- 1School of Health Policy and Management, Nanjing Medical University, Nanjing, China
- 2Center for Global Health, Nanjing Medical University, Nanjing, China
- 3School of Health Sciences, Western Sydney University, Campbelltown, NSW, Australia
- 4The George Institute for Global Health, University of New South Wales, Kensington, NSW, Australia
Background: Cancer, the leading cause of mortality in China, is a significant burden on patients, their families, the medical system, and society at large. However, there is minimal data on health service utilization and catastrophic health expenditure (CHE) among cancer patients in China. The objective of this study was to identify factors associated with health care utilization and CHE in Chinese cancer patients.
Methods: The 2018 wave of a nationally representative dataset, the China Health and Retirement Longitudinal Study, was used in our study. Of 18,968 respondents recruited for the analysis, 388 were clinically diagnosed with cancer. CHE was defined as household health expenditure that exceeded 40% of non-food household expenses. A binary logistic regression model was used to identify the risks of cancer exposure among all participants, along with the likelihood of CHE in households with cancer patients at the 40% threshold. A negative binomial regression model was used to identify determinants of health service utilization among cancer patients.
Results: Contracting a family physician (incidence rate ratio IRR: 2.38, 1.18–4.77), Urban Employee Basic Medical Insurance (IRR: 4.02, 1.91–8.46, compared to the uninsured), Urban and Rural Resident Basic Medical Insurance (IRR: 3.08, 1.46–6.49, compared to the uninsured), and higher per-capita household consumption were positively associated with inpatient service utilization. Patients with a college education and above reported a greater number of outpatient visits (IRR: 5.78, 2.56–13.02) but fewer inpatient hospital days (IRR: 0.37, 0.20–0.67). Being diagnosed with a non-cancer chronic non-communicable disease was associated with an increased number of outpatient visits (IRR: 1.20, 1.10–1.31). Of the 388 participants, 50.1% of households had CHE, which was negatively correlated with a larger household size (odds ratio OR: 0.52, 0.32–0.86) and lower socioeconomic status [for quintile 5 (lowest group) OR: 0.32, 0.14–0.72].
Conclusions: The socioeconomic characteristics of cancer patients had a considerable impact on their healthcare utilization. Individualized and targeted strategies for cancer management should be implemented to identify high-risk populations and trace the utilization of care among Chinese cancer patients. Strategic purchasing models in cancer care and social health insurance with expanded benefits packages for cancer patients are crucial to tackling the cancer burden in China.
Introduction
Cancer is a leading cause of mortality worldwide and a substantial impediment to an optimal expected lifespan (1). There were an estimated 4.5 million new cancer cases and 3 million cancer mortalities in 2020 in China, which with the largest population in the world accounts for the highest percentage of total new cancer cases (~23.7%) and mortalities (30.2%) worldwide (2). Cancer incidence and mortality have been rapidly rising in China (2) due to an aging population and cancer-associated lifestyle behaviors (3). Cancer represents a significant burden on patients, their families, the medical system, and society at large.
Aiming to alleviate the burden of non-communicable diseases including cancer, China initiated comprehensive healthcare reform in 2009 committed to delivering equitable accessibility to primary healthcare services with appropriate quality and financial risk protection for all citizens by strengthening healthcare infrastructure, broadening public health insurance coverage, and reforming the healthcare delivery system (4). The Urban Resident Basic Medical Insurance (URBMI) and New Rural Cooperative Medical Scheme (NRCMS) were merged into the Urban and Rural Resident Basic Medical Insurance (URRBMI) in early 2016, which enhanced the health insurance system's ability to pool financial risks for cancer patients (5). Universal Health Coverage improved the availability and utilization of health services (6), although deficiencies remain in quality, efficiency, spending, and patient satisfaction (4). Cancer patients experienced inequitable access to cancer care due to inequalities in health financing, particularly in rural China (7).
Accessing healthcare services can improve patient health but potentially lead to catastrophic health expenditure (CHE), which we defined as the proportion of out-of-pocket (OOP) spending exceeding 40% of household non-food expenses (8). Delivering high-quality care and protecting families from CHE are widely accepted desirable objectives of the healthcare system. These objectives assume that we understand what health system characteristics benefit patients and the factors that affect health service use and CHE. The demand for cancer care spans from the time of diagnosis to the terminal phase of life, making cancer patients particularly susceptible to CHE. Identifying particularly vulnerable groups via susceptibility factors and household characteristics may steer cancer patients to utilize appropriate healthcare services and prevent CHE attributable to cancer care.
Previous studies have highlighted issues related to health service use and economic burden among patients with non-communicable diseases, such as hypertension, diabetes, as well as patients with multiple chronic diseases (9–12). However, factors associated with cancer care utilization and CHE in China remain unclear. Health service use reflects individual behaviors related to obtaining health services to meet their health demands. Existing literature has shown that health service use is affected by individual demographic and socioeconomic factors such as age, gender, marital and employment status, education level, insurance, income (13), and health care system characteristics such as the availability, affordability, and accessibility of drugs and healthcare services (14). Previous studies have reported that health service use among cancer patients differs by sex, age, residence, employment, education, health insurance, household income, tumor site, and tumor stage (15–18). A study of rural-urban disparities among Chinese cancer patients found that rural cancer patients utilized fewer screening and treatment services than urban patients, and that care disparities were significantly influenced by socioeconomic and clinical characteristics (15). Another study on socioeconomic disparities in cancer treatment in China found that a higher proportion of patients with high socioeconomic status underwent surgery and chemotherapy than those with low socioeconomic status (19). Further, socioeconomic status was identified as the most important determinant of treatment modalities for esophageal cancer (16). Evidence from Beijing, China indicated that inpatient costs were 58.6% of total cancer treatment costs, with anti-cancer medication costs accounting for the majority of this burden. Total costs were highly associated with age, tumor type, hospital level, and payment system (20). More than 75% of cancer patients were reported to experience death and catastrophic payments within 1 year in Southeast Asia, especially those without health insurance (21). Other studies performed in China found that CHE occurred in 78.1% of the families of lung cancer patients and 66.28% of the families of breast cancer patients, representing ultra-high OOP expenditures on healthcare in these patient groups (22, 23). Health insurance is thought to be effective against OOP spending, but large disparities exist in the benefit packages between regions with different levels of economic development (24). The Urban Employee Basic Medical Insurance (UEBMI) provides the highest reimbursement cap of the available governmental options.
