
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 11 July 2022
Sec. Public Health Education and Promotion
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.936275
This article is part of the Research Topic Accessible Health Programs Promoting Physical Activity and Fitness Level View all 14 articles
Background: The national essential public health service (NEPHS) has been in operation for more than a decade. Numerous studies examined the utilization of NEPHS by migrants and the factors that influence it, but few examined the effect of NEPHS awareness and utilization on the health of inhabitants, particularly migrants. The purpose of this study is to ascertain the level of awareness and utilization of NEPHS, as well as to examine their health-improving effects on migrants.
Methods: Based on the data from the 2017 China Migrants Dynamic Survey, linear probability model, ordered logit model and the propensity score matching methods were employed to investigate impact of awareness and utilization of NEPHS on the health among Chinese migrants. Mediating effect model were used to identify the mechanism of the impact of NEPHS on health.
Results: The findings indicated that migrants' awareness and utilization of NEPHS are still insufficient. After adjusting for other factors, the study discovered that increased awareness and use of NEPHS had a beneficial influence on migrants' self-rated health. Further heterogeneity analysis revealed significant disparities in the health consequences of NEPHS awareness and utilization across subgroups. The effect of increased awareness and usage of NEPHS on health is stronger for middle-aged and elderly people, women, and low-educated migrants with urban household registration. The estimated results of the mediating effect model supported the mechanism that increased NEPHS awareness among the floating population could encourage its utilization and further improve the floating population's health.
Conclusions: Given that migrants' NEPHS utilization is still low and that NEPHS utilization has a positive effect on health, some targeted strategies, such as a variety of new media communication methods, health education related to occupational disease and tuberculosis prevention, and targeted NEPHS projects for specific groups, such as men, young and middle-aged groups, those with a high level of education, and rural migrants, should be conducted to improve the health of migrants.
The country's urbanization and economic development have benefited significantly from the floating population (1, 2). Sustaining economic and social progress has also facilitated population movement (3). China's entire migrant population has been expanding over the last few decades. According to the 7th National Population Census, China's migrant population has surpassed 370 million, a 69.73 percent growth over 2010 (4). The health of this population is jeopardized by high occupational health risks and exposure to substandard living conditions (5, 6), and the existence of the household registration system places the floating population at a significant disadvantage in terms of social welfare and employment opportunities when compared to local residents (7, 8). Additionally, it denies them the same access to healthcare as local residents (9, 10).
To effectively protect the floating population's right to health, China has developed a number of health regulations for migrants in China, and clear arrangements have been established to improve this population's fundamental public health service (11). China began implementing national essential public health services (NEPHS) in 2009; In 2013, the National Health and Family Planning Commission issued Guidance on the implementation of pilot projects for the administration and equalization of public health services and family planning for migrants, and the pilot to provide equal access to NEPHS for migrants was launched. To more effectively promote equal access to basic public health services for migrants, the National Health and Family Planning Commission, in collaboration with relevant departments, issued Guidance on the management of basic public health services and family planning for migrants in 2014. The guidance emphasized the importance of prioritizing the implementation of six basic public health services for migrants, including child vaccination, prevention and control of infectious diseases, maternal and child health care, health records, family planning and health education (12). Additionally, the Report of the 19th Communist Party of China National Congress made a strong case for expediting the equalization of basic public services and implementing the Healthy China agenda. As demand for basic public health care increases among people, China gradually increases investment in basic public health services. The standard for NEPHS per capita subsidy was increased to 79 yuan in 2021 (13). Currently, basic public health services consist mostly of 14 service components, such as health record establishment. In actuality, national primary health care services are based on the notion of voluntary participation. Effective evaluation of the project's health impact lays the groundwork for continued development and optimization of the NEPHS implementation process.
Although it has been some years since migrants received equitable access to basic public health services. However, existing research indicates that there are still issues such as underutilization and disparity in the use of NEPHS by migrants in inflow areas (14). Numerous studies have been conducted to determine the state of affairs and the factors that influence the floating population's use of specific NEPHS projects. Furthermore, these studies consistently demonstrated that migrants' overall utilization of NEPHS remains low (15–19). Analyses of specific regions have yielded similar conclusions (20–23). Additionally, research have been conducted on certain subgroups of migrants, including those with hypertension and type 2 diabetes, the elderly, and the younger generation. It was also discovered that patients with chronic diseases had a poor level of utilization of NEPHS items such as follow-up evaluation, establishment of health records, physical examination, and health education (24, 25). The elderly and young migrants also have a low degree of utilization of NEPHS (26–29).
Some studies discovered significant differences in NEPHS utilization between local residents and migrants when comparing the two groups (30). The proportion of migrants with urban household registration who establish health records is significantly greater than that of migrants with rural household registration (31). While numerous studies have examined the determinants of NEPHS utilization among migrants, few have examined the health benefits associated with increased awareness and utilization of NEPHS among residents, particularly migrants. Local residents' surveys indicated that the NEPHS project can significantly improve hypertension treatment and control (32). Maternal and child healthcare utilization and outcomes have improved markedly (33). NEPHS implementation improved hypertension and diabetes control, as well as the level of health management in patients with severe mental disorders and children (34). Additionally, NEHS has the potential to close the health disparity between residents by increasing health literacy and influencing poor residents' health-related behavior (35). Furthermore, it can help migrants access healthcare (36).
