- 1Aga Khan University, Karachi, Pakistan
- 2Centre for Medical Education, School of Medicine, Cardiff University, Cardiff, United Kingdom
- 3Department of Surgery, Washington University in St. Louis, St. Louis, MO, United States
- 4Department of Medicine, Aga Khan University, Karachi, Pakistan
- 5Department of Family Medicine, Aga Khan University, Karachi, Pakistan
- 6School of Nursing and Midwifery, Aga Khan University, Karachi, Pakistan
Objectives: During COVID-19 the re-opening of educational institutes was frequently debated, however with the decline in the number of COVID-19 cases, The Aga Khan University (AKU) in Karachi, Pakistan opened its campus for medical and nursing students after more than 6 months of closure. To ensure gradual resumption of activities on-campus, a combination of interventions was diligently deployed to minimize student infection rates. Scarce literature exists on students' perceptions regarding decisions implemented by university leadership. The aim of the study was to determine the efficacy of these interventions.
Methods: We conducted a convergent, parallel, mixed-methods observational study targeting medical and nursing students. An online questionnaire was disseminated to elicit students' degree of (dis)agreement on a four-point Likert scale. Focused group discussions (FGDs) were conducted to comprehend reasons for (dis)agreement.
Results: Total of 183 students responded to questionnaire (59.0% nursing, 67.8% female), 11 FGDs were conducted with 85 students. Interventions with highest agreement were mandatory face masks policy (94.54%), weekly mandated COVID-testing (92.35%) and students' Academic Bubble (91.26%); highest disagreement was for Sehat Check application (41.53%); and stay strong campaign (40.44%). Four themes emerged from FGDs: Effective safety interventions, Safety interventions with limited effectiveness, Utility of Sehat Check Application and Future recommendations for informing policy.
Conclusion: It is paramount to seek student-feedback at forefront of university re-opening strategy. Clear communication channels are as important as an administrative response system's robustness. Bidirectional communication channels are fundamental and requisite during ever-changing policies and regulations. Engaging student representatives in decision making or implementation processes (such as “pilot” before “roll-out”) would allow any potential issues to be managed early on. Gather real-time anonymous feedback and identify key areas that need further promulgation and those that need to be replaced with more effective ones.
Introduction
The COVID-19 pandemic has cut a swath globally, resulting in an unprecedented disruption in social, economic and educational systems. The rapid evolution of the pandemic dictated that critical decisions be made regarding the closure of educational institutions to curb the spread of disease and put a halt to soaring infection rates (1, 2). While clinical clerkships and in-person educational activities are of paramount importance to the practical learning of medical students, the Association of American Medical Colleges (AAMC) released guidelines for the immediate suspension of clinical activities on-campus in medical schools across United States (3). A similar trend also followed worldwide, with increasing concerns regarding the quality of education and practical training received by medical students, the attainment of profound clinical skills and the “imposter syndrome” (4–6). Consequently, traditional training and teaching methods have been gradually replaced by synchronous and asynchronous virtual modalities (5, 7, 8).
With the global trends of disease spiraling, one of the most contentious topics has been the re-opening of universities and campuses, while adequately ensuring effective safety measures for students returning back to campus vicinities (9–11). Since a one-size-fits-all approach cannot be effectively utilized in a global context, most educational institutions have employed a multi-pronged approach, leveraging a variety of public health strategies for reducing infection rates on campus (12).
On February 26, 2020, the first positive case of coronavirus disease (COVID-19) was identified in Pakistan (13). To counter the spread effectively, the government of Pakistan shut down all educational institutions, mosques, and leisure areas (14). All meetings and services were postponed, marriage halls closed and sporting events canceled. A full lockdown was enforced in the country on March 23, 2020 (14).
Other preventive measures included were travel restrictions, quarantine shelters, cordoning off areas, testing and contact tracing, implementation of mask, sanitizers, and social distancing, awareness campaigns, and production of ventilators (15).
With the decline in the number of COVID-19 cases in September 2020, the Federal Ministry announced a phased approach of opening educational institutions, depending on the evolving situation (16). The Aga Khan University (AKU) in Karachi, Pakistan also opened its campus for medical and nursing students after more than 6 months of closure. To ensure gradual resumption of activities on-campus, a combination of interventions was diligently deployed by the COVID-19 Command Center at AKU to minimize student infection rates. While studies (17–19) have reported data on the efficacy of such interventions, there is a dearth of literature on the perspectives of key stakeholders impacted by these policies—students themselves. All interventions impact students either positively or negatively, and therefore their perceptions are important to ensure maximum support is provided to facilitate them in their academic endeavors (20, 21).
Therefore, the aim of this present study was to explore students' perceptions around these interventions: Specifically, the research objectives were:
1. To determine the usefulness of the interventions in creating a safe and controlled environment on campus (systems-level feedback).
2. To evaluate the ability of the intervention to influence students practice of safety measures and adherence to infection-control protocols (behavior change feedback).
Methods
Study design
We selected a convergent, parallel, mixed methods study design to explore students' perceptions and degree of agreement toward usefulness of interventions to control student infection rates on campus (22–24). Prior to commencement, we obtained ethical approval by the Institutional Review Board (ERC Reference No: 2020-5640-15085).
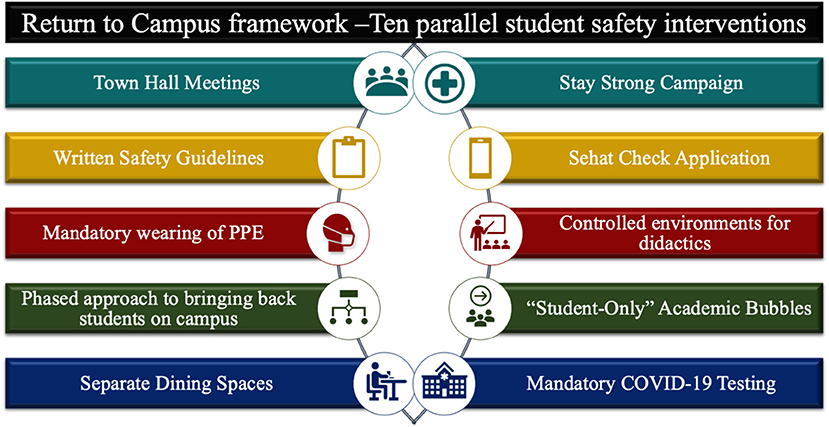
The organizational committee implemented a combination of 10 cross-cutting and concurrent interventions to create a safe and controlled environment (23) (Figure 1).
