- 1Department of Environmental Health and Occupational Medicine, West China School of Public Health and West China Fourth Hospital, Sichuan University, Chengdu, China
- 2Cochrane China Center, West China Hospital, Sichuan University, Chengdu, China
- 3Chinese Evidence-Based Medicine Center, West China Hospital, Sichuan University, Chengdu, China
- 4Sichuan Provincial Center for Mental Health, Sichuan Academy of Medical Sciences and Sichuan Provincial People's Hospital, Chengdu, China
- 5West China School of Nursing, West China Hospital, Sichuan University, Chengdu, China
- 6Department of Occupational Hazard Assessment, West China School of Public Health and West China Fourth Hospital, Sichuan University, Chengdu, China
Objective: During the COVID-19 pandemic, the occupational stress of medical staff has been a major issue. This study aimed to suggest a new strategy to identify high-risk factor sets of occupational stress in medical staff using fuzzy-set qualitative comparative analysis (fs-QCA) and provide ideas for the prevention and intervention of occupational stress.
Methods: A total of 1,928 medical staff members were surveyed and tested using the Acceptance and Action Questionnaire-II (AAQ-II), Occupational Stress Inventory-Revised edition (OSI-R), and Eysenck Personality Questionnaire-Revised Short Scale (EPQ-RSC). The fs-QCA was used to explore the high-risk factors for occupational stress among medical staff.
Results: The psychological strain (PSY) score of the medical staff was 26.8 ± 7.13, and the physical strain (PHS) score was 24.3 ± 6.50. Low psychological flexibility score-introversion-high role overload, introversion-neuroticism-high role overload, and low psychological flexibility score-neuroticism were high-risk factor sets for PSY. Low psychological flexibility score-introversion-high role overload, low psychological flexibility score-introversion-neuroticism, low psychological flexibility score-neuroticism-high role overload, low psychological flexibility score-psychoticism-neuroticism, and psychoticism-neuroticism-high role overload were high-risk factor sets for PHS.
Conclusion: There are different combinations of high-risk factors for occupational stress among the medical staff. For occupational stress intervention and psychological counseling, targeted and individualized health intervention measures should be implemented according to specific characteristic combinations of different individuals.
Introduction
Stress is a health problem commonly faced by occupational groups, and medical staff are a high-risk group for mental health problems (1–3). A cohort study published in 2018 reported that the prevalence of depression, anxiety, and stress among Australian nurses was reported as 32.4, 41.2, and 41.2%, respectively (4). In addition, a cross-sectional survey conducted in China found that 68.3% of nurses reported high levels of occupational stress (5). A meta-analysis reported that the prevalence of burnout syndrome was highest among nurses, younger persons, and trainees (6). During the COVID-19 pandemic, the situation of the medical staff has been more complex and severe. It is reported that depression and anxiety of workers who had unprotected contact with infectious patients was reported a significant increase in the estimated risk compared to control (7, 8). Francesco et al. (9) found that a significant proportion of workers in emergency care reported more severe burnout symptoms than those engaged in non-healthcare social and administrative duties. In the first wave of COVID-19 pandemic, the prevalence of burnout syndrome in voluntary psychologists was nearly 17%, and neuroticism was positively associated with burnout symptoms (10, 11). In addition, a meta-analysis found that the overall prevalence of occupational stress among medical staff caring for patients with COVID-19 was 45% (12).
Many factors are associated with occupational stress, and work patterns are complex. Stress is not only closely related to working conditions in the occupational environment but is also related to individual characteristics, personality traits, and sociopsychological factors (13–16). Reportedly, individuals with a type A personality (more self-motivated, self-confidence, aggressive, and a sense of achievement) are more likely to suffer from occupational stress (17). Several studies have also found that medical staff and older adults with introverted personalities and negative emotions usually have more severe stress symptoms than control groups (18, 19). In addition, poor psychological resilience, self-efficacy, psychological flexibility, and coping resources are also believed to be related to occupational stress (14, 20). Faced with such a complicated situation, the quick identification of high-risk factors or high-risk factor sets to take targeted intervention measures is the key point for preventing occupational stress.
In previous studies, we focused on the individual effects of target factors, such as social support, self-efficacy, and workload, after adjusting for other variables, such as demographic characteristics (14, 18, 20). However, in most actual situations, several risk factors may exist simultaneously, such as introverted nurses who lack social support but are engaged in high-load work or individuals with low self-efficacy engaged in high-load work. The combination of different traits is complex and variable for different individuals. Identifying the risk of stress among different individuals in occupational activities and what combination of different traits are more likely to cause occupational stress are the issues we want to discuss.
