
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
EDITORIAL article
Front. Public Health , 05 August 2022
Sec. Environmental Health and Exposome
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.932922
This article is part of the Research Topic One Health, Environmental Health, Global Health, and Inclusive Governance: What can we do? View all 12 articles
Editorial on the Research Topic
One health, environmental health, global health, and inclusive governance: What can we do?
“One Health” is a broad conceptual platform that encompasses a global view of human and animal health, along with the environment, encompassing air, water, soil, and plants. It requires integrating interactions both from bottom-up and top-down perspectives, anchored in an inclusive government (1) and supported by interactive science, i.e., scientific cooperation across disciplines. At the ground level, what is done in practice must influence those governing, leading to more responsive, effective, and inclusive governance and in so doing, much-improved outcomes. Human and veterinary medicine, public health, social sciences, educators, and legislators have to be involved and contribute to what is decided and done at the national and local levels.
An integral element of the One Health concept is the critical importance of addressing the effects of the devastating environmental imbalance of today. This is a major task for our generation and our children, with very limited time left to avoid a planetary catastrophe, aspects of which are already visible. Worldwide, and in many regions and individual countries, current economic, social, and environmental policies are too dangerous and unsustainable. The future state of the environment is, in short, central to One Health's aspirations. The imbalances between developing and developed countries are crucial aspects of this, with many examples that demonstrate this point. For example in this research volume, Streichert et al. discuss the pandemic response, outlining that “lack of opportunities is a commonly reported barrier to involvement globally, with lack of funding the largest barrier in the WHO African region.” Eliakimu and Mans promote the concept of inclusive governance to cope with global inequalities. Differences in COVID-19 vaccine availability showcase the challenge (Figure 1)1:
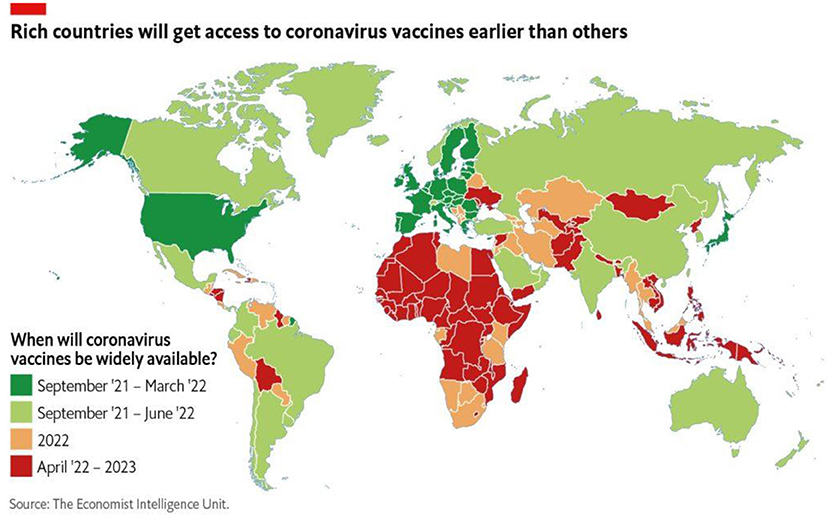
Figure 1. When will coronavirus vaccines be widely available? Source: The Economist Intelligence Unit.
The basic framework for One Health research is captured in THE WORLD IN 2050 INITIATIVE (TWI) (2), which defines six sustainable development pathways:
(1) Education, gender, and inequality.
(2) Health, well-being, and demography.
(3) Energy de-carbonization and sustainable industry.
(4) Sustainable food, land, water, and oceans.
(5) Sustainable cities and communities.
(6) Digital revolution for sustainable development.
These six areas provide the broad framework for the contributions within this Frontiers for Public Health Research Topic. The contributions can be further divided into four groups, of which there are 11 articles published to date.
The first group comprises more familiar topics including tobacco control policies in the Indonesian mining industry (Prabandari et al.). Another article in this grouping explores one health perspective regarding diarrhea in Pakistan (Abbasi et al.) while another discusses the quality of life connected with living near a solid waste facility (Phan et al.).
The second group deals with the COVID-19 pandemic, such as a paper on variations of COVID-19 in the three Palestinian territories, the West-Bank, East-Jerusalem, and Gaza Strip (Abed et al.), covering the spread, risk factors, and interventions. Mahadi discusses the post-COVID AMR threat in LMIC, taking Bangladesh as an example. Another analyses participation in One Health networks as part of a COVID-19 response (Streichert et al.).
The third group covers information and policies. Coming from the same background as Streichert et al., i.e., the One Health Commission, Eliakimu and Mans review inequalities toward inclusive governance. Roopnarine et al. discuss the missing professional perspective of One Health for medical, veterinary, and public health students. LeBlanc et al. underline bioethics and One Health to build reflexive governance. Finally, Yu et al. analyze the effects of environmental information on elderly people in China.
