- 1School of Public Health, Guizhou Medical University, Guiyang, China
- 2Guiyang Public Health Clinical Center, Guiyang, China
- 3Second Affiliated Hospital of Guizhou University of Traditional Chinese Medicine, Guiyang, China
- 4School of Humanities and Management, Institute for Health Law and Policy, Guangdong Medical University, Dongguan, China
- 5Primary Health Department of Guizhou Provincial Health Commission, Guiyang, China
- 6School of Medicine and Health Management, Guizhou Medical University, Guiyang, China
Background: Inappropriate use of glucocorticoids in primary care institutions is serious. It not only causes economic burden, but leads to many adverse reactions. The purpose of this study is to explore systemic glucocorticoid prescription pattern and factors of inappropriate use in primary care institutions.
Methods: This is a retrospective study. Systemic glucocorticoids prescribed in 58 primary care institutions in Guizhou province of Southwest China in 2020 were selected from the Health Information System. All prescriptions were classified as appropriate or inappropriate use. Inappropriate use was classified into the following two categories: (a) Inappropriate indications; (b) Inappropriate selection of glucocorticoids. Multivariate analysis was used to explore the factors associated with inappropriate use of systemic glucocorticoids.
Results: A total of 63,315 glucocorticoid prescriptions were included in the analysis. Diseases of the respiratory system (60.8%) and diseases of the skin and subcutaneous tissue (23.1%) were the most common indications for use. Injections (89.8%) predominated and dexamethasone (86.5%) was the most prescribed glucocorticoid. 68.2% of all prescriptions were inappropriate. Compared to physicians with a college degree, physicians with a junior college (OR: 1.12, 95% CI: 1.08–1.17) and technical secondary education (OR: 1.12, 95% CI:1.05–1.19) were more likely to prescribe glucocorticoids inappropriately as were attending physicians (OR: 1.12, 95% CI: 1.01–1.25) and resident physicians (OR: 1.31, 95% CI: 1.15–1.48) compared to associate chief physicians. The risk of inappropriate glucocorticoid use was highest in patients 65 years of age and older (OR: 6.00, 95% CI: 5.62–6.40). In contrast, prescriptions given by injection were more likely to be used inappropriately than those given orally (OR: 0.44, 95% CI: 0.41–0.46).
Conclusion: Inappropriate use of systemic glucocorticoids without appropriate indications was extremely prominent in primary care institutions of Guizhou Province, especially in diseases of the respiratory system and among the elderly. The risk of inappropriate glucocorticoid use was highest in patients 65 years of age and older. It is important to note that physicians younger than 33, with more than 40 years of service, and attending or residents were more likely to inappropriately prescribe glucocorticoids.
Introduction
Since 1950, systemic glucocorticoids have been widely used to treat various inflammatory and autoimmune diseases, such as asthma, chronic obstructive pulmonary disease, and rheumatoid arthritis (1, 2). Although systemic glucocorticoids (oral or injection) play a significant role in clinical treatment, their inappropriate use can induce adverse consequences such as adrenal insufficiency, osteoporosis, hypertension, Cushing's syndrome, and gastrointestinal bleeding, which could increase the burden on medical care and even endanger the patient's life (3–12). Therefore, systemic glucocorticoids should be used strictly according to their indication (13).
Over the past 20 years, prescriptions for oral glucocorticoids have risen by 34% in the United Kingdom (14). Among 113 patients surveyed in India, 88.4% of glucocorticoids were considered inappropriate, including imprecise diagnosis and incorrect indications by standard clinical and evidence-based practice guidelines (15). In France, oral glucocorticoid prescription rates are over 17%, yet most were inappropriately used (16). In the United States, systemic glucocorticoids were used in more than 11% of acute respiratory tract infections, yet guidelines failed to support this practice (17). Inappropriate use of glucocorticoids is also common in China (18, 19), and this phenomenon is more prominent in primary care institutions (20, 21). A previous study reported that glucocorticoids accounted for 63.5% of inappropriate prescriptions in 27 primary care institutions (22). In order to promote the rational use of glucocorticoids, the Chinese government promulgated the clinical use guidelines of glucocorticoids as early as 2011 (23), but the expected effects have not been achieved in primary care institutions (20, 21).
Previous studies have focused on oral glucocorticoid prescribing patterns in adults, including trends in the prevalence of oral glucocorticoids (14, 16, 24, 25), common indications for glucocorticoids therapy (14, 25, 26), and common types of glucocorticoids use (14, 27). A recent study reported characteristics of patients and their association with inappropriate use of systemic glucocorticoids in upper respiratory tract infections (28). Several studies (15, 29, 30) have also focused on the inappropriate use of systemic glucocorticoids in primary care institutions. Other studies have described prescribing patterns of topical glucocorticoids (31–35), and factors associated with their inappropriate use (36–39). However, few studies have comprehensively examined the prescription patterns and factors associated with inappropriate use of systemic glucocorticoid in primary care institutions.
Therefore, we conducted an in-depth analysis on the prescription of systemic glucocorticoids in primary care institutions in Southwest China. The objective of this study is to describe the prescription patterns and determine associated factors for the inappropriate use of systemic glucocorticoids. The influencing factors of inappropriate use of systemic glucocorticoids were analyzed from the perspective of physicians and patients.
Materials and methods
This study was approved by the Ethics Committee of Guizhou Medical University (REC. 2021 Ethics Approval No. 249).
Study setting
The retrospective study was conducted in Guizhou, one of the poorest provinces in Southwest China. In China, the public hospital system consists of three levels from top to bottom: tertiary hospitals, secondary hospitals, and primary care institutions. Primary care institutions include township health centers and community health service centers. Primary care institutions do not require high education and certificates. People who have a technical secondary school degree and pass professional physician training can become junior outpatient physicians. Out of 1,399 township public hospitals in Guizhou rural areas, there are 132 hospitals using the same health information system (HIS) that was developed by Guizhou Lianke Weixin Technology Co., LTD (LWTC) authorized by the Information Center of Guizhou Health Commission. Due to the high mobility of primary physicians, our inclusion criteria were: outpatient physicians who had been in the primary care institutions for the whole year of 2020 and had prescribed glucocorticoids. Eventually, 58 eligible primary care institutions were included in this study.
