
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 29 September 2022
Sec. Children and Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.956422
This article is part of the Research TopicNeonatal Health in Low- and Middle-Income CountriesView all 41 articles
 Vaishali Deshmukh1
Vaishali Deshmukh1 Shibu John2
Shibu John2 Abhijit Pakhare3
Abhijit Pakhare3 Rajib Dasgupta4
Rajib Dasgupta4 Ankur Joshi3
Ankur Joshi3 Sanjay Chaturvedi5
Sanjay Chaturvedi5 Kiran Goswami6
Kiran Goswami6 Manoja Kumar Das1
Manoja Kumar Das1 Rupak Mukhopadhyay1
Rupak Mukhopadhyay1 Rakesh Singh1
Rakesh Singh1 Pradeep Shrivastava1
Pradeep Shrivastava1 Bhavna Dhingra7
Bhavna Dhingra7 Steven Bingler8
Steven Bingler8 Bobbie Provosty Hill8
Bobbie Provosty Hill8 Narendra K. Arora1*
Narendra K. Arora1*Background: Home visitation has emerged as an effective model to provide high-quality care during pregnancy, childbirth, and post-natal period and improve the health outcomes of mother- new born dyad. This 3600 assessment documented the constraints faced by the community health workers (known as the Accredited Social Health Activists, ASHAs) to accomplish home visitation and deliver quality services in a poor-performing district and co-created the strategies to overcome these using a nexus planning approach.
Methods: The study was conducted in the Raisen district of Madhya Pradesh, India. The grounded theory approach was applied for data collection and analysis using in-depth interviews, and focus group discussions with stakeholders representing from health system (including the ASHAs) and the community (rural population). A key group of diverse stakeholders were convened to utilize the nexus planning five domain framework (social-cultural, educational, organizational, economic, and physical) to prioritize the challenges and co-create solutions for improving the home visitation program performance and quality. The nexus framework provides a systemic lens for evaluating the success of the ASHAs home visitation program.
Results: The societal (caste and economic discrimination), and personal (domestic responsibilities and cultural constraints of working in the village milieu) issues emerged as the key constraints for completing home visits. The programmatic gaps in imparting technical knowledge and skills, mentoring system, communication abilities, and unsatisfactory remuneration system were the other barriers to the credibility of the services. The nexus planning framework emphasized that each of the above factors/domains is intertwined and affects or depends on each other for home-based maternal and newborn care services delivered with quality through the ASHAs.
Conclusion: The home visitation program services, quality and impact can be enhanced by addressing the social-cultural, organizational, educational, economic, and physical nexus domains with concurrent efforts for skill and confidence enhancement of the ASHAs and their credibility.
Home visitation is an effective and community-wide acceptable model to provide intensive care during pregnancy, childbirth, and postnatal care to improve maternal and child health outcomes (1, 2). Most of the home visitation programs are grounded on the ecological theory suggesting that the children develop in multi-layered environmental conditions (3). It links the parents-child-family and the health systems (4) and is a cost- and time-effective intervention (5, 6) that empowers skill, knowledge, and awareness of the mother on childcare, early identification of sickness, and care-seeking (7, 8), thereby improves the maternal and neonatal outcomes (9, 10).
ASHAs (Accredited Social Health Activists) are the community health functionaries stationed in the villages (1 ASHA per 1,000 population) and over a million ASHAs are working in 600000 villages across India (11). As part of the Janani Shishu Suraksha Karyakaram (JSSK, June 2011) (12) and Home Based Newborn Care (HBNC, August 2011) programs, ASHAs have been entrusted to visit pregnant women, facilitate institutional delivery, and make 6–7 home visits during the post-natal period to empower the mothers and mobilize the beneficiaries to health facilities, when required (13). Later in 2013, as part of the Norwegian India Partnership Initiative (NIPI) (14), the Home-Based New-born Care Plus (HBNC plus) program was piloted in four states of India (Rajasthan, Madhya Pradesh, Bihar, and Odisha). The HBNC Plus involved four more home visits for the infants after the postnatal period, at ages 3, 6, 9 and, 12 months to provide counseling for age-appropriate feeding, hand washing, regular play and, communication for early child care and development (ECCD), immunization, prophylactic oral rehydration solutions (ORS) and Iron and folic acid (IFA) distribution and growth monitoring.
Studies have shown that when an adequate number of home visits are made for newborns and infants accomplishments of the tasks assigned to community health workers lead to both better physical and cognitive development and early identification of sickness. High-quality home visitations also decreased the mortality and morbidities in this age group (15–17). An ASHA evaluation across seven Indian states demonstrated heterogeneity in-home visitation patterns both in terms of number and quality of visits (18). Mothers rated the performance of ASHAs as poor for advice/counseling regarding obstetric danger signs, neonatal assessment and, care in Karnataka, India (19). The internal program evaluation document of the NIPI program also showed that home visitations by ASHAs under HBNC and HBNC Plus programs were both inadequate and poor in quality and < 10% of sick young infants were mobilized by the frontline workers to health facilities (20). The barriers to timely home visitation and high-quality service delivery by the ASHAs are only partially understood. The social, cultural, and personal constraints have not been comprehensively researched in most of the studies, and the focus was generally limited to programmatic challenges (21). The HBNC Plus program evaluation highlighted the difficulty of translating the inputs, such as training and incentives into the desired outputs, such as home visits, both quantity- and quality-wise (20). The current study was therefore undertaken to document the barriers to completion of expected home visitation and quality of service delivery by the ASHAs as part of the HBNC (during the first six weeks after birth) and HBNC Plus programs (during the post-neonatal period through the first year of life) in Raisen district of Madhya Pradesh, India.
We applied the nexus planning framework (NPF), which is based on 360-degree assessment of the challenges, interlinkages, synergies and, trade between the challenges with emphasis on cross-sectoral sustainability and enhancing the socio-economic-cultural-and organizational resilience against current and future barriers. The NPF method was a further refinement of the traditional formative component recognizing the importance of sub-group and sub-constituencies of the stakeholders and attempts to incorporate their respective concerns, hesitancy and, fears and unique solutions (22).
The study was conducted in Raisen district of Madhya Pradesh, India from October 2016 to September 2018. Madhya Pradesh has one of the highest neonatal and infant mortality rates in the country and is one of the eight socio-economically backward states (Bihar, Chhattisgarh, Jharkhand, Orissa, Rajasthan, Uttaranchal and, Uttar Pradesh), also referred to as the Empowered Action Group (EAG) states (23). In Madhya Pradesh, HBNC Plus pilot program was rolled out by NIPI in four districts (out of 51 districts) namely Raisen, Hoshangabad, Betul and, Narsinghpur. These districts are not part of the 123 aspirational districts declared by NITI Aayog but their overall rankings for development including health indicators are in the lower one-third of all districts of the country (24). Raisen district had poor indicators for mobilization of home- delivered mother-child dyad to skilled health personnel within 48 h, and dispensing of ORS to diarrhea patients among the four NIPI districts (25, 26). The Department of Health and Family Welfare, Government of Madhya Pradesh, NIPI leadership and, the investigators jointly decided to include Raisen district for the evaluation of ASHA performance for home visitations under HBNC and HBNC Plus programs. In the district, four administrative blocks were purposively selected for the study i.e., Gairat Ganj (53 kms), Begam Ganj (78 kms), Silwani (86 kms), and Udaipur (80 kms), based on their distance from the district headquarter.
