
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 28 July 2022
Sec. Infectious Diseases – Surveillance, Prevention and Treatment
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.938642
This article is part of the Research TopicPublic Health Policy and Health Communication Challenges in the COVID-19 Pandemic and InfodemicView all 15 articles
 Ramya Nagarajan1
Ramya Nagarajan1 Polani Rubeshkumar2
Polani Rubeshkumar2 Murugesan Jagadeesan3
Murugesan Jagadeesan3 Mohankumar Raju2
Mohankumar Raju2 Manikandanesan Sakthivel1
Manikandanesan Sakthivel1 Sharan Murali1
Sharan Murali1 Muthappan Sendhilkumar1
Muthappan Sendhilkumar1 Kumaravel Ilangovan1
Kumaravel Ilangovan1 Dineshkumar Harikrishnan1
Dineshkumar Harikrishnan1 Vettrichelvan Venkatasamy1
Vettrichelvan Venkatasamy1 Parasuraman Ganeshkumar2
Parasuraman Ganeshkumar2 Prabhdeep Kaur1*
Prabhdeep Kaur1*Background: Wearing a mask is one of the simplest ways to reduce the spread of COVID-19. Studies reported poor mask compliance in Greater Chennai Corporation, India. Hence, we described the knowledge, attitude, and practice regarding mask use among adults (≥18 years) in Greater Chennai Corporation, Tamil Nadu, India.
Methods: We conducted a cross-sectional survey among residents of Greater Chennai Corporation in March 2021. We estimated the sample size to be 203 per strata (slum and non-slum). We used a simple random sampling technique to select 20 locations using a digital map in the slum and non-slum areas. After reaching the location chosen, we selected 10 consecutive households and one adult (≥18 years of age) from each household. We used a validated, semi-structured questionnaire for collecting data regarding knowledge, attitudes, and practices for mask use. We estimated proportions and 95% CI for key variables and compared the variables between slums and non-slums.
Results: Of 430 participants included in the study, 51.4% were males. The mean (S.D.) age of the participants is 41.1 (14.6) years. The majority (86.7%) of the participants felt that wearing a mask helped in reducing the spread of coronavirus and the knowledge differed (p-value < 0.05) between the slum (81.4%) and non-slum (92.3%). Nearly half (46.5%) of the participants did not like being forced to wear the mask. About 63.9% of the participants reported the practice of mask use while going out which was similar across slums and non-slums.
Conclusion: Although the knowledge regarding mask use was good among the public, the attitude was unfavorable. We suggest continuous reinforcement by spreading awareness and educating the community on the appropriate use of the mask.
Mask usage is considered one of the vital non-pharmacological interventions to control the spread of COVID-19 (1). It has been scientifically proven and recommended by global public health organizations to reduce the transmissibility and risk of infection due to SARS-CoV-2 (2–8). The World Health Organization (WHO), the U.S. Centers for Disease Control and Prevention (CDC), the Government of India, and numerous other government and public health agencies have recommended that people use masks in public settings when SARS-CoV-2, the virus that causes COVID-19, is being transmitted in the community (9–11). Early in the pandemic, before accumulating evidence that mask-wearing can reduce the spread of COVID-19, some countries with no history of the practice resisted adopting mask-wearing recommendations (12). In settings, mainly in Asia, where mask-wearing is common for people with even a minor cold, people were likelier to wear masks in public spaces, even without mandates.
As scientific understanding of COVID-19 has evolved, the importance of widespread use of masks has become clear, in part because of the transmission dynamics of the virus (13). People with COVID-19 are most infectious early in the disease, including before symptoms develop, and many people infected with COVID-19 never develop symptoms (14). The higher prevalence of asymptomatic infection makes wearing masks crucial, even among people who feel healthy (15). Promotion of mask-wearing should be part of a package of measures that includes handwashing, physical distancing, and interventions to reduce indoor exposures, find infected people and their contacts quickly, and provide rapid and supportive isolation and quarantine services (16).
Even with the increased necessity of face mask use, there is a wide variation in the knowledge, attitude and practice of mask use across the globe. While Tajvar et al. has documented poor knowledge with good attitude and practice toward mask use in Iran (17), Pramana et al. has documented satisfactory results in Indonesia (18). However, according to Azlan et al., Malaysia majority had a positive attitude toward mask use, but only half of the study participants were using face masks regularly (19). But a study by Tan et al. in China showed good compliance to mask use (20).
Although transmission risk is higher in indoor settings, the mask mandate was monitored, and authorized officials-imposed fines on non-compliant individuals, predominantly in public places such as traffic signals and streets (21). Our team previously conducted three surveys to monitor mask compliance in Chennai. We conducted the surveys in October 2020, December 2020, and March 2021. We selected outdoor public places for the first survey and added indoor settings in the second and third surveys. The compliance to appropriate mask use in three rounds was 28, 29, and 21% in the slums. The compliance was 36%, 35%, and 27% in non-slums after observing 3,600 individuals from 64 selected city streets (22). Additionally, indoor compliance was 11% in slums and 10% in the non-slums, while malls in the city showed the highest compliance for appropriate use of masks (57%) during the second round (22).
Although we documented poor compliance, there was limited understanding regarding attitudes and awareness in the population, which could influence their behaviors. Understanding the knowledge, attitude and practices (KAP) of the population will help the program managers and policy makers in strategizing the Information, Education and Communication (IEC) activities related to mask use. Based on our literature search there are no other studies on mask use from Greater Chennai Corporation or Tamil Nadu in community setting to determine KAP regarding mask use in India. Hence, we carried out this study to bridge this gap by estimating the knowledge and practices regarding the appropriate mask use and attitude toward wearing masks among adults in Greater Chennai Corporation, Tamil Nadu, India.