Data retrieval process
Glucocorticoid prescriptions and demographic characteristics of the patients visiting outpatient departments in 2020 were collected in primary care institutions of Guizhou using the HIS. Personal details of the physicians were obtained from the Personnel Management Department of each primary care institution. According to the 10th edition of the International Classification of Diseases (ICD-10) (40), the common related diagnoses were grouped into 5 diagnostic categories (Diseases of the respiratory system; Diseases of the skin and subcutaneous tissue; Diseases of the musculoskeletal system and connective tissue; Diseases of the digestive system; and Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified). Systemic glucocorticoids are more likely to cause side effects than topical glucocorticoids (41). Therefore, we only included systemic glucocorticoids, excluding topical glucocorticoids prescriptions such as nasal inhalation and skin creams. Systemic glucocorticoids were divided into long-acting glucocorticoids such as dexamethasone and betamethasone, intermediate-acting glucocorticoids such as prednisolone, methylprednisolone and triamcinolone, and short-acting glucocorticoids such as hydrocortisone and cortisone (42).
Categorization of appropriateness of glucocorticoids use
As there is no international standard clinical guidelines for glucocorticoids, we referred to the Chinese Clinical Application Guidelines for glucocorticoids (summary of S1 documents), Chinese Ministry of Health Standards for Hospital Prescription Review and Management (summary of S2 documents) and the articles of Liu et al. (42) and Yasir et al. (43). Based on the above guidelines and references, glucocorticoid prescriptions were divided into two broad categories: appropriate and inappropriate. Since HIS did not provide glucocorticoid doses, treatment duration nor patient's characteristics, we could only classify inappropriate use of all prescriptions into the following two categories. (a) Inappropriate indication, such as systemic glucocorticoids prescribed for the common cold, fever, and pain relief; and (b) Inappropriate selection of glucocorticoids, such as short-acting rather than long-acting systemic glucocorticoids.
Statistical analysis
Appropriate and inappropriate prescribing frequencies were calculated to quantify the patterns and appropriateness of systemic glucocorticoid prescriptions. Univariate analysis was performed to initially exclude irrelevant factors of inappropriate use of systemic glucocorticoid. Multivariate analysis under the framework of Generalized Estimating Equations (GEE) was used to further determine independent predictors of inappropriate use of systemic glucocorticoids. All statistical tests were two-sided and a p-value <0.05 was considered statistically significant. R version 4.1.1 was used for all statistical analyses.
Results
A total of 69,554 systemic glucocorticoid prescriptions were retrieved. Prescriptions given to patients with diagnoses in the top five diagnoses accounted for 91.0% of the total prescriptions. For this reason, we included only prescriptions given to these patients, resulting in 63,315 prescriptions in our analysis. The number of patients was 61,500.
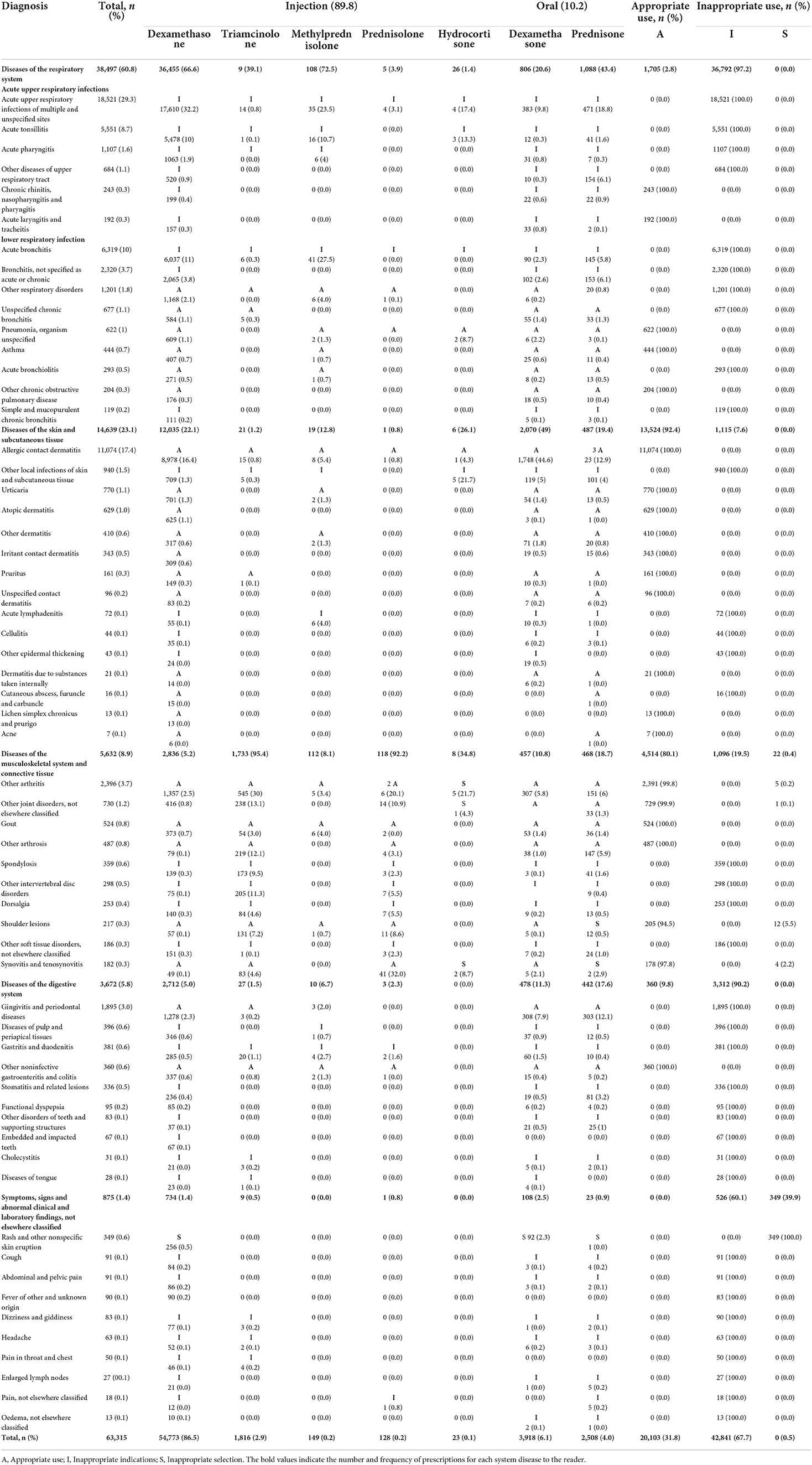
Table 1 shows the distribution of systemic glucocorticoid prescriptions stratified by diagnosis, drugs and rationality. Out of the 63,315 prescriptions, 43,212 (68.2%) were used inappropriately, of which inappropriate indication prescriptions accounted for 67.7% and inappropriate selection of glucocorticoids prescriptions accounted for 0.5%. In the table, “A” represents “Appropriate use”, “I” represents “Inappropriate indications”, “S” represents “Inappropriate selection”. Diseases of the respiratory system (60.8%) was the most common diagnosis, followed by diseases of the skin and subcutaneous tissue (23.1%). Glucocorticoid prescriptions were inappropriate for 97.2% of respiratory diseases and 90.2% of digestive diseases.