The study had two phases data collection, analysis and, synthesis. During Phase I (formative research), we applied the qualitative research methods using grounded theory for data collection and analysis. In-depth interviews (IDIs) and focus group discussions (FGDs) with various participants were conducted at their respective locations. Phase-II: Data from Phase-I were used for conducting the multi-stakeholder nexus planning (NP) exercise.
Community engagement: Before commencing our community activities, we had a series of meetings with village leaderships (Panchayat members) in the four study blocks to explain to them the purpose and methods of the study and obtain their buy-in. We purposively selected the respondents for IDIs and FGDs ensuring the representativeness at different levels (national, state, district, and community levels) (Figure 1). We purposively selected the respondents from different stakeholder categories (home visitation beneficiaries, ASHAs, and other frontline health and Anganwadi workers residing and working in these four blocks, healthcare providers and, program managers working at block, district, state and, national levels). At this stage, the caste of the stakeholder (lower/backward and upper/forward) was neither considered for the selection nor was not recorded to avoid any bias. The investigator group decided following definitions to define beneficiary mothers as utilizers of the home visitation by ASHA: (a) under HBNC program: 4 or more home visits done during 1.5 months after birth; (b) under HBNC Plus program: 2 or more home visits done between 3 and 12 months of age. Non-utilizers had not received any home visits. The quality of each home visit was assessed with reference to the program guidelines (13, 27). A prior appointment was taken with the interviewee before all interactions and during the face-to-face interaction.
We collected data using pretested semi-structured IDI and FGD guides developed by the investigators/authors, a multi-disciplinary team. A team of four female social scientists trained in qualitative data collection conducted the IDIs and FGDs at places convenient to the interviewee and no observer was allowed. The IDIs and FGDs were conducted in the local language (Hindi) and audio recorded with consent. Some of the IDIs with health managers at the state and national level were in English; these were also recorded. Study investigators (VD, AP) conducted the IDIs at the national, state and district levels and facilitated the FGDs. Senior researchers (NKA, VD, AP, and SJ) with at least 15 years of experience in qualitative research, supervised data collection, and analysis. Most of the IDIs and FGDs lasted for about one hour (range 50 to 120 min).
All IDIs and FGDs were transcribed (i.e., Hindi) and then translated into English. The transcriptions/translations of all IDIs and FGDs were entered using INCLEN qualitative data analysis software (IQDAS) (28) for systematic organization and retrieval of data for analysis. During quality assessments, four IDIs were rejected due to incompleteness (one) and poor quality audio (three). We adopted the grounded theory (29) approach for data analysis. All the IDI and FGD transcripts were carefully read by two trained social scientists and reconfirmed by a senior author (VD), to interpret the data. The researchers inductively analyzed the data using the following steps: (i) free-listing and open-coding of the responses and marking the relevant/introductory statements for use as quotable quotes; (ii) axial coding of the responses keeping in mind the connection/relationship between free-listed responses/small units, and (iii) develop selective codes (wherever applicable) for the clusters of axial codes communicating common theme. The emerging patterns/themes from the responses, helped the researchers to interpret the ASHA's functioning in the light of the different challenges. The emerging codes and themes were regularly discussed with the senior author (NKA) to resolve inconsistencies. All analytic steps were followed (open, axial, and selective coding) consistently to have inter-coder reliability and stability, and reproducibility (30). Data quality was ensured by triangulating data collection methods at two levels-across methods and across respondents (trustworthiness). The findings were expressed semi-quantitatively using qualifiers to express findings systematically: very few (< 10%), some (10–24%), about half (25–49%), the majority (50–75%), most (76–89%), and almost all (>90%). The quasi-quantitative expressions are based on how many times the code was mentioned (28, 31).
Nexus approach is currently used in a large number of sectors to define solutions to complex, multidimensional, and layered challenges. Under the nexus approach, interlinkages, synergies, and trade-offs are analyzed, with the aim of identifying solutions and improving the performance of ecosystems. Thus, nexus planning emphasizes cross-sectoral sustainability and enhances socio-economic-cultural-organizational resilience against current and future challenges. We have used NPF as a participatory co-creation process to ensure ownership of all stakeholders including their sub-constituencies in decision-making and bringing about accord among all stakeholders including the program implementers to improve the performance of ASHAs, particularly for home visitations under HBNC and HBNC Plus program. NPF systematically focuses on the challenges and attempts to identify the possible solutions under five nexus domains: social-cultural, economic, physical, organizational, and educational (22, 32–34) (Figure 2).
The nexus planning process had three steps after the initial formative research component using qualitative methods (Phase I), which identified the barriers and facilitators to the home visitations by the ASHAs from a large number of stakeholders including the mothers and ASHAs (Figure 1). The data from Phase-I were analyzed and organized according to the five nexus domains for sharing with different stakeholders.
An extensive discussion was held between the investigators, field staff, and Panchayat members to identify essential sub-groups/constituencies of all stakeholders, which had different perspectives and social dynamics at the ground level. Through the discussion, then it was decided to conduct three nexus meetings/consultations considering the caste groups of the community and the frontline workers and larger community of service providers; one each including the representatives from lower and higher/upper castes (as per the local knowledge) and the third with mixed representatives drawn from all caste groups.
Each of the caste-specific nexus planning meetings/ consultation had 20–30 participants drawn from the same caste group (community and parents from all the four blocks, ASHAs from the respective blocks and two program managers from the district). The meetings were facilitated by the authors. The objectives of these nexus planning meetings/consultations were to discuss the findings from Phase-I (formative research); validate the sub-group specific observations emerging from the data analysis; identify the challenges categorized according to the nexus domains and suggest solutions appropriate for their respective caste groups.
Following the caste-specific nexus planning meetings/consultations, the final larger heterogeneous stakeholder group consultation (59 participants) was organized to bring synergy between the perspectives of the two sub-groups, smoothen the points of disagreement and develop final recommendations for improving the performance of the ASHAs in the communities. This nexus planning method is a further refinement of traditional formative components recognizing the importance of sub-group and sub-constituencies of the stakeholders, bringing about synergies, accord and identifying the points of negotiations so that the recommendations incorporate their respective concerns, hesitancy and fears, and unique solutions.
The nexus planning process was facilitated by two experts, who are the innovators of the process (BH, SB) and authors having experience in community engagement. The participants for nexus planning meetings included: (i) community stakeholders engaged in the process of home visitation directly or indirectly i.e., mothers, family members, village leadership (religious, social, and cultural); (ii) elected village leadership (Panchayat - local self-Government), Village Health, Sanitation, and Nutrition committee (VHSNC) members; (iii) representatives from education, revenue, and administration departments; (iv) respondents from the health department– ASHAs, ANMs, doctors from PHC/CHC and Chief Medical Officer of the district, ASHA supervisor; and (v) department of women and child welfare-AWWs. Three NPMs were organized: two preliminary NPMs considering the social demographic sensitivity [the community stakeholders were purposely drawn from low (first NPM) and high castes (second NPM)] and the third with a mix of community and representatives from the health system (Figure 1). No such differentiation was done for the healthcare providers and frontline workers for these NPMs.
First (32 participants; community members drawn from 15 villages) and second (31 participants; community members drawn from 8 villages) NPMs reviewed the findings of the IDIs and FGDs and indicated their views about the correctness of the data and its interpretation. The rationale of giving importance and hearing to all the sub-group stakeholders/constituencies brought out items and matters which required joint discussion to arrive at a mutually acceptable way forward. The challenges faced by ASHAs from forward and backward communities were different and had to be handled in a manner that required suggestions from both sides.
