- 1Department of Brain and Behavioral Sciences, University of Pavia, Pavia, Italy
- 2Developmental Psychobiology Lab, IRCCS Mondino Foundation, Pavia, Italy
- 3Division of Neonatology and Pediatrics, Ospedale Versilia, Viareggio, Italy
- 4AUSL Toscana Nord Ovest, Pisa, Italy
Background: High levels of mental health problems have been consistently reported among neonatal healthcare professionals. While studies suggest that personality, coping strategies and safety culture might contribute to the psychological wellbeing of healthcare professionals, they have not been systematically investigated in low-risk (i.e., neonatal wards; NWs) and high-risk (i.e., neonatal intensive care units; NICUs) neonatal contexts. The current study investigated potential predictors of professionals' emotional distress and whether they differ according to the work setting (i.e., NICUs vs. NWs).
Methods: Healthcare professionals (N = 314) from 7 level-3 (i.e., NICUs) and 6 level-2 (i.e., NWs) neonatal units in Tuscany were included. Emotional distress (i.e., anxiety, depression, psychosomatic, post-traumatic stress symptoms and emotional exhaustion), Behavioral Inhibition System (BIS) and Behavioral Approach System (BAS) sensitivity, coping strategies and safety culture were assessed through well-validated, self-reported questionnaires.
Results: Greater BIS/BAS sensitivity, avoidance coping strategies and a sub-dimension of safety culture (i.e., stress recognition) were significantly associated with greater risk of emotional distress, whereas job satisfaction emerged as a protective factor. Three specific profiles of professionals in term of personality, coping and safety culture were identified and further predicted emotional distress. Neonatal wards and NICUs personnel presented different associations between personality, coping and safety culture.
Conclusion: These findings highlighted significant modifiable contributors of neonatal mental healthcare professionals' wellbeing. Institutional initiatives that target these factors and, particularly, job satisfaction may promote professionals' emotional wellbeing and thus improve caring processes.
Introduction
The healthcare environment is inherently complex, demanding, and stressful. Stress experienced by healthcare professionals, especially by physicians and nurses, results from their responsibility for health and wellbeing of other people, patients' behavior and complaints, coping with death and injury (1, 2). Among healthcare professionals, those who work in neonatal contexts and, particularly, in neonatal intensive care units (NICUs), are exposed to an additional amount of stress related to caring for the youngest and for their parents in very at-risk situations and to exposure to potentially traumatic events (3). Furthermore, the ever-mounting business competition, together with the recent health emergency, have led to an enormous increase in the amount of workload, job pressure and stress on professionals working in these settings (4–6). Thus, serious concerns have been raised for the psychological wellbeing of this occupational group which might have a cascade impact on the quality of services provided (7).
Estimates showed that a significant proportion of neonatal and pediatric healthcare professionals reports high levels of anxiety, depression, psychosomatic symptoms, post-traumatic stress symptoms, and emotional exhaustion (8–10). Professionals working in the NICUs have been reported to be at higher risk of developing emotional distress as compared to their colleagues working in lower-risk settings such as neonatal wards (NWs) (11, 12). Emotional distress is defined in literature as a “multi-factor, general mood disorder defined as subjective feelings that vary in intensity from sadness, uncertainty, confusion and worry to more significant symptoms such as anxiety, the expression of anger, social isolation and hopelessness” (13). The recent sanitary crisis due to the COVID-19 pandemic has further raised the rate of mental health problems among healthcare workers reaching epidemic levels (14), even in neonatal care settings (15–17).
Notably, not all individuals develop mental health problems in response to stress conditions. The way individuals experience, approach, appraise, and manage stress can make a difference. This means that personality characteristics, coping strategies and perception of working safety have the potential to provide an explanation as to why some individuals thrive under stress conditions, while for other the same stressful experience may disrupt their physical and mental health wellbeing. The current study investigated how personality, coping and safety culture associate with emotional distress in healthcare professionals from NWs and NICUs settings.
The Reinforcement Sensitivity Theory [RST, (18, 19)] is a biologically-based theory of personality that might offer one of the most accurate descriptions of the link between personality and psychopathology (20, 21). According to this theory, individuals differ in their reinforcement sensitivity which reflects the activity of two basic brain sub-systems, the Behavioral Inhibition System (BIS) and the Behavioral Approach System (BAS). The BIS is associated with response to threat by motivating withdrawal behavior, whereas the BAS is associated with reward-seeking behavior by motivating approach behavior. Extreme under- or over-sensitivity of these systems is proposed to predict psychopathology (19), with high BIS sensitivity being considered a risk factor for internalizing symptoms, whereas elevated BAS activity being hypothesized to increase vulnerability to externalizing problems in the general population (20).
Coping strategies refer to the behavioral and cognitive efforts put in place to manage stressful situations (22) and are important factors that might modulate individuals' responses to stress in the workplace. A study reported that the most common coping strategies used by healthcare workers included acceptance of the critical situation and use of a positive outlook while working (23, 24). Importantly, distinct coping strategies have been found to, respectively, increase or reduce the risk of emotional distress in healthcare workers (25, 26). Specifically, a positive attitude, problem solving and seeking social support are regarded as adaptive coping styles (27) and they have been associated with reduced emotional distress (28), stress symptoms (29), anxiety and depression (30). In contrast, avoidance strategies are considered negative coping styles, being associated with an increase of psychological distress (31), emotional exhaustion (32), post-traumatic stress symptoms and fatigue (33).
Safety culture, as the professionals' attitudes and behavior about the organization's current health and safety performance (34), is strongly related with healthcare workers' wellbeing (35). Mounting evidence indicates that healthcare environments in which professionals have autonomy, control over the environment and good relationships within the team result in lower levels of burnout (36). This is even more critical in high-risks settings such as the NICUs. Safety culture within the NICUs has been shown to vary widely (37) and one study indicates that it might negatively associate with NICUs nurses' burnout (8).
While studies suggest that personality, coping strategies and safety culture might predict the occurrence of burnout syndrome in health professionals (28, 35, 38), they have not been systematically investigated in relation to professionals emotional distress, encompassing a broader range of mental health outcomes, and within neonatal contexts. A better understanding of factors that contribute to neonatal healthcare professionals' emotional wellbeing will enable to develop prevention strategy and has important implications for the quality of care provided to the youngest. Based on these premises, the aim of the current study was twofold: (1) to examine the associations between personality factors, coping strategies and safety culture and professionals' emotional distress and exploratorily identify specific profiles of professionals (2) to investigate whether the contributors to professionals' emotional distress differ according to the work setting (i.e., NICUs vs. NWs). We hypothesized lower BIS/BAS scores, adaptive coping strategies and a stronger safety culture to be negatively associated with workers' emotional distress. Due to the lack of available evidence, aims 2 was exploratory and we made no a priori predictions.
