- 1Department of Emergency, Affiliated Hospital of North Sichuan Medical College, Nanchong, China
- 2Disinfection Supply Center, The Second Affiliated Hospital of Chongqing Medical University, Chongqing, China
Introduction: Needle-stick injuries (NSI) are a serious threat to the health of healthcare workers, nurses, and nursing students, as they can expose them to infectious diseases. Different prevalence rates have been reported for this type of injury in different studies worldwide. Therefore, this study aimedto estimate the pooled prevalence of NSI among nursing students.
Methods: This study was conducted by searching for articles in Web of Science, PubMed, Scopus, Embase, and Google Scholar without time limitation using the following keywords: needle-stick, needle stick, sharp injury, and nursing student. The data were analyzed using the meta-analysis method and random-effects model. The quality of the articles was evaluated with Newcastle-Ottawa Quality Assessment Scale (NOS). The heterogeneity of the studies was examined using the I2 index, and the collected data were analyzed using the STATA Software Version 16.
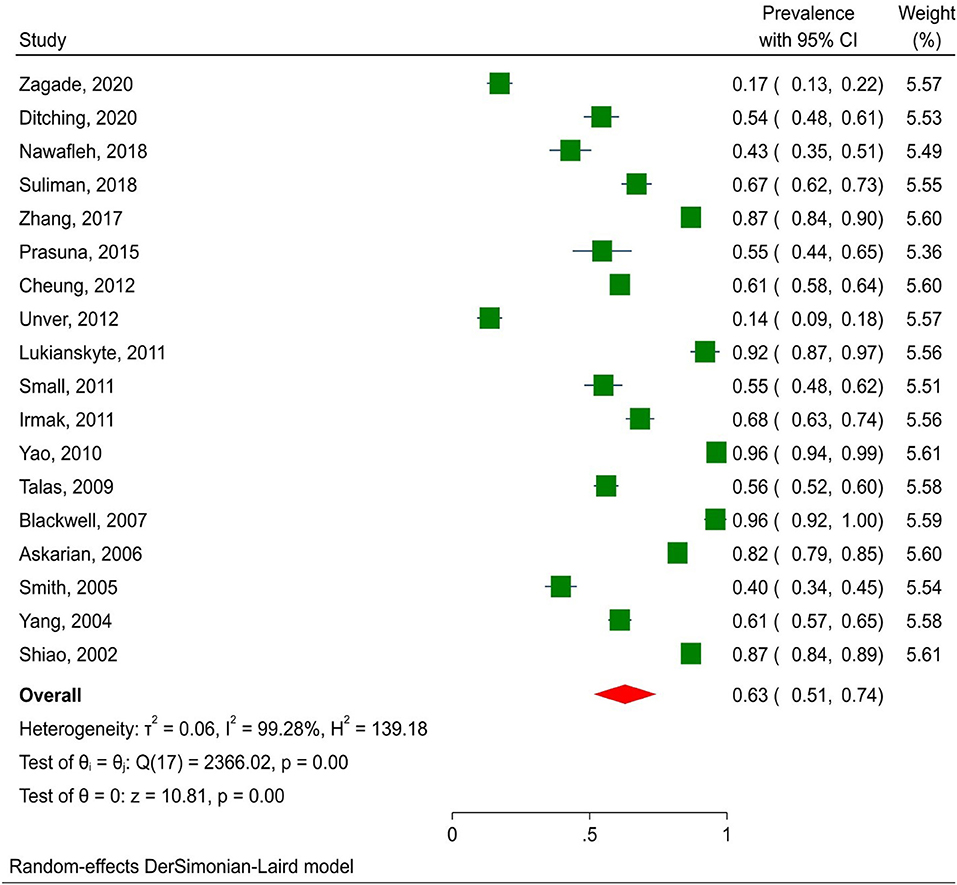
Results: Initially, 1,134 articles were retrieved, of which 32 qualified articles were included in the analysis. Nursing students reported 35% of NSI (95% CI: 28–43%) and 63% (95% CI: 51–74%) did not report their needle-stick injuries. The highest prevalence was related to studies conducted in Asia (39.7%; 95% CI: 31.7–47.7%). There was no significant correlation among NSI prevalence and age of samples, and article year of publication.
Conclusion: A third of nursing students reported experiencing NSI. Consequently, occupational hazard prevention training and student support measures need to be considered.
Introduction
An injury caused by a needle or a sharp object is known as a needle-stick injury (NSI). The injury is usually not serious, so this does not pose a serious risk, but it may pose problems if the needle is contaminated with blood or other body fluids (1). The risk of a single exposure to virus-infected blood for hepatitis B, hepatitis C, and Human Immunodeficiency Virus (HIV) is 6–30%, B, 0–7%, and 0.2–0.5%, respectively (2). Around 80,000 infections per year were estimated to occur in healthcare staff globally in 2,000 due to lack of intervention to prevent NSI (3). Health care staff were estimated to contract 80,000 infections per year as a result of NSIs not being prevented in 2000 (4, 5). Healthcare workers can suffer mental distress, anxiety, depression, and post-traumatic stress disorder due to NSI, leading to more work absences and lost workdays (3, 5–8). These injuries are more common in nurses and nursing students than in other healthcare workers (9, 10). The majority of nursing students' training takes place in clinical settings, where they learn various nursing skills, including injection techniques, taking blood samples, and monitoring blood sugar levels using glucometers under the supervision of instructors. However, these nurses more vulnerable to NSI than experienced nurses due to inadequate knowledge and experience in terms of handling needles and sharp objects in a clinical setting (11).