Setting and participants
The Aga Khan University Hospital is a tertiary-care, teaching hospital centered in the metropolitan city of Karachi, Pakistan (25). It offers two flagship health sciences' programs amongst other academic programs. The 5-year medical school program, comprises of pre-clinical years (Years 1–2) focusing on basic sciences, and clinical years (Years 3–5), where students are immersed in discipline-based clinical clerkships (26). Similarly, the School of Nursing and Midwifery (SONAM) offers a Bachelor of Science in Nursing (BScN), a 4-year program with the last 2 years (Years 3–4) focusing on clinical rotations (27).
Our study enrolled students in clinical years both in medical school (group A) and nursing school (group B). These cohorts were selected because they returned to campus premises following commencement of classes in mid-September, in accordance with regulations of the Ministry of Education in Pakistan (16). Using convenience sampling, all students who volunteered to participate and signed the written informed consent form participated in the study.
Interventions
The 10 interventions were developed by the COVID-19 Command Center at the Aga Khan University. This overarching governance body has representation from academic leadership, hospital and service leadership, infection prevention teams and student health teams. Student representation was integral to the development of these interventions and rigorous, continuous feedback on a regular basis. The Student Taskforce Against COVID-19 (STAC-19), a student volunteer taskforce, routinely interacted with the Command Center leadership for discussions around strategy, implementation, and feedback of these interventions (28).
The interventions can be divided into four major categories: 1. Communications and student wellbeing, 2. University strategy and hospital policy, 3. Screening application “Sehat Check” and 4. Protective measures and Testing.
Communications and student wellbeing
To ensure students' queries were aptly conveyed and acted upon, the leadership regularly met students via town-hall meetings (online/in-person). Written safety guidelines and pictorials were disseminated through emails and displayed in clinical areas and student spaces. The “Stay Strong” campaign targeted students' wellbeing by encouraging them to follow safety guidelines (via social media, socially distant gatherings, and university communications -brochures and posters) and providing access to important contact information.
University strategy and hospital policy
Every study space and academic teaching room had “Maximum Capacity” posters displayed on entrance doors to limit the number of students during didactic in-person sessions. An “Academic Bubble” was created, by restricting certain areas as student-only zones, prohibiting access to visitors and patients. A separate dining space was arranged for students (previously combined with the hospital dining space). Students returned in a staggered manner, starting with senior clinical years, followed by junior years (Year 5, then Year 4, then Year 3) with a gap of 2 weeks between consecutive batches.
Sehat check application
A novel mobile application “Sehat Check App” (Sehat = Urdu word for Health) was launched which deemed it necessary for students to screen themselves (symptom-based) regularly each morning to enter the university (29). It consisted of brief screening questions (e.g., presence of cough, fever, body aches etc. or exposure to a person with COVID). Answering “yes” to any one of the screening questions resulted in the application showing a red mark, indicating the need for further assessment and guided the user for testing purposes.
Protective measures and testing
Students were mandated to wear personal protective equipment from day one. Mandatory wearing of masks was instituted in all areas of the university and hospital. However, certain higher-risk areas such as the Emergency Room and the Endoscopy Suite, also required the additional wearing of face-shields and gowns. New face masks and face shields were biweekly distributed. Weekly mandatory COVID-19 testing was instituted (each Monday morning) to identify asymptomatic cases early on.
Quantitative component
A structured questionnaire was developed to elicit students' perceptions about the usefulness of interventions. In November and December 2020, an online questionnaire was disseminated to all students (n = 557), using a secure link provided via email. The first part of questionnaire enquired demographic details of students, level of exposure to other people based on time spent on campus, number of individuals in their household and mode of transportation. The second part of questionnaire, split into two parts consisting of 10-items each, focused on assessing the effectiveness of interventions. Students had to rate their degree of (dis)agreement on a four-point Likert Scale. All questionnaires were pilot tested, anonymized with de-identified codes assigned to each participant to maintain confidentiality.
Qualitative component
Students were invited via email to participate in focused group discussions (FGDs) to comprehend reasons for effectiveness of interventions and explore further recommended strategies. Participation in FGDs was voluntary and confidentiality of data was maintained by assigning unique de-identified codes to each participant. A semi-structured interview guide was developed, pilot tested, and six trained interviewers discussed its final version to ensure standardization. Each session spanned an hour and included between 8 and 12 students. Eleven FGDs were conducted, involving 54 medical and 31 nursing students. Data collection was completed upon thematic saturation.
Data analysis
Quantitative analysis
Data from quantitative surveys were analyzed using StataCorp. 2019 (Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC). Frequency and percentages were used to calculate the demographic characteristics and variables.
Qualitative analysis
Initially, the audio recordings from the students' discussions were transcribed. In the transcriptions, no identifying features/characteristics were included. Colaizzi's analysis method (30) was used to analyze the transcript. The analysis included steps such as familiarization, identifying significant statements, formulating meanings, clustering themes, developing an exhaustive description, producing the fundamental structure, and seeking verification of the fundamental structure. This was done through an iterative process where participants' data were coded, compared, contrasted, and refined to develop emergent themes. The transcribed text was separated into “meaningful units” which were further shortened and labeled with a “code.” Codes were then analyzed and assembled into similar categories. In the last step, comparable categories were grouped under subthemes and main themes. Two researchers were involved in independently reviewing the data and formulating the themes after summarizing and extracting the meaningful contents, bracketing the presuppositions of the researchers (using QSR NVivo—version 12, Melbourne, Australia). Any inconsistencies were solved through discussion until a mutual agreement was reached.