Qualitative comparative analysis (QCA) is a suitable tool to solve this problem. QCA is a data processing method between probability statistical analysis and single-case analysis, and was first launched by Charles Ragin in 1987 (21). It was originally developed in the fields of political science and historical sociology to determine which intervention or combination of interventions might be the most effective (22). QCA brings together qualitative and quantitative data derived from cases to identify the necessary and sufficient conditions for an outcome (23). It has unique advantages in the analysis of complex social problems formed by multiple concurrent causalities (24, 25). QCA subsequently developed a class of models, including clear-set qualitative comparative analysis (cs-QCA), multivalued qualitative comparative analysis (mv-QCA), and fuzzy-set qualitative comparative analysis (fs-QCA) (21, 26). In recent years, fs-QCA has been actively applied in the field of public health. Initially, it was used to evaluate public health interventions, including mental health interventions (27), medication adherence interventions (28) and health promotion interventions (29, 30). At the same time, the fs-QCA also has applications in the discussion of risk factors, such as children's language barriers (31), nurses' ability (32), and adolescent self-esteem and life satisfaction (33). However, no relevant research has been conducted on the interventions and influencing factors of occupational stress.
Occupational stress is a physical and mental health problem caused by multiple factors such as working conditions, personality, and social psychological factors. In this study, we used the fs-QCA method to analyze the effects of role overload, personality, and psychological flexibility on occupational stress among medical staff and explore high-risk factor sets of occupational stress. This study aimed to provide a theoretical basis for effectively coping with occupational stress and formulating intervention measures.
Materials and Methods
Study Population
This study used a cross-sectional research design. A self-administered questionnaire and three standardized scales were used to collect data on basic characteristics, personality characteristics, psychological flexibility, and occupational stress from 15 public hospitals. The inclusion criteria were as follows: medical staff in public hospitals above the municipal level; participants including doctors, medical technicians, and nurses; at least 18 years of age; and at least 1 year of service. The exclusion criteria were temporary staff or trainees, logistical administrative staff, retired staff, and rehired staff. The survey was jointly organized by the research group and the hospital personnel department. Specially trained investigators were assigned to different clinical departments to carry out investigations. The task of investigators was to distribute questionnaires and guide the completion of the questionnaires. A total of 1,928 medical staffs were invited as participants using multistage random cluster sampling. During the study, 127 subjects were additionally excluded (withdrew or did not complete the questionnaire and test), and 1,801 subjects were finally included. The ratio of responders over invitations was 93.4%. This study was approved by the Ethics Committee of the West China School of Public Health, Sichuan University (No. Gwll2021070).
Outcome Measurements
Personality was measured using the Eysenck Personality Questionnaire-Revised Short Scale for Chinese (EPQ-RSC), which includes three dimensions: extraversion, neuroticism, and psychoticism (34). In the extraversion dimension, high scores indicate extroversion (E) and low scores indicate introversion (e). A high score for neuroticism means more emotional reactions such as anxiety and worry, and even irrational behavior (N), while low scores indicate weaker emotional reactions (n). High scores in psychoticism indicate loneliness, indifference, and difficulty adapting to the external environment (P), while low scores are normal (p).
Psychological flexibility was measured using the Acceptance and Action Questionnaire-II (AAQ-II), which contains 10 items. The AAQ-II adopts a Likert-style 7-point scoring system, with one point for complete non-compliance and seven points for complete compliance. Items 1, 6, and 10 were scored positively, and items 2, 3, 4, 5, 7, 8, and 9 were scored backwards. The sum of item scores is the total score of the scale, which ranges from 10 to 70 points. Higher scores indicate stronger psychological flexibility (A) and lower scores indicate weaker psychological flexibility (a). Cronbach's α coefficient for the scale was 0.705 (35).
Occupational stress was measured using a simplified version of the Occupational Stress Inventory-revised edition (OSI-R). We chose three dimensions of the OSI-R, including role overload (RO), psychological strain (PSY) and physical strain (PHS). A high RO score indicates a self-perceived high workload (R), whereas a low score indicates an acceptable workload (r). All the items were retained for each dimension to ensure the construct validity of the questionnaire. The simplified version of the OSI-R has good test-retest reliability and good homogeneity with the OSI-R (36).