There were 20,103 (31.8%) prescriptions for appropriate use of glucocorticoids. The main indications for appropriate use of systemic glucocorticoids were asthma (100%), other chronic obstructive pulmonary disease (100%), skin and subcutaneous tissue diseases (92.4%), and musculoskeletal system and connective tissue diseases (80.1%).
Injection and oral glucocorticoids accounted for 89.8% and 10.2% of all prescriptions, respectively. There were 5 types of glucocorticoids for injection and only 2 types for oral route. Dexamethasone (86.5% and 6.2%) was the most frequently used glucocorticoid for both injection and oral routes.
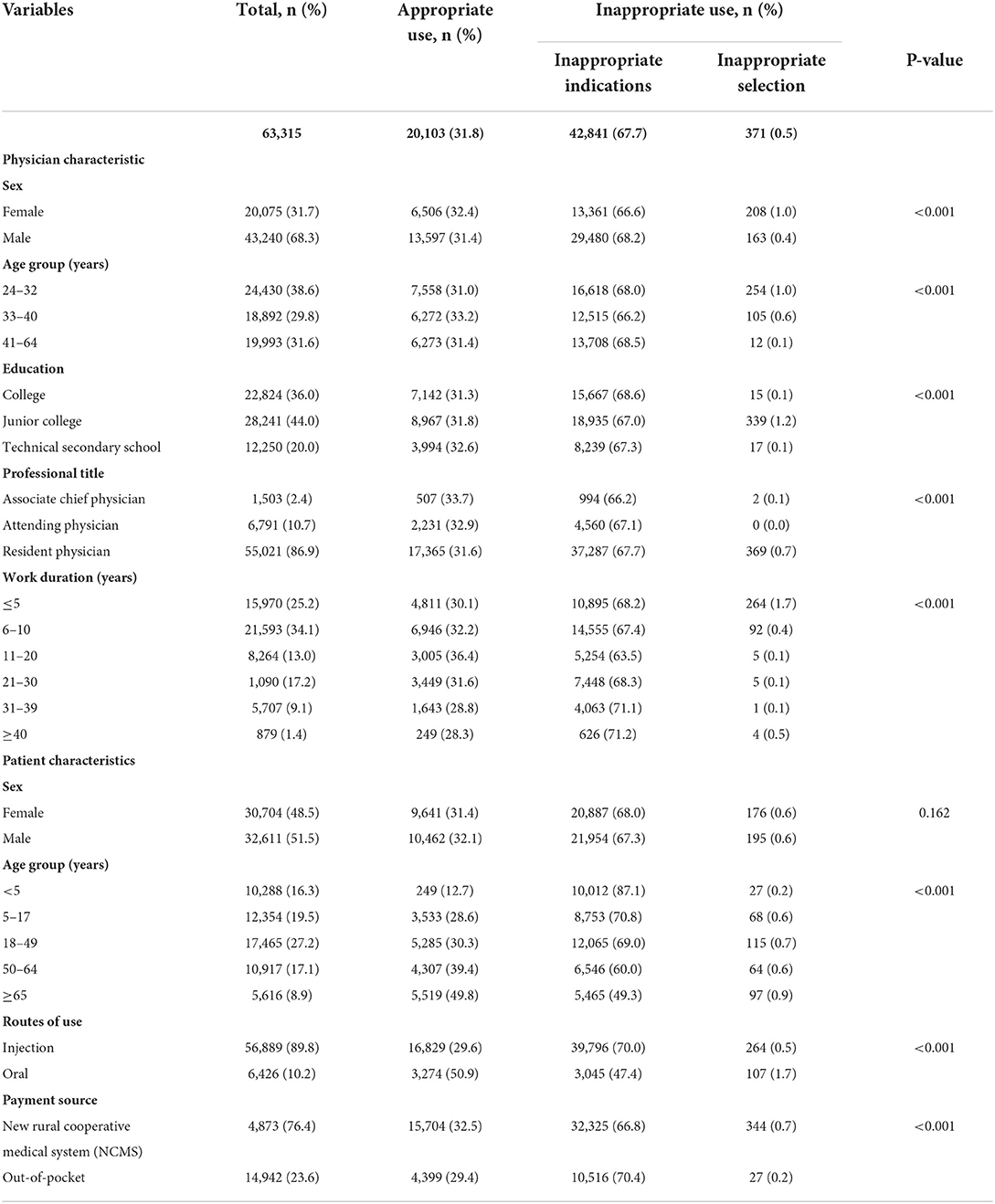
Table 2 compares prescription patterns by physicians' and patients' characteristics. The majority (76.4%) of prescriptions were covered by the new rural cooperative scheme. On univariate analysis, there were significant differences in prescribing patterns among physicians by sex, age group, education, professional title and work duration (P < 0.001). In addition to patients' sex (P = 0.162), the appropriateness of glucocorticoid prescription was also related to patients' age, source of payment and route of use (P < 0.001). Therefore, patients' sex was excluded in the initial multivariate model.
