
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 05 October 2022
Sec. Public Mental Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.962083
This article is part of the Research TopicThe Importance of the Body-Mind Relationship in Mental Functioning and Development of Body-Focused Disorders in AdolescenceView all 9 articles
Objective: Weight issues, dysmorphic concerns and eating disorders are common among individuals with polycystic ovary syndrome (PCOS) and are linked to poor quality of life (QoL). The goal of the current study was to examine whether the association between body mass index (BMI) and QoL was mediated by dysmorphic concerns, examining also the relations with eating disorder symptomatology.
Methods: Questionnaires were administered to 435 individuals with PCOS aged between 18 and 40 years (M = 27.62; SD = 4.83) to measure dysmorphic concerns, eating disorder symptoms and QoL. Participants were also asked to report their height and weight to compute their BMI.
Results: Structural equation modeling was used to observe the relationship between the variables. The results revealed a direct relationship between QoL, BMI, dysmorphic concerns and eating disorder symptomatology. In addition, dysmorphic concerns were related to BMI and eating disorder symptomatology. Furthermore, the results showed the mediating role of dysmorphic concerns and eating disorder symptoms in the relationship between BMI and QoL.
Conclusion: The current results highlight the potential importance of harmful relationships with one's own body and food, explaining why weight issues may be linked to different levels of QoL in PCOS individuals. The implications of these findings are discussed.
Polycystic ovary syndrome (PCOS) is a disabling endocrinopathy affecting approximately 6–10% of women of childbearing age (1). The condition is multifactorial and often difficult to diagnose due to the existence of different diagnostic criteria (2), mainly based on the presence of a combination of clinical signs of anovulation or menstrual irregularities, polycystic ovaries and androgen excess (3). Weight management issues exacerbate the clinical significance of the disease, leading to important clinical concerns such as diabetes and cardiovascular disease (4, 5). Not surprisingly, research has shown that weight problems are among the most burdening symptoms of this condition, whereas others, such as infertility or menstrual irregularity, have a moderately negative impact on individuals' quality of life (QoL) (6).
Past findings showed how patients with PCOS are more likely to be overweight compared to controls and that PCOS is common in obese women (7, 8). Likewise, previous research has found that the prevalence of PCOS in women with weight problems is about 25% and it is widespread in patients undergoing bariatric surgery (9, 10). The research emphasized how a problematic body mass index (BMI) may foster a negative self-view (11–13) and may negatively influence one's own perceived body image. For instance, past findings showed how BMI is related to dissatisfaction with one's own body in both normal (14–17) and clinical populations (12, 18); furthermore, longitudinal research (19) revealed that BMI was a risk factor for decreased body satisfaction at the time of initial assessment and 5 years later.
Adherence to a healthy lifestyle, namely, proper nutrition and adequate physical activity, is therefore an important part of optimal PCOS management (20). Thus, lifestyle interventions focused on weight and diet to reduce symptoms and improve health outcomes have been indicated as first-line treatment for individuals with PCOS (20). However, previous research observing these kinds of treatments suggested that they provide small or short-term effects (21). It is thus necessary to identify alternative target areas to improve their clinical efficacy.
Given that people with PCOS who have a high BMI are more likely to report poor health status (22, 23) and that having a problematic body weight can lead to fear of social evaluation and perceptions of flaws in appearance (24–26), it is reasonable to assume that dysmorphic concerns are likely to occur.
Dysmorphic concerns refer to perceived aesthetic flaws and the use of strategies to disguise them, withdrawal from social events due to appearance concerns and also reassurance-seeking about one's own appearance from significant others (27). While body dissatisfaction refers to a negative subjective evaluation of a person's physical body size and/or shape (28–30), dysmorphic concern is a more specific concept that encapsulates not only behavioral, emotional, and cognitive components related with negative body image (27, 31) but also the presence of maladaptive behaviors aimed at altering one's body (32, 33). One of the components of dysmorphic concerns is in fact the presence of potentially harmful behaviors aimed at altering the body through excessive fasting and physical exercise, performance enhancing substances, engaging in excessive grooming, and undergoing cosmetic surgical treatments (34, 35). As such, dysmorphic concerns entail distorted beliefs that one's body is defective that lead to marked social withdrawal (32, 33) and they seem more recurrent in women (36). Previous findings showed a strong association between PCOS and dysmorphic concerns (37–39), and showed that patients with PCOS have worse dysmorphic concerns than individuals without this condition (37). In particular, concerns about weight have been identified as a major component of self-perceived impairment in patients with PCOS (20). In effect, negative thoughts and feelings, such as those associated with dysmorphic concerns, are closely related to impaired QoL (40). The nature of the relationship between dysmorphic concerns and QoL in individuals with PCOS was examined in a meta-analysis by Bazarganipour et al. (41), who found that QoL impairment was exerted by dysmorphic concerns through a significant link with the physical manifestations of hyperandrogenism. Furthermore, dysmorphic concerns have been correlated to a variety of risk factors for poor QoL in people with PCOS, including appearance evaluation, body area satisfaction, overweight preoccupation and higher self-classified weight (42, 43).
Of note, body image disturbances such as dysmorphic concerns are key components of eating disorders (44, 45). Eating disorders are a set of pathologies based on abnormal food intake and preoccupation with weight that can hinder a person's functioning (46). The burden of eating disorder symptomatology on many spheres of a person's life is well documented, with studies revealing diminished interpersonal functioning (47, 48) and increased morbidity and healthcare costs (49). It is thus reasonable to argue that more severe eating disorder symptoms may be positively related to worsened QoL. A connection between PCOS and eating disorders has been suggested by a few studies (50) and some insights have shown that individuals with PCOS display altered dietary intakes and higher odds of presenting with food cravings (42–45, 47–52). For instance, Bernadett and Szemán (53) underlined that the prevalence of clinical and subclinical bulimia nervosa is higher among individuals with PCOS compared to controls. In addition, those with PCOS appear to be more likely to report food restriction and weight concerns, which are also key factors in eating disorders, compared with healthy individuals (50, 54, 55). The development of disordered eating in individuals with PCOS seems to be significantly linked to distorted perceptions and beliefs about one's own body image (56–58). In particular, body self-evaluation and drive for thinness appear to be among the most prominent components in the maintenance and development of eating disorders, even in individuals with PCOS (59, 60).