The fourth area deals with satisfaction in life, which is often integrated under the Subjective Well-being (SWB) rubric, as documented here for three countries in the Western Balkans: Montenegro, North Macedonia, and Serbia by Bjegovic-Mikanovic et al. As outlined in this study, Montenegro takes a top position in almost all dimensions.
To achieve significant One Health breakthroughs, there must be diminishing global economic and social disparities between countries and within countries. Even in the most developed countries, underserved populations are substantial in numbers. Their lot has to be improved if we want to follow a civil discourse, both within countries and between them, and at global levels. The unfortunate reality is exemplified during these last two pandemic years by the case of vaccine availability and supporters attacked by the anti-vax movement.
The question remains, can we expect those without power and those who are being deprived to behave according to One Health approaches? In most societies, waiting in the wings, and not being able to access essential services can result in aggressive communication or even physical attack. There are differences, of course, inherent in culture to not tolerate such conduct, such as in the Scandinavian countries. In many other countries and may be in Scandinavia as well, there are risks that a pandemic like that of COVID-19 and its restrictions will continue to unlock latent resentment and anger of those less fortunate. The many implications of largely unregulated social media make it easier to develop extremist views that grow fast in times of general hardship when people look desperately for information and support, and unfortunately often encounter facile answers (3).
Addressing the fundamental question of what we can do at this time to save future generations, the following four areas can contribute to our social and scientific environments (4, 5):
(1) Identify the barriers to changing unsustainable behaviors.
(2) Employ various commitment strategies.
(3) Produce and communicate effective messages.
(4) Enhance motivation and invite participation (active civility).
Despite the promise of these strategies, limitations are also evident. The present trajectories cannot be redirected by the global North alone; effective international cooperation will be of central relevance. Physicians and veterinarians are essential professions that likewise cannot change the presently prevailing trends alone, and contributions from the social and political sciences are vital for implementing change successfully. In summary, the space between bottom-up and top-down, between grassroots and organized action needs to be filled by all of us. To progress toward One Health, it will not be enough to organize the Connected: we must also proactively engage impoverished and marginalized Disconnected populations (3) to negotiate dangerous times and unpredictable futures.
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. ^https://www.eiu.com/n/rich-countries-will-get-access-to-coronavirus-vaccines-earlier-than-others/
1. Abed Y, Sahu M, Ormea V, Mans L, Lueddeke G, Laaser U, et al. Introduction to One Health: Special Volume No. 1, 2021: The Global One Health Environment. Bielefeld: South Eastern European Journal of Public Health (SEEJPH) (2021).
2. TWI2050-The World in 2050. Transformations to Achieve the Sustainable Development Goals. Report prepared by the World in 2050 Initiative. International Institute for Applied Systems Analysis (IIASA), Laxenburg (2018). Available online at: www.twi2050.org; http://pure.iiasa.ac.at/15347.
3. Laaser U. How to Save our Common Future: The Global One Health One Welfare Approach. Impacter (2022). Available online at: https://impakter.com/save-common-future-global-one-health-one-welfare/
4. Seifman R.. A guide towards One Health action. In: Abed Y, Sahu M, Ormea V, Mans L, Lueddeke G, Laaser U, Hokama T, Goletic R, Eliakimu E, Dobe M, and Seifman R. Introduction to One Health: Special Volume No. 1, 2021: The Global One Health Environment. Bielefeld: South Eastern European Journal of Public Health (SEEJPH) (2021).
5. Laaser U. What can we do to improve One Health? In: Abed Y, Sahu M, Ormea V, Mans L, Lueddeke G, Laaser U, Hokama T, Goletic R, Eliakimu E, Dobe M, and Seifman R. Introduction to One Health: Special Volume No. 1, 2021: The Global One Health Environment. Bielefeld: South Eastern European Journal of Public Health (SEEJPH) (2021).
Keywords: One Health, environmental health, global health, inclusive governance, bottom-up, top-down
Citation: Laaser U, Bjegovic-Mikanovic V, Seifman R, Senkubuge F and Stamenkovic Z (2022) Editorial: One health, environmental health, global health, and inclusive governance: What can we do? Front. Public Health 10:932922. doi: 10.3389/fpubh.2022.932922
Received: 30 April 2022; Accepted: 03 June 2022;
Published: 05 August 2022.
Edited and reviewed by: Gianluca Severi, Institut National de la Santé et de la Recherche Médicale (INSERM), France
Copyright © 2022 Laaser, Bjegovic-Mikanovic, Seifman, Senkubuge and Stamenkovic. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ulrich Laaser, dWxyaWNoLmxhYXNlckB1bmktYmllbGVmZWxkLmRl; bGFhc2VydUBnbWFpbC5jb20=
†These authors have contributed equally to this work
‡Senior U.S. Foreign Service Officer (retired)
§ORCID: Ulrich Laaser orcid.org/0000-0001-5889-4471
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.