
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 10 August 2022
Sec. Children and Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.966055
 Atalay Goshu Muluneh1
Atalay Goshu Muluneh1 Melaku Hunie Asratie2
Melaku Hunie Asratie2 Tesfamichael Gebremariam3
Tesfamichael Gebremariam3 Aynalem Adu3
Aynalem Adu3 Mihretu Molla Enyew4
Mihretu Molla Enyew4 Endeshaw Admasu Cherkos2
Endeshaw Admasu Cherkos2 Senetsehuf Melkamu3
Senetsehuf Melkamu3 Martha Berta2
Martha Berta2 Worku Mamo5
Worku Mamo5 Dawit Kassahun6
Dawit Kassahun6 Nuhamin Tesfa Tsega2
Nuhamin Tesfa Tsega2 Azmeraw Ambachew Kebede4
Azmeraw Ambachew Kebede4 Desale Bihonegn Asmamaw7*
Desale Bihonegn Asmamaw7* Getahun Molla Kassa1
Getahun Molla Kassa1 Muhabaw Shumye Mihret4
Muhabaw Shumye Mihret4Background: In developing countries, adverse pregnancy outcomes are major public health issues. It is one of the leading causes of neonatal morbidity and mortality worldwide. Despite the fact that ending prenatal mortality and morbidity is one of the third Sustainable Development Goals (SDG), the burden of the problem continues to be a huge concern in developing countries, including Ethiopia. Hence, this study aimed to determine the prevalence and associated factors of lifetime adverse pregnancy outcomes among antenatal care (ANC) booked women in Northwest Ethiopia.
Methods: An institutional-based cross-sectional study design was conducted in Northwest Ethiopia, between March 2021 and June 2021. A multi-stage stratified random sampling technique was employed to recruit participants. An interviewer-administered and checklist questionnaire were used to collect the data. The data were entered into Epi-data version 4.6 software and exported to Stata version 16 for analysis. The binary logistic regression model was fitted to identify an association between associated factors and the outcome variable. Variables with a p-value of < 0.05 in the multivariable logistic regression model were declared as statistically significant.
Results: In this study, the lifetime prevalence of adverse pregnancy outcome among study participants was 14.53% (95%CI: 11.61, 18.04). Road access to the health facilities (AOR = 2.62; 95% CI: 1.14, 6.02) and husband-supported pregnancy (AOR = 2.63; 95 CI: 1.46, 4.72) were significantly associated with adverse pregnancy outcomes.
Conclusions: More than one in 10 reproductive age women had adverse pregnancy outcome throughout their life. Road access to health facilities and husband-supported pregnancy were statistically significant factors for adverse events in pregnancy. Therefore, it is better to give more attention to expanding infrastructure like road accessibility and increasing husband-supported pregnancy to reduce adverse pregnancy outcomes.
Pregnancy is a delightful natural gift when it is completed without any problems or grief. However, if the result is unsatisfactory, it could be an unpleasant experience for the mother, even for the whole family (1). Stillbirth, premature delivery, low birth weight, and birth defects are some of the adverse pregnancy outcomes (2). These adverse pregnancy effects will not be limited to death but also cause long-term physical and neurological impairments for the survived babies (3).
Despite substantial efforts made to decrease adverse pregnancy outcomes, a large number of pregnancies remain complicated with disastrous results. Regarding this, in the year 2014, the World Health Assembly authorized a target aimed at lowering the worldwide stillbirth rate to 12 per 1,000 births by the year 2030 in all countries (4). However, the stillbirth rate is alarmingly rising. Globally, ≈2 million pregnancies resulted in stillbirth (i.e., one stillbirth every 16 s) (5), 98% of these occurring in resource-limited countries (6). Of these, about 0.88 million stillbirths have occurred in Sub-Saharan Africa (SSA) and 24.6 stillbirth rate per 1,000 total births in Ethiopia (5).
Along with stillbirth, low birth weight, congenital anomalies, and premature deliveries, these are public health issues that cause profound depression, loneliness, and economic impact on women and their families (7). Low birth weight complicates about 15–20% (2 million deliveries per year) around the world (8). As a result, the World Health Organization (WHO) established a strategy to reduce the global rate of low birth weight (LBW) by 30% by the year 2025 (9).