Methods
Participants and procedures
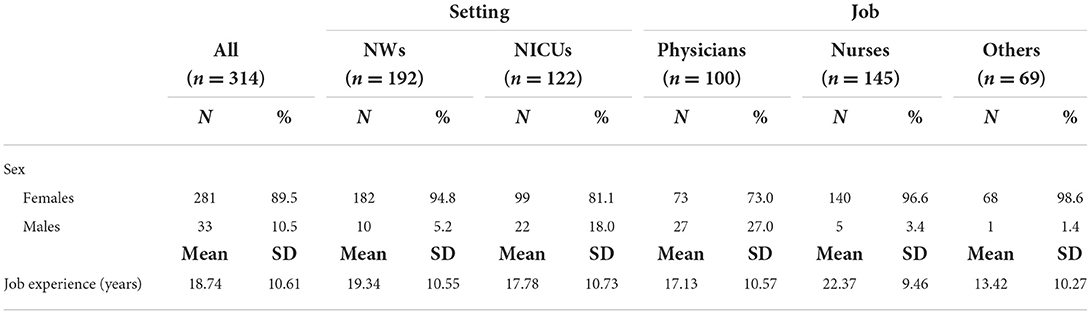
Healthcare professionals (N = 314) were recruited as part of the SPACE-NET project (16), a multicentre cross-sectional survey whereby questionnaires were distributed to doctors and nurses across 7 level-3 neonatal units (i.e., NICUs that provide intensive care to newborns <32 weeks of gestation or <1,500 g birth weight, NICUs) in Tuscany, and all 6 level-2 neonatal units (i.e., NWs that provide care to infants ≥32 weeks or >1,500 g) of AUSL Toscana Nord Ovest. The majority were females (n = 281, 89.5%) and working as nurses (n = 145, 46.2%) or physicians (n = 100, 31.8%). One hundred ninety-two participants were working in NWs (61.1%) whereas the remaining (N = 122, 38.5%) were working in NICUs. Healthcare professionals were contacted by email. Those who agreed to participate in the study provided an informed consent and anonymously filled in a set of on-line questionnaires to assess their mental health during the COVID-19 emergency, personality factors, coping strategies and safety culture. Filling in the online survey took approximately 30 min. The study has been approved by the Ethics Committee of the participant parties.
Measures
Emotional distress
Several domains of professionals' mental health were investigated. Depressive symptoms were assessed through the 21-items Beck Depression Inventory – II (BDI-II) (39), a widely employed scale that evaluates subclinical and clinical depressive symptomatology. Each item is rated on a 4-point Likert scale; a global sum score is computed with higher scores indicating higher depressive symptoms. Anxiety symptoms were measured using the 20-items State anxiety subscale of the State-Trait Anxiety Inventory – Y form (STAI-Y) (40). Each item is rated on a 4-point Likert scale and sum up in a global score, with higher scores indicating greater levels of current anxiety symptoms. Psychosomatic symptoms were assessed through the 17-items Psychosomatic Symptom Checklist (41) on a 6-point Likert scale. A mean score was obtained with higher scores indicating greater psychosomatic symptoms. Emotional Exhaustion was measured through a 9-items subscale of the Maslach Burnout Inventory (MBI) (42). Each item is rated on a 7-point Likert scale and sum up in a global score with higher ratings indicating greater emotional exhaustion. Lastly, post-traumatic stress symptoms were assessed using the 22-items Impact of Event Scale (IES) (43). Each item is rated on a 5-point Likert scale and a global sum score is obtained with higher scores indicating greater risk for post-traumatic stress symptoms.
As all mental health domains were moderately to strongly correlated (rs range = 0.27–0.71), to limit the number of statistical comparisons, we employed a principal component analysis (PCA) to estimate a global index of emotional distress (EDI) that would explain the largest portion of variance in mental health outcomes (i.e., depressive symptoms, anxious symptoms, psychosomatic symptoms, post-traumatic symptoms, and emotional exhaustion), as done in prior work (16). For this analysis we set the minimum Eigenvalue to 1 and we adopted a non-rotated solution. The principal component with the highest loading and explaining the highest portion of variance was employed as the primary outcome variable in subsequent analyses. The Principal Component Analysis yielded a one-component solution (i.e., emotional distress index, EDI), explaining the 65.3% of total variance and with loadings ranging from 0.67 to 0.90.
BIS and BAS sensitivity
Individual differences in BIS and BAS sensitivity were assessed using the widely employed 20-items Behavioral Inhibition/Activation Scale (BIS/BAS) (44). This include seven items that assess BIS sensitivity (e.g., “I worry about making mistakes” or “I feel pretty worried or upset when I think or know somebody is angry at me”) and 13 that assess BAS sensitivity (e.g., “I'm always willing to try something new if I think it will be fun”) on a 4-point Likert scale. Higher scores reflect higher BIS or BAS sensitivity. The BIS scale is unidimensional, while the BAS items can be scored on three different BAS domains: Reward Responsiveness (BAS-R), that focuses on responses to the occurrence or anticipation of reward (e.g., “When good things happen to me, it affects me strongly”), Drive (BAS-D), concerned with the persistent pursuit of desired goals (e.g., “When I want something, I usually go all out to get it”), and Fun Seeking (BAS-F) which reflects a desire for new rewards (e.g., “I'm always willing to try something new if I think it will be fun”).
Coping style
Coping strategies were assessed using the Italian validation of the short version of the Coping Orientation to the Problems Experienced (COPE-NVI-25) (26). The COPE-NVI-25 consists of 25 items evaluating how often individuals use a particular coping strategy in stressful situations. Items are scored on a 4-point Likert scale with higher scores indicating a greater use of that strategy. Individual differences in the use of five substantially independent dimensions of coping are assessed: Social Support (e.g., “I try to get advice from someone about what to do”), Avoidance Strategies (e.g., “I admit to myself that I can't deal with it, and quit trying”), Positive Attitude (e.g., “I look for something good in what is happening”), Problem Solving (e.g., “I focus on dealing with this problem, and if necessary let other things slide a little”) and Trascendent Orientation (e.g., “I pray more than usual”). Good psychometric properties have been reported for this version of the questionnaire (26).
Safety culture
Professionals' perception of safety in their workplace was investigated through 22 items from the Safety Attitudes Questionnaire Short Form (SAQ) (45). Four of the six domains measured by the SAQ were used in the present study: Teamwork climate, measuring perceived quality of collaboration between personnel (e.g., “Our doctor and nurses work together as a well-coordinated team”), Job satisfaction, assessing positivity about the work experience (e.g., “I like my job”), Safety climate, that focuses on perceptions of a strong and proactive organizational commitment to safety (e.g., “I would feel perfectly safe being treated here”), and Stress recognition, that measures acknowledgment of how performance is influenced by stressors (e.g., “When my workload become excessive, my performance is impaired”). Items are scored on a 5-point Likert scale with higher scores reflecting more positive perceptions.
