
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 26 September 2022
Sec. Family Medicine and Primary Care
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.948533
This article is part of the Research Topic New Trends in Type 2 Diabetes Diagnosis and Management in Primary Care View all 14 articles
 Jin-Hua Jie1
Jin-Hua Jie1 Dan Li1
Dan Li1 Li-Na Jia1
Li-Na Jia1 Yifeng Chen2
Yifeng Chen2 Yan Yang2
Yan Yang2 Bailing Zheng2
Bailing Zheng2 Chuancheng Wu2
Chuancheng Wu2 Baoying Liu2
Baoying Liu2 Rongxian Xu3
Rongxian Xu3 Jianjun Xiang2*
Jianjun Xiang2* Hai-Lin Zhuang1*
Hai-Lin Zhuang1*Background: Type 2 diabetes mellitus (T2DM) is an independent risk factor for functional limitations among the older population. The predicted increase in T2DM cases combined with the ongoing rapidly aging population may further burden the already overloaded healthcare system and aggravate the loss of economic self-sufficiency. This study aimed to investigate the activities of daily living (ADL) and its influencing factors on older people with T2DM, and to provide implications for the development and improvement of community nursing services in the context rapidly aging population in China.
Methods: From March 2019 to June 2020, we conducted a cross-sectional questionnaire survey among older T2DM patients in Fuzhou, using a multi-stage cluster sampling approach. Functional status was measured by the Lawton ADL scale. Stata “nptrend” test was used to examine the trend of ordinal variables on ADL. Non-conditional logistic regression was used to identify factors affecting ADL limitations.
Results: A total of 2016 questionnaires were received, with a response rate of 96%. 12.4% of participants suffered from varying degrees of functional impairment. ADL limitations increased with age. More comorbidities were associated with a greater risk of developing functional limitations in ADLs. the following sub-groups were more likely to suffer from ADL impairment: those aged 70 and over years (OR = 1.99, 95%CI 1.77–2.56), living in an aged care house or with spouse/children (OR = 2.31, 95%CI 1.25–4.26), low monthly income (OR = 1.49, 95%CI 1.28–1.64), without health insurance (OR = 1.82, 95%CI 1.40–2.40), tight family expenses (OR = 1.95, 95%CI 1.42–2.69), having stroke (OR = 6.70, 95%CI 2.22–20.23) or malignant tumor (OR = 4.45, 95%CI 1.27–15.53), irregular eating habit (OR = 2.55, 95%CI 2.23–2.92), smoking (OR = 1.40, 95%CI 1.22–1.60), sedentary lifestyle (OR = 2.04, 95%CI 1.46–2.85), lack of physical exercise (OR = 1.35, 95%CI 1.19–1.53), sleeping difficulty (OR = 1.25, 95%CI 1.10–1.42), and lack of family support (OR = 1.19, 95%CI 1.10–1.29).
Conclusion: Older adults (≥70 years) with T2DM had a high prevalence of functional limitations across a range of daily living tasks, which not only affect individual life of quality but also present a huge burden on the family, health services system, and the whole society. Identified factors associated with ADL limitations may provide useful information for targeted nursing practice and health promotion.
Type 2 diabetes mellitus (T2DM) is a serious public health concern. According to the latest 10th Edition IDF (International Diabetes Federation) Report (1), about 537 million people were living with diabetes (over 90% being T2DM) worldwide in 2021 and ~6.7 million people have died from it or its complications at the same year. Driven by a complex interplay of multifarious factors such as the rapidly aging population, increased sedentary lifestyle, and abrupt changes in traditional dietary habits (2), T2DM has become one of the fastest-growing global health emergencies in this century, with the projected prevalence rate reaching 7,079 individuals per 100,000 by 2030 (3). China has the largest numbers of both current (accounting for about one-quarter of global cases) and projected T2DM cases partly due to its large population size (1). From 1990 to 2016, the all-age morbidity and mortality rates in China have dramatically increased by 78.4 and 63.5% (4), respectively, presenting huge healthcare and economic burden on the society.
T2DM is a prevalent chronic health condition more frequently affecting people aged 65 and over. Results of the 2017 national epidemiological survey showed that the prevalence of diabetes was 30.2% in people aged ≥60 years and the pre-diabetes prevalence rate reached 47.7%, although the proportion of undiagnosed cases was estimated to be 51.7% (1). Older T2DM patients were found to have an accelerated decline in leg lean mass, muscle strength and functional capacity when compared with normoglycemic control groups (5). Evidence has shown that T2DM is an independent risk factor for functional limitations among the older population (6), impairing about 60% of activities of daily living (ADL) for diabetic people aged>65 years compared with only 34% for the same age group without T2DM in the USA (7), especially among older Mexican Americans with T2DM (8). Moreover, T2DM patients were two to three times more likely to suffer from disability than their counterparts (9), and utilized healthcare services more frequently as well. Therefore, the predicted increase in T2DM cases combined with the ongoing rapidly aging population may further burden the already overloaded healthcare system and aggravate the loss of economic self-sufficiency.
Effective diabetes self-management is critical for maintaining health and preventing the occurrence of further diabetes-related complications such as diabetic ketoacidosis, hypoglycemia, cardiovascular diseases, retinopathy, nephropathy, vascular nephropathy, and foot complications (6). However, self-management can be especially challenging for elderly people with T2DM, as they are more likely to suffer from functional limitations and develop geriatric syndromes than those without diabetes (8, 9). Results of a survey including 1,691 individuals sampled from 5 provinces of China showed that T2DM patients especially those living in a low socioeconomic status were moderately satisfied with urban community health services (10), indicating room to improve diabetes caring services at a community level in the aspects of healthcare services quality, health promotion, health insurance, and the essential drug system (10, 11). Currently, few studies in China have investigated the extent to which older adults suffer from functional limitations due to T2DM and its related complications. This study aims to investigate older T2DM patients' activities of daily living (ADL) and identify its influencing factors. Findings of this study can provide useful evidence for the provision of targeted community healthcare services for older people with T2DM to improve their quality of life.
