
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 24 November 2022
Sec. Public Health Education and Promotion
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.928148
This article is part of the Research Topic Implementation Mapping for Selecting, Adapting and Developing Implementation Strategies View all 16 articles
 Melissa A. Valerio-Shewmaker1,2*
Melissa A. Valerio-Shewmaker1,2* Natalia I. Heredia2,3
Natalia I. Heredia2,3 Catherine Pulicken2
Catherine Pulicken2 Patenne D. Mathews2
Patenne D. Mathews2 Roshanda Chenier2
Roshanda Chenier2 Tracy L. Swoboda3,4
Tracy L. Swoboda3,4 Ella R. Garza1,2
Ella R. Garza1,2 Fernanda Velasco-Huerta2
Fernanda Velasco-Huerta2 Maria E. Fernandez2,3
Maria E. Fernandez2,3Background: Despite the availability of multilevel evidence-based interventions for blood pressure management, poor hypertension control is common among community health center patient populations across the state of Texas and the United States. Target:BPTM is a national initiative from the American Heart Association and the American Medical Association to assist healthcare organizations and care teams in improving blood pressure control rates using evidence-based approaches and recognition of organizations who have successfully integrated the program in their practice. Using the Implementation Mapping approach, we identified determinants of Target:BPTM adoption and use and developed implementation strategies to improve program uptake and implementation in Community Health Centers in Texas.
Methods: We used Implementation Mapping (IM) to identify barriers and facilitators influencing the adoption and implementation of the Target:BPTM program and develop strategies to increase program adoption and use. We recruited four clinics across four counties in Texas and assessed barriers and facilitators at the organizational level, including electronic health records and data use. We used this data to inform clinic-specific implementation strategies based on the organization capacity and priorities feedback. We developed an implementation plan and timeline designed to improve the implementation and maintenance of Target:BPTM.
Results: As part of the needs and capacity assessment, we collected data through interviews with CHC staff, examining gaps in needs and services (e.g., what do clinics need to implement Target:BPTM?), and assets to leverage. We worked with Community Health Centers to a) identify individuals who would be involved in the adoption, implementation, and maintenance of Target:BPTM, b) describe adoption and implementation actions, and c) identify barriers and facilitators influencing adoption and implementation. Together with partners from Community Health Center, we used the IM approach to identify and develop program goals, identify methods and strategies to address barriers, and create an implementation plan. Our strategies included monthly or biweekly meetings to provide technical support, reviewing program goals and timeline to ensure program implementation, progress toward reaching goals, and address quality improvement needs at each clinic site. We developed a Target:BPTM implementation protocol for each clinic based on the needs and capacity assessment, identification of technology use and capacity, and gap analysis. We reviewed Target:BPTM program strategies and self-measured blood pressure protocols tailored to the clinic patient population. We developed a collaborative plan, reviewed funding and capacity for implementation, and provided continuous quality improvement guidance. Ongoing process and impact evaluations using the Reach, Effectiveness, Adoption, Implementation, and Maintenance (RE-AIM) framework are underway.
Discussion: This paper provides an example of using Implementation Mapping to develop strategies to increase the adoption and implementation of evidence-based cardiovascular risk reduction interventions in Community Health Centers. The use of implementation strategies can increase the use of Target:BPTM in Community Health Centers and improve hypertension control.
Despite the availability of multilevel evidence-based interventions (EBI's) for blood pressure (BP) management, poor hypertension control is common among community health center (CHC) patient populations across the United States. It is estimated that almost 46.6% of the U.S. adult population aged 20 and over have high BP (i.e., systolic BP greater than 130 mmHg or diastolic BP greater than 80 mmHg) and/or are taking antihypertensive medications (1). Unscheduled physician and emergency room visits with hypertension as the primary diagnosis is of critical concern, with over 33.6 million health care and 1.1 million emergency room visits annually, costing over $131 billion each year (2). Moreover, half of all adults diagnosed with hypertension have uncontrolled hypertension and accounts for more than half a million deaths (12.7 deaths per 100,000 population) in the United States each year (3).