Statistical analyses
Variables were first examined for outliers and skewness. Positively skewed distributions were natural log transformed to approximate normal distributions. All variables found to be significantly associated with the EDI were included as covariates in subsequent analyses. Differences in mean levels of personality, coping and safety between professionals from NICUs or NWs were determined by Student's t tests. Forward stepwise multivariate regression analyses were performed to identify significant predictors of EDI. At each step, the predictor that had the highest correlation with the outcome variable were entered in the model, if it satisfied the default criterion (i.e., has a p < 0.05). The procedure stopped when there were no variables left that satisfied the entry criterion (i.e., when all remaining variables have a p > 0.05 if included in the model). Furthermore, we performed a two-step cluster analysis in order to exploratorily identify specific profiles of professionals in terms of personality, coping strategies and safety culture and their relationship with emotional distress. When the groups or clusters had been identified, a univariate ANOVA was performed to determine the existence of significant differences between the groups with respect to the EDI. To determine which means were significantly different, the Scheffé post-hoc comparison test was applied.
Lastly, regression models were performed separately for professionals from NWs and NICUs to assess the impact of working setting on these associations.
For all the statistical tests performed, a p-value threshold of 0.05 was set to determine statistical significance. Statistical analyses were conducted using IBM SPSS Statistics for Windows, ver. 25.
Results
Preliminary analyses
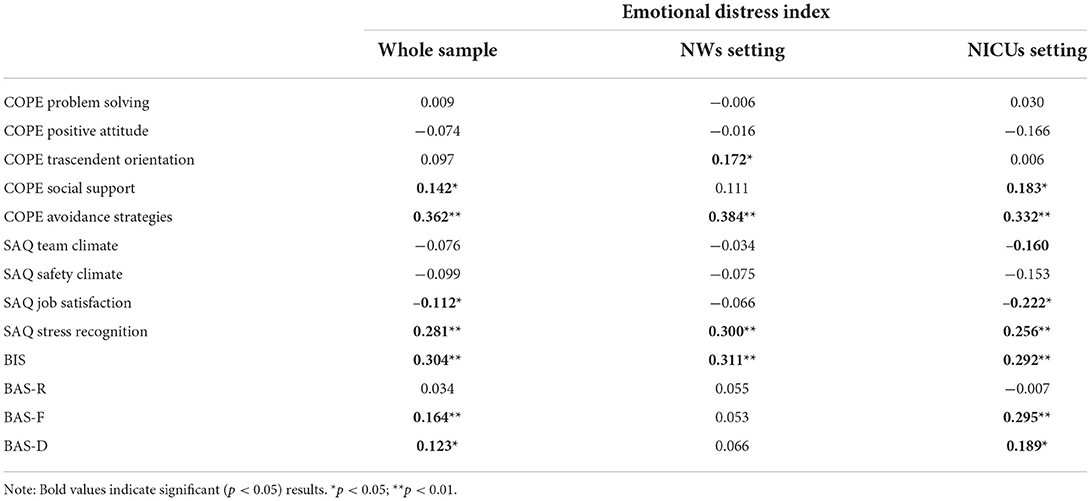
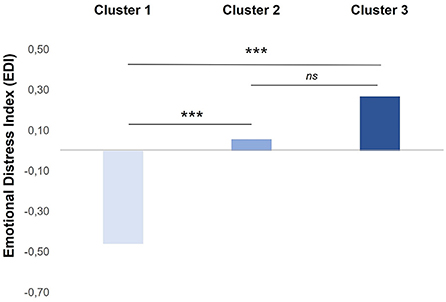
A total of 314 healthcare professionals participated in the study, out of 941 invited (32.9%). Socio-demographic variables (i.e., sex, job, and years of experiences; see Table 1) were not significantly associated with the EDI (all p > 0.05), nor there were statistically significant differences in EDI scores depending on work setting (i.e., NICUs vs. NWs). Spearman bivariate correlations between EDI scores and predictors of interest are reported in Table 2 for the whole sample, NWs and NICUs settings. Descriptive statistics and t-test results for personality, coping strategies, and safety culture in NWs and NICUs are reported in Table 3. Significant differences were reported only for SAQ job satisfaction, with professionals from the NICUs reporting higher levels of job satisfaction as compared to professionals from the NWs (p = 0.04).
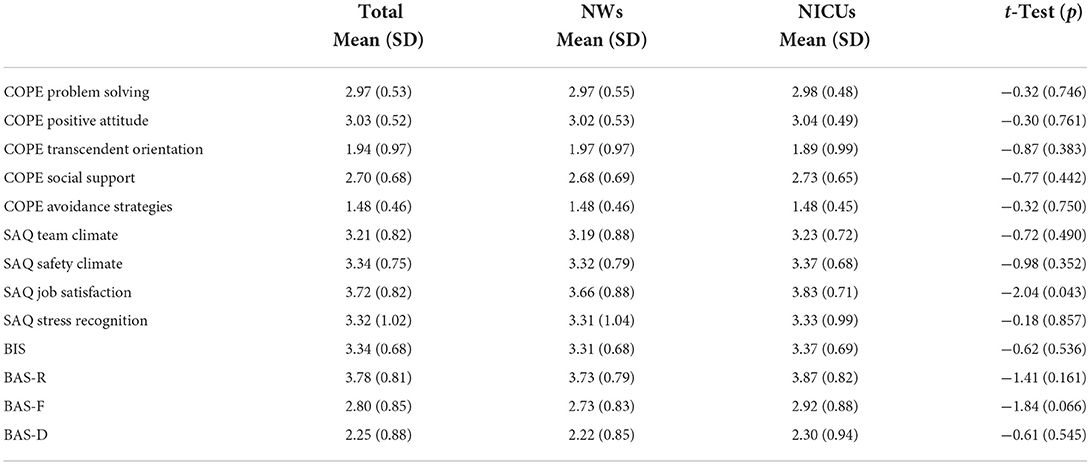
Table 3. Descriptive statistics (raw values) and t-test results comparing professionals from neonatal wards (NWs) and neonatal intensive care units (NICUs) on study variables.
