
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 24 August 2022
Sec. Public Mental Health
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.936700
This article is part of the Research Topic The COVID-19 Pandemic, Problematic Internet Use, Post-traumatic Stress and Mental Health View all 21 articles
 Xiaoyu Luo1†
Xiaoyu Luo1† Qingqing Xu1†
Qingqing Xu1† Keliang Fan1
Keliang Fan1 Juan Wang1
Juan Wang1 Dandan Wei1
Dandan Wei1 Xian Wang1
Xian Wang1 Xiaomin Lou1
Xiaomin Lou1 Hualiang Lin2
Hualiang Lin2 Chongjian Wang1
Chongjian Wang1 Cuiping Wu1
Cuiping Wu1 Zhenxing Mao1*
Zhenxing Mao1*Objective: College students are one of the most vulnerable populations to the COVID-19 pandemic's mental health effects. During the coronavirus disease 2019 (COVID-19) outbreak, we wanted to see how common depressive symptoms were among college students and what factors contributed to that.
Methods: Between 21 and 27 May 2021, 140,259 college students from three cities in Henan Province, China, were involved. The Patient Health Questionnaire-9 was used to determine depressive symptoms (PHQ-9). Multiple logistic regression analysis was used to calculate odds ratios (ORs) and 95% CIs for potential depressive symptom factors.
Results: Mild depressive symptoms and above are present in 21.12% of college students. Women had a higher prevalence of mild depressive symptoms than men (61.38 vs. 59.75%), and depressive symptoms were most prevalent among rural students and least prevalent among city students (21.44 vs. 20.29%). Participants with depressive symptoms are also more likely to have a poor-behavioral status. From none-to-severe depressive symptoms, 78.88, 15.78, 2.80, 1.67, and 0.88% had them. Gender, residential location, and behavioral status were found to be associated with depressive symptoms after adjusting for potential confounders.
Conclusion: This cross-sectional study identified the factors that influence the prevalence of depression in college students. It found that the government should pay more attention to mental health issues affecting college students in combating the COVID-19 epidemic normalization.
A new-type coronavirus, which has been identified in December 2019 (1), has caused global health concerns due to its devastating impact (2, 3). The imported cases from abroad have been controlled in China at this stage. The epidemic situation in China is sporadic on the whole, and there are occasional small-scale epidemic situations in some parts. In response to the outbreak of the virus, the Chinese government has implemented various measures to prevent the spread of the disease. These include the suspension of public transportation and the closure of non-essential leisure and entertainment establishments (4). A longitudinal population-based study shows that symptoms of anxiety and depression are significant during COVID-19 and increase during lockdown (5, 6). At the same time, some studies have shown that being isolated from others can lead to depressive symptoms. The link between isolation and anxiety has been linked to a variety of mental health issues (7, 8). It has been known that students who are forced to stay at home and are socially isolated are more prone to experiencing higher levels of depression (9, 10).
The depressive symptom is a common mental health disorder that affects the mental health of the general population. It has a worldwide prevalence of 17.3% when using self-reporting instruments to assess depression and is considered to be a mental health disorder (11). In comparison to their counterparts throughout the world, college students have greater rates of mental disorders such as depressive symptoms (12), which can cause horrible feelings such as fear, inadequacy, and wrath, and also psychological and physical morbidities (13–15). Loneliness and illness management measures increase the risk of depression in previously healthy children and adolescents, according to a comprehensive systematic evaluation of data from over 50,000 children and adolescents in 63 research (16, 17). It is clear that the COVID-19 pandemic's direct and indirect psychological and social consequences are pervasive (18–21).
Most of the current literature on the psychological impact of COVID-19 has focused on health workers, patients, and children the general population (22–26). Studies have shown that COVID-19 exposure can lead to high levels of anxiety and depressive symptoms among healthcare workers (27), which raises widespread concern. Of note, college students are at the age of high risk for the onset of mental illness (28, 29). Despite growing evidence of mental health complications from COVID-19 among middle- and high-school students in China (30), there is sparse evidence of psychological or mental health effects of the COVID-19 pandemic on college students, and large sample survey evidence for this group of college students is still very limited. In the face of COVID-19 outbreak, expansion in China and other parts of the world, this study assessed the prevalence of depressive symptoms among college students and identified potential risk and protective factors contributing to depressive symptoms to assist government agencies and healthcare professionals in safeguarding the school's psychological wellbeing.