The above studies underline how interactions between biopsychosocial factors may account for different levels of QoL in individuals with PCOS. There is, in fact, good evidence that body dissatisfaction and/or eating-disordered behavior mediate the association between (elevated) BMI and impairment in quality of life among both women and men in the general population and among both young people and adults (29, 61) and thus is reasonable to infer that said interactions are likely to occur in individuals with PCOS as well. Indeed, it has been highlighted that BMI is a biological dimension that is closely associated with lower body dissatisfaction (62, 63), thereby suggesting that problematic body fatness may constitute a plausible antecedent accounting for individual variation in the preoccupation with one's own physical characteristics (25, 64) and thus dysmorphic concerns. Dysmorphic concerns are in fact a constellation of preoccupations with perceived defects in one's own body that previous findings have shown to foster harmful relationships with food and weight management.
PCOS, as a chronic condition associated with unhealthy BMI and several psychosocial impairments (65–67), is thought to impair one's own QoL. For these reasons, the aim of the current study is to test the hypothesis that an association between BMI and QoL in women with PCOS would be mediated by dysmorphic concerns, examining also the relations with eating disorder symptomatology. Specifically, the goal of this research was to test a model in which higher BMI predicts higher levels of dysmorphic concerns, which in turn lead to higher levels of eating disorder symptomatology that consequently lowers the QoL. It is also expected that higher BMI and dysmorphic concerns predict lower QoL.
Questionnaires were administered to 435 individuals with PCOS aged between 18 and 40 years (M = 27.62; SD = 4.83).
Polycystic Ovary Syndrome Health-Related Quality of Life Questionnaire (PCOSQ; (68)). It is a self-report questionnaire designed to s assess specifically the QoL of individuals with PCOS. The questionnaire consists of 26 items that investigate the impact of the disease on several aspects of one's quality of life (e.g., “Concerned with infertility problems”). Individuals must respond on a seven-point Likert scale (7 = optimal function, 1 = poorest function). High scores indicate good HRQoL. In our study, Cronbach's alpha was 0.91.
Eating Attitudes Test [EAT-26; (69)]. It is a 26-item self-report questionnaire designed to assess eating disorders symptomatology (e.g., “I am terrified about being overweight”). Participants are asked to respond using a six-point Likert scale ranging from zero (= “Never”) to five (= “Always”). High scores indicate abnormal eating behaviors. In our study, Cronbach's alpha was 0.88.
Italian Body Image Concern Inventory (I-BICI; (31)). It is a self-report questionnaire that evaluates dysmorphic concerns (e.g.: “I spend a significant amount of time checking my appearance in the mirror”). Participants are asked to respond on a five-point Likert-type scale ranging from one (= “Never”) to five (= “Always”). Higher scores indicate greater dysmorphic concerns. This questionnaire was widely used to assess PCOS patients (70–72) and it was previously used in cross-sectional research in the Italian context to observe dysmorphic concerns (73, 74). In our study, Cronbach's alpha was 0.93.
The protocol was created using an online survey and participants were recruited through social networks by targeted posts on individuals suffering from PCOS in thematic groups from 21 December 2021 to 22 March 2022. Inclusion criteria were: having physician-diagnosed PCOS for at least 1 year, being ≥18 years of age and being able to speak Italian. Participants were considered ineligible if the following were present: lack of a PCOS diagnosis from a health professional, the presence of gynecological or endocrinological comorbidities, pregnant at the moment of protocol administration, insufficient fluency in Italian or < 18 years of age.
All participants declared that they voluntarily participated in the research and filled out the questionnaire anonymously, with consent implied by submission. The protocol took about 30 minutes to be completed. All questions in the survey were set as mandatory, hence there were no missing answers. The data were then analyzed using IBM SPSS and RStudio. This study was conducted in accordance with the recommendations of the ethical code of the Italian Association of Psychology (AIP) and the ethical standards described in the 1964 Declaration of Helsinki. The materials and procedures used in this study were approved by the Ethical Committee for Scientific Research at the authors' institution (Ethics Committee Num. 36360).
A hybrid Structural Equation Modeling (SEM), with BMI as an observed variable and dysmorphic concerns, eating disorders, and QoL as latent variables was used to examine a model in which BMI is considered the predictor variable, dysmorphic concerns the first mediator, eating disorders the second mediator, and QoL the outcome.
A parceling approach to obtain the indicators of the latent variables present in the current model was used, which consists of the aggregation of items (randomly selected) from the questionnaires in three indicators of each latent variable (75). Parcels are more likely to meet the assumptions of normality and less likely to be influenced by method effects (75, 76). The lavaan Package for R with the integration of RStudio were used to carry out the analysis of the covariance matrices and solutions were generated on the basis of maximum-likelihood estimation.
Fifty nine percentage of the sample was on medication and median duration of PCOS diagnosis was 7.43 (5.69) years. Most of the individuals had medium-high educational qualifications. Specifically, 39% had a high school diploma, 56% had a university degree, and 2% had a post-graduate degree, whilst the remaining 3%, had a middle school certification. Concerning occupational status, 45% were employed, 14% were self-employed, 33% were students, 7% were unemployed, and 1% were housewives. With regard to marital status, 31% of individuals were single, 27% were engaged, 25% were living with a partner, 16% of individuals were married, and 1% were divorced. Furthermore, the participants reported having the following symptoms associated with PCOS: 88% had an irregular cycle, 75% had hirsutism, 58% were overweight or had difficulty maintaining a healthy weight, 55% had acne, 32% had infertility problems, and 21% had alopecia. Finally, concerning BMI, 57% had normal weight, 23% were overweight, 11% had obesity class I, 6% had obesity class II, and 3% had obesity class III (Table 1).
The values of skewness and kurtosis were examined to explore the distribution of the data (Table 2), suggesting that no problems were observed regarding the violation of the normal distribution. Furthermore, Table 2 shows the correlations among the dimensions of the questionnaires. Furthermore, Table 2 illustrates the correlations among the observed dimensions. BMI positively correlated with dysmorphic concerns and eating disorders, while negatively related with HRQoL. Furthermore, a positive association was found between dysmorphic concerns and eating disorders, while a negative correlation was observed between dysmorphic concerns and HRQoL. Finally, there was a negative correlation between eating disorders and HRQoL.
The model showed acceptable fit indices: χ2(30) = 167.93; p < 0.001, CFI =0.95, RMSEA =0.10 (90% CI =0.09 −0.12), SRMR =0.04 (Figure 1).