Table 3 shows factors associated with inappropriate glucocorticoids use on multivariate analysis. Physicians who were male or older than 32 years (compared to those aged less than or equal to 32 years) were less likely to prescribe glucocorticoids inappropriately. Physicians with a junior level of education (compared to those who completed a college degree) and attending/resident physicians (compared to associate chief physicians) were more likely to prescribe glucocorticoids inappropriately. Compared to physicians with 5 or fewer years of work duration, those who had worked for 11–39 years were less likely to prescribe glucocorticoids inappropriately. However, physicians with 40 or more years of service were more likely to prescribe glucocorticoids inappropriately. From the patient's perspective, those who were five years of age or older (compared to those younger than 5 years) were more likely to be prescribed glucocorticoids inappropriately and the odds was the highest in patients aged 65 years or more. Injection prescriptions and prescriptions covered by the new rural cooperative medical system had a higher odds of inappropriate use.
Discussion
In this retrospective study, we analyzed 63,315 systemic glucocorticoid prescription patterns in 58 primary care institutions in Guizhou, China. Inappropriate use accounted for 68.2% of all glucocorticoid prescriptions, in which inappropriate indications was the majority (67.7%), and inappropriate selection of glucocorticoids accounted for 0.5%. Diseases of the respiratory system (60.8%) and diseases of the skin and subcutaneous tissue (23.1%) were the most common diagnoses among the patients who received the prescriptions. The proportion of inappropriate prescriptions was higher in diseases of the respiratory system (97.2%) and diseases of the digestive system (90.2%). Most (89.8%) glucocorticoid prescriptions were injected with only 10.2% given orally. Dexamethasone was the most used in both oral (6.2%) and injectable forms (86.5%). The younger physicians were more likely to prescribe inappropriately and the risk of inappropriate prescription was higher for physicians with lower educational and professional titles.
Among all patients prescribed systemic glucocorticoids in this study, prescriptions for diseases of the respiratory system (60.8%) were the most common, of which 97.2% of the prescriptions were inappropriate. A study from Ethiopia (27) showed glucocorticoids were used in 63.5% of respiratory diseases. Another study from China also reported that 60.48% of glucocorticoids were used for respiratory diseases (44). In Puerto Rico, 75% patients with of common colds were prescribed corticosteroids (45). Studies from the US and South Korea reported that 11% and 6.8% of systemic glucocorticoids were used for acute upper respiratory tract infections, respectively (28, 46). However, evidence-based clinical practice guidelines and Centers for Disease Control and Prevention (CDC) (47–51) suggest that systemic glucocorticoids are ineffective in acute respiratory tract infections since respiratory tract infections are usually caused by viruses such as acute bronchitis and acute tonsillitis. These conditions are self-healing with symptomatic treatment.
A previous study of digestive diseases showed an inappropriate rate of 69.0% (52). In this study, inappropriate use of systemic glucocorticoids was also common in diseases of the digestive system (90.2%). The largest number of prescriptions were for gingivitis and periodontal diseases. The main reason for using glucocorticoids was to relieve the patient's pain and reduce swelling during acute attacks. However, gingivitis is caused by the accumulation of substances produced by microbial plaque in or near the gum groove (53). Periodontitis may be associated with bacteria and the herpes viruses (54). Studies have shown that non–operative treatment for gingivitis and periodontitis should begin with special mechanical removal of plaque and calculus. Adjuvant therapy with antibiotics may also be used, but glucocorticoids are not recommended (55–58). In addition, a review study indicated that glucocorticoid use may increase the incidence of periodontitis (58).
In this study, systemic glucocorticoids used for COPD (204, 0.3%), asthma (444, 0.7%), and arthritis other arthritis (2,396, 3.7%), other joint disorders, not elsewhere classified (730,1.2%), other arthrosis (487,0.8 %), respectively. We only analyzed systemic glucocorticoid prescriptions, excluding topical glucocorticoid prescriptions. All diseases are classified according to the first three codes of ICD-10. In fact, these prescriptions for “Other Chronic obstructive pulmonary disease (J44)” contained only “acute exacerbation of undesignated COPD (J44.155) in the HIS”. Short-term, systemic glucocorticoids were prescribed to relieve symptoms. In addition, primary care physicians reported that systemic glucocorticoids are often used in conjunction with bisphosphonates in rheumatoid arthritis or osteoarthritis disease. The STOPP-START criteria mention that moderate to severe asthma or chronic obstructive pulmonary disease should be treated with regular inhaled glucocorticoids rather than long-term systemic glucocorticoids. And long-term use of glucocorticoids for rheumatoid arthritis or osteoarthritis should also be concomitant with bisphosphonates (59). And previous studies have shown that short-term systemic glucocorticoids could be used for remission in severe or acute asthma (60, 61), COPD (62), and arthritis (63, 64). Therefore, we comprehensively considered that short-term use of systemic glucocorticoids in severe COPD and rheumatoid arthritis was appropriate in this study.
Up to 68.2% of systemic glucocorticoids were used inappropriately in this study. A study in China found that 56.55% of glucocorticoid prescriptions were inappropriate (65). Similarly, Masih et al. (15) also reported that 88.4% of glucocorticoids were inappropriately used, which was a common phenomenon in rural areas of India. Due to the difficulty of finding the optimal induction and maintenance doses, glucocorticoids were also commonly misused in systemic lupus erythematosus in Spain (66). A United States study (30) reported that primary physicians often prescribed systemic corticosteroids for no apparent reason. Among the inappropriate prescriptions, 67.7% of prescriptions were inappropriate indications and 0.5% of prescriptions were inappropriate selection of glucocorticoids in this study. This suggests that most primary physicians may not have sufficient knowledge of the indications for glucocorticoids and individual physicians may have poor understanding of the characteristics of glucocorticoid drugs.
Injectable of glucocorticoids (89.8%) was more common than oral glucocorticoids in this study. In China (67), the proportion of glucocorticoids used for injection reached 71.42% while in Serbian (27) 52.6% of systemic glucocorticoid prescriptions were injections. A study reported that 22.5% of acute respiratory infections were treated with intramuscular glucocorticoids in the United States (68). Overuse of injected glucocorticoids not only increases medical costs, but also increases the transmission of iatrogenic diseases and the probability of side effects (21). Generally, systemic glucocorticoids are used in patients with exacerbations or emergencies. However, there is no advanced equipment to assist in the examination or rescuing patients in primary care institutions (69). Once suffering from acute or serious illness, most outpatients will choose to go to higher level health care institutions. Therefore, they are mild in primary care institutions in China. In general, injection glucocorticoids are not necessary in primary care institutions (70, 71). In this study, dexamethasone was the most prescribed glucocorticoid. Li Jia et al. (67) also reported a high prevalence (90.92%) of dexamethasone use in China. This is similar to a study by Masih (15) where dexamethasone (58.3%) is also the most commonly prescribed drug in India.