Most pregnancy adverse outcomes might have been avoided if women had received high-quality preconception, pregnancy, and delivery care (10, 11). Many adverse pregnancy outcomes are the result of poor quality care during pregnancy and childbirth, a lack of emphasis on prevention treatments, a failure to recognize the social consequences of adverse pregnancy outcomes, and a poor data recording system (5). Thus, to effectively manage adverse pregnancy outcomes, there is a need for contemporary data on the causes (12).
Multiple factors like older maternal age (13), experiencing delays in getting treatment (14), high-risk pregnancy (15, 16), lack of antenatal care visits (17), multiple pregnancies (18), and having chronic medical conditions (19) are some of the identified factors that can affect the adverse pregnancy outcome. Thus, adverse pregnancy outcomes can be prevented and treated with immunization, nutritional supplementation, and routine screening for specific diseases (20).
Ethiopia has implemented different strategies to decrease adverse pregnancy outcomes. Despite this, adverse pregnancy outcomes in Ethiopia remain significantly higher because predictors are poorly understood and prevention strategies are inadequate (21–23). Identifying the probable causes linked to poor pregnancy outcomes and developing a practical strategy would thus be beneficial in reversing the alarming trend. Therefore, this study aimed to assess the lifetime prevalence of adverse pregnancy outcomes and associated factors in northwest Ethiopia.
An institutional-based cross-sectional study design was applied. The study was performed in central Gondar (Central Gondar zone and Gondar city administration), Northwest Ethiopia, from the period of March 2021 to June 2021. The Central Gondar zone is located 738 km northwest of Addis Ababa. The central Gondar includes the Central Gondar Zone with 15 districts and the Gondar City administration. According to the national reports conducted by the Central Statistical Agency of Ethiopia, Central Gondar has a total population of 2,711,329, of which 91,372 pregnancies were projected for 2020/21 by the zonal statistical agency. In the study area, maternal health services like antenatal care (ANC), skilled delivery, and postnatal care (PNC) services are freely available for women without any cost. All health centers and hospitals give maternal and neonatal health services.
All ANC booked pregnant women in the central Gondar zone and Gondar City were the source population. All ANC booked pregnant women in the selected health facilities were the study population. All women who had at least one normal live birth or adverse pregnancy outcome history before and were booked for ANC at the selected health facilities were included in our study. All women who had at least one normal live birth or adverse pregnancy outcome history before and were booked for ANC at the selected health facilities with mothers who died and critically ill were excluded.
The sample size for the present study was calculated using a single population proportion formula by considering the following assumptions: 95% level of confidence, 18% proportion of adverse pregnancy outcome (19), and 5% margin of error.
Where, n = required sample size, α = level of significant, z = standard normal distribution curve value for 95% confidence level = 1.96, p = proportion of adverse pregnancy outcome, and d = margin of error. After considering a non-response rate of 10% and a design effect of 2, we obtained a total sample size of 500. A multistage stratified sampling technique was used to select the study participants. At the first stage, three districts ( Gondar zuria, West Dembia and Wogera) and one city administration were selected by using lottery methods, and from each district, 20% of the health facilities were selected. From the selected districts and Gondar city, five health facilities (160 participants), four health facilities (145 participants), two health facilities (75 participants), and three health facilities (88 participants) were selected from Gondar zuria district, Gondar city, West Dembia district, and Wogera district, respectively.
The dependent variable was life time adverse pregnancy outcome whereas the independent variables were age, marital status, education, residence, religion, occupation, and parity, number of living children, insurance membership, distance to the nearest health facility, pregnancy wontedness, pregnancy supported by the husband, the reason for the first ANC, and history of chronic illness.
Adverse pregnancy outcome: was considered as “yes,” if women had at least one of the following before her current pregnancy: still birth, abortion, intrauterine growth restriction, congenital anomalies, gestational hypertension disorders, gestational diabetes, and preterm birth (2).
If born before 37 completed weeks of gestation but after 28 weeks of gestation or low birth weight (24).