Regression analyses
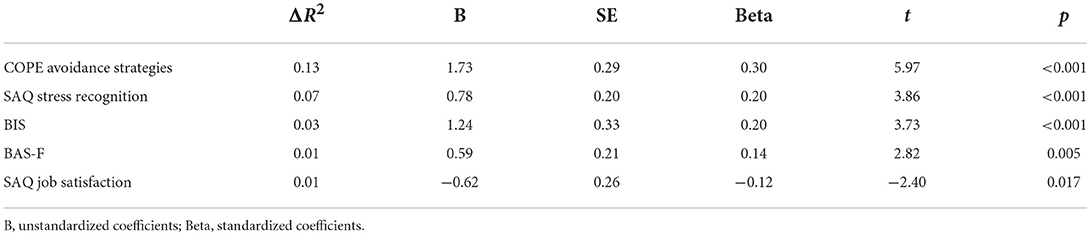
Results of the linear regression analyses used to test the association between personality, coping and safety culture with the EDI are summarized in Table 4. The final model accounted for a significant proportion of the variance in the EDI [R2 =0.25; F (5,308) = 21.865; p < 0.001]. Higher avoidance strategies, BIS sensitivity, BAS-F and SAQ stress recognition were all associated with higher EDI (Beta's range = 0.14–0.30, p < 0.005). SAQ job satisfaction was negatively associated with the EDI (Beta = −0.12, p = 0.017). All other predictors were excluded from the equation as not statistically significant.
Importantly, the association between personality, coping and safety culture and EDI differed depending on working setting. In NWs a model that includes COPE avoid, BIS and SAQ stress recognition explain a significant proportion of the variance in EDI [R2 = 0.26; F (3,188) = 22.96; p < 0.001], with higher scores on these scales being associated with greater emotional distress in health care professionals. Differently, in NICU professionals a significant proportion of the variance in EDI [R2 = 0.27; F (4,117) = 12.34; p < 0.001] was predicted by a four-predictor model that include COPE avoid, BIS, BAS-F and SAQ job satisfaction. COPE avoid, BIS, BAS-F were all positively related to the EDI (Beta's range = 0.23, 0.30, p < 0.005), whereas SAQ job satisfaction was negatively associated with this score (Beta = −0.24, p = 0.003).
Cluster analysis
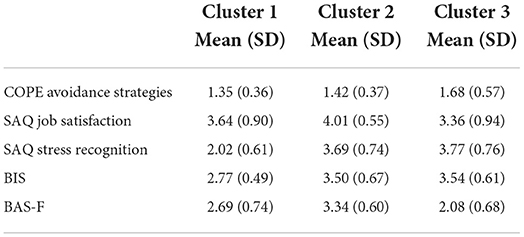
A two-step cluster analysis was performed including all the significant predictors of EDI emerged from the regression analysis in the whole sample. A three-group solution was found with the following distribution: 23.6% (n = 74) of the participants in Cluster 1, 45.9% (n = 144) in Cluster 2 and 30.6% (n = 96) in Cluster 3. As summarized in Table 5 and shown in Figure 1, the first group resulting from the cluster analysis (Cluster 1) was characterized by low scores on BIS, COPE avoidance strategies and SAQ-Stress recognition, moderate levels of BAS-F and SAQ job satisfaction. The second group (Cluster 2) identified professionals with high levels of BAS-F, BIS, SAQ stress recognition and SAQ Job satisfaction while low COPE avoidance strategies. The third group (Cluster 3) clusters professionals with high scores in COPE avoidance strategies, SAQ Stress Recognition and BIS, while low scores on BAS-F and SAQ job satisfaction.
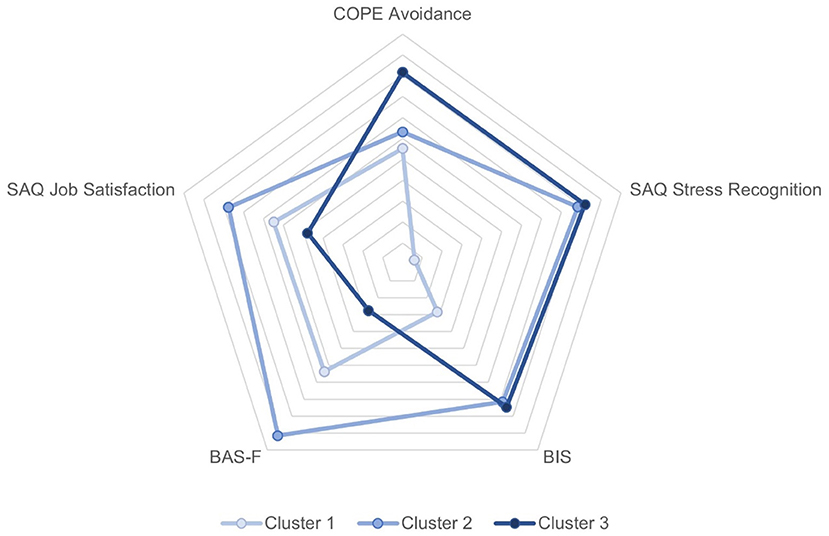
Figure 1. Radar plot of mean scores on personality, coping and safety culture by clusters. A greater distance from the center represents a more positive score on the scale.
After classification into groups based on the three-cluster solution, a univariate analysis of variance (ANOVA) was performed to investigate differences in the EDI scores between clusters. The results of the comparative analysis between clusters on the EDI (Figure 2) demonstrated statistically significant differences among clusters [F (2,311) = 12.36, p < 0.001]. Post-hoc Scheffè-adjusted comparisons showed that Cluster 1 had a significantly lower score on the EDI (M = −0.46, SD = 0.76) than Cluster 2 (M = 0.06, SD = 0.99) and Clusters 3 (M = 0.27, SD = 1.06).
Discussion
This study examined the relative contributions of personality, coping factors and safety culture on healthcare professionals' emotional distress in neonatal low-risk (i.e., NWs) and high-risk (i.e., NICUs) settings. BIS/BAS sensitivity, avoidance coping strategies, stress recognition and job satisfaction were all significant predictors of workers' mental health outcomes, including depression, anxiety, psychosomatic symptoms, post-traumatic stress symptoms and emotional exhaustion. Further, we showed that these associations varied according to the working settings (i.e., NICUs vs. NWs). Lastly, an exploratory cluster analyses revealed three specific profiles of professionals in term of personality, coping and safety culture, which further predicted individuals' emotional distress.
In line with our prediction, greater BIS sensitivity, BAS fun-seeking sensitivity, avoidance coping strategies and stress recognition were all associated with greater emotional distress in the whole sample. BIS and BAS dimensions have been previously associated with emotion regulation difficulties (20) and implicated in the development of psychopathology in the general population (46). The current study extends this evidence by showing, for the first time, that both high BIS and BAS fun-seeking are associated with emotional distress in healthcare professionals. Strong empirical support exists for an association between high BIS sensitivity and anxiety (21), depression (47), and post-traumatic stress symptoms (48). In contrast, the BAS dimension is less well-understood (49). High BAS sensitivity has been consistently associated with the externalizing dimension of psychopathology (50), whereas evidence concerning the link with internalizing symptoms is mixed (21, 51–53). The multi-faceted nature of the BAS construct may partly explain inconsistencies in the literature (49). While BAS Reward Responsiveness subscale has been found to uniquely predict lower behavioral problems and heightened psychological wellbeing (54), the BAS-Fun seeking subscale is thought to reflect a more maladaptive dimension of BAS encompassing impulsivity and lack of control (54, 55). The current findings support this hypothesis by showing that high BAS-Fun seeking predict greater emotional distress in healthcare professionals. Importantly, BAS-Fun Seeking, but not the other BAS subscales, has been positively associated with self-reported emotion regulation difficulties (56), dysfunctional impulsivity (49), experiential avoidance strategies (57) and substance use (58). We might hypothesize that seeking rewards or pleasurable experiences may lead, in the long term, to maladaptive consequences for individuals' mental health. However, this remains an open question for future studies adopting a longitudinal design.