There are only two studies that we are aware of that examine the effects of NEPHS on migrant health. Both of them, however, use the fact that the city implements NEPHS as an explanatory variable in order to examine the impact on the health of migrants (37, 38). Variables constructed at the city level may not accurately reflect the details of NEPHS utilization by migrants, introducing estimation bias into estimates of the health effect. This paper examined the current state of awareness and utilization of NEPHS among Chinese migrants using data from the 2017 China Migrants Dynamic Survey (CMDS) conducted by the National Health Commission. We examined the effect of NEPHS awareness and utilization on population health, which is one of the contributions to existing research; Additionally, there may be a difficulty in studying the aforementioned effect. Migrants who live closer to a community health facility, those who have chronic diseases, and those who have had recent illnesses or injuries are more likely to use NEPHS. Thus, a direct comparison of the health disparity between migrants who use NEPHS and those who do not may lead to the conclusion that NEPHS worsens migrants' health. As a result, the estimation is skewed. Therefore, the estimation is skewed. As a result, this study controls for the above variables in the benchmark regression on the one hand and uses propensity score matching to identify the net effect of NEPHS on the health of migrants on the other hand, which is another contribution of this paper. Finally, in order to examine the distinct effects of NEPHS awareness and utilization on the health of various groups, heterogeneity analysis was used to accurately quantify the impact of NEPHS on the health of various floating populations.
Knowledge, Attitude / Belief, and Practice Theory (KABP) is the most prevalent model used to guide and explain how knowledge and beliefs influence health behavior change (39). According to this theory, health care knowledge and information are the foundation for building positive and accurate beliefs and attitudes, consequently altering health-related behaviors, which can improve an individual's health. Figure 1 depicts the study's conceptual framework. Clearly, information is the first step in altering an individual's behavior. Only if the floating population has a certain awareness of NEPHS will they be more likely to establish the correct health concepts and attitudes and effectively increase the health level of them. Importantly, it is only possible to utilize the related NEPHS services if they are understood beforehand. By getting health education and establishing health records, individuals can increase their focus on health management and health behavior modification, which has a substantial positive effect on their own health. Based on the preceding analysis, the following hypotheses are proposed:
Hypothesis 1: The awareness of NEPHS can effectively increase the health level of individuals, and the floating population whose health records are established and who receives health education has a higher health level. Awareness of NEPHS can promote the establishment of health records and the potential of receiving health education, so contributing to the enhancement of the health status of the floating population.
It is important to note that NEPHS may influence the self-rated health of the floating population with varying features in a way that results in differences in self-rated health. From the standpoint of age, the risk of illness will increase as persons age, and elderly usually pay greater attention to their health. Therefore, NEPHS has a greater impact on the health state of the elderly than on that of the young. In addition, as a special group, NEPHS provides once-yearly health management services for the aged, such as lifestyle and health assessment, physical examination, auxiliary examination, and health counseling. Consequently, it is likely that the health improvement effects of NEPHS will be more pronounced among the older floating population. From gender perspective, there are intrinsic differences in the health condition of men and women, with women paying greater attention to their health status when they are ill and being more ready to seek assistance for illness prevention (40). Consequently, women are more likely to be impacted by NEPHS. From the perspective of education, people with a higher level of education tend to have higher health literacy and greater health knowledge, so they have greater advantages in self-health management, but their health is less affected by NEPHS for the same reason; In addition, urban areas have more medical resources than rural areas, and there are also differences in the allocation of health human resources between urban and rural areas. Urban floating population enjoys greater accessibility and quality of medical care, thus we anticipate that the health improvement effect of NEPHS will be greater in urban regions. Based on the preceding analysis, we suggest the second hypothesis:
Hypothesis 2: Due to diverse characteristics, the impact of NEPHS awareness and utilization on the health of floating populations is heterogeneous. Specifically, NEPHS has a greater impact on the health improvement of middle-aged and elderly, women, urban floating population with low levels of education.
The data for this study came from the National Health Commission's 2017 China Migrants Dynamic Survey (CMDS). The National Health Commission conducted the survey (formerly the National Health and Family Planning Commission). Sample points were chosen randomly from areas where the floating population was concentrated in 31 provinces (autonomous regions and municipalities) and the Xinjiang Production and Construction Corps. The stratified, multistage, and probability proportional to size sampling method was used to investigate migrants aged 15 and over who had lived in the inflow places for at least 1 month but were not district residents (county or city). The survey collects data on family members, household income and expenditure, employment status, mobility, and healthcare utilization, among other things. In 2017, a total of 169,989 valid samples of the floating population were collected. Because NEPHS items are primarily distributed to residents who have lived in the area for more than 6 months, samples of residents who have lived in the area for <6 months were excluded from this study. For inclusion analysis, the final valid sample size was 152,695.
Self-reported health status was used as a proxy for individual health. Each respondent was asked in the CMDS, “How do you feel about your health currently?” 1 = healthy, 2 = basically healthy, 3 = unhealthy, but able to take care of themselves, 4 = unable to take care of themselves.
Each respondent to the CMDS survey was asked if they had heard of the National Essential Public Health Service. This question has two possible answers: 1 indicates yes, and 0 indicates no.
In terms of NEPHS utilization, this study referred to previous research (15) and used two binary variables to determine NEPHS utilization: whether to establish health records and whether to receive any health education in the previous year. Respondents were asked whether local health records had been established. There are four options available: 1 indicates that it is established, 2 indicates that it is not established and that it has not been heard of, 3 indicates that it is not established but has been heard of, and 4 indicates that it is unclear. We unified recoded 2, 3, and 4 as 0, indicating that the individual did not establish health records in the local area. Each respondent was asked in turn if they had received health education in the following areas: occupational disease prevention, sexually transmitted diseases/AIDS prevention, reproductive health and contraception, tuberculosis prevention and control, smoking control, mental health, chronic disease prevention and control, maternal and child healthcare/healthy birth, and self-rescue in public emergencies. We combined the binary variables above and coded respondents as 1 if they had received at least one of the health education activities and 0 if they had received none.