Statistical Analysis
STATA 14.0 software was used for analysis. Statistical analysis methods included partial correlation analysis, variance analysis, and fs-QCA. The fs-QCA evaluates the relationship between an outcome and all possible Boolean combinations of the predictors. The degree of contribution of each combination of predictors in a given outcome was assessed using Boolean logistic tests for solution consistency and total coverage of the outcome and combinations of multiple binary predictive risk factors (26, 37).
The basic steps of fs-QCA are as follows: (1) Use the setgen command to fuzzify the data to a range between 0 and 1 without changing the distribution of the original data; (2) Generate a set of combinations of independent variables and test the consistency of all combinations with the outcome (solution consistency); (3) Use the reduce command to reduce the factor combination set of the consistency test to obtain the final factor combination set that is meaningful or explanatory for the outcome, and calculate the overall coverage of the factor combination set (total coverage) (37).
In this study, the fs-QCA included a total of five independent variables: extroversion (E/e), neuroticism (N/n), psychoticism (P/p), psychological flexibility (A/a) and role overload (R/r). All independent variables were automatically divided into a high-score and a low-score group during the analysis process, where uppercase letters represent higher scores, and lowercase letters represent lower scores on the corresponding dimension.
Results
Occupational Stress of Medical Staff
Among the 1,801 participants, 357 were male (19.82%), and 1,444 (80.18%) were female. The age range of the subjects was 18–61 years old, with an average age of 30.9 ± 8.35 years. The PSY score of the participants was 26.8 ± 7.13, and the PHS score was 24.3 ± 6.50. The level of individual stress responses of the medical staff is shown in Table 1.
Relationship Between Role Overload, Personality, Psychological Flexibility, and Stress
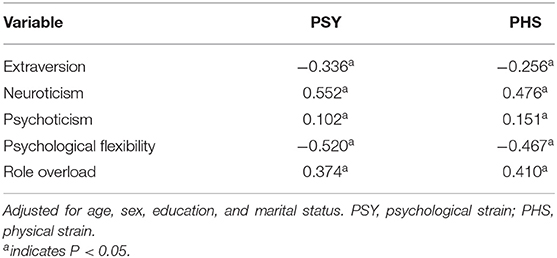
The partial correlation analysis among the included factors after adjusting for basic demographic characteristics is shown in Table 2. The results showed that there were statistically significant correlations between personality, psychological flexibility, role overload, and occupational stress (PSY and PHS) of the medical staff (P < 0.05). The correlation coefficients between neuroticism and PSY (0.552) and between psychological flexibility and PSY (0.520) were >0.50.
High-Risk Factor Sets of Occupational Stress
To explore the high-risk factor sets of PSY and PHS among medical staff, we conducted an fs-QCA that included personality, psychological flexibility, and role overload. The setgen command was used to fuzzify the d/ata to a range between zero and one without changing the distribution of the original data. In addition, the independent variables were A/a (psychological flexibility), P/p (psychoticism), E/e (extroversion), N/n (neuroticism), and R/r (role overload). The fs-QCA was carried out with PSY and PHS as the dependent variables.