The third NPM (59 participants; community members from 22 villages) discussed the barriers and strategies for overcoming these in a harmonized, negotiated, and comprehensive manner. Each NPM had a similar work process. The objective of the initial plenary of 60 min, was to apprise the heterogeneous audience of the perceptions of the diverse sub-group stakeholders and emerging themes that required careful attention. The group was divided into 3 smaller groups and each comprised mix of community sub-groups/constituencies and geographies of the district along with health providers. Nexus planning charts were used primarily to keep the discussion on track document discussions according to specific domains, and develop final recommendations for improving the performance of the ASHAs in actual field settings (Figure 3). Finally, the plenary session of 90 min summarized the findings from all the sub-groups. The total duration of these meetings was approximately 3.5 to 4 h (including conduction). During the final plenary session, the three groups came together to build a consensus about the barriers and solutions and organized into the NPF. The summary also identified action for different stakeholders to improve the frequency and quality of home visitation and sustain these during the immediate post-partum period (HBNC period) and up to 15 months of age (HBNC Plus period).
The NPM facilitators noted down the observations and comments of every participant on ‘post-it/sticky notes' and collected these on the nexus domain chart. The findings from the first and second NPMs were shared with 3rd large group NPMs. The final plenary of the 3rd NPM helped in the co-identification of the barriers, and co-creation of the solutions and recommendations under the five nexus domains i.e., socio-cultural, physical, organizational, economic, and education.
Figure 1 and Table 1 provide the distribution of stakeholders, and demographic profile of mothers and frontline workers participating in Phase-I of the study. A total of 119 IDIs were conducted: mothers (64), ASHAs (16), Auxiliary Nurse Midwives (ANMs) (4), Aganwadi workers (AWW) (4), ASHA supervisors (ASHA Sahyogini) (6), VHSNC members (2) and health system representatives at block, district, state and national levels (23). We also conducted five FGDs: one each with mothers of an infant under < 6 months old infants (for HBNC) and one with mothers of an infant 6 months to 15 months for (HBNC Plus program); one with ASHAs and Asha supervisors; one with ANMs and one with AWWs to supplement the IDIs for data saturation and data triangulation (Figure 1).
Data from Phase-I has been organized under the nexus domains with the emerging themes and sub-themes along with an illustrative statement from the participants.
The majority of the state and district level stakeholders, ANMs, and approximately half of the ASHAs identified socio-economic divide and caste/religion-based discrimination making the home visitations difficult and the reluctance of families to accept the health and wellness messages for childcare and more so for male children. Socio-cultural beliefs such as seclusion of post-partum mother and child and belief in the tradition of the‘evil eye effect' also made it difficult for ASHAs to deliver the desired services.
“Some refuse to put the child in the weighing bag. They say that you took the weight of the Muslim child, the Scheduled tribes (ST) Child and now you will put our child in the same bag” [ASHA Sahyogini]
“She is from a rich family. Why will she will come to a low-income family house?” [Mother non-utilizers]
“Some are Harijan (Scheduled caste), and some are Vasur (scheduled caste)?, so she differentiates. She is not comfortable coming to our house. She does not touch our child.” [Mother non-utilizers]
Stakeholders from the administrative hierarchy and community perceived trust deficit and lack of respect and credibility of ASHA due to lower education status, inadequate training, and lack of confidence demonstrated while communicating with the family members. Similarly, the community questioned the ASHA's credibility, when the family experienced ‘inadequate or suboptimal' services at the health facility to which ASHA referred them. Several elders in the family preferred traditional childcare methods over ASHA's suggestions. Common superstitious beliefs such as ‘Sutak' (prohibitions observed during post-partum period), when the mother-neonate are confined indoors, were used as an excuse to refuse both contact/examination by the ASHA and referral. The front-line workers (ANMs, AWWs, and ASHA supervisors) perceived that it was difficult for ASHAs to convince the community and families about immunization and the associated minor side effects. Families also showed deep-rooted resistance in following advice, such as play and communication with the child and washing hands with soap, which considerably differed from their existing practices and were perceived as irrelevant to them. Approximately half of the non-utilizers mothers complained of the lack of resources required to follow ASHAs' advice. We also found a better understanding of utiliser mothers' knowledge of program components like exclusive breastfeeding, IFA syrup, hand washing, and ORS preparation when compared with the non-utilizers mothers.
“People doubt her motive when she visits their house again and again”. [AWW]
“ASHA instructs mother what all things she should follow after delivery. Family members get irritated that why she is instructing her”. [ASHA Sahyogini]
“We don't expect much from ASHA since she doesn't know much herself.” [Mother, hard to reach]
“If ASHA asks them for vaccination and child has a mild fever, then they immediately say no. Few people don't behave well with the ASHA.” [ANM]
The majority of the ASHAs felt that they were caught between their domestic (looking after children and husbands, household chores) and professional responsibilities. According to the ASHAs, the non-availability of a mother at the time of the home visit or the mother's engagements with social responsibilities posed additional challenges. Mothers were unhappy that most ASHAs did not maintain a timetable for upcoming home visits or were informed of a home visit beforehand. Many mothers went back to their natal homes after childbirth for 6–12 weeks. As a result, either the HBNC visits remained incomplete, or HBNC Plus visits began late.
“I was having an issue with my mother-in-law because she repeatedly kept asking where I went. I have to tell her that I have to measure weight by going house to house as an ASHA responsibility. Then she allows me to go.” [ASHA]
“Other issues are mother goes to her maternal place along with child or if the child is underweight then she is referred to hospital and sometime ASHA is herself tied up with some work in such cases she is not available to make home visits.” [ASHA Sahyogini]
The health supervisors expressed concern about the ASHA training including residential training (staying away from the residence), curriculum design and its poor translation; and organization of practical skill training. However, most ASHAs and ASHA supervisors did not point out any difficulty in attending residential training. ASHAs and their supervisors reported that the training was insufficient and unsuitable; difficulty in comprehending technical terms related to many health and medical science by the ASHAs with less formal education, the content of the curriculum material, and the pace of knowledge imparting procedures in real-life situations.
“As and when we come back home, then we cannot learn further anything under the supervision and become busy with village and family chores. And after some time, many forget their training.” [ASHA]
“Personally I feel ASHA is not a proper person to identify neonatal sepsis. We have trained we have to define the criteria for what are the danger signs and how to identify them. I think it is difficult for women from the field with a limited knowledge.” [State Officer]
“ASHAs hardly retain about 50% of training.” [ASHA Sahyogini]
One of the most critical determinants of ASHA's credibility and acceptability in the community was its technical competence and communication skills. The ASHAs' inability to recognize sickness in children and the rationale and basis of nutritional and play therapy made it challenging to communicate messages correctly, effectively, and confidently. State and district level stakeholders acknowledged the poor quality of home visits because of the ASHAs' technical and communication competence challenges despite frequent contact. Although half of the ASHAs responded that they don't experience any difficulty performing HBNC/HBNC Plus responsibilities, almost a similar proportion accepted that they encountered problems while making home visits. ASHAs acknowledged that some of the poor response from mothers and family members was on account of their inability to communicate clearly and effectively. Some ASHAs reported having difficulty in performing technical tasks such as measuring temperature, weighing new-born, and making growth charts.