Reliable predictors of healthcare utilization and CHE are needed to provide further insight for policy makers. This is particularly important now as the cancer spectrum in China transitions from a developing country to a developed one due to its dynamic socio-economic development (25). Efficient cancer control and management systems should be designed and optimized to fit this transition. This work utilized a nationally representative database to investigate factors pertinent to cancer incidence, health service utilization, and CHE among cancer patients in China. Findings may be useful in the development and refinement of individualized and targeted policies to relieve the cancer burden in China.
Methods
Data source
Data used for the current study were derived from the China Health and Retirement Longitudinal Study (CHARLS) in 2018. The CHARLS is a nationwide representative longitudinal survey performed by the National Development Institute of Peking University to serve the needs for scientific and policy research on aging issues by concentrating on Chinese people aged 45 and older and their families. CHARLS included variables related to the demographics, lifestyle habits, health status, health care, household income and consumption, and health insurance of both urban and rural residents (26). CHARLS included 150 districts and 450 rural/urban communities in 28 provinces with a multiple-stage stratified random sampling method to ensure a nationally representative sample. A total of 19,507 respondents were involved in the 2018 wave, which included 392 individuals who were clinically diagnosed with cancer. We eliminated respondents with missing health information or household consumption data, leaving a sample of 18,968 individuals (388 cancer patients).
Indicators
In CHARLS, all respondents were interviewed if they self-identified as clinically diagnosed with cancer through the following question: “Have you been diagnosed with cancer or malignant tumor (excluding minor skin cancers) by a doctor?” The cancer site was recorded. Respondents with minor skin cancers were excluded from the questionnaire as their cancer survivorship care demands tended to be relatively mild (18).
The number of monthly outpatient visits and annual inpatient days were used to measure health care utilization among the cancer patients. In CHARLS, individuals self-reported their utilization of outpatient and inpatient care through the questions: “How many times did you visit/been visited by medical facilities for outpatient care during the last month?” and “How many days did you spend in the hospital during the past year?” CHARLS gathered information on self-reported medical expenditure and total household expenditure for each family. Medical expenditure referred to the patient's outpatient expenses over the past month multiplied by 12 and inpatient expenses over the past year, including OOP expenditure and the portion reimbursed by health insurance. Regarding the total annual household expenditure, we multiplied monthly household expenses on rent, food, clothing, communication, water and electricity, fuel, services, education, traveling, entertainment, beauty, donations, daily necessities, and healthcare by 12.
Annual per-capita household consumption expenditure was adopted to gauge socioeconomic status as household consumption captured the actual living situation of each household (8). We identified five socioeconomic groups using quintiles of annual per-capita household consumption expenditure. Socioeconomic quintiles were established within each county or district and then combined across all sampled counties and districts to reflect the variable level of economic development across the targeted areas.
We defined an OOP payment on health care to be catastrophic if it surpassed 40% of the household's affordability, defined as non-food household consumption spending (8). Based on previous studies, CHE is a binary variable (8). We determined if CHE occurred by calculating the Ei:
Where oop denotes direct medical expenses, deducting reimbursement by health insurance, i represents various households, x is total household consumption expenditure, f(x) is food expenditure, and Z is the CHE threshold, which is set at 40%.
Variables
We considered the following individual-level and household-level variables to be covariates: gender (male and female); age (45~65 and >65 years); household registration (agriculture and non-agriculture); education level (primary school and below, secondary school, and college and above); marital status (married, unmarried, divorced, and widowed); employment status (employed, unemployed, jobless, and retired); physical examination (yes vs. no); family physician (contracted vs. non-contracted); impoverishment status (impoverished vs. non-impoverished); household size (1~2 and ≥3 members); sleep duration; number of chronic diseases; basic health insurance (uninsured, UEBMI, URRBMI, URBMI, NRCMS and the other); socioeconomic groups; and geographic region (east, central, west and northeast).
Statistical analysis
The sociodemographic characteristics of cancer patients were described using frequencies and percentages of categorical variables (e.g., education level, marital status, work status, health insurance, and region). A binary logistic regression model was created to identify the risks of cancer among all participants and CHE in the households of cancer patients. A negative binomial regression analysis was utilized to investigate correlations between demographic and socioeconomic variables and the number of outpatient visits and inpatient days among cancer patients. Odds ratios (OR) and incidence rate ratios (IRR) were quantified to measure the degree of correlations between each contributor and the dependent variables. A sensitivity analysis was performed to investigate the relationship between socioeconomic status quintiles and CHE exposure using the World Bank's various definitions of CHE thresholds, which were computed as OOP expenditures on healthcare of 25 and 40% of non-food household consumption expenditures (27). All statistical analyses were performed using SPSS V.26.0. A two-tailed P < 0.05 was considered significant.