Many studies have investigated NSI among health professionals, but students have often been neglected. Thus, NSI prevalence should be investigated among students. A recent systematic review and meta-analysis focused only on nursing interns, and few studies (eight papers) were retrieved and analyzed due to the limitation in the target population and searched databases (12). In addition, it is impossible to put them all in one group and estimate the pooled prevalence of NSI because the nature of the nursing students' work is different from that of students in other medical fields. Therefore, this study focused on nursing students. Previous studies worldwide have estimated the prevalence of NSI in nursing students and reported different results. Based on the literature review, the prevalence of NSI among nursing students has varied between 8.7 and 71% (13, 14). Our first step in preventing this problem is to gain an understanding of its exact prevalence. Therefore, this study aimedto estimate the pooled prevalence of NSI in nursing students all over the world.
Methods
Search strategy
The present systematic review and meta-analysis were conducted according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The search was conducted in databases of Web of Science, PubMed, Scopus, and Google Scholar without time limitation using the following keywords: needle-stick, needle stick, sharp injury, nursing student, and their possible combinations. The discussion section and reference list of each article was reviewed for more access to articles. The search strategy in the PubMed database was as follows: (“Needlestick Injuries” [Mesh] OR “Needle?stick Injur*”[tiab] OR “Needle?stick*”[tiab] OR “Sharps Injur*”[tiab]) AND (“Students, Nursing”[Mesh] OR “Nursing Student*”[tiab] OR “Pupil Nurse*”[tiab] OR “Nursing Staff*”[tiab]).
Study selection and data extraction
The study included all observational studies published in English that examined NSI among nursing students. Nursing students' data were analyzed when available for studies conducted on diverse groups of healthcare workers; otherwise, they were excluded from the analysis. In addition, interventional, review, and qualitative studies, as well as editor letters, and conference papers were excluded. Two independent authors selected eligible articles by reviewing their titles and abstracts. Article information, including first author, publication year, the mean age of samples, sample size, place of study, number of students with NSI, and number of students not reporting their injury, was extracted. Disagreements between the authors were resolved through discussion.
Quality assessment
Methodological quality was evaluated for the selected articles to minimize bias. For this purpose, the Newcastle-Ottawa Quality Assessment Scale (NOS) was used to evaluate each study using six items in three groups, including selection, exposure, and comparability with the maximum score as much as 9. The opinion of the corresponding author was applied in case of disagreement in scoring the selected articles (15).
Data analysis
Heterogeneity across studies was examined using Cochran's Q test (p < 0.1) and I2 statistics. According to I2 statistic, heterogeneity was divided into three categories of below 25% (low heterogeneity), between 25 and 75% (medium heterogeneity), and over 75% (high heterogeneity) (16). The random effects model was used to estimate the pooled prevalence of NSI with a 95% confidence interval. The pooled prevalence of NSI was estimated using the random effects model due to a high heterogeneity across the studies, and the heterogeneity was 99.10%. This type of meta-analysis is limited by high heterogeneity, which is inevitable in meta-analyses that aim to estimate pooled prevalence (17). The subgroup analysis was performed by continent (Asia, Europe, and others) and work time (NSI prevalence in the last year, NSI prevalence during the internship, and unknown) to identify potential sources of heterogeneity. NSI prevalence was examined using univariate meta-regression analysis based on the mean age of samples and the year of publication of the article. Publication error was visually analyzed by examining funnel plots using Egger's method. Statistically significant results were only included in the analysis because publication bias was present, and negative or non-significant results were excluded because they had not been published (18). All the statistical analyses were performed using Stata Software, Version 16.