Results
Demographics
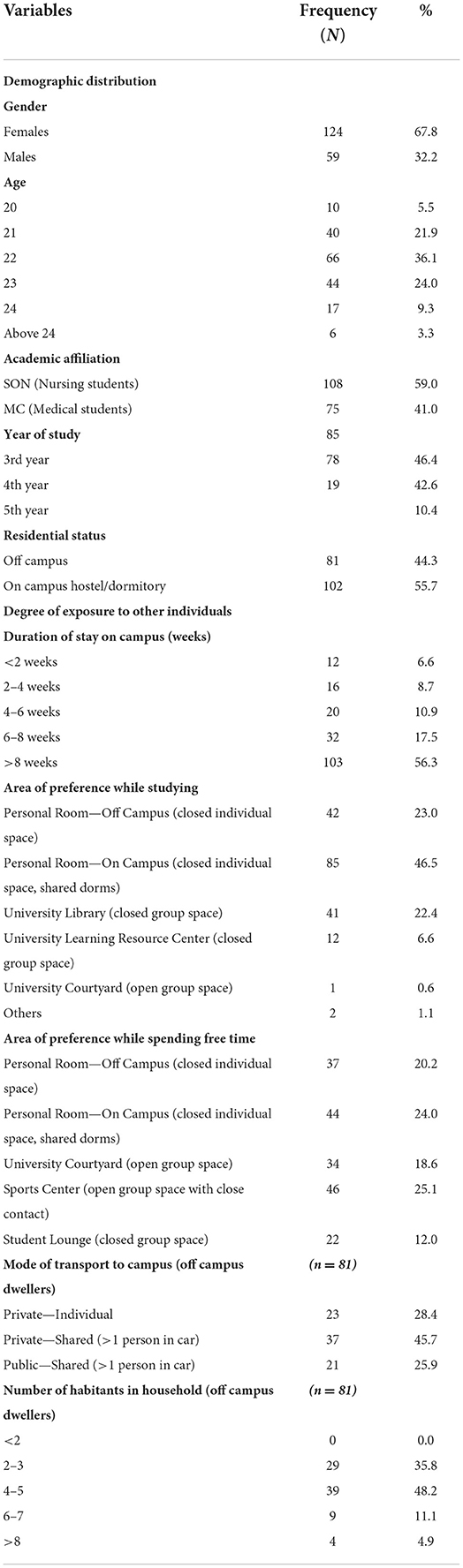
A total of 183 students completed the survey, of which 124 (67.8%) were females and 59 (32.2%) males. 108 (59.0%) nursing and 75 (41.0%) medical students participated. The highest number of students belonged to third year, 85 (46.4%), followed by fourth year 78 (42.6%). 102 (55.7%) of the students lived in campus dormitories and 81 (44.3%) lived off campus and commuted to the university daily. Of these 81 students, most students lived in households with 4–5 inhabitants 29 (35.8%) and 2–3 inhabitants 39 (48.15%). Further, 37 (45.7%) students used shared private transport and 21 (25.7%) used shared public transport to commute to campus (Table 1).
A total of 85 students participated in 11 FGDs. Six were conducted at medical college and five at school of nursing. Within these FGDs, 54 medical students from third, fourth and fifth year along with 31 nursing students from third and fourth year participated in the study.
Quantitative
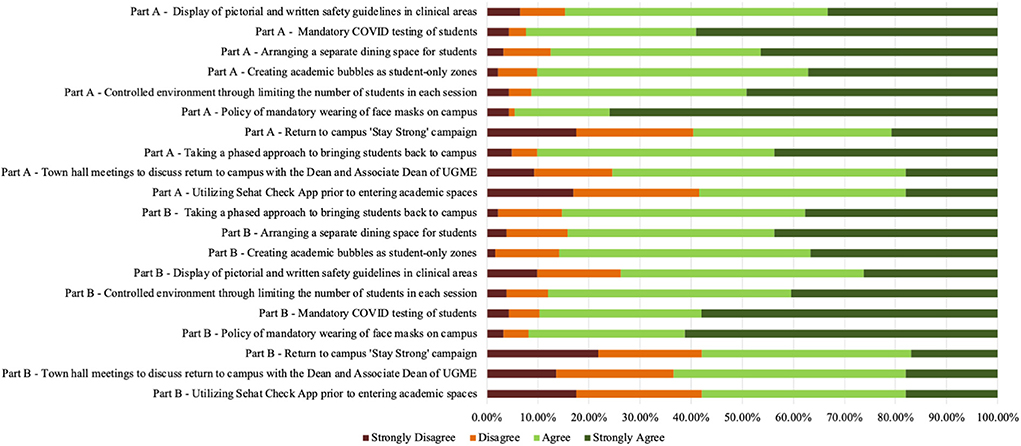
The first part of survey asked students to assess the intervention's ability to create a safe environment for infection control. Significant agreement (strongly agree and agree) was recorded for the following interventions (Figure 2): policy of mandatory wearing of face masks on campus (94.54%), weekly mandatory COVID testing of students (92.35%), limiting number of students on campus (91.26%), using a phased approach to bring students back to campus (90.17%) and creating academic bubbles as student-only safe zones (90.17%). Students showed highest disagreement toward Sehat Check application (41.53%) and stay strong campaign (40.44%).
The second part of survey focused on the contribution of intervention to respondents' practice of safety measures and adherence to infection-control protocols. Similar results were observed, with highest agreement shown for the face mask policy (91.80%), weekly mandatory COVID testing of students (89.61%) and limiting number of students in each session (87.98%). Likewise, highest disagreement was observed for the Sehat Check application (42.08%) and the Stay Strong campaign (42.08%).
Qualitative
Based on the data collection and thematic analysis, four overarching themes were identified. Table 2 shows the main themes along with their sub-themes and codes. Table 3 identifies pertinent quotations from students' verbatim.