Results
Sociodemographic characteristics of cancer patients
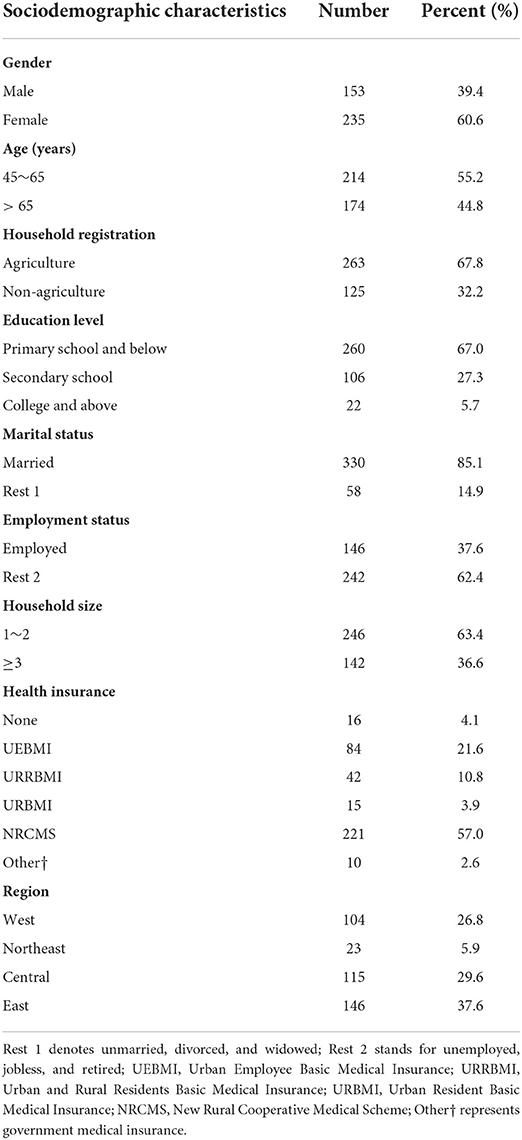
The descriptive sociodemographic statistics of 388 participants with clinically-diagnosed cancer in 2018 are shown in Table 1. A total of 153 (39.4%) respondents were male and 235 (60.6%) were female. Mean age was 63.9 years, with 214 (55.2%) participants 45–65 years old and 174 (44.8%) over 65 years old. Most participants were from rural areas (67.8% of total) and had only primary education or below (67.0% of total). Three hundred thirty (85.1%) participants were married, and 146 (37.6%) were employed. Regarding household size, 246 (63.4%) households with cancer patients had less than three people. The majority (372, 95.9%) of participants were enrolled in at least one type of public health insurance, with 221 (57.0%) participating in the NRCMS. A plurality (146, 37.6%) of participants were from eastern China, followed by its central (29.6%), western (26.8%), and northeastern (5.9%) regions.
Cancer incidence and associated factors
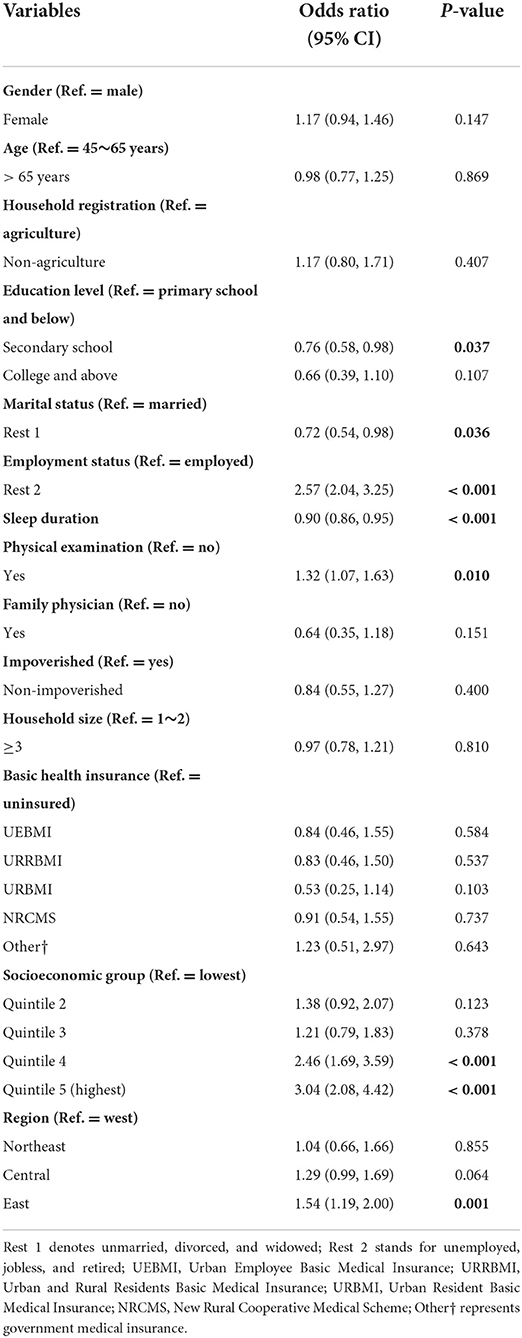
Overall cancer incidence among Chinese adults aged 45 and older in 2018 was 2.05% (388 of 18,968). Participants in higher socioeconomic quintiles had a higher likelihood of reporting a cancer diagnosis compared than those with the lowest socioeconomic status [Quintile 4: OR = 2.46, 95% CI 1.69–3.59; Quintile 5 (highest): OR = 3.04, 95% CI 2.08–4.42]. The likelihood of cancer was higher among participants who lived in eastern China than those in western China (OR = 1.54, 95% CI 1.19–2.00). Compared to employed participants, those who were unemployed, jobless, or retired had a greater incidence of cancer (OR = 2.57, 95% CI 2.04–3.25). Compared with participants who had not had a physical examination, those who obtained a medical check-up had a higher probability of being diagnosed with cancer (OR = 1.32, 95% CI 1.07–1.63). The prevalence of cancer decreased among participants who slept longer (OR = 0.90, 95% CI 0.86–0.95), received a secondary education (OR = 0.76, 95% CI 0.58–0.98 compared with those who had a primary education or less), and were unmarried, divorced, or widowed (OR = 0.72, 95% CI 0.54–0.98, compared to those who were married) (Table 2).