“I don't have enough knowledge to know whether he has a fever or not. We make an idea by seeing whether he is playing or not. [ASHA]
“She is not able to explain when and how much IFA syrup is to be given and why it should be given”. [Block Medical Officer]
“ASHAs hardly retain about 50% of training.” (Echoed by many ASHA Sahyoginis)”
“She is unable to form connectivity. When she goes for a home visit, she talks about general household things such as cooking and does not discuss health services. They forget total about health and wellness issues. It is the main gap.” [District Level ASHA Trainer]
ASHA supervisors claimed that they monitored and supported the ASHA's activities. State and regional managers, however, acknowledged that the supervision of ASHAs was both poor and unsatisfactory because of vacancies in the supervisory cadre (ASHA Supervisors). The HBNC/HBNC Plus performance formats/reports were reviewed infrequently and supervision was of limited utility. The program managers strongly contended that state and district-level officers should also visit the field to understand and address the managerial bottlenecks. Block and community-level stakeholders mentioned the availability of a limited mobility budget for monitoring was also a hurdle in program monitoring.
“Supportive Supervision is one of the weakest links in-home visitation, which was the strongest in the Abhay Bang Gadchiroli project.” [National level stakeholder].
“At the block level, we have to check the filled forms; we are unable to check it properly due to a high number of forms being submitted at the block level every month. It becomes difficult to review all the forms properly.” [Block community mobilizer]
ASHAs, their supervisors, and senior officers consistently accepted that the tasks assigned to ASHAs were complex. The ASHAs were imparted limited exposure to planning and prioritization exercises during training. Not infrequently, ASHAs re-prioritized their work based on directives from higher-ups for health and non-health exigencies beyond the planned activities. Vacancies and rapid turnover among ASHAs and vacant positions in supervisory cadres added to poor planning and management.
“ASHA has many other responsibilities, prioritization and non-adherence to the schedule should be seen in that context.” (Echoed by many ASHA Sahyoginis)
“There are 5-10 percent vacancies for the post of ASHA Sahyogini, ASHA, and BM (block mobilizer)” [Programme Officer]
Irregular and insufficient supply of products (such as ORS and IFA syrup) and stationery adversely affected the HBNC/HBNC Plus related functioning of the ASHAs. The managers attributed this to distribution process-related challenges and delays by ASHAs to indent the supplies.
“Last year in January, my BP and weighing machine were not working. So I deposited in last February, and I got this February.” [ASHA]
ASHAs are remunerated on the basis of the completed tasks (such as vaccination or home visits). Most ASHAs complained about the delay in receiving the incentives. The factors identified for the delays included: late receipt of funds, inability to fill the records appropriately, and refusal by the families to comply with their advice regarding immunization and sickness and hospital referrals. On the other hand, supervisors pointed to the challenges in releasing the incentives due to incorrect and incomplete maintenance of records and mismatch between claims and feedback from the field; shortage of funds was infrequent and not considered as significant concern. While most of the ASHAs and ASHA Supervisors reported receipt of only 50 percent to 70 percent of their entitled monthly incentives, the managers at the district level didn't agree with it and claimed that the full amount was distributed. The family members of ASHAs were reportedly unhappy about the lesser amount of incentives, delay in payments, and being paid less than other frontline workers (e.g., Anganwadi workers); which pose challenge in obtaining adequate support from their own family itself to perform the duties.
“We get money after 2 or 3 months, and it's not monthly. Everyone gets after this much time. When we say this to sir, he says that I am the only person managing it, so delay happens, and there is no such work for which we should pay early.” [ASHA]
The ASHAs and several program managers at different levels acknowledged the hurdles related to reaching outlying and hamlets, tribal areas, and areas with hilly terrain. Few of the ASHAs were not from the same village communities (though this is an essential mandate) and therefore needed to travel to their place of work.
“Tribal population is living in far off areas. So need a strategy for better reach”. [NIPI Programme Officer]
“Some villages are too big, and houses are scattered. The area might be split into smaller ASHA jurisdictions.” [PHC Medical Officer]
The details of the discussion held during the preliminary two caste-specific NPMs are presented in Table 2. The purpose of the NPMs was to identify the strategies to negotiate these challenges of the constructs by each of the social groups and help ASHAs better accomplish their other tasks in their community settings. The emerging themes and potential solutions were noted for both caste sub-groups. Most of the obstacles and the suggested approaches to overcome were similar across the groups, the lower and higher caste groups. The lower caste groups came up with suggestions to mitigate the caste and religion-related biases through awareness generation about the purpose of ASHAs' home visitations. Awareness regarding the value of home visitation and the role of ASHAs were considered essential for men from all communities, elder women who are particularly prejudiced, and the village leadership. The higher caste groups made additional recommendations on earning respect for ASHA by imparting her technical competence and good communication skills that would facilitate acceptance and performance. Through these collective efforts and discussions, we synthesized a broad range of views echoed by participants of the NPMs. The recommendations facilitated building contextual ownership and finding solutions to the barriers in making home visitation by the ASHAs.
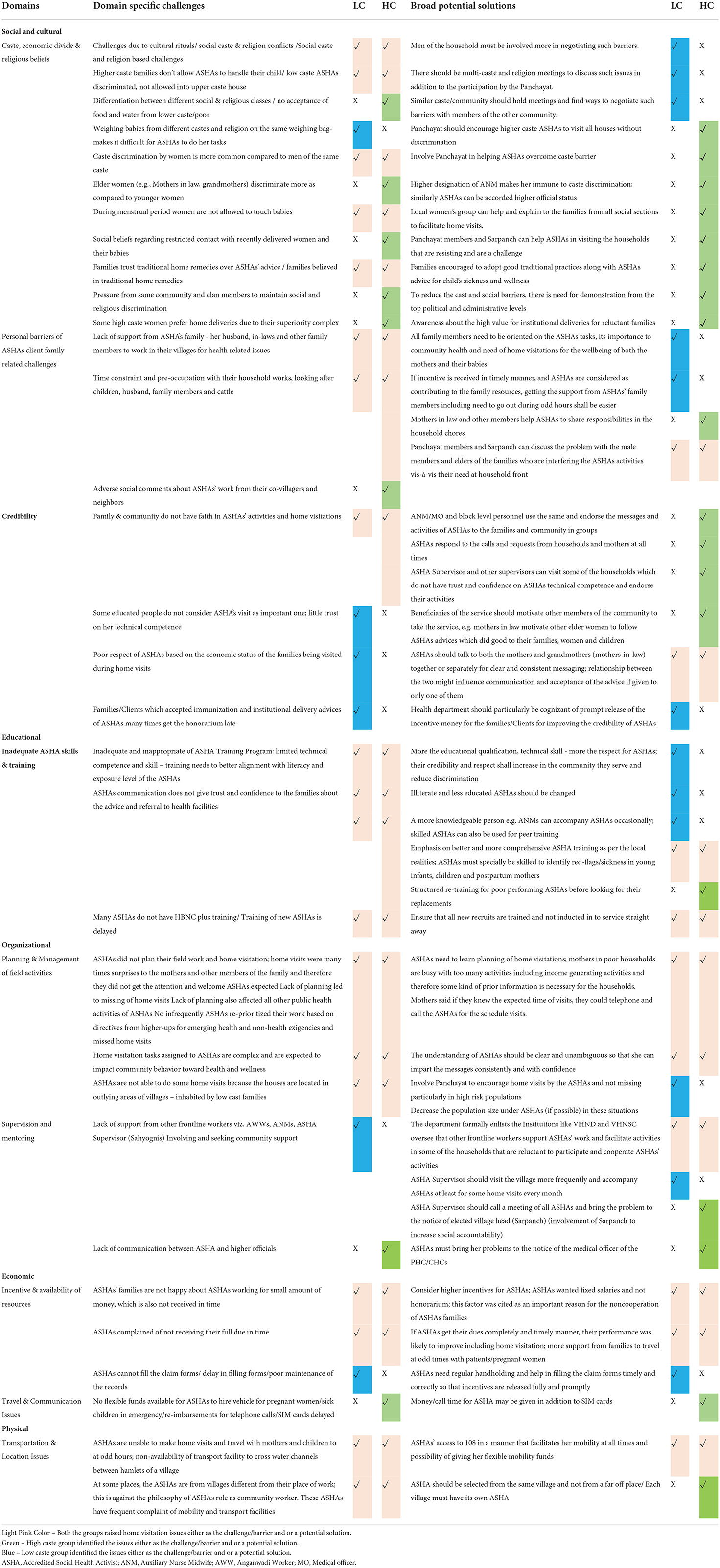
Table 2. Preliminary nexus planning meetings with stakeholders (community, families, parents, ASHAs) separately with the lower caste (LC) and higher caste (HC) groups: summary of issues influencing home visitation by the ASHAs under HBNC & HBNC Plus programs.