In accordance with previous studies (38, 41), this study included additional variables affecting the health of migrants in the model. Individual demographic characteristics (gender, age, ethnic minorities, marital status, education level, family size, and household registration), socioeconomic status (including household income, health insurance, and employment status), flow range, presence of chronic diseases in the past year, presence of any disease or injury in the past year, and time to the nearest health facilities are all included. Among them, marital status is a dichotomous variable; 0 indicates that the respondent is single, divorced, or widowed, while 1 indicates that the respondent is married for the first time, remarried, or cohabiting. Education level is a triadic variable, with 1 indicating primary school or less, 2 indicating junior high school, and 3 indicating senior high school or more. Household registration is a binary variable, with 1 indicating rural household registration and 0 indicating urban household registration. The model contained five dummy variables that indicated whether interviewees had participated in the New Cooperative Medical System (NCMS), the Coordinating of Urban and Rural Basic Medical Insurance (CURBMI), the Urban Resident Basic Medical Insurance (URBMI), the Urban Employee Basic Medical Insurance (UEBMI), or Free Medical Care (FMC). When assessing individual employment, we incorporate variables representing individual employment status into the model. These variables are classified as follows: 1 = unemployed, 2 = employed, 3 = employer, 4 = self-employed worker, and 5 = other. Respondents' flow range is a three-category variable, with 1 representing inter-provincial flow, 2 representing inter-city flow within the province, and 3 representing inter-county flow within the city. Respondents were asked if they had a doctor's diagnosis of high blood pressure or type 2 diabetes, with 1 indicating they had one or both and 0 indicating they did not. Similarly, respondents were asked if they had experienced any disease or injury in the preceding year, which we recoded as a binary variable, with 1 indicating yes and 0 indicating no. The time to the nearest health facility represented healthcare accessibility, which is a four-category variable: 1 equals <15 min, 2 equals 15–30 min, 3 equals 30–60 min, and 4 equals more than 60 min.
We used descriptive statistics to examine NEPHS awareness and use among Chinese migrants, and then used the chi-square test to determine whether there were significant differences in self-rated health between those who were aware of and used NEPHS and those who were unaware of and did not use NEPHS items.
For regression analysis, we used two models: the linear probability model (LPM) and the ordered logit model. Due to the numerous positive properties of self-rated health (42), it can be treated as a continuous variable. To facilitate comparison of propensity score matching estimate results in the following section, this study used LPM results as the benchmark. Meanwhile, our study presents the regression results for the ordered Logit model. LPM's regression model is as follows:
Where Healthi denotes the individual's self-rated health; NEPHSi denotes whether the individual is aware of or uses the NEPHS; Xi denotes other covariates affecting the migrants' self-rated health; εi is the error term in the model. β is the coefficient effect that we are interested in, as it reflects the effect of migrants' awareness or use of NEPHS on their self-rated health. Additionally, because self-rated health is an ordered variable, we report the estimated results of ordered Logit model.
As mentioned previously, to account for the possibility of estimation bias caused by a variety of factors affecting individuals' awareness of and use of NEPHS, this study used propensity score matching to identify two groups of samples with otherwise similar characteristics in order to estimate the average treatment effect (ATT) on the health of migrants.
In Equation (2), Di denotes the dummy variable of ith migrant's awareness or utilization of NEPHS; Di = 1 indicates that the migrant was aware of or utilized NEPHS; Di = 0 indicates that the migrant was unaware of or did not utilize NEPHS. y1i refers to individual's self-rated health when they are aware of or use NEPHS; y0i refers to the self-rated health when they are unaware or do not use NEPHS. P (X) denotes the probability that migrants are aware of or use NEPHS, also referred to as the propensity score.
For example, to examine the effect of NEPHS awareness on migrants' self-rated health, we first divide the population into those who were aware of NEPHS and those who had not heard of it. The two groups of samples were then matched using four PSM matching strategies (nearest neighbor matching, radius matching, kernel matching, and local linear regression matching). Finally, the treatment group's and control group's self-reported health scores were obtained, as well as the differences between the two groups. A similar approach was used to examine the effect of health education and the establishment of health records on migrants' self-rated health.
To further test the hypothesis of the mediating effect proposed in the conceptual framework, namely, that the awareness of NEPHS can improve the self-rated health of the floating population by increasing the likelihood of establishing health records and receiving health education in the previous year, we developed the mediating effect model (43). Analysis of the mediating impact has been widely utilized as the primary tool for testing the mechanism (44). The most popular method for confirming the mediating effect is the stepwise regression test. It is a technique for determining the existence of a mediating effect by creating three regression models and evaluating the magnitude and significance of the coefficients of key variables. This study employs the same methodology. Three regression models comprise the stepwise regression test:
Among them, Healthi refers to the health of the floating population, Awarenessi to the dummy variable representing NEPHS awareness, and Xi to the other covariates. The mediating variable is Mi. In this study, the variables that serve as mediators are the establishment of health records and the receipt of health education during the past year. The coefficient β1 in Equation (3) represents the total effect of NEPHS awareness on health, the coefficient β2 in Equation (4) represents the effect of NEPHS awareness on mediating variables, and the coefficient γ in Equation (5) represents the effect of mediating variables on the health of the floating population after controlling for Awareness. When β1 is significant, it is possible to verify the statistical significance of 2 and. If both variables are significant, then the mediating effect is significant.