Factors associated with health care utilization
Factors associated with health care utilization and CHE among cancer patients are presented in Table 3. An increasing number of non-communicable diseases (IRR = 1.20, 95% CI 1.10–1.31) and contracting a family physician (IRR = 2.72, 95% CI 1.01–7.35) were associated with more frequent outpatient visits. Compared with those with a primary education and below, patients with college education and above reported more frequent outpatient visits (IRR = 5.78, 95% CI 2.56–13.02) but fewer inpatient hospital days (IRR = 0.37, 95% CI 0.20–0.67). Fewer inpatient hospital days were also found to be positively associated with patients who were female (IRR = 0.55, 95% CI 0.43–0.71), non-agricultural (IRR = 0.25, 95% CI 0.14–0.44), unmarried, divorced, or widowed patients (IRR = 0.57, 95% CI 0.40–0.82), and from eastern China (IRR = 0.68, 95% CI 0.49–0.93). Fewer outpatient visits were also positively associated with patients in families of more than 2 persons (IRR = 0.53, 95% CI 0.34–0.83) and those enrolled in URRBMI (IRR = 0.30, 95% CI 0.10–0.86). Longer inpatient hospital stays were positively associated with patients who were unemployed, jobless, or retired (IRR = 3.37, 95% CI 2.56–4.44), contracted with a family physician (IRR = 2.38, 95% CI 1.18–4.77), in a household of more than two members (IRR = 1.51, 95% CI 1.16–1.96), and enrolled in UEBMI (IRR = 4.02, 95% CI 1.91–8.46), URRBMI (IRR = 3.08, 95% CI 1.46–6.49). The likelihood of inpatient service use decreased substantially with economic status. The number of inpatient hospital days reported among patients in other socioeconomic quintiles were 0.23 (IRR = 0.23, 95% CI 0.16–0.33), 0.11 (IRR = 0.11, 95% CI 0.08–0.16), 0.10 (IRR = 0.10, 95% CI 0.06–0.15), and 0.07 (IRR = 0.07, 95% CI 0.05–0.11) times as many as those in the highest socioeconomic quintile, respectively.

Table 3. Factors associated with health care utilization and catastrophic health expenditure among cancer patients in China, 2018.
CHE incidence and associated factors
50.1% of households with cancer patients were considered to have CHE when a 40% threshold was used. The prevalence of CHE was greater amongst patients who were unemployed, jobless, or retired (OR = 2.68, 95% CI 1.59–4.53) than those who were employed. Compared with households of fewer than three members, a larger family size was protective from CHE (OR = 0.52, 95% CI 0.32–0.86). Further, patients in a lower socioeconomic class had a smaller probability of reporting CHE than those in a higher socioeconomic class. There was no discernible relationship between health insurance and CHE (Table 3). A sensitivity analysis suggested that there was a non-significant correlation between economic status and CHE when the World Bank's definition of CHE at a 25% threshold was used (Supplementary Table S1), which was inconsistent with the base case analysis. In addition, the odds of CHE were lower in non-agricultural households (OR = 0.33, 95% CI 0.12–0.92, compared with agricultural households).
Discussion
This study identifies factors potentially associated with health care utilization and CHE among Chinese cancer patients using a nationwide representative longitudinal survey of the middle-aged and elderly population. These findings provide insights into health service utilization and economic burden of cancer patients. The socioeconomic characteristics (public health insurance and household consumption level) of the patients and their families appear to have significant influence on cancer care. CHE was reported by approximately half of the families of cancer patients, with it occurring more prevalently in higher-income families than in lower-income ones. We also found that cancer was more commonly reported by people with a lower educational level, who were married, unemployed, jobless, or retired, who self-reported a shorter sleep duration, who underwent regular physical examinations, who were in a higher socioeconomic group, and who resided in eastern China.
We observed that cancer was more commonly reported by respondents who were in a higher socioeconomic category. This may be because respondents living in higher-income families had greater access to better healthcare delivery and better wellness education, and therefore were more likely to have an underlying cancer diagnosed than those who lived in lower-income families (28). Individuals from the eastern region reported an increased prevalence of cancer, which likely reflects under-reporting in the western region due to the relative shortage of health resources and accessibility (29). In agreement with a previous study, sleeping for fewer hours was correlated with cancer in Chinese people, which may be the result of physiologic mechanisms (30). Given the cross-sectional nature of our data, we were only able to establish a longitudinal association between sleep duration and cancer incidence.
Health service use by cancer patients in our study was primarily driven by gender, age, household registration, education level, marital status, employment status, physical examination, family physician, household size, health insurance, per-capita household consumption (socioeconomic status), and the number of chronic non-communicable diseases. We observed that the utilization of outpatient care increased as the number of chronic non-communicable diseases increased. This is likely due to the fact that cancer patients with additional diseases are more likely to have complications, and the subsequent demand for intensified care and coordinated treatment could increase outpatient visits (31). This association has been well documented in other studies on multimorbidity (31–33). Also, in agreement with other studies, cancer patients in higher socioeconomic groups were more likely to access and utilize both outpatient and inpatient services (28, 34, 35), exposing inequalities in cancer care. If the economic struggles resulting from cancer are not addressed, its negative impact on healthcare access and utilization may contribute to the deteriorated health status of patients in lower socioeconomic categories and increased cancer mortality (36). In contrast, patients with a higher socioeconomic status had a better prognosis, which may be associated with a higher level of care or even over-medication (17). Our results also found that patients who contracted with a family physician had more frequent outpatient visits and longer inpatient stays. A plausible explanation might be that contracting with a family physician is associated with higher income levels, which could enhance patient disease awareness and treatment compliance (37). However, family physicians serve as the gatekeepers to health care, aiming to prevent chronic diseases by intervening in disease-related lifestyle behaviors in addition to delivering primary health care services that can efficiently lower the hospitalization and mortality of patients and mitigate the burden of chronic disease in China (37). The effect of family physician contracting on the outpatient and inpatient services that were utilized by cancer patients remains for consideration.