It defined as any abnormality of physical structure found at birth or during the first few weeks of life; or any irreversible condition existing in a child before birth in which there is sufficient deviation in the usually number, size, shape, location of any part, organ, and cell to warrant its designation as abnormal (25).
If the infant died in the womb or during the intrapartum period after 28 weeks of gestation (26).
Fetus removed or expelled from the uterus before 28 weeks or weighing < 500 g (27).
The data collection tool was developed by reviewing the literature (13, 17–19, 28–30). A structured, interviewer-administered and checklist questionnaire were employed to collect the data through face-to-face interviews and observing charts. The questionnaire was developed in English first, then translated to Amharic (the local language), and re-translated back to the English language to check its consistency. The questionnaire contains socio-demographic characteristics, maternity health services, and reproductive-related characteristics of the participants. A total of 18-trained midwives collected the data under the supervision of six MSc holders. Data collectors and supervisors were oriented and trained for 1 day, focusing on how to select and interview the participants. The questionnaires were pretested on 24 study participants (5%) and modifications were made according to the results of the pretest.
Data were checked for completeness and entered into Epi-data version 4.6 Statistical software and transferred to the Stata version 16 for further cleaning and analysis. Descriptive statistics were described using frequencies, percentages, mean and standard deviation, which were further presented using tables, and texts. Normality tests such as kurtosis and skewness were employed to see the normal distribution of the variables and to identify which summary measures were appropriate to use.
A binary logistic regression model was used with a cut-off P-value <0.25 and <0.05 in the bi-and multi-variable analysis respectively. Adjusted odds ratio with 95% confidence intervals was computed to see the presence of an association between dependent and independent variables. The 95% CI was used to declare the statistical association. We tested the chi-square assumption and model goodness of fit was tested using the Hosmer Lemeshow test. Besides, the multi-collinearity assumption was tested using pseudo variance inflation factor (VIF), and standard error. Thus, parity was excluded from the final analysis because of the significant multi-collinearity effect.
A total of 468 women with a 93.6% response rate were involved in this study, of which 198 (42.49%) were in the age group of 26–30, with a median age of 28 (IQR = 25, 31) years. The majority of the mothers 443 (94.66%) were married, and 279 (59.62%) mothers were rural residents. Regarding educational status, 287 (61.32%) had no formal education (Table 1).
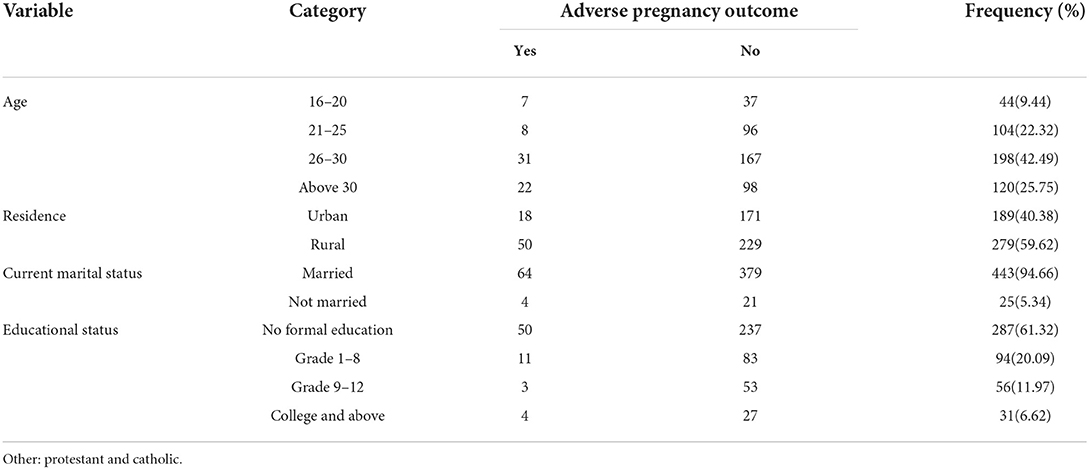
Table 1. Socio-demographic characteristics of study participants in Northwest, Ethiopia, 2021 (n = 468).
Among the study participants, 200 (49.57%) mothers were multi-gravidas. Nearly half (49.79%) of mothers had community-based health insurance membership. Regarding husband-supported pregnancy, the majority of (80.56) pregnancies were husband-supported pregnancies (Table 2).