The cross-sectional study is to investigate the impact of the COVID-19 pandemic on the college student depressive symptoms by using an online questionnaire through an online survey platform (“SurveyStar,” Changsha Ranxing Science and Technology, Shanghai, China) during 21–27 May 2021. In the three cities in Henan Province, China, college students were selected and invited to participate in the survey using a cluster sampling method. In total, 148,999 participants were recruited. For quality control, we excluded the data of participants aged <18 years or aged >25 years or those who took ≤ 100 s to fully respond to the questions (n = 8,740). After this exclusions process, a total of 140,259 participants, aged 18–25 years, were included in this analysis.
The study protocol was approved by the Ethics Committee of Zhengzhou University (ZZUIRB2021-118).
To collect sociodemographic data, a standard questionnaire was devised (age, gender, grade, and residential location). The behavioral status about COVID-19 includes “Has the number of handwashing increased significantly after the outbreak,” “The situation of wearing masks when going out after the outbreak,” as well as mental state (worry and fear levels) and depressive symptoms. City, rural, and county-level cities were used to classify residential locations. The worry and fear levels were divided into five levels (extremely, very, somewhat, not so, and not at all) based on 5-point Likert scale (31). To examine depressive symptoms, the Patient Health Questionnaire-9 (PHQ-9) was employed (32). The PHQ-9 is based on the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition's diagnostic criteria for depressed symptoms (DSM-IV). The PHQ-9's psychometric qualities have already been established in the Chinese populations and developing-country medical settings (32–34). On a 27-point scale, participants were asked how often nine symptoms had emerged in their lives in the previous two weeks: 0 = “not at all,” 1 = “several days,” 2 = “more than half the days,” 3 = “nearly every day.” The severity of depressive symptoms was scored as follows: 0–4 for no depression symptoms, 5–9 for mild, 10–14 for moderate, 15–19 for moderately severe, and 20–27 for severe depressed symptoms (35). A cutoff of 10 or more is reported as diagnostic (35).
Continuous data were presented as mean ± standard deviation (SD) and compared using the t-test, while categorical variables were presented as frequencies (%) and the significance of categorical variable differences was determined using the chi-squared test. The odds ratios (ORs) and 95% CIs of depressed symptoms were calculated using a logistic regression model. Multivariable adjustment modeling was performed: Model 1 was the crude model. Model 2 was adjusted for gender, residential location, worried level, and fear level. Statistical Package for the Social Sciences (SPSS) (version 26) was used for all statistical analyses, with P values of <0.05 indicating statistical significance. Imputation or other substitution procedures were not employed, and only respondents who provided complete data were included in the analysis.
In total, 140,259 participants (aged 18–25 years), which include 70,123 men and 70,136 women, were invited in to participate in the survey from 27 May to 27 May. The characteristics of the participants were listed in Table 1 along with their relationships with depressed symptom status. The study population contained 6,384 cases of depressive symptoms (4.54%). Participants with depressive symptoms had different proportions of age, gender, residence location, and behavioral status than those without depressive symptoms (all P values of <0.05).
The overall depressive symptoms prevalence was 4.54% among college students during the COVID-19 pandemic in China. The prevalence of depressive symptoms in participants was shown in Figure 1 by gender and home region. Male participants living in country-level cities had the highest prevalence of depressive symptoms at 5.03%. Women who resided in rural areas had the lowest prevalence of depressed symptoms, at 4.16%. Overall, the prevalence of depressive symptoms was higher among men than among women, whether in cities, rural, or county-level cities. Figure 2A showed that whether in cities, rural, or country-level cities, the prevalence of depressive symptoms among students who did not change the number of handwashing was higher than those who increased the number of handwashing. Figure 2B showed that the prevalence of participants who lived in rural who do not wear masks was higher than participants who lived in the country-level city who do not wear masks (34.51 vs. 26.92%), but the opposite was true in participants who wear masks occasionally, where participants who lived in the country-level city was higher than the participants who lived in the rural areas (16.62 vs. 14.75%).