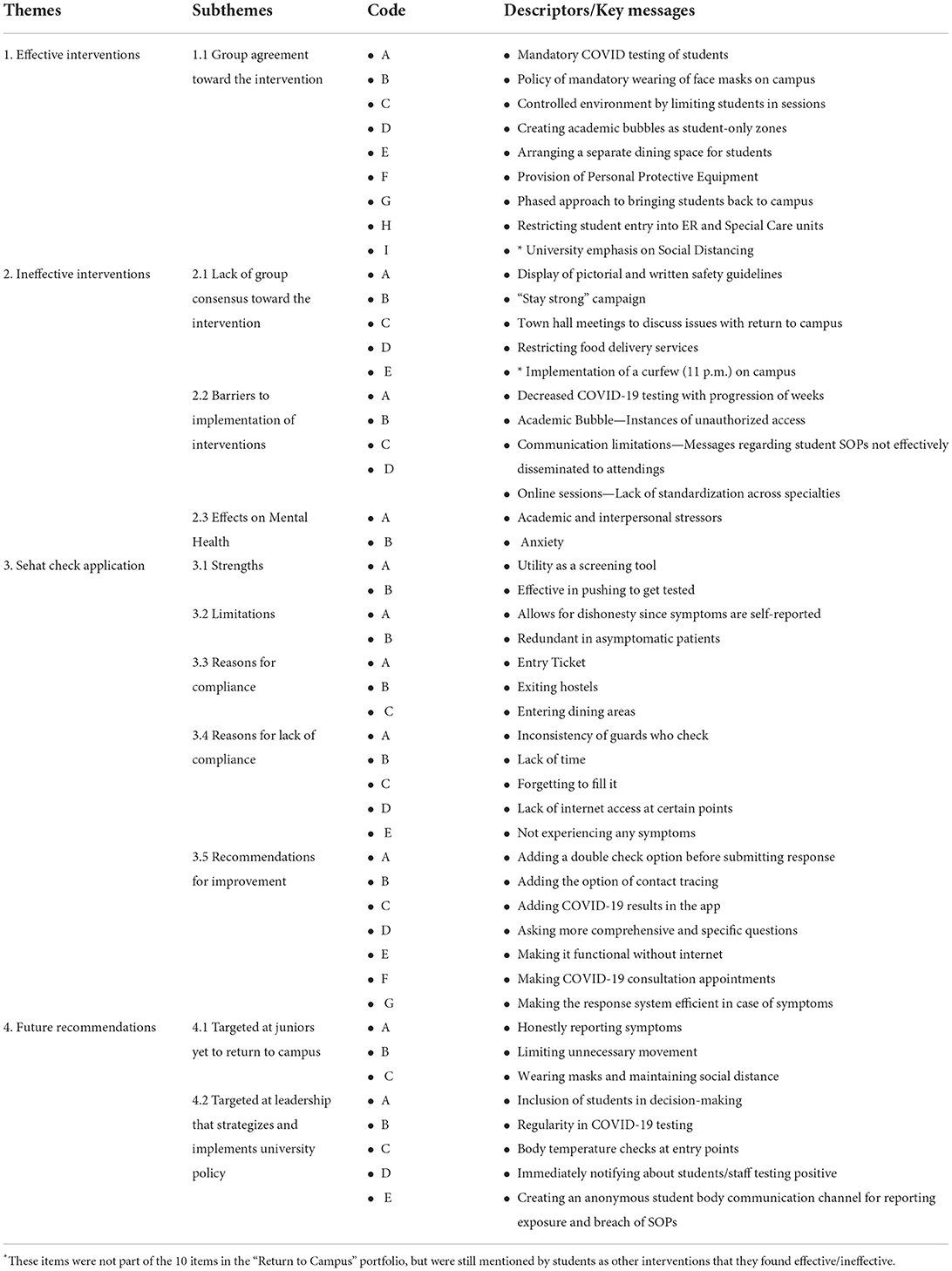
Table 2. Thematic analysis of focused group discussions with themes, sub-themes, codes, and key messages.
Effective safety interventions
Students appreciated certain safety interventions implemented by the university administration for their safe return to campus during the pandemic. Most students expressed agreement toward the weekly COVID-19 testing.
“Mandatory COVID-19 testing for students was effective in picking up asymptomatic infections which would otherwise have been missed, hence stopping the source of transmission then and there.” (5th year, MBBS student, 24 y Male)
Students mentioned that “… because most people who were infected were (actually) asymptomatic so mandatory testing was most effective in limiting spread of infection.” (3rd Year, BSCN student, 21 y Female)
With regards to subsequent effects of mask wearing policy, a student reported: “the culture created on campus of mask wearing is great. (Hence) there is peer pressure associated for patients as well as attendings.” (3rd Year, MBBS student, 22 y Male)
An important step in teaching was having classes in a hybrid online-onsite fashion. A student noted that, “online sessions along with limiting the number of people in physical sessions has also been effective but online sessions are still more preferable” (4th Year, MBBS student, 23y Female).
Safety interventions with limited effectiveness
The “Stay Strong” campaign was regarded as less effective intervention. Students claimed being well versed with SOPs regarding COVID-19 and wanted interventions translating into actions. One student stated that “the stay strong campaign was initially good for motivation, however, there are better approaches that can be taken like opening up SRC.” (5th Year, MBBS Student, 23y Male)
Some students also commented unfavorably on the restrictions placed on student spaces (specifically the policy to stay within academic bubbles after 11 p.m.). A student reported that “we are not allowed to leave the hostels after 11 p.m. But the campus is empty at that time. The main exposure that we have is during the day, in our clinics” (4th Year, MBBS Student, 23y Male).
