the French civil-military operation which was entitled “resilience” and launched on 25 March 2020. The military adapted their support to the local needs and circumstances, a permanent dialogue between the civilian and military partners was important (51).
In a global analysis of military deployments in the COVID-19 crisis, Kalkman described circumstances, motivations and societal imitations of these endeavors. As such, the political framing of the pandemic as a “war,” e.g., in the US, in France, and in the UK, leveraged and triggered a military response as a logical consequence out of this narrative (52). Moreover, these deployments were also in the interest of the militaries, because they strengthened their operational readiness and societal standing as they assisted the population (52). Of note, Kalkman emphasized the necessity of civilian control and respect of civil rights for reasons of a cooperative leadership culture and balanced disaster management approach (52).
Assessment of military preparedness for civil-military cooperation in a disaster situation can be challenging and complex. Therefore, Tušer and colleagues developed a capacity and capability assessment procedure based on questionnaires and a mathematical model which includes Saaty's method (53). The goal was to determine the degree of preparedness of the Czech army for cooperation with civilian partners in disaster management including the COVID-19 crisis. and to identify specific areas for improvement (53). The four assessment criteria included (1) human resources, (2) technical security of allocated forces, (3) command and control of allocated forces, and (4) planning; these criteria were further subdivided into two or three indicators each (53).
Consistent with the report by Gad, Lopez-Garcia observed a high degree of visibility of the military and other security institutions in the crisis communication strategy of the Spanish government (46, 54). The four key axes of the crisis communication in Spain were (1) continuous communication, (2) seriousness of the crisis, (3) feeling of control, and (4) unity (54). This highly visible presence was a result of the high degree of trust that the military was enjoying in Spain compared with other public, political, private, and religious institutions. Thus, an association with the military during the COVID-19 crisis had a protective function for Spanish politicians against critics from the opposition (54).
Bacchus and colleagues emphasized the necessity of thorough inter-agency preparedness for disasters in advance (55). The report civil-military experience with the rapid deployment—initially a high readiness exercise in January 2020—of a military mobile biological field analysis laboratory and the development of a polymerase chain reaction (PCR) test in order to facilitate the diagnosis of SARS-CoV-2 infections (55). This project was a collaboration of the Swedish Armed Forces, the Public Health Agency, and a civilian hospital (55).
In Switzerland, civilian pharmacists were enlisted as reserve officers in the military and supported the civil-military crisis response in hospital battalions and medical logistics battalions (56). Overall, 5,000 mostly medical soldiers including pharmacists were mobilized 6 March to 30 June 2020 within the Swiss militia system (56). In the hospital battalion, they mainly managed supply of medical material to military and civilian entities and coordinated hygiene measures to reduce the risk of staff contamination with SARS-CoV-2 (56). Their main duty in the medical logistics battalion included pharmaceutical production support in civilian and military facilities (56).
There were two remarkable project reports on civil-military cooperation from the US. First, Dutta et al. described the deployment of 500 Navy Reserve medical professionals to New York City (57). Some of these reservists supported eleven local hospitals that were overburdened with the COVID-19 surge which led to the exhaustion of the civilian staff. This civil-military mission was an example for successful rapid deployment of medical forces and cohesive cooperation in a diverse professional setting across all specialties (57). Likewise, the Army medical service supported New York City as well. They rapidly activated and operationalized a COVID-19 inpatient care facility in a civilian congress center in New York City, successfully integrating uniformed services, governmental agencies, and private healthcare organizations (58).
In the context of the socioeconomic tensions, the military was deployed in the streets during nightly curfews based on two government decrees in Chile, reported Dragnic, a sociologist at the University of Chile (59).
Fealy, a scholar from The Australian National University published a critical but important analysis of the role of the Indonesian armed forces in the COVID-19 crisis. The Indonesian armed forces and state intelligence service had very prominent roles during the pandemic—which he considered disproportionate—that resulted in weakening democracy in Indonesia (60). Specifically, despite lacking expertise, they were involved in the production of anti-COVID-19 medicine and COVID-19 testing (60). Furthermore, the military was tasked with the enforcement of restrictions mandated by the spread of the virus in the society and were given the authority to impose punishment on citizens (60).
In Iran, Revolutionary Guards and the affiliated militia supported the COVID-19 disaster response by building field hospitals and enforcing quarantine (61).