We conducted a cross-sectional survey among residents of Greater Chennai Corporation in March 2021. Chennai is a city in southern India governed by Greater Chennai Corporation. It is administratively divided into 15 zones covering 200 wards. This study was conducted in all the zones of Greater Chennai Corporation, covering both the slum and non-slum populations equally. The study population was adults ≥18 years of age residing within Greater Chennai Corporation.
The sample size was estimated separately for the slum and non-slum populations. As per our previous survey (22), 70% of the population followed inappropriate mask use. With that we assumed that 70% of the study participants did not have the knowledge of appropriate mask use and estimated the sample size as 203 with 10% absolute precision, 95% confidence level, 20% non-response rate, and a design effect of 2. We included two strata, namely slum and non-slums. Hence sample size is 406 with 203 per strata.
All the zones under Greater Chennai Corporation limits were included in the study. We created a linelist of street separately for slums and non-slums. We randomly selected 20 sreets each from slums and non-slums. In each street we randomly selected a starting point using digital map. After selecting the starting point, we surveyed 10 consecutive households in the same street. We surveyed one adult (≥18 years of age) from each household available at home for the interview. If more than one eligible individual was available at home during the visit, we randomly selected one individual.
We reviewed the sample questionnaire on mask use from other studies and adapted it to the local setting (23). It was a validated, semi-structured questionnaire. We collected details on the sociodemographic profile, information on exposure to COVID-19, knowledge regarding masks used in different settings such as public places, public transport, attitude related to the mandatory mask use, and mask disposal practices. Most knowledge, attitude, and practice questions were asked on a Likert scale. However, the scales varied across the questions depending upon the nature of the question (Supplementary File 1). The data collection tool was translated into the vernacular language, pre-tested, and revised before the survey. We trained the field-level data collection team members and conducted simulation sessions to minimize the inter-observer variation. The data collection teams then interviewed the selected members face-to-face using the Open Data Kit (ODK) tool. COVID-19 appropriate behaviors were followed during the interview process.
We defined “mask” as any cloth mask, medical mask, or N95 respirator worn over the face. “Public places” included both indoor and outdoor settings open to the public and did not have any entry restrictions (e.g., streets, bus stops, railway stations, grocery shops, vegetable shops, pharmacies, religious places, and apparel stores). Indoor Public places included places such as gyms, convention centers, and marriage halls. Outdoor places included places such as shops, bus stops, railway station, and religious places. “Workplace” included occupational settings open only to employees with limited access to the general public.
We estimated the proportions with a 95% confidence interval (CI) using Stata version 16. We estimated the proportion of individuals who felt adopting appropriate mask use while in public places and at public transportation is needed. We also estimated the proportion of individuals who thought they shouldn't be forced to use masks and those who adopted appropriate mask disposal methods. We also used the chi-square test to compare the variables between the slum and non-slum populations. A p-value < 0.05 was considered statistically significant.
The approval for the study was obtained from the Institutional Ethics Committee, ICMR–NIE Chennai. Informed verbal consent was obtained from the study participants before collecting the data.
Of 430 participants in our study, 221 were from slum areas and 209 from non-slum areas. Nearly half of the study participants (51.4%) were males (Table 1). The mean (S.D.) age of the participants was 41.1 (14.6) years (Slum: 42.4 (14.8) years; non-slum: 39.8 (14.3) years). Most of the study participants from the slums had secondary school education (34.3%), while those from the non-slums had graduate-level education (41.1%). Nearly 29.3% of the study participants were homemakers, followed by government employees (16.2%), and daily wage workers (8.8%), while rest of the population were self-employed, non-government employees, non-paid workers, students, retired personnel, and unemployed. Although the distribution of occupation did not vary between slums and non-slums (Table 1).
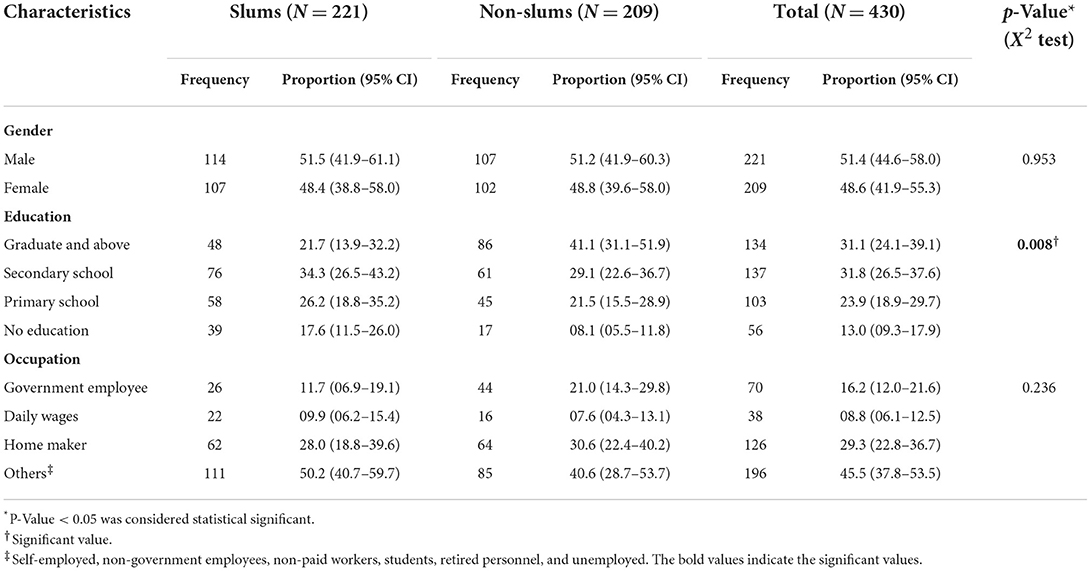
Table 1. Sociodemographic profile of the study participants, Greater Chennai Corporation, India, March 2021 (N = 430).
