- 1Department of Nephrology, Affiliated Hospital of Hebei University, Baoding, China
- 2Tianjin Beichen Center for Disease Control and Prevention, Tianjin, China
- 3Hebei University, Baoding, China
- 4Department of Nephrology, Peking University People‘s Hospital, Beijing, China
Objective: The aim of this study was to analyze the epidemiological characteristics of the causes of chronic kidney disease (CKD) stage 5 patients in North China and to investigate the economic burden of those on hemodialysis (HD) or peritoneal dialysis (PD), as well as the associated influencing factors.
Methods: General clinical information, etiological categories, and hospitalization costs for HD or PD were collected from 1,515 patients hospitalized with stage 5 CKD at the Affiliated Hospital of Hebei University from 2016 to 2018. Logistic regression analysis was used to analyze the independent influencing factors affecting patients' financial burden.
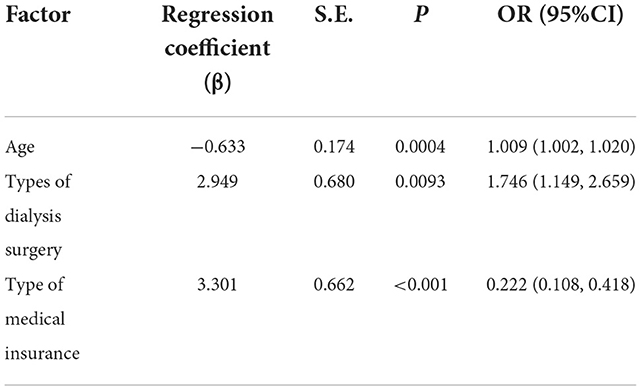
Results: The highest rate of DN was found in patients aged 70 years or older (27.0%) and the highest incidence of primary glomerulopathy was found in patients aged <50 years (24.3%). Age, type of dialysis, and type of health insurance were independent influences on the total financial burden of patients, and the results of multifactorial logistic regression analysis showed that age [OR (95% CI): 1.009 (1.002, 1.020)] and type of dialysis [OR (95% CI): 1.746 (1.149, 2.659)] would increase the total financial burden. The type of health insurance would reduce the total financial burden [OR (95% CI): 0.222 (0.108, 0.418)].
Conclusion: Chronic kidney disease, with its complex etiology and the heavy financial burden required for treatment, remains a more serious public health problem globally, and it is therefore necessary to further improve medical coverage for dialysis patients, increase management efforts, broaden pro-poor policies and increase the accessibility of medical services in low- and middle-income areas.
Background
Chronic kidney disease (CKD) is defined as structural and functional disturbances of the kidney caused by various etiologies with a history of kidney damage of ≥3 months. The fifth stage of CKD is the end stage of irreversible decline in kidney function and is also known as end-stage renal disease (ESRD). In recent years, the prevention and treatment of CKD has become an important public health issue worldwide due to its increasing incidence and prevalence (1, 2). According to an epidemiological survey published in The Lancet, the prevalence of CKD in China exceeds 10.8% and the number of patients is estimated to reach 119.5 million. In recent years, in addition to the two most common causes of CKD, hypertension and diabetes, more causes have been identified that may contribute to CKD (3, 4), and because of the multiple causes of CKD and the interaction of various chronic diseases, it is difficult to contain or slow down the development of CKD from its causes. In addition to this, kidney damage is irreversible and kidney function gradually declines, making dialysis the main clinical treatment for ESRD (5–7). However, ESRD patients need to receive lifelong treatment, which imposes a heavy financial burden on the patients' families and society (8). In this study, information on 1,515 patients with stage 5 CKD admitted to the Hebei University Hospital from 2016 to 2018 was collected to analyze the economic burden of different treatments in order to reduce the economic burden on patients and the public health system, and to describe the epidemiological distribution of the associated etiology.
Materials and methods
Study subjects
Patients with five stages of CKD who were hospitalized at the Affiliated Hospital of Hebei University from January 1, 2016 to December 31, 2018 were selected to analyze the epidemiological characteristics and economic burden of their etiology. A total of 1,607 patients with stage 5 CKD were hospitalized during the period. One thousand one hundred and fifteen patients were included and 92 were excluded according to the inclusion and exclusion criteria. This study was approved by the Ethics Committee of the Affiliated Hospital of Hebei University to be conducted (HDFY-LL-2020-028).