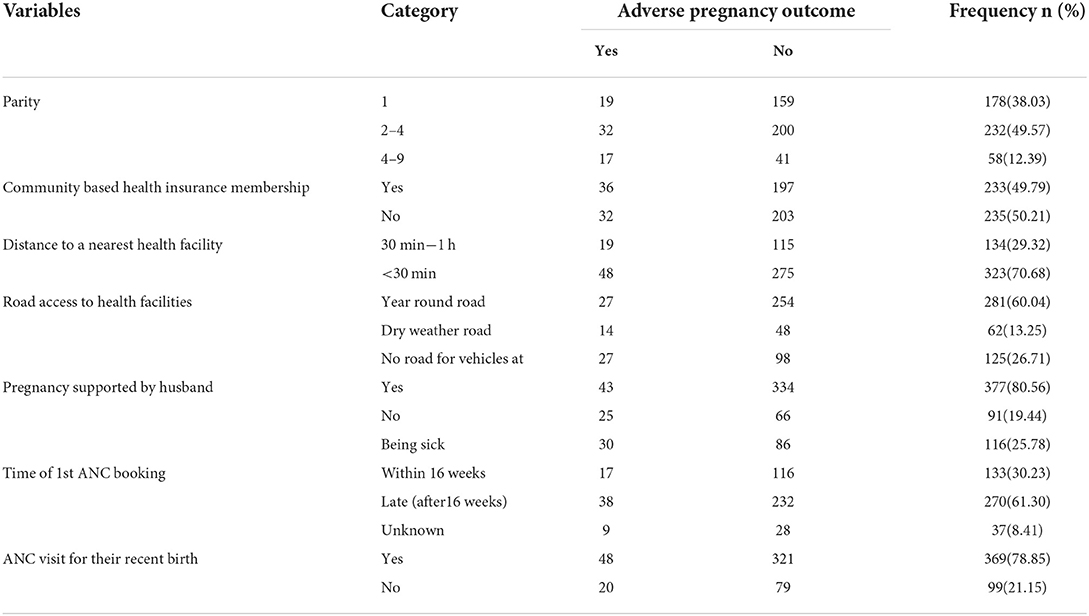
Table 2. Obstetrics related characteristics of study participants in Northwest, Ethiopia, 2021 (n = 468).
The study found that the lifetime prevalence of adverse pregnancy outcome among study participants was 14.53% (95%CI: 11.61, 18.04). Out of which, the commonest adverse pregnancy outcomes was abortion 33 (7.05%) followed by stillbirth 15 (3.21%) (Table 3).
In the multivariable logistic regression analysis, road access to health facilities and husband-supported pregnancy had a statistically significant association with adverse pregnancy outcome.
The odds of adverse pregnancy outcome among women who had no road access to the health facilities was 2.62 times (AOR = 2.62; 95% CI: 1.14, 6.02) higher than those with road access to the health facilities. The odds of adverse pregnancy outcome among women with no husband-supported pregnancy were 2.62 times (AOR = 2.63; 95 CI: 1.46, 4.72) higher than those women with a husband-supported pregnancy (Table 4).

Table 4. Binary logistic regression analysis for factors associated with adverse pregnancy outcome, Northwest, Ethiopia, 2021(n = 468).
This study was conducted to assess the lifetime prevalence of adverse pregnancy outcome and associated factors among ANC booked women in Northwest, Ethiopia. The overall lifetime prevalence of adverse pregnancy outcome in the current study was found to be 14.53% (95%CI: 11.61, 18.04). This is in line with a study conducted in southern Ethiopia (13.9%) (31), Tanzania (18%) (32). However, this finding is higher than a systematic review conducted in Ethiopia 5.3% (33). The possible explanations may be due to the current study being at a one zone in which total populations are different when we compare with the national and gap in the year of study and a lot of strategies and work has been implemented since then to improve maternal and child health service utilization (34).