A large proportion (86.7%) of respondents reported that mask-wearing reduces Coronavirus spread (Table 2). The knowledge was higher among respondents in non-slums compared to slums (92.3 vs. 81.4%, p < 0.05). The majority (87.6%) of the participants knew that masks should be worn while going to a public place, while 85.1% knew that masks should be worn while traveling in public transport. Nearly 80.9 and 83.9% of the participants knew that masks should be worn indoors and in public places. The indicators assessing the knowledge related to mask use in a public place and public transportation were similar among slums and non-slums (Table 2).
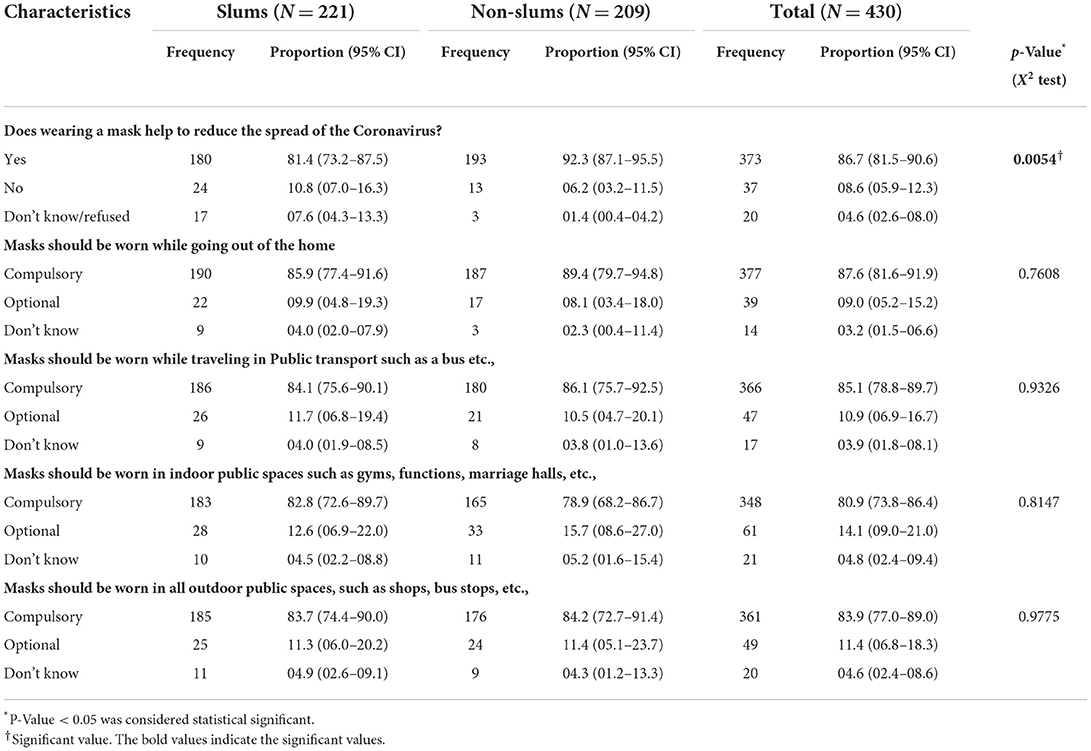
Table 2. Knowledge of mask use among the slum and non-slum population, Greater Chennai Corporation, India, March 2021 (N = 430).
Nearly half (46.5%) of the participants felt they should not be forced to wear masks (Table 3). One-quarter (23.4%) of the participants reported that if they wear a mask in public, others will think they are affected by COVID-19. Nearly half of the subjects said masks disrupted breathing, caused overheating, and disturbed conversations. The proportion for attitude-related questions was similar among slums and non-slums. Out of 430 participants, 285 (66.2%) felt masks were not expensive.