Inclusion criteria were as follows: (i) no history of psychiatric disorders; (ii) complete clinical data; (iii) patients aged 18 years or older.
Exclusion criteria were as follows: (i) suffering from severe gastrointestinal diseases, serious infections, malignancies or other serious diseases; (ii) bedbound dialysis patients.
Methods
The information of all 1,515 inpatients with stage 5 CKD was collected, and information cards were created for data collection. The collected case information included the demographic characteristics (gender, age, ethnicity), place of residence (urban/rural), type of surgical operation (indwelling catheter PD/HD access), hospitalization costs, type of health insurance, etc. The etiology of the patients was examined and classified in the clinical examination data of the subjects, and the data was collected and collated from the patients' clinical data, and the patients' etiology was clearly classified and pathologically supported in their clinical data. The etiological factors and economic burden of patients with stage 5 CKD were analyzed. In all hospitals from where data were extracted, they used digital data record systems, and they were all under the university using same variables in data record files.
Statistical methods
SAS 9.4 statistical software was used for data analysis. The data were tested for normality before the statistical methods used to select the data for analysis. Two-person and two-computer independent data entry was performed using EpiData 3.1. Statistical descriptions of the count information were made using rates or composition ratios (%). For continuous data variables with skewed distribution, the median was used for statistical description. Comparisons of count data between multiple groups were made using the rank sum test and P < 0.05 was considered statistically significant. Independent influences on financial burden were analyzed using logistic regression analysis.
Results
The general characteristics
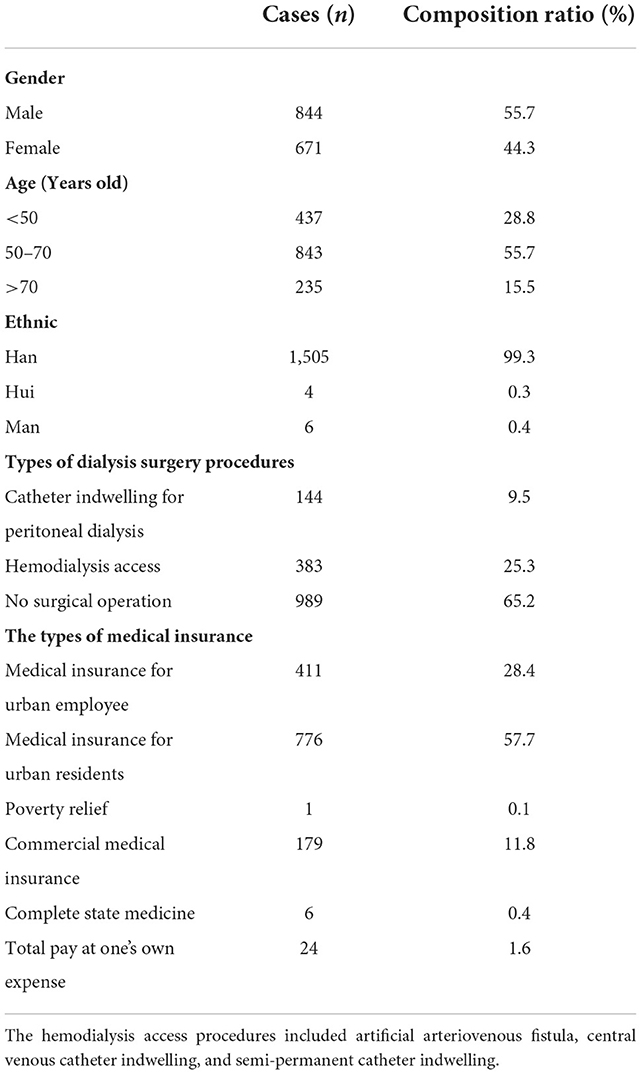
Among the 1,515 patients with stage 5 CKD, 55.7% were male, and 44.3% were female. The average age was 55.7 ± 13.6 years old, 99.3% were Han Chinese, 0.3% were Hui and 0.4% were Man. 51.2% from rural areas and 27.1% from urban areas. Five hundred and twenty seven patients (34.8%) underwent dialysis-related procedures, of whom 144 (9.5%) had indwelling catheter PD and 383 (25.3%) underwent HD access-related procedures. The details are shown in Table 1.