The larger NPM group framed the recommendation at two levels: (i) administrative and organizational level; and (ii) community/family level. Task-oriented skill-building of ASHAs along with frequent re-orientation through supportive supervision and handholding was considered essential to improve ASHA performance, get her rightful place in her own family and the community, and even reduce caste-based prejudices. This will require re-engineering of the whole training curriculum in a manner that is aligned to the objectives of the HBNC and HBNC Plus programs. The ASHA was expected to prepare a micro-plan for her activities and communicate preventive, promotive, and curative knowledge to the families with confidence and conviction in their homes and community settings. Equally essential was to release the incentive money rightfully due to the ASHAs in a timely and regular manner. The health system was also asked by the nexus group to consider raising the incentive amount or making ASHAs regular salaried employees and consider the possibility of providing them with health insurance. The availability of flexible funds with ASHAs was considered useful for hiring vehicles at odd hours for the transport of sick children and pregnant women when ambulance services were not available. Another significant intervention proposed was increased male engagement in community meetings through village fora like VHND/VHSNC. These fora could help negotiate and reduce social discrimination and also strengthen social accountability (Figure 4).
The study adds to the existing knowledge that societal issues and personal challenges for ASHAs at their home and community fronts are among the more important barriers/challenges that prevented them from completing home visits and associated tasks with quality. The other reasons for incomplete age-appropriate home visits included gaps in the monitoring of ASHA's performance and mentoring system. Almost half of the ASHAs also accepted their lack of confidence in technical knowledge and communication skills. These factors shook community confidence in her capabilities and the importance given to her advice. The field-level staff including the ANMs, AWWs, block mobilizers, and ASHA supervisors strongly endorsed ASHAs viewpoint with particular emphasis on their social and domestic challenges, and importantly these were often overlooked. Mothers, even those never visited by ASHAs at home, felt that, ASHAs also lacked planning skills and consequently did not get the desired support from families for optimum performance.
The interconnectedness and complexity of the challenges in different sectors and aspects of human ecosystem have led to the recognition of the importance of transformative approaches in addressing and achieving sustainability (35). Nexus thinking and scenario planning have changed the way of doing things from linear to integrated and from monocentric to polycentric approaches (36). The novelty of the study is that it provides evidence of the interrelatedness of the multitude of barriers/challenges faced by the ASHAS along with solutions falling under the five nexus framework domains.
NPMs unambiguously recommended managing all the domains synchronously if the ASHA performance was to improve. The study data recommended interventions at the communication, organizational and educational levels to improve the quality of visits through enhanced skills and confidence of the ASHAs. This would necessitate reengineered training and follow up mentoring methods to enhance her credibility and respect in the community and abate to a certain extent the social and religious prejudices against the ASHAs. The social and family commitments of the ASHAs are important and complex challenges and need to be handled through engagement with the community at different levels e.g., Panchayati Raj members and the participation of men and elderly women in their families to help in negotiating ASHA's usefulness to the community with reduction of social discrimination; and enhancing her stature and respect in the community through reinforcement of her technical and communication skills. Incentives alone are insufficient to motivate the ASHAs for better performance as was done for HBNC Plus program. Timely release of due remuneration can be additional factors for motivating the ASHAs and soliciting their family support. The primary focus and responsibility of ASHAs can be better defined: if it remains maternal and child health activities, regular feedback, and monitoring will make them feel more responsible as well as accountable for different components of maternal and child health services.
The majority of the ASHAs in the current study perceived conflict between their domestic and professional responsibilities. Several previous studies have also shown that the personal needs and family commitments of community health workers interfered with their ability to make home visitations regularly and at times convenient to the beneficiaries (37–39). During the NPMs, the participants informed that the credibility and respect for the ASHAs particularly those from lower caste improved, and discrimination was less likely if they were technically competent, were not vague in their advice, and had good communication skills to impart messages with confidence and conviction.
The ASHAs have to navigate societal and cultural prejudices during their fieldwork (38) and household visits beyond their own “beradari” (caste/tribe/community group) were either not appreciated or trusted (40, 41). Another study reported maximum odds of getting ASHA's services if she belonged to a lower caste as she did not hesitate to visit a household from any community. In the present study, the reluctance to visit low caste households was more among the ASHAs from a higher caste (42). Communities are likely to trust their health workers if they are seen as part of the same community and background (43–46). The trust deficit compounded if ASHA's competence is suspected (47). Probandri et al. observed traditional practices related to the care of the new mother-child dyads also influenced the utilization of postpartum care advice and services. The social architecture further reinforced such practices when the mothers or mothers-in-law, members of the extended families, neighbors, and communities lived in the same or adjoining houses (48).
Mentoring and hand-holding emerged as important tools for the ASHAs' performance and quality of home visitations in several studies. Gilson et al. reported that high-quality supervision helped in the restoration and sustenance of trust of the community in the health system and its services (49). In a study from Ghana, 81% of the midwives had not been visited by their supervisors in time (50). Lack of supervision led to poor technical skills (51), stock-outs, and problems arising out of human resource deficit (52). The other reasons for the poor quality of home visitations were: inconsistent and non-reliable health messages, ‘always in hurry' attitude of the health worker during home visits, difficulty in contacting them when in need, non-provision of relevant health education materials, non-adherence to follow-up schedule (53, 54), and unwelcoming attitude toward the ASHAs by family members (55). Nammazi et al. found that knowledge of new born danger signs rapidly declined from 85.5 to 58.9% 1-year post-training and the main predictors of retention of community health worker knowledge were age (≥35 years) and post-primary level of education (56). The final NPM consultation observed that with the low level of education and social status in the community, current training formats were not suited for the ASHAs to acquire an adequate understanding of the complexity of the subject matter, and their subsequent translation in actual conditions. The group strongly recommended the need for re-engineering of training curricula, with a strong focus on technical skill building, developing self-assurance, and contextually understandable communication skills. Similar concerns and recommendations were reported in several other studies as well (57–60).
Complex interconnected challenges when addressed singly, at times may reduce one problem while exacerbating others. Studies have shown that tackling the challenges piecemeal has not helped to improve the ASHA's performance (61, 62). In a recent implementation study, the performance of ASHAs for home visitation and identification of sick young didn't improve significantly despite efforts by district health authorities to improve skill and technical competence (63). In a study by Creanga et al. (64) the mothers avoided accepting services from the ASHAs who couldn't deliver satisfactory quality postnatal home visitation despite having undergone training due to poor communication skills (64). Our study indicated that timely disbursement of incentives not only helped maintain their morale and motivation but also sent a positive message about their worth to their own families. Several studies have demonstrated a strong association between financial incentives and ASHAs performance (65, 66). Lewis and Bahety et al. also reported that low and delayed incentives were considered a major barrier to the service delivery by the ASHAs (67).