Sehat check application
Students considered the application to be a good initiative. It prompted them to get the COVID-19 test done in case of entering relevant symptoms in the app. A student stated that “It's a brilliant innovation and a step forward in reducing the manpower and man hours required to screen everyone manually.” (3rd Year, MBBS Student, 21 male)
However, they also felt that improving the app would increase its usage and efficacy. A student suggested “You can ask me what kind of cough and its frequency. Probes leading up from generalized questions would help streamline who (should) get (the) COVID test.” (3rd Year, MBBS Student, 21 y, Female)
Students also stated that human errors while filling out application led to successive steps in the protocol that cannot be averted in time: “Once I accidently clicked yes instead of no and it showed red, and I had multiple e-mails and calls” (5th Year, MBBS Student, 24y old male). Another student recommended that “there should be a double check system in the app, like ‘are you sure' before pressing enter.” (5th Year, MBBS Student, 24y old male)
Future recommendations
Suggestions for bringing junior students back to campus mostly focused on strict adherence to SOPs. “(Juniors) need to be respectful of the fact that hard work has been put into bringing and phasing in batches, so think of the community less than the individual” (4th Year, MBBS, 23y old female).
Other ideas to inform policy for safe return to campus included initiating contact tracing systems and anonymous communication channels to report COVID-19 exposure or breach of relevant SOPs. A student proposed “more rigorous contact tracing and not associating shame with it, because most students don't approach people, they were in touch with for fear of getting them into trouble. So, an anonymous channel for safely reporting exposure would be helpful.” (5th Year, MBBS student, 24y female)
Discussion
Main findings
This study is the first account of the outcomes of 10 interventions targeting safe return of students back to campus at a large teaching hospital in Pakistan. These outcomes focus on the primary stakeholders and recipients of these interventions, students themselves, by shedding light on their perspectives around safety, usefulness of these interventions and behavior change. The results of this study center around four main findings: 1 surveys and FGDs were congruent in highlighting the three most successful interventions to be regular COVID testing, mandatory wearing of face masks at all times and a phased approach to bringing students back; 2 interventions perceived to be less effective being restrictions in student movement (both in terms of time and space), Town Hall meetings and the Stay Strong campaign; 3 need for bidirectional communication channels and feedback forums to help bolster and refine policy; and 4 feasibility of Sehat Check Application.
Interventions with highest agreement
Frequent testing can help in timely detection of COVID-19 and curbing its spread (15). Studies have shown that regular, on-campus testing for COVID-19 is a highly favorable and adhered to prevention strategy among university students (31, 32). It is associated with lowered anxiety, feeling safe on campus and satisfaction toward university administration in taking effective steps to ensure student safety (31). This is in accordance with our findings which showed that students felt content after testing negative for the infection. It also helped them make more informed decisions about meeting people and engaging in activities. As global restrictions eased (33) presently, although frequent testing is less carried out, students are encouraged to get tested if they feel any symptoms similar to COVID-19. And this facility is easily accessible to students for all hours in the university.
Wearing face masks is important for preventing the spread of COVID-19 infection in the community. About 97% students in three medical universities in Karachi held positive attitudes toward wearing face masks as a protective measure against COVID-19 (34). A vast majority of students in our study also considered the mandatory policy of wearing face masks as a robust safety measure. Considering global restrictions are eased on wearing masks, sanitization, and social distancing (35), within the university academic settings it is no longer mandatory to do so, however for all clinical rotations' students are obliged to wear masks, continue sanitization and maintain social distancing.
As per directives of the Higher Education Pakistan (HEC), students whose learning depended on in-person training and learning were brought back on campus (36). These included the clinical batches of third, fourth and fifth year students. Using a staggering approach helped acquaint each batch with the new campus SOPs while giving them adequate time to adjust. A similar approach was adopted internationally in which positive outcomes of using a phased approach to resume on campus classes were reported (37, 38).
Interventions that need reform
An emerging theme in FGDs was the unfavorable attitude of students residing in dormitories toward the curfew as they perceived on-campus exposure to be low during nighttime. Considering the university teaching hospital is attached, the curfew was there to ensure students do not leave the academic bubble and be exposed to the infection. In addition, it is more difficult to maintain infection control in hostels and any outbreaks can have serious consequences for all the residents (39). However, perhaps this was not clearly communicated to the students, and implies effective communication is needed between the leadership and students to resolve any conflicts or disagreements. In the present study, the curfew was removed once the Pakistan government lifted all COVID related restrictions (40).
In the present study, students did not favor both virtual or in person Town hall meetings held by leadership. These meetings were held to keep students informed of the actions taken by the university regarding their academics and general environment. Town hall meetings have been reported to increase students' awareness and knowledge regarding programme (41). However, students in the present study questioned its purpose. Although students were also encouraged to voice their concerns during these meetings, perhaps they felt it more as authoritarian, rather as a dialogue. Although in person town hall meetings have resumed after ease of restrictions (40), the findings of the present study imply that it's important to rethink the purpose of town hall meetings and clarify it from the perspective of students, for example to convey information, rules, and procedures, or as a means of engaging students in decision making.
With regards to “Stay Strong Campaign,” students claimed to be aware of the precautions related to COVID-19, hence they found pictorial displays of safety measures on campus to be of little value. Although this pictorial display discontinued once the pandemic eased (40), it implies as adult learners (42) students want to create meaningful interpretation of all activities. While initially this pictorial display was helpful, later it could have been replaced by a better alternative, for example, more interactive virtual content offering updated information would get better engagement or infographics depicting a selection of topics from the social and behavioral sciences relevant during a pandemic (43).
Need for communication and feedback
In the present study, students preferred to be involved in formulating policies that affected them. Presently student representation is on certain academic committees such as research and curriculum, perhaps it's time to consider how best to further engage them in academic and health policies and procedures considering their opinions will enable the administration to foresee and maximize policy impact along with ensuring stronger student compliance. As part of bidirectional communication, regular student feedback could help in giving them a sense of ownership and motivation to adhere to safety protocols. Evidence also indicates that engaging students in medical education can promote better academic and health outcomes (44, 45).