Characteristics of the epidemiological distribution of the etiology of patients with CKD stage 5
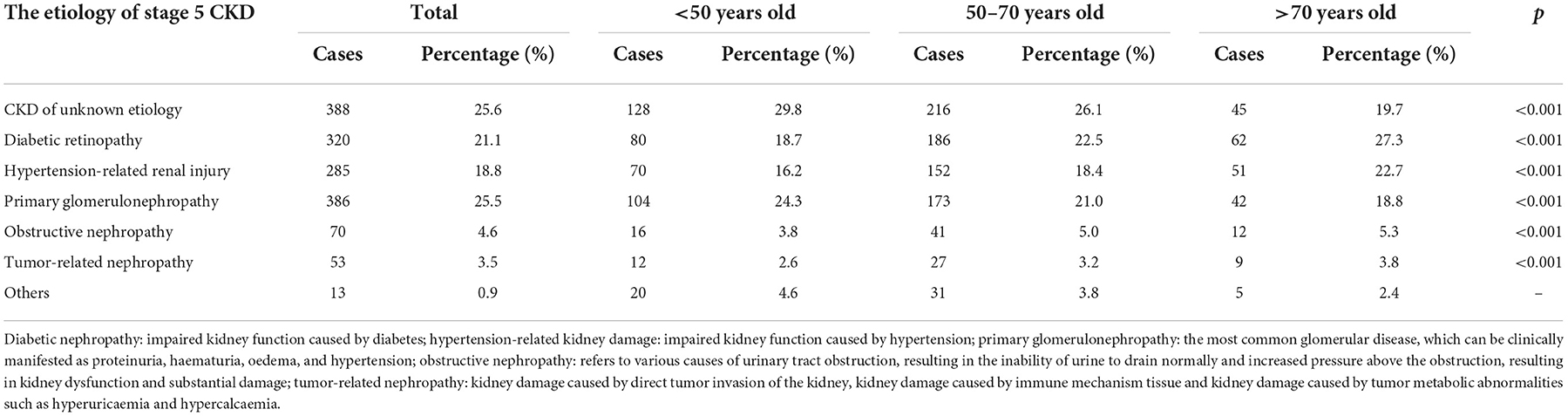
Patients were divided into three groups according to age and the epidemiological distribution of causes between the groups was analyzed, as shown in Table 2.
The predominant age group of patients with stage 5 CKD of different etiologies was 50–70 years, followed by patients younger than 50 years, with the smallest proportion of patients older than 70 years.
Among the different age groups, excluding CKD of unknown etiology, the prevalence of diabetic nephropathy (DN), hypertension-related kidney injury, obstructive nephropathy and tumor-related nephropathy was significantly higher in patients aged >70 years than in other age groups, with prevalence rates of 27.3, 22.7, 5.3, and 3.8%, respectively. In this study, the rates of DN were found to be 18.0 and 23.0% in patients aged <50 years and 50–70 years, respectively, and the highest rate (27.0%) was found in patients aged 70 years or older. The incidence of primary glomerulopathy was significantly higher in patients aged <50 years than in other groups, with an incidence of 24.3%.
Analysis of the economic burden of patients with stage 5 CKD
The median total medical cost of a single hospital stay for patients with stage 5 CKD was RMB 16,358.1, of which the median cost of Western medicine was RMB 6,064.5. There were 765 patients with no co-infections. Seven hundred and fifty patients (49.5%) developed infections and used antibiotics, with a median cost of RMB 1624.9 for antibiotic use.