As shown in Table 1, the average age of migrants is 37.10 ± 11.00 years; 48.5% are female; 83.75% are married; and 9.19% are members of minority groups. The majority of migrants have completed junior middle school or less, and the proportion of migrants living in rural areas is even higher, at 82.16%. The study population's annual household income per capita was 30360.10 ± 25748.25 yuan, and employees accounted for 46.68%, the highest rate. NCMS, CURBMI, URBMI, UEBMI, and FMC participation rates were 62.30, 4.81, 7.23, 22.28, and 2.19%, respectively. According to the floating range, the majority of migrants are interprovincial, followed by intercity, and intercounty, with 48.47, 33.42, and 18.11%, respectively. Additionally, 5.74% of them had been diagnosed with hypertension or type 2 diabetes by a physician, and 49.14% had suffered from diseases or injuries in the previous year. In terms of healthcare accessibility, the majority of migrants live <15 min from the nearest health facility (83.51%).
Figure 2 depicted Chinese migrants' specific awareness and use of NEPHS. 59.96% of migrants are aware of the NEPHS, while more than 40% have never heard of it. 30.01% of the population has established health records, while 22.69% of the population has not established health records but has heard about them. 31.14% of migrants who have not established health records and have not been informed about them, and 16.15% of the general population who are unsure whether they have established health records. 75.53% of the population has received some form of health education, while 24.27% has received no form of health education. The participation rate of migrants in each health education activity was depicted in Figure 2D. As can be seen, each health education program has a participation rate of <50%. Occupational disease and tuberculosis prevention education have the lowest participation rates, at 33.37 and 33.67%, respectively.
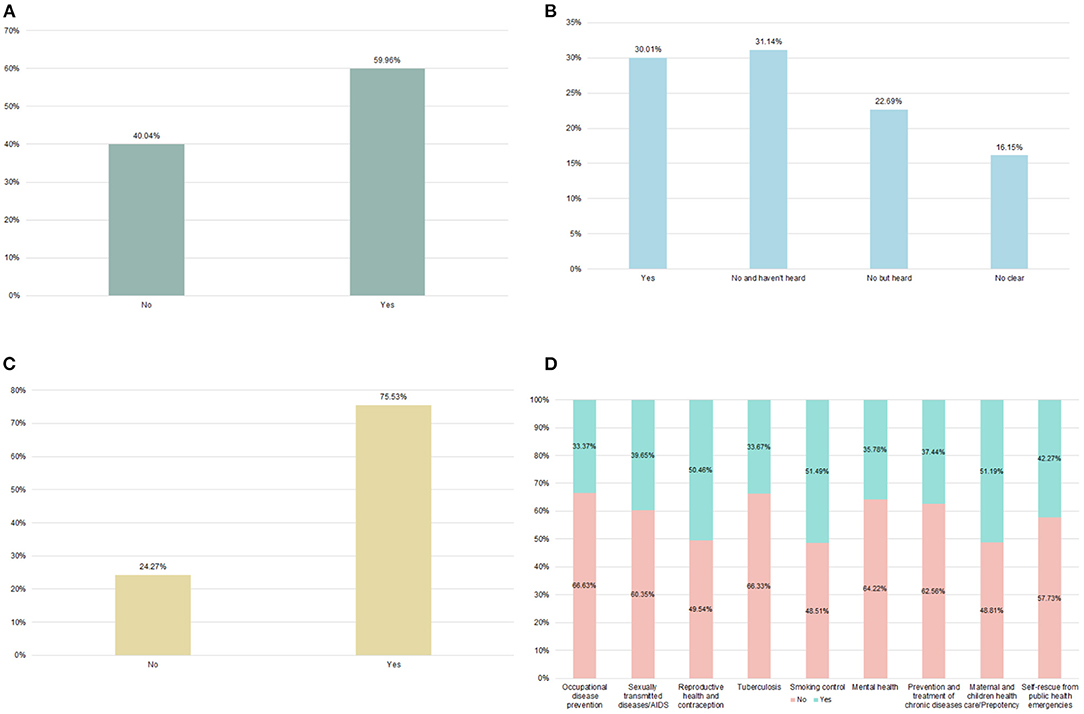
Figure 2. Awareness and utilization of national essential public health services (2017). (A) Awareness of NEPHS (B) Established health record (C) Accepted health education in past year (D) The health education participation rate of different types.
The differences in self-rated health between those who heard about and used NEPHS and those who did not are shown in Table 2. The proportion of healthy migrants who have heard of NEPHS is significantly higher than those who have not (83.03 vs. 79.55%). The proportion of those who are basically healthy, unhealthy and unable to take care of themselves was lower among those who are aware of NEPHS (14.63 vs. 16.83%, 2.27 vs. 3.46%, 0.07 vs. 0.16%). The chi-square test revealed a significant difference in self-rated health between those aware of NEPHS and those who were not (P < 0.01). Similar findings were discovered when it came to health education and the establishment of a health record.
LPM and ordered logit model were used to investigate the effect of NEPHS awareness and utilization on migrants' self-rated health, Table 3 summarizes the estimation results for Models 1–3, which used linear probability model, and Models 4–6, which used non-linear ordered logit model. Regardless of the LPM or Ordered Logit model used, after adjusting for the province fixed effect and other covariates, self-rated health was significantly better for migrants who had heard about NEPHS, received at least one type of health education in the preceding year, and established health records in their place of residence. All of the above effects were statistically significant at the 1% level (P < 0.01). The LPM findings indicated that awareness of NEPHS could improve migrants' self-rated health by ~0.038 units on average, and that receiving at least one type of health education in the previous year could improve migrants' self-rated health by ~0.03 units. Similarly, establishing a health record in the residence area increases self-rated health by an average of 0.035 units.
Although we controlled for as many covariates as possible that could introduce bias into the benchmark regression, we used propensity score matching to determine the homogeneous individuals between those who knew or used NEPHS and those who did not. By comparing the self-reported health of two groups of homogeneous migrants, the average effect of NEPHS on the migrants' self-reported health could be determined.