Results
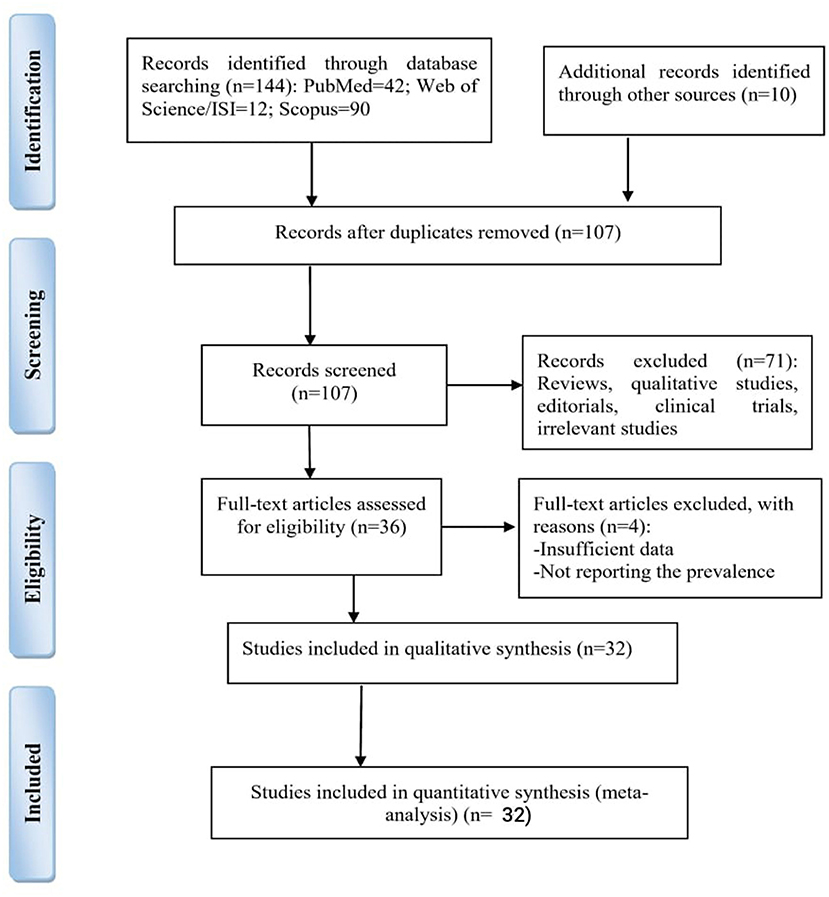
A total of 1,134 articles were found in the initial search, of which 516 duplicate articles were excluded. In the next step, the titles and abstracts of the remaining articles (n = 618) were reviewed, and the qualified articles were included in the analysis based on the inclusion criteria (Figure 1).
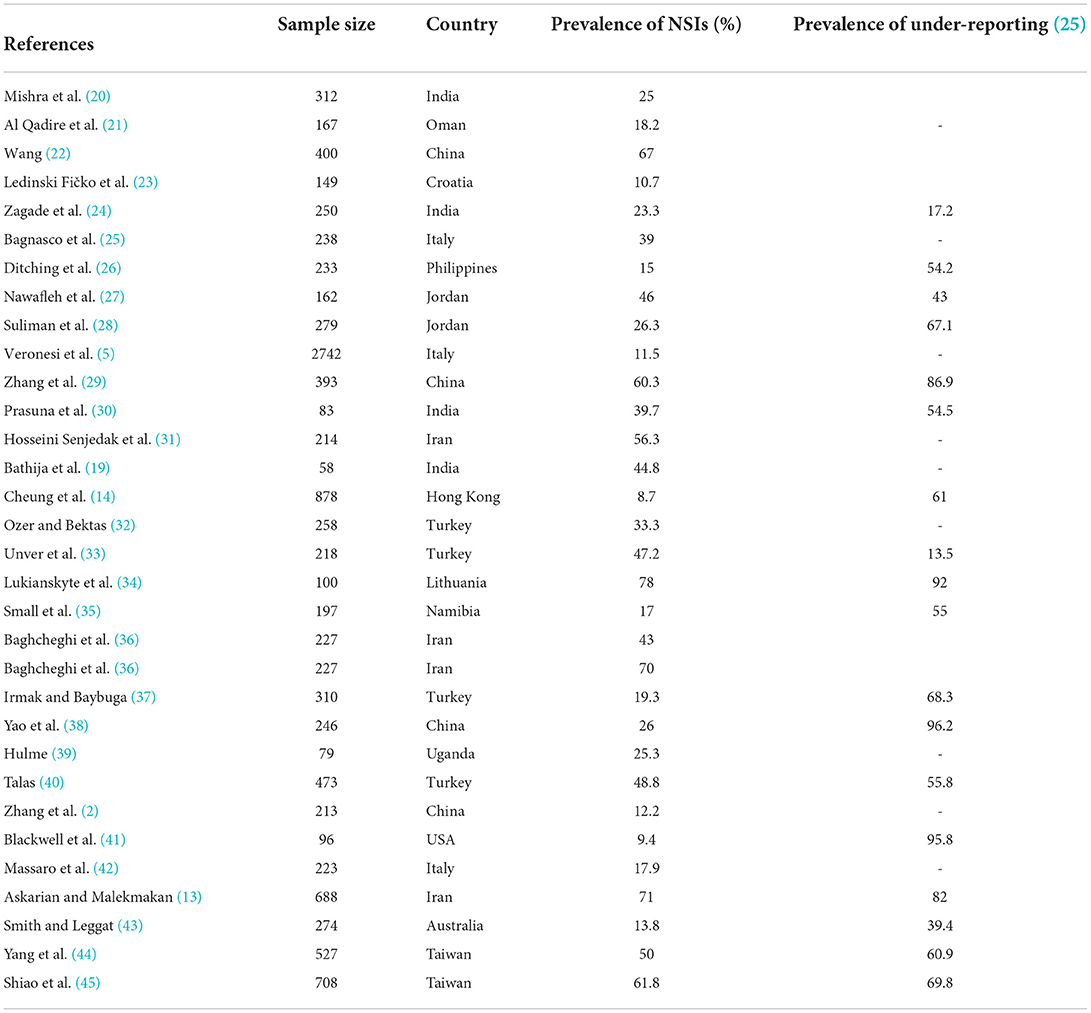
A total of 32 studies with a sample size of 11,622 were included in the analysis. There were 13 studies that did not report NSI. Most studies were conducted in Turkey, China, Iran, and India (every four studies), respectively. The large stand lowest sample sizes were related to Veronesi et al. (5) (n = 2,742) and Bathija et al. (19) (n = 58), respectively (Table 1).