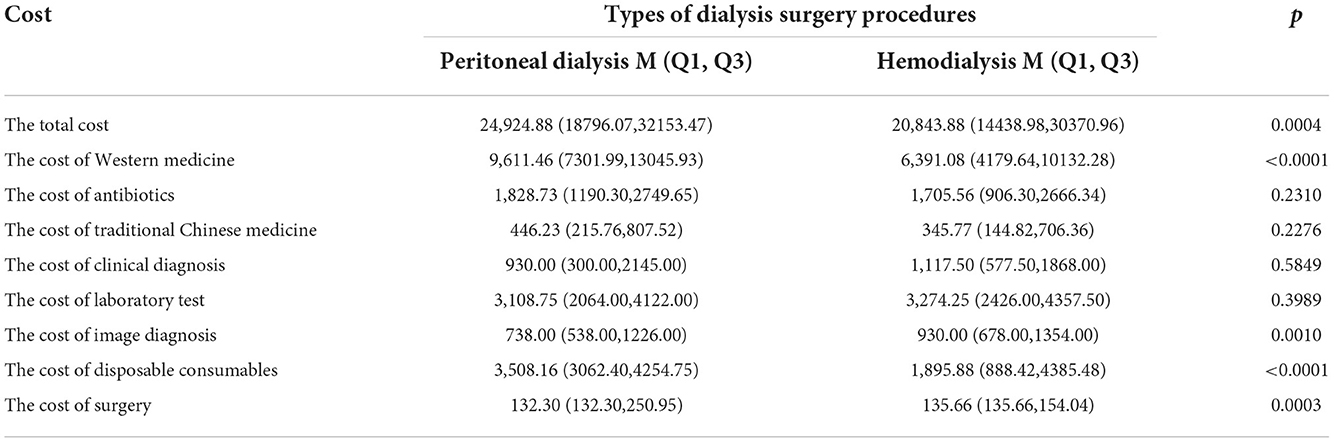
Comparison of the financial burden on dialysis patients
Of the patients with stage 5 CKD, 526 underwent dialysis, 144 underwent indwelling catheter PD and 383 underwent HD access surgery. In this study, the medical costs of patients who underwent dialysis procedures were analyzed and the differences between the two groups were statistically significant (p < 0.05) in terms of the cost of Western medicine, disposable consumables and type of surgical operation. There was no statistically significant difference between the two groups in the costs of Chinese medicine, clinical diagnostics and laboratory tests as shown in Table 3.
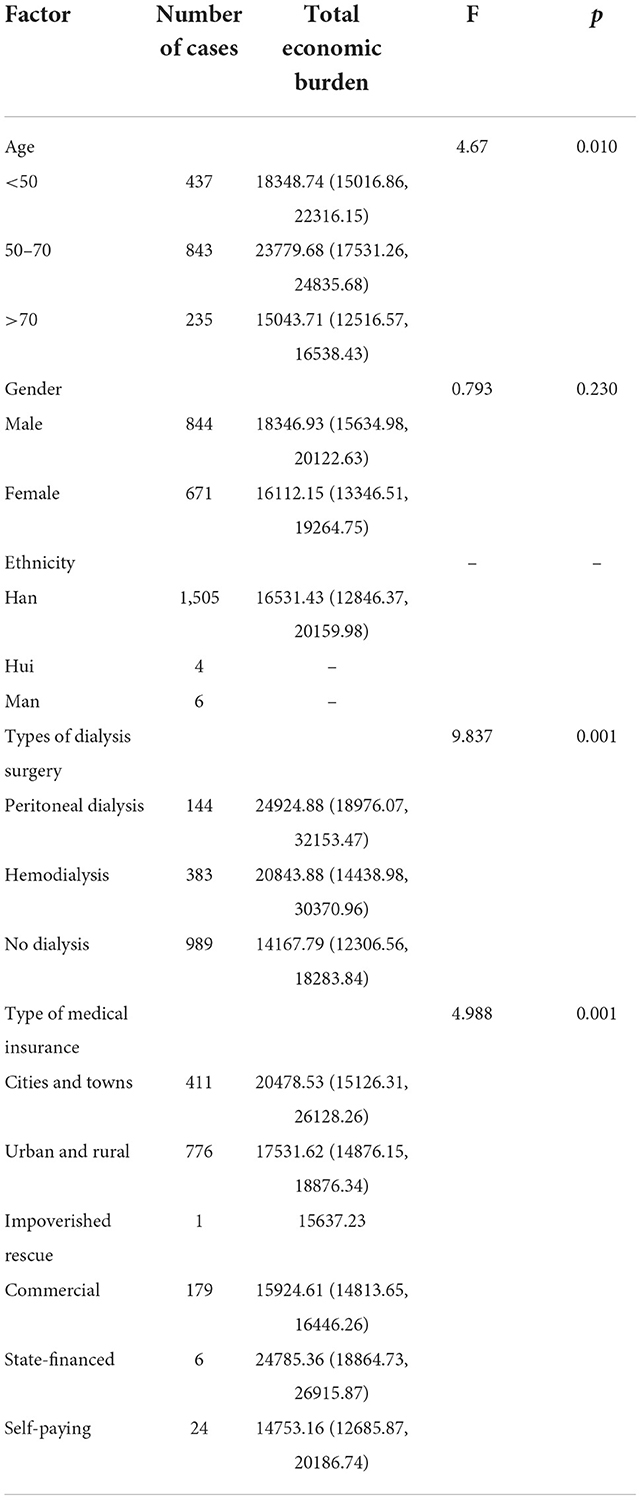
Univariate analysis of total economic burden on subjects
A univariate analysis of the total financial burden for all subjects showed that age, type of dialysis procedure and type of health insurance were independent influences on the total financial burden as shown in Table 4.