This study has some limitations. We applied NPF as a co-creation exercise involving a wide range of stakeholders and sectors for inductively developing a comprehensive understanding of the factors affecting home visitations by the ASHA, and the interrelatedness between barriers and potential solutions. We modified the broad principles of nexus planning for health system strengthening and improving the performance of frontline workers in resource constraint environments which also have deeply entrenched social, cultural, and other contextual factors. The rationale of giving importance and hearing to all the sub-group stakeholders/constituencies separately brought out several items and matters which required joint discussion to arrive at a mutually acceptable way forward. The challenges faced by ASHAs from forward and backward communities were different and had to be handled in a manner that required suggestions from both sides. The nexus approach guided us to identify and pursue synergies between health and non-health sectors i.e., Panchayati Raj [local self-government] recognizing their significant function and responsibilities to iron out some of the socio-cultural and economic biases operating at the village level. The feasibility and widespread applicability of NPF can be a concern. As mentioned above, successful NPF processes are dependent on identifying the sub-groups and sub-constituencies strategically for a series of group meetings/consultations. This will require deep insight into the local cultural, social, economic and, organizational milieu. Notwithstanding these limitations, the nexus framework did provide robust findings which can be triangulated with several published studies albeit done in a piecemeal manner from India and other low and middle- income countries (LMIC) settings. NPF has been successfully applied in environment, urban development, scrum methodology, water-energy-food (WEF) nexus approach in the MENA (Middle East and North Africa) countries, and many other areas for achieving sustainable development goals (SDGs) with sector-specific modifications (68). NPF offers a comprehensive structure for future researchers and implementation scientists to unravel the complexity and layers of health ecosystems and pursue efforts to improve the performance of community health workers. Research is also required to further refine NPF for wider application but its core philosophy should remain intact. Another limitation of the study can be the applicability of the findings from Raisen district to other parts of the state and country and other LMICs. The health indicators particularly related to tasks executed by ASHAs, Raisen falls in the lower one-third of the ranking of the Indian district (26). However, context and geography will continue to influence the relative significance of each of the five nexus domains.
In conclusion, the present study took a 360-degree view of the factors impacting the home visitation and related performance of the ASHAs and nexus planning groups emphatically recommended that each factor had an effect on or was dependent on the other factors and hence the remedies should include a more comprehensive approach rather trying for piecemeal solutions. The study showed that barriers and challenges of ASHAs can be classified under five broad domains. NPF stressed the imperative of approaching these barriers as interlinked challenges and resolution of any one component alone would not facilitate positive change. Future research and implementation agenda roadmap should include simultaneous interventions to improve the technical and communication skills to build the confidence of the ASHAs through reengineered training and follow-up mentoring methods; which is likely to enhance her credibility and respect in the community and abate a certain extent the social and religious prejudices against her. The social and family commitments of the ASHAs are important and complex challenges and need to be handled through engagement with the community at different levels. Another useful research agenda can be to determine the applicability of NPF in diverse settings and health system challenges.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Ethics approval was obtained from the independent Ethics Committee of the INCLEN Trust International, New Delhi [DCGI reg no: ECR/109/Indt/DL/2014/RR-17]. Written informed consent to participate in this study was provided by the participants. Informant identity during the data analysis was kept anonymized. Verbal consent was taken from community representative and individual to participate in the nexus group meeting.
NA designed the study. Data curation was done by VD, SJ, AP, RD, SC, KG, SB, BH, MD, RM, RS, and PS. Data analysis was done by NA, VD, SJ, AP, RD, and SC. NA, VD, and SJ prepared the first version of the manuscript. All authors provided comments on subsequent drafts and approved the final version of the manuscript.
This work was supported by the Norway India Partnership Initiative (NIPI). [IND-16/0003 study of HBNC plus Project].
We acknowledge and thank the team who collected data. We are grateful to the Ministry of Health and Family Welfare, Madhya Pradesh and Raisen district authorities, health providers, managers, community representatives, and families who generously shared their time and insight in this research. We would also like to thank the members of the Norwegian India Partnership Initiative (NIPI) for their constant support.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ASHA, Accredited Social Health Activists; ANM (Auxiliary nurse midwives, ; AWW, Aganwadi worker; BPM, Block program manager; BCM, Block community mobilizer; CDPO, Child Development Project Officer; DIO, District immunization officer; FGD, Focus group discussion; HBNC, Home-based newborn care; IFA, Iron and folic acid; IDI, In-depth-Interviews; LMIC, Low and middle income countries (LMIC); MENA, Middle East and North Africa; NPF, Nexus Planning Framework; NIPI, Norwegian India Partnership Initiative; ORS, Oral rehydration solutions; SDG, Sustainable development goals; VHSNC, Village Health Sanitation &; Nutrition Committee, ; WEF, Water-energy-food.
1. Babyar JC. Design matters in home visiting improvement. Int J Commun Med Public Health. (2017) 4:4370–6. doi: 10.18203/2394-6040.ijcmph20175307
2. Ashwell HE, Barclay, L. Outcome evaluation of community health promotion intervention within a donor funded project climate in Papua. New Guinea Rural Remote Health. (2009) 9:12–9. doi: 10.22605/RRH1219
3. Bronfenbrenner U. Ecological systems theory. In R. Vasta (Ed.), Six Theories of Child Development, 187–249. London: Kingsley (1992).
4. Yoshikawa H. Long-term effects of early childhood programs on social outcomes and delinquency. The Future Child. (1995) 5:51–75. doi: 10.2307/1602367
5. Olds DL, Kitzman H. Review of research on home visiting for pregnant women and parents of young children. The Future of Children. (1998) 3:53–92. doi: 10.2307/1602543
6. Chapman J, Siegel E, Cross A. Home visitors and child health: analysis of selected programs. Pediatrics. (1990) 85:1059–68. doi: 10.1542/peds.85.6.1059
7. Magwood O, Kpadé V, Thavorn K, Oliver S, Mayhew AD, Pottie K. Effectiveness of home-based records on maternal, newborn and child health outcomes: A systematic review and meta-analysis. PLoS One. (2019) 1:e0209278. doi: 10.1371/journal.pone.0209278
8. Lassi ZS, Kumar R, Bhutta ZA. Community-Based Care to Improve Maternal, Newborn, and Child Health. In: Black RE, Laxminarayan R, Temmerman M, etal., editors. Reproductive, Maternal, Newborn, and Child Health: Disease Control Priorities, Third Edition. Washington (DC): The International Bank for Reconstruction and Development. (2016) Chapter 14, The World Bank. doi: 10.1596/978-1-4648-0348-2_ch14
9. Baqui AH, El-Arifeen S, Darmstadt GL, Ahmed S, Williams EK, Seraji HR, et al. Effect of community-based newborn-care intervention package implemented through two service-delivery strategies in Sylhet district, Bangladesh: a cluster-randomized controlled trial. The Lancet. (2008) 371:1936–44. doi: 10.1016/S0140-6736(08)60835-1
10. Peacock S, Konrad S, Watson E, Nickel D, Muhajarine N. Effectiveness of home visiting programs on child outcomes: a systematic review. BMC Public Health. (2013) 13:1–14. doi: 10.1186/1471-2458-13-17
11. Nandan D. National rural health mission: turning into reality. Indian J Commun Med. (2010) 35:453–4. doi: 10.4103/0970-0218.74338
12. India's MoH launches initiative to finance institutional deliveries. Available online at: https://www.who.int/pmnch/media/news/2011/20110601_govt_india/en/ (accessed June, 2022).