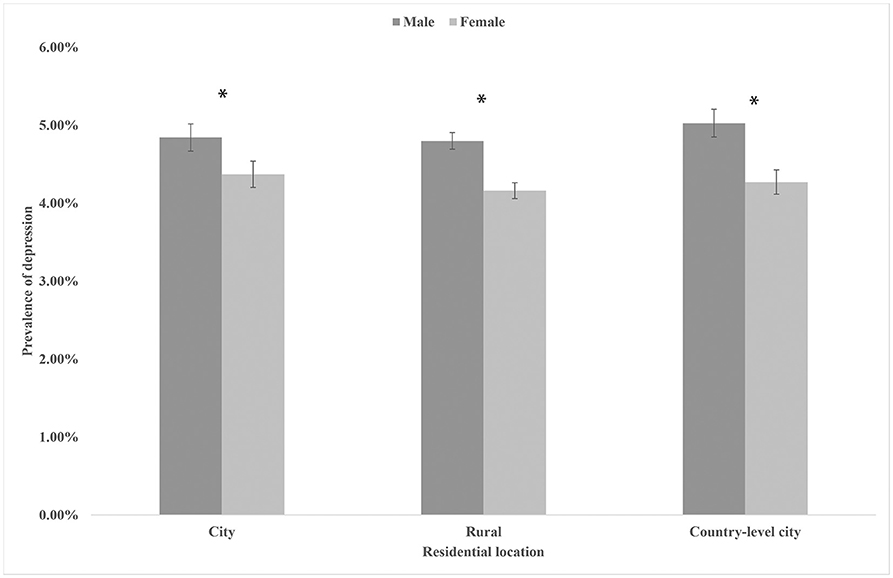
Figure 1. The prevalence of depression symptoms in participants by residential location and gender. * P < 0.05.
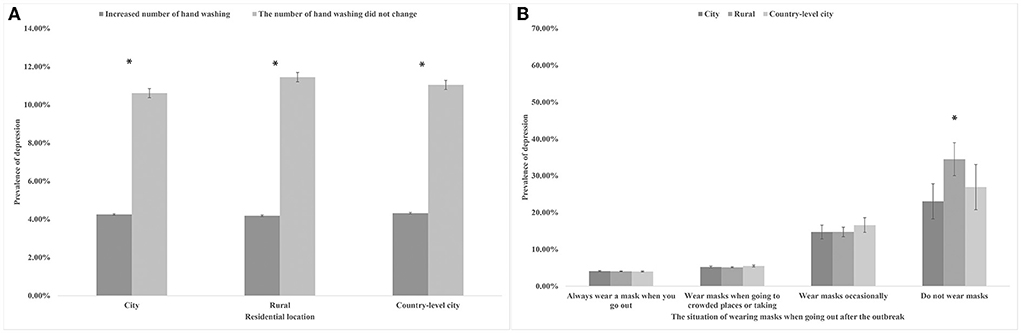
Figure 2. (A) The prevalence of depression symptoms in participants by degree of handwashing and residential location. * P < 0.05. (B) The prevalence of depression symptoms in participants by degree of wearing masks and residential location. * P < 0.05.
Table 2 shows the percentage of pupils with varying levels of depressive symptoms. The proportion of depressive symptoms from none to severe were 78.88, 15.78, 2.79, 1.67, and 0.88%, respectively. Mild depressive symptoms were most common. Compared to men, there were more women who had depressive symptoms (61.38%). But men were more likely to be moderately severe and severe. Obviously, the largest proportion of depressive symptoms occurred in rural (21.44%). The proportion of severe depressive symptoms was the highest (1.07%), although the city proportion of depressive symptoms was the lowest (20.29%). In participants with depressive symptoms, there was a variation in response rates across the nine PHQ symptoms, as shown in Figure 3. Obviously, feeling tired or inactive (78%) and difficulty falling asleep, uneasy sleep, or excessive sleep (75%) were the most common symptoms.