Multi-factor analysis of the total economic burden on subjects
Based on the results of the univariate analysis, this study included age, type of dialysis procedure and type of health insurance in a multiple logistic regression model for analysis, which showed that age [OR (95% CI): 1.009 (1.002, 1.020)] and type of dialysis [OR (95% CI): 1.746 (1.149, 2.659)] had a There was a negative impact of Type of health insurance had a beneficial effect on total financial burden [OR (95% CI): 0.222 (0.108, 0.418)] as shown in Table 5.
Discussion
Characteristics of the etiological distribution of CKD patients
Domestic and international studies have shown that the epidemiological characteristics of CKD stage 5 vary from time to time and region to region (9). Influenced by environmental factors, lifestyle, economic conditions and level of treatment, the prevalence rate varies among regions and ethnic groups (10). In this study, patients with CKD in a specific time period were selected from the Affiliated Hospital of Hebei University. It was found that after excluding stage 5 CKD of unknown etiology among the subjects, the first and second most common etiologies among patients aged 70 years or older were DN and hypertension-related kidney injury, respectively, and primary glomerulonephritis was less common than the above two. As age decreases, DN and hypertension-related kidney injury gradually decrease, while primary glomerulonephritis gradually increases and ranks first. In patients under 50 years of age, primary glomerular disease remained the most common cause (25.5%), in line with national and international studies (11, 12). This study also showed that the proportion of hypertension-associated kidney injury increased progressively with age. The proportion of hypertension-related kidney injury ranked first among patients over 70 years of age (23%). Possible reasons for the increased incidence of tubular injury are (13, 14): more underlying disease, a natural decline in renal function with age, and increased use of contrast agents, antibiotics, NSAIDs and chemotherapy drugs in older patients (15, 16). In addition, as the incidence of tumors increases with age, tumor infiltration, metastasis, metabolic abnormalities, chemical administration and contrast agents may lead to impaired renal function, while conditions such as prostatic hypertrophy, urological and genital tumors or ureteral compression by metastatic pelvic tumors may lead to obstructive nephropathy (17), so greater attention should be paid to tumor-related nephropathy as well as obstructive nephropathy.