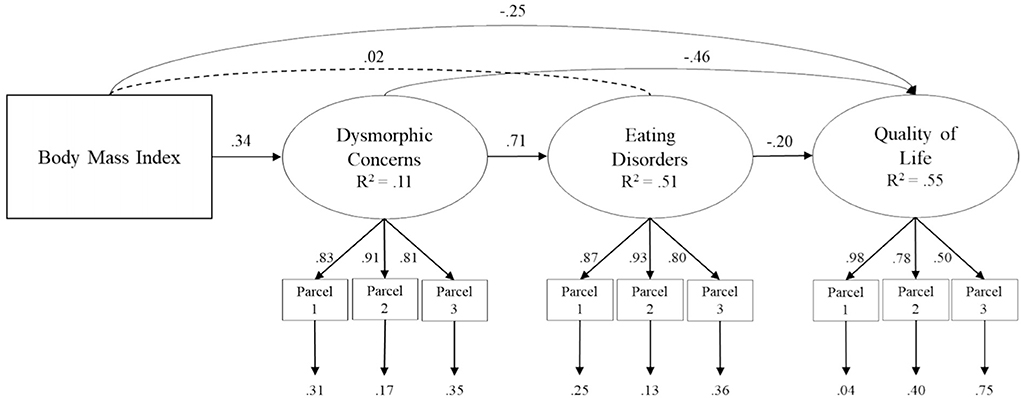
Figure 1. Structural model of association between body mass index, dysmorphic concerns, eating disorder and quality of life of life in individuals with PCOS. Coefficient shown are standardized path coefficients. Dotted lines represent not significance relations.
Significant paths were found from BMI to dysmorphic concerns (β = 0.34; p < 0.001) and HRQoL (β = −0.25; p < 0.001). Furthermore, the results showed a significant path from dysmorphic concerns to eating disorders (β = 0.71; p < 0.001) and HRQoL (β = −0.46; p < 0.001). Finally, eating disorders was related to HRQoL (β = −0.20; p < 0.001).
To explore the significance of the indirect effects that emerged (i.e., drop from the total to direct effect) we used the bootstrap-generated bias-corrected confidence interval approach (77, 78). A statistically significant indirect association was found from BMI to eating disorders by dysmorphic concerns (β = 0.24; p < 0.001) and from BMI to HRQoL by dysmorphic concerns (β = −0.15; p < 0.001). In addition, there was a significant indirect association from dysmorphic concerns to HRQoL by eating disorders (β = −0.14; p < 0.001). Finally, a statistically significant indirect relationships was found from BMI to HRQoL by dysmorphic concerns and eating disorders (β = −0.05; p = 0.002) (Table 3).
The current study tested a mediation model in which the relationship between BMI and QoL in individuals with PCOS is mediated by dysmorphic concerns, examining also the relations with eating disorders. In line with the expectations, the results showed that BMI was related to QoL not only directly but also indirectly through the mediation of dysmorphic concerns. In line with other studies supporting the relationship between body weight and body dissatisfaction (79, 80), the present findings corroborate the concept that excess body weight is one of the main factors contributing to impaired physical and mental functioning (81) and highlight how dissatisfaction with some aspect of one's own appearance contributes to shaping self-reported health status (82, 83). This may be due to the fact that a higher BMI fosters weight stigma and discrimination (84–86), which in turn may encourage social alienation and loneliness and thus decreased psychosocial adjustment. It may also be that weight problems due to PCOS negatively influence thoughts about attractiveness (87) and thus concerns about one's own potential appearance flaws are likely to occur.
Moreover, the present findings showed that individuals with PCOS reported lower QoL when dysmorphic concerns and eating disorders were higher because greater dysmorphic concerns involve fear of others' evaluations and constant approval-seeking, predisposing the person to a sense of incompetence and diminished social functioning (88–92). At the same time, given that eating disorder symptomatology impairs several dimensions of one's own functioning (47, 48), a lowered QoL is likely to occur. These results confirmed a plausible role for both variables in defining different levels of QoL and deepened their effects in the context of a burdensome condition such as PCOS. Furthermore, these findings support the hypothesis that BMI is connected to one's own QoL via the mediation of both dysmorphic concerns and eating disorders. Women with PCOS are more likely to have problems losing weight due to the metabolic features of the disease (93) and to have other comorbidities, including acne and hirsutism, which can cause dysmorphic concerns (39). These may foster maladaptive compensatory strategies used as a means of controlling food intake and body size, such as eating disorders. In the long run, this may alter individuals' functioning and result in impaired social, physical and mental adjustment. Moreover, the results of this study show that dysmorphic concerns, in addition to an indirect association with QoL by eating disorder symptomatology, have a direct link with this outcome dimension. Apprehensions of perceived defects in appearance may lead to increased dietary restriction and the use of compensatory strategies aimed at controlling body size and shape (73, 79, 94), contributing to an increased likelihood of disordered eating behaviors (79, 94). Consonant with previous findings revealing the direct link between body image dissatisfaction and disordered eating in women with PCOS (37, 57), the present study also found that dysmorphic concerns were related to eating disorder-related symptomatology. PCOS is often associated with a body shape that is culturally described as undesirable due to difficulties in weight management, which may lead individuals to undertake unhealthy dieting behaviors in an attempt to adhere to the idealized slim female figure, believed to be sexually attractive and healthy (63, 95, 96). In the long run, this may favor maladaptive eating habits used as a means for shaping one's own body (97). Overall, the results of the present study are consistent with the insights provided by Dokras et al. (98), who showed that health-related QoL scores are consistently reduced in PCOS, with difficulties in weight management playing a significant role in determining this condition. Interestingly, these results are consonant with recent advances that postulated from a biopsychosocial perspective that upregulated activation of the central HPG axis leading to PCOS may be epigenetically altered by abnormal eating patterns (55). Additionally, problematic body size, which typically denotes abnormal eating patterns, may hinder normal appetite signaling regulated by leptin and ghrelin, two important hormones controlling hunger and fullness (55). The present research has some limitations. First, it is a cross-sectional study, therefore future research could attempt to verify the findings and the direction of the hypothesized associations using a longitudinal design. Furthermore, the exclusive use of self-reports may introduce measurement bias and future studies may want to use a multi-informant approach to reduce this possibility. In addition, the research was conducted by reaching participants through social networks, so there may be problems with generalization in that only individuals with access to the Internet could be reached. It should be noted that the