In the present study, students were not in favor of the Sehat check application. For the present study, the intent of the Sehat check application was purely observational—that is disease surveillance and limiting infection spread by informing the regulating bodies of student infection rate for preventive measures. Although the idea of a screening application was appreciated and successful in this aspect, some technical limitations hindered its potential. Numerous health applications have been developed globally in response to COVID-19 (37, 46–48). Most commonly reported limitation of these applications was lack of methodological rigor (49). In the present study students' suggestions for improving the application included asking comprehensive questions for symptom detection, features for contact tracing, and providing updated information regarding pandemic globally. Incorporating these changes can refine the application to better achieve its objective. However, following ease of restrictions (40), the screening application was discontinued and the university plans to refine it for better usage and outcomes.
Strengths
This study employed a carefully curated, multifaceted, approach to evaluate the efficacy of policies instituted and explore challenges faced by students upon returning to campus. A thorough literature search made it evident that there is a relative dearth of similar literature in the region and in developing countries. Moreover, while significant strides have been made in understanding policy experts' perspectives, a concerted effort is needed to delve into the primary stakeholders and recipients of these targeted policies -the students. Our study maintains these vital perspectives at the forefront, making it one of the first endeavors from a resource-limited setting. Our rigorous de-identification processes ensured that the feedback was anonymous, and protected. By amassing perspectives on the ability of each intervention to provide a safe environment and its effect on student behavior (self-reflected), we got valuable insights on perceptions around safety and behavioral patterns. An unexpectedly high proportion of students participated in FGDs, which further elucidates the importance of hearing and sharing the recipient side of the story. Pre-interview training of the study leads allowed standardization among different groups thereby strengthening reliability of the results. Both the execution and the assessment of our screening mobile application shed light on the scope, experiences, and efficacy of technology-driven innovations in a developing country.
Limitations
Although the target population was diverse and well-spread over five different academic years from two programs, our study was limited to a cross-sectional single setting design in an urban environment. There was a slightly suboptimal response rate (33%) which can be attributed to two possible reasons. First, with the major paradigm shift from conventional platforms to virtual ones during the pandemic, it is possible that there was an information overload on students' emails (announcements, teaching instruction and other research dissemination) leading to less responsiveness overall. Second, the survey was disseminated a few weeks after students had returned to campus, which also coincided with the time that they were catching up on the significant backlog because of the pandemic. This could have resulted in students having less time to enroll as volunteer participants in research projects. However, it is reported that response representativeness is more important than response rate in survey research and in the present study, the sample is representative of both the medical and nursing students (50). Also, the aim of the study was to explore the usefulness of these intervention to support students for their learning, and in addition to the survey based responses, focus group discussions allowed to explore in depth to address the research objectives.
Future implications
This study demarcates that mandatory COVID-19 regular testing and wearing of facemasks were the most effective interventions in curbing the spread of pandemic. In resource and time limited settings, these two key strategies should be the focus of efforts and budgeting. We also found that bidirectional communication channels are fundamental and requisite during ever-changing policies and regulations. Where possible, this needs to also gather real-time anonymous feedback and identify key areas that need further promulgation and those that need to be replaced with more effective ones. Thus, for practitioners, it is paramount to establish mechanisms to clearly communicate, implement and evaluate strategies at regular intervals. Concurrently, engaging student representatives in decision making or implementation processes (such as “pilot” before “roll-out”) would allow any potential issues to be managed early on.
Conclusion
These findings can be used to conduct further research, after a follow-up period, to implement, evaluate and categorize policies into one of many such arms: those that have long-term sustainability, those that saw attenuation after an initial peak and those that improved over time (both in terms of safety of intervention and its effect on student behavior patterns). To ensure depth and a holistic understanding, gathering faculty perspectives on the same or similar policies could follow this process. Likewise, to augment the breath of perspectives, more work should ensue on institutions spread over diverse socioeconomic and cultural setups. Bidirectional communication channels are fundamental and requisite during ever-changing policies and regulations. Engaging student representatives in decision making or implementation processes (such as “pilot” before “roll-out”) would allow any potential issues to be managed early on. Gather real-time anonymous feedback and identify key areas that need further promulgation and those that need to be replaced with more effective ones.
Practice points
1 Bidirectional communication channels are fundamental and requisite during ever-changing policies and regulations
2 Engaging student representatives in decision making or implementation processes (such as “pilot” before “roll-out”) would allow any potential issues to be managed early on.
3 Gather real-time anonymous feedback and identify key areas that need further promulgation and those that need to be replaced with more effective ones.
4 In resource and time limited settings. mandatory COVID-19 regular testing and wearing of facemasks were the most effective interventions in curbing the spread of pandemic.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Ethical Review Committee (ERC) Aga Khan University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
SM, SI, AN, RK, UI, and MT contributed to the conception and design of the study. HS, AH, NA, AJ, SZ, and KA contributed to the acquisition and interpretation of the data. All authors contributed to the write-up of early versions of the manuscript, agree accountability for the accuracy and integrity of the work and approved the final version of the submitted manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Esposito S, Principi N. School closure during the Coronavirus disease 2019 (COVID-19) pandemic: an effective intervention at the global level? JAMA Pediatr. (2020) 174:921–2. doi: 10.1001/jamapediatrics.2020.1892
2. Harries AJ, Lee C, Jones L, Rodriguez RM, Davis JA, Boysen-Osborn M, et al. Effects of the COVID-19 pandemic on medical students: a multicenter quantitative study. BMC Med Educ. (2021) 21:14. doi: 10.1186/s12909-020-02462-1
3. Association of American Medical Colleges. Important Guidance for Medical Students on Clinical Rotations During the Coronavirus (COVID-19) Outbreak [press release]. Association of American Medical Colleges (2020).