Financial burden analysis
Dialysis imposes a huge financial burden on patients, and in recent years, with the increasing number of patients with CKD, the increasing number of patients developing CKD stage 5, and the application of new technologies and drugs, the upgrading of treatments for quality of life, the overall healthcare costs are increasing. The results of this study showed that mainly the cost of western drugs, the cost of disposable consumables and the cost of laboratory tests accounted for a greater proportion of the costs required for PD than HD. This is somewhat different from previous cost-effectiveness-based studies that concluded that PD was more cost-effective than HD, which may be due to the following reasons: (1) this study investigated the cost of a single hospital stay for stage 5 CKD, rather than the annual cost of maintenance dialysis (2) most of the patients undergoing the procedure were first-time RRT patients and disposable consumables, such as abdominal dialysis tubing, were more expensive; (3) the influence of the general national health policy environment, with lower drug costs and upward adjustments in the cost of medical consumables. As patients with CKD stage 5 require continuous dialysis, it is possible that PD is more cost effective than HD for the costs incurred by continuous dialysis, and we will continue to collect more data for further research. Based on the data collected so far, we further analyzed the relevant influences on the financial burden of patients with stage 5 CKD and found that age, dialysis and type of health insurance were independent influences on the financial burden of patients with stage 5 CKD. The effect of age on financial burden was small, with an OR value nearly equal to 1, indicating that age had almost no effect on financial burden. In contrast, dialysis and type of health insurance had a greater impact on financial burden, with dialysis patients experiencing a 0.746-fold increase in financial burden, while those using health insurance had a 0.222-fold increase in financial burden compared to those not using health insurance. Although various health insurance systems can be effective in reducing the financial burden of HD patients, patients still have to bear a greater financial hardship. For patients with stage 5 CKD, data from previous studies show that patients fail to choose the treatment that is most beneficial to their quality of survival, but rather the one with the least financial burden, given the direct financial burden (18). In low- and middle-income countries, dialysis reimbursement is not sufficient to treat all CKD patients, so there is a need to further improve health care coverage for dialysis patients, increase management efforts, broaden pro-poor policies and increase access to health care in low- and middle-income areas. However, we still have some limitations, such as no follow up visits, which will be conducted in future studies.
Conclusion
Chronic kidney disease (CKD) affects more than 10% of the global population and poses a huge challenge to societies and healthcare systems worldwide (19). Different countries and localities can improve the affordability and accessibility of RRT (blood purification) for patients with stage 5 CKD by recommending scientifically effective, appropriate and affordable treatments based on their own circumstances (20). This study investigated the etiology and financial burden of patients with stage 5 CKD and found that the main financial burden of patients with stage 5 CKD in northern China comes from dialysis, while medical insurance and reimbursement can reduce the medical burden. However, at present, CKD patients in North China still bear a huge financial burden, and the state still does not take up enough of the financial share. The national government should push forward the reform of universal medical insurance in depth, establish a supplementary medical insurance system such as major medical insurance, implement medical assistance for serious illnesses, etc., and develop various forms of commercial health insurance to build up a multi-level and wide-ranging medical security system. It is hoped that this study will provide reference and ideas for the country to adjust the reimbursement system of medical insurance.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study was conducted with approval from the Ethics Committee of the Affiliated Hospital of Hebei University (HDFY-LL-2020-028). The patients/participants provided their written informed consent to participate in this study.
Author contributions
S-SG and Y-LG: conception and design of the research and writing of the manuscript. YH and J-DL: acquisition of data. X-JZ: analysis and interpretation of the data. H-FZ: statistical analysis. HC: obtaining financing and critical revision of the manuscript for intellectual content. All authors read and approved the final draft.