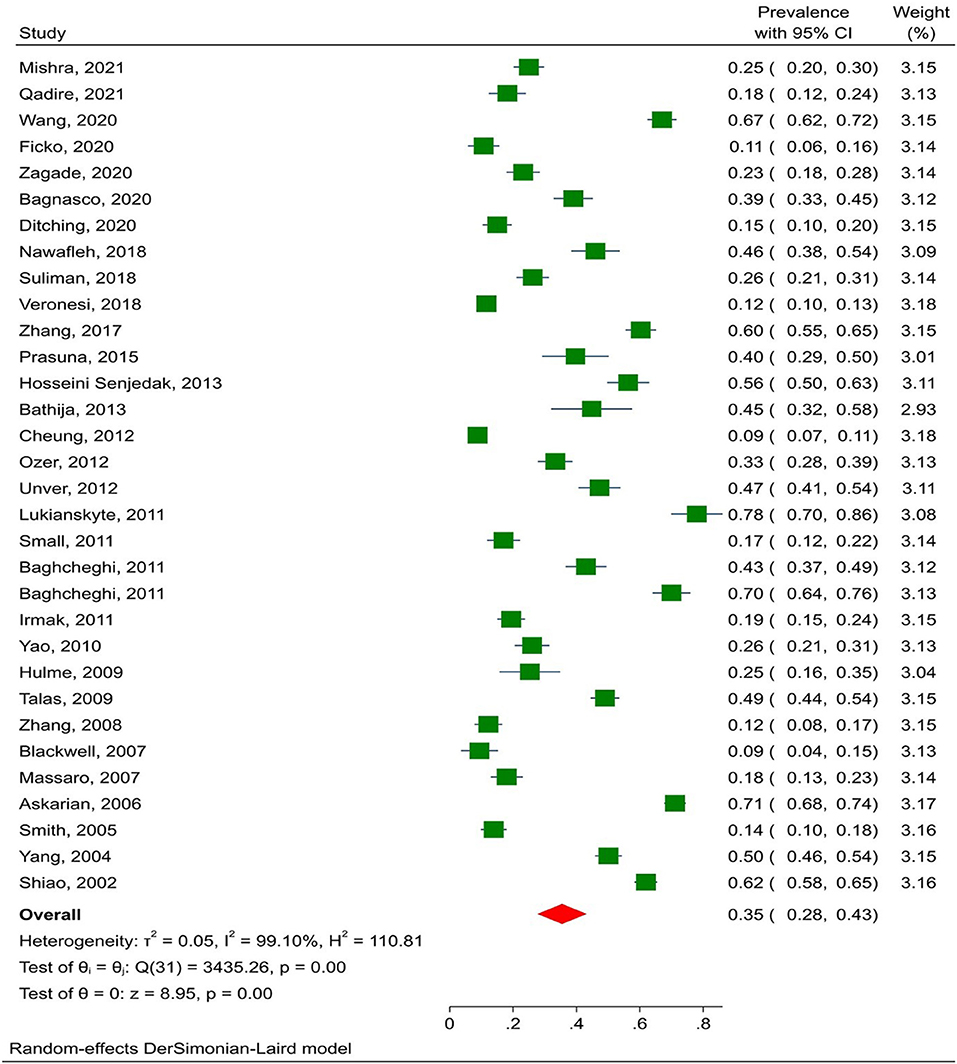
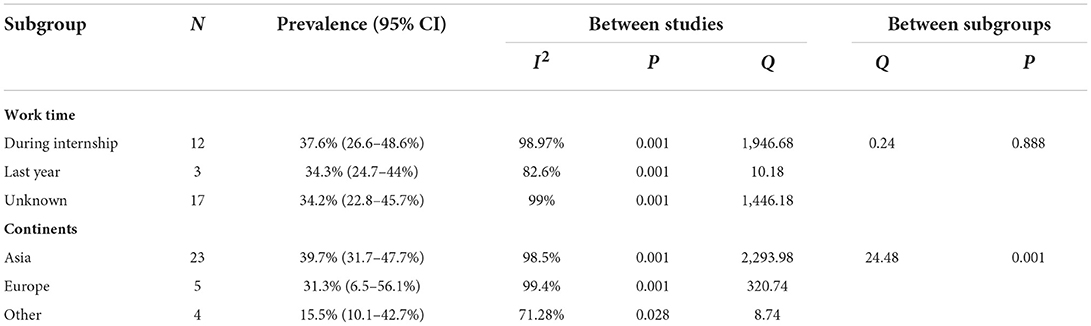
The prevalence of NSI among nursing students was assessed for publication bias to ensure that all relevant studies were included in the analysis. The results showed that publication bias was significant (p = 0.169), and the pooled prevalence of NSI in nursing students was 35% (95% CI: 28–43%) (I2 = 98.9%, p = 0.001) (Figure 2). In addition, the subgroup analysis by continent and injury time showed that the highest prevalence rates of NSI were related to Asia (39.7% with 95% CI: 31.7–47.7%) and internship period (37.6%; 95% CI: 26.6–48.6%). In some studies, the injury time was not specified, and the injury time was broken down into last year or the internship period. The prevalence of NSI was higher in the internship period than in other periods (p = 0.888; Table 2). Meta-regression analysis found no relationship between NSI prevalence and article publication year, sample size, or mean age of students.