As anticipated, avoidant coping strategies were related to greater emotional distress among healthcare professionals. This result is in line with previous literature on the link between avoidant coping and emotional distress (27, 59). Coping is a critical aspect of person-environment transactions that occurs when an individual appraises a situation as stressful (60). The current finding suggests that adopting strategies based on avoidance when faced with stressful situations represents a dysfunctional response and might increase the risk of psychological problems in neonatal healthcare professionals. As these working contexts, particularly within the NICUs, are inherently characterized by high levels of stress, improving professionals coping strategies should be a priority.
Safety attitudes were significantly associated with professionals' mental health problems in the current study. Specifically, greater stress recognition (i.e., acknowledgment of how performance is influenced by stressors) was related to an increase in emotional distress, whereas job satisfaction predicted lower distress. This is in line with a previous work showing an association between stress recognition and anxiety, depression, and burnout in healthcare professionals during the pandemic (35). Likewise, evidence suggests that job satisfaction plays a protective role against emotional disturbances in healthcare professionals (8, 35, 61). Although the direction of these associations is unclear, they highlighted that safety attitudes are important indicators of professional wellbeing. Importantly, safety attitudes are modifiable and sensitive to quality improvement interventions (62). Institutional initiatives that sustain safety culture and particularly job satisfaction may promote professionals' psychological wellbeing and thus improve caring processes.
Critically, the current study suggests differential associations between personality, coping and safety culture and professionals' emotional distress in low-risk (i.e., NWs) and high-risk (i.e., NICUs) working contexts. While avoidant coping strategies and BIS sensitivity were risk factors for professionals' psychological wellbeing in both settings, SAQ stress recognition predicted greater emotional distress in NWs only, whereas BAS sensitivity and job satisfaction were significant contributors of professional's mental outcomes in NICUs. It is important to emphasize that the current findings are exploratory and are based on a sample of healthcare workers with mild-to-moderate levels of emotional distress. Replication in larger and clinical samples of healthcare workers with full-blown emotional disorders is needed. It has been well-documented that hospital intensive care units are inherently stressful work environments (63). It can be hypothesized that the stress-related nature of the working context might interact with individuals' characteristics to determine mental health outcomes (64, 65). The current findings are in line with previous evidence which showed a protective role of job satisfaction, while no effects of stress recognition, on emotional distress in professionals working within NICUs (8, 37). Critically, the degree of emotional distress of care providers has been related to healthcare-associated infection rates (9, 66) and adverse events within the NICUs (67), with the neonates admitted to NICUs being more vulnerable to the negative impacts of medical errors and adverse events compared to other patients (68). Thus, enhancing professionals' job satisfaction might be an important intervention target, particularly within the NICUs, in order to mitigate the consequences and the likelihood of these events.
Furthermore, findings showed that high BIS and high BAS-Fun seeking are associated with an increased risk of emotional disturbances for workers within the NICUs, but not within NWs. NICUs providers are exposed to extreme life experiences and daily controversial ethical decision. We might speculate that when facing this kind of stressful experiences individuals that are high on both BIS and BAS may frequently find themselves in approach–avoidance conflicts due to the potential threats and rewards present which may, in turn, lead to high levels of distress. More robust research is needed to understand the mechanisms underlining the observed association as well as the interplay between stress at the workplace and individual personality traits to determine health outcomes.
Lastly, in an exploratory cluster analysis we identified three different profiles of professionals based on personality, coping and safety attitudes. The first one had low scores on all the dimensions analyzed, except for job satisfaction. The second profile referred to professionals that show few avoidant coping strategies but were high on all other dimensions. Finally, the third group consisted of providers with high levels of avoidance, BIS and stress recognition, while low levels of job satisfaction and BAS. Importantly, professionals from the first group reported lower levels of emotional distress than those from the other two groups. Albeit preliminary, these findings suggest that a combination of low levels of BIS/BAS, low avoidance, low stress recognition and high job satisfaction significantly contribute to professional's wellbeing. A psychologically healthy workforce may promote patient safety and quality of care.
Some limitations of the present study are noteworthy. First, results are based on a sample of self-selected professionals, which may bias our findings in an unpredictable direction. Second, we included only a number of NW and NICUs from Tuscany, thus limiting generalizability to different units or locations. Third, we relied on self-report for all measures, which may have artificially inflated observed associations due to shared method variance. Fourth, while the influence of a number of potential confounders (i.e., sex, job, years of experience) on the observed associations was statistically tested, we cannot rule out the effects of other potential psychological and working determinants of emotional distress (such as previous mental health problems, lifestyle variables, hours of overtime work, and/or work overload) which remains open questions for future investigations. Lastly, although it is tempting to interpret the observed associations as suggestive of causative pathways, the cross-sectional and observational design does not allow to establish any causal relationship (69).
Conclusion
Studies conducted in neonatal and pediatric care units have commonly reported high levels of mental health problems among the professional team (8, 15, 16, 70). This study identified a number of factors related to the personality, coping strategies and safety attitudes that contribute to the psychological wellbeing of professionals working in these contexts. The precise mechanisms of the observed associations require further exploration through prospective studies. However, the protective role of job satisfaction suggests that this might be an important intervention target. For example, the literature suggests that job satisfaction can be enhanced by implementing effective performance assessment processes, facilitating communications between professionals and patients, particularly in the case of adverse events, and improving professionals' sense of belonging and involvement (71, 72). In a clinical area where healthcare workers are satisfied with their job, they are likely to be less emotionally distressed and, thus, more likely to deliver safe and high-quality care and be mindful of their patients' needs.
Data availability statement
The raw data of this article can be retrieved in Zenodo using this link: 10.5281/zenodo.7079093.
Ethics statement
The studies involving human participants were reviewed and approved by Comitato Etico Regionale Sperimentazione Clinica della Regione Toscana. The patients/participants provided their written informed consent to participate in this study.