Using multivariable logistic regression analysis, Table 3 showed the relationship between participant characteristics and depressive symptoms. Compared with men, women had 17% [OR 0.83 (95%CI: 0.79–0.88)] reduced odds of depressive symptoms. Meanwhile, after adjusted, students from rural had 8% reduced odds of anxiety [OR 0.92 (95%CI: 0.86–0.98)] compared to the cities. Compared with students with correct behavioral status about epidemic characteristics, students with incorrect behavioral status had higher odds of depressive symptoms. For example, students who make the number of hand-washing unchanged after the outbreak had 232% [OR 3.32 (95%CI: 3.05–3.61)] increased odds of depressive symptoms, compared with students who has the number of handwashing increased significantly after the outbreak. Similarly, compared with students who always wear a mask when they go out, students who wear masks when going to crowded places or taking public transport had 49% [OR 1.49 (95%CI: 1.41–1.57)] increased odds of depressive symptoms. Meanwhile, students who wear masks occasionally [OR 4.67 (95%CI: 4.02–5.42)] and students who do not wear masks [OR 11.26 (95%CI: 8.48–14.96)] had higher odds of depressive symptoms.
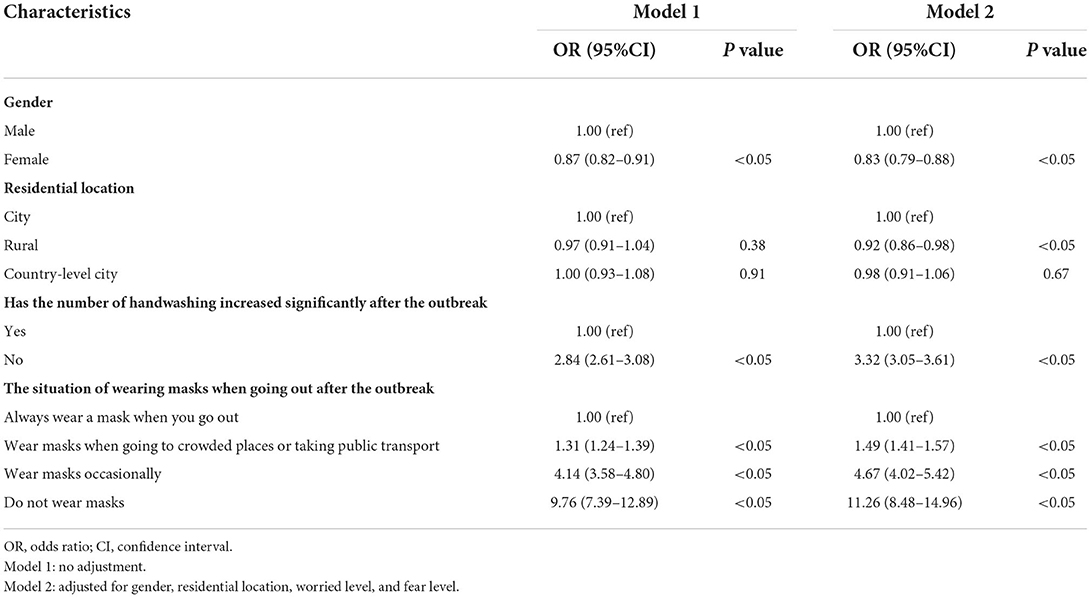
Table 3. Independent association of characteristics of study participants and depression during the COVID-19 epidemic in Henan province.
This is a large-scale cross-sectional epidemiological investigation that took place in Henan Province. We investigated the prevalence of depressive symptoms among 140,259 college students during an outbreak of COVID-19. Our study showed that the prevalence of mild depressive symptoms and above among college students is 21.12%, which was lower than previous studies (37%) (36). Gender, residential location, and behavioral status were found to be associated with depressive symptoms among college students.
The overall prevalence of depressive symptoms in the present study was higher than in previous studies, which may be due to the introduction of epidemic prevention and control measures during the COVID-19 period (30). Some studies have found that female students have higher levels of depressive symptoms than male students (23, 37, 38). However, in contrast to previous findings (39), in our study, male students had more depressing symptoms than female students. Previous research has found similar differences in depressive symptoms between male and female students (40, 41). This could be due to the fact that in China, conventional gender roles and divisions still exist (42). During China's COVID-19, Chinese men as family pillars must bear more psychological pressure to ensure adequate supply and family safety, such as taking high-risk family matters. This differs from studies in other countries (43). At the same time, in the case of COVID-19, the lack of coping strategies will exacerbate male mental health problems (44).
Meanwhile, participants in our study who lived in rural areas had the highest proportion of depressed symptoms (Table 2). Differences in education, family income, medical insurance, and other social-culture factors could explain the disparity between city and rural residents (45). Students from rural areas are more likely to have come from poor families and are regarded as having a lower social status, resulting in disadvantages (46). Lower economic development levels in rural have reduced the ability to solve the problems brought by COVID-19.