According to the results, the prevalence of not-reported NSI among nursing students was 63% (95% CI: 51–74%) (Figure 3). Asian studies reported NSIs at a lower rate than those on other continents (60.7% vs. 63.5%, p < 0.01). Furthermore, the frequency of non-reporting of injury was 56.4% during internship and 69.4% in other periods (p = 0.256). There was no significant correlation between NSI prevalence, age, and publication year of articles.
Discussion
This study aimed to estimate the pooled prevalence of NSI in nursing students worldwide. The results showed that 35% of nursing students had experienced NSI. Bouya et al. (46) analyzed 11 studies and found a prevalence rate of 45.3% for NSI among nursing students, which was a higher prevalence rate than in the present study. The studies were conducted during different periods, which can explain the difference. The results of another meta-analysis in China showed that the prevalence of NSI in nursing students was 33%, which is consistent with those of the present study (47). A recent systematic review and meta-analysis investigated occupational injuries among nursing interns and found that the prevalence of NSI in this group was 27%, which is lower than the present study (12). The previous systematic review and meta-analysis analyzed eight studies, two of which were semi-experimental. Bringing these studies together with observational studies to estimate the pooled prevalence is methodologically incorrect because the nature of these studies is different. There were also three studies performed on medical students (not nursing students) and one retrospective study. The remaining two studies were included in our analysis. In addition, Scopus (the world's largest database) and Web of Science/ISI were not searched. The present study resolved the limitations mentioned above, and covered the NSI in all nursing students by searching all four primary databases (without a time limit).
The literature review indicated that most previous studies were focused on the prevalence of NSI in healthcare professionals, and examining this problem in nursing students had primarily been ignored by previous studies. Infectious diseases such as hepatitis and AIDS can be spread through NSI in students, preventing them from obtaining future employment opportunities. A previous study showed that half of the healthcare workers had an NSI during their work time, and one-third had it the previous year (48). Nursing students appear more vulnerable to NSI than healthcare professionals due to inadequate knowledge and experience.
The study results related to the continent revealed that the prevalence of NSI among nursing students was higher in Asia than in other continents. Bouya et al. (46) found that the highest prevalence rates had been reported in the studies conducted in Asian countries regarding exploring the prevalence of NSI in healthcare professionals. Although different prevalence rates of NSI are reported in different regions, the high prevalence of this problem in Asian countries may be related to different study designs, sample sizes, and national and local prevention policies.
This study showed that 62.9% of nursing students suffering from NSI did not report their injuries. Students deprive themselves of timely medical examination and receiving prophylaxis and examination of early changes in serum antibodies immediately after exposure by not reporting their NSI (49), which may transmit the potential viruses to their family members (50, 51). Not reporting NSI is a significant clinical challenge that may have undermined the validity of the existing data regarding this problem (52). Some of the most important reasons for not reporting NSI include stigma, lack of awareness (53), negative career consequences, shame (54), fear of being blamed, fear of creating more problems (55), thinking that NSI is none of others' business, and believing that reporting the injury would not be helpful (56).
Overall, the study results indicated that NSI is widespread among nursing students and that most do not report their injuries. NSI and its negative consequences can be reduced by holding workshops regarding workplace safety, providing more support for nursing students in clinical settings, and encouraging students to report their injuries.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
Concept and design: XX and FW. Acquisition, analysis, or interpretation of data: YY. Drafting of the manuscript: YY and XX. Critical revision of the manuscript for important intellectual content: HW. Statistical analysis: FW. All authors gave their final approval of this version of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
HBV, Hepatitis B Virus; HCV, Hepatitis B Virus; HIV, Human Immunodeficiency Virus; NOS, Newcastle-Ottawa Scale; NSI, Needle-Stick Injury; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
References
1. Rais N, Jamil HM. Prevalence of needle stick injuries among health care providers. Int J Endorsing Health Sci Res. (2013) 1:73–9. doi: 10.29052/IJEHSR.v1.i2.2013.73-79
2. Zhang Z, Moji K, Cai G, Ikemoto J, Kuroiwa C. Risk of sharps exposure among health science students in northeast China. Biosci Trends. (2008)2:105–11.