current results showed a higher number of women with problematic body sizes than those reported in a recent study based on the Italian population (99), which reported that the prevalence of obesity is about eight percent and 30 percent for overweight. PCOS often results in difficulties with weight management (7, 8), and this may partially explain the higher number of individuals with PCOS who reported overweight or obesity. Of note, the current study did not account for the different phenotypes of PCOS and focused only on the presence of dysmorphic concerns and eating disorder symptoms in this clinical population. Future studies should replicate this model for different PCOS phenotypes in order to provide a more nuanced description of the disease. Furthermore, although our study reported the number of participants currently on medication, it did not take into account important factors such as the type of medication used and adherence to the treatment plan. Future studies are needed in which the influence of drug treatment on individual quality of life is also observed. However, our study advances the current state of knowledge by explaining the relationships between BMI and QoL in individuals with PCOS. It would be thought-provoking to implement future studies in which a retrospective approach is used to observe the potential influence of the COVID-19 pandemic scenario (100, 101) because recent findings observed that during isolation due to the COVID-19 outbreak, weight gain was slightly more pronounced in individuals suffering from PCOS and this may be due to impaired sleep quality and eating habits rather than reduced physical activity (102). In a similar vein, future studies may assess how different eating patterns ad caloric restriction protocols like ketogenic diet (103, 104) may interact with individuals' perception of the condition of their own health. Similarly, future studies may benefit from the implementation of other biological variables, such as energy expenditure and fat mass (105), as they may influence adaptations of metabolism and body composition. More importantly, this study contributes to the evidence by investigating the role that dysmorphic concerns and eating disorder symptomatology may have in explaining the individual differences in the association between BMI and QoL in individuals with PCOS. In light of the findings of this study, there may be important clinical and research implications. This study highlights how people with PCOS and problematic weight have a poorer QoL. Individuals suffering from PCOS would benefit from a multidisciplinary intervention aimed at managing weight and dealing with problematic thoughts concerning appearance and weight. In addition, our results show how both dysmorphic concerns and eating disorders are relevant in the context of PCOS. Individuals with PCOS may benefit from periodic assessments aimed at detecting disordered eating (98). Practitioners should therefore screen individuals with the condition for a problematic relationship with food or excessive concerns about their bodies. Intervention and prevention programmes may also want to include women's partners in order to improve their effectiveness, as the disease may negatively affect women's intimate relationships (67). From a public health perspective, these results emphasize the detrimental effects of dysmorphic concerns and eating pathology on PCOS patients and require the urgent implementation of health promotion interventions. Policy makers and health institutions should thus create health promotion interventions aimed at improving knowledge, communication, and beliefs about the impact of PCOS on quality of life. This is consonant with recent advances arguing that mental health literacy may help promote individuals' psychosocial functioning (106). In addition, these programmes should not only involve PCOS patients, but also socialization agents such as family, peers, and the media through the transmission of messages aimed at raising awareness about appearance-related pressures that may come from social sources to prevent the onset of unhealthy body image (28). Finally, this study provided a holistic approach to the understanding of complex conditions such as PCOS.
The data that support the findings of this study are available from the corresponding author.
The studies involving human participants were reviewed and approved by Ethics Committee of the Center for Research and Psychological Intervention of the University of Messina. The patients/participants provided their written informed consent to participate in this study.
NB assisted with manuscript preparation, study design, data analysis and interpretation and data were gathered on-line under her supervision. DC assisted with manuscript preparation and data interpretation. MC assisted with manuscript preparation and data interpretation and served as corresponding author. VV assisted with concept and study supervision. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Głowińska A, Zielona-Jenek M, Pawelczyk A. Determinants of emotional problems and mood disorders in women with polycystic ovary syndrome. Ginekol Pol. (2016) 87:405–10. doi: 10.5603/GP.2016.0016
2. Bani Mohammad M, Majdi Seghinsara A. Polycystic Ovary Syndrome (PCOS), diagnostic criteria, and AMH. Asian Pac J Cancer Prev. (2017) 18:17–21. doi: 10.22034/APJCP.2017.18.1.17
3. Wekker V, Van Dammen L, Koning A, Heida KY, Painter RC, Limpens J, et al. Long-term cardiometabolic disease risk in women with PCOS: a systematic review and meta-analysis. Hum Reprod Update. (2020) 26:942–60. doi: 10.1093/humupd/dmaa029
4. Bayona A, Martínez-Vaello V, Zamora J, Nattero-Chávez L, Luque-Ramírez M, Escobar-Morreale HF, et al. Prevalence of PCOS and related hyperandrogenic traits in premenopausal women with type 1 diabetes: a systematic review and meta-analysis. Hum Reprod Update. (2022). doi: 10.1093/humupd/dmac011
5. Hart R, Doherty DA. The potential implications of a PCOS diagnosis on a woman's long-term health using data linkage. J Clin Endocrinol Metab. (2015) 100:911–9. doi: 10.1210/jc.2014-3886
6. Zangeneh FZ, Jafarabadi M, Naghizadeh MM, Abedinia N. Psychological distress in women with polycystic ovary syndrome from Imam Khomeini Hospital, Tehran. J Reprod Infertil. (2012) 13:111–5.