In our study, physicians younger than 33 years and attending or resident physicians were more likely to prescribe glucocorticoids inappropriately. Most of these physicians are non-undergraduates and their professional knowledge and clinical experience are also inadequate. Physicians with more than 40 years of service were also more likely to prescribe glucocorticoids inappropriately. It has been reported that most elderly physicians in rural China have no formal education (72). In China, most young and middle-aged primary physicians still lack higher education (73). Xu et al. (72) recommended that better welfare policies be set up to attract more highly educated physicians to the countryside while Li et al. (74) suggested that remote education and clinical continuing education could be used to train rural physicians to improve the professional knowledge of physicians.
Inappropriate use of systemic glucocorticoids was also associated with patient's age and route of use in this study. The inappropriate use of glucocorticoids became more pronounced with the patient's age, especially those 65 years and older. In rural China, most elderly citizens lack formal education (75). Education level is positively correlated with health literacy (76, 77). Yuan et al. (78) also reported that rural residents over 65 years old had the lowest rate of health knowledge. In our study, injection glucocorticoids were more likely to be used inappropriately than those given orally. Indeed, it is still widely believed that injections are more convenient and effective than oral drugs (21). Because few people are aware of the harmful consequences of inappropriate use of injections, it is common for patients to request injectable treatment to quickly recover from their disease (79). In addition, glucocorticoid use covered by the New Rural Cooperative Medical scheme were more likely to be inappropriate than those paid out-of-pocket. In rural China, most people have rural health insurance, which reduces the cost of medical care and thus may increase patient's demand for drugs (80). Therefore, health education on the rational use of injections among the general population should be strengthened, and more targeted prescription medication policies and program management in primary care institutions should be formulated. It is also necessary to strengthen the public awareness of the potential risks of glucocorticoids to change traditional consumer attitudes. Dogba et al. (81) proposed the use of information and communication technologies to provide health education to the public in rural and remote areas.
Our study has some limitations. First, the appropriateness of glucocorticoids was classified based on incomplete retrospective data. So far as we know, the HIS of most primary care institutions in less developed areas of China are still being improved, and factors such as dose, treatment time, and patient's disease history are difficult to obtain. It is hoped that future studies will provide a more comprehensive classification of appropriateness. Secondly, as this study was conducted in only one province of China, the results may not be representative of systemic glucocorticoid use in all primary care institutions of China, its representation may not be sufficient. Even so, the study still can be replicated in areas of countries like the study, the results of the study are consistent with those set out in the objectives and the size of the sample allows these objectives to be measured, reaching the final conclusions. Thirdly, there is no international clinical medication guidelines for glucocorticoids at present, so the results of our evaluation might be inconsistent with the medication practices of other countries. We therefore call for the formulation of more comprehensive guidelines for the clinical use of glucocorticoids to promote their rational use and reduce the occurrence of adverse side effects.
Conclusion
The inappropriate use of systemic glucocorticoids is an urgent problem in primary care institutions of Guizhou Province. The use of systemic glucocorticoids without appropriate indications was extremely prominent, especially in diseases of the respiratory system. It is important to note that physicians younger than 33, with more than 40 years of service, and attending or residents were more likely to inappropriately prescribe glucocorticoids.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
YC provided conceptualization and design for this study. LW provided support and assistance for data acquisition. Clinical pharmaceutical technical support was provided by SY and ZZ. YC, XL, and JH analyzed the data. YC and XL completed the manuscript. XZ and YL provided supervision and assistance for the whole research process. All authors played an important role and approved the submitted version.
Funding
This study was supported by the Natural Science Foundation of Guizhou Province, Feedback intervention model of Gradient Boosting Decision Tree (GBDT) technology on glucocorticoid prescription control in primary care institutions Guizhou Science And Technology Foundation -ZK [2021] General 499. And this study was also funded by the Medical Economics and Management Research Center of Guizhou Medical University (GMUMEM2022-A05).
Acknowledgments
We thank all the participating institutions for providing information and assistance during the study. The authors also thank all members of the investigational team who collected the data. We acknowledge the assistance of Edward McNeil, Prince of Songkla University, Songkhla, Thailand for reading the proposal and making suggestions to improve it.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Adcock IM, Mumby S. Glucocorticoids. Handb Exp Pharmacol. (2017) 237:171–96. doi: 10.1007/164_2016_98
2. TG B. History of the development of corticosteroid therapy. Clin Exp Rheumatol. (2011) 29(Suppl. 68):S−5–12
3. Fardet L, Nazareth I, Petersen I. Long-term systemic glucocorticoid therapy and weight gain: a population-based cohort study. Rheumatology. (2021) 60:1502–11. doi: 10.1093/rheumatology/keaa289rheumatology/keaa289
4. Hu K, Adachi JD. Glucocorticoid induced osteoporosis. Expert Rev Endocrinol Metab. (2019) 14:259–66. doi: 10.1080/17446651.2019.1617131
5. Compston J. Glucocorticoid-induced osteoporosis: an update. Endocrine. (2018) 61:7–16. doi: 10.1007/s12020–018–1588–2
6. Liu XX, Zhu XM, Miao Q, Ye HY, Zhang ZY, Li YM. Hyperglycemia induced by glucocorticoids in nondiabetic patients: a meta-analysis. Ann Nutr Metab. (2014) 65:324–32. doi: 10.1159/000365892
7. Mebrahtu TF, Morgan AW, West RM, Stewart PM, Pujades-Rodriguez M. Oral glucocorticoids and incidence of hypertension in people with chronic inflammatory diseases: a population-based cohort study. CMAJ. (2020) 192:E295–301. doi: 10.1503/cmaj.191012
8. Caplan A, Fett N, Rosenbach M, Werth VP, Micheletti RG. Prevention and management of glucocorticoid-induced side effects: a comprehensive review: a review of glucocorticoid pharmacology and bone health. J Am Acad Dermatol. (2017) 76:1–9. doi: 10.1016/j.jaad.2016.01.062
9. Rostaing L, Malvezzi P. Steroid-based therapy and risk of infectious complications. PLoS MED. (2016) 13:e1002025. doi: 10.1371/journal.pmed.1002025
10. Oray M, Abu Samra K, Ebrahimiadib N, Meese H, Foster CS. Long-term side effects of glucocorticoids. Expert Opin Drug Saf. (2016) 15:457–65. doi: 10.1517/14740338.2016.1140743
11. Joseph RM, Hunter AL, Ray DW, Dixon WG. Systemic glucocorticoid therapy and adrenal insufficiency in adults: a systematic review. Semin Arthritis Rheum. (2016) 46:133–41. doi: 10.1016/j.semarthrit.2016.03.001
12. Doumeizel PM, Robin F, Ballerie A, Moreau B, Le Bot A, Polard É, et al. Side effects of longterm oral corticosteroid therapy. Rev Prat. (2021) 71:587–96.