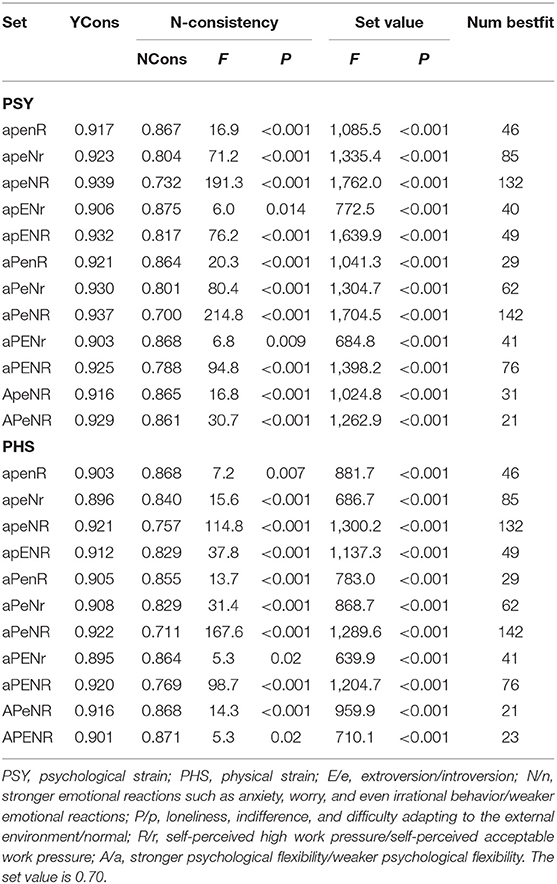
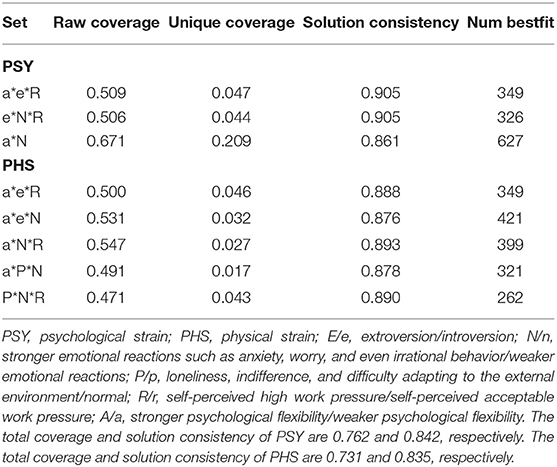
The consistency test showed that there were 12 common sets (apenR, apeNr, apeNR, apENr, apENR, aPenR, aPeNr, aPeNR, aPENr, aPENR, ApeNR and APeNR) with statistical significance in PSY (Table 3). The reduce command was used for the dimensionality reduction (Table 4). The results showed that low psychological flexibility score-introversion-high role overload (a*e*R), introversion-neuroticism-high role overload (e*N*R), and low psychological flexibility score-neuroticism (a*N) were high-risk factor sets for PSY. The above factor sets were sufficient, but not necessary for PSY (Figure 1). The coverage of different sets and the corresponding solution consistencies are listed in Table 4. The overall coverage and solution consistency values were 0.762 and 0.842, respectively.
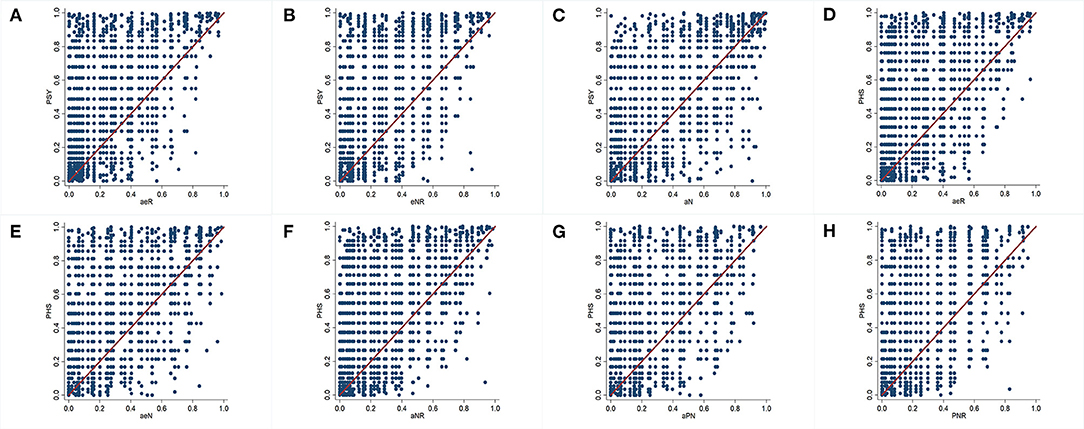
Figure 1. Sufficiency and necessity graph between different factor sets for psychological strain (PSY) and physical strain (PHS). The horizontal axis represents factor sets, and the vertical axis represents PSY or PHS. (A) Set “a*e*R” is a sufficient but not necessary condition for PSY. In other words, set “a*e*R” is a fuzzy subset of PSY. (B) Set “e*N*R” is a sufficient but not necessary condition for PSY and a fuzzy subset of PSY. (C) Set “a*N” is a sufficient but not necessary condition for PSY and a fuzzy subset of PSY. (D) Set “a*e*R” is a sufficient but not necessary condition for PHS and a fuzzy subset of PHS. (E) Set “a*e*N” is a sufficient but not necessary condition for PHS and a fuzzy subset of PHS. (F) Set “a*N*R” is a sufficient but not necessary condition for PHS and a fuzzy subset of PHS. (G) Set “a*P*N” is a sufficient but not necessary condition for PHS and a fuzzy subset of PHS. (H) Set “P*N*R” is a sufficient but not necessary condition for PHS and a fuzzy subset of PHS. E/e, extroversion/introversion; N/n, stronger emotional reactions such as anxiety, worry, and even irrational behavior/weaker emotional reactions; P/p, loneliness, indifference, and difficulty adapting to the external environment/normal; R/r, self-perceived high work pressure/self-perceived acceptable work pressure; A/a, stronger psychological flexibility/weaker psychological flexibility.