We found that individuals with a better educational background utilized more outpatient services but fewer inpatient services. There are several possible reasons for this discrepancy. First, individuals with higher levels of education tend to rank higher in socioeconomic status and capture more appropriate pathways of care (38), such as well check-ups, consultations, and outpatient visits, permitting diseases to be identified at an early stage. Second, populations with lower levels of education may have inadequate knowledge of cancer-related symptoms and signs, so if they took these lightly or lacked illness awareness, they would not approach a clinician for a timely diagnosis (39). The observation that individuals with lower levels of education are at higher risk of cancers of the esophagus, stomach, rectum, rectosigmoid colon, liver, pancreas, lung, kidney, and urinary tract has been previously reported (40), and patients with these cancers often require radiotherapy, chemotherapy, or more intensive treatment (41), requiring a longer inpatient stay.
Social health insurance plans are designed to promote nationwide access to healthcare. Our results showed that patients enrolled in UEBMI and URRBMI reported significantly longer inpatient stays compared with non-enrolled patients, whereas URBMI and NCRMS did not influence this outcome. An explanation for this observation is that fewer inpatient services were available to people who were covered by URBMI and NCRMS due to restricted benefits packages and reduced coverage compared with other schemes (24). Cancer patients enrolled in UEBMI were more likely to spend more time in the hospital, suggesting that UEBMI is superior to URRBMI in terms of reimbursement level. Regarding outpatient visits, our findings showed that health insurance plans seemed to have minimal impact on the decision to utilize outpatient services except for the URRBMI, whose members had fewer outpatient visits compared with uninsured patients. A previous study reported that Chinese people tended to favor inpatient services over outpatient services regardless insurance type (42), and that cancer patients might have a stronger preference toward hospitalization due to their unique treatment needs.
Our study reported that the prevalence of families with cancer patients that experienced CHE was 50.1% at a 40% threshold. Compared with other cancer studies that used the same definition and threshold of CHE, our study of Chinese showed a higher prevalence of CHE than Iran (13.77%) (43) and Malaysia (47.8%) (44), which might be attributed to the disparities in the income levels and health insurance packages between these countries. The overall prevalence of CHE among the general Chinese population was only 8.94% in 2016 in China (45). The significant discrepancy indicates that OOP spending on cancer care imposes a substantial financial burden on more than half of Chinese families with cancer patients. Moreover, the calculation of OOP spending we used only captured the direct expenses of cancer care, and our statistic is therefore conservative given the exclusion of indirect expenses such as transport and accommodation. Our findings also suggest that a large household size could shelter some families with cancer patients against CHE. One potential hypothesis for this is that family members would care for each other and provide both material and psychological assistance to those with severe diseases. A larger household size may also represent increased household consumption and income, and therefore may be a protective factor when income exceeds consumption.
While it is generally acknowledged that better-off families were more capable of coping with healthcare spending than poorer families (21), our study found that households with cancer patients that were at a higher socioeconomic level had a higher probability of experiencing CHE. There are several possible explanations for this inconsistency. First, most cancer patients with a low economic status in our study were from agricultural families. They were less likely to purchase health services due to their inadequate health knowledge of the incidence of cancer and inefficient allocation of health resources to rural regions, which may reduce the incidence of CHE (39, 46). Secondly, cancer therapy is highly expensive due to the need for repetitive hospitalizations, multiple consultations, advanced laboratory examinations, chemotherapy, rare and costly drugs, surgery and radiation therapy, and other essential care (47). Cancer patients with a low economic status might therefore forgo therapy on account of the high OOP payments and the potential impact of their care on the livelihoods of other family members, making it possible for families to avert CHE but resulting in worse health outcomes. In contrast, people in higher-income classes require greater absolute levels of spending than people in lower-income classes to trigger the so-called CHE threshold. Our results suggest that higher OOP expenses could be reflective of receiving more intensive and expensive health-care services (36), or the purchase of high-quality services from private facilities by bypassing the inconvenience of public facilities. Private healthcare services are generally more expensive than public services because they are primarily driven by the demand of better-off individuals for high-quality services (48). Finally, while the improved survival of better-off cancer patients was the result of proactive therapy, post-cancer care requires sustained financial support (17), which may increase the risk of CHE. We also found that CHE had no significant association with health insurance, indicating that public health insurance failed reduce the financial risks posed by cancer to the patient's family.