4. Ahmed H, Allaf M, Elghazaly H. COVID-19 and medical education. Lancet Infect Dis. (2020) 20:777–8. doi: 10.1016/S1473-3099(20)30226-7
5. Dedeilia A, Sotiropoulos MG, Hanrahan JG, Janga D, Dedeilias P, Sideris M. Medical and surgical education challenges and innovations in the COVID-19 era: a systematic review. In Vivo. (2020) 34(3 Suppl.):1603–11. doi: 10.21873/invivo.11950
6. Farooq F, Rathore FA, Mansoor SN. Challenges of online medical education in Pakistan during COVID-19 pandemic. J Coll Physicians Surg Pak. (2020) 30:67–9. doi: 10.29271/jcpsp.2020.Supp1.S67
7. Noorali AA, Inam M, Shahbaz H, Rauf H, Aamir FB, Khalid F, et al. A nationwide virtual research education program for medical students in Pakistan: methodological framework, feasibility testing, and outcomes. Front Public Health. (2021) 9:812130. doi: 10.3389/fpubh.2021.812130
8. Reinholz M, French LE. Medical education and care in dermatology during the SARS-CoV2 pandemia: challenges and chances. J Eur Acad Dermatol Venereol. (2020) 34:e214–6. doi: 10.1111/jdv.16391
9. Cheng SY, Wang CJ, Shen AC, Chang SC. How to safely reopen colleges and universities during COVID-19: experiences from Taiwan. Ann Intern Med. (2020) 173:638–41. doi: 10.7326/M20-2927
10. Edmunds WJ. Finding a path to reopen schools during the COVID-19 pandemic. Lancet Child Adolesc Health. (2020) 4:796–7. doi: 10.1016/S2352-4642(20)30249-2
11. Yamey G, Walensky RP. COVID-19: re-opening universities is high risk. BMJ. (2020) 370:m3365. doi: 10.1136/bmj.m3365
12. Bradley EH, An MW, Fox E. Reopening colleges during the Coronavirus disease 2019 (COVID-19) pandemic-one size does not fit all. JAMA Netw Open. (2020) 3:e2017838. doi: 10.1001/jamanetworkopen.2020.17838
13. Government of Pakistan. Pakistan Statistical Year Book 2018 (Provisional). Islamabad: Bureau of Statistics: Government of Pakistan [2020-03-16] (2018).
14. Abid K, Bari YA, Younas M, Tahir Javaid S, Imran A. Progress of COVID-19 epidemic in Pakistan. Asia Pac J Public Health. (2020) 32:154–6. doi: 10.1177/1010539520927259
15. Akhtar H, Afridi M, Akhtar S, Ahmad H, Ali S, Khalid S, et al. Pakistan's response to COVID-19: overcoming national and international hypes to fight the pandemic. JMIR Public Health Surveill. (2021) 7:e28517. doi: 10.2196/28517
16. Ali I. Educational institutions to reopen countrywide in phases from Sept 15 - Pakistan [press release]. Dawn News. Islamabad: Dawn (September 7, 2020).
17. Woolliscroft JO. Innovation in response to the COVID-19 pandemic crisis. Acad Med. (2020) 95:1140–2. doi: 10.1097/ACM.0000000000003402
18. Ross DA. Creating a “quarantine curriculum” to enhance teaching and learning during the COVID-19 pandemic. Acad Med. (2020) 95:1125–6. doi: 10.1097/ACM.0000000000003424
19. Papapanou M, Routsi E, Tsamakis K, Fotis L, Marinos G, Lidoriki I, et al. Medical education challenges and innovations during COVID-19 pandemic. Postgraduate Med J. (2022) 98:321–7. doi: 10.1136/postgradmedj-2021-140032
20. Lin Y, Kang YJ, Lee Hj, Kim D-H. Pre-medical students' perceptions of educational environment and their subjective happiness: a comparative study before and after the COVID-19 pandemic. BMC Med Educ. (2021) 21:619. doi: 10.1186/s12909-021-03065-0
21. Klasen JM, Schoenbaechler Z, Bogie BJM, Meienberg A, Nickel C, Bingisser R, et al. Medical students' perceptions of learning and working on the COVID-19 frontlines: '… a confirmation that I am in the right place professionally'. Med Educ Online. (2022) 27:2082265. doi: 10.1080/10872981.2022.2082265
22. Curry LA, Krumholz HM, O'Cathain A, Plano Clark VL, Cherlin E, Bradley EH. Mixed methods in biomedical and health services research. Circ Cardiovasc Qual Outcomes. (2013) 6:119–23. doi: 10.1161/CIRCOUTCOMES.112.967885
23. Kimmons R. Mixed methods. In: Education Research EdTech Books. (2022). Available online at: https://edtechbooks.org/education_research/mixed_methods (accessed May 25, 2022).
24. Schifferdecker KE, Reed VA. Using mixed methods research in medical education: basic guidelines for researchers. Med Educ. (2009) 43:637–44. doi: 10.1111/j.1365-2923.2009.03386.x
25. The Aga Khan University Hospital MC Karachi. (2022). Available online at: https://hospitals.aku.edu/pakistan/karachi/Pages/default.aspx (accessed May 25, 2022).
26. The Aga Khan University. Bachelor of Medicine BoS-UPMC, Pakistan. (2022). Available online at: https://www.aku.edu/mcpk/undergraduate/Pages/mbbs.aspx (accessed May 24, 2022).
27. The Aga Khan University. Bachelor of Science in Nursing | School of Nursing & Midwifery PIcJ. Available online at: https://www.aku.edu/sonampk/Pages/home.aspx (accessed May 24, 2022).
28. Ehsan AN, Noorali AA, Ahmed KS. Social incubation in Pakistan: enabling student mobilization during the COVID-19 pandemic. J Pak Med Assoc. (2022) 72:384. doi: 10.47391/JPMA.4786
29. University AK. AKUH Sehat Check App - User Guide for Students. (2020). Available online at: https://www.aku.edu/students/Documents/Sehat Check App - UserGuide Student.pdf
30. Colaizzi PF. Psychological research as the phenomenologist views it. In: Valle RS, King M, editors. Existential-Phenomenological Alternatives for Psychology. Oxford University Press (1978). p. 6.