The consistency test showed that there were 11 common sets (apenR, apeNr, apeNR, apENR, aPenR, aPeNr, aPeNR, aPENr, aPENR, ApeNR, and APENR) with statistical significance in the PHS (Table 3). The reduce command was used for the dimensionality reduction (Table 4). The results showed that low psychological flexibility score-introversion-high role overload (a*e*R), low psychological flexibility score-introversion-neuroticism (a*e*N), low psychological flexibility score-neuroticism-high role overload (a*N*R), low psychological flexibility score-psychoticism-neuroticism (a*P*N), and psychoticism-neuroticism-high role overload (P*N*R) were high-risk factor sets for PHS. The above factor sets were sufficient, but not necessary for PHS (Figure 1). The coverage of different sets and the corresponding solution consistencies are listed in Table 4. The overall coverage and solution consistency values were 0.731 and 0.835, respectively.
Discussion
Medical staff are a high-risk group for occupational stress and a key population that should be considered in stress interventions. A systematic review focused on the mental health of medical staff showed that the overall prevalence of occupational stress ranged from 29.8 to 63.0%, with more severe symptoms among nurses, and female and young workers (13). During the COVID-19 pandemic, medical staff faced greater pressure and challenges than ever. At the beginning of the COVID-19 pandemic, reports stated that the scores of medical staff on various indicators of stress were significantly higher than those of the control group (38, 39). One year after the COVID-19 pandemic, a survey of medical staff in Saudi Arabia reported widespread symptoms of depression, anxiety, and stress (40).
It is generally believed that demographic factors, social psychological factors, and personality are related to occupational stress (15, 19), while excessive workload, task conflicts, and exposure to occupational hazards in the workplace are risk factors for stress (18, 41, 42). In this study, we found that personality, psychological flexibility, and role overload were associated with PSY and PHS among the medical staff. Neuroticism, psychoticism, and RO were positively correlated with occupational stress, whereas psychological flexibility and extraversion were negatively correlated with occupational stress. The results of the partial correlation analysis were consistent with those of previous studies that focused on the individual effects of specific factors (9).
From a sociological perspective, individuals are complex combinations of various characteristics. If we want to conduct interventions on occupational stress, we should first determine the combination of traits that are more prone to stress. This study further conducted in-depth discussions on occupational stress with the help of the fs-QCA. The results showed that low psychological flexibility score-introversion-high role overload, introversion-neuroticism-high role overload, and low psychological flexibility score-neuroticism are high-risk for PSY, while low psychological flexibility score-introversion-high role overload, low psychological flexibility score-introversion-neuroticism, low psychological flexibility score-neuroticism-high role overload, low psychological flexibility score-psychoticism-neuroticism, and psychoticism-neuroticism-high role overload are high-risk for PHS. The above factor sets were sufficient but not necessary conditions for occupational stress. This means that individuals with a combination of the above factors are more likely to suffer from stress than those in the non-carrier group.
During the COVID-19 pandemic, medical staff are at a higher risk than ever for mental health issues, such as occupational stress, anxiety, and burnout. For occupational stress interventions and psychological counseling, targeted and individualized measures should be taken according to the specific characteristic combinations of different individuals. In fact, a unified and universal intervention method is insufficient to fully deal with the mental health problems currently faced by the medical staff. In addition, in terms of job suitability and human resource management, the conclusions based on fs-QCA have certain benefits.
Despite its important findings, this study has some limitations. First, the cross-sectional nature of this article that prevents inference on a casualty. From an epidemiological point of view, the observed associations in our study cannot be interpreted in a causal sense. Second, the study only included role overload, personality characteristics, and psychological flexibility for fs-QCA, and did not include other factors and dimensions of occupational stress. It should be noted that including too many independent variables complicates the interpretation of the fs-QCA results, which is one of the inherent limitations of QCA. Further, fs-QCA, as a qualitative analysis method, cannot provide the quantitative effect of a single independent variable.