On the other hand, this finding is also lower than the findings of studies conducted in Hossana town, Ethiopia (24.5%) (35), Wollo zone, Ethiopia (31.8%) (17), Ghana (19%) (36), and Uganda (37%) (37). The possible reasons for this discrepancy may be the difference in the study setting, time gap, and socio-demographic variations. For instance, the study done in Ghana was hospital-based, unlike the present study, which was also conducted at health centers. Commonly, health centers are located in remote areas where the inaccessibility of infrastructure makes it difficult to provide service to remote areas and is attributed to socio-economic variations and the quality of maternal health services. In addition, the variation of nutritional and cultural practices may contribute to the observed variations.
In this study, we found that women who had no husband-supported pregnancy were more likely to have an adverse pregnancy outcome than those who had a husband supported pregnancy. This is supported by studies conducted in the United States (28), and Nepal (38). The possible explanation might be that those who had no husband-supported pregnancy have been shown to have effects on women's behaviors prenatally (39). Those who have no husband-supported pregnancy may experience stress, decrease social support, are less likely to enter preconception and prenatal care, and husband unsupported pregnancy is usually an unwanted pregnancy. Which may increase the likelihood of negative pregnancy outcomes (40–42). Furthermore, evidence suggests that an unsupported pregnancy by a husband has no effect on maternal health care service access and utilization, such as ANC, institutional delivery, and postnatal care. It can affect pregnancy and childbirth through responding to health problems that can occur during pregnancy (preeclampsia, preterm birth, and infection), seeking medical help, paying for transport, and allocating household resources (42, 43).
The odds of an adverse pregnancy outcome among women who had no road access to the health facilities was 2.62 times higher than those who had road access to the health facilities. This could be because inaccessibility of roads restricts utilization of basic maternal health services like ANC, health facility delivery, and postnatal care, which leads to an increased adverse pregnancy outcome (44–46). Poor accessibility of road and transport facilities also affects hospital supplies, often resulting in a stock-out of essential medicines. Impediment of accessing timely referral care, which exacerbates the cost of accessing maternal health care services, and pregnant women conveyed by inappropriate transport, which exacerbates the already existing poor health. Moreover, the inaccessibility of transport is also directly responsible for adverse pregnancy outcomes (47, 48).
More than one in 10 reproductive-age women had an adverse pregnancy outcome at some point in their life. Road access to health facilities and husband-supported pregnancy were statistically significant factors for adverse events in pregnancy. Therefore, it is better to give more attention to expanding infrastructure like road accessibility and increasing husband-supported pregnancy to reduce adverse pregnancy outcomes.
The original contributions presented in the study are included in the article/supplementary files, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by University of Gondar. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
AM: Conceived and designed the study, performed analysis and writing original draft and critically evaluated and made progressive suggestions throughout the study. GK, TG, EC, WM, NT, AA, MA, and MM: Participated in the design, developing methods and critically reviewed the manuscript. AM, GK, AK, DK, SM, MB, and DA: Participated in the study design, data analysis, interpretation and draft manuscript. AM, MM, DK, and DA: Participated in the data entry, analysis, interpretation, and critically revise the manuscript. All authors have read and approved the final manuscript.
We would like to thank the University of Gondar for providing study ethical clearance. Our thankfulness also goes to all data collectors and study participants. In addition, we are glad to the district health office for giving us a permission letter.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AOR, Adjusted Odds Ratio; ANC, Antenatal Care; CI, Confidence Interval; COR, Crude Odds Ratio; COVID-19, Coronavirus disease; WHO, World Health Organization.
1. Lawn JE, Lee ACC, Kinney M, Sibley L, Carlo WA, Paul VK, et al. Two million intrapartum-related stillbirths and neonatal deaths: where, why, and what can be done? Int J Gynecol Obstet. (2009) 107:S5–19. doi: 10.1016/j.ijgo.2009.07.016
2. NBGo H. Preventing Prematurity and Adverse Birth Outcomes: What Employers Should Know. USA Center for Prevention and Health Services (2009).
4. World Health Organization. 67th World Health Assembly (WHA). Geneva: World Health Organization (2014).
5. Hug L, Mishra A, Lee S, You D, Moran A, Strong KL, et al. A Neglected Tragedy. The Global Burden of Stillbirths: Report of the UN Inter-agency Group for Child Mortality Estimation, 2020. New York, NY: United Nations Children's Fund (2020).