Correct behavioral status was identified as a protective factor for our study. Even if only 0.17% of participants stated that they did not wear a mask during the outbreak, they were 1,026% more likely to exhibit depressive symptoms. Depressive symptoms were substantially more common among pupils who had an inappropriate behavioral status. This research emphasizes the need for educational intervention and the dissemination of accurate information. Our research found that knowing the correct type of mask was linked to a lower likelihood of depressive symptoms among college students. Wearing masks has been proven in patients with subclinical or mild COVID-19 to minimize the production of salivary and respiratory droplets (47). Wearing a mask, which is likely the most effective psychological sign for the general public, is necessary as a vital piece of personal protection equipment (48). Furthermore, our findings on COVID-19 health beliefs and face mask use point to some critical health literacy challenges. Because effective communicable disease prevention necessitates individuals to avoid activities that pose a high risk of infection and comprehending the rationale behind suggestions calling for societal responsibility to combat the pandemic, high levels of health literacy are critical (49). Europeans, on the other hand, have mixed feelings about face masks for cultural reasons. The need to utilize them is typically difficult for Europeans to accept (50). It also recommends that we should boost COVID-19 knowledge promotion, particularly in the behavioral status (51). Students can have a better understanding of COVID-19 through public awareness and education, allowing them to protect themselves from COVID-19-related depressed symptoms by practicing good hygiene, wearing a mask, exercising, and eating well (30).
Furthermore, we differentiated the severity of depression symptoms. The findings revealed that the majority of college students had mild depressive symptoms, with only a minority having moderate-to-severe depressive symptoms. It is worth noting that among the students who have depressive symptoms, feeling tired or inactive (78%) and difficulty falling asleep, uneasy sleep, or excessive sleep (75%) are the most common symptoms. As a result, we proposed that the health department establish an online psychological intervention platform where students can seek online psychological assistance if they are experiencing the two symptoms listed earlier (30).
To our knowledge, this is a large sample study of the prevalence of depressive symptoms among college students. Second, to diagnose depression symptoms, we employed the PHQ-9 standardized questionnaire. Finally, to make our results more realistic, we removed participants who did not match the study's conditions. However, some limitations should be recognized when discussing our findings. First, although we corrected several covariates, some potential confounding effects cannot be excluded. Second, because the study is cross-sectional, it is unable to draw inferences regarding the cause-and-effect linkages between the variables. Third, the behavioral status represents the participants' awareness of the COVID-19 pandemic characteristics, although its effectiveness cannot be guaranteed. Finally, because the participants in this study were college students, our findings may not apply to students in other grades.
In conclusion, the prevalence of depressive symptoms among college students was not optimal during the COVID-19 pandemic normalization, particularly among students residing in the rural areas. Furthermore, in the follow-up work, factors such as gender, home location, and behavioral status should be evaluated as part of the overall management of depressive symptoms. These findings imply that in order to prevent COVID-19, governments should pay attention to college' student's mental health, and we should increase the COVID-19 knowledge promotion, particularly in behavioral status.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Ethics Committee of the Zhengzhou University (ZZUIRB2021-118). The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Conceptualization: XLu and QX. Data curation, visualization, and writing—original draft: XLu. Investigation: KF, JW, DW, XW, XLo, and HL. Writing—review and editing: QX, KF, CWa, CWu, and ZM. All authors contributed to the article and approved the submitted version.
This work was supported by the National Natural Science Foundation of China (82041021).