13. Home Based Newborn Care Operational Guidelines (Revised 2014). Ministry Of health and family Welfare. Available from https://www.healthynewbornnetwork.org/hnn-content/uploads/Revised_Home_Based_New_Born_Care_Operational_Guidelines_2014.pdf (accessed June, 2022).
14. Pappu K, Kumar H. N Pradhan, Misra A, Brusletto K. Experiences with implementation of a district-based comprehensive newborn care package. J Neonatol. (2011) 25:98–101. doi: 10.1177/0973217920110210
15. Bang AT, Bang RA, Battule SB, Reddy MH, Deshmukh MD. Effect of home-based neonatal care and management of sepsis on neonatal mortality: field trial in rural India. Lancet. (1999) 354:1955–61. doi: 10.1016/S0140-6736(99)03046-9
16. S Gogia and H Sachdev. Home-based neonatal care by community health workers for preventing mortality in neonates in low- and middle-income countries: a systematic review. J Perinatol. (2016) 36:S55-73. doi: 10.1038/jp.2016.33
17. Kumar SM. A Kumar, M Rajendra, P Misra, M Santosham. Effect of community-based behaviour change management on neonatal mortality in Shivgarh, Uttar Pradesh, India: a cluster-randomised controlled trial. Lancet. (2008) 372:1151–62. doi: 10.1016/S0140-6736(08)61483-X
18. Evaluation of Accredited Social Health Activists (ASHA). Press information bureau, Government of India, Ministry of Health and Family Welfare. (2015) Available online at: https://pib.gov.in/newsite/PrintRelease.aspx?relid=116029
19. Ministry Ministry of Health and Family Welfare Government Government of India. Health Management Information System: Performance of Key HIMS Indicators 2018–2019. Available online at: https://nrhm-mis.nic.in/hmisreports/frmstandard_reports.aspx (accessed June 2022).
20. Baseline report. Impact evaluation of the Norway India partnership initiative phase-II for maternal and child health. (2014). Oxford policy management Limited and Sambodhi Research and Communications: Delhi. Available online at: https://info.undp.org/docs/pdc/Documents/IND/00073062-Baseline%20report_Impact%20Evaluation-NIPI%20Ph%20II-00086024.pdf (accessed July 2022).
21. Glenton C, Colvin CJ, Carlsen B, Swartz A, Lewin S, Noyes J, et al. Barriers and facilitators to the implementation of lay health worker programmes to improve access to maternal and child health: qualitative evidence synthesis. Cochrane Database Sys Rev. (2013) 10:CD010414. doi: 10.1002/14651858.CD010414.pub2
22. Bingler S. Rebuilding for the Community in New Orleans, CELE Exchange, Centre for Effective Learning Environments, No. 2010/14. Paris:OECD Publishing (2010).
23. Arokiasamy P, Gautam A. Neonatal mortality in the empowered action group states of India: trends and determinants. J Biosoc Sci. (2008) 40:183–201. doi: 10.1017/S0021932007002623
24. SDG India Index & Dashboard National Institution for Transforming India (NITI) Aayog government government of India. (2019). OECD Publishing. https://www.niti.gov.in/sites/default/files/2020-07/SDG-India-Index-2.0.pdf
25. Bora JK, Saikia N. Neonatal and under-five mortality rate in Indian districts with reference to Sustainable Development Goal 3: An analysis of the National Family Health Survey of India (NFHS). PLoS One. (2018) 13:e0201125. doi: 10.1371/journal.pone.0201125
26. National Family Health Survey (NFHS-4) (2015–16) India. Mumbai: IIPS. International Institute for Population Sciences (IIPS) and ICF. 2017. Available online at: https://dhsprogram.com/pubs/pdf/FR339/FR339.pdf (accessed June 2022).
27. Operational guidelines. Home based care for young child (HBYC). Strengthening of health & Nutrition through home visits. Joint initiative by Ministry of Health and family Welfare & Ministry of Women and Child Development, Delhi, India (2018).
28. Das MK, Arora NK, Gaikwad H, Chellani H, Debata P, Rasaily R, et al. Grief reaction and psychosocial impacts of child death and stillbirth on bereaved North Indian parents: a qualitative study. PLoS ONE. (2021) 16:e0240270. doi: 10.1371/journal.pone.0240270
29. Strauss A, Corbin J. Basics of qualitative research: Grounded theory procedures and technique, 2nd Edition. Newbury Park, London: SAGE Publications (1998).
30. Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago: Aldine Publishing Company (1996).
31. Dasgupta R, Chaturvedi S, Adhish SV, Ganguly KK, Rai S, Sushant L, et al. Social determinants and polio ‘Endgame': a qualitative study in high risk districts of India. Indian Pediatr. (2008) 45:357–65.
32. Deshmukh V, John S, Arora NK. Utilization of postnatal healthcare services delivered through home visitation and health facilities for mothers and newborns: an integrative review from developing countries. The Indian Journal of Paediatrics. (2020) 87:207–16. doi: 10.1007/s12098-019-03101-4
33. Nhamo L, Ndlele B. Nexus planning as pathway towards sustainable environmental and human health post covid-19. Environ Res. (2021) 192:110376. doi: 10.1016/j.envres.2020.110376
34. Gondhalekar D, Erlbeck R. Application of the nexus approach as an integrated urban planning framework: from theory to practice and back again. Front Sust Cities. (2021) 3:751682. doi: 10.3389/frsc.2021.751682
35. Burch S, Gupta A, Inoue CY, Kalfagianni A, Persson A, Gerlak AK, et al. New directions in earth system governance research. Earth Sys Govern. (2019) 1:100006. doi: 10.1016/j.esg.2019.100006
36. Nyström ME, Karltun J, Keller C, Gäre BA. Collaborative and partnership research for improvement of health and social services: researcher's experiences from 20 projects. Health Res Pol Sys. (2018) 16:1–17. doi: 10.1186/s12961-018-0322-0
37. Kawade A, Gore M, Lele P, Chavan U, Pinnock H, Smith P, et al. Interplaying role of healthcare activist and homemaker: a mixed-methods exploration of the workload of community health workers (Accredited Social Health Activists) in India. Human Res Health. (2021) 19:7. doi: 10.1186/s12960-020-00546-z
38. Saprii L, Richards E, Kokho P, Thebald S. Community health workers in rural India: analysing the opportunities and challenges accredited social health activists (ASHAs) face in realising their multiple roles. Hum Resour Health. (2015) 13:95. doi: 10.1186/s12960-015-0094-3
39. Oliver M, Geniets A, Winters N, Rega I, Mbae SM. What do community health workers have to say about their work, and how can this inform improved programme design? A case study with CHWs within Kenya. Glob Health Action. (2015) 8:27168. doi: 10.3402/gha.v8.27168
40. Sarin E, Lunsford SS. How female community health workers navigate work challenges and why there are still gaps in their performance: a look at female community health workers in maternal and child health in two Indian districts through a reciprocal determinism framework. Hum Resour Health. (2017) 15:44. doi: 10.1186/s12960-017-0222-3