6. Lawn JE, Blencowe H, Waiswa P, Amouzou A, Mathers C, Hogan D, et al. Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet. (2016) 387:587–603. doi: 10.1016/S0140-6736(15)00837-5
7. Heazell AEP, Siassakos D, Blencowe H, Burden C, Bhutta ZA, Cacciatore J, et al. Stillbirths: economic and psychosocial consequences. Lancet. (2016) 387:604–16. doi: 10.1016/S0140-6736(15)00836-3
8. Marete I, Ekhaguere O, Bann CM, Bucher SL, Nyongesa P, Patel AB, et al. Regional trends in birth weight in low-and middle-income countries 2013–2018. Reprod Health. (2020) 17:1–8. doi: 10.1186/s12978-020-01026-2
9. World Health Organization. Global Nutrition Targets 2025: Low Birth Weight Policy Brief. Geneva: World Health Organization (2014).
10. Vogel JP, Souza JP, Mori R, Morisaki N, Lumbiganon P, Laopaiboon M, et al. WHO multicountry survey on maternal and newborn health research network. Maternal complications and perinatal mortality: findings of the World Health Organization Multicountry Survey on Maternal and Newborn Health. BJOG. (2014) 121:76–88. doi: 10.1111/1471-0528.12633
11. Bhutta ZA, Das JK, Bahl R, Lawn JE, Salam RA, Paul VK, et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet. (2014) 384:347–70. doi: 10.1016/S0140-6736(14)60792-3
12. Aminu M, Bar-Zeev S, White S, Mathai M, van den Broek N. Understanding cause of stillbirth: a prospective observational multi-country study from sub-Saharan Africa. BMC Pregnancy Childbirth. (2019) 19:1–10. doi: 10.1186/s12884-019-2626-7
13. Frick AP. Advanced maternal age and adverse pregnancy outcomes. Best Pract Res Clin Obstet Gynaecol. (2021) 70:92–100. doi: 10.1016/j.bpobgyn.2020.07.005
14. Adeoye IA, Onayade AA, Fatusi AO. Incidence, determinants and perinatal outcomes of near miss maternal morbidity in Ile-Ife Nigeria: a prospective case control study. BMC Pregnancy Childbirth. (2013) 13:1–10. doi: 10.1186/1471-2393-13-93
15. Adane AA, Ayele TA, Ararsa LG, Bitew BD, Zeleke BM. Adverse birth outcomes among deliveries at Gondar University hospital, Northwest Ethiopia. BMC Pregnancy Childbirth. (2014) 14:1–8. doi: 10.1186/1471-2393-14-90
16. Shattnawi KK, Khader YS, Alyahya MS, Al-Sheyab N, Batieha A. Rate, determinants, and causes of stillbirth in Jordan: findings from the Jordan Stillbirth and Neonatal Deaths Surveillance (JSANDS) system. BMC Pregnancy Childbirth. (2020) 20:1–8. doi: 10.1186/s12884-020-03267-2
17. Kassahun EA, Mitku HD, Getu MA. Adverse birth outcomes and its associated factors among women who delivered in North Wollo zone, northeast Ethiopia: a facility based cross-sectional study. BMC Res Notes. (2019) 12:1–6. doi: 10.1186/s13104-019-4387-9
18. Degno S, Lencha B, Aman R, Atlaw D, Mekonnen A, Woldeyohannes D, et al. Adverse birth outcomes and associated factors among mothers who delivered in Bale zone hospitals, Oromia Region, Southeast Ethiopia. J Int Med Res. (2021) 49:03000605211013209. doi: 10.1177/03000605211013209
19. Tsegaye B, Kassa A. Prevalence of adverse birth outcome and associated factors among women who delivered in Hawassa town governmental health institutions, south Ethiopia, in 2017. Reprod Health. (2018) 15:1–10. doi: 10.1186/s12978-018-0631-3
20. Chaibva BV. Determinants of Adverse Pregnant Outcomes in Mutare District Clinics, Manicaland Province, Zimbabwe. Pretoria: University of Pretoria (2014).