Located on the southeast coast of China, Fuzhou is the capital city of Fujian Province, with a population of around 8 million in 2020. In line with the national trend, Fuzhou has stepped into an aging society since 2000 (12). The aging of Fuzhou's population is still ongoing at a rapid pace, and the proportion of people aged >60 years increased from 12.1% in 2011 to 19.1% in 2020 (13). In terms of T2DM, the age-standardized prevalence rate (12.3%) of T2DM in Fuzhou was slightly higher than the national average level (11.2%) in 2017 and similarly for the age-standardized mortality rate (14.7 per 100,000 vs. 12.7 per 100,000) (14–16). Since 2009, Chinese government launched the National Basic Public Health Service Program (NBPHSP) to provide 14 categories of health services to all urban and rural residents free of charge. NBPHSP covers the management of T2DM patients, including screening, regular follow-up, and health education (17). Local community health service centers and village clinics are responsible for the provision of NBPHSP services.
From March 2019 to June 2020, we conducted a cross-sectional questionnaire survey among T2DM patients in Fuzhou to investigate their ADLs. T2DM patients were approached under the support of local community health service centers when they carried out the NBPHSP services for T2DM patients. In this study, T2DM patients were recruited through a multi-stage random cluster sampling process. Firstly, two of the five urban districts in Fuzhou were randomly selected through drawing lots (Names of the five districts were put into a bowl and two names were randomly chosen). The two sampled districts (Taijiang District and Gulou District) have 22 community health service centers; Secondly, we assigned a unique number from 1 to 22 to each of the 22 community health service centers. Then, 11 of the 22 community health service centers were randomly selected as our study sites through an online random number generator (https://epitools.ausvet.com.au/randomnumbers). The inclusion criteria were T2DM patients aged ≥60 years. Those could not answer the survey questions because of health issues (e.g., dementia or/and mental disorders) were excluded. Participation was completely voluntary and no incentives were offered. Informed consent was obtained from individual participants. The study has been approved by the Medical Ethics Committee of Fujian Health College.
The questionnaire consists of two parts. The first section requested the following demographic information: age, gender, education level, marital status, household income, comorbidities, family support, and individual living habits (e.g., smoking, drinking, sleeping, physical exercise, eating pattern). The second section is the widely used Lawton ADL scale (validated Chinese version) to measure two important domains of functioning of older people with T2DM: physical self-maintenance scale (PSMS) and instrumental activities of daily living (IADL) (18). PSMS contains ratings of self-care ability necessary for living in the community in areas of toileting, feeding, dressing, bathing, and locomotion. In contrast, IADL contains a more complex set of behaviors required for independent living skills, including the following eight areas: telephoning, shopping, food preparation, housekeeping, laundering, use of transportation, use of medicine, and financial behavior. Each item of PSMS and IADL was measured using a 4-point Likert scale question: “do it completely by yourself,” “a little difficult to do it independently,” “do it with assistance,” and “must be done by others.” They were assigned 1–4 scores, respectively. Therefore, PSMS has a summary score from 4 to 24 and IADL has a summary score from 8 to 32. The higher the score means the greater the person's functional limitation. ADL consists of PSMS and IADL, with a summary score from 14 to 56. The severity of ADL was classified into three levels: normal (14 scores), somewhat impaired (15–21 scores), and severely impaired (≥22 scores). PSMS and IADL were defined as “impaired” if the summary scores exceeded 6 and 8, respectively.
After a pilot survey, the questionnaire was revised to ensure all questions were clear and understandable. The questionnaire has also been reviewed by relevant experts. All investigators received unified training to ensure the survey was carried out consistently. Participants filled out the questionnaire by themselves under the support/assistance of an on-site investigator in the local community health service center. Completed questionnaires were checked and collected by the investigators on the spot.
Data entry was facilitated using EpiData 3.1 software (EpiData Association, Odense M, Denmark). The demographic characteristics of ADL were descriptively analyzed. The scores of functional impairments were summarized as mean ± standard deviation. Kruskal-Wallis H test and Mann-Whitney U test were conducted as the first step to identifying factors associated with ADL. Stata “nptrend” test was used to examine the trend of ordinal variables on ADL (19). Then, we put statistically significant factors into a non-conditional logistic regression model to identify the factors influencing ADL (inclusion criterion α = 0.05, elimination criterion α = 0.10). Stata 16.0 was used to perform all statistical analyses. Results were considered statistically significant at a P < 0.05.
A total of 2,016 questionnaires were received, with a response rate of 96%, including 995 participants recruited from Taijiang District and 1,021 participants from the Gulou District. As shown in Table 1, the average ADL self-care ability score was 14.91 ± 3.38 points. 12.4% of participants suffered from varying degrees of functional impairment, of which 8.2% were mild and 4.2% were severe. The average points for PSMS and IADL were 6.20 ± 1.10 and 8.71 ± 2.49, respectively. Accordingly, the percentages of participants with impaired function for PSMS and IADL were 5.2 and 12.0%, respectively.
Differences in the functional capability of participants with T2DM by demographic characteristics are summarized in Table 2. We found ADL functions were significantly affected by the following demographic factors: age (H = 52.13, P < 0.01), gender (Z = −2.53, P = 0.01), marital status (Z = −4.19, P < 0.01), monthly income (H = 68.31, P < 0.01), and health insurance status (H = 14.41, P < 0.01). Moreover, with the increase in age ADL functions demonstrated a decreasing trend (Z = 12.06, P < 0.001). Conversely, education level (Z = −2.4, P = 0.017) and financial status (Z = −3.99, P < 0.001) showed an increasing trend with ADL functions.