According to the results of propensity score matching (Table 4), awareness of NEPHS, having received at least one health education in the preceding year, and maintaining health records could significantly improve migrants' self-rated health (P < 0.01). NEPHS awareness would improve migrants' self-rated health by ~0.03–0.039 units on average. Receiving health education has been shown to improve the population's self-rated health by ~0.022–0.025 units. Establishing health records could improve the floating population's self-rated health by an average of 0.028–0.031 units.
Given that the effects of NEPHS on migrants are likely to be influenced by their age, gender, level of education, and household registration, the study samples were further divided into subgroups based on four variables mentioned above. As before, similar LPM regressions were conducted, and Table 5 displayed the corresponding estimation results. The NEPHS had significantly different effects on the self-rated health of different subgroups of migrants. Specifically, awareness of the NEPHS, recent health education, and the establishment of health records had a greater impact on the self-rated health of migrants over 45 years old, particularly the elderly, and a relatively smaller impact on the health of migrants aged 15–44 years old. In terms of gender, the three NEPHS variables have a greater effect on the health of female migrants than on male migrants. Migrants with a primary education level or less were more likely to have their self-rated health influenced by NEPHS. Additionally, NEPHS improved urban migrants' health more than rural migrants' health.
To validate the mechanism of NEPHS on the health of the floating population, we developed a model of the mediating effect. In Table 3, we have established Equation (3) for the model of the mediating effect. Here, we estimated Equations (4) and (5) using the establishment of health records and receiving health education in the previous year as the mediating variables, respectively. Table 6 displayed the estimation results. Model 1 in Table 3 represented the effect of NEPHS awareness on the self-rated health of the floating population, which is denoted by the coefficient β1 in Equation (3). In Table 6, Model 1 illustrated the impact of NEPHS awareness on the establishment of health record. It is evident that NEPHS awareness could significantly increase the possibility of establishing health record for the floating population (P < 0.01). Model 2 estimated the impact of NEPHS awareness on health after controlling the establishment of health record variable and which was statistically significant at the 1% level (P < 0.01). NEPHS awareness still had a favorable influence on the self-rated health of the floating population. Similarly, awareness of NEPHS might considerably improve the likelihood that the floating population has received health education in the previous year (P < 0.01). Awareness of NEPHS remains to have a beneficial influence on the self-rated health of the floating population when the mediating variable is included in the model (P < 0.01).
China has proposed the goal of equalization of national essential public health services for the population since 2013 in order to improve the health status of migrants. Due to the mobility characteristics of the population, it is difficult to conduct NEPHS. The CMDS survey data from 2017 were analyzed in this study to determine the effect of NEPHS awareness or utilization on the health of migrants. Analyses of the current state of awareness and utilization of NEPHS could be used to target areas for improvement in NEPHS implementation. Further investigation of the floating population's health effects and heterogeneity enables evaluation of the NEPHS project's effectiveness, clarification of the NEPHS project's primary improvement direction, and effective improvement of the floating population's health and welfare.
NEPHS's mission is to increase access to and equity in essential public health services. However, our study found that migrants' awareness and utilization of NEPHS are still insufficient, impeding health equity. This is consistent with previous research findings (15, 45, 46). Although the NEPHS project has been in operation for more than a decade, public awareness and utilization of basic public health services remain low. According to a survey conducted in some regions of China, only 0.2 percent of the surveyed floating population was familiar with the entire content of NEPHS items, and there was also an issue of unbalanced development across service items (46). The possible reason is that the floating population's mobility makes it difficult to implement the NEPHS strictly, and the migrants' coverage rate for health records, health education, and health examinations, as well as other services, is mediocre (14). Migrants' ability and initiative to obtain relevant NEPHS information is less developed than that of local residents (23, 47). Simultaneously, the unbalanced allocation of health resources and a lack of human resources for NEPHS contribute to migrants' low awareness and utilization of NEPHS (16, 45).
After adjusting for other covariates, our study demonstrated that increased awareness and use of NEPHS have a beneficial effect on the health of migrants. Our study also indicated that the awareness of NEPHS will promote the establishment of health record of floating population and the likelihood of receiving health education in the last year, consequently increasing their health status. According to the KABP model, the awareness of NEPHS would increase the floating population' s cognition and comprehension of public health services, and then promote them to gradually build a belief that is favorable to their own health. Finally, this positive belief and attitude can be turned into healthy behaviors. By establishing health records and receiving health education, the health literacy of the floating population can be effectively increased, so that individuals attach importance to the monitoring and management of self-health, and thus have a beneficial impact on the health of the floating population.
To a certain extent, awareness of NEPHS reflects the population's health literacy. Several studies found that equalizing NEPHS among migrants via a quasi-natural experiment found that equalizing NEPHS could improve the population's health literacy (38). Individuals with a higher level of health literacy have a greater likelihood of being in better health (48). Improving migrants' health literacy increased their chances of establishing health records and receiving additional health education, which had a positive effect on their use of NEPHS (49). This increase in healthcare utilization would also have a positive effect on health outcomes (50). The establishment of health records can significantly increase awareness of individual health management (45), and also assist health facilities and personnel in monitoring the health of migrants on a regular basis. As a result, it is critical for improving the population's health outcomes. It is self-evident that health education benefits migrants' health. Health education assists the floating population in developing a healthy lifestyle and behavior, and increasing their sense of self-efficacy for behavior change, thereby facilitating their health level improvement (51).