13. Longui CA. Glucocorticoid therapy: minimizing side effects. J Pediatr. (2007) 83(Suppl. 5):S163–77. doi: 10.1590/S0021-75572007000700007
14. Fardet L, Petersen I, Nazareth I. Prevalence of long-term oral glucocorticoid prescriptions in the UK over the past 20 years. Rheumatology. (2011) 50:1982–90. doi: 10.1093/rheumatology/ker017
15. Masih S, Cynthia Stephen S, Joy Armstrong L, Finny P. Use and misuse of glucocorticoids in the community of Raxaul Block, North Bihar. Trop Doct. (2015) 45:68–72. doi: 10.1177/0049475514567756
16. Benard-Laribiere A, Pariente A, Pambrun E, Begaud B, Fardet L, Noize P. Prevalence and prescription patterns of oral glucocorticoids in adults: a retrospective cross-sectional and cohort analysis in France. BMJ Open. (2017) 7:e015905. doi: 10.1136/bmjopen-2017-015905
17. Dvorin EL, Lamb MC, Monlezun DJ, Boese AC, Bazzano LA. Price–Haywood EG. High frequency of systemic corticosteroid use for acute respiratory tract illnesses in ambulatory settings. JAMA Intern Med. (2018) 178:852–4. doi: 10.1001/jamainternmed.2018.0103
18. Tang Y, Shang N, Zang Y–x, Wang D–z. Evaluation of off-label use of oral glucocorticoids in outpatients. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. (2015) 37:430–4. doi: 10.3881/j.issn.1000–503X.2015.04.011
19. Chen G, Hu W, Xuan N, Fan H, Zhu J, Cui W, et al. Survey on the use of glucocorticoids in severe community-acquired pneumonia in intensive care unit of forty-five hospitals in Zhejiang Province. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. (2019) 31:488–92. doi: 10.3760/cma.j.issn.2095–4352.2019.04.023
20. Zhang JY XS, Xu C. Investigation on the status of systemic glucocorticoid use in 271 medical institutions in Guizhou Province. Chinese J Hosp Pharm. (2020) 40:219–24. doi: 10.13286/j.1001-5213.2020.02.18
21. Jiang Q, Yu BN, Ying G, Liao J, Gan H, Blanchard J, et al. Outpatient prescription practices in rural township health centers in Sichuan Province, China. BMC Health Serv Res. (2012) 12:324. doi: 10.1186/1472-6963-12-324
22. Mayang Ll-mYXH. Review on essential medicine prescriptions in 27 township hospitals in Jiangxi Province. Herald Med. (2014) 33:811–4. doi: 10.3870/yydb.2014.06.035
23. China Health Commission. Guidelines for Clinical Application of Glucocorticoids (2011). Available online at: http://www.nhc.gov.cn/yzygj/s3585u/201102/91566d6e98df4916b8aa018e37605603.shtml
24. Overman RA, Yeh JY, Deal CL. Prevalence of oral glucocorticoid usage in the United States: a general population perspective. Arthritis Care Res. (2013) 65:294–8. doi: 10.1002/acr.21796
25. Waljee AK, Rogers MA, Lin P, Singal AG, Stein JD, Marks RM, et al. Short term use of oral corticosteroids and related harms among adults in the United States: population based cohort study. BMJ. (2017) 357:j1415. doi: 10.1136/bmj.j1415
26. Einarsdottir MJ, Ekman P, Trimpou P, Olsson DS, Johannsson G, Ragnarsson O. High prescription rate of oral glucocorticoids in children and adults: a retrospective cohort study from Western Sweden. Clin Endocrinol. (2020) 92:21–8. doi: 10.1088/1475-7516/2019/04/023
27. Wondmkun YT, Ayele AG. Assessment of prescription pattern of systemic steroidal drugs in the outpatient department of menelik ii referral hospital, addis ababa, Ethiopia, 2019. Patient Prefer Adherence. (2021) 15:9–14. doi: 10.2147/PPA.S285064
28. Lin KJ, Dvorin E, Kesselheim AS. Prescribing systemic steroids for acute respiratory tract infections in United States outpatient settings: a nationwide population-based cohort study. PLoS Med. (2020) 17:e1003058. doi: 10.1371/journal.pmed.1003058
29. Nalli C, Armstrong L, Finny P, Thomas N. Glucocorticoid misuse in a rural and semi-urban community of North Bihar: a pilot study. Trop Doct. (2012) 42:168–70. doi: 10.1258/td.2012.120139
30. Dvorin EL, Ebell MH. Short-term systemic corticosteroids: appropriate use in primary care. Am Fam Physician. (2020) 101:89–94.