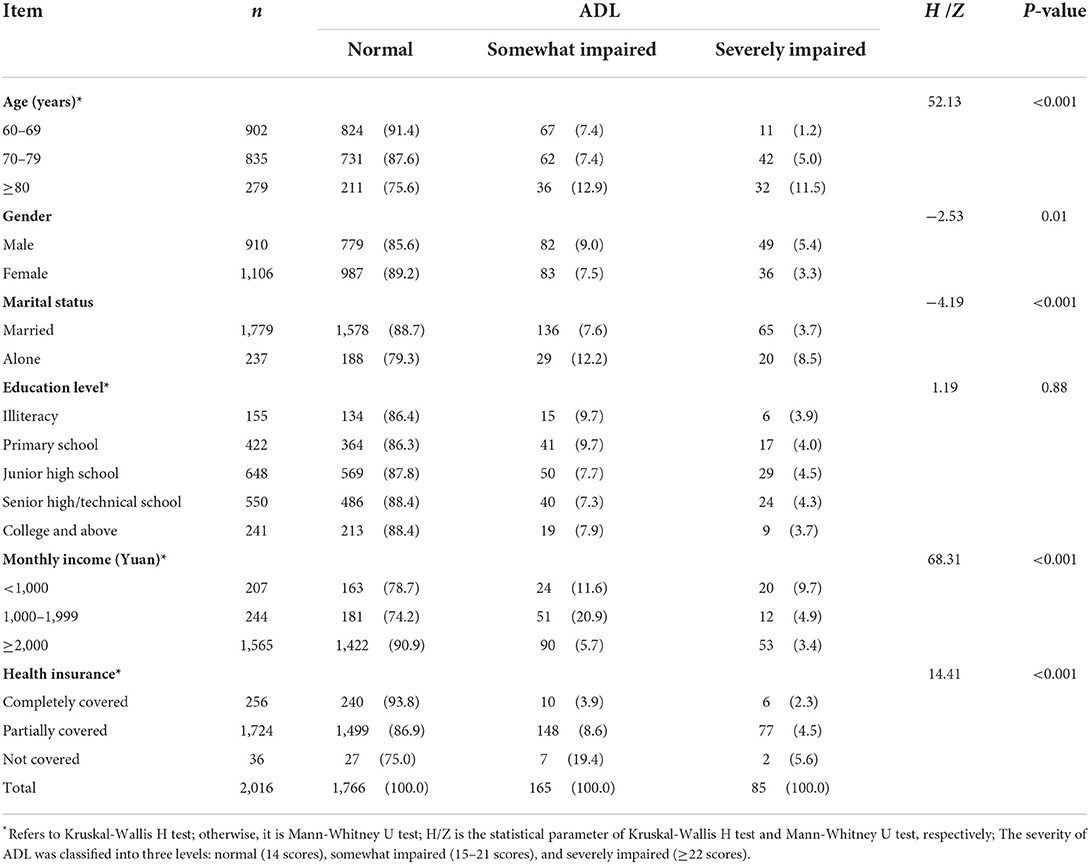
Table 2. Comparison of activities of daily living (ADL) by demographic characteristics in older people with type 2 diabetes.
Table 3 summarizes the differences in ADL functions by individual behaviors. We found the following factors significantly affected ADL functions of older people with T2DM: eating habits (H = 138.92, P < 0.001), smoking (H = 14.88, P < 0.001), drinking (Z = −3.28, P < 0.001), doing exercise (H = 32.82, P < 0.001), sedentary lifestyle (Z = –7.66, P < 0.001), and sleeping difficulty (H = 29.17, P < 0.001). Results of trend analysis show that those eating more regularly (Z = 17.77, P < 0.001) and doing more exercise (Z = –10.76, P < 0.001) had relatively fewer ADL function restrictions.
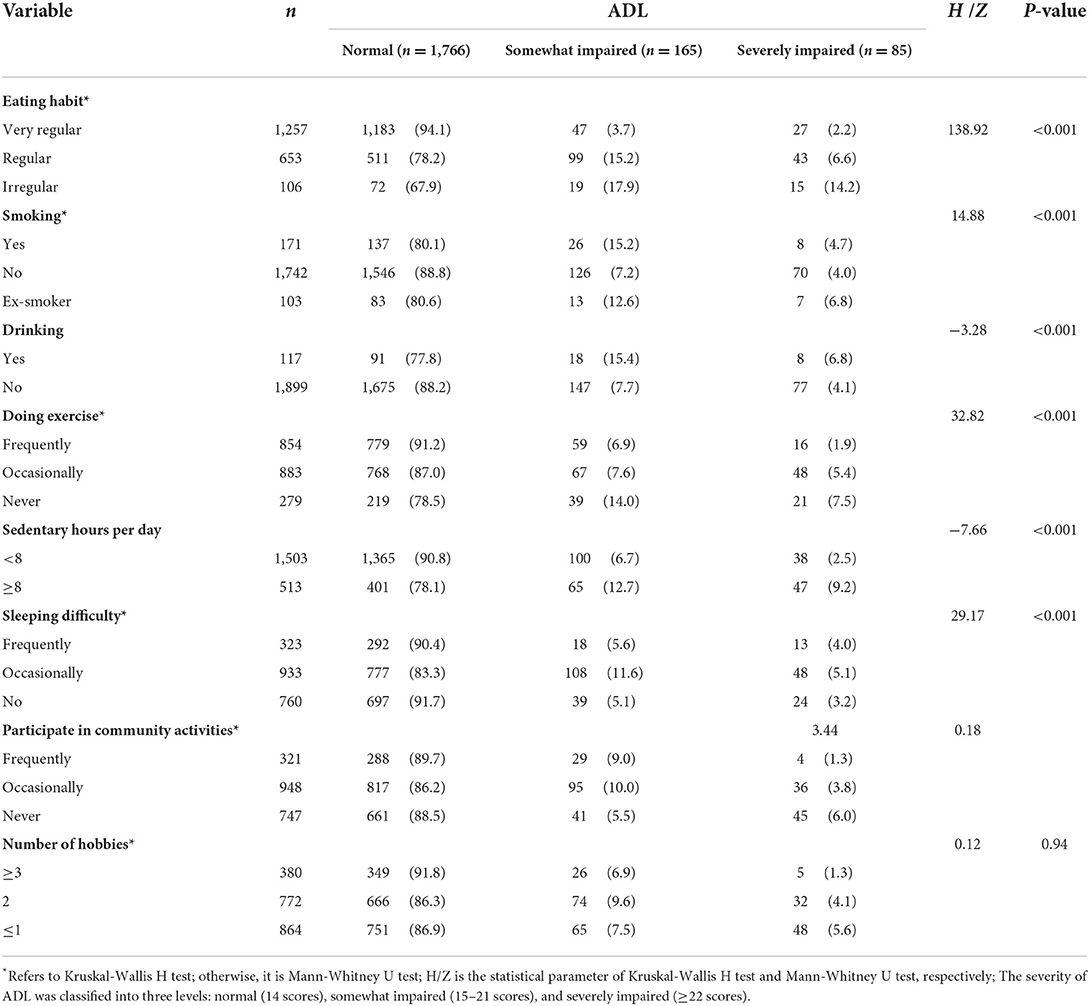
Table 3. Comparison of activities of daily living (ADL) functions by individual behaviors in older people with type 2 diabetes in Fuzhou.