3. Mannocci A, De Carli G, Di Bari V, Saulle R, Unim B, Nicolotti N, et al. How much do needlestick injuries cost? A systematic review of the economic evaluations of needlestick and sharps injuries among healthcare personnel. Infect Control Hosp Epidomol. (2016) 37:635–46. doi: 10.1017/ice.2016.48
4. Rapiti E, Pruss-Ustun A, Hutin YJ. Sharps Injuries: Assessing the Burden of Disease From Sharps Injuries to Health-Care Workers at National Local Levels. Geneva (2005). Available online at: https://www.who.int/publications/i/item/sharps-injuries-assessing-the-burden-of-disease-from-sharps-injuries-to-health-care-workers-at-national-and-local-levels
5. Veronesi L, Giudice L, Agodi A, Arrigoni C, Baldovin T, Barchitta M, et al. A multicentre study on epidemiology and prevention of needle stick injuries among students of nursing schools. Annali di igiene: medicina preventiva e di comunita. (2018) 30(Suppl. 2):99–110. doi: 10.7416/ai.2018.2254
6. Green B, Griffiths E. Psychiatric consequences of needlestick injury. Occup Med. (2013) 63:183–8. doi: 10.1093/occmed/kqt006
7. Jeong JS, Son HM, Jeong IS, Son JS, Shin K-s, Yoonchang SW, et al. Qualitative content analysis of psychologic discomfort and coping process after needlestick injuries among health care workers. Am J Infect Control. (2016) 44:183–8. doi: 10.1016/j.ajic.2015.09.002
8. Oh HS, Chang SWY, Choi JS, Park ES, Jin HY. Costs of postexposure management of occupational sharps injuries in health care workers in the Republic of Korea. Am J Infect Control. (2013) 41:61–5. doi: 10.1016/j.ajic.2012.01.030
9. Puro V, De Carli G, Di Bari V. Il panorama epidemiologico nazionale e applicazione della direttiva europea 2010/32/UE. Studio Italiano sul Rischio Occupazionale da HIV Servizio di Epidemiologia dell'Istituto Nazionale per le Malattie Infettive “L Spallanzani” Servizio sanitario regionale Emilia-Romagna Bologna. Istituto Nazionale per le Malattie Infettive Lazzaro Spallanzani ROMA (2014). p. 27.
10. Schmid K, Schwager C, Drexler H. Needlestick injuries and other occupational exposures to body fluids amongst employees and medical students of a German university: incidence and follow-up. J Hosp Infect. (2007) 65:124–30. doi: 10.1016/j.jhin.2006.10.002
11. Kebede A, Gerensea H. Prevalence of needle stick injury and its associated factors among nurses working in public hospitals of Dessie town, Northeast Ethiopia, 2016. BMC Res Notes. (2018) 11:143. doi: 10.1186/s13104-018-3529-9
12. Chen M, Zhang L. Prevalence of needlestick injuries among nursing interns: a systematic review and meta-analysis. Ann Palliat Med. (2021) 10:7525–33. doi: 10.21037/apm-21-703
13. Askarian M, Malekmakan L. The prevalence of needle stick injuries in medical, dental, nursing and midwifery students at the University Teaching Hospitals of Shiraz, Iran. Indian J Med Sci. (2006) 60:227–32. doi: 10.4103/0019-5359.25904
14. Cheung K, Ching SSY, Chang KKP, Ho SC. Prevalence of and risk factors for needlestick and sharps injuries among nursing students in Hong Kong. Am J Infect Control. (2012) 40:997–1001. doi: 10.1016/j.ajic.2012.01.023
15. Luchini C SB, Solmi M, Veronese N. Assessing the quality of studies in meta-analyses: advantages and limitations of the Newcastle Ottawa Scale. World J Meta-Anal. (2017) 5:80–4. doi: 10.13105/wjma.v5.i4.80
16. Ades A, Lu G, Higgins J. The interpretation of random-effects meta-analysis in decision models. Med Dec Making. (2005) 25:646–54. doi: 10.1177/0272989X05282643
17. Imrey PB. Limitations of meta-analyses of studies with high heterogeneity. JAMA Network Open. (2020) 3:e1919325-e. doi: 10.1001/jamanetworkopen.2019.19325
18. Nair AS. Publication bias-Importance of studies with negative results! Indian J Anaesth. (2019) 63:505. doi: 10.4103/ija.IJA_142_19
19. Bathija GV, Bant DD, Itagimath SR. A study on prevalence of needle stick injuries among junior doctors and nursing students in Kims, Hubli. Indian J Public Health Res Dev. (2013) 4:84–8. doi: 10.5958/j.0976-5506.4.2.019