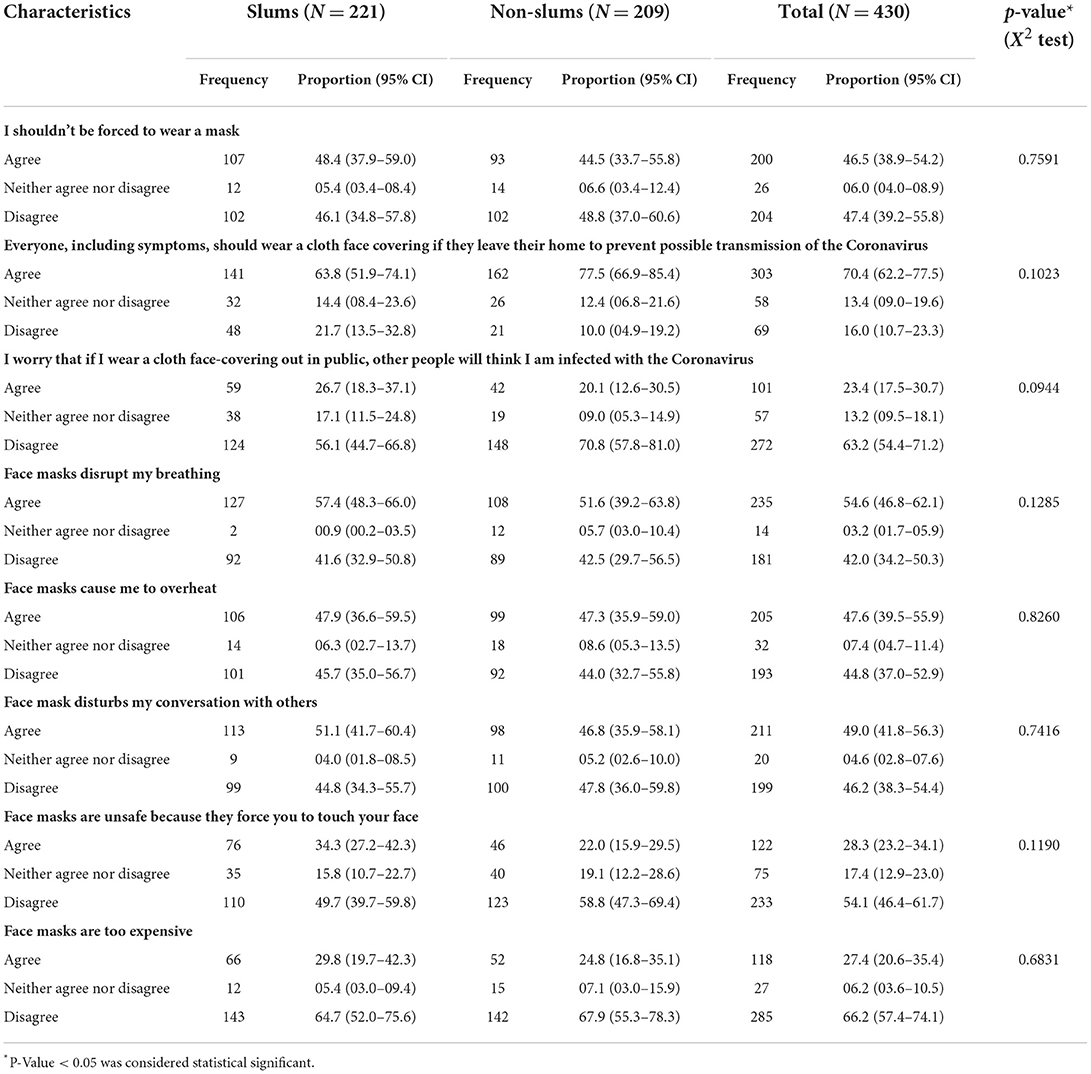
Table 3. Attitude toward mask use among the slum and non-slum population, Greater Chennai Corporation, India, March 2021 (N = 430).
About 63.9% of the participants reported consistent mask use while going out (Table 4), while 58.8% used masks at their workplaces (Table 5). Most participants (86.7%) reported covering their chin, mouth, and nose while wearing the mask (Table 4). Handwashing after mask use was higher among non-slum respondents than among slum (47.4 vs. 26.2%, p < 0.05). Most participants disposed of their masks in a closed or public bin (91.2%).
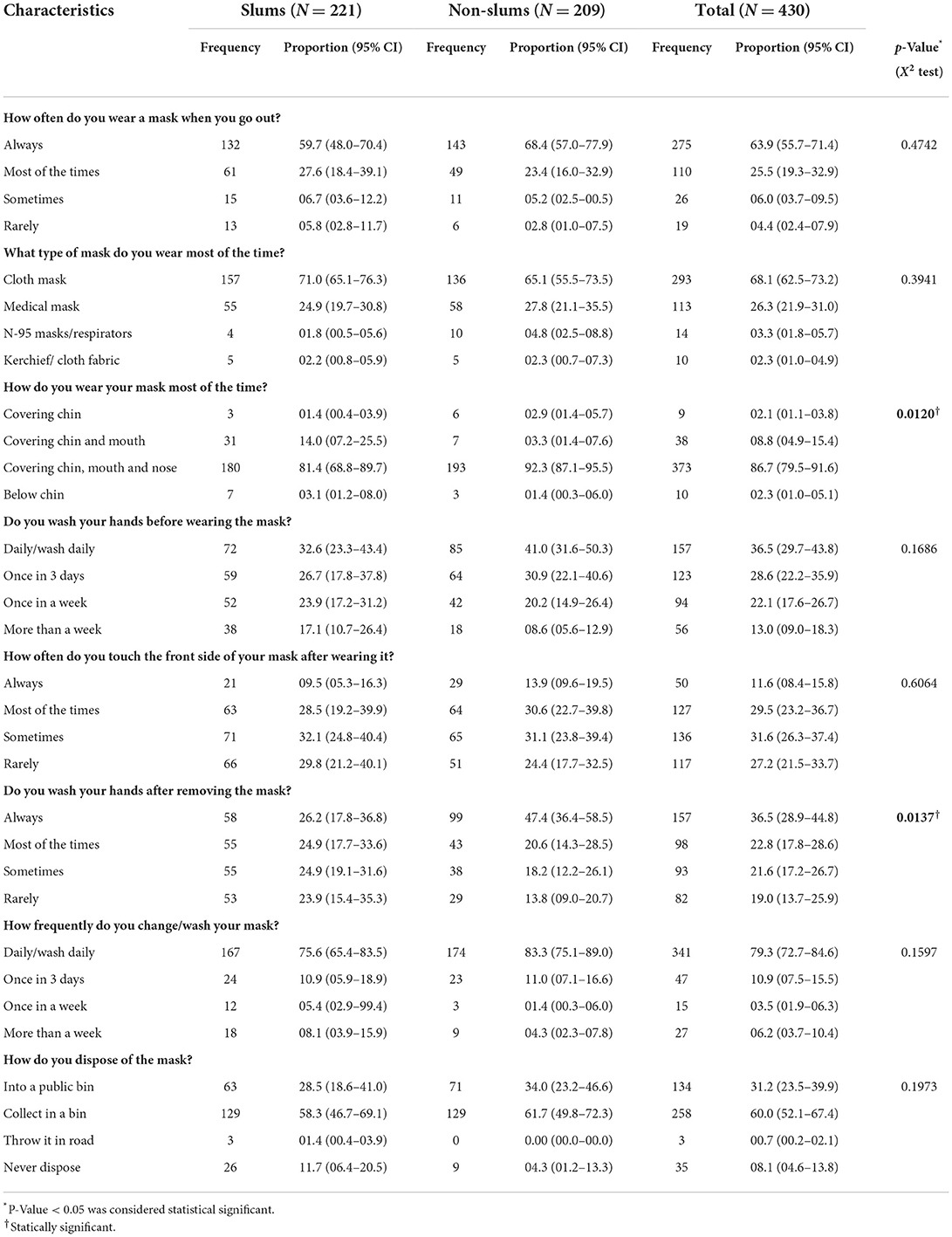
Table 4. Practice of Mask use in Public Places among the slum and non-slum population, Greater Chennai Corporation, India, March 2021 (N = 430).