41. Mumtaz Z, Salway S, Nykiforuk C, Bhatti A, Ataullahjan A, Ayyalasomayajula B. The role of social geography on lady health workers' mobility and effectiveness in Pakistan. Soc Sci Med. (2013) 91:48–57. doi: 10.1016/j.socscimed.2013.05.007
42. Sharma R, Webster P, Bhattacharyya S. Factors affecting the performance of community health workers in India: a multi-stakeholder perspective. Glob Health Action. (2017) 7:25352. doi: 10.3402/gha.v7.25352
43. Seth A, Tomar S, Singh K, Chandurkar D, Chakraverty A, Dey A, et al. Differential effects of community health worker visits across social and economic groups in Uttar Pradesh, India: a link between social inequities and health disparities. Int J Equity Health. (2017) 16:46. doi: 10.1186/s12939-017-0538-6
44. George A, Menotti EP, Rivera S, Marsh DR. Community case management in Nicaragua: lessons in fostering adoption and expanding implementation. Health Policy Plan. (2011) 26:327–37. doi: 10.1093/heapol/czq048
45. Kaler A, Watkins SC. Disobedient distributors: Street-level bureaucrats and would-be patrons in community-based family planning programs in rural Kenya. Stud Fam Plann. (2001) 32:254–69. doi: 10.1111/j.1728-4465.2001.00254.x
46. Heaman M, Chalmers K, Woodgate, R. Early childhood home visiting programme: factors contributing to success. J Adv Nurs. (2006) 55:291–300. doi: 10.1111/j.1365-2648.2006.03914.x
47. Davies, H. Falling public trust in health services: implications for accountability (editorial). J Health Ser Res Pol. (1999) 4:93–194. doi: 10.1177/135581969900400401
48. Probandari A, Arcita A, Kothijah K, Pamungkasari EP. Barriers to utilization of postnatal care at village level in Klaten district, central Java Province, Indonesia. BMC Health Serv Res. (2017) 17:541. doi: 10.1186/s12913-017-2490-y
49. Gilson L. Trust in health care: theoretical perspectives and research needs. J Health Organ Manag. (2006) 20:359–75. doi: 10.1108/14777260610701768
50. Frimpong JA, Helleringer S, Awoonor-Williams JK, Yeji F, Phillips JF. Does supervision improve health worker productivity? Evidence from the upper East region of Ghana. Trop Med Int Health. (2011) 16:1225–33. doi: 10.1111/j.1365-3156.2011.02824.x
51. Pepperall J, Garner P, Fox-Rushby J, Moji N, Harpham T. Hospital or health centre? A comparison of the costs and quality of urban outpatient services in Maseru, Lesotho. Int J Health Plann Manag. (1995) 10:59–71. doi: 10.1002/hpm.4740100106
52. Neogi SB, Sharma J, Chauhan M, Khanna R, Chokshi M, Srivastava R, et al. Care of new-born in the community and at home. J Perinatol. (2016) 36:S13–7. doi: 10.1038/jp.2016.185
53. Lomoro OA, Ehiri JE, Qian X, Tang SL. Mothers' perspectives on the quality of postpartum care in Central Shanghai, China. Int J Quality Health Care. (2002) 4:393–401. doi: 10.1093/intqhc/14.5.393
54. McLellan J, Laidlaw A. Perceptions of postnatal care: factors associated with primiparous mothers perceptions of postnatal communication and care. BMC Preg Childbirth. (2013) 13:227. doi: 10.1186/1471-2393-13-227
55. Paphassarang CE. privatization and cost recovery in urban health care: the case of Lao PDR. Health Policy Plan. (2002) 17:72–84. doi: 10.1093/heapol/17.suppl_1.72
56. Namazzi G, Okuga M, Tetui M, Kananura RM, Kakaire A, Namutamba S, et al. Working with community health workers to improve maternal and newborn health outcomes: implementation and scale-up lessons from eastern Uganda. Glob Health Action. (2017) 10:1345495. doi: 10.1080/16549716.2017.1345495
57. Ganguly E, Garg BS. Quality of health assistants in primary health centers in rural Maharashtra, India. Health Serv Insig. (2013) 6:9–13. doi: 10.4137/HSI.S11226
58. Okuga M, Kemigisa M, Namutamba S, Namazzi G, Waiswa P. Engaging community health workers in maternal and new-born care in eastern Uganda. Glob Health Action. (2015) 8:23968. doi: 10.3402/gha.v8.23968
59. Crisp N, Gawanas B, Sharp I. Training the health workforce: scaling up, saving lives. Lancet. (2008) 371:689–91. doi: 10.1016/S0140-6736(08)60309-8
60. Tinker A, Hoope-Bender P, Azfar S, Bustreo F, Bell R, A. continuum of care to save new-born lives. Lancet. (2005) 365:822–5. doi: 10.1016/S0140-6736(05)71016-3
61. Rowe SY, Kelly JM, Olewe MA. Kleinbaum, McGowan JE, McFarland DA, et al. Effect of multiple interventions on community health workers' adherence to clinical guidelines in Saiya district, Kenya. Transact Royal Soc Trop Med Hyg. (2007) 101:188–202. doi: 10.1016/j.trstmh.2006.02.023
62. Scott K, George AS, Ved RR. Taking stock of 10 years of published research on the ASHA programme: examining India's national community health worker programme from a health systems perspective. Health Res Pol Sys. (2019) 17:29. doi: 10.1186/s12961-019-0427-0
63. Mukhopadhyay R, Arora NK, Sharma PK, Dalpath S, Limbu P, Kataria G, et al. Lessons from implementation research on community management of Possible Serious Bacterial Infection (PSBI) in young infants (0–59 days), when the referral is not feasible in Palwal district of Haryana, India. PLoS ONE. (2121) 16:e0252700. doi: 10.1371/journal.pone.0252700
64. Creanga AA, Gullo S, Kuhlmann AKS, Msiska TW, Galavotti C. Is quality of care a key predictor of perinatal health care utilization and patient satisfaction in Malawi? BMC Preg Childbirth. (2017) 17:150. doi: 10.1186/s12884-017-1331-7
65. Scott K, Shanker S. Tying their hands? Institutional obstacles to the success of the ASHA community health worker programme in rural north India. AIDS Care. (2010) 2:1606–12. doi: 10.1080/09540121.2010.507751
66. Joshi S, Mathews G. Healthcare through community participation: role of ASHAs. Econ Political Weekly. (2012) 47:70–6.
67. Newton-Lewis TA, Bahety G. Evaluating the effectiveness of Community Health Worker home visits on infant health: a quasi-experimental evaluation of home based newborn care plus in India. J Glob Health. (2021) 11:04060. doi: 10.7189/jogh.11.04060
Keywords: home visitation, new-born care, community health worker (CHW), ASHAs (accredited social health activists), India, nexus planning
Citation: Deshmukh V, John S, Pakhare A, Dasgupta R, Joshi A, Chaturvedi S, Goswami K, Das MK, Mukhopadhyay R, Singh R, Shrivastava P, Dhingra B, Bingler S, Hill BP and Arora NK (2022) Barriers in reaching new-borns and infants through home visits: A qualitative study using nexus planning framework. Front. Public Health 10:956422. doi: 10.3389/fpubh.2022.956422
Received: 30 May 2022; Accepted: 19 August 2022;
Published: 29 September 2022.
Edited by:
Andrew Steenhoff, Children's Hospital of Philadelphia, United StatesReviewed by:
Mathilde Crone, Leiden University Medical Center (LUMC), NetherlandsCopyright © 2022 Deshmukh, John, Pakhare, Dasgupta, Joshi, Chaturvedi, Goswami, Das, Mukhopadhyay, Singh, Shrivastava, Dhingra, Bingler, Hill and Arora. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Narendra K. Arora, bmthcm9yYUBpbmNsZW50cnVzdC5vcmc=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.