20. Mishra R, Sharma SK, Gupta PK, Gupta P, Kalyani CV. Occupational health cognizance: needle stick injuries among student nurses. Int J Africa Nurs Sci. (2021) 15:100370. doi: 10.1016/j.ijans.2021.100370
21. Al Qadire M, Ballad CAC, Al Omari O, Aldiabat KM, Shindi YA, Khalaf A. Prevalence, student nurses' knowledge and practices of needle stick injuries during clinical training: a cross-sectional survey. BMC Nurs. (2021) 20:187. doi: 10.1186/s12912-021-00711-2
22. Wang D, Anuwatnonthakate A, Nilvarangkul K. Knowledge attitude and practice regarding prevention of needle stick injuries among nursing students in Henan province, China. J Pak Med Assoc. (2021) 71:2420–2. doi: 10.47391/JPMA.03-429
23. Ledinski Fičko S, Mlinar M, Hošnjak AM, Smrekar M, Kurtović B, Babić J. Nursing student's knowledge about understanding and prevention of needle stick injury. Croatian Nurs J. (2020) 4:73–80. doi: 10.24141/2/4/1/6
24. Zagade H, Nilesh K, Zagade T, Vande AV. Study to evaluate prevalence, knowledge and awareness of needle stick injury among dental and nursing: under graduate students. Indian J Public Health Res. (2020) 11:194784. doi: 10.37506/v11/i2/2020/ijphrd/194784
25. Bagnasco A, Zanini M, Catania G, Watson R, Hayter M, Dasso N, et al. Predicting needlestick and sharps injuries in nursing students: development of the SNNIP scale. Nursing Open. (2020) 7:1578–87. doi: 10.1002/nop2.540
26. Ditching NA, Furatero AGF, Iquiña RVS, Sabulao ADM, Supremo JM, Oducado RMF. factors associated with nursing students' intention to report needlestick injuries: applying the theory of planned behavior. Nurse Media J Nurs. (2020) 10:234–43. doi: 10.14710/nmjn.v10i3.31975
27. Nawafleh HA, El Abozead S, Mohamed FR, Ahmed AM, Altaif KI. Muhbes FJJHSJ. The incidence and circumstances of needle sticks injury (NSI) among Arab nurses students: comparative study. Health Sci. J. (2019) 13:1–6. doi: 10.21767/1791-809X.1000649
28. Suliman M, Al Qadire M, Alazzam M, Aloush S, Alsaraireh A, Alsaraireh FA. Students nurses' knowledge and prevalence of Needle Stick Injury in Jordan. Nurse Educ Today. (2018) 60:23–7. doi: 10.1016/j.nedt.2017.09.015
29. Zhang XJ, Chen Y, Li Y, Hu J, Zhang C, Li Z, et al. Needlestick and sharps injuries among nursing students in Nanjing, China. Workplace Health Saf. (2018) 66:276–84. doi: 10.1177/2165079917732799
30. Prasuna J, Sharma R, Bhatt A, Arazoo Painuly D, Butola H, et al. Occurrence and knowledge about needle stick injury in nursing students. J Ayub Med Coll Abbottabad JAMC. (2015) 27:430–3.
31. Hosseini senjedak SM, Fani Makki O, Vagharseyyedin S. Prevalence of needle stick injuries and some related factors among the nursing students. J Health Care. (2013) 15:30–8.
32. Ozer ZC, Bektas HA. Needlestick injuries during education period in nursing students in Turkey. In: Baskan GA, Ozdamli F, Kanbul S, Ozcan D, editors. 4th World Conference on Educational Sciences. Procedia Social and Behavioral Sciences 462012. p. 3798-801.
33. Unver V, Tastan S, Coskun H. The frequency and causes of occupational injuries among nursing students in Turkey. Arch Environ Occup Health. (2012) 67:72–7. doi: 10.1080/19338244.2011.573024
34. Lukianskyte R, Gataeva J, Radziunaite L. Needle sticks and sharps injuries experienced by staff nurses and nursing students and their prevention. Int J Infect Control. (2012) 8:12. doi: 10.3396/ijic.v8i1.002.12
35. Small L, Pretorius L, Walters A, Ackerman MJ. A surveillance of needle-stick injuries amongst student nurses at the University of Namibia. Health SA Gesondheid. (2011) 16:1–8. doi: 10.4102/hsag.v16i1.507
36. Baghcheghi N, Koohestani HR, Rezaei K, Seraji A, Abedi AR. Prevalence of needlestick/sharps injuries among nursing students and related factors. Iran Occupational Health. (2011) 7:32–9.