Conclusion
Based on the fs-QCA strategy, this study conducted an innovative approach and attempted to explore the high-risk factor set of occupational stress in medical staff, instead of being limited to the study of single-factor effects. This study provides new strategies and ideas for the exploration of occupational stress risk factors and formulation of intervention measures for medical staff during the COVID-19 pandemic.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of the West China School of Public Health, Sichuan University (No. Gwll2021070). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
LH, YLa, and LQ designed the study. LQ and YZ analyzed the data and drafted the manuscript. LQ, YZ, FJ, YLi, YLa, and LH edited the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the National Nature Science Foundation of China (No. 82073521), Scientific research fund for young teachers of Sichuan University (No. 2015SCU11009), Scientific research project of Health Commission of Sichuan Province (No. 17PJ451), and Scientific research project of Department of Education of Sichuan Province (No. 17ZB0247).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank all the participants in this study, and those all who provide help to this study.
References
1. Chou LP, Li CY, Hu SC. Job stress and burnout in hospital employees: comparisons of different medical professions in a Regional Hospital in Taiwan. BMJ Open. (2014) 4:e004185. doi: 10.1136/bmjopen-2013-004185
2. Nowrouzi B, Nguyen C, Casole J, Nowrouzi-Kia B. Occupational stress: a comprehensive review of the top 50 annual and lifetime cited articles. Workplace Health Saf. (2017) 65:197–209. doi: 10.1177/2165079916666300
3. Zhang Y, Huang L, Wang YW, Lan YJ, Zhang YG. Characteristics of publications on occupational stress: contributions and trends. Front Public Health. (2021) 9:9. doi: 10.3389/fpubh.2021.664013
4. Maharaj S, Lees T, Lal S. Prevalence and risk factors of depression, anxiety, and stress in a cohort of Australian Nurses. Int J Environ Res Public Health. (2018) 16:61. doi: 10.3390/ijerph16010061
5. Gu B, Tan Q, Zhao S. The association between occupational stress and psychosomatic wellbeing among Chinese Nurses: a cross-sectional survey. Medicine. (2019) 98:e15836. doi: 10.1097/MD.0000000000015836
6. Chirico F, Afolabi AA, Ilesanmi OS, Nucera G, Ferrari G, Sacco A, et al. Prevalence, risk factors and prevention of burnout syndrome among healthcare workers: an umbrella review of systematic reviews and meta-analyses. J Health Soc Sci. (2021) 6:465–91. doi: 10.19204/2021/prvl3
7. Magnavita N, Tripepi G, Di Prinzio RR. Symptoms in health care workers during the COVID-19 epidemic. A cross-sectional survey. Int J Environ Res Public Health. (2020) 17:5218. doi: 10.3390/ijerph17145218
8. Magnavita N, Soave PM, Antonelli M. Treating anti-vax patients, a new occupational stressor-data from the 4th wave of the prospective study of intensivists and Covid-19 (Psic). Int J Environ Res Public Health. (2022) 19:5889. doi: 10.3390/ijerph19105889
9. Chirico F, Crescenzo P, Sacco A, Riccò M, Ripa S, Nucera G, et al. Prevalence of burnout syndrome among Italian volunteers of the red cross: a cross-sectional study. Ind Health. (2021) 59:117–27. doi: 10.2486/indhealth.2020-0246
10. Crescenzo. P, Chirico. F, Ferrari. G, Szarpak. L, Nucera. G, Marciano. R, et al. Prevalence and predictors of burnout syndrome among Italian psychologists following the first wave of the COVID-19 pandemic: a cross-sectional study. J Health Soc Sci. (2021) 6:509–26. doi: 10.19204/2021/prvl5
11. Crescenzo. P, Marciano. R, Maiorino. A, Denicolo. D, D'Ambrosi. D, Ferrara. I, et al. First Covid-19 wave in Italy: coping strategies for the prevention and prediction of Burnout Syndrome (Bos) in voluntary psychologists employed in telesupport. Psychol Hub. (2021) 38:31–8. doi: 10.13133/2724-2943/17435
12. Salari N, Khazaie H, Hosseinian-Far A, Khaledi-Paveh B, Kazeminia M, Mohammadi M, et al. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum Resour Health. (2020) 18:100. doi: 10.1186/s12960-020-00544-1
13. Vizheh M, Qorbani M, Arzaghi SM, Muhidin S, Javanmard Z, Esmaeili M. The mental health of healthcare workers in the COVID-19 pandemic: a systematic review. J Diabetes Metab Disord. (2020) 19:1–12. doi: 10.1007/s40200-020-00643-9
14. Labrague LJ. Psychological resilience, coping behaviours and social support among health care workers during the COVID-19 pandemic: a systematic review of quantitative studies. J Nurs Manag. (2021) 29:1893–905. doi: 10.1111/jonm.13336