Additionally, our study discovered significant differences in the health effects of NEPHS awareness and utilization across subgroups. The effect of increased awareness and use of NEPHS on health is greater for middle-aged and elderly people, women, and low-educated migrants with urban household registration. Wang et al. found that women establish health records at a higher rate than men, and older immigrants establish health records at a higher rate than younger migrants due to their increased risk of chronic diseases. Additionally, the elderly and women are NEPHS's primary target groups (45). Simultaneously, due to their increased health risks, women and the elderly are more concerned about their own health (52). As a result, the health benefits associated with increased awareness and use of NEPHS are greater for women and elderly migrants. Individuals with a higher education degree are more likely to use NEPHS, which is consistent with our study conclusion (45). By and large, those with a higher level of education have a higher level of health literacy, which means they pay more attention to their health. However, they also have greater access to health knowledge as a result of their higher education level. As a result, NEPHS have a lower effectiveness in improving their health. Additionally, while China is currently reforming its household registration system in order to eliminate social welfare disparities between urban and rural residents, the household registration system continues to have an effect on how urban and rural residents use NEPHS (45). Residents of rural areas have a lower awareness of NEPHS than residents of urban areas (34). Urban migrants, in comparison to rural migrants, are more likely to establish health records (31, 45, 53). Furthermore, NEPHS's health-improving effect is severely limited by a shortage of professional talent and an unbalanced structure of primary health care facilities in rural areas (54).
This study has policy implications, first and foremost, because migrants' awareness of NEPHS is still low, and existing public health publicity methods have been unable to meet resident demand. As a result, a variety of new media communication channels, such as WeChat and other new media, were required to increase the visibility and reach of NEPHS, to fully exploit the subjective initiative in utilizing NEPHS, and to improve NEPHS utilization; Second, health education and public awareness about health issues should be bolstered for migrants. Health administration departments should conduct low-participation health education activities, such as occupational disease and tuberculosis prevention, and utilize information technology to establish health records and fully utilize electronic health records in order to achieve dynamic health management of migrants within the local community. Finally, given the heterogeneity of NEPHS's health effects and the individual characteristics of migrants, targeted NEPHS projects should be conducted for specific groups, such as men, young and middle-aged people, those with a high level of education, and rural migrants, in order to maximize the health benefits of NEPHS.
Additionally, our study has some limitations. Based on the cross nature of the CMDS data, we are unable to accurately determine the long-term effect of NEPHS on health among migrants. Second, due to variable limitations in the data, we are unable to verify the specific mechanism by which NEPHS utilization affects health. Numerous studies have established a link between NEPHS use and health literacy. Our future research will examine whether the use of NEPHS can help individuals improve their health literacy and develop healthy behaviors, thereby improving their health outcomes.
The purpose of this study was to determine the level of awareness and utilization of NEPHS among Chinese migrants and to assess their health-improving effect. The findings indicated that, despite the fact that NEPHS has been in place for over a decade, awareness and utilization of NEPHS remain low among migrants. NEPHS awareness and use had a significant positive effect on the health of migrants. The awareness of NEPHS could promote its utilization and further improve the health status of floating population. However, there are significant differences in the health effects of NEPHS awareness and use across subgroups. During the implementation of NEPHS, targeted measures such as increasing NEPHS publicity efforts and scope, conducting health education activities with a low participation rate, and focusing on males, young and middle-aged adults, those with a high level of education, and rural migrants should be taken.
The data analyzed in this study is subject to the following licenses/restrictions: The datasets employed in our study are not readily available because the data is provided by the Migrant Population Service Center, National Health Commission P.R. China and we have signed a legally binding agreement with the institution that we would not share any original data to any third parties. Requests to access these datasets should be directed to XX, eHV4aW5wZW5nQG5qbXUuZWR1LmNu.
Ethical approval for the study was not required since it was based exclusively on the publicly available data, CMDS. Hence the study subjects were not directly approached.
XX and HY designed the study. QZ and XX led the data analysis and wrote the manuscript. HY, QZ, XX, and QW participated in the revision of the manuscript and approved the final version for publication.
This study was supported by the Open Project of Adverse Drug Reaction Monitoring Center of Family Planning Drugs of National Health Commission/Jiangsu Health Development Research Center (JSHD2021050), Cultivation Project of Decision-making Consultation, Institute of Healthy Jiangsu Development, Nanjing Medical University (7).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We thank the Migrant Population Service Center, National Health Commission P.R. China, very much for providing the data of CMDS 2017.
NEPHS, National Essential Public Health Service; CMDS, China Migrants Dynamic Survey; NCMS, New Cooperative Medical System; CURBMI, Coordinating of Urban and Rural Basic Medical Insurance; URBMI, Urban Resident Basic Medical Insurance; UEBMI, Urban Employee Basic Medical Insurance; FMC, Free Medical Care.
1. Gong X, Kong ST, Li S, Meng X. Rural-urban migrants: a driving force for growth. In: China's Dilemma: Economic Growth, the Environment and Climate Change. Canberra, ACT: Asia Pacific Press (2008). p. 110–52. doi: 10.22459/CD.07.2008.06
2. Du Y, Cai F, Qu X, Cheng J. Sustain the China miracle: reaping the dividends from Hukou Reforms. Econ Res J. (2014) 49:4–13+78.
3. Yuan X. Empirical analysis on current trait and problems of urban floating population in Shanghai. East China Econ Manag. (2008) 139:4–8. doi: 10.19629/j.cnki.34-1014/f.2008.07.001
4. National Bureau of Statistics. Bulletin of the Seventh National Census. Available online at: http://www.stats.gov.cn/ztjc/zdtjgz/zgrkpc/dqcrkpc/ggl/202105/t20210519_1817700.html (accessed January 10, 2022).