The members of the SPACE-NET group
Roberta Cacciavellani, Giulia Placidi, Marzia Gentile, Armando Cuttano, Angelina Vaccaro, Claudia Maggi, Beatrice Gambi, Letizia Magi, Laura Crespin, Graziano Memmini, Cinzia Ceccarelli, Marcello DeFilippo, Elena Verucci, Roberto Danieli, Liliana Malandra, Giovanni Gaeta, Laura Mele, Pierluigi Vasarri, Elena Sandini, Angelo Azzarà, Patrizio Fiorini, Carlo Dani, and Alessandra Cecchi.
Author contributions
LG and LP conceived the study. SG, SN, and LP made substantial contributions to the design of the work and drafted the manuscript. SC and IM organized and coordinated the acquisition of data for the work. SN performed the analysis and interpretation of the data and also prepared the first draft of the manuscript. All authors revised the manuscript critically for important intellectual content and approved the files for final submission.
Funding
This study was funded by Regione Toscana (Bando Ricerca Regione Toscana COVID 19, Decreto, Dirigenziale Regionale n. 7731 del 26 maggio 2020).
Acknowledgments
We are thankful to all the colleagues of the SPACE-NET project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Chen C, Meier ST. Burnout and depression in nurses: a systematic review and meta-analysis. Int J Nurs Stud. (2021) 124:104099. doi: 10.1016/j.ijnurstu.2021.104099
2. Yates SW. Physician stress and burnout. Am J Med. (2020) 133:160–4. doi: 10.1016/j.amjmed.2019.08.034
3. Bresesti I, Folgori L, De Bartolo P. Interventions to reduce occupational stress and burn out within neonatal intensive care units: a systematic review. Occup Environ Med. (2020) 77:515–9. doi: 10.1136/oemed-2019-106256
4. Nemteanu MS, Dinu V, Dabija DC. Job insecurity, job instability, and job satisfaction in the context of the COVID-19 pandemic. J Compet. (2021) 13:65–82. doi: 10.7441/joc.2021.02.04
5. Nemteanu MS, Dabija DC. The influence of internal marketing and job satisfaction on task performance and counterproductive work behavior in an emerging marketing during the covid-19 pandemic. Int J Environ Res Public Health. (2021) 18:3670. doi: 10.3390/ijerph18073670
6. Bliese PD, Edwards JR, Sonnentag S. Stress and well-being at work: a century of empirical trends reflecting theoretical and societal influences. J Appl Psychol. (2017) 102:389–402. doi: 10.1037/apl0000109
7. Hall LH, Johnson J, Watt I, Tsipa A, O'Connor DB. Healthcare staff wellbeing, burnout, and patient safety: a systematic review. PLoS ONE. (2016) 11:1–12. doi: 10.1371/journal.pone.0159015
8. Profit J, Sharek PJ, Amspoker AB, Kowalkowski MA, Nisbet CC, Thomas EJ, et al. Burnout in the NICU setting and its relation to safety culture. BMJ Qual Saf . (2014) 23:806–13. doi: 10.1136/bmjqs-2014-002831
9. Tawfik DS, Phibbs CS, Sexton JB, Kan P, Sharek PJ, Nisbet CC, et al. Factors associated with provider burnout in the NICU. Pediatrics. (2017) 139: e20164134. doi: 10.1542/peds.2016-4134
10. Lin TC, Lin HS, Cheng SF, Wu LM, Ou-Yang MC. Work stress, occupational burnout and depression levels: a clinical study of paediatric intensive care unit nurses in Taiwan. J Clin Nurs. (2016) 25:1120–30. doi: 10.1111/jocn.13119
11. Favrod C, du Chêne LJ, Soelch CM, Garthus-Niegel S, Tolsa JF, Legault F, et al. Mental health symptoms and work-related stressors in hospital midwives and NICU nurses: a mixed methods study. Front Psychiatry. (2018) 9: 364 doi: 10.3389/fpsyt.2018.00364
12. Fumagalli M, Provenzi L, Sorrentino G, Ciceri F, Fontana C, Passera S, et al. Self-report and biological indexes of work-related stress in neonatal healthcare professionals: a repeated-measures observational study. Adv Neonatal Care. (2021) 21:E120–8. doi: 10.1097/ANC.0000000000000848
13. Moscoso MS, Lengacher C. The assessment of the perceived emotional distress: the neglected side of cancer care. Psicooncologia. 9, 277–88. (2012).
14. Barello S, Palamenghi L, Graffigna G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res. (2020) 290:113129. doi: 10.1016/j.psychres.2020.113129
15. Cena L, Biban P, Janos J, Lavelli M, Langfus J, Tsai A, et al. The collateral impact of COVID-19 emergency on neonatal intensive care units and family-centered care: challenges and opportunities. Front Psychol. (2021) 12:1–10. doi: 10.3389/fpsyg.2021.630594
16. Gagliardi L, Grumi S, Gentile M, Cacciavellani R, Placidi G, Vaccaro A, et al. The COVID-related mental health load of neonatal healthcare professionals: a multicenter study in Italy. Ital J Pediatr. (2022) 48:136. doi: 10.1186/s13052-022-01305-7
17. Haidari E, Main EK, Cui X, Cape V, Tawfik DS, Adair KC, et al. Maternal and neonatal health care worker well-being and patient safety climate amid the COVID-19 pandemic. J Perinatol. (2021) 41:961–9. doi: 10.1038/s41372-021-01014-9
18. Gray JA. Neural systems, emotion and personality. In: Madden IV J, editor. Neurobiology of Learning, Emotion and Affect. New York, NY: Raven Press (1991). pp. 273–306.
19. Pickering AD, Gray JA. The neuroscience of personality. In: Pervin LA, John OP, editors. Handbook of Personality: Theory and Research. Guilford Press (1999). pp. 277–99.
20. Bijttebier P, Beck I, Claes L, Vandereycken W. Gray's reinforcement sensitivity theory as a framework for research on personality-psychopathology associations. Clin Psychol Rev. (2009) 29:421–30. doi: 10.1016/j.cpr.2009.04.002
21. Kimbrel NA, Nelson-Gray RO, Mitchell JT. Reinforcement sensitivity and maternal style as predictors of psychopathology. Pers Individ Dif. (2007) 42:1139–49. doi: 10.1016/j.paid.2006.06.028
22. Folkman S, Lazarus RS. If it changes it must be a process: Study of emotion and coping during three stages of a college examination. J Pers Soc Psychol. (1985) 48:150–70. doi: 10.1037/0022-3514.48.1.150
23. Wong TW, Yau JKY, Chan CLW, Kwong RSY, Ho SMY, Lau CC, et al. The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. Eur J Emerg Med. (2005) 12: 13–8. doi: 10.1097/00063110-200502000-00005
24. Khalid I, Khalid TJ, Qabajah MR, Barnard AG, Qushmaq IA. Healthcare workers emotions, perceived stressors and coping strategies during a MERS-CoV outbreak. Clin Med Res. (2016) 14:7–14. doi: 10.3121/cmr.2016.1303
25. Sica C, Magni C, Ghisi M, Altoè G, Sighinolfi C, Chiri LR, et al. Coping orientation to the problems experiences-new Italian version (COPE-NVI). Psicoterapia Cognitiva e Comportamentale. (2008) 14:27–53.