Table 4 shows the differences in ADL functions of older people with T2DM by family characteristics. We found ADL functions were significantly affected by living conditions (H = 28.20, P < 0.001), family support (H = 19.33, P < 0.001), and family income (H = 31.51, P < 0.001). Moreover, results of trend analysis suggest that more family support (Z = –6.07, P < 0.001) and better economic status (Z = –3.99, P < 0.001) were associated with fewer ADL function restrictions.
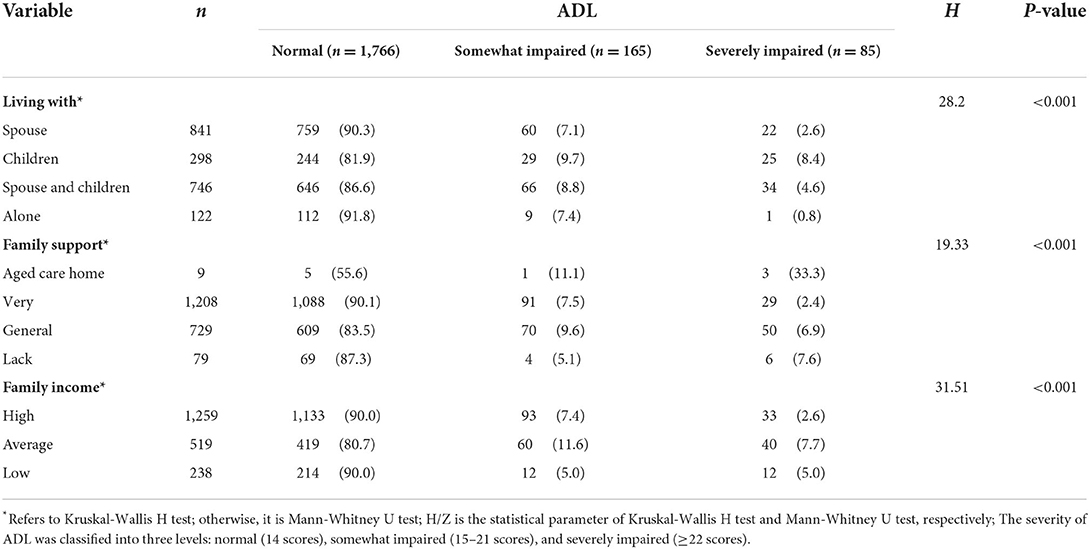
Table 4. Comparison of activities of daily living (ADL) functions by family characteristics in older people with type 2 diabetes in Fuzhou.
As shown in Table 5, among the 2016 participants with T2DM, 82.7% of them lived with other chronic diseases. Moreover, the results of trend analysis suggest that those with more existing chronic diseases had more ADL function restrictions (Z = 3.38, P = 0.001). In addition to T2DM, we found the following two chronic diseases may compromise older people's ADL functions: stroke (Z = –3.40, P < 0.001) and malignant tumors (Z = –2.63, P = 0.01).