Our findings add to the body of evidence that supports the development of targeted policies and strategies to address China's growing cancer burden. The occurrence of cancer among middle-aged and elderly patients is significantly affected by social variables such as education level, marital status, employment and socioeconomic status, and geography, which involve multiple societal domains. Contemporary public health strategies require cross-sectoral collaboration to improve social determinants of health and implement effective prevention strategies that target high-risk populations (49). We also observed a significant association between health care utilization and the socioeconomic characteristics of cancer patients. Policymakers should take the socioeconomic burdens experienced by cancer patients into consideration when formulating practice guidelines on cancer management so as to facilitate efficient and individualized treatment solutions. For example, a nationwide representative cancer registry with enhanced quality and targeting will facilitate the identification of treatment priorities and care utilization among Chinese cancer patients (50). To alleviate the burden of providing cancer care and improve disease prognosis, the government needs to raise screening awareness among targeted vulnerable populations and enhance the likelihood of detecting cancer at an early stage. A cancer screening and early detection network is present in 31 provinces of China as of 2015, but whole population screenings are not offered except for breast and cervical cancer (51). OOP spending is the most significant determinant of catastrophic expenditure. In China, the high OOP expenditures on healthcare may be due to fee-for-service payment mechanisms and the failure of public health insurance to bear financial risks (52). Cancer care payment model reform is required to improve the financial burden that cancer treatment places on Chinese families. A patient-centered and value-oriented alternative payment model for oncology is recommended due to its significant associations with improved cancer care quality and reduced resource use and care costs (53). China has almost achieved universal health insurance coverage, yet catastrophic payments for cancer patients remain too high. This may be due to the restrictions of current benefit packages and the small scale of medical aid (54). Future health insurance schemes should strengthen financial protection for Chinese cancer patients in a targeted manner.
Our study had several limitations. First, given that cancer diagnosis was self-reported, the incidence of cancer in China was potentially underestimated. This assumption is even more profound in vulnerable populations who are less likely to be diagnosed with cancer at an early stage. Second, health service use and health payments among cancer patients were also self-reported. These are also prone to underestimation, especially among older adults and those with a lower education level. Third, our sample size was rather small for this type of study. A larger sample should be used in future work. Given that many of our findings indicate that better-off families were less likely to experience CHE (45), future studies should use other indicators of socioeconomic groups beyond socioeconomic status quintiles. Future work should also take into consideration variables related to mental health because of its significant impact on care-seeking behaviors (55). Finally, this research only recruited Chinese people aged 45 years and older. Future studies should consider the impact of cancer on younger cohorts.
Conclusion
The socioeconomic characteristics of cancer patients had a considerable impact on their healthcare utilization, especially health insurance and socioeconomic status. OOP spending on cancer care imposed a substantial financial burden on more than half of Chinese households with cancer patients, particularly those from better-off households. Public health insurance failed to reduce the financial risks posed to cancer patients' families. Individualized and targeted guidelines for cancer management, strategic purchasing models in cancer care, and social health insurance with expanded benefit packages are crucial to easing the burden of cancer care in China.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
PD led the study including the interpretation of the results and manuscript drafting. LS and MC conceived and supervised the study. YF contributed to data analysis and drafting of the manuscript. All authors reviewed and approved the final manuscript.
Funding
This study was funded by the National Natural Science Foundation of China (Grant Numbers: 71874086 and 72174093) and the Postgraduate Research and Practice Innovation Program of Jiangsu Province (Grant Number: KYCX21_1561).
Acknowledgments
We appreciate the China Health and Retirement Longitudinal Study Team. We are also very grateful to the support by the Public Health Policy and Management Innovation Research Team, which is an Excellent Innovation Team of Philosophy and Social Sciences in Jiangsu Universities granted by the Jiangsu Education Department.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.943271/full#supplementary-material
References
1. Bray F, Laversanne M, Weiderpass E, Soerjomataram I. The ever-increasing importance of cancer as a leading cause of premature death worldwide. Cancer. (2021) 127:3029–30. doi: 10.1002/cncr.33587
2. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660
3. Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, et al. Cancer statistics in China, 2015. CA Cancer J Clin. (2016) 66:115–32. doi: 10.3322/caac.21338
4. Yip W, Fu H, Chen AT, Zhai T, Jian W, Xu R, et al. 10 years of health-care reform in China: progress and gaps in universal health coverage. Lancet. (2019) 394:1192–204. doi: 10.1016/S0140-6736(19)32136-1