21. Zenebe K, Awoke T, Birhan N. Low birth weight & associated factors among newborns in Gondar town, North West Ethiopia: institutional based cross-sectional study. Indo Glob J Pharm Sci. (2014) 4:74–80. doi: 10.35652/IGJPS.2014.110
22. Taabia FZ. Maternal Determinants of Adverse Birth Outcomes (ASPHYXIA, LBW and PPH) IN Lambussie District, Ghana. Francis zinenuba taabia (2018).
23. Demographic I. Health Survey 2016: Key Indicators Report. Addis Ababa; Rockville, MD: Ethiopia Demographic and Health Survey (2016).
24. Walani SR. Global burden of preterm birth. Int J Gynecol Obstet. (2020) 150:31–3. doi: 10.1002/ijgo.13195
25. Ali A, Zahad S, Masoumeh A, Azar A. Congenital malformations among live births at Arvand Hospital, Ahwaz, Iran-A prospective study. Pak J Med Sci. (2008) 24:33.
26. Da Silva FT, Gonik B, McMillan M, Keech C, Dellicour S, Bhange S, et al. Stillbirth: case definition and guidelines for data collection, analysis, and presentation of maternal immunization safety data. Vaccine. (2016) 34:6057. doi: 10.1016/j.vaccine.2016.03.044
27. Samandari G, Wolf M, Basnett I, Hyman A, Andersen K. Implementation of legal abortion in Nepal: a model for rapid scale-up of high-quality care. Reprod Health. (2012) 9:1–11. doi: 10.1186/1742-4755-9-7
28. Shah MK, Gee RE, Theall KP. Partner support and impact on birth outcomes among teen pregnancies in the United States. J Pediatr Adolesc Gynecol. (2014) 27:14–9. doi: 10.1016/j.jpag.2013.08.002
29. Chaibva BV. Determinants of Adverse Pregnant Outcomes in Mutare District Clinics, Manicaland Province, Zimbabwe. Pretoria: University of Pretoria (2014).
30. Abebe H, Shitu S, Workye H, Mose A. Predictors of stillbirth among women who had given birth in Southern Ethiopia, 2020: a case-control study. PLoS ONE. (2021) 16:e0249865. doi: 10.1371/journal.pone.0249865
31. Lolaso T, Oljira L, Dessie Y, Gebremedhin M, Wakgari N. Adverse birth outcome and associated factors among newborns delivered in Public Health Institutions, southern ethiopia. East Afr J Health Biomed Sci. (2019) 3:35–44.
32. Watson-Jones D, Weiss HA, Changalucha JM, Todd J, Gumodoka B, Bulmer J, et al. Adverse birth outcomes in United Republic of Tanzania: impact and prevention of maternal risk factors. Bull World Health Organ. (2007) 85:9–18. doi: 10.2471/BLT.06.033258
33. Belay DM, Bayih WA, Alemu AY, Sinshaw AE, Mekonen DK, Ayele AS, et al. Adverse birth outcome and associated factors among diabetic pregnant women in Ethiopia: systematic review and meta-analysis. PLoS ONE. (2020) 15:e0241811. doi: 10.1371/journal.pone.0241811
34. Debelo BT, Danusa KT. Level of late initiation of antenatal care visit and associated factors amongst antenatal care attendant mothers in Gedo General Hospital, West Shoa Zone, Oromia Region, Ethiopia. Front Public Health. (2022) 10:866030. doi: 10.3389/fpubh.2022.866030
35. Abdo R, Endalemaw T, Tesso F. Prevalence and associated factors of adverse birth outcomes among women attended maternity ward at Negest Elene Mohammed Memorial General Hospital in Hosanna Town, SNNPR, Ethiopia. J Women's Health Care. (2016) 5:1000324. doi: 10.4172/2167-0420.1000324
36. Asundep NN, Carson AP, Turpin CA, Tameru B, Agidi AT, Zhang K, et al. Determinants of access to antenatal care and birth outcomes in Kumasi, Ghana. J Epidemiol Glob Health. (2013) 3:279–88. doi: 10.1016/j.jegh.2013.09.004