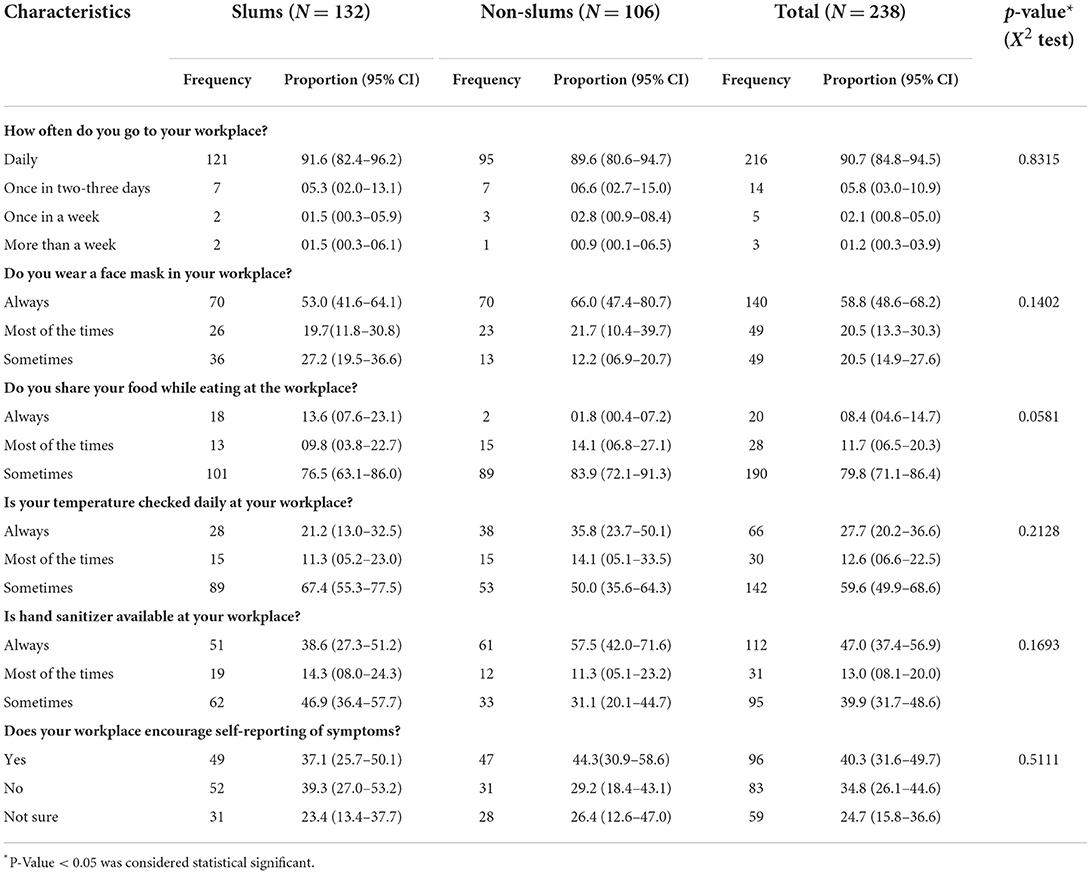
Table 5. Practice of Mask use at Workplaces among the slum and non-slum population, Greater Chennai Corporation, India, March 2021 (N = 238).
Only one-third (34.6%) reported that physical distancing is strictly followed at their workplace (Table 6). A large proportion (59.4%) felt that maintaining physical distancing was difficult in the local context.