5. Mao W, Tang S, Zhu Y, Xie Z, Chen W. Financial burden of healthcare for cancer patients with social medical insurance: a multi-centered study in urban China. Int J Equity Health. (2017) 16:180. doi: 10.1186/s12939-017-0675-y
6. Chen M, Zhou G, Si L. Ten years of progress towards universal health coverage: has China achieved equitable healthcare financing? BMJ Glob Health. (2020) 5:e003570. doi: 10.1136/bmjgh-2020-003570
7. Zhou G, Jan S, Chen M, Wang Z, Si L. Equity in healthcare financing following the introduction of the unified residents' health insurance scheme in China. Health Policy Plan. (2022) 37:209–17. doi: 10.1093/heapol/czab124
8. O'Donnell O, Doorslaer EV, Wagstaff A, Lindelow M. Analyzing health equity using household survey data: a guide to techniques and their implementation. The World Bank. (2008). doi: 10.1596/978-0-8213-6933-3
9. Liu X, Sun X, Zhao Y, Meng Q. Financial protection of rural health insurance for patients with hypertension and diabetes: repeated cross-sectional surveys in rural China. BMC Health Serv Res. (2016) 16:481. doi: 10.1186/s12913-016-1735-5
10. Zhao Y, Mahal AS, Haregu TN, Katar A, Oldenburg B, Zhang L. Trends and inequalities in the health care and hypertension outcomes in China, 2011 to 2015. Int J Environ Res Public Health. (2019) 16:4578. doi: 10.3390/ijerph16224578
11. Fu Y, Chen M, Si L. Multimorbidity and catastrophic health expenditure among patients with diabetes in China: a nationwide population-based study. BMJ Glob Health. (2022) 7:e007714. doi: 10.1136/bmjgh-2021-007714
12. Zhao Y, Atun R, Oldenburg B, McPake B, Tang S, Mercer SW, et al. Physical multimorbidity, health service use, and catastrophic health expenditure by socioeconomic groups in China: an analysis of population-based panel data. Lancet Global Health. (2020) 8:e840–e9. doi: 10.1016/S2214-109X(20)30127-3
13. Hu H, Jian W, Fu H, Zhang H, Pan J, Yip W. Health service underutilization and its associated factors for chronic diseases patients in poverty-stricken areas in China: a multilevel analysis. BMC Health Serv Res. (2021) 21:707. doi: 10.1186/s12913-021-06725-5
14. Haque MR, Parr N, Muhidin S. Parents' healthcare-seeking behavior for their children among the climate-related displaced population of rural Bangladesh. Soc Sci Med. (2019) 226:9–20. doi: 10.1016/j.socscimed.2019.02.032
15. Wang H, Hua X, Yao N, Zhang N, Wang J, Anderson R, et al. The urban-rural disparities and associated factors of health care utilization among cancer patients in China. Front Public Health. (2022) 10:842837. doi: 10.3389/fpubh.2022.842837
16. Wang N, Cao F, Liu F, Jia Y, Wang J, Bao C, et al. The effect of socioeconomic status on health-care delay and treatment of esophageal cancer. J Transl Med. (2015) 13:241. doi: 10.1186/s12967-015-0579-9
17. Kenzik KM. Health care use during cancer survivorship: review of 5 years of evidence. Cancer. (2019) 125:673–80. doi: 10.1002/cncr.31852
18. Coughlin SS, Chen J, Cortes JE. Health care access and utilization among adult cancer survivors: results from the national institutes of health “all of us” research program. Cancer Med. (2021) 10:3646–54. doi: 10.1002/cam4.3924
19. Zhao Y, Tang S, Mao W, Akinyemiju T. Socio-economic and rural-urban differences in healthcare and catastrophic health expenditure among cancer patients in China: analysis of the China health and retirement longitudinal study. Front Public Health. (2021) 9:779285. doi: 10.3389/fpubh.2021.779285
20. Yin X, Xu Y, Man X, Liu L, Jiang Y, Zhao L, et al. Direct costs of both inpatient and outpatient care for all type cancers: the evidence from Beijing, China. Cancer Med. (2019) 8:3250–60. doi: 10.1002/cam4.2184
21. Group AS, Kimman M, Jan S, Yip CH, Thabrany H, Peters SA, et al. Catastrophic health expenditure and 12-month mortality associated with cancer in Southeast Asia: results from a longitudinal study in eight countries. BMC Med. (2015) 13:190. doi: 10.1186/s12916-015-0433-1
22. Sun CY, Shi JF, Fu WQ, Zhang X, Liu GX, Chen WQ, et al. Catastrophic health expenditure and its determinants in households with lung cancer patients in China: a retrospective cohort study. BMC Cancer. (2021) 21:1323. doi: 10.1186/s12885-021-09030-w
23. Sun CY, Shi JF, Fu WQ, Zhang X, Liu GX, Chen WQ, et al. Catastrophic health expenditure and its determinants among households with breast cancer patients in China: a multicentre, cross-sectional survey. Front Public Health. (2021) 9:704700. doi: 10.3389/fpubh.2021.704700
24. Meng Q, Fang H, Liu X, Yuan B, Xu J. Consolidating the social health insurance schemes in China: towards an equitable and efficient health system. Lancet. (2015) 386:1484–92. doi: 10.1016/S0140-6736(15)00342-6
25. Qiu H, Cao S, Xu R. Cancer incidence, mortality, and burden in China: a time-trend analysis and comparison with the United States and United Kingdom based on the global epidemiological data released in 2020. Cancer Commun. (2021) 41:1037–48. doi: 10.1002/cac2.12197
26. Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. (2014) 43:61–8. doi: 10.1093/ije/dys203
27. Cylus J, Thomson S, Evetovits T. Catastrophic health spending in Europe: equity and policy implications of different calculation methods. Bull World Health Organ. (2018) 96:599–609. doi: 10.2471/BLT.18.209031
28. Nuche-Berenguer B, Sakellariou D. Socioeconomic determinants of participation in cancer screening in argentina: a cross-sectional study. Front Public Health. (2021) 9:699108. doi: 10.3389/fpubh.2021.699108
29. Liu W, Liu Y, Twum P, Li S. National equity of health resource allocation in China: data from 2009 to 2013. Int J Equity Health. (2016) 15:68. doi: 10.1186/s12939-016-0357-1
30. Chen Y, Tan F, Wei L, Li X, Lyu Z, Feng X, et al. Sleep duration and the risk of cancer: a systematic review and meta-analysis including dose-response relationship. BMC Cancer. (2018) 18:1149. doi: 10.1186/s12885-018-5025-y