26. Foà C, Tonarelli A, Caricati L, Fruggeri L. COPE-NVI-25: validazione italiana della versione ridotta della coping orientation to the problems experienced (COPE-NVI). Psicologia Della Salute. (2015) 2:123–40. doi: 10.3280/PDS2015-002007
27. Labrague LJ. Psychological resilience, coping behaviours and social support among health care workers during the COVID-19 pandemic: a systematic review of quantitative studies. J Nurs Manag. (2021) 29:1893–905. doi: 10.1111/jonm.13336
28. Babore A, Lombardi L, Viceconti ML, Pignataro S, Marino V, Crudele M, et al. Psychological effects of the COVID-2019 pandemic: perceived stress and coping strategies among healthcare professionals. Psychiatry Res. (2020) 293:113366. doi: 10.1016/j.psychres.2020.113366
29. Nie A, Su X, Zhang S, Guan W, Li J. Psychological impact of COVID-19 outbreak on frontline nurses: a cross-sectional survey study. J Clin Nurs. (2020) 29:4217–26. doi: 10.1111/jocn.15454
30. Zhu J, Sun L, Zhang L, Wang H, Fan A, Yang B, et al. Prevalence and influencing factors of anxiety and depression symptoms in the first-line medical staff fighting against COVID-19 in Gansu. Front Psychiatry. (2020) 11:386. doi: 10.3389/fpsyt.2020.00386
31. Flesia L, Monaro M, Mazza C, Fietta V, Colicino E, Segatto B, et al. Predicting perceived stress related to the covid-19 outbreak through stable psychological traits and machine learning models. J Clin Med. (2020) 9:1–17. doi: 10.3390/jcm9103350
32. Di Monte C, Monaco S, Mariani R, Di Trani M. From resilience to burnout: psychological features of Italian general practitioners during COVID-19 emergency. Front Psychology. (2020) 11:567201. doi: 10.3389/fpsyg.2020.567201
33. Hou T, Zhang R, Song X, Zhang F, Cai W, Liu Y, et al. Self-efficacy and fatigue among non-frontline health care workers during COVID-19 outbreak: a moderated mediation model of posttraumatic stress disorder symptoms and negative coping. PLoS ONE. (2020) 15:1–21. doi: 10.1371/journal.pone.0243884
34. Cooper MD. Towards a model of safety culture. Saf Sci. (2000) 36:111–36. doi: 10.1016/S0925-7535(00)00035-7
35. Denning M, Goh ET, Tan B, Kanneganti A, Almonte M, Scott A, et al. Determinants of burnout and other aspects of psychological well-being in healthcare workers during the COVID-19 pandemic: a multinational cross-sectional study. PLoS ONE. (2021) 16:1–18. doi: 10.1371/journal.pone.0238666
36. Aiken LH, Sermeus W, Van Den Heede K, Sloane DM, Busse R, McKee M, et al. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ. (2012) 344:1–14. doi: 10.1136/bmj.e1717
37. Profit J, Etchegaray J, Petersen LA, Sexton JB, Hysong SJ, Mei M, Thomas EJ. Neonatal intensive care unit safety culture varies widely. Arch Dis Child Fetal Neonatal Ed. (2012) 97:F127–32. doi: 10.1136/archdischild-2011-300612
38. Tan BYQ, Kanneganti A, Lim LJH, Tan M, Chua YX, Tan L, et al. Burnout and associated factors among health care workers in Singapore during the COVID-19 Pandemic. J Am Med Dir Assoc. (2020) 21:1751–8.e5. doi: 10.1016/j.jamda.2020.09.035
39. Beck AT, Steer RA, Carbin MG. Psychometric properties of the beck depression inventory: twenty-five years of evaluation. Clin Psychol Rev. (1988) 8:77–100. doi: 10.1016/0272-7358(88)90050-5
40. Spielberger CD, Gorsuch RL, Lushene RE, Vagg PR, Jacobs GA. State-trait anxiety inventory. Palo Alto. (1970). Unpublished manual.
41. Attanasio V, Andrasik F, Blanchard EB, Arena JG. Psychometric properties of the SUNYA revision of the psychosomatic symptom checklist. J Behav Med. (1984) 7:247–57. doi: 10.1007/BF00845390
43. Horowitz M, Wilner N, Alvarez W. Impact of event scale: a measure of subjective stress. Psychosom Med. (1979) 41:209–18. doi: 10.1097/00006842-197905000-00004
44. Carver CS, White TL. Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: the BIS/BAS scales. J Pers Soc Psychol. (1994) 67:319–33. doi: 10.1037/0022-3514.67.2.319
45. Nguyen G, Gambashidze N, Ilyas SA, Pascu D. Validation of the safety attitudes questionnaire (short form 2006) in Italian in hospitals in the northeast of Italy. BMC Health Serv Res. (2015) 15:284. doi: 10.1186/s12913-015-0951-8
46. Corr PJ. Reinforcement sensitivity theory and personality. Neurosci Biobehav Rev. (2004) 28:317–32. doi: 10.1016/j.neubiorev.2004.01.005
47. McFarland BR, Shankman SA, Tenke CE, Bruder GE, Klein DN. Behavioral activation system deficits predict the six-month course of depression. J Affect Disord. (2006) 91:229–34. doi: 10.1016/j.jad.2006.01.012
48. Contractor AA, Elhai JD, Ractliffe KC, Forbes D. PTSD's underlying symptom dimensions and relations with behavioral inhibition and activation. J Anxiety Disord. (2013) 27:645–51. doi: 10.1016/j.janxdis.2013.07.007
49. Leone L, Russo PM. Components of the behavioral activation system and functional impulsivity: a test of discriminant hypotheses. J Res Pers. (2009) 43:1101–4. doi: 10.1016/j.jrp.2009.08.004
50. Hundt NE, Kimbrel NA, Mitchell JT, Nelson-Gray RO. High BAS, but not low BIS, predicts externalizing symptoms in adults. Pers Individ Dif. (2008) 44:565–75. doi: 10.1016/j.paid.2007.09.018
51. Markarian SA, Pickett SM, Deveson DF, Kanona BB. A model of BIS/BAS sensitivity, emotion regulation difficulties, and depression, anxiety, and stress symptoms in relation to sleep quality. Psychiatry Res. (2013) 210:281–6. doi: 10.1016/j.psychres.2013.06.004
52. Struijs SY, Lamers F, Rinck M, Roelofs K, Spinhoven P, Penninx BWJH. The predictive value of approach and avoidance tendencies on the onset and course of depression and anxiety disorders. Depress Anxiety. (2018) 35:551–9. doi: 10.1002/da.22760