31. Sharma R, Abrol S, Wani M. Misuse of topical corticosteroids on facial skin. A study of 200 patients. J Dermatol Case Rep. (2017) 11:5–8. doi: 10.3315/jdcr.2017.1240
32. Manchanda K, Mohanty S, Rohatgi PC. Misuse of topical corticosteroids over face: a clinical study. Indian Dermatol Online J. (2017) 8:186–91. doi: 10.4103/idoj.IDOJ_535_15
33. Chaudhary RG, Rathod SP, Jagati A, Baxi K, Ambasana A, Patel D. Prescription and usage pattern of topical corticosteroids among out-patient attendees with dermatophyte infections and its analysis: a cross-sectional, survey-based study. Indian Dermatol Online J. (2019) 10:279–83. doi: 10.4103/idoj.IDOJ_335_18
34. Shrestha S, Joshi S, Bhandari S. Prevalence of misuse of topical corticosteroid among dermatology outpatients. JNMA J Nepal Med Assoc. (2020) 58:834–8. doi: 10.31729/jnma.5271
35. El-Khoury M, Thay R. N'Diaye M, Fardet L. Use of topical glucocorticoids: a population-based cohort study. J Eur Acad Dermatol Venereol. (2017) 31:1044–7. doi: 10.1111/jdv.14149
36. Jaccob AA, Yaqoub AA, Rahmani MA. Impact of abuse of topical corticosteroids and counterfeit cosmetic products for the face: prospective demographic study in basrah city, Iraq. Curr Drug Saf. (2020) 15:25–31. doi: 10.2174/1574886314666191001100357
37. Thomas M, Wong CC, Anderson P, Grills N. Magnitude, characteristics and consequences of topical steroid misuse in rural North India: an observational study among dermatology outpatients. BMJ Open. (2020) 10:e032829. doi: 10.1136/bmjopen-2019-032829
38. Jha AK, Sinha R, Prasad S. Misuse of topical corticosteroids on the face: a cross-sectional study among dermatology outpatients. Indian Dermatol Online J. (2016) 7:259–63. doi: 10.4103/2229-5178.185492
39. Mahar S, Mahajan K, Agarwal S, Kar HK, Bhattacharya SK. Topical corticosteroid misuse: the scenario in patients attending a tertiary care hospital in New Delhi. J Clin Diagn Res. (2016) 10:FC16–20. doi: 10.7860/JCDR/2016/23419.8986
40. World Health Organization International International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10)-2014-WHO Version for 2014. Geneva, Switzerland: WHO (2014). Available online at: http://apps.who.int/classifications/icd10/browse/2014/en#/X (accessed April 13, 2015).
42. Liu D, Ahmet A, Ward L, Krishnamoorthy P, Mandelcorn ED, Leigh R, et al. A practical guide to the monitoring and management of the complications of systemic corticosteroid therapy. Allergy Asthma Clin Immunol. (2013) 9:30. doi: 10.1186/1710-1492-9-30
43. Yasir M, Goyal A, Bansal P, Sonthalia S. Corticosteroid Adverse Effects. StatPearls Treasure Island (FL): StatPearls Publishing Copyright ©. (2021).
44. Yuanqing B, Yanmei L. Analysis of 1480 outpatient prescriptions for glucocorticoids. China Herb Depot. (2013) 22:69–70.
45. Quevedo J, Marsh W, Yulfo J, Alvarez O, Felici M, Rojas ME. Prescribing patterns and safety of mezclitas for respiratory illnesses. P R Health Sci J. (2012) 31:138–44. doi: 10.1176/appi.ps.201100349
46. Kim T, Do YK. Prescription of systemic steroids for acute respiratory infections in korean outpatient settings: Overall patterns and effects of the prescription appropriateness evaluation policy. J Prev Med Public Health. (2020) 53:82–8. doi: 10.3961/jpmph.19.090
47. Francis NA, Cannings-John R, Waldron CA, Thomas-Jones E, Winfield T, Shepherd V, et al. Oral steroids for resolution of otitis media with effusion in children (OSTRICH): a double-blinded, placebo-controlled randomised trial. Lancet. (2018) 392:557–68. doi: 10.1016/S0140-6736(18)31490-9
48. Venekamp RP, Thompson MJ, Hayward G, Heneghan CJ, Del Mar CB, Perera R, et al. Systemic corticosteroids for acute sinusitis. Cochrane Database Syst Rev. (2014) 3:Cd008115. doi: 10.1002/14651858.CD008115.pub3
49. Hay AD, Little P, Harnden A, Thompson M, Wang K, Kendrick D, et al. Effect of oral prednisolone on symptom duration and severity in nonasthmatic adults with acute lower respiratory tract infection: a randomized clinical trial. JAMA. (2017) 318:721–30. doi: 10.1001/jama.2017.10572
50. Sadeghirad B, Siemieniuk RAC, Brignardello-Petersen R, Papola D, Lytvyn L, Vandvik PO, et al. Corticosteroids for treatment of sore throat: systematic review and meta-analysis of randomised trials. BMJ. (2017) 358:j3887. doi: 10.1136/bmj.j3887
51. Adult Treatment Recommendations. CDC. Adult Treatment Recommendations (2017). Available online at: https://wwwcdcgov/antibiotic-use/community/for-hcp/outpatient-hcp/adult-treatment-rechtml
52. Yankao W. Analysis of inappropriate use of drugs for digestive system diseases. Guide China Med. (2015) 13:62.
53. Page RC. Gingivitis. J Clin Periodontol. (1986) 13:345–59. doi: 10.1111/j.1600-051X.1986.tb01471.x
54. Slots J. Periodontitis: facts, fallacies and the future. Periodontol 2000. (2017) 75:7–23. doi: 10.1111/prd.12221
56. Sanz M, Herrera D, Kebschull M, Chapple I, Jepsen S, Beglundh T, et al. Treatment of stage I-III periodontitis-The EFP S3 level clinical practice guideline. J Clin Periodontol. (2020) 47(Suppl. 22):4–60. doi: 10.1111/jcpe.13290
57. Trombelli L, Farina R, Silva CO, Tatakis DN. Plaque-induced gingivitis: case definition and diagnostic considerations. J Periodontol. (2018) 89 Suppl 1:S46–73. doi: 10.1002/JPER.17-0576
58. Brasil-Oliveira R, Cruz Á A, Sarmento VA, Souza-Machado A, Lins-Kusterer L. Corticosteroid use and periodontal disease: a systematic review. Eur J Dent. (2020) 14:496–501. doi: 10.1055/s-0040-1713954
59. Gallagher P, Ryan C, Byrne S, Kennedy J, O'Mahony D. STOPP(Screening Tool of Older Person's Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther. (2008) 46:72–83. doi: 10.5414/CPP46072
60. Expert Expert Panel Working Group of the National Heart L Blood Institute a coordinated National Asthma E Prevention Program Coordinating C Cloutier MM Baptist AP . 2020 focused updates to the asthma management guidelines: a report from the national asthma education and prevention program coordinating committee expert panel working group. J Allergy Clin Immunol. (2020) 146:1217–70. doi: 10.1016/j.jaci.2020.10.003
61. Bleecker ER, Menzies-Gow AN, Price DB, Bourdin A, Sweet S, Martin AL, et al. Tran TN: systematic literature review of systemic corticosteroid use for asthma management. Am J Respir Crit Care Med. (2020) 201:276–93. doi: 10.1164/rccm.201904-0903SO
62. Mirza S, Clay RD, Koslow MA, Scanlon PD. COPD Guidelines: a review of the 2018 GOLD report. Mayo Clin Proc. (2018) 93:1488–502. doi: 10.1016/j.mayocp.2018.05.026
63. Gossec L, Baraliakos X, Kerschbaumer A, de Wit M, McInnes I, Dougados M, et al. EULAR recommendations for the management of psoriatic arthritis with pharmacological therapies: 2019 update. Ann Rheum Dis. (2020) 79:700–12. doi: 10.1136/annrheumdis-2020-217159
64. Moore MN, Wallace BI. Glucocorticoid and opioid use in rheumatoid arthritis management. Curr Opin Rheumatol. (2021) 33:277–83. doi: 10.1097/BOR.0000000000000788
65. Man C, Wenyuan W. Analysis of irrational use of glucocorticoids in outpatients of three hospitals in Zhuhai in 2013. Eval Anal Hosp Drug Use China. (2016) 16:104–6. doi: 10.14009/j.issn.1672-2124.2016.01.0037
66. Ruiz-Irastorza G, Danza A, Khamashta M. Glucocorticoid use and abuse in SLE. Rheumatology. (2012) 51:1145–53. doi: 10.1093/rheumatology/ker410
67. Jia L, Li J, Rubing L. Analysis of the use of glucocorticoids in inpatients in our hospital in 2017. China Medical Herald. (2018) 15:162–164+173.