Funding
This study was funded by the Key Research and Development Program of Hebei Province (No. 20377705D).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Luyckx VA, Cherney DZI, Bello AK. Preventing CKD in developed countries. Kidney Int Rep. (2019) 5:263–77. doi: 10.1016/j.ekir.2019.12.003
2. Swartling O, Rydell H, Stendahl M, Segelmark M, Trolle Lagerros Y, Evans M. CKD progression and mortality among men and women: a nationwide study in Sweden. Am J Kidney Dis. (2021) 78:190–9.e1. doi: 10.1053/j.ajkd.2020.11.026
3. Vallianou NG, Mitesh S, Gkogkou A, Geladari E. Chronic kidney disease and cardiovascular disease: is there any relationship? Curr Cardiol Rev. (2019) 15:55–63. doi: 10.2174/1573403X14666180711124825
4. Banerjee D, Wang AY. Personalising heart failure management in CKD patients. Nephrol Dial Transplant. (2021) 37:2055–62. doi: 10.1093/ndt/gfab026
6. Ma Y, Yu H, Sun H, Li M, Li L, Qin M. Economic burden of maintenance hemodialysis patients' families in Nanchong and its influencing factors. Ann Palliat Med. (2020) 9:3877–84. doi: 10.21037/apm-20-1787
7. Basile C, Davenport A, Mitra S, Pal A, Stamatialis D, Chrysochou C, et al. Frontiers in hemodialysis: innovations and technological advances. Artif Organs. (2021) 45:175–82. doi: 10.1111/aor.13798
8. Obrador GT, Levin A. CKD hotspots: challenges and areas of opportunity. Semin Nephrol. (2019) 39:308–14. doi: 10.1016/j.semnephrol.2019.02.009
9. Adamczak M, Surma S. Metabolic acidosis in patients with CKD: epidemiology, pathogenesis, and treatment. Kidney Dis. (2021) 7:452–67. doi: 10.1159/000516371
10. Zhang L, Zhao MH, Zuo L, Wang Y, Yu F, Zhang H, et al. China Kidney Disease Network (CK-NET) 2016 annual data report. Kidney Int Suppl. (2020) 10:e97–185. doi: 10.1016/j.kisu.2020.09.001
11. van der Tol A, Lameire N, Morton RL, Van Biesen W, Vanholder R. An international analysis of dialysis services reimbursement. Clin J Am Soc Nephrol. (2019) 14:84–93. doi: 10.2215/CJN.08150718
12. Jankowski J, Floege J, Fliser D, Böhm M, Marx N. Cardiovascular disease in chronic kidney disease: pathophysiological insights and therapeutic options. Circulation. (2021) 143:1157–72. doi: 10.1161/CIRCULATIONAHA.120.050686
13. VanDeVoorde RG III. Acute poststreptococcal glomerulonephritis: the most common acute glomerulonephritis. Pediatr Rev. (2015) 36:3–12; quiz 13. doi: 10.1542/pir.36.1.3
14. Li S, Liu QQ. A study on the mechanism of the protective effect of GuangeFang on sepsis-associated acute kidney injury. World J Trad Chin Med. (2021) 7:414–8. doi: 10.4103/2311-8571.328618
15. Satoskar AA, Parikh SV, Nadasdy T. Epidemiology, pathogenesis, treatment and outcomes of infection-associated glomerulonephritis. Nat Rev Nephrol. (2020) 16:32–50. doi: 10.1038/s41581-019-0178-8
16. Cheng YQ Li J, Qu HS, Zhang XZ, Zhang HL, Zhang J, et al. Clinical effect of tripterygium glycosides combined with glucocorticoids in the treatment of refractory nephrotic syndrome patients: a systematic review and meta-analysis. World J Trad Chin Med. (2020) 6:249–59. doi: 10.4103/wjtcm.wjtcm_20_20
17. Liang S. [Characteristics and Prognostic Risk Factors of Chronic Kidney Disease in Elderly Inpatients]. People's Liberation Army Medical College (2018).
18. Wu H, Li Q, Cai Y, Zhang J, Cui W, Zhou Z. Economic burden and cost-utility analysis of three renal replacement therapies in ESRD patients from Yunnan Province, China. Int Urol Nephrol. (2020) 52:573–9. doi: 10.1007/s11255-020-02394-1
19. Elshahat S, Cockwell P, Maxwell AP, Griffin M, O'Brien T, O'Neill C. The impact of chronic kidney disease on developed countries from a health economics perspective: a systematic scoping review. PLoS ONE. (2020) 15:e0230512. doi: 10.1371/journal.pone.0230512
Keywords: stage 5 CKD, hemodialysis, peritoneal dialysis, etiology analysis, economic burden
Citation: Guo S-S, Gou Y-L, Li J-D, Zhang H-F, Huang Y, Zheng X-J, Chen H and Sui Z (2022) An analysis of the etiologies and economic indexes of inpatients with stage 5 chronic kidney disease in North China. Front. Public Health 10:956463. doi: 10.3389/fpubh.2022.956463
Received: 30 May 2022; Accepted: 29 September 2022;
Published: 01 December 2022.
Edited by:
Rajendra Bhimma, University of KwaZulu-Natal, South AfricaReviewed by:
Chao Yang, First Hospital, Peking University, ChinaRajat Sanker Roy Biswas, Chattagram Maa-O-Shishu Hospital Medical College, Bangladesh
Ricardo Adrian Nugraha, Airlangga University, Indonesia
Copyright © 2022 Guo, Gou, Li, Zhang, Huang, Zheng, Chen and Sui. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hang Chen, ZHJjaGVuX2NoQG91dGxvb2suY29t; Zhun Sui, c3Vpemh1bnNuQDIxY24uY29t
†These authors have contributed equally to this work
 Shan-Shan Guo1†
Shan-Shan Guo1† Hang Chen
Hang Chen