5. Li S, Huang H, Cai Y, Xu G, Huang F, Shen X. Characteristics and determinants of sexual behavior among adolescents of migrant workers in Shangai (China). BMC Public Health. (2009) 9:195. doi: 10.1186/1471-2458-9-195
6. Hu X, Cook S, Salazar MA. Internal migration and health in China. Lancet. (2008) 372:1717–9. doi: 10.1016/S0140-6736(08)61360-4
7. Yao H, Xu X, Xue D. Research progress on urban floating population in China. Urban Problem. (2008) 155:69–76.
8. Lin Y, Zhang Q, Chen W, Ling L. The social income inequality, social integration and health status of internal migrants in China. Int J Equity Health. (2017) 16:139. doi: 10.1186/s12939-017-0640-9
9. Zheng L, Hu R, Dong Z, Hao Y. Comparing the needs and utilization of health services between urban residents and rural-to-urban migrants in China from 2012 to 2016. BMC Health Serv Res. (2018) 18:717. doi: 10.1186/s12913-018-3522-y
10. Gong P, Liang S, Carlton EJ, Jiang Q, Wu J, Wang L, et al. Urbanisation and health in China. Lancet. (2012) 379:843–52. doi: 10.1016/S0140-6736(11)61878-3
11. Zheng Y, Ji Y, Chang C, Liverani M. The evolution of health policy in China and internal migrants: continuity, change, and current implementation challenges. Asia Pac Policy Stud. (2020)7:81–94. doi: 10.1002/app5.294
12. National Health and Family Planning Commission, Central Public Security Comprehensive Management Commission, State State Council (Working Group on Migrant Workers), and Ministry of Civil Affairs; Ministry of Finance. Guidance on the management of basic public health services and family planning for migrants. Available online at: http://www.nhc.gov.cn/ldrks/s3577/201411/053b067aa3c84bbd9b87bf51da0c1199.shtml (accessed January 10, 2022).
13. National Health and Family Planning Commission. Notice on the delivery of basic public health services in 2021. Available online at: http://www.gov.cn/zhengce/zhengceku/2021-07/14/content_5624819.htm (accessed January 5, 2022).
14. He H, Zhang J, Xiu D. China's migrant population and health. China Popul Dev Stud. (2019) 3:53–66. doi: 10.1007/s42379-019-00032-7
15. Leng C, Zhu Z. Basic public health services for floating population in China: current situation and factor analysis. Reform Econ Syst. (2020) 6:36–42.
16. Zhang J, Lin S, Liang D, Qian Y, Zhang D, Hou Z. Public health services utilization and its determinants among internal migrants in China: evidence from a Nationally Representative Survey. Int J Environ Res Public Health. (2017) 14:1002. doi: 10.3390/ijerph14091002
17. Guo J, Wen H, Zhou Q. Status quo and determinants on basic public health services of floating population. Chin J Health Policy. (2014) 7:51–6. doi: 10.3969/j.issn.1674-2982.2014.08.011
18. Zhang J, Cai J, He Z, Huang Y, Tang G. Current status of migrant population health education and its influencing factors in China. Chin J Health Educ. (2021) 37:291–6. doi: 10.16168/j.cnki.issn.1002-9982.2021.04.001
19. Cao X, Zhang W, Wang N, Du J, Zhao M, Lin J. Analysis of the current situation and influencing factors of occupational disease prevention and control education of the floating population. Modern Prev Med. (2021) 21:3866–9+3934.
20. Zhang H, Chen L, Zhang Q, Liu S, Tian J, Tan S. Analysis on the utilization and influencing factors of basic public health services of migrant population in Guangdong Province. Chin J Health Educ. (2021) 37:553–7. doi: 10.3390/ijerph18020553
21. Li X, Zhang X, Ren Z, Fan X, Guo X, Shi H, et al. Status Quo of establishment of health records among floating population in western china and its influencing factors. Med Soc. (2021) 3:12–6+22. doi: 10.13723/j.yxysh.2021.03.003
22. Guo X, Huang L, Guo X, Huang L. The situation and influence factors of health records of floating population–based on the national dynamic monitoring data on floating population survey of Sichuan Province in 2014. Popul Dev. (2016) 22:84–9+53.
23. Yue J, Li X. Health consciousness and health service utilization of the floating population in the pearl river Delta area: a community perspective. J Public Manag. (2014) 4:125–35+144.
24. Song Y, Zhang G. Utilization of public health services and its influencing factors among migrant people with hypertension or diabetes in China. Chin J Public Health. (2021) 37:198–202. doi: 10.11847/zgggws1123492
25. Deng B, Liang J. Utilization status and influencing factors of public health services for chronic disease patients in floating population. Chin J Prev Control Chronic Dis. (2020) 28:401–5. doi: 10.16386/j.cjpccd.issn.1004-6194.2020.06.001
26. Du J, Gao L, Wang N, Lin J. Status of the establishment of health files and its influencing factors among the elderly migrants in China. Modern Prev Med. (2020) 47:4033–7.
27. Tang D, Wang F. Influencing factors of basic public health service utilization of the migrant elderly. Chin J Health Policy. (2018) 11:17–22. doi: 10.1186/s12939-018-0861-6
28. Yan Q, Tong L. Utilization of basic public health services and its influence factors among young migrants. Chin J Public Health. (2019) 35:680–4. doi: 10.11847/zgggws1119401
29. Lin Y, Wang T, Zhu T. Do Migration characteristics influence the utilization of basic public health services in internal elderly migrants in China? Front Public Health. (2021) 9:1103. doi: 10.3389/fpubh.2021.514687
30. Yang, Xin. Difference in utilization of basic public health service between registered and migrant population and its related factors in China, 2015. Chin J Public Health. (2018) 34:781–5. doi: 10.11847/zgggws1115819
31. Qian Y, Ge D, Zhang L, Sun L, Li J, Zhou C. Does Hukou origin affect establishment of health records in migrant inflow communities? A nation-wide empirical study in China. BMC Health Serv Res. (2018) 18:704. doi: 10.1186/s12913-018-3519-6
32. Zhang D, Pan X, Li S, Liang D, Hou Z, Li Y, et al. Impact of the national essential public health services policy on hypertension control in China. Am J Hypertens. (2018) 31:115–23. doi: 10.1093/ajh/hpx139
33. Feng H, Zhang Y, Zheng Y, Zhang Y, Zhang L, Han Y, et al. Comprehensive assessment on implementation and effect of basic public maternal and child health service in Guizhou province from the year 2009 to 2015. Modern Prev Med. (2017) 44:1814–8.