The authors thank the participants for their support during the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Wang YH Li JQ, Shi JF, Que JY, Liu JJ, Lappin JM, et al. Depression and anxiety in relation to cancer incidence and mortality: a systematic review and meta-analysis of cohort studies. Mol Psychiatry. (2020) 25:1487–99. doi: 10.1038/s41380-019-0595-x
2. Wang C, Chudzicka-Czupala A, Tee ML, Nunez MIL, Tripp C, Fardin MA, et al. A chain mediation model on COVID-19 symptoms and mental health outcomes in Americans, Asians and Europeans. Sci Rep. (2021) 11:6481. doi: 10.1038/s41598-021-85943-7
3. Wang C, Tee M, Roy AE, Fardin MA, Srichokchatchawan W, Habib HA, et al. The impact of COVID-19 pandemic on physical and mental health of Asians: a study of seven middle-income countries in Asia. PLoS ONE. (2021) 16:e0246824. doi: 10.1371/journal.pone.0246824
4. Han Z, Ai X, Veuthey J. How is COVID-19 being contained in China? An observational study on the local level. Disaster Med Public Health Prep. (2020) 2020:1–8. doi: 10.1017/dmp.2020.491
5. Chandola T, Kumari M, Booker CL, Benzeval M. The mental health impact of COVID-19 and lockdown-related stressors among adults in the UK. Psychol Med. (2020) 2020:1–10. doi: 10.1017/S0033291720005048
6. Pierce M, McManus S, Hope H, Hotopf M, Ford T, Hatch SL, et al. Mental health responses to the COVID-19 pandemic: a latent class trajectory analysis using longitudinal UK data. Lancet Psychiatry. (2021) 8:610–9. doi: 10.1016/S2215-0366(21)00151-6
7. Sinha M, Pande B, Sinha R. Impact of COVID-19 lockdown on sleep-wake schedule and associated lifestyle related behavior: A national survey. J Public Health Res. (2020) 9:1826. doi: 10.4081/jphr.2020.1826
8. Parrello S, Sommantico M, Lacatena M, Iorio I. Adolescents' dreams under Covid-19 isolation. Int J Dream Res. (2021) 14:10–20. doi: 10.11588/ijodr.2021.1.73858
9. Traunmuller C, Stefitz R, Gaisbachgrabner K, Schwerdtfeger A. Psychological correlates of COVID-19 pandemic in the Austrian population. BMC Public Health. (2020) 20:1395. doi: 10.1186/s12889-020-09489-5
10. Russo C, Giordano G, Marsico G. The social pandemic from SARS-CoV-2 among Italian university students: a pilot study. Psychology Hub. (2022) 39:55–68. doi: 10.13133/2724-2943/17718
11. Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep. (2018) 8:2861. doi: 10.1038/s41598-018-21243-x
12. Boyas JF, Moon SS, Kim YK, Villareal-Otalora T. Applying a classification and regression tree approach to identify individual, socioenvironmental, and psychological interactions associated with suicidal ideation among Latinx adolescents. J Health Social Sci. (2021) 4:527–43. doi: 10.19204/2021/pply6
13. Amarasuriya SD, Jorm AF, Reavley NJ. Prevalence of depression and its correlates among undergraduates in Sri Lanka. Asian J Psychiatr. (2015) 15:32–7. doi: 10.1016/j.ajp.2015.04.012
14. Bostanci M, Ozdel O, Oguzhanoglu NK, Ozdel L, Ergin A, Ergin N, et al. Depressive symptomatology among university students in Denizli, Turkey: prevalence and sociodemographic correlates. Croat Med J. (2005) 46:96–100. Available online at: http://www.cmj.hr/2005/46/1/15726682.htm
15. Eller T, Aluoja A, Vasar V, Veldi M. Symptoms of anxiety and depression in Estonian medical students with sleep problems. Depress Anxiety. (2006) 23:250–6. doi: 10.1002/da.20166
16. Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. (2020) 59:1218–1239.e1213. doi: 10.1016/j.jaac.2020.05.009
17. Singh S, Roy D, Sinha K, Parveen S, Sharma G, Joshi G. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res. (2020) 293:113429. doi: 10.1016/j.psychres.2020.113429
18. Gonzalez-Sanguino C, Ausin B, Castellanos MA, Saiz J, Munoz M. Mental health consequences of the Covid-19 outbreak in Spain. A longitudinal study of the alarm situation and return to the new normality. Prog Neuro-Psychoph. (2021) 107:110219. doi: 10.1016/j.pnpbp.2020.110219
19. Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. (2020) 7:547–60. doi: 10.1016/S2215-0366(20)30168-1
20. Mattila E, Peltokoski J, Neva MH, Kaunonen M, Helminen M, Parkkila AK. COVID-19: anxiety among hospital staff and associated factors. Ann Med. (2021) 53:237–46. doi: 10.1080/07853890.2020.1862905
21. Daniels M, Sharma M, Batra K. Social media, stress and sleep deprivation: a triple “S” among adolescents. J Health Soc Sci. 8:159–66. doi: 10.19204/2021/sclm3
22. Zhang XR, Huang QM, Wang XM, Cheng X, Li ZH, Wang ZH, et al. Prevalence of anxiety and depression symptoms, and association with epidemic-related factors during the epidemic period of COVID-19 among 123,768 workers in China: a large cross-sectional study. J Affect Disord. (2020) 277:495–502. doi: 10.1016/j.jad.2020.08.041
23. Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. (2020) 277:55–64. doi: 10.1016/j.jad.2020.08.001
24. Hao F, Tan W, Jiang L, Zhang L, Zhao X, Zou Y, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. (2020) 87:100–6. doi: 10.1016/j.bbi.2020.04.069
25. Tan W, Hao F, McIntyre RS, Jiang L, Jiang X, Zhang L, et al. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav Immun. (2020) 87:84–92. doi: 10.1016/j.bbi.2020.04.055
26. Nguyen LH, Nguyen LD, Ninh LT, Nguyen HTT, Nguyen AD, Dam VAT, et al. COVID-19 and delayed antenatal care impaired pregnant women's quality of life and psychological well-being: what supports should be provided? Evidence from Vietnam. J Affect Disord. (2022) 298(Pt A):119–25. doi: 10.1016/j.jad.2021.10.102
27. Chew NWS, Lee GKH, Tan BYQ, Jing MX, Goh YH, Ngiam NJH, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. (2020) 88:559–65. doi: 10.1016/j.bbi.2020.04.049
28. Duffy A, Saunders KEA, Malhi GS, Patten S, Cipriani A, McNevin SH, et al. Mental health care for university students: a way forward? Lancet Psychiatry. (2019) 6:885–7. doi: 10.1016/S2215-0366(19)30275-5
29. Ren Z, Xin Y, Ge J, Zhao Z, Liu D, Ho RCM, et al. Psychological impact of COVID-19 on college students after school reopening: a cross-sectional study based on machine learning. Front Psychol. (2021) 12:641806. doi: 10.3389/fpsyg.2021.641806
30. Xu Q, Mao Z, Wei D, Liu P, Fan K, Wang J, et al. Prevalence and risk factors for anxiety symptoms during the outbreak of COVID-19: a large survey among 373216 junior and senior high school students in China. J Affect Disord. (2021) 288:17–22. doi: 10.1016/j.jad.2021.03.080
31. Gupta AK, Maity C. Efficacy and safety of Bacillus coagulans LBSC in irritable bowel syndrome: a prospective, interventional, randomized, double-blind, placebo-controlled clinical study (CONSORT Compliant). Medicine (Baltimore). (2021) 100:e23641. doi: 10.1097/MD.0000000000023641
32. Yu X, Tam WW, Wong PT, Lam TH, Stewart SM. The Patient Health Questionnaire-9 for measuring depressive symptoms among the general population in Hong Kong. Compr Psychiatry. (2012) 53:95–102. doi: 10.1016/j.comppsych.2010.11.002
33. Vu TTM, Le TV, Dang AK, Nguyen LH, Nguyen BC, Tran BX, et al. Socioeconomic vulnerability to depressive symptoms in patients with chronic hepatitis B. Int J Environ Res Public Health. (2019) 16:255. doi: 10.3390/ijerph16020255
34. Tran BX, Dang AK, Truong NT, Ha GH, Nguyen HLT, Do HN, et al. Depression and quality of life among patients living with HIV/AIDS in the era of universal treatment access in Vietnam. Int J Environ Res Public Health. (2018) 15:2888. doi: 10.3390/ijerph15122888
35. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
36. Wang C, Wen W, Zhang H, Ni J, Jiang J, Cheng Y, et al. Anxiety, depression, and stress prevalence among college students during the COVID-19 pandemic: a systematic review and meta-analysis. J Am College Health. (2021) 2021:1–8. doi: 10.1080/07448481.2021.1960849