7. Barber TM, McCarthy MI, Wass JA, Franks S. Obesity and polycystic ovary syndrome. Clin Endocrinol. (2006) 65:137–45. doi: 10.1111/j.1365-2265.2006.02587.x
8. Huang X, Wang Q, Liu T, Pei T, Liu D, Zhu H, et al. Body fat indices as effective predictors of insulin resistance in obese/non-obese polycystic ovary syndrome women in the Southwest of China. Endocrine. (2019) 65:81–5. doi: 10.1007/s12020-019-01912-1
9. Álvarez-Blasco F, Botella-Carretero JI, San Millán JL, Escobar-Morreale HF. Prevalence and characteristics of the polycystic ovary syndrome in overweight and obese women. Arch Intern Med. (2006) 166:2081. doi: 10.1001/archinte.166.19.2081
10. Escobar-Morreale HF, Botella-Carretero JI, Alvarez-Blasco F, Sancho J, San Millán JL. The Polycystic Ovary Syndrome Associated with Morbid Obesity May Resolve after Weight Loss Induced by Bariatric Surgery. J Clin Endocrinol Metab. (2005) 90:6364–9. doi: 10.1210/jc.2005-1490
11. Claes L, Hart TA, Smits D, Van den Eynde F, Mueller A, Mitchell JE, et al. Validation of the social appearance anxiety scale in female eating disorder patients. Eur Eat Disord Rev. (2011) 20:406–9. doi: 10.1002/erv.1147
12. Kaminsky LA, Dewey D. The association between body mass index and physical activity, and body image, self esteem and social support in adolescents with type 1 diabetes. Can J Diabetes. (2014) 38:244–9. doi: 10.1016/j.jcjd.2014.04.005
13. Radwan H, Hasan HA, Ismat H, Hakim H, Khalid H, Al-Fityani L, et al. Body mass index perception, body image dissatisfaction and their relations with weight-related behaviors among University students. Int J Environ Res Public Health. (2019) 16:1541. doi: 10.3390/ijerph16091541
14. Dalley SE, Buunk AP, Umit T. Female body dissatisfaction after exposure to overweight and thin media images: the role of body mass index and neuroticism. Pers Individ Differ. (2009) 47:47–51. doi: 10.1016/j.paid.2009.01.044
15. Kantanista A, Król-Zielińska M, Borowiec J. Is underweight associated with more positive body image? Results of a cross-sectional study in adolescent girls and boys. Span J Psychol. (2017) 20:E8. doi: 10.1017/sjp.2017.4
16. Lynch E, Liu K, Wei GS, Spring B, Kiefe C, Greenland P, et al. The relation between body size perception and change in body mass index over 13 years: The coronary artery risk development in young adults (CARDIA) study. Am J Epidemiol. (2009) 169:857–66. doi: 10.1093/aje/kwn412
17. Warren CS, Gleaves DH. Cepeda-Benito A, Fernandez MD, Rodriguez-Ruiz S. Ethnicity as a protective factor against internalization of a thin ideal and body dissatisfaction. Int J Eat Disord. (2005) 37:241–9. doi: 10.1002/eat.20102
18. Shloim N, Hetherington MM, Rudolf M, Feltbower RG. Relationship between body mass index and women's body image, self-esteem and eating behaviours in pregnancy: a cross-cultural study. J Health Psychol. (2013) 20:413–26. doi: 10.1177/1359105313502568
19. Paxton SJ, Eisenberg ME, Neumark-Sztainer D. Prospective predictors of body dissatisfaction in adolescent girls and boys: a five-year longitudinal study. Dev Psychol. (2006) 42:888–99. doi: 10.1037/0012-1649.42.5.888
20. Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Fertil Steril. (2018) 110:364–79. doi: 10.1016/j.fertnstert.2018.05.004
21. Kataoka J, Tassone E, Misso M, Joham A, Stener-Victorin E, Teede H, et al. Weight management interventions in women with and without PCOS: a systematic review. Nutrients. (2017) 9:996. doi: 10.3390/nu9090996
22. Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L. The influence of body weight on sexual function and quality of life in women with polycystic ovary syndrome. Arch Gynecol Obstet. (2015) 291:451–5. doi: 10.1007/s00404-014-3423-1
23. Lim SS, Norman RJ, Davies MJ. The effect of obesity on polycystic ovary syndrome: a systematic review and meta-analysis. Int J Obes. (2013) 14:95–109. doi: 10.1111/j.1467-789X.2012.01053.x
24. Ahadzadeh AS, Rafik-Galea S, Alavi M, Amini M. Relationship between body mass index, body image, and fear of negative evaluation: Moderating role of self-esteem. Health Psychol Open. (2018) 5:205510291877425. doi: 10.1177/2055102918774251
25. Porras-Garcia B, Ferrer-Garcia M, Yilmaz L, Sen YO, Olszewska A, Ghita A, et al. Body-related attentional bias as mediator of the relationship between body mass index and body dissatisfaction. Eur Eat Disord Rev. (2020) 28:454–64. doi: 10.1002/erv.2730
26. Streeter VM, Milhausen RR, Buchholz AC. Body image, body mass index, and body composition: In young adults. Can J Diet Pract Res. (2012) 73:78–83. doi: 10.3148/73.2.2012.78
27. Littleton HL, Axsom D. Development of the body image concern inventory. Behav Res Ther. (2005) 43:229–41. doi: 10.1016/j.brat.2003.12.006
28. McLean SA. Body image in the context of eating disorders. Psychiatr Clin North Am. (2019) 42:145–56. doi: 10.1016/j.psc.2018.10.006
29. Gall K, Van Zutven K, Lindstrom J, Bentley C, Gratwick-Sarll K, Harrison C, et al. Obesity and emotional well-being in adolescents: roles of body dissatisfaction, loss of control eating, and self-rated health. Obesity. (2016) 24:837–42. doi: 10.1002/oby.21428
30. Goldschmidt AB, Aspen VP, Sinton MM, Tanofsky-Kraff M. Disordered eating attitudes and behaviors in overweight youth. Obesity. (2008) 16:257–64. doi: 10.1038/oby.2007.48
31. Luca M, Giannini M, Gori A, Littleton H. Measuring dysmorphic concern in Italy: psychometric properties of the Italian Body Image Concern Inventory (I-BICI). Body Image. (2011) 8:301–5. doi: 10.1016/j.bodyim.2011.04.007
32. Onden-Lim M. Intrusive imagery experiences in a high dysmorphic concern population. J Psychopathol Behav Assess. (2013) 35:99–105. doi: 10.1007/s10862-012-9318-1
33. Senín-Calderón C, Valdés-Díaz M, Benítez-Hernández MM, Núñez-Gaitán MC, Perona-Garcelán S, Martínez-Cervantes R, et al. Validation of Spanish language evaluation instruments for body dysmorphic disorder and the dysmorphic concern construct. Front Psychol. (2017). doi: 10.3389/fpsyg.2017.01107. [Epub ahead of print].