Of interest, in Iraq, paramilitary forces and militia took over roles and responsibilities that one would expect being led and fulfilled by the government as well as the public health sector. Specifically, Iraqi paramilitary units and militia contributed to mitigating the impact of the pandemic by providing logistic support, i.e., transporting medical supplies, personal protective equipment, and food (61). They supported hygiene measures by sanitizing public spaces, but also covered typical public health activities such as medical information campaigns (61). Their approach appeared to be comprehensive and covered mental health support to medical personnel and the construction of field hospitals including a 200-bed hospital in Baghdad (61). In addition, these groups helped burying the deceased while respecting diverse religious rituals including both Muslim and Christian faith (61).
Jabbar and Makki analyzed civil-military cooperation during the COVID-19 pandemic from a leadership perspective (62). They focused on four themes, i.e., (1) the significance of CIMIC in disaster management, (2) challenges associated with CIMIC during the COVID-19 pandemic, (3) the role of a common civil-military comment operation center, and (4) government policies and practices related to disaster management (62). Of interest, most funding is spent into measures responding to a disaster rather than in prevention (62). This is not an isolated phenomenon, but a frequent global shortcoming, which is being addressed by the Sendai Framework for Disaster Risk Reduction 2015–2030 (63). Tasks of the Pakistani army included support in SARS-CoV-2-testing, logistics (i.e., distribution of medical equipment including testing kits, ventilators, personal protective equipment and drugs), disaster response coordination, and information management (62). In Pakistan, overcoming a communication gap and fostering collaboration between civilian actors was important during the COVID-19 crises (62). In the absence of international guidelines for CIMIC, a definition of the overall framework and guidelines are helpful (62). Joint training of civilian and military stakeholders improved functioning and mutual understanding, and increases trust, while previous military training of civilian actors proved to be beneficial in this regard (62).
In a New England Journal of Medicine editorial, Michael emphasized a tradition of influence from of military medicine on to its civilian partners (64). Two recent examples in the COVID-19 pandemic corroborated this relationship and dialogue. Successful management of SARS-CoV-2 outbreaks on a ship and in a Marines boot camp delivered valuable insight into virus transmission, disease understanding, diagnosis, tracking and tracing as well as appropriate quarantine measures in the early phase of the pandemic that could be extrapolated into civilian community settings such as schools, dorms, or other shared living environments (64). Katz and colleagues considered items of military medicine such as preparedness, team-based care, echelons of care, augmenting the effort, effective triage, and servant leadership as important lessons learned for adaptation into cardiac critical care during the COVID-19 pandemic (65). While hierarchical top-down, command-and control structures in healthcare may have worked well in the past in military operations, crisis management, and certain healthcare settings, they do not meet today's standards due to generational value change and complexity issues in the operational environment (66). There has been a slow shift in healthcare leadership culture toward the emphasis on emotional intelligence in order to (1) foster respect and civility to empower teams, (2) lead with transparency and open communication to promote psychological safety, and (3) lead with compassion when tackling severe problems. This change process may now experience push-backs and regression into the old-school system because of the pressure during the pandemic (66). Role model articles originated from the U.S. and Canada.
The purpose of this work was to identify, map, and render world-wide key concepts of civil-military cooperation in disaster management during the COVID-19 crisis visible. This scoping review of identified three key thematic clusters in the published literature: (1) Medico-scientific contributions with the participation of military medical personnel or institutions (2) CIMIC field experiences or analyses and (3) the military as a role model for crisis management. Pertinent authors were from 22 countries covering five continents.
For medico-scientific contributions, members of the military acted as subject matter experts, clinical and experimental (co-) investigators as well as co-founders for enabling COVID-19 relevant research. Areas covered were relevant to the COVID-19 patient's clinical journey from prevention, exposure, diagnostics, and treatment and included pertinent fields such as digital health and telemedicine, global and public health, critical care, emergency and disaster medicine, radiology, neurology, as well as other medical specialties, i.e., respiratory care, pulmonology, burn medicine, and transfusion medicine. Environmental and occupational sciences as well as materials science were represented, too.
CIMIC field experiences and analysis included areas such as political framework, strategy, structure, nature of civil-military interaction and concrete mission reports in selected countries. Themes covered a broad spectrum of pandemic disaster management subjects such as capacity and surge capacity building, medical and pharmaceutical logistics, patient care under austere circumstances, SARS-CoV-2 testing support, intelligent and innovative information management, vaccination support, and disaster communication (Figure 5).