15. Lecic-Tosevski D, Vukovic O, Stepanovic J. Stress and personality. Psychiatrike. (2011) 22:290–7.
16. Tarchi L, Crescenzo P, Talamonti K. Prevalence and predictors of mental distress among Italian Red Cross Auxiliary Corps: a cross-sectional evaluation after deployment in anti-COVID-19 operations. Mil Psychol. (2022):1-14. doi: 10.1080/08995605.2022.2069983
17. Dearborn MJ, Hastings JE. Type a personality as a mediator of stress and strain in employed women. J Human Stress. (1987) 13:53–60. doi: 10.1080/0097840X.1987.9936795
18. Huang L, Zhang Y, Yao YC, Cui FF, Shi T, Wang YW, et al. Effects of personality and psychological acceptance on medical workers' occupational stress. Chin J Hyg Occup Dis. (2018) 36:519–22. doi: 10.3760/cma.j.issn.1001-9391.2018.07.011
19. McHugh JE, Lawlor BA. Social support differentially moderates the impact of neuroticism and extraversion on mental wellbeing among community-dwelling older adults. J Ment Health. (2012) 21:448–58. doi: 10.3109/09638237.2012.689436
20. Shahrour G, Dardas LA. Acute stress disorder, coping self-efficacy and subsequent psychological distress among nurses amid COVID-19. J Nurs Manag. (2020) 28:1686–95. doi: 10.1111/jonm.13124
21. Ragin CR. The Comparative Method: Moving Beyond Qualitative and Quantitative Methods: Berkeley: University of California Press (1987). 454 p.
22. Thomas J, O'Mara-Eves A, Brunton G. Using Qualitative Comparative Analysis (QCA) in systematic reviews of complex interventions: a worked example. Syst Rev. (2014) 3:67. doi: 10.1186/2046-4053-3-67
23. Kane H, Lewis MA, Williams PA, Kahwati LC. Using qualitative comparative analysis to understand and quantify translation and implementation. Transl Behav Med. (2014) 4:201–8. doi: 10.1007/s13142-014-0251-6
24. Hill LG, Cooper BR, Parker LA. Qualitative comparative analysis: a mixed-method tool for complex implementation questions. J Prim Prev. (2019) 40:69–87. doi: 10.1007/s10935-019-00536-5
25. McAlearney AS, Walker D, Moss AD, Bickell NA. Using qualitative comparative analysis of key informant interviews in health services research: enhancing a study of adjuvant therapy use in breast cancer care. J Medical Care. (2016) 54:400–5. doi: 10.1097/MLR.0000000000000503
27. Breuer E, Subba P, Luitel N, Jordans M, De Silva M, Marchal B, et al. Using qualitative comparative analysis and theory of change to unravel the effects of a mental health intervention on service utilisation in Nepal. BMJ Global Health. (2018) 3:e001023. doi: 10.1136/bmjgh-2018-001023
28. Kahwati L, Jacobs S, Kane H, Lewis M, Viswanathan M, Golin CE. Using qualitative comparative analysis in a systematic review of a complex intervention. Syst Rev. (2016) 5:82. doi: 10.1186/s13643-016-0256-y
29. Kane H, Hinnant L, Day K, Council M, Tzeng J, Soler R, et al. Pathways to program success: a Qualitative Comparative Analysis (QCA) of communities putting prevention to work case study programs. J Public Health Manag Pract JPHMP. (2017) 23:104–11. doi: 10.1097/PHH.0000000000000449
30. Warren J, Wistow J, Bambra C. Applying Qualitative Comparative Analysis (QCA) in public health: a case study of a health improvement service for long-term incapacity benefit recipients. J Public Health. (2014) 36:126–33. doi: 10.1093/pubmed/fdt047
31. Short K, Eadie P, Kemp L. Paths to language development in at risk children: a Qualitative Comparative Analysis (QCA). BMC Pediatr. (2019) 19:94. doi: 10.1186/s12887-019-1449-z