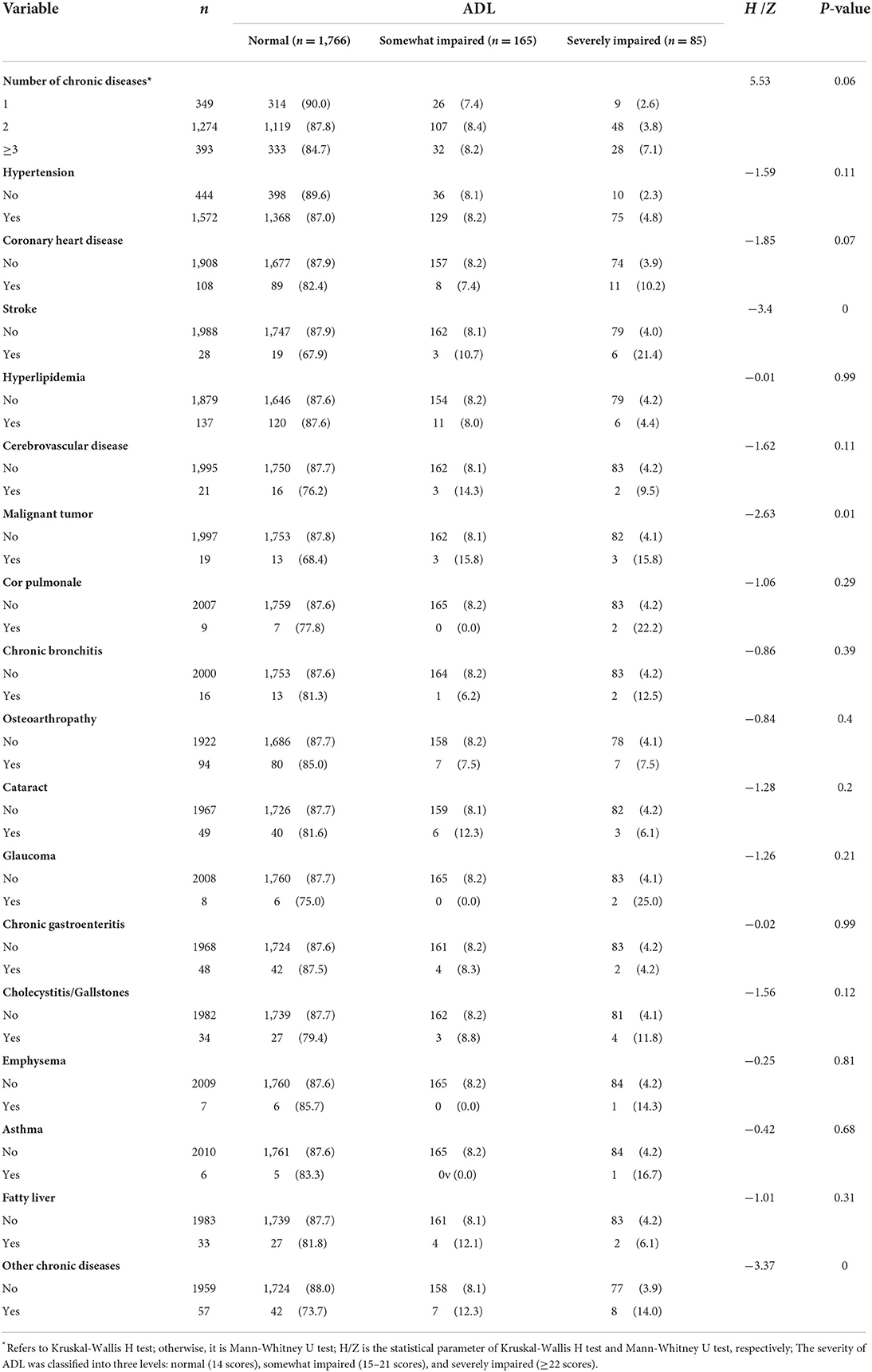
Table 5. Comparison of activities of daily living (ADL) functions by different chronic diseases in older people with type 2 diabetes in Fuzhou.
Table 6 summarizes the results of multivariate unconditional logistic regression analysis to identify factors affecting ADL functions. We found the following sub-groups were more likely to suffer from ADL impairment: those aged 70 and over years old (OR = 1.99, 95%CI 1.77–2.56), living in an aged care house or with spouse/children (OR = 2.31, 95%CI 1.25–4.26), low monthly income (OR = 1.49, 95%CI 1.28–1.64), without health insurance (OR = 1.82, 95%CI 1.40–2.40), tight family expenses (OR = 1.95, 95%CI 1.42–2.69), having stroke (OR = 6.70, 95%CI 2.22–20.23) or malignant tumor (OR = 4.45, 95%CI 1.27–15.53), irregular eating habit (OR = 2.55, 95%CI 2.23–2.92), smoking (OR = 1.40, 95%CI 1.22–1.60), sedentary lifestyle (OR = 2.04, 95%CI 1.46–2.85), lack of physical exercise (OR = 1.35, 95%CI 1.19–1.53), sleeping difficulty (OR = 1.25, 95%CI 1.10–1.42), and lack of family support (OR = 1.19, 95%CI 1.10–1.29).
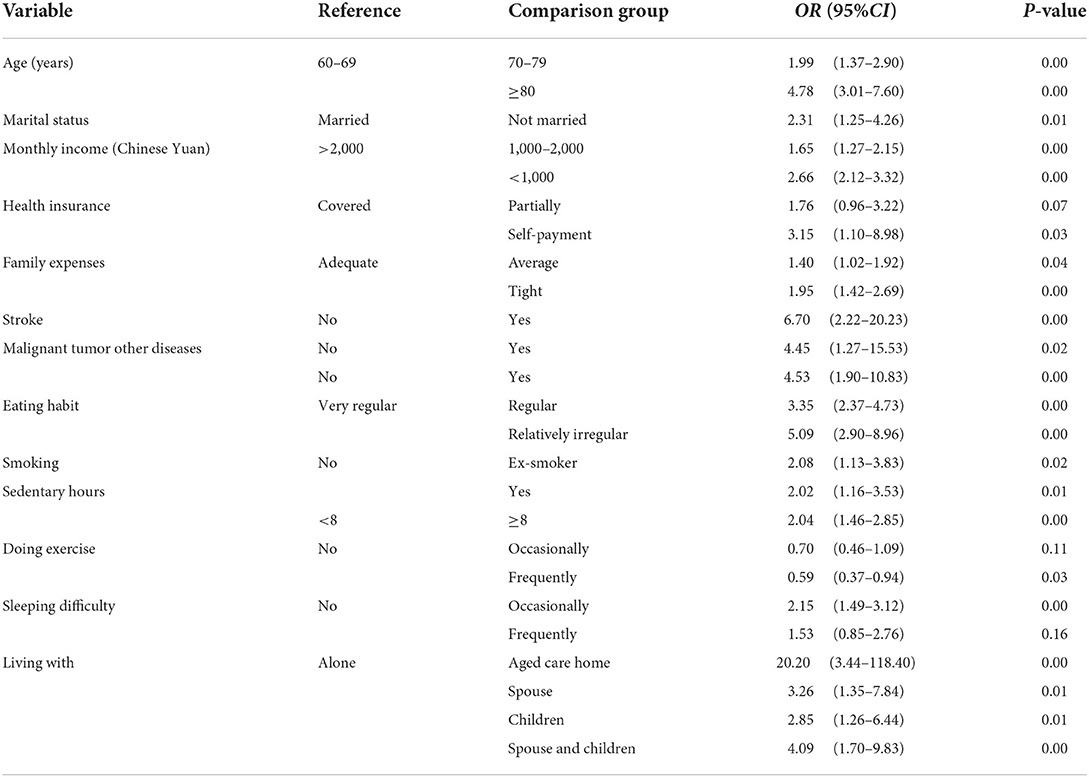
Table 6. Identification of factors affecting activities of daily living (ADL) limitation in older people with type 2 diabetes in Fuzhou.