53. Toyoshima K, Inoue T, Kameyama R, Masuya J, Fujimura Y, Higashi S, et al. BIS/BAS as moderators in the relationship between stressful life events and depressive symptoms in adult community volunteers. J Affect Disord Rep. (2021) 3:100050. doi: 10.1016/j.jadr.2020.100050
54. Taubitz L, Pedersen W, Larson C. BAS reward responsiveness: a unique predictor of positive psychological functioning. Pers Individ Dif. (2015) 80:107–12. doi: 10.1016/j.paid.2015.02.029
55. Gomez R, Gomez A. Convergent, discriminant and concurrent validities of measures of the behavioural approach and behavioural inhibition systems: confirmatory factor analytic approach. Pers Individ Dif. (2005) 38:87–102. doi: 10.1016/j.paid.2004.03.011
56. Tull MT, Gratz KL, Latzman RD, Kimbrel NA, Lejuez CW. Reinforcement sensitivity theory and emotion regulation difficulties: a multimodal investigation. Pers Individ Dif. (2010) 49:989–94. doi: 10.1016/j.paid.2010.08.010
57. Pickett SM, Bardeen JR, Orcutt HK. Experiential avoidance as a moderator of the relationship between behavioral inhibition system sensitivity and posttraumatic stress symptoms. J Anxiety Disord. (2011) 25:1038–45. doi: 10.1016/j.janxdis.2011.06.013
58. Voigt DC, Dillard JP, Braddock KH, Anderson JW, Sopory P, Stephenson MT. BIS/BAS scales and their relationship to risky health behaviours. Pers Individ Dif. (2009) 47:89–93. doi: 10.1016/j.paid.2009.02.003
59. Teasdale E, Yardley L, Schlotz W, Michie S. The importance of coping appraisal in behavioural responses to pandemic flu. Br J Health Psychol. (2012) 17:44–59. doi: 10.1111/j.2044-8287.2011.02017.x
60. Cooper CL, Dewe PJ, O'Driscoll MP. Organizational Stress: A Review and Critique of Theory, Research, and Applications. London: Sage Publications. (2001).
61. Huang Y, Liu Y, Wang Y, Liu D. Family function fully mediates the relationship between social support and perinatal depression in rural Southwest China. BMC Psychiatry. (2021) 21:151. doi: 10.1186/s12888-021-03155-9
62. Pettker CM, Thung SF, Norwitz ER, Buhimschi CS, Raab CA, Copel JA, et al. Impact of a comprehensive patient safety strategy on obstetric adverse events. Am J Obstet Gynecol. (2009) 200:492.e1–8. doi: 10.1016/j.ajog.2009.01.022
63. Cronqvist A, Theorell T, Burns T, Lützén K. Dissonant imperatives in nursing: a conceptualization of stress in intensive care in Sweden. Intensive Crit Care Nurs. (2001) 17:228–36. doi: 10.1054/iccn.2000.1588
64. Yu F, Raphael D, Mackay L, Smith M, King A. Personal and work-related factors associated with nurse resilience: a systematic review. Int J Nurs Stud. (2019) 93:129–40. doi: 10.1016/j.ijnurstu.2019.02.014
65. Evanoff BA, Strickland JR, Dale AM, Hayibor L, Page E, Duncan JG, et al. Work-related and personal factors associated with mental well-being during the COVID-19 response: survey of health care and other workers. J Med Internet Res. (2020) 22:e21366–e21366. doi: 10.2196/21366
66. Profit J, Sharek PJ, Kan P, Rigdon J, Desai M, Nisbet CC, et al. Teamwork in the NICU setting and its association with health care-associated infections in very low-birth-weight infants. Am J Perinatol. (2017) 34:1032–9. doi: 10.1055/s-0037-1601563
67. Winning AM, Merandi JM, Lewe D, Stepney LMC, Liao NN, Fortney CA, et al. The emotional impact of errors or adverse events on healthcare providers in the NICU: The protective role of coworker support. J Adv Nurs. (2018) 74:172–80. doi: 10.1111/jan.13403
68. Haerkens MH, Jenkins DH, van der Hoeven JG. Crew resource management in the ICU: the need for culture change. Ann Intensive Care. (2012) 2:39. doi: 10.1186/2110-5820-2-39
69. Williams TC, Bach CC, Matthiesen NB, Henriksen TB, Gagliardi L. Directed acyclic graphs: a tool for causal studies in paediatrics. Pediatr Res. (2018) 84:487–93. doi: 10.1038/s41390-018-0071-3
70. Guirardello EB. Impact of critical care environment on burnout, perceived quality of care and safety attitude of the nursing team. Rev Lat Am Enfermagem. (2017) 25:e2884. doi: 10.1590/1518-8345.1472.2884
71. Jiménez R, Swartz M, McCorkle R. Improving quality through nursing participation at bedside rounds in a pediatric acute care unit: a pilot project. J Pediatr Nurs. (2018) 43:45–55. doi: 10.1016/j.pedn.2018.08.010
72. Wagner A, Hammer A, Manser T, Martus P, Sturm H, Rieger MA. Do occupational and patient safety culture in hospitals share predictors in the field of psychosocial working conditions? findings from a cross-sectional study in German university hospitals. Int J Environ Res Public Health. (2018) 15:2131. doi: 10.3390/ijerph15102131
Keywords: neonatal healthcare professionals, stress, coping, safety culture, NICUs, behavioral activation, behavioral inhibition
Citation: Nazzari S, Grumi S, Ciotti S, Merusi I, Provenzi L and Gagliardi (2022) Determinants of emotional distress in neonatal healthcare professionals: An exploratory analysis. Front. Public Health 10:968789. doi: 10.3389/fpubh.2022.968789
Received: 17 June 2022; Accepted: 08 September 2022;
Published: 29 September 2022.
Edited by:
Francesco Chirico, Catholic University of the Sacred Heart, ItalyReviewed by:
Gabriele d'Ettorre, ASL Lecce, ItalyTobias Weigl, Hochschule Fresenius–University of Applied Sciences Düsseldorf, Germany
Copyright © 2022 Nazzari, Grumi, Ciotti, Merusi, Provenzi and Gagliardi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Livio Provenzi, bGl2aW8ucHJvdmVuemlAdW5pcHYuaXQ=
 Sarah Nazzari
Sarah Nazzari Serena Grumi
Serena Grumi Sabina Ciotti3,4
Sabina Ciotti3,4 Ilaria Merusi
Ilaria Merusi Livio Provenzi
Livio Provenzi Luigi Gagliardi
Luigi Gagliardi