31. Blake H, Corner J, Cirelli C, Hassard J, Briggs L, Daly JM, et al. Perceptions and experiences of the University of Nottingham pilot SARS-CoV-2 asymptomatic testing service: a mixed-methods study. Int J Environ Res Public Health. (2020) 18:188. doi: 10.3390/ijerph18010188
32. Gillam TB, Cole J, Gharbi K, Angiolini E, Barker T, Bickerton P, et al. Norwich COVID-19 testing initiative pilot: evaluating the feasibility of asymptomatic testing on a university campus. J Public Health. (2021) 43:82–8. doi: 10.1093/pubmed/fdaa194
33. Stokel-Walker C. COVID restrictions are lifting - what scientists think. Nature. (2022) 603:563. doi: 10.1038/d41586-022-00620-7
34. Ahmed N, Khan A, Naveed HA, Moizuddin SM, Khan J. Concerns of undergraduate medical students towards an outbreak of COVID-19. Int J Curr Med Pharm Res. (2020) 6:17. doi: 10.24327/23956429.ijcmpr202003863
35. Han E, Tan MMJ, Turk E, Sridhar D, Leung GM, Shibuya K, et al. Lessons learnt from easing COVID-19 restrictions: an analysis of countries and regions in Asia Pacific and Europe. Lancet. (2020) 396:1525–34. doi: 10.1016/S0140-6736(20)32007-9
36. Strategy for Gradual Reopening of Higher Education Institutes. Higher Education Commission (Pakistan). (2022). Available online at: https://hec.gov.pk/english/HECAnnouncements/Documents/nCoVirus/Reopening-of-HEIs.pdf (accessed May 25, 2021).
37. Intawong K, Olson D, Chariyalertsak S. Application technology to fight the COVID-19 pandemic: lessons learned in Thailand. Biochem Biophys Res Commun. (2021) 534:830–6. doi: 10.1016/j.bbrc.2020.10.097
38. Rennert L, Kalbaugh CA, McMahan C, Shi L, Colenda CC. The impact of phased university reopenings on mitigating the spread of COVID-19: a modeling study. BMC Public Health. (2021) 21:1520. doi: 10.1186/s12889-021-11525-x
39. Lewer D, Braithwaite I, Bullock M, Eyre MT, White PJ, Aldridge RW, et al. COVID-19 among people experiencing homelessness in England: a modelling study. Lancet Respir Med. (2020) 8:1181–91. doi: 10.1016/S2213-2600(20)30396-9
41. Comp G, Townley K, Blazar E, Webb T, Keuchel M, Bhattarai B, et al. Virtual town hall meetings to convey emergency medicine residency program information to students. West J Emerg Med. (2022) 23:525–31. doi: 10.5811/westjem.2022.4.54637
42. Knowles MSea. The Adult Learner: The Definitive Classic in Adult Education and Human Resource Development. 7th ed. Oxon: Routledge (2012).
43. Bavel JJV, Baicker K, Boggio PS, Capraro V, Cichocka A, Cikara M, et al. Using social and behavioural science to support COVID-19 pandemic response. Nat Human Behav. (2020) 4:460–71. doi: 10.1038/s41562-020-0884-z
44. Geraghty JR, Young AN, Berkel TDM, Wallbruch E, Mann J, Park YS, et al. Empowering medical students as agents of curricular change: a value-added approach to student engagement in medical education. Perspect Med Educ. (2020) 9:60–5. doi: 10.1007/s40037-019-00547-2
45. Gonzalo JD, Dekhtyar M, Hawkins RE, Wolpaw DR. How can medical students add value? Identifying roles, barriers, and strategies to advance the value of undergraduate medical education to patient care and the health system. Acad Med. (2017) 92:1294–301. doi: 10.1097/ACM.0000000000001662
46. Islam MN, Islam I, Munim KM, Islam A. A review on the mobile applications developed for COVID-19: an exploratory analysis. IEEE Access. (2020) 8:145601–10. doi: 10.1109/ACCESS.2020.3015102
47. Timmers T, Janssen L, Stohr J, Murk JL, Berrevoets MAH. Using eHealth to support COVID-19 education, self-assessment, and symptom monitoring in the Netherlands: observational study. JMIR Mhealth Uhealth. (2020) 8:e19822. doi: 10.2196/19822
48. Zhang H, Dimitrov D, Simpson L, Plaks N, Singh B, Penney S, et al. A web-based, mobile-responsive application to screen health care workers for COVID-19 symptoms: rapid design, deployment, and usage. JMIR Form Res. (2020) 4:e19533. doi: 10.2196/19533
49. Kondylakis H, Katehakis DG, Kouroubali A, Logothetidis F, Triantafyllidis A, Kalamaras I, et al. COVID-19 mobile apps: a systematic review of the literature. J Med Internet Res. (2020) 22:e23170. doi: 10.2196/23170
Keywords: feedback, medical education research, public health, COVID-19, mixed-methods study, medical students, nursing-education
Citation: Mahmood S, Ijaz Haider S, Shahbaz H, Noorali AA, Afzal N, Jiwani A, Zaki S, Iqbal Khan U, Ajani K, Tariq M, Karmaliani R and Haider AH (2022) The impact of COVID-19 safety interventions on creating a controlled environment on campus. Front. Public Health 10:962478. doi: 10.3389/fpubh.2022.962478
Received: 06 June 2022; Accepted: 29 August 2022;
Published: 23 September 2022.
Edited by:
Surapaneni Krishna Mohan, Panimalar Medical College Hospital and Research Institute, IndiaReviewed by:
Ihua Chen, Qufu Normal University, ChinaVasuki R., Yonsei University Health System, South Korea
Copyright © 2022 Mahmood, Ijaz Haider, Shahbaz, Noorali, Afzal, Jiwani, Zaki, Iqbal Khan, Ajani, Tariq, Karmaliani and Haider. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sonia Ijaz Haider, ZHJzb25pYWhhaWRlckBnbWFpbC5jb20=
 Sana Mahmood1
Sana Mahmood1 Sonia Ijaz Haider
Sonia Ijaz Haider Ali Aahil Noorali
Ali Aahil Noorali Noreen Afzal
Noreen Afzal Samar Zaki
Samar Zaki