Physical disability is a major socioeconomic and public health issue, as it not only diminishes the quality of life of those affected but also may result in a greater increase in healthcare services utilization such as physician visits and hospitalizations (4, 20). Diabetes is associated with functional disability through mechanisms such as decreased cardiopulmonary reverse, inflammatory or sarcopenic process, extreme of blood glucose, muscle catabolism, cognitive impairment, and inflexible treatment regimens (5, 21–23). Presence of diabetes and associated complications can lead to a significant decline in physical functioning, especially among older patients (8, 24). Currently, there are limited studies in China investigated to what extent older T2DM patients' activities of daily living were affected and its influencing factors. The limitations in ADL and IADL have been widely used as an indicator to assess disability in basic life activities among the population over 65 years old (25, 26). In this study, we found unhealthy lifestyle had significant impacts on older T2DM patients' functional limitations. Specifically, a high level of physical activity, being married, regular eating habits, and non-smoking are protective factors for performing ADLs. On the contrary, a sedentary lifestyle, suffering from stroke or malignant tumor, and sleeping difficulty may increase the risk of ADL limitations among older T2DM patients. We also found that household composition was associated with physical limitations in ADLs. Participants living alone performed ADLs much better than those lived in aged care homes or living with spouse or/and children, probably because those with severe ADL impairment were lack of self-care capability and had to live with others. These findings may provide useful information for the development of nursing practice and the improvement of effective health management for older T2DM patients.
Currently, most published epidemiological research findings support that diabetes was associated with ADL limitations (27). According to a cohort study from China, the risk of ADL impairment was increased by 102% (HR = 2.02, 95%CI 1.29–3.17) for T2DM patients aged 65–74 years, compared to those without T2DM in the same age group (28). Nevertheless, inconsistency still exits. Results of a multi-country study showed that diabetes was not associated with ADL limitations in China after controlling for confounding factors such as socioeconomic status, but significant associations were found in Mexico, Barbados, Brazil, Chile, Cuba, and Uruguay (29).
In this study, we found the prevalence of functional limitations (ADL) among the older T2DM patients in Fuzhou was 12.4%. It is much lower than the national average ADL impairment rate (32.3%) according to the survey data from China Health and Retirement Longitudinal Study (CHARLS) (30, 31). The differences in the prevalence of ADL disability among T2DM patients across studies have been reported by international literature as well (8, 29), which may be due to the varied criteria used to define functional limitations. Moreover, differences in socioeconomic and healthcare services levels (e.g., early diagnosis, medical treatment, and rehabilitation) across regions/cities may also contribute to the disparity. Another possible explanation is that the CHARLS survey data were collected between 2015 and 2016, and evidence has shown that the incidence of ADL disability among the Chinese older adult population with T2DM had a declining trend over time (26), mainly due to the considerable improvements in living standard, biological environment, and healthcare services.
We found ADL limitations increased with age, as older people were more likely to experience T2DM-related comorbidities (32). Moreover, our results showed that more comorbidities were associated with a greater risk of developing ADL limitations. It is in line with previous studies (8, 26). As to gender differences in ADL limitations among T2DM patients, there is no consistency. Most previous literature suggests that older female T2DM patients usually reported more ADL functional limitations and physical disability than their male counterparts (8, 26, 28), although women generally utilized healthcare services more often than men. The greater prevalence and severity of arthritis and musculoskeletal disease among older women may partly explain the difference (33). Another explanation is that women were more likely to report or over-report their ill health and disability than men (34). However, we found males reported more ADL limitations than their female counterparts, probably because males were older than females in this study.
Our results also indicate that those living with a low socioeconomic status were at higher risk of developing functional limitations in ADLs. It is consistent with previous studies (27). Moreover, lower socioeconomic status in older age seems to predict ADL limitations more than socioeconomic status at younger age (27). In recent years, some social security programs have been launched or reformed by the government to provide better welfare to the older population, especially in health. The coverage of basic pension insurance has expanded to about one billion people in 2020 (35). Currently, there are three categories of government-funded health insurance programs, namely urban employee medical insurance, urban resident medical insurance, and new rural cooperation medical insurance, with aims to improve the accessibility for medical treatment. However, social medical insurance schemes in China adopts the “payment-before-reimbursement” principle. The insurers are required to pay the medical expenses in advance when seeking medical treatment, then a certain proportion of medical expenses are reimbursed after treatment. A large amount of prepayment may become one of the reasons restricting low-income groups from seeking timely medical treatment (36), which may potential increase risk of ADL limitations due to lack of heath care access. To reduce the healthcare burden for those with serious chronic diseases, in recent years the reimbursement cap for more than 20 chronic diseases including diabetes has been increased to 140,000 Yuan per year, compared to 6,000 Yuan for general diseases in outpatient clinics (37). Targeted supportive policies for those vulnerable subgroups are helpful for maintaining T2DM patients' ADL functions.
There are several limitations to this study. First, some older T2DM patients with severe functional limitations such as having mobility problems or staying in bed may not go to the community service center during the study period and are possibly under-represented. This may lead to the ADL function impaired rate underestimated. Second, evidence has shown that older patients in poorer health were more likely to participate in health services related research (38). Patients who gave explicit written consent may mischaracterize the health status of the larger population. In this study, we did not count how many people were excluded due to not meeting the inclusion criteria or refusing to participate. It is unclear how people who refused differ from those who agreed to participate. Therefore, the generalization of the results should be cautious due to the potential selection bias. Third, cautious should be exercised if extending the results to rural communities. Lastly, the duration of participants' diseases may be associated with functional limitations in ADLs. However, we did not take it into account in the analysis due to unavailability issue.