37. Chang J-J, Ji Y, Li Y-H, Pan H-F, Su P-Y. Prevalence of anxiety symptom and depressive symptom among college students during COVID-19 pandemic: a meta-analysis. J Affect Disord. (2021) 292:242–54. doi: 10.1016/j.jad.2021.05.109
38. Batra K, Sharma M, Batra R, Singh TP, Schvaneveldt N. Assessing the psychological impact of COVID-19 among college students: an evidence of 15 countries. Healthcare (Basel). (2021) 9:222. doi: 10.3390/healthcare9020222
39. Mikolajczyk RT, Maxwell AE, El Ansari W, Naydenova V, Stock C, Ilieva S, et al. Prevalence of depressive symptoms in university students from Germany, Denmark, Poland and Bulgaria. Soc Psychiatry Psychiatr Epidemiol. (2008) 43:105–12. doi: 10.1007/s00127-007-0282-0
40. Bayram N, Bilgel N. The prevalence and socio-demographic correlations of depression, anxiety and stress among a group of university students. Soc Psychiatry Psychiatr Epidemiol. (2008) 43:667–72. doi: 10.1007/s00127-008-0345-x
41. Ren Z, Zhou Y, Liu Y. The psychological burden experienced by Chinese citizens during the COVID-19 outbreak: prevalence and determinants. BMC Public Health. (2020) 20:1617. doi: 10.1186/s12889-020-09723-0
42. Pineles SL, Arditte Hall KA, Rasmusson AM. Gender and PTSD: different pathways to a similar phenotype. Curr Opin Psychol. (2017) 14:44–8. doi: 10.1016/j.copsyc.2016.11.002
43. Sommantico M, DeCicco TL, Osorio Guzmán M, Prado Romero C, Le Bel S, Parrello S. Illness attitudes, mood, and dreams during the second wave of the COVID-19 pandemic: an international study. Int J Dream Res. (2022) 15:104–17. doi: 10.11588/ijodr.2022.1.84712
44. Liu C, Liu D, Huang N, Fu M, Ahmed JF, Zhang Y, et al. The combined impact of gender and age on post-traumatic stress symptoms, depression, and insomnia during COVID-19 outbreak in China. Front Public Health. (2020) 8:620023. doi: 10.3389/fpubh.2020.620023
45. Lei XY, Xiao LM, Liu YN, Li YM. Prevalence of depression among Chinese University students: a meta-analysis. PLoS ONE. (2016) 11:e0153454. doi: 10.1371/journal.pone.0153454
46. Meng H, Li J, Loerbroks A, Wu J, Chen H. Rural/urban background, depression and suicidal ideation in Chinese college students: a cross-sectional study. PLoS ONE. (2013) 8:e71313. doi: 10.1371/journal.pone.0071313
47. Cheng VC, Wong SC, Chuang VW, So SY, Chen JH, Sridhar S, et al. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J Infect. (2020) 81:107–14. doi: 10.1016/j.jinf.2020.04.024
48. Goh Y, Tan BYQ, Bhartendu C, Ong JJY, Sharma VK. The face mask: How a real protection becomes a psychological symbol during Covid-19? Brain Behav Immun. (2020) 88:1–5. doi: 10.1016/j.bbi.2020.05.060
49. Greenhalgh T, Schmid MB, Czypionka T, Bassler D, Gruer L. Face masks for the public during the covid-19 crisis. BMJ. (2020) 369:m1435. doi: 10.1136/bmj.m1435
50. Wang C, Chudzicka-Czupala A, Grabowski D, Pan R, Adamus K, Wan X, et al. The association between physical and mental health and face mask use during the COVID-19 pandemic: a comparison of two countries with different views and practices. Front Psychiatry. (2020) 11:569981. doi: 10.3389/fpsyt.2020.569981
Keywords: depressive symptoms, COVID-19, college students, factors, China
Citation: Luo X, Xu Q, Fan K, Wang J, Wei D, Wang X, Lou X, Lin H, Wang C, Wu C and Mao Z (2022) Prevalence and risk factors of depressive symptoms among 140,259 college students during the COVID-19 epidemic normalization in China: A cross-sectional survey. Front. Public Health 10:936700. doi: 10.3389/fpubh.2022.936700
Received: 08 June 2022; Accepted: 01 August 2022;
Published: 24 August 2022.
Edited by:
Guohua Zhang, Wenzhou Medical University, ChinaCopyright © 2022 Luo, Xu, Fan, Wang, Wei, Wang, Lou, Lin, Wang, Wu and Mao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhenxing Mao, bWFvemhyQGdtYWlsLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.