31. Palladino R, Tayu Lee J, Ashworth M, Triassi M, Millett C. Associations between multimorbidity, healthcare utilisation and health status: evidence from 16 European countries. Age Ageing. (2016) 45:431–5. doi: 10.1093/ageing/afw044
32. Harrington RL, Qato DM, Antoon JW, Caskey RN, Schumock GT, Lee TA. Impact of multimorbidity subgroups on the health care use of early pediatric cancer survivors. Cancer. (2020) 126:649–58. doi: 10.1002/cncr.32201
33. Kone AP, Scharf D. Prevalence of multimorbidity in adults with cancer, and associated health service utilization in Ontario, Canada: a population-based retrospective cohort study. BMC Cancer. (2021) 21:406. doi: 10.1186/s12885-021-08102-1
34. Kumachev A, Trudeau ME, Chan KK. Associations among socioeconomic status, patterns of care and outcomes in breast cancer patients in a universal health care system: Ontario's experience. Cancer. (2016) 122:893–8. doi: 10.1002/cncr.29838
35. Lundon DJ, Dovey Z, Tewari AK. Access and socioeconomic status play an important role in outcomes for African American patients with prostate cancer. Cancer. (2020) 126:4257–8. doi: 10.1002/cncr.33063
36. Merletti F, Galassi C, Spadea T. The socioeconomic determinants of cancer. Environ Health. (2011) 10(Suppl 1):S7. doi: 10.1186/1476-069X-10-S1-S7
37. Li Z, Li J, Fu P, Chen Y, Jing Z, Yuan Y, et al. Family doctor contract services and health-related quality of life among patients with chronic diseases in rural China: what is the role of socioeconomic status? Int J Equity Health. (2021) 20:191. doi: 10.1186/s12939-021-01530-2
38. Galobardes B, Shaw M, Lawlor DA, Lynch JW, Davey Smith G. Indicators of socioeconomic position (part 1). J Epidemiol Community Health. (2006) 60:7–12. doi: 10.1136/jech.2004.023531
39. Esther N, Julius S, Deogratius MA. Understanding health-seeking and adherence to treatment by patients with esophageal cancer at the Uganda cancer Institute: a qualitative study. BMC Health Serv Res. (2021) 21:159. doi: 10.1186/s12913-021-06163-3
40. Larsen IK, Myklebust TA, Babigumira R, Vinberg E, Moller B, Ursin G. Education, income and risk of cancer: results from a Norwegian registry-based study. Acta Oncol. (2020) 59:1300–7. doi: 10.1080/0284186X.2020.1817548
41. Miller KD, Nogueira L, Mariotto AB, Rowland JH, Yabroff KR, Alfano CM, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. (2019) 69:363–85. doi: 10.3322/caac.21565
42. Tan SY, Wu X, Yang W. Impacts of the type of social health insurance on health service utilisation and expenditures: implications for a unified system in China. Health Econ Policy Law. (2019) 14:468–86. doi: 10.1017/S174413311800018X
43. Ahmadi F, Farrokh-Eslamlou H, Yusefzadeh H, Alinia C. Incidence of household catastrophic and impoverishing health expenditures among patients with breast cancer in Iran. BMC Health Serv Res. (2021) 21:327. doi: 10.1186/s12913-021-06330-6
44. Azzani M, Yahya A, Roslani AC, Su TT. Catastrophic health expenditure among colorectal cancer patients and families: a case of Malaysia. Asia Pac J Public Health. (2017) 29:485–94. doi: 10.1177/1010539517732224
45. Ma X, Wang Z, Liu X. Progress on catastrophic health expenditure in China: evidence from China family panel studies (CFPS) 2010 to 2016. Int J Environ Res Public Health. (2019) 16:4775. doi: 10.3390/ijerph16234775
46. Sun J, Luo H. Evaluation on equality and efficiency of health resources allocation and health services utilization in China. Int J Equity Health. (2017) 16:127. doi: 10.1186/s12939-017-0614-y
47. Barr RD, Feeny D, Furlong W. Economic evaluation of treatments for cancer in childhood. Eur J Cancer. (2004) 40:1335–45. doi: 10.1016/j.ejca.2004.01.033
48. Somkotra T, Lagrada LP. Which households are at risk of catastrophic health spending: experience in Thailand after universal coverage. Health Aff. (2009) 28:w467–78. doi: 10.1377/hlthaff.28.3.w467
49. DeSalvo KB, O'Carroll PW, Koo D, Auerbach JM, Monroe JA. Public health 3.0: time for an upgrade. Am J Public Health. (2016) 106:621–2. doi: 10.2105/AJPH.2016.303063
50. Wei W, Zeng H, Zheng R, Zhang S, An L, Chen R, et al. Cancer registration in China and its role in cancer prevention and control. Lancet Oncol. (2020) 21:e342–e9. doi: 10.1016/S1470-2045(20)30073-5
51. Zou XN. Epidemic trend, screening, and early detection and treatment of cancer in Chinese population. Cancer Biol Med. (2017) 14:50–9. doi: 10.20892/j.issn.2095-3941.2016.0047
52. Hu S, Tang S, Liu Y, Zhao Y, Escobar M-L, de Ferranti D. Reform of how health care is paid for in China: challenges and opportunities. Lancet. (2008) 372:1846–53. doi: 10.1016/S0140-6736(08)61368-9
53. Nejati M, Razavi M, Harirchi I, Zendehdel K, Nejati P. The impact of provider payment reforms and associated care delivery models on cost and quality in cancer care: a systematic literature review. PLoS ONE. (2019) 14:e0214382. doi: 10.1371/journal.pone.0214382
54. Fang H, Eggleston K, Hanson K, Wu M. Enhancing financial protection under China's social health insurance to achieve universal health coverage. BMJ. (2019) 365:l2378. doi: 10.1136/bmj.l2378
Keywords: health care utilization, catastrophic health expenditure, factors, cancer, China
Citation: Deng P, Fu Y, Chen M and Si L (2022) Factors associated with health care utilization and catastrophic health expenditure among cancer patients in China: Evidence from the China health and retirement longitudinal study. Front. Public Health 10:943271. doi: 10.3389/fpubh.2022.943271
Received: 13 May 2022; Accepted: 26 October 2022;
Published: 10 November 2022.
Edited by:
Xuefeng Xie, Anhui Medical University, ChinaReviewed by:
ShaoLiang Tang, Nanjing University of Chinese Medicine, ChinaChun Xia, Anhui Normal University, China
Copyright © 2022 Deng, Fu, Chen and Si. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mingsheng Chen, Y21zQG5qbXUuZWR1LmNu
 Penghong Deng
Penghong Deng Yu Fu
Yu Fu Mingsheng Chen
Mingsheng Chen Lei Si
Lei Si