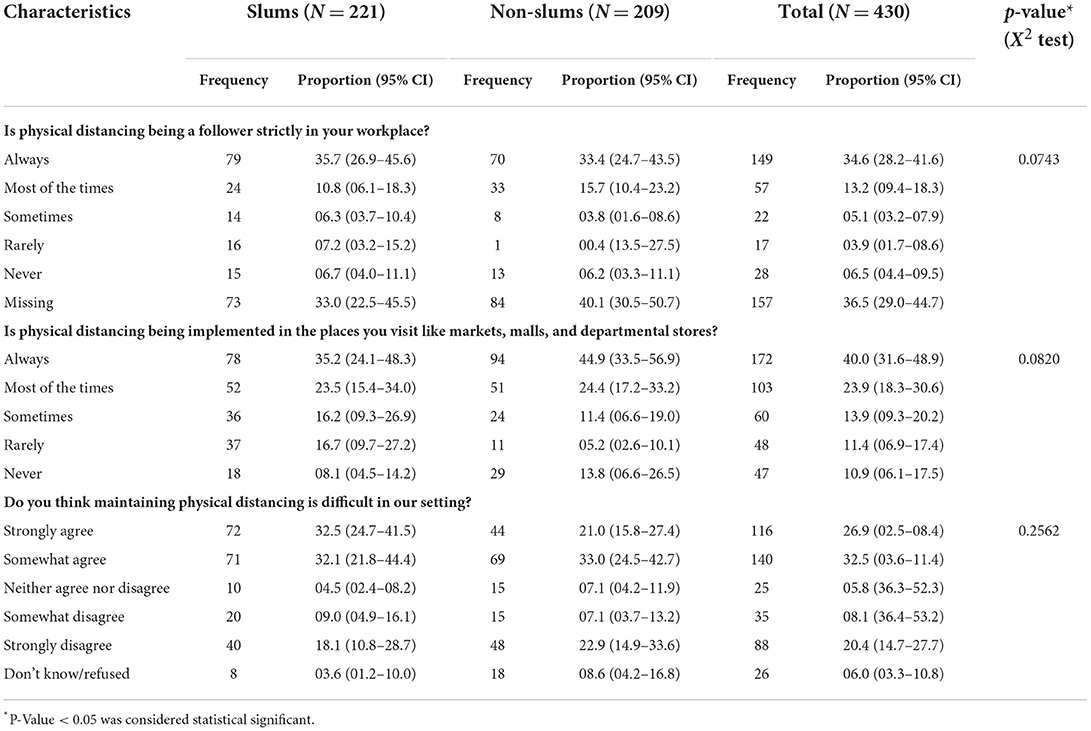
Table 6. Physical distancing practices among the slum and non-slum population, Greater Chennai Corporation, India, March 2021 (N = 430).
Most of the study participants knew that wearing a mask reduced the spread of COVID-19. The knowledge of mask use was higher in the non-slum population (92.3%) compared to the slum (81.4%). However, there was also a negative attitude toward wearing the mask (46.5%). Two-thirds (63.9%; slum: 59.7%; non-slum: 68.4%) of the participants reported consistent use of masks while going out, which was incompatible with our previous three surveys (slum: 28, 29, and 21%; non-slum: 36, 35, and 27%) based on observations in public places (22).
Our findings were consistent with studies from other low and middle-income countries, which reported high awareness about mask use (24, 25). A survey of 1,114 participants in Uganda reported knowledge of protection against COVID-19 by face masks among 86.4%. Another study conducted in Nepal among 381 individuals reported adequate knowledge of face mask use among 95.5% of the participants (24, 25). The knowledge was high in all the study settings, possibly due to frequent mentions of masks used in social media and mass media (26).
The attitude toward mask use was not encouraging, consistent with our previous surveys in the city that reported poor compliance (22). One in two study participants felt that they should not be forced to wear masks because masks interfered with breathing and speaking and caused overheating—a study conducted by Taylor et al. (27). Canada reported a negative attitude toward mask use. The respondents felt wearing a facemask was a hassle, looked ugly and silly, made other people uncomfortable and untrustworthy, and caused breathing difficulty and overheating (27).
We observed a disconnect between knowledge and attitude regarding mask use among the general public. Our study reported two-thirds of the study participants self-reported mask use while going to a public place, but this was not consistent with earlier surveys, which showed only 32% were using masks properly (22). Safe disposal was an important issue of concern with the increasing use of a mask during the pandemic (28). Disposal of the mask using a closed bin or a public bin was followed by more than two-thirds of the participants, according to WHO guidelines (29, 30). Whereas, previous study by Islam et al. in Bangladesh stated that only half of the study participants followed a safe disposal of the used mask (31). Mask use has also been an essential strategy in reducing the spread of infection in the workplace. Though WHO recommends using a mask by everyone at the workplace, only half of our study participants comply with it (32). We recommend strictly enforcing rules on mask use in public and workplaces.
Apart from mask use, physical distancing is an effective way of reducing the spread of infection in the community (1). WHO has recommended maintaining physical distancing in public and workplaces (33). The same is also adapted in India to prevent SARS-CoV-2 infection (34–36). Even from the previous influenza pandemic, several studies supported the social distanceing at workplace to prevent spread of infection (37). However, only one-third of the study participants followed physical distancing at the workplace. This could be possibly due to practical challenges in distancing at markets, workplaces, and slums in our setting. Therefore, masks will be more important in crowded cities, especially where many people come together in closed spaces.
This major strength of our study was that we surveyed a representative sample of respondents from the slum and non-slum population in a large metropolitan city in India. Hence, the results can be generalized to the slum and non-slum of a meteropolitan city in India. One of the limitations was we could not observe the study participants for mask use. Hence, the reported practice of mask use could be overestimated as it was based on self-reporting by the respondents. Hence, we recommend combining methods, including questionnaire-based surveys and observation-based studies, to understand the mask use. The second limitation was inter-observer variation during the data collection as multiple teams collected data simultaneously. However, we tried to minimize this error through training all the data collectors simultaneously and simulation of the interviews.
We conclude that the community knew the benefits of masks used in a large metropolitan city in India. However, the attitudes and practice were not satisfactory. We suggest continuous reinforcement by spreading awareness and educating on the appropriate use of the mask in the community using mass media. We also suggest addressing the misconceptions related to mask use such as difficulty in breathing, conversation, and overheating. We also recommend strict enforcement of regulations in public places and workplaces to contain the spread of COVID-19 in the community.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Indian Council of Medical Research–National Institute of Epidemiology. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
RN: conceptualization, methodology, data collection, analysis, manuscript writing, and preparation of first draft. PK, PG, and MJ: conceptualization, methodology, and critical review and revision of the manuscript. VV and DH: data management and critical review and revision of the manuscript. KI and MSe: data collection, management of field activities,data analysis, and critical review and revision of the manuscript. SM and MSa: data collection, data analysis, and critical review and revision of the manuscript. MR: methodology, data collection, data analysis, and critical review and revision of the manuscript. PR: conceptualization, data collection, analysis, and preparation of first draft. All authors contributed to the article and approved the submitted version.