37. Asiki G, Baisley K, Newton R, Marions L, Seeley J, Kamali A, et al. Adverse pregnancy outcomes in rural Uganda (1996–2013): trends and associated factors from serial cross sectional surveys. BMC Pregnancy Childbirth. (2015) 15:1–12. doi: 10.1186/s12884-015-0708-8
38. Lewis S, Lee A, Simkhada P. The role of husbands in maternal health and safe childbirth in rural Nepal: a qualitative study. BMC Pregnancy Childbirth. (2015) 15:1–10. doi: 10.1186/s12884-015-0599-8
39. Atashi V, Kohan S, Salehi Z, Salehi K. Maternal-fetal emotional relationship during pregnancy, its related factors and outcomes in Iranian pregnant women: a panel study protocol. Reprod Health. (2018) 15:1–7. doi: 10.1186/s12978-018-0620-6
40. Alio AP, Kornosky JL, Mbah AK, Marty PJ, Salihu HM. The impact of paternal involvement on feto-infant morbidity among Whites, Blacks and Hispanics. Matern Child Health J. (2010) 14:735–41. doi: 10.1007/s10995-009-0482-1
41. Ghosh JKC, Wilhelm MH, Dunkel-Schetter C, Lombardi CA, Ritz BR. Paternal support and preterm birth, and the moderation of effects of chronic stress: a study in Los Angeles County mothers. Arch Women's Ment Health. (2010) 13:327–38. doi: 10.1007/s00737-009-0135-9
42. Ngui E, Cortright A, Blair K. An investigation of paternity status and other factors associated with racial and ethnic disparities in birth outcomes in Milwaukee, Wisconsin. Matern Child Health J. (2009) 13:467–78. doi: 10.1007/s10995-008-0383-8
43. Lu MC, Jones L, Bond MJ, Wright K, Pumpuang M, Maidenberg M, et al. Where is the Fin MCH? Father involvement in African American families. Ethn Dis. (2010) 20:S2–49.
44. Zeleke LB, Wondie AT, Tibebu MA, Alemu AA, Tessema MT, Shita NG, et al. Postnatal care service utilization and its determinants in East Gojjam Zone, Northwest Ethiopia: a mixed-method study. PLoS ONE. (2021) 16:e0256176. doi: 10.1371/journal.pone.0256176
45. Fisseha G, Berhane Y, Worku A, Terefe W. Distance from health facility and mothers' perception of quality related to skilled delivery service utilization in northern Ethiopia. Int J Women's Health. (2017) 9:749. doi: 10.2147/IJWH.S140366
46. Datta S, Kodali BS, Segal S. Maternal physiological changes during pregnancy, labor, and the postpartum period. In: Obstetric Anesthesia Handbook. New York, NY; Dordrecht; Heidelberg: Springer (2010), p. 1–14. doi: 10.1007/978-0-387-88602-2_1
47. Kinney M, Lawn J, Kerber K. Science in Action: Saving the Lives of Africa's Mothers, Newborns, and Children. African Science Academy Development Initiative (2009).
Keywords: lifetime, adverse outcomes, pregnancy, factors, Ethiopia
Citation: Muluneh AG, Asratie MH, Gebremariam T, Adu A, Enyew MM, Cherkos EA, Melkamu S, Berta M, Mamo W, Kassahun D, Tsega NT, Kebede AA, Asmamaw DB, Kassa GM and Mihret MS (2022) Lifetime adverse pregnancy outcomes and associated factors among antenatal care booked women in Central Gondar zone and Gondar city administration, Northwest Ethiopia. Front. Public Health 10:966055. doi: 10.3389/fpubh.2022.966055
Received: 10 June 2022; Accepted: 22 July 2022;
Published: 10 August 2022.
Edited by:
Sunjoo Kang, Yonsei University, South KoreaReviewed by:
Chalie Marew Tiruneh, Debre Tabor University, EthiopiaCopyright © 2022 Muluneh, Asratie, Gebremariam, Adu, Enyew, Cherkos, Melkamu, Berta, Mamo, Kassahun, Tsega, Kebede, Asmamaw, Kassa and Mihret. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Desale Bihonegn Asmamaw, ZGVzYWxlYmlob25lZ24xOTg4QGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.