34. Coelho GM, Gomes AI, Ribeiro BG, Soares E. Prevention of eating disorders in female athletes. Open Access J Sports Med. (2014) 5:105–13. doi: 10.2147/OAJSM.S36528
35. Monks H, Costello L, Dare J, Reid Boyd E. “We're continually comparing ourselves to something”: navigating body image, media, and social media ideals at the nexus of appearance, health, and wellness. Sex Roles. (2021) 84:221–37. doi: 10.1007/s11199-020-01162-w
36. Senín-Calderón C, Gálvez-González J, Perona-Garcelán S, Camacho C, Rodríguez-Testal JF. Dysmorphic concern and behavioural impairment related to body image in adolescents. Int J Psychol. (2020) 55:832–41. doi: 10.1002/ijop.12646
37. Alur-Gupta S, Chemerinski A, Liu C, Lipson J, Allison K, Sammel MD, et al. Body-image distress is increased in individuals with polycystic ovary syndrome and mediates depression and anxiety. Fertil Steril. (2019) 112:930–8.e1. doi: 10.1016/j.fertnstert.2019.06.018
38. Annagür BB, Tazegül A, Akbaba N. Body image, self-esteem and depressive symptomatology in individuals with polycystic ovary syndrome. Noro psikiyatri arsivi. (2014) 51:129–32. doi: 10.4274/npa.y6778
39. Bazarganipour F, Ziaei S, Montazeri A, Foroozanfard F, Kazemnejad A. Body image satisfaction and self-esteem status among the patients with polycystic ovary syndrome. Iran J Reprod Med. (2013) 11:829–36. doi: 10.1186/1477-7525-11-141
40. Weinberger NA, Kersting A, Riedel-Heller SG. The relationship between weight status and depressive symptoms in a population sample with obesity: the mediating role of appearance evaluation. Obes Facts. (2018) 11:514–23. doi: 10.1159/000492000
41. Bazarganipour F, Taghavi SA, Montazeri A, Ahmadi F, Chaman R. The impact of polycystic ovary syndrome on the health-related quality of life: a systematic review and meta-analysis. Iran J Reprod Med. (2015) 13:61–70.
42. Jeanes Y, Reeves S, Gibson E, Piggott C, May V, Hart K, et al. Binge eating behaviours and food cravings in women with polycystic ovary syndrome. Appetite. (2017) 109:24–32. doi: 10.1016/j.appet.2016.11.010
43. Lee I, Dokras A. Mental health and body image in polycystic ovary syndrome. Curr Opin Endocr Metab Res. (2020) 12:85–90. doi: 10.1016/j.coemr.2020.04.004
44. Dingemans AE, van Rood YR, de Groot I, van Furth EF. Body dysmorphic disorder in patients with an eating disorder: prevalence and characteristics. Int J Eat Disord. (2012) 45:562–9. doi: 10.1002/eat.20972
45. Stice E, Shaw HE. Role of body dissatisfaction in the onset and maintenance of eating pathology: a synthesis of research findings. J Psychosom Res. (2002) 53:985–93. doi: 10.1016/S0022-3999(02)00488-9
46. Anderson DK, Lord C, Risi S, DiLavore PS, Shulman C, Thurm A, American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edition. (2013). p. 175. doi: 10.1176/appi.books.9780890425596
47. Cardi V, Tchanturia K, Treasure J. Premorbid and illness-related social difficulties in eating disorders: an overview of the literature and treatment developments. Curr Neuropharmacol. (2018) 16:1122–30. doi: 10.2174/1570159X16666180118100028
48. Patel K, Tchanturia K, Harrison A. An exploration of social functioning in young people with eating disorders: a qualitative study. PLoS ONE. (2016) 11:e0159910. doi: 10.1371/journal.pone.0159910
49. Van Hoeken D, Hoek HW. Review of the burden of eating disorders: mortality, disability, costs, quality of life, and family burden. Curr Opin Psychiatry. (2020) 33:521–7. doi: 10.1097/YCO.0000000000000641
50. Başar Gökcen B, Akdevelioglu Y, Canan S, Bozkurt N. Increased risk of eating disorders in women with polycystic ovary syndrome: a case-control study. Gynecol Endocrinol. (2020) 36:764–7. doi: 10.1080/09513590.2020.1744554
51. Larsson I, Hulthén L, Landén M, Pålsson E, Janson P, Stener-Victorin E, et al. Dietary intake, resting energy expenditure, and eating behavior in women with and without polycystic ovary syndrome. Clin Nutr. (2016) 35:213–8. doi: 10.1016/j.clnu.2015.02.006
52. Lee I, Cooney LG, Saini S, Smith ME, Sammel MD, Allison KC, et al. Increased risk of disordered eating in polycystic ovary syndrome. Fertil Steril. (2017) 107:796–802. doi: 10.1016/j.fertnstert.2016.12.014
53. Bernadett M, Szemán NA. Evészavarok prevalenciája policisztás ováriumszindrómás nok körében [Prevalence of eating disorders among women with polycystic ovary syndrome]. Psychiatr Hung. (2016) 31:136–45.