This study was funded by the Intra-Mural Fund of ICMR–National Institute of Epidemiology, Chennai, India. The funders had no role in study design, data collection, analysis, publishing decisions, or manuscript preparation.
We acknowledge the field data collectors for dedicating their time to the study's purpose. We also acknowledge the participants in our study for dedicating their time to providing valuable data.
Author MJ was employed by Greater Chennai Corporation. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.938642/full#supplementary-material
1. Talic S, Shah S, Wild H, Gasevic D, Maharaj A, Ademi Z, et al. Effectiveness of public health measures in reducing the incidence of covid-19, SARS-CoV-2 transmission, and covid-19 mortality: Systematic review and meta-analysis. BMJ. (2021) 375:1–15. doi: 10.1136/bmj-2021-068302
2. Abaluck J, Kwong LH, Styczynski A, Haque A, Kabir MA, Bates-Jefferys E, et al. Impact of community masking on COVID-19: a cluster-randomized trial in Bangladesh. Science. (2022) 80:375. doi: 10.1126/science.abi9069
3. Payne DC, Smith-Jeffcoat SE, Nowak G, Chukwuma U, Geibe JR, Hawkins RJ, et al. SARS-CoV-2 infections and serologic responses from a sample of U.S. Navy Service Members — USS Theodore Roosevelt, April 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:714–21. doi: 10.15585/mmwr.mm6923e4
4. Wang Y, Tian H, Zhang L, Zhang M, Guo D, Wu W, et al. Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: a cohort study in Beijing, China. BMJ Glob Heal. (2020) 5:e002794. doi: 10.1136/bmjgh-2020-002794
5. Nelson SB, Dugdale CM, Bilinski A, Cosar D, Pollock NR, Ciaranello A. Prevalence and risk factors for in-school transmission of SARS-CoV-2 in Massachusetts K-12 public schools, 2020-2021. medRxiv. (2021) 21263900. doi: 10.1101/2021.09.22.21263900
6. Doung-ngern P, Suphanchaimat R, Panjangampatthana A, Janekrongtham C, Ruampoom D, Daochaeng N, et al. Case-control study of use of personal protective measures and risk for SARS-CoV 2 infection, Thailand. Emerg Infect Dis. (2020) 26:2607–16. doi: 10.3201/eid2611.203003
7. Jehn M, McCullough J Mac, Dale AP, Gue M, Eller B, Cullen T, et al. Association between K−12 school mask policies and school-associated COVID-19 outbreaks — maricopa and pima counties, Arizona, July–August 2021. MMWR Morb Mortal Wkly Rep. (2021) 70:1372–3. doi: 10.15585/mmwr.mm7039e1
8. Freedman DO, Wilder-Smith A. In-flight transmission of SARS-CoV-2: a review of the attack rates and available data on the efficacy of face masks. J Travel Med. (2020) 27:taaa178. doi: 10.1093/jtm/taaa178
9. World Health Organization. Advice on the Use of Masks in the Context of COVID-19: Interim Guidance. Geneva: World Health Organization (2020).
10. Center for Diseases Prevention and control. Coronavirus Disease 2019 (COVID-19). Atlanta, GA: Center for Diseases Prevention and Control (2020).
11. Governmnet of India. Ministry of Health and Family Welfare. Novel Coronavirus Disease COVID-19: Guidelines on Use of Masks by Public. New Delhi: Ministry of Health and Family Welfare (2020).
12. Martinelli L, Kopilaš V, Vidmar M, Heavin C, Machado H, Todorović Z, et al. Face masks during the COVID-19 pandemic: a simple protection tool with many meanings. Front Public Heal. (2021) 13:8. doi: 10.3389/fpubh.2020.606635
13. Howard J, Huang A, Li Z, Tufekci Z, Zdimal V, van der Westhuizen H-M, et al. An evidence review of face masks against COVID-19. Proc Natl Acad Sci. (2021) 118:e2014564118. doi: 10.1073/pnas.2014564118
14. Johansson MA, Quandelacy TM, Kada S, Prasad PV, Steele M, Brooks JT, et al. SARS-CoV-2 transmission from people without COVID-19 symptoms. JAMA Netw Open. (2021) 4:e2035057. doi: 10.1001/jamanetworkopen.2020.35057
15. Feng S, Shen C, Xia N, Song W, Fan M, Cowling BJ. Rational use of face masks in the COVID-19 pandemic. Lancet Respir Med. (2020) 8:434–6. doi: 10.1016/S2213-2600(20)30134-X
16. Chiu N-C, Chi H, Tai Y-L, Peng C-C, Tseng C-Y, Chen C-C, et al. Impact of wearing masks, hand hygiene, and social distancing on influenza, enterovirus, and all-cause pneumonia during the coronavirus pandemic: retrospective national epidemiological surveillance study. J Med Internet Res. (2020) 22:e21257. doi: 10.2196/21257
17. Tajvar A, Aghamolaei T, Mohseni S, Fakherpour A, Damiri Z, Jahangiri M, et al. Knowledge, performance, and attitude towards mask use to prevent and control COVID-19 outbreak among a group of iranian people: a cross-sectional study. Shiraz E Med J. (2021) 22:e111491. doi: 10.5812/semj.111491