68. Parsel SM, Mohammed AE, Fort D, Barton BM, McCoul ED. Intramuscular corticosteroids for acute upper respiratory infections affects healthcare utilization. Ann Otol Rhinol Laryngol. (2020) 129:988–95. doi: 10.1177/0003489420929717
69. Zhang W, Ung COL, Lin G, Liu J, Li W, Hu H, et al. Factors contributing to patients' preferences for primary health care institutions in China: A qualitative study. Front Public Health. (2020) 8:414. doi: 10.3389/fpubh.2020.00414
70. Dong L, Wang D, Gao J, Yan H. Doctor's injection prescribing and its correlates in village health clinics across 10 Provinces of Western China. J Public Health. (2011) 33:565–70. doi: 10.1093/pubmed/fdr019
71. Arora NK. Injection practices in India. WHO South East Asia J Public Health. (2012) 1:189–200. doi: 10.4103/2224-3151.206931
72. Xu H, Zhang W, Gu L, Qu Z, Sa Z, Zhang X, et al. Aging village doctors in five counties in rural China: situation and implications. Hum Resour Health. (2014) 12:36. doi: 10.1186/1478-4491-12-36
73. China Health Statistics Yearbook (2020). Available online at: http://www.nhc.gov.cn//mohwsb/mohwsbwstjxxzx/tjtjnj/202112/dcd39654d66c4e6abf4d7b1389becd01.shtml
74. Li X, Liu J, Huang J, Qian Y, Che L. An analysis of the current educational status and future training needs of China's rural doctors in 2011. Postgrad Med J. (2013) 89:202–8. doi: 10.1136/postgradmedj-2012-131094
75. Xin Y, Ren X. The impact of family income on body mass index and self-rated health of illiterate and non-illiterate rural elderly in china: evidence from a fixed effect approach. Front Public Health. (2021) 9:722629. doi: 10.3389/fpubh.2021.722629
76. Xie Y, Ma M, Zhang Y, Tan X. Factors associated with health literacy in rural areas of Central China: structural equation model. BMC Health Serv Res. (2019) 19:300. doi: 10.1186/s12913-019-4094-1
77. Yang Q, Yu S, Wang C, Gu G, Yang Z, Liu H, et al. Health literacy and its socio-demographic risk factors in Hebei: a cross-sectional survey. Medicine. (2021) 100:e25975. doi: 10.1097/MD.0000000000025975
78. Yuan F, Qian D, Huang C, Tian M, Xiang Y, He Z, et al. Analysis of awareness of health knowledge among rural residents in Western China. BMC Public Health. (2015) 15:55. doi: 10.1186/s12889-015-1393-2
79. Gyawali S, Rathore DS, Shankar PR, Maskey M, Vikash KK. Injection practices in Nepal: health policymakers' perceptions. BMC Int Health Hum Rights. (2014) 14:21. doi: 10.1186/1472-698X-14-21
80. Ma J, Xu J, Zhang Z, Wang J. New cooperative medical scheme decreased financial burden but expanded the gap of income-related inequity: evidence from three provinces in rural China. Int J Equity Health. (2016) 15:72. doi: 10.1186/s12939-016-0361-5
Keywords: systemic glucocorticoids, prescription patterns, appropriateness, inappropriate use, primary care institutions
Citation: Luo X, Yu S, Zeng Z, Zhou X, Liu Y, Wang L, Hu J and Chang Y (2022) Systemic glucocorticoid prescriptions pattern and factors of inappropriate use in primary care institutions of Southwest China. Front. Public Health 10:952098. doi: 10.3389/fpubh.2022.952098
Received: 24 May 2022; Accepted: 24 August 2022;
Published: 12 September 2022.
Edited by:
Ana Clavería, Instituto de Investigación Sanitaria Galicia Sur (IISGS), SpainReviewed by:
Isabel Rey Gomez-Serranillos, Servicio Gallego de Salud, SpainLlxs Jiang, Kunming Children's Hospital, China
Klejda Harasani, University of Medicine, Tirana, Albania
Copyright © 2022 Luo, Yu, Zeng, Zhou, Liu, Wang, Hu and Chang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yue Chang, NDU2NzQwMSYjeDAwMDQwO3FxLmNvbQ==; Xunrong Zhou, MjM5ODY2Mjc3OSYjeDAwMDQwO3FxLmNvbQ==; Yuxi Liu, eXV4aWxpdTEyMyYjeDAwMDQwOzEyNi5jb20=
†These authors have contributed equally to this work
 Xiaobo Luo
Xiaobo Luo Shitao Yu2†
Shitao Yu2† Yue Chang
Yue Chang