54. Paganini C, Peterson G, Stavropoulos V, Krug I. The overlap between binge eating behaviors and polycystic ovarian syndrome: an etiological integrative model. Curr Pharm Des. (2018) 24:999–1006. doi: 10.2174/1381612824666171204151209
55. Steegers-Theunissen RP, Wiegel RE, Jansen PW, Laven JS, Sinclair KD. Polycystic ovary syndrome: a brain disorder characterized by eating problems originating during puberty and adolescence. Int J Mol Sci. (2020) 21:8211. doi: 10.3390/ijms21218211
56. Azizi Kutenaee M, Amirjani S, Asemi Z, Taghavi S, Allan H, Kamalnadian S, et al. The impact of depression, self-esteem, and body image on sleep quality in patients with PCOS: a cross-sectional study. Sleep Breath. (2019) 24:1027–34. doi: 10.1007/s11325-019-01946-9
57. Kogure GS, Ribeiro VB, Lopes IP, Furtado CL, Kodato S, de Sá MF, et al. Body image and its relationships with sexual functioning, anxiety, and depression in individuals with polycystic ovary syndrome. J Affect Disord. (2019) 253:385–93. doi: 10.1016/j.jad.2019.05.006
58. Scaruffi E, Franzoi IG, Civilotti C, Guglielmucci F, La Marca L, Tomelini M, et al. Body image, personality profiles and alexithymia in patients with polycystic ovary syndrome (PCOS). J Psychosom Obstet Gynaecol. (2018) 40:294–303. doi: 10.1080/0167482X.2018.1530210
59. de Bruin AK, Oudejans RR. Athletes' body talk: the role of contextual body image in eating disorders as seen through the eyes of elite women athletes. J Clin Sport Psychol. (2018) 12:675–98. doi: 10.1123/jcsp.2018-0047
60. Wang FF, Wu Y, Zhu YH, Ding T, Batterham RL, Qu F, et al. Pharmacologic therapy to induce weight loss in women who have obesity/overweight with polycystic ovary syndrome: a systematic review and network meta-analysis. Obes Rev. (2018) 19:1424–45. doi: 10.1111/obr.12720
61. Van Zutven K, Mond J, Latner J. Obesity and psychosocial impairment: mediating roles of health status, weight/shape concerns and binge eating in a community sample of women and men. Int J Obes. (2014) 39:346–52. doi: 10.1038/ijo.2014.100
62. Pastore LM, Patrie JT, Morris WL, Dalal P, Bray MJ. Depression symptoms and body dissatisfaction association among polycystic ovary syndrome women. J Psychosom Res. (2011) 71:270–6. doi: 10.1016/j.jpsychores.2011.02.005
63. Stapinska-Syniec A, Grabowska K, Szpotanska-Sikorska M, Pietrzak B. Depression, sexual satisfaction, and other psychological issues in women with polycystic ovary syndrome. Gynecol Endocrinol. (2018) 34:597–600. doi: 10.1080/09513590.2018.1427713
64. Jones CL, Fowle JL, Ilyumzhinova R, Berona J, Mbayiwa K, Goldschmidt AB, et al. The relationship between body mass index, body dissatisfaction, and eating pathology in sexual minority women. Int J Eat Disord. (2019) 52:730–4. doi: 10.1002/eat.23072
65. Riestenberg C, Jagasia A, Markovic D, Buyalos RP, Azziz R. Health care-related economic burden of polycystic ovary syndrome in the United States: pregnancy-related and long-term health consequences. J Clin Endocrinol Metab. (2022) 107:575–85. doi: 10.1210/clinem/dgab613
66. Sulaiman M, Al-Farsi Y, Al-Khaduri M, Waly M, Saleh J, Al-Adawi S, et al. Psychological burden among women with polycystic ovarian syndrome in Oman: a caseandndash;control study. Int J Womens Health. (2017) 9:897–904. doi: 10.2147/IJWH.S145383
67. Thannickal A, Brutocao C, Alsawas M, Morrow A, Zaiem F, Murad MH, et al. Eating, sleeping and sexual function disorders in women with polycystic ovary syndrome (PCOS): a systematic review and meta-analysis. Clin Endocrinol. (2020) 92:338–49. doi: 10.1111/cen.14153
68. Jones GL, Benes K, Clark TL, Denham R, Holder MG, Haynes TJ, et al. The Polycystic Ovary Syndrome Health-Related Quality of Life Questionnaire (PCOSQ): a validation. Hum reprod. (2004) 19:371–7. doi: 10.1093/humrep/deh048
69. Garner DM, Olmsted MP, Bohr Y, Garfinkel PE. The eating attitudes test: psychometric features and clinical correlates. Psychol Med. (1982) 12:871–8. doi: 10.1017/S0033291700049163
70. Bazarganipour F, Ziaei S, Montazeri A, Foroozanfard F, Kazemnejad A. Health-related quality of life in patients with polycystic ovary syndrome (PCOS): a model-based study of predictive factors. J Sex Med. (2014) 11:1023–32. doi: 10.1111/jsm.12405
71. Joshi RD, Sawant N. How common are depressive-anxiety states, body image concerns and low self-esteem in patients of PCOS? J Obstet Gynaecol India. (2021) 72:72–7. doi: 10.1007/s13224-021-01505-x
72. Moradi F, Ghadiri-Anari A, Dehghani A, Reza Vaziri S. The effectiveness of counseling based on acceptance and commitment therapy on body image and self-esteem in polycystic ovary syndrome: an RCT. Int J Reprod Biomed. (2020) 18:243–52. doi: 10.18502/ijrm.v13i4.6887
73. Gori A, Topino E, Pucci C, Griffiths MD. The relationship between Alexithymia, dysmorphic concern, and exercise addiction: the moderating effect of self-esteem. J Pers Med. (2021) 11:1111. doi: 10.3390/jpm11111111
74. Piacentino D, Kotzalidis GD, Longo L, Pavan A, Stivali L, Stivali G, et al. Body image and eating disorders are common among professional and amateur athletes using performance and image enhancing drugs: a cross-sectional study. J Psychoactive Drugs. (2017) 49:373–84. doi: 10.1080/02791072.2017.1359708
75. Little TD, Cunningham WA, Shahar G, Widaman KF. To parcel or not to parcel: exploring the question, weighing the merits. Struct Equ Model. (2002) 9:151–73. doi: 10.1207/S15328007SEM0902_1
76. Marsh HW, Hau KT, Balla JR, Grayson D. Is more ever too much? The number of indicators per factor in confirmatory factor analysis. Multivariate Behav Res. (1998) 33:181–220. doi: 10.1207/s15327906mbr3302_1
77. Preacher KJ, Hayes AF, SPSS. and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. (2004) 36:717–31. doi: 10.3758/BF03206553
78. Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol Methods. (2002) 7:422–45. doi: 10.1037/1082-989X.7.4.422
79. Tang C, Cooper M, Wang S, Song J, He J. The relationship between body weight and dietary restraint is explained by body dissatisfaction and body image inflexibility among young adults in China. Eat Weight. (2020) 26:1863–70. doi: 10.1007/s40519-020-01032-0
80. Wendell JW, Masuda A, Le JK. The role of body image flexibility in the relationship between disordered eating cognitions and disordered eating symptoms among non-clinical college students. Eat Behav. (2012) 13:240–5. doi: 10.1016/j.eatbeh.2012.03.006