18. Pramana C, Kurniasari L, Santoso B, Afrianty I, Syahputra A. Knowledge, attitudes, and practices of using masks by the community during the Covid-19 pandemic in Indonesia. PalArch”s J Archael Egypt/Egyptol. (2020) 17:4800–8. Available online at: https://archives.palarch.nl/index.php/jae/article/view/4673
19. Azlan AA, Hamzah MR, Sern TJ, Ayub SH, Mohamad E. Public knowledge, attitudes and practices towards COVID-19: a cross-sectional study in Malaysia. PLoS ONE. (2020) 15:1–15. doi: 10.1101/2020.04.29.20085563
20. Tan M, Wang Y, Luo L, Hu J. How the public used face masks in China during the coronavirus disease pandemic: a survey study. Int J Nurs Stud. (2021) 115:103853. doi: 10.1016/j.ijnurstu.2020.103853
21. Jones NR, Qureshi ZU, Temple RJ, Larwood JPJ, Greenhalgh T BL. Two metres or one: what is the evidence for physical distancing in covid-19? BMJ. (2020) 370:m3223. doi: 10.1136/bmj.m3223
22. Jagadeesan M, Rubeshkumar P, Raju M, Sakthivel M, Murali S, Nagarajan R, et al. Surveillance for face mask compliance, Chennai, Tamil Nadu, India, October- December, 2020. PLoS ONE. (2021) 16:1–10. doi: 10.1371/journal.pone.0257739
23. Resolve To Save Lives. Promoting Mask-Wearing During the COVID-19 Pandemic: A POLICYMAKER'S GUIDE 2020. Available online at: https://preventepidemics.org/wp-content/uploads/2020/08/Promoting-Mask-Wearing-During-COVID-19.pdf (accessed June 10, 2022).
24. Sikakulya FK, Ssebuufu R, Mambo SB, Pius T, Kabanyoro A, Kamahoro E, et al. Use of face masks to limit the spread of the COVID-19 among western Ugandans: Knowledge, attitude and practices. PLoS ONE. (2021) 16:1–13. doi: 10.1371/journal.pone.0248706
25. Alam K, Palaian S, Shankar PR, Jha N. General public's knowledge and practices on face mask use during the COVID-19 pandemic: a cross-sectional exploratory survey from Dharan, Nepal. F1000Res. (2021) 10:376. doi: 10.12688/f1000research.52661.1
26. Ahmed W, Vidal-Alaball J, Lopez Segui F, Moreno-Sánchez PA. A social network analysis of tweets related to masks during the COVID-19 pandemic. Int J Environ Res Public Health. (2020) 17:8235. doi: 10.3390/ijerph17218235
27. Taylor S, Asmundson GJG. Negative attitudes about facemasks during the COVID-19 pandemic: the dual importance of perceived ineffectiveness and psychological reactance. PLoS ONE. (2021) 16:1–15. doi: 10.1371/journal.pone.0246317
28. Sangkham S. Face mask and medical waste disposal during the novel COVID-19 pandemic in Asia. Case Stud Chem Environ Eng. (2020) 2:100052. doi: 10.1016/j.cscee.2020.100052
29. Shiferie F. Improper disposal of face masks during COVID-19: unheeded public health threat. Pan Afr Med J. (2021) 38:366. doi: 10.11604/pamj.2021.38.366.29063
30. World Health Organization. How to Put on, Use, Take Off and Dispose of a Mask. Geneva: World Health Organization (2020).
31. Islam SMD-U, Safiq MB, Bodrud-Doza M, Mamun MA. Perception and attitudes toward PPE-related waste disposal Amid COVID-19 in Bangladesh: an exploratory study. Front Public Heal. (2020) 13:8. doi: 10.3389/fpubh.2020.592345
32. World Health Organization. Mask Use in the Context of COVID-19. Geneva: World Health Organization (2020).
33. World Health Organization. COVID-19: Physical Distancing. Geneva: World Health Organization (2022).
34. Government of India. Ministry of Health and Family Welfare. SOP on Preventive Measures to Contain Spread of COVID-19 in Offices. New Delhi: Ministry of Health and Family Welfare (2021).
35. Government of India. Ministry of Health and Family Welfare. SOP on Preventive Measures to be Followed in Entertainment Parks and Similar Places to Contain Spread of COVID-19. New Delhi: Government of India. Ministry of Health and Family Welfare (2021).
36. Government of India. Ministry of Health and Family Welfare. An Illustrated Guide on COVID Appropriate Behaviour. New Delhi: Ministry of Health and Family Welfare (2020).
Keywords: masks, COVID-19, compliance, public place, knowledge
Citation: Nagarajan R, Rubeshkumar P, Jagadeesan M, Raju M, Sakthivel M, Murali S, Sendhilkumar M, Ilangovan K, Harikrishnan D, Venkatasamy V, Ganeshkumar P and Kaur P (2022) Knowledge, attitude, and practice towards face mask use among residents of Greater Chennai Corporation, India, March 2021. Front. Public Health 10:938642. doi: 10.3389/fpubh.2022.938642
Received: 07 May 2022; Accepted: 06 July 2022;
Published: 28 July 2022.
Edited by:
Chuhan Wu, Tsinghua University, ChinaCopyright © 2022 Nagarajan, Rubeshkumar, Jagadeesan, Raju, Sakthivel, Murali, Sendhilkumar, Ilangovan, Harikrishnan, Venkatasamy, Ganeshkumar and Kaur. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Prabhdeep Kaur, a3ByYWJoZGVlcEBuaWVpY21yLm9yZy5pbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.