32. Giménez-Espert MDC, Prado-Gascó VJ. The role of empathy and emotional intelligence in nurses' communication attitudes using regression models and fuzzy-set qualitative comparative analysis models. J Clin Nurs. (2018) 27:2661–72. doi: 10.1111/jocn.14325
33. Guasp Coll M, Navarro-Mateu D, Giménez-Espert MDC, Prado-Gascó VJ. Emotional intelligence, empathy, self-esteem, and life satisfaction in spanish adolescents: regression vs. QCA models. Front Psychol. (2020) 11:1629. doi: 10.3389/fpsyg.2020.01629
34. Qian MY, Wu GC, Zhu RC, Zhang X. Revision of the Eysenck Personality Questionnaire Short Scale for China (EPQ-RSC). Acta Psychologica Sinica. (2000) 32:317–23. doi: 10.4236/psych.2014.513166
35. Cao J, Ji Y, Zhu ZH. Reliability and validity of the Chinese version of the Acceptance and Action Questionnaire-Second Edition (Aaq-II) in College Students. Chin Ment Health J. (2013) 27:873–7. doi: 10.3969/j.issn.1000-6729.2013.11.014
36. Li J, Lan YJ, Wang ZM, Wang MZ, Wang MC, Liu GQ. The test of occupational stress inventory revised edition. Chinese J Indus Hyg Occupat Dis. (2001) 34–7.
37. Longest KC, Vaisey S. Fuzzy: a program for performing qualitative comparative analyses (Qca) in Stata. Stata J. (2008) 8:79–104. doi: 10.1177/1536867X0800800106
38. Wu W, Zhang Y, Wang P, Zhang L, Wang G, Lei G, et al. Psychological stress of medical staffs during outbreak of COVID-19 and adjustment strategy. J Med Virol. (2020) 92:1962–70. doi: 10.1002/jmv.25914
39. Trumello C, Bramanti SM, Ballarotto G, Candelori C, Cerniglia L, Cimino S, et al. Psychological adjustment of healthcare workers in Italy during the COVID-19 pandemic: differences in stress, anxiety, depression, burnout, secondary trauma, and compassion satisfaction between frontline and non-frontline professionals. Int J Environ Res Public Health. (2020) 17:8358. doi: 10.3390/ijerph17228358
40. Almalki AH, Alzahrani MS, Alshehri FS, Alharbi A, Alkhudaydi SF, Alshahrani RS, et al. The psychological impact of COVID-19 on healthcare workers in Saudi Arabia: a year later into the pandemic. Front Psychiatry. (2021) 12:797545. doi: 10.3389/fpsyt.2021.797545
41. Lu Y, Zhang Z, Yan H, Rui B, Liu J. Effects of occupational hazards on job stress and mental health of factory workers and miners: a propensity score analysis. Biomed Res Int. (2020) 2020:1754897. doi: 10.1155/2020/1754897
Keywords: medical staff, occupational stress, fuzzy-set qualitative comparative analysis (fs-QCA), workload, personality, psychological flexibility
Citation: Quan L, Zhang Y, Jiang F, Liu Y, Lan Y and Huang L (2022) Influence of Workload, Personality, and Psychological Flexibility on Occupational Stress Among Medical Staff: A Fuzzy-Set Qualitative Comparative Analysis. Front. Public Health 10:929683. doi: 10.3389/fpubh.2022.929683
Received: 27 April 2022; Accepted: 20 June 2022;
Published: 15 July 2022.
Edited by:
Francesco Chirico, Catholic University of the Sacred Heart, ItalyReviewed by:
Pietro Crescenzo, Volunteer Military Corps, ItalyNicola Magnavita, Università Cattolica del Sacro Cuore, Italy
Copyright © 2022 Quan, Zhang, Jiang, Liu, Lan and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lei Huang, aGxzdDA2MTAmI3gwMDA0MDsxNjMuY29t
 Liming Quan
Liming Quan Yang Zhang2,3
Yang Zhang2,3 Fugui Jiang
Fugui Jiang Ying Liu
Ying Liu Yajia Lan
Yajia Lan Lei Huang
Lei Huang