37. Irmak Z, Baybuga MS. Needlestick and sharps injuries among Turkish nursing students: a cross-sectional study. Int J Nurs Pract. (2011) 17:151–7. doi: 10.1111/j.1440-172X.2011.01920.x
38. Yao WX, Yang BA, Yao C, Bai PS, Qian YR, Huang CH, et al. Needlestick injuries among nursing students in China. Nurse Educ Today. (2010) 30:435–7. doi: 10.1016/j.nedt.2009.09.018
39. Hulme P. Incidence of needlestick injuries among Ugandan student nurses in a rural hospital. Rural Remote Health. (2009) 9:1185. doi: 10.22605/RRH1185
40. Talas MS. Occupational exposure to blood and body fluids among Turkish nursing students during clinical practice training: frequency of needlestick/sharp injuries and hepatitis B immunisation. J Clin Nurs. (2009) 18:1394–403. doi: 10.1111/j.1365-2702.2008.02523.x
41. Blackwell L, Bolding J, Cheely E, Coyle E, McLester J, McNeely E. Nursing students' experiences with needlestick injuries. J Undergr Nurs Schol. (2007) 9:9–12.
42. Massaro T, Cavone D, Orlando G, Rubino M, Ciciriello M, Musti EM. Needlestick and sharps injuries among nursing students: an emerging occupational risk. G Ital Med Lav Ergon. (2007) 29:631–2.
43. Smith DR, Leggat PA. Needlestick and sharps injuries among nursing students. J Adv Nurs. (2005) 51:449–55. doi: 10.1111/j.1365-2648.2005.03526.x
44. Yang YH, Wu MT, Ho CK, Chuang HY, Chen LM, Yang CY, et al. Needlestick/sharps injuries among vocational school nursing students in southern Taiwan. Am J Infect Control. (2004) 32:431–5. doi: 10.1016/j.ajic.2004.02.007
45. Shiao JSC, McLaws ML, Huang KY, Guo YL. Student nurses in Taiwan at high risk for needlestick injuries. Ann Epidemiol. (2002) 12:197–201. doi: 10.1016/S1047-2797(01)00303-9
46. Bouya S, Balouchi A, Rafiemanesh H, Amirshahi M, Dastres M, Moghadam MP, et al. Global prevalence and device related causes of needle stick injuries among health care workers: a systematic review and meta-analysis. Ann Global Health. (2020) 86:2698. doi: 10.5334/aogh.2698
47. Yanting Z, Lesan W. Protection education towards needle stick injuries among nursing students in China: a meta-analysis. Chin J Evid Based Med. (2013) 13:754–9.
48. Mengistu DA, Tolera ST, Demmu YM. Worldwide prevalence of occupational exposure to needle stick injury among healthcare workers: a systematic review and meta-analysis. Can J Infect Dis Med Microbiol. (2021) 2021:9019534. doi: 10.1155/2021/9019534
49. Ghanei Gheshlagh R, Nazari M, Baghi V, Dalvand S, Dalvandi A, Sayehmiri K. Underreporting of needlestick injuries among healthcare providers in Iran: a systematic review and meta-analysis. J Hayat. (2017) 23:201–13.
50. Boal WL, Leiss JK, Sousa S, Lyden JT Li J, Jagger J. The national study to prevent blood exposure in paramedics: exposure reporting. Am J Ind Med. (2008) 51:213–22. doi: 10.1002/ajim.20558
51. Ghanei Gheshlagh R, Fallahi Khoshknab M. Needle stick injuries, culture of silence: a systematic review. J Health Promot Manag. (2015) 4:31–50.
52. Trim J, Elliott T. A review of sharps injuries and preventative strategies. J Hosp Infect. (2003) 53:237–42. doi: 10.1053/jhin.2002.1378
53. Mill J, Nderitu E, Richter S. Post-exposure prophylaxis among Ugandan nurses: “Accidents do happen” Int J Africa Nurs Sci. (2014) 1:11–7. doi: 10.1016/j.ijans.2014.05.003
54. Costigliola V, Frid A, Letondeur C, Strauss K. Needlestick injuries in European nurses in diabetes. Diab Metab. (2012) 38:S9–S14. doi: 10.1016/S1262-3636(12)70976-X
55. Quinn MM, Markkanen PK, Galligan CJ, Kriebel D, Chalupka SM, Kim H, et al. Sharps injuries and other blood and body fluid exposures among home health care nurses and aides. Am J Public Health. (2009) 99:S710–S7. doi: 10.2105/AJPH.2008.150169
Keywords: needle-stick injury, nursing student, not reporting needle-stick injury, meta-analysis, sharp injury
Citation: Xu X, Yin Y, Wang H and Wang F (2022) Prevalence of needle-stick injury among nursing students: A systematic review and meta-analysis. Front. Public Health 10:937887. doi: 10.3389/fpubh.2022.937887
Received: 13 June 2022; Accepted: 28 July 2022;
Published: 15 August 2022.
Edited by:
Xiaodong Gao, Fudan University, ChinaReviewed by:
Reza Ghanei Gheshlagh, Kurdistan University of Medical Sciences, IranDechasa Adare Mengistu, Haramaya University, Ethiopia
Copyright © 2022 Xu, Yin, Wang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fengxia Wang, d2FuZ2Z4MTAxOEBzaW5hLmNvbQ==
†These authors share first authorship
‡ORCID: Fengxia Wang orcid.org/0000-0003-4266-7201
 Xu Xu1†
Xu Xu1† Fengxia Wang
Fengxia Wang