The growing number of older T2DM patients coupled with a rapidly aging population continues to be a major public health concern in China. Older adults with T2DM especially among those aged ≥70 years had a high prevalence of functional limitations across a range of daily living tasks, which not only affect individual life of quality but also present a huge burden on the family, health services system, and the whole society. Identified factors associated with ADL limitations may provide useful information for targeted nursing practice and health promotion.
The data collected during the current study is not publicly available as the ethics approval only allows for members of the research team access. Upon reasonable request and with permission of the ethics committee, access can be granted. Any queries should be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by Medical Ethics Committee of Fujian Health College. The patients/participants provided their written informed consent to participate in this study.
J-HJ, JX, L-NJ, and H-LZ conceived the study. J-HJ, DL, and H-LZ designed the questionnaire. J-HJ, DL, L-NJ, YC, YY, and BZ did the field work and collected the data. J-HJ, DL, YC, YY, and BZ entered and cleaned the data. J-HJ, JX, and DL analyzed the data. J-HJ drafted the manuscript. JX, DL, L-NJ, YC, YY, CW, BL, RX, and H-LZ reviewed and edited the manuscript. All authors read and approved the final manuscript.
The study was funded by the Medical Innovation Project of Fujian Province (2018-CXB-16) and the Applied Technology Collaborative Innovation Research Project of Fujian Health College (2019-5-1).
The authors would like to thank all participants for participating in this survey and are greatly appreciated for their contributions.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. International Diabetes Federation. IDF Diabetes Atlas 2021. 10th Edn. Available online at: https://diabetesatlas.org/atlas/tenth-edition/ (accessed March 25, 2022).
2. Hu C, Jia W. Diabetes in China: epidemiology and genetic risk factors and their clinical utility in personalized medication. Diabetes. (2018) 67:3–11. doi: 10.2337/dbi17-0013
3. Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of type 2 diabetes–global burden of disease and forecasted trends. J Epidemiol Glob Health. (2020) 10:107–11. doi: 10.2991/jegh.k.191028.001
4. Liu M, Liu SW, Wang LJ, Bai YM, Zeng XY, Guo HB, et al. Burden of diabetes, hyperglycaemia in China from to 2016: Findings from the 1990 to 2016, global burden of disease study. Diabetes Metab. (2019) 45:286–93. doi: 10.1016/j.diabet.2018.08.008
5. Leenders M, Verdijk LB, Van der HL, Adam JJ, Van KJ, Nilwik R, et al. Patients with type 2 diabetes show a greater decline in muscle mass, muscle strength, and functional capacity with aging. J Am Med Dir Assoc. (2013) 14:585–92. doi: 10.1016/j.jamda.2013.02.006
6. Li TJ, Zhou J, Ma JJ, Luo HY, Ye XM. What are the self-management experiences of the elderly with diabetes? A systematic review of qualitative research. World J Clin Cases. (2022) 10:1226–41. doi: 10.12998/wjcc.v10.i4.1226
7. Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for U.S. adults: national health interview survey, 2012. Vital Health Stat 10. (2014) 1–161.
8. Wu JH, Haan MN, Liang J, Ghosh D, Gonzalez HM, Herman WH. Diabetes as a predictor of change in functional status among older Mexican Americans: a population-based cohort study. Diabetes Care. (2003) 26:314–9. doi: 10.2337/diacare.26.2.314
9. Tucker KL, Falcon LM, Bianchi LA, Cacho E, Bermudez OI. Self-reported prevalence and health correlates of functional limitation among Massachusetts elderly Puerto Ricans, Dominicans, and non-Hispanic white neighborhood comparison group. J Gerontol A Biol Sci Med Sci. (2000) 55:M90–7. doi: 10.1093/gerona/55.2.M90
10. Yin T, Yin DL, Xiao F, Xin QQ, Li RL, Zheng XG, et al. Socioeconomic status moderates the association between patient satisfaction with community health service and self-management behaviors in patients with type 2 diabetes: a cross-sectional survey in China. Medicine. (2019) 98:e15849. doi: 10.1097/MD.0000000000015849
11. Dong W, Zhang Q, Yan C, Fu W, Xu L. Residents' satisfaction with primary medical and health services in Western China. BMC Health Serv Res. (2017) 17:298. doi: 10.1186/s12913-017-2200-9
12. Han Y, He Y, Lyu J, Yu C, Bian M, Lee L. Aging in China: perspectives on public health. Glob Health J. (2020) 4:11–7. doi: 10.1016/j.glohj.2020.01.002
13. Fuzhou Government. Population of Fuzhou in 2020 2021. Available online at: http://www.fuzhou.gov.cn/zgfzzt/zjrc/qhyg/202111/t20211123_4251039.htm (accessed March 26, 2022).