Figure 5. Themes covered in CIMIC field experiences and analyses. Within individual reports, themes overlapped in part.
Finally, specific aspects of leadership, training, and operational capacities within the military were considered helpful and could provide role models in certain civilian emergency and disaster situations, recognizing at the same time that leadership cultures are subject to particular circumstances and change over time.
The vast majority of articles the role of the military during the COVID-19 pandemic was reported in a neutral or positive perspective in the literature reviewed here. Positive experiences included the military contribution to the advancement of medical and scientific knowledge, and providing medical care in austere circumstances. Furthermore, the use particular, sometimes even unique capabilities of the military such as leadership, technical, logistical, and organizational skills, innovative thinking, as well as the availability of rapidly deployable manpower and equipment for the purpose of serving the population and resulting in tangible disaster relief were positive, and well-received examples that should be followed in the future. On the contrary, the political frameworks of civil-military cooperation in particular in Indonesia and Chile were discussed critically by other authors (59, 60). Likewise, Medeiros Passos and Acácio analyzed the impact of military involvement in Latin American countries, in particular policing missions in the Dominican Republic, Ecuador, El Salvador, Guatemala, Bolivia, Honduras, Chile, as well as Peru, and addressed the important issue of short term-human rights degradation and aggravation of police violence (67). Furthermore, they concluded that the attribution of disaster management positions to military personnel in Brazil, Chile, Bolivia, and Peru may have weakened the civilian control of the armed forces in the future (67).
When thinking about disaster management in general, it is of utmost importance to have a fundamental understanding about the basic needs of the potentially afflicted population including the vulnerable (68, 69). For a general assessment of civil-military cooperation and a complementary regard on Gibson-Fall's valuable analysis of the three different trends of national military involvement during the COVID-19 pandemic (47), the humanitarian perspective of the United Nations is very interesting in terms of workload sharing and degree of military visibility. The UN cluster approach provides a helpful overview and orientation for main sectors of humanitarian action and disaster relief. The following functional areas are considered: camp management, early recovery, children and education, emergency telecommunications, food security, health, logistics, nutrition, protection, shelter, WaSH (water, sanitation, hygiene) (70). In principle, the UN recognizes that the military's specific capabilities and capacities are a valuable asset in humanitarian actions which includes disaster management (71). When wanting to work successfully together with a non-governmental or humanitarian organization in a disaster relief mission, it is of specific importance to both medical and non-medical military CIMIC officers to take into account the humanitarian principles—humanity, neutrality, impartiality, and operational independence—that guide these organizations, because they provide the fundamental principles for their members' cultural and social mindsets (71, 72). From a UN perspective, the framework for CIMIC-relationships between the military and civilian humanitarian organizations is determined by two key considerations: is the situation (1) a natural, technological, or environmental emergency in times of peace assuming a stable government and the state providing for security, or (2) is the emergency situation complex, i.e., military and other armed actors are or are perceived as party to the conflict and thus humanitarian actors would avoid any association with military actors and minimize their interaction (72). In peacetime, humanitarian actors would seek a cooperative approach to civil-military interaction, whereas in complex emergency situation with direct involvement of the military in the conflict, they would rather choose a co-existent, i.e., a more distant and indirect, less visible relationship with military actors in disaster relief (72). Therefore, in humanitarian actions or disaster relief situations, the United Nations distinguish three types of military assistance with decreasing visibility to the public: (1) direct assistance, (2) indirect assistance, or (3) infrastructure support. This graduated visibility concept is illustrated in Table 4 which provides an overview about these three concepts and further details and examples. As COVID-19 crisis management occurred in general in a peace time setting, direct civilian-military information exchange and even direct military assistance to the population—within the constitutional framework under civilian leadership—would not pose any issue to civilian organizations including NGOs or other humanitarian actors. In any case, a close dialogue between military and civilian or humanitarian actors is considered essential and key elements of humanitarian civil-military interaction includes information sharing, task division and joint planning as well as practical partnership and operative engagement (71, 74).