34. Pu X, Gen S, Cao Z, Wu S. A study of the effect of basic public health services. Health Econ Res. (2018) 3:17–20. doi: 10.14055/j.cnki.33-1056/f.20180302.018
35. Zhang Z, Miao Y. Analysis on the contribution of primary public health service on public health disparity. Chin J Popul Sci. (2020) 6:78–89+127–8.
36. Wang H, Cheng Q, Ni Z. Can the policy of equalization of basic public services for health and family planning improve the utilization of medical services by migrant population. Public Fin Res. (2019) 434:91–101. doi: 10.19477/j.cnki.11-1077/f.2019.04.008
37. Fu M, Liu C, Yang M. Effects of public health policies on the health status and medical service utilization of Chinese internal migrants. China Econ Rev. (2020) 62:101464. doi: 10.1016/j.chieco.2020.101464
38. Cheng Q, Li Y. The health effect analysis of basic public health services equalization for floating population. Northwest Popul J. (2021) 6:26–35. doi: 10.15884/j.cnki.issn.1007-0672.2021.06.003
39. Kaliyaperumal K. Guideline for conducting a knowledge, attitude and practice (KAP) study. AECS Illumin. (2004) 4:7–9. Available online at: http://v2020eresource.org/content/files/guideline_kap_Jan_mar04.pdf
40. Verbrugge LM, Wingard DL, Features Submission HC. Sex differentials in health and mortality. Women Health. (1987) 12:103–45. doi: 10.1300/J013v12n02_07
41. Ren G, Hu M. Analysis of self-assessment health status of interprovincial floating population and its influencing factors based on data of national floating population dynamic monitoring survey in 2014. Chin Health Serv Manag. (2021) 8:587–93+625.
42. Pan J, Lei X, Liu GG. Health insurance and health status: exploring the causal effect from a policy intervention. Health Econ. (2016) 25:1389–402. doi: 10.1002/hec.3225
43. Wen Z, Ye B. Analyses of mediating effects: the development of methods and models. Adv Psychol Sci. (2014) 22:731. doi: 10.3724/SP.J.1042.2014.00731
44. Yang H, Wu Y, Lin X, Xie L, Zhang S, Zhang S, et al. Internet use, life satisfaction, and subjective well-being among the elderly: evidence from 2017 China General Social Survey. Front Public Health. (2021) 9:677643. doi: 10.3389/fpubh.2021.677643
45. Wang J, Zhu J, Wang X, Che Y, Bai Y, Liu J. Sociodemographic disparities in the establishment of health records among 0.5 million migrants from 2014 to 2017 in China: a nationwide cross-sectional study. International J Equity Health. (2021) 20:250. doi: 10.1186/s12939-021-01584-2
46. Guo J, Yang H, Liu L, Shao F. Status quo and determinants of awareness on basic public health service among migrant population. Chin J Public Health. (2019) 35:63–6. doi: 10.11847/zgggws1117247
47. Hou Z, Lin S, Zhang D. Social capital, neighbourhood characteristics and utilisation of local public health services among domestic migrants in China: a cross-sectional study. BMJ Open. (2017) 7:e014224. doi: 10.1136/bmjopen-2016-014224
48. van der Heide I, Wang J, Droomers M, Spreeuwenberg P, Rademakers J, Uiters E. The relationship between health, education, and health literacy: results from the dutch adult literacy and life skills survey. J Health Commun. (2013) 18:172–84. doi: 10.1080/10810730.2013.825668
49. Yu Y, He A, Zheng S, Jiang J, Liang J, Shrestha B, et al. How does health literacy affect the utilization of basic public health services in Chinese migrants? Health Prom Int. (2021) 37:daab040. doi: 10.1093/heapro/daab040
50. Yu H-Y, Wu W-L, Yu L-W, Wu L. Health literacy and health outcomes in China's floating population: mediating effects of health service. BMC Public Health. (2021) 21:691. doi: 10.1186/s12889-021-10662-7
51. Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. (2000) 15:259–67. doi: 10.1093/heapro/15.3.259
52. Tian H, Liu Y, Yang Y, Chun M, Zou Q, Ye Y. Study on the status and influencing factors of awareness of hypertension prevention and health behavior among the patients with hypertension. Modern Prev Med. (2016) 24:4481–4.
53. Wang Z, Wu Q, Ming J. The relationship between homeownership and the utilization of local public health services among rural migrants in China: a nationwide cross-sectional study. Front Public Health. (2020) 8:808. doi: 10.3389/fpubh.2020.589038
Keywords: awareness, utilization, national essential public health service, health, migrants
Citation: Xu X, Zhang Q, You H and Wu Q (2022) Awareness, Utilization and Health Outcomes of National Essential Public Health Service Among Migrants in China. Front. Public Health 10:936275. doi: 10.3389/fpubh.2022.936275
Received: 05 May 2022; Accepted: 20 June 2022;
Published: 11 July 2022.
Edited by:
Youcheng Liu, Wayne State University, United StatesCopyright © 2022 Xu, Zhang, You and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xinpeng Xu, eHV4aW5wZW5nQG5qbXUuZWR1LmNu; Hua You, eW91aHVhOThAMTYzLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.