81. Ul-Haq Z, Mackay DF, Fenwick E, Pell JP. Meta-analysis of the association between body mass index and health-related quality of life among adults, assessed by the SF-36. Obesity. (2013) 21:E322–7. doi: 10.1002/oby.20107
82. Purton T, Mond J, Cicero D, Wagner A, Stefano E, Rand-Giovannetti D, et al. Body dissatisfaction, internalized weight bias and quality of life in young men and women. Qual Life Res. (2019) 28:1825–33. doi: 10.1007/s11136-019-02140-w
83. Tod D, Edwards C. Relationships among muscle dysmorphia characteristics, body image quality of life, and coping in males. J Sci Med Sport. (2015) 18:585–9. doi: 10.1016/j.jsams.2014.07.015
84. Barberis N, Costa S, Gitto L, Larcan R, Buemi M. Role of emotional intelligence as a mediating factor between uncertainty and anxiety hospital in chronic renal patients. Illn Crises Loss. (2016) 27:71–86. doi: 10.1177/1054137316667595
85. Emmer C, Bosnjak M, Mata J. The association between weight stigma and mental health: a meta-analysis. Obes Rev. (2019) 21. doi: 10.1111/obr.12935
86. Hunger JM, Dodd DR, Smith AR. Weight discrimination, anticipated weight stigma, and disordered eating. Eat Behav. (2020) 37:101383. doi: 10.1016/j.eatbeh.2020.101383
87. Louwers YV. Characteristics of polycystic ovary syndrome throughout life. Ther Adv Reprod Health. (2020) 14:2633494120911038. doi: 10.1177/2633494120911038
88. Barberis N, Costa S, Cuzzocrea F, Quattropani MC. Trait EI in the relationship between needs fulfillment and symptoms and attitudes associated with EDs. Ment Health Prev. (2018) 10:50–5. doi: 10.1016/j.mhp.2018.01.003
89. Barberis N, Quattropani MC. Relationship between motivation, adherence to diet, anxiety symptoms, depression symptoms and quality of life in individuals with celiac disease. J Psychosom Res. (2019) 124:109787. doi: 10.1016/j.jpsychores.2019.109787
90. Barberis N, Gugliandolo MC, Costa S, Cannavò M. Healthy and binge eating behaviours: The motivational processes underlying peer pressure. Psychol Health Med. (2021) 27:1144–53. doi: 10.1080/13548506.2021.1903054
91. Collison J, Barnier E. Eating disorders, body dysmorphic disorder, and body image pathology in female Australian models. Clin Psychol. (2020) 24:155–65. doi: 10.1111/cp.12208
92. Ritzert TR, Brodt M, Kelly MM, Menard W, Phillips KA. Social avoidance as a predictor of psychosocial functioning in body dysmorphic disorder: a prospective longitudinal analysis. Cognit Ther Res. (2019) 44:557–66. doi: 10.1007/s10608-019-10069-0
93. Ozgen Saydam B, Yildiz BO. Weight management strategies for patients with PCOS: current perspectives. Expert Rev Endocrinol Metab. (2021) 16:49–62. doi: 10.1080/17446651.2021.1896966
94. Gori A, Topino E, Griffiths MD. Protective and risk factors in exercise addiction: a series of moderated mediation analyses. Int J Environ Res Public Health. (2021) 18:9706. doi: 10.3390/ijerph18189706
95. Costa S, Barberis N, Larcan R. The incremental role of trait emotional intelligence on perceived cervical screening barriers. Psychol Health Med. (2018) 23:880–90. doi: 10.1080/13548506.2018.1437278
96. Nasiri Amiri F, Ramezani Tehrani F, Simbar M, Montazeri A. The experience of women affected by polycystic ovary syndrome: a qualitative study from iran. Int J Endocrinol Metab. (2014) 12:e13612. doi: 10.5812/ijem.13612
97. Pedersen L, Hicks RE, Rosenrauch S. Sociocultural pressure as a mediator of eating disorder symptoms in a non-clinical Australian sample. Cogent Psychol. (2018) 5:1523347. doi: 10.1080/23311908.2018.1523347
98. Dokras A, Stener-Victorin E, Yildiz BO Li R, Ottey S, Shah D, et al. Androgen excess- Polycystic ovary syndrome society: position statement on depression, anxiety, quality of life, and eating disorders in polycystic ovary syndrome. Fertil Steril. (2018) 109:888–99. doi: 10.1016/j.fertnstert.2018.01.038
99. Gallus S, Lugo A, Murisic B, Bosetti C, Boffetta P. Overweight and obesity in 16 European countries. Eur J Nutr. (2014) 54:679–89. doi: 10.1007/s00394-014-0746-4
100. Barberis N, Cannavò M, Cuzzocrea F, Verrastro V. Suicidal behaviours during COVID-19 pandemic: A review. Clin Neuropsychiatry. (2022) 19:84–96. doi: 10.36131/cnfioritieditore20220202
101. Devoe DJ, Han A, Anderson A, Katzman DK, Patten SB, Soumbasis A, et al. The impact of the COVID-19 pandemic on eating disorders: A systematic review. Int J Eat Disord. (2022). doi: 10.1002/eat.23704. [Epub ahead of print].
102. Eyupoglu ND, Aksun S, Ozturk M. Impact of social isolation during COVID-19 pandemic on health behaviors and weight management in women with polycystic ovary syndrome. Eat Weight Disord. (2022). doi: 10.1007/s40519-022-01369-8. [Epub ahead of print].
103. Monda V, Polito R, Lovino A, Finaldi A, Valenzano A, Nigro E, et al. Short-term physiological effects of a very low-calorie ketogenic diet: effects on adiponectin levels and inflammatory states. Int J Mol Sci. (2020) 21:3228. doi: 10.3390/ijms21093228
104. Paoli A, Mancin L, Giacona MC, Bianco A, Caprio M. Effects of a ketogenic diet in overweight women with polycystic ovary syndrome. J Transl Med. (2020) 18. doi: 10.1186/s12967-020-02277-0
105. Monda M, Messina G, Mangoni CB. Resting energy expenditure and fat-free mass do not decline during aging in severely obese women. Clin Nutr. (2008) 27:657–9. doi: 10.1016/j.clnu.2008.04.005
Keywords: body mass index, dysmorphic concerns, eating disorders, health-related quality of life, polycystic ovary syndrome
Citation: Barberis N, Calaresi D, Cannavò M and Verrastro V (2022) Body mass index and quality of life in individuals with polycystic ovary syndrome: Dysmorphic concerns and eating disorders as mediators. Front. Public Health 10:962083. doi: 10.3389/fpubh.2022.962083
Received: 05 June 2022; Accepted: 06 September 2022;
Published: 05 October 2022.
Edited by:
Stefania Cella, University of Campania Luigi Vanvitelli, ItalyReviewed by:
Giovanni Messina, University of Foggia, ItalyCopyright © 2022 Barberis, Calaresi, Cannavò and Verrastro. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marco Cannavò, bWFyY28uY2FubmF2b0BzdHVkZW50aS51bmljei5pdA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.