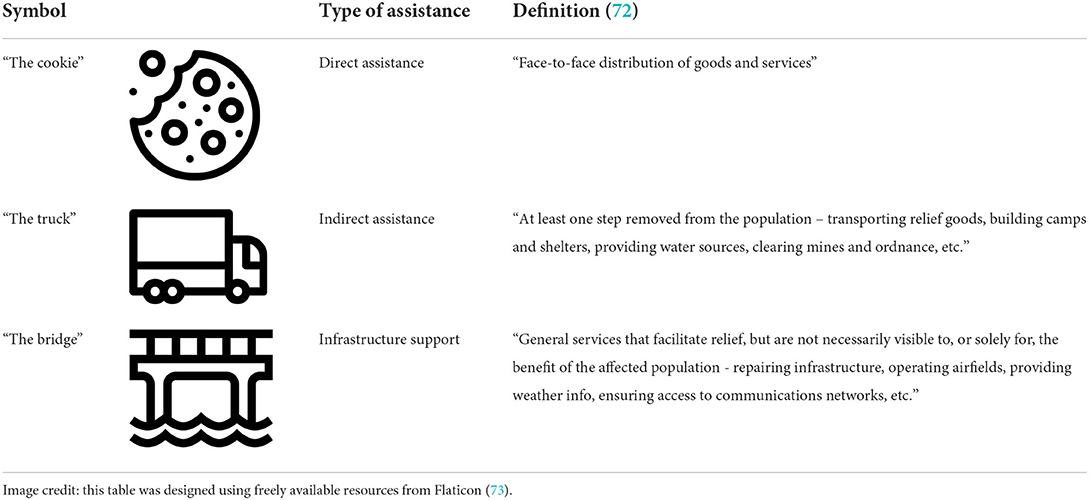
Table 4. Types of military assistance in humanitarian or disaster situations according to the United Nations Civil-Military-Coordination Field Handbook (72).
This work has several limitations that have to be taken into account for the appropriate interpretation of this scoping review. In order to avoid selection bias, a systematic and transparent literature search, screening and inclusion was conducted. This work probably under-reports the full extent of civil-military cooperation during the COVID-19 pandemic, because it is very likely that not all CIMIC experiences in the field were published in the literature. The inclusion of other databases or even gray literature may have resulted in further nuances. The qualitative analysis within the present work was—as in any qualitative study—subjected to the characteristics and reflexivity of the researcher, therefore, subjectivity bias cannot be excluded. Nevertheless, this report covers information from established, robust and credible medical and scientific databases which might contribute to the specificity of this scoping review. We consider this scoping review informative, because common global themes of the pandemic were identified, and we consider these data generalizable within the context of the above-described, important limitations.
Data in this scoping review suggest, in general, that civil-military cooperation substantially contributed to societal resilience in crisis management on a global scale in a broad spectrum of core abilities during the COVID-19 pandemic—presumably at a high cost. If the health care system in a particular country is overstretched before a crisis occurs, the mitigation potential be limited whoever the health agent would be. Therefore, from a holistic perspective, decisive measures to prevent the next pandemic should receive considerable attention in the future (75). Future work could analyze medico-scientific contributions, field experiences, and role model aspects in more detail. The awareness of military's potential of threat and intimidation is crucial in order to prevent abuse. As success of disaster management in COVID-19 had a very strong local, tactical component, a thorough analysis of lessons learned from a micro-level CIMIC perspective may be informative to further strengthen cities and communities.
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
MR conceived and designed this work, analyzed the data, wrote, and revised the manuscript and approved the submission. This work is part of MR's thesis project for a Master of Arts in Civil-Military Interaction at the Helmut Schmidt University/University of the Federal Armed Forces Hamburg, Germany.
I acknowledge financial support by Deutsche Forschungsgemeinschaft within the funding program Open Access Publikationskosten as well as by Heidelberg University.
I am indebted to Lorna Stimson, for language editing, and Sophie Ries, for proofreading the manuscript.
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The views and opinions expressed in this publication are those of the author and do not necessarily reflect those of the affiliated institutions.
1. World Health Organization. Timeline: WHO's COVID-19 Response. Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline (accessed June 9, 2022).
2. Johns Hopkins University. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Johns Hopkins Coronavirus Resource Center. Available online at: https://coronavirus.jhu.edu/map.html (accessed June 9, 2022).