14. Su B, Wang Y, Dong Y, Hu G, Xu Y, Peng X, et al. Trends in diabetes mortality in urban and rural China, 1987-2019: a joinpoint regression analysis. Front Endocrinol. (2021) 12:777654. doi: 10.3389/fendo.2021.777654
15. Zheng WH, Lin H. Death status of patients with diabetes mellitus in Fuzhou City from 2011 to 2016 (in Chinese). Chronic Pathematology J. (2018) 19:251–8. doi: 10.16440/j.cnki.1674-8166.2018.03.005
16. Xu YQ, Huang RM, Lu L, Lin LK, Zhang XY. Investigation on the prevalence of diabetes and its influencing factors in Fuzhou residents (in Chinese). Diabetes New World. (2020) 23:40–5. doi: 10.16658/j.cnki.1672-4062.2020.21.040
17. Wang L, Wang Z, Ma Q, Fang G, Yang J. The development and reform of public health in China from 1949 to 2019. Global Health. (2019) 15:45. doi: 10.1186/s12992-019-0486-6
18. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. (1969) 9:179–86. doi: 10.1093/geront/9.3_Part_1.179
20. Lin X, Xu Y, Pan X, Xu J, Ding Y, Sun X, et al. Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci Rep. (2020) 10:14790. doi: 10.1038/s41598-020-71908-9
21. Sinclair A, Abdelhafiz A. Cognitive dysfunction in older adults with type 2 diabetes: links, risks, and clinical implications. Clin Geriatr Med. (2020) 36:407–17. doi: 10.1016/j.cger.2020.04.002
22. Saunders T. Type 2 diabetes self-management barriers in older adults: an integrative review of the qualitative literature. J Gerontol Nurs. (2019) 45:43–54. doi: 10.3928/00989134-20190211-05
23. Wang T, Feng X, Zhou J, Gong H, Xia S, Wei Q, et al. Type 2 diabetes mellitus is associated with increased risks of sarcopenia and pre-sarcopenia in Chinese elderly. Sci Rep. (2016) 6:38937. doi: 10.1038/srep38937
24. Gregg EW, Beckles G, Williamson DF, Leveille SG, Langlois JA, Engelgau MM, et al. Diabetes and physical disability among older US adults. Diabetes Care. (2000) 23:1272–7. doi: 10.2337/diacare.23.9.1272
25. Graf C. The Lawton instrumental activities of daily living scale. Am J Nurs. (2008) 108:52–62. doi: 10.1097/01.NAJ.0000314810.46029.74
26. Li ZH, Lv YB, Kraus VB, Yin ZX, Liu SM, Zhang XC, et al. Trends in the incidence of activities of daily living disability among Chinese older adults from 2002 to 2014. J Gerontol A Biol Sci Med Sci. (2020) 75:2113–8. doi: 10.1093/gerona/glz221
27. Van VA, Zijlstra GR, Witte ND, Duppen D, Stuck AE, Kempen GI, et al. Limitations in activities of daily living in community-dwelling people aged 75 and over: a systematic literature review of risk and protective factors. PLoS ONE. (2016) 11:e0165127. doi: 10.1371/journal.pone.0165127
28. Li Z, Wu J, Li J, Pei L. A cohort study on the influence of the chronic diseases on activities of daily living of the elderly aged 65 years and over in China. Chin J Epidemiol. (2019) 40:33–40. doi: 10.3760/cma.j.issn.0254-6450.2019.01.008
29. Assari S, Lankarani RM, Lankarani MM. Cross-country differences in the association between diabetes and disability. J Diabetes Metab Disord. (2014) 13:3. doi: 10.1186/2251-6581-13-3
30. Qian JH, Cao PY, Wu K, Luo HQ, Ren XH. Investigation of effects of chronic eiseases on activities of eaily living abilities of the elderly in China. J Chin Gen Pract. (2016) 19:4364–9. doi: 10.3969/j.issn.1007-9572.2016.35.015
31. Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China health and retirement longitudinal study (CHARLS). Int J Epidemiol. (2014) 43:61–8. doi: 10.1093/ije/dys203
32. Kalyani RR, Saudek CD, Brancati FL, Selvin E. Association of diabetes, comorbidities, and A1C with functional disability in older adults: results from the National Health and Nutrition Examination Survey (NHANES), 1999–2006. Diabetes Care. (2010) 33:1055–60. doi: 10.2337/dc09-1597
33. Crimmins EM, Kim JK, Hagedorn A. Life with and without disease: women experience more of both. J Women Aging. (2002) 14:47–59. doi: 10.1300/J074v14n01_04
34. Kandrack MA, Grant KR, Segall A. Gender differences in health related behaviour: some unanswered questions. Soc Sci Med. (1991) 32:579–90. doi: 10.1016/0277-9536(91)90293-L
35. Department Department of Aging Health, National National Health Commission of the People's Republic of China. National bulletin on the development of aging health affairs in 2020. Available online at: http://www.nhc.gov.cn/lljks/pqt/202110/c794a6b1a2084964a7ef45f69bef5423.shtml (accessed at May 12, 2022).
36. Yuan H, Chen S, Pan G, Zheng LY. Social pension scheme and health inequality: evidence from China's new rural social pension scheme. Front Public Health. (2021) 9:837431. doi: 10.3389/fpubh.2021.837431
37. Fujian Provincial Healthcare Scurity Bureau. Which types of verified special diseases are eligible for compensation and which diseases are counted as special diseases? Available online at: http://ybj.fujian.gov.cn/hdjl/cjwt/dybz/202108/t20210803_5659361.htm (accessed May 15, 2022).
Keywords: type 2 diabetes, ADL, elderly, functional limitation, comorbidities, Fuzhou
Citation: Jie J-H, Li D, Jia L-N, Chen Y, Yang Y, Zheng B, Wu C, Liu B, Xu R, Xiang J and Zhuang H-L (2022) Activities of daily living and its influencing factors for older people with type 2 diabetes mellitus in urban communities of Fuzhou, China. Front. Public Health 10:948533. doi: 10.3389/fpubh.2022.948533
Received: 06 July 2022; Accepted: 31 August 2022;
Published: 26 September 2022.
Edited by:
Aleksandra Klisic, Primary Health Care Center Podgorica, MontenegroReviewed by:
Shengshu Wang, People's Liberation Army General Hospital, ChinaCopyright © 2022 Jie, Li, Jia, Chen, Yang, Zheng, Wu, Liu, Xu, Xiang and Zhuang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jianjun Xiang, amlhbmp1bi54aWFuZ0Bmam11LmVkdS5jbg==; Hai-Lin Zhuang, MzkyOTY1MTE1QHFxLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.