Considerable racial/ethnic, sex, and socio-economic disparities exist in hypertension diagnosis, treatment, and control. For example, Hispanic and Black males are disproportionally more likely to have hypertension than their female counterparts (4). Among adults with a diagnosis of hypertension, BP control is higher among non-Hispanic Whites (32%) compared with non-Hispanic Blacks (25%), non-Hispanic Asians (19%), and Hispanics (25%) (5). Further disparities are found by geographic regions, with Texas having a 32% prevalence of self-reported hypertension among adults compared to lower rates across the U.S. This reported prevalence may be an underestimation for Texas given the large uninsured and underinsured population; 18.4 percent of Texans were uninsured in 2019, double the national average, and numbers have risen due to the economic impact of COVID-19 and job losses (6).
Given these continuing health disparities, evidence based interventions addressing patient and organization level strategies to control BP in patients are highly needed. The Target:BPTM program is a national initiative from the American Heart Association (AHA) and the American Medical Association (AMA) to assist healthcare organizations and care teams improve BP control rates through the implementation of evidence-based programming and recognition of organizations with successful integration. The unique aspect of Target:BP is the focus on building community clinic capacity to implement and maintain guideline-based care and promote accurate hypertension monitoring to improve patient-level outcomes. There are other EBIs that have been designed and implemented to address different aspects of hypertension control have been successfully implemented in community and clinic settings. For example, the Million Hearts Collaboration focuses on the alignment of cardiovascular disease prevention efforts through community linkages (7), the Healthy Heart Ambassador program supports community efforts through trained, certified ambassadors who provide one-on-one and group counseling to participants (8), and the WISEWOMAN program provides tools and resources to clinics that help women understand and reduce their risk of heart disease and stroke (9). Using the Implementation Mapping approach, we identified determinants of Target:BPTM adoption and use them to develop implementation strategies to improve Target:BPTM uptake and implementation in Texas CHCs, primarily Federally Qualified Health Centers (FQHCs) and look-alikes.
The Target:BPTM program is a national initiative formed by the AHA and the AMA to aid health care organizations to improve BP control through evidence-based quality improvement and clinical redesign. The program achieves this goal by helping practices ensure accurate BP measurement, empowering providers to start or increase treatment when BP is high at 2 or more office visits (10), and promoting shared decision-making and a patient-provider partnership to support patients' BP self-management through self-measured BP (SMBP), lifestyle changes and/or medication adherence, as appropriate (11).
The program provides participating clinics patient-facing materials on BP control to raise awareness, along with tools and resources for systems and process changes at the practice and/or health system level to improve BP management (12). The program promotes the use of 6 evidence- based activities to ensure accurate BP measurement (13): 1) calibrating BP measurement devices per manufacturer recommendations, 2) ensuring semi- and fully automated BP measurement devices are validated for clinical accuracy, 3) using a structured curriculum of at least 30 min every 6–12 months to increase staff knowledge and skills related to BP measurement, 4) using an objective skills demonstration assessment to test staff skills every 6–12 months, 5) using a BP measurement protocol to obtain consistent, accurate BP measurements, and 6) posting an infographic displaying best practices for accurately measuring BP in all locations where BP is measured.
For program recognition, practices are required to submit evaluation data (14), including their total adult patient population and breakdown by age, sex, ethnicity (15), those with hypertension, and those with controlled hypertension. Instructional videos and a data collection worksheet are provided to assist practices with collecting and submitting the evaluation data. The program recognizes organizations committed to improving BP control utilizing a tier system of recognition (Table 1) (16). Practices that achieve these successes are acknowledged by the AHA and AMA via various platforms (e.g., website, AMA and AHA national meetings) and provided with both promotional digital assets (e.g., digital seal for emails, social media messaging) and office items (e.g., plaque) to indicate achievement. While several of the activities recommended as part of the Target:BPTM program can be considered implementation strategies themselves (training staff in BP measurement), the need to develop strategies to implement the Target:BPTM program as a whole remained. Thus, we used Implementation Mapping for this purpose.