3. Schulze C, Welker A, Kühn A, Schwertz R, Otto B, Moraldo L, et al. Public Health Leadership in a VUCA World Environment: lessons learned during the regional emergency rollout of SARS-CoV-2 vaccinations in Heidelberg, Germany, during the COVID-19 pandemic. Vaccines. (2021) 9:887. doi: 10.3390/vaccines9080887
4. Ries M. The COVID-19 infodemic: mechanism, impact, and counter-measures—A review of reviews. Sustainability. (2022) 14:2605. doi: 10.3390/su14052605
5. Ries M, Mechler K, Smith DL, Herfort B, Visintini J, Santana AV, et al. Intuitive global insight into COVID-19 clinical research activities-The “COVID-19 Map of Hope.” J Clin Pharmacol. (2020) 60:826–7. doi: 10.1002/jcph.1643
6. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616
7. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/M18-0850
8. O'Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. (2014) 89:1245–51. doi: 10.1097/ACM.0000000000000388
9. National Center for Biotechnology Information. PubMed. PubMed. (2022). Available online at: https://pubmed.ncbi.nlm.nih.gov/ (accessed January 26, 2022).
10. Clarivate. Advanced Search - Web of Science Core Collection. (2022). Available online at: https://www.webofscience.com/wos/woscc/advanced-search (accessed January 26, 2022).
11. Cochrane. Advanced Search | Cochrane Library. (2022). Available online at: https://www.cochranelibrary.com/advanced-search (accessed January 26, 2022).
12. Zotero. Zotero | Your personal research assistant. (2022). Available online at: https://www.zotero.org/ (accessed January 26, 2022).
13. Creswell JW. “Narrative Research”. Qualitative Inquiry & Research Design: Choosing Among Five Approaches. Washington, DC, USA: Sage (2012). p. 70–76.
14. Creswell JW. Phenomenological Research. Qualitative Inquiry & Research Design: Choosing Among Five Approaches. Washington, DC: Sage (2012). p. 76–83.
15. R Project. Welcome to RQDA Project. (2022). Available online at: http://rqda.r-forge.r-project.org/ (accessed March 4, 2022).
16. R Project. R: The R Project for Statistical Computing. (2022). Available online at: https://www.r-project.org/ (accessed March 4, 2022).
17. Linux Mint. Home - Linux Mint. (2022). Available online at: https://linuxmint.com/ (accessed March 4, 2022).
18. United States Geological Survey. Planetary Names: Abbreviations for Continents, Countries, Ethnic Groups. (2022). Available online at: https://planetarynames.wr.usgs.gov/Abbreviations (accessed February 13, 2022).
19. QGIS.org. QGIS Geographic Information System. QGIS Association. Available online at: https://www.qgis.org/en/site/ (accessed June 18, 2022).
20. Natural Earth - Free vector and raster map data at 1:10m 1:50m and 1:110m scales. Available online at: https://www.naturalearthdata.com/ (accessed June 18, 2022).
21. MindMaster, a Versatile Mind Mapping Tool. Edrawsoft. Available online at: https://www.edrawsoft.com/mindmaster/ (accessed June 16, 2022).
22. Scott BK, Miller GT, Fonda SJ, Yeaw RE, Gaudaen JC, Pavliscsak HH, et al. Advanced digital health technologies for COVID-19 and future emergencies. Telemed J E Health. (2020) 26:1226–33. doi: 10.1089/tmj.2020.0140
23. Pavlov I, He H, McNicholas B, Perez Y, Tavernier E, Trump M, et al. Awake prone positioning in non-intubated patients with acute hypoxemic respiratory failure due to COVID-19. Respir Care. (2022) 67:102–14. doi: 10.4187/respcare.09191
24. Holcomb JB, Spinella PC, Apelseth TO, Butler FK, Cannon JW, Cap AP, et al. Civilian walking blood bank emergency preparedness plan. Transfusion. (2021) 61:S313–25. doi: 10.1111/trf.16458
25. Dacunto P, Moser D, Ng A, Benson M. Classroom aerosol dispersion: desk spacing and divider impacts. Int J Environ Sci Technol. (2022) 19:1057–70. doi: 10.1007/s13762-021-03564-z
26. Turc J, Dupré H-L, Beaussac M, Murris S, Koch L, Paris R, et al. Collective aeromedical transport of COVID-19 critically ill patients in Europe: a retrospective study. Anaesth Crit Care Pain Med. (2021) 40:100786. doi: 10.1016/j.accpm.2020.11.004
27. Sasidharan S, Dhillon H. Ebola, COVID-19 and Africa: what we expected and what we got. Dev World Bioethics. (2021) 21:51–4. doi: 10.1111/dewb.12292
28. Herpe G, Lederlin M, Naudin M, Ohana M, Chaumoitre K, Gregory J, et al. Efficacy of chest CT for COVID-19 pneumonia diagnosis in France. Radiology. (2021) 298:E81–7. doi: 10.1148/radiol.2020202568
29. Roger C, Collange O, Mezzarobba M, Abou-Arab O, Teule L, Garnier M, et al. French multicentre observational study on SARS-CoV-2 infections intensive care initial management: the FRENCH CORONA study. Anaesth Crit Care Pain Med. (2021) 40:100931. doi: 10.1016/j.accpm.2021.100931
30. Quinn JM, Wilson JM, McNamara T, Goebbels S, Hansen J-C, Opitz A. Global Health Security Alliance (GloHSA). Disaster Med Public Health Prep. (2020) 14:691–3. doi: 10.1017/dmp.2019.118
31. Nogueira RG, Qureshi MM, Abdalkader M, Martins SO, Yamagami H, Qiu Z, et al. Global impact of COVID-19 on Stroke Care and IV Thrombolysis. Neurology. (2021) 96:e2824–38. doi: 10.1212/WNL.0000000000011885
32. Laura P, José A, Nikki A, Khaled A, Barret JP, Jeffery C, et al. Impact of COVID-19 on global burn care. Burns. (2021) S0305-4179(21)00312-0. doi: 10.1016/j.burns.2021.11.010
33. Khorram-Manesh A, Dulebenets M, Goniewicz K. Implementing public health strategies-The need for educational initiatives: a systematic review. Int J Environ Res Public Health. (2021) 18:5888. doi: 10.3390/ijerph18115888
34. Escalera-Antezana JP, Mariaca-Cerball CA, Alvarado-Arnez LE, Balderrama-Saavedra MA, Bonilla-Aldana DK, Rodriguez-Morales AJ. Incidence of SARS-CoV-2/COVID-19 in military personnel of Bolivia. BMJ Mil Health. (2021) 167:215–6. doi: 10.1136/bmjmilitary-2020-001705
35. Amit M, Kimhi H, Bader T, Chen J, Glassberg E, Benov A. Mass-surveillance technologies to fight coronavirus spread: the case of Israel. Nat Med. (2020) 26:1167–9. doi: 10.1038/s41591-020-0927-z
36. Moscicka A, Araszkiewicz A, Wabinski J, Kuzma M, Kiliszek D. Modeling of various spatial patterns of SARS-CoV-2: the case of Germany. J Clin Med. (2021) 10:1409. doi: 10.3390/jcm10071409
37. Atkinson MK, Cagliuso NV, Hick JL, Singer SJ, Bambury EA, Hayirli TC, et al. Moving forward from COVID-19: organizational dimensions of effective hospital emergency management. Health Secur. (2021) 19:508–20. doi: 10.1089/hs.2021.0115
38. Castro B, de Melo Y, dos Santos N, Barcellos A, Choren R, Salles R. Multi-agent simulation model for the evaluation of COVID-19 transmission. Comput Biol Med. (2021) 136:104645. doi: 10.1016/j.compbiomed.2021.104645
39. Danguy des Déserts M, Mathais Q, Morvan JB, Rager G, Escarment J, Pasquier P. Outcomes of COVID-19-Related ARDS patients hospitalized in a military field intensive care unit. Mil Med. (2021) usab268. doi: 10.1093/milmed/usab268
40. Bricknell M, Horne S. Personal view: security sector health systems and global health. BMJ Mil Health. (2020) bmjmilitary-2020-001607. doi: 10.1136/bmjmilitary-2020-001607
41. Suh Y, Hong H, Ohana M, Bompard F, Revel M, Valle C, et al. Pulmonary embolism and deep vein thrombosis in COVID-19: a systematic review and meta-analysis. Radiology. (2021) 298:E70–80. doi: 10.1148/radiol.2020203557
42. Crameri G, Bielecki M, Zust R, Buehrer T, Stanga Z, Deuel J. Reduced maximal aerobic capacity after COVID-19 in young adult recruits, Switzerland, May 2020. Eurosurveillance. (2020) 25:2001542. doi: 10.2807/1560-7917.ES.2020.25.36.2001542
43. Bielecki M, Zust R, Siegrist D, Meyerhofer D, Crameri G, Stanga Z, et al. Social distancing alters the clinical course of COVID-19 in young adults: a comparative cohort study. Clin Infect Dis. (2021) 72:598–603. doi: 10.1093/cid/ciaa889
44. Wang X, Li H, Wang P, Gong X, Li G, Jiang Z, et al. The difficulties, opportunities and challenges of COVID-19 by Chinese medicine on China. Indian J Pharm Sci. (2021) 83:13–20. doi: 10.36468/pharmaceutical-sciences.745
45. Wu F, He P, Chang X, Jiao W, Liu L, Si Y, et al. Visible-Light-Driven and Self-Hydrogen-Donated nanofibers enable rapid-deployable antimicrobial bioprotection. Small. (2021) 17:e2100139. doi: 10.1002/smll.202100139
46. Gad M, Kazibwe J, Quirk E, Gheorghe A, Homan Z, Bricknell M. Civil-military cooperation in the early response to the COVID-19 pandemic in six European countries. BMJ Mil Health. (2021) 167:234–43. doi: 10.1136/bmjmilitary-2020-001721
47. Gibson-Fall F. Military responses to COVID-19, emerging trends in global civil-military engagements. Rev Int Stud. (2021) 47:155–70. doi: 10.1017/S0260210521000048
48. Connolly J, Pyper R. Developing capacity within the British civil service: the case of the Stabilisation Unit. Public Money Manag. (2020) 40:597–606. doi: 10.1080/09540962.2020.1750797
49. James RH, Doyle CP, Cooper DJ. Descriptive record of the activity of military critical care transfer teams deployed to London in April 2020 to undertake transfer of patients with COVID-19. BMJ Mil Health. (2020) bmjmilitary-2020-001619. doi: 10.1136/bmjmilitary-2020-001619
50. Roßmann K, Wegner H, Stark H, Grossmann G, Jansen A, Frangoulidis D. COVID-19 pandemic & bureaucracy: the crisis inside the crisis. Front Public Health. (2021) 9:665323. doi: 10.3389/fpubh.2021.665323
51. Barreau F. [Operation Resilience, care at the crossroads of skills in civil-military cooperation]. Rev Infirm. (2021) 70:42–5. doi: 10.1016/j.revinf.2020.12.017
52. Kalkman J. Military crisis responses to COVID-19. J Contingencies Crisis Manag. (2021) 29:99–103. doi: 10.1111/1468-5973.12328
53. Tušer I, Jánský J, Petráš A. Assessment of military preparedness for naturogenic threat: the COVID-19 pandemic in the Czech Republic. Heliyon. (2021) 7:e06817. doi: 10.1016/j.heliyon.2021.e06817
54. Lopez-Garcia G. Discipline and punish: the role of the military, police and civil guards in communicating the COVID-19 crisis in Spain. Prof Inf. (2020) 29:1–15. doi: 10.3145/epi.2020.may.11
55. Bacchus P, Nissen K, Berg J, Bråve A, Gyll J, Larsson C, et al. Civil-military collaboration to facilitate rapid deployment of a mobile laboratory in early response to COVID-19: a high-readiness exercise. Health Secur. (2021) 19:488–97. doi: 10.1089/hs.2021.0011
56. Widmer N, Abbet C, Brunner J, Barros J, Ullmann S, Beeler C, et al. Swiss Armed Forces deployment during the COVID-19 pandemic: militia pharmacy officers' roles and duties. BMJ Mil Health. (2021) 167:141. doi: 10.1136/bmjmilitary-2020-001605
57. Dutta EH, Barker M, Gherman R. Together: navy reserve's response to COVID-19 pandemic. Am J Perinatol. (2021) 38:307–9. doi: 10.1055/s-0040-1721710
58. McGee LJ, Michael CT. Prevent, detect, and treat: the military's flexible approach for a whole-of-nation pandemic response. Front Health Serv Manage. (2020) 37:27–32. doi: 10.1097/HAP.0000000000000095
59. Dragnic M. Crisis of wellbeing and popular uprising: the logic of care as a path to social emancipation in Chile. J Lat Am Cult Stud. (2020) 29:311–23. doi: 10.1080/13569325.2020.1822791
60. Fealy G. Jokowi in the COVID-19 era: repressive pluralism, dynasticism and the overbearing state. Bull Indones Econ Stud. (2020) 56:301–23. doi: 10.1080/00074918.2020.1846482
61. Al-Marashi I. Demobilization minus disarmament and reintegration: Iraq's security sector from the US invasion to the COVID-19 pandemic. J Intervent Statebuilding. (2021) 15:441–58. doi: 10.1080/17502977.2021.1934284
62. Jabbar R, Makki M. Managing health disasters and Civil-Military Cooperation: a case of COVID-19 in Pakistan. Jamba. (2021) 13:1113. doi: 10.4102/jamba.v13i1.1113
63. PreventionWeb. Sendai Framework for Disaster Risk Reduction. Available online at: https://www.preventionweb.net/sendai-framework/sendai-framework-for-disaster-risk-reduction (accessed February 23, 2022).
64. Michael N. SARS-CoV-2 in the US Military - Lessons for civil society. N Engl J Med. (2020) 383:2472–3. doi: 10.1056/NEJMe2032179
65. Katz JN, Sinha SS, Alviar CL, Dudzinski DM, Gage A, Brusca SB, et al. COVID-19 and disruptive modifications to cardiac critical care delivery: JACC review topic of the week. J Am Coll Cardiol. (2020) 76:72–84. doi: 10.1016/j.jacc.2020.04.029
66. Smith K, Bhavsar M. A new era of health leadership. Healthc Manage Forum. (2021) 34:332–5. doi: 10.1177/08404704211040817
67. Passos AM, Acácio I. The militarization of responses to COVID-19 in Democratic Latin America. Rev Adm Pública. (2021) 55:261–72. doi: 10.1590/0034-761220200475
68. Ries M, Zielonka M, Ries N, Breil T, Garbade S, Mechler K. Disasters in Germany and France: an analysis of the emergency events database from a pediatric perspective. Disaster Med Public Health Prep. (2019) 13:958–65. doi: 10.1017/dmp.2019.24
69. Brennenstuhl H, Will M, Ries E, Mechler K, Garbade S, Ries M. Patterns of extreme temperature-related catastrophic events in Europe including the Russian Federation: a cross-sectional analysis of the Emergency Events Database. BMJ Open. (2021) 11:e046359. doi: 10.1136/bmjopen-2020-046359
70. UN OCHA Services. What is the Cluster Approach? | HumanitarianResponse. (2020). Available online at: https://www.humanitarianresponse.info/en/about-clusters/what-is-the-cluster-approach (accessed February 7, 2022).
71. United Nations Office for the Coordination of Humanitarian Affairs (OCHA). Guide for the Military 2.0. (2017). Available online at: https://www.unocha.org/sites/unocha/files/Guide%20for%20the%20Military%20v2.pdf (accessed February 7, 2022).
72. United Nations Office for the Coordination of Humanitarian Affairs (OCHA). UNCMCoord Field Handbook 2.0 (2018). Available online at: https://www.unocha.org/sites/unocha/files/%5BE-Version%5D%20UNCMCoord%20Field%20Handbook%202.0%20%282018%29.pdf (accessed February 6, 2022).
73. Flaticon. Free Icons and Stickers - Millions of resources to download. Flaticon. (2022). Available online at: https://www.flaticon.com/ (accessed February 5, 2022).
74. Khorram-Manesh A, Mortelmans LJ, Robinson Y, Burkle FM, Goniewicz K. Civilian-Military Collaboration before and during COVID-19 Pandemic—A systematic review and a pilot survey among practitioners. Sustainability. (2022) 14:624. doi: 10.3390/su14020624
75. U. N. Environment. Preventing the next pandemic - Zoonotic diseases and how to break the chain of transmission. UNEP - UN Environment Programme. (2020) http://www.unep.org/resources/report/preventing-future-zoonotic-disease-outbreaks-protecting-environment-animals-and (accessed June 13, 2022).
Keywords: COVID-19, pandemic, SARS-CoV-2, resilience, civil-military cooperation (CIMIC), disaster response, disaster management, disaster and emergency medicine
Citation: Ries M (2022) Global key concepts of civil-military cooperation for disaster management in the COVID-19 pandemic—A qualitative phenomenological scoping review. Front. Public Health 10:975667. doi: 10.3389/fpubh.2022.975667
Received: 22 June 2022; Accepted: 15 August 2022;
Published: 15 September 2022.
Edited by:
Paulo Cesar Peiter, Oswaldo Cruz Foundation (Fiocruz), BrazilReviewed by:
Henrique Lopes, Portuguese Catholic University, PortugalCopyright © 2022 Ries. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Markus Ries, markus.ries@uni-heidelberg.de
†ORCID: Markus Ries orcid.org/0000-0002-5054-5741
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.