Implementation Mapping, a systematic process for developing or choosing implementation strategies is based on the Intervention Mapping, a protocol to guide the development of multi-level interventions (17). Specifically, Implementation Mapping expands on step 5 of Intervention Mapping (development of an implementation plan) and integrates both implementation science and health promotion to increase understanding of factors influencing implementation within a specific setting, and to guide the development of implementation strategies to increase intervention adoption, use, and sustainment (18). Implementation Mapping includes five tasks: 1) conduct an implementation needs and assets assessment and identify program implementers, 2) identify adoption and implementation outcomes, determinants, performance objectives (this includes the specific tasks or sub-behaviors required to carry out program adoption, implementation, and maintenance objectives), and develop matrices of change objectives (defined as the changes required for each determinant that will influence success of each performance objective), 3) select theory-based methods and identify practical applications associated with these methods, 4) produce implementation protocols and materials, and 5) evaluate implementation outcomes (18). For this project, we used an iterative process to identify barriers and facilitators influencing the adoption and implementation of the Target:BP program within the partner CHCs, and to develop a comprehensive plan for program integration (Figure 1).
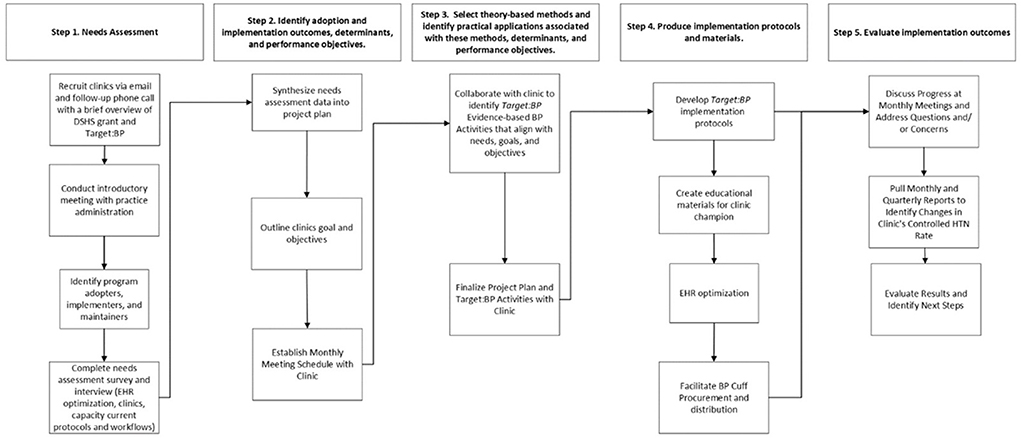
Figure 1. This workflow was created using the implementation mapping steps from Bartholomew Eldredge et al. (17). The adoption and implementation performance objectives examples influencing the adoption and implementation of the Target:BPTM shown in this table came from the project planning. DSHS, Department of State Health Services; HER, Electronic Health Record; HTN, Hypertension; BP, Blood Pressure.
We recruited four clinics from both rural and urban counties within Public Health Regions (PHR) 2/3 and 11, representing the greater Dallas-Fort Worth area and the Rio Grande Valley area of Texas, respectively. In collaboration with clinical leadership from the selected clinics and the research team, we used a team-based approach to promote and implement the Target:BP program. Our goal was to recruit a total of 5 clinics, a total of 20 clinics were contacted by email and telephone. Clinics were identified by location, previous history in partnership with the university, and by searching for Federally Qualified Health Centers serving the region. There were no financial incentives provided to the participating clinics.
As part of the recruitment, we completed discussions with the clinic office manager and or senior leadership to ensure decision making authority and need, priority, and interest in the program. The onboarding process differed at each clinic site. After the introductory meeting (i.e., within the following 2 weeks) the team and clinic partners completed the Needs Assessment survey and a program and organization capacity review. For each clinic, we first identified implementers and a program champion or primary contact to participate in the Implementation Mapping process to ensure each step was tailored to the clinic setting and the patient's needs. To recruit clinics, we followed a 4-step process: (1) identified clinics by email and follow-up phone call with a brief overview of the overall contract goals and Target:BP, (2) once agreed to serve as a site, we held an introductory meeting with clinic administration to learn about current practices, (3) conducted a needs assessment, and (4) synthesized information from the needs assessment to present to our clinic partner as part of our adoption/implementation step.
We began by assessing the clinic's EHR, hypertension practices, and collection of hypertension management data. Since utilization of EHR technology is an anchor for successful implementation of the Target:BP program, each clinic partner agreed to share EHR data and information with the UTHealth team. Thus, each clinic team collected data on-site and shared the data with the UTHealth team; the UTHealth team then reviewed and synthesized these data to inform discussions and assist each of the clinics with the EHR optimization needed to support and track the implementation of the Target:BP program.
We used a standardized needs assessment instrument using both qualitative and quantitative measures to collect data at the start of the program. As part of this needs and capacity assessment, we conducted interviews with the staff at each clinic, examining gaps in needs and services (e.g., what do clinics need to implement Target:BPTM), and assets to leverage. Additional data and reporting occurred during the partner clinic's leadership and the research team monthly meetings to identify adoption and implementation outcomes while integrating strategies to enhance implementation of Target:BPTM per CHC goals.
Following the limited data sharing agreements, each of the clinics provided the UTHealth team with quarterly data reports. Each of the clinics extracted data form the EHR and shared with UTHealth via secure email. The data reports helped us estimate baseline control hypertension rates and assess improvements over time as well as were included in funder reports. Additionally, as part of the Target:BP recognition program, each site submits annual data on hypertension rates and the activities completed the year prior.
For each CHC, we completed a needs assessment to determine organizational, patient, and capacity needs. We payed particular attention to barriers and facilitators at the organizational level to ensure the success and integration of changes within the CHC setting. We identified specific barriers and facilitators for adoption and implementation of Target:BPTM including action steps for adoption and implementation of Target:BPTM (e.g., who would complete what to implement) and determinants. Additionally, we developed and tailored clinic-specific implementation strategies which were informed by theory, empirical evidence, and organizational implementation team, including the program champion, leadership and others identified at the organization, feedback. Working in partnership with each of the four CHCs, we developed a tailored implementation plan and timeline designed to promote and enhance fidelity of implementation to promote maintenance of Target:BPTM at each clinic.
To guide the successful adoption of the Target:BP program, we had to understand each clinic's organizational capacity and identify program adopters, implementers, and maintainers. Thus, the first task involved conducting a thorough needs and capacity assessment. We initially contacted each of the selected CHC's leadership via email or telephone. During this initial contact, we provided the CHC with a general overview and scope of the Target:BP program as well as an introduction of the services our research team could provide to their clinics to facilitate the implementation of Target:BP. It is important to note that unlike many implementation research studies where participating clinics have previously agreed to implement a program, the approach described here included clinics who had not yet agreed to adopt or implement Target:BP.
Once the CHC was engaged and interested, an introductory virtual (e.g., Zoom or Microsoft Teams) meeting with the clinic's leadership was scheduled to present an overview of the Target:BP program (e.g., program participation levels, Target:BPTM evidence-based activities for recognition, enrollment, and registration). During the virtual meeting, we also discussed clinical characteristics and practices and the patient population (e.g., type of organization, number of sites and providers, patient volume and sociodemographics, etc.). Clinics then identified and set goals for implementation of the program including EHR optimization, and hypertension management and prevention. We also used this opportunity to identify clinical staff and members of the clinical leadership team (i.e., Chief Operating Officer, IT/Data Analyst, Practice Administrator) who would be potential program adopters, implementers, and maintainers.
We then worked with the CHCs to identify their Target:BPTM team, that is, the individuals who would be involved in the adoption and implementation of the Target:BPTM program, to describe the adoption and implement actions, and identify barriers and facilitators from the needs assessment. Strategies were collaboratively developed to identify patient needs and program goals for their unique setting, and to develop methods and strategies to inform the implementation of Target:BPTM. We developed a Target:BPTM implementation protocol based on the needs assessment for each clinic based on the needs and capacity assessment, identification of technology capacity and use, and gap analysis findings. We reviewed Target:BPTM program strategies and SMBP protocols tailored to the clinic patient population. Details on clinic characteristics and identified patients' needs were used to address the multi-level needs for dissemination and implementation of this evidence-based program (Table 2).
The next steps included completion of a Memorandum of Understanding (MOU), needs assessment, project plan development, and program delivery. After completion of the MOU between the designated CHC and UTHealth, a needs assessment survey was administered via Qualtrics to determine the CHC's hypertension workflow, the use of clinical decision support (CDS) tools for hypertension-related practices (i.e., patient identification, treatment, and management), recommendation of evidence-based activities (i.e., self-measured BP monitoring [SMBP]), patient portal usage, as well as hypertension outcomes related to BP control.
Identifying the CHC's implementation capacity was a critical step since many times, the CHC's staff may not have time to assess and identify all variables needed for the implementation of an EBI. These tasks were completed in collaboration with the CHC and the UTHealth team, which allowed for real-time data sharing to inform the tailoring of the Target:BP program implementation. Following these first steps, an in-depth interview was scheduled with clinical leadership to further assess current workflows and data reporting, and identify the CHC's barriers and facilitators for the implementation of Target:BP. After completion of the needs assessment, a follow-up meeting was scheduled with the CHC's stakeholders to discuss results, identify areas for improvement and initiate a project implementation plan.
As noted above, the initial meeting with each of the clinics and follow-up meetings were conducted by videoconference, and the scheduling and coordination were completed by email and based on the availability of the clinic sites. Communication with each of the clinics related to activities and goals between program implementation meetings was completed by email and phone calls. Specifically, UTHealth scheduled and provided support to each of the clinics and the program consultants to ensure coordination and facilitation of meetings and focus on activities, partnerships and goals. At each clinic site, attendance at meetings usually included the clinic's leadership, management team and implementers including medical directors, nurse team members, patient navigators, operation managers and information technology team members.
To facilitate the development of a project implementation plan that aligned with each CHC's hypertension management goals, the UTHealth team created a project planning guide to identify gaps in hypertension management and address specific priorities and tasks for program implementation. In collaboration with each of the CHC's program adopters and implementers, the project plan was finalized by the UTHealth research team and the CHC's leadership. The planning team identified adoption and implementation outcomes for adopters, implementers and maintainers (e.g., clinic's leadership, providers, administrative staff, non-physician team members [community health workers, physicians' assistants, etc.]) for each CHC see implementation outcomes for each (Table 3). The team worked together in the creation of performance objectives to identify “who needs to do what to ensure that the program is adopted, implemented, and maintained?” For example, the CHC's leadership (decision-makers) agree to participate in the Target BP program by enrolling in the Target:BP program with an AHA representative. These performance objectives served as a roadmap essential for the adoption, implementation, and maintenance of the Target:BP program.
After the identification of program outcomes and performance objectives for each of the CHC's stakeholder groups, we defined determinants for Target:BP program implementation (Table 4).
These determinants are derived from theoretical constructs that aligned with the barriers and facilitators identified in the needs assessment. The UTHealth team completed a thorough literature review related to Target:BP program implementation and similar evidence-based BP control programs. At this point, we used literature to inform the identification of the priority determinants given the results from each of the CHC's needs assessment, allowing us to identify potential determinants that could impact the CHC stakeholder group's ability to achieve their outcomes. Once determinants were reviewed by the teams, we created the change matrices. The matrices of change objectives for each CHC's stakeholder group list the various changes in each determinant necessary to achieve the associated performance objective. The use of these matrices helped ensure that content and messaging for the implementation of Target:BP addressed the most salient performance objectives and determinants to facilitate successful implementation.
While each clinic implemented the program based on their own goals and capacity, the team recognized some key factors that promoted implementation including the collaboration of change agents, such as the clinic site leadership team and stakeholders that were aware of the community and organization capacity as well as could identified potential resources.
After defining the necessary changes needed within the CHCs for successful Target:BP program implementation, we then identified evidence- and theory-based strategies to address these changes at the provider and administrative levels, and developed tables highlighting methods and practical applications (Table 3). These strategies addressed determinants identified using theoretical constructs from the social cognitive theory and organizational level frameworks. We reviewed the behavioral and implementation science literature to ensure that the appropriate methods were identified to facilitate change and address determinants and change objectives for each CHC. For Target:BP, these methods and applications were developed from existing materials, messages, and recommended practices. For each of the recommended practices and steps of Target:BP, we identified how their implementation would address determinants and change objectives. This facilitated CHCs' staff training, identification of materials needed for Target:BP implementation, and strategies to gain access to the materials needed. For example, in one CHC we found that while training addressed knowledge, self- efficacy and perceived norms for BP monitoring and capacity, the CHC did not have the proper equipment to implement the Target:BP protocols at the patient level. Specifically, many of the CHCs could not afford the BP cuffs for the necessary patient population and cuffs were not available in all the needed sizes (e.g., XL BP cuffs). However, we were able to work with other partners (i.e., AHA) to identify potential sources for the equipment at discounted prices. Implementation Mapping facilitated the review of contextual factors that influenced implementation and allowed for CHCs to identify resources and other actions needed to properly implement Target:BPTM.
Working together with the CHC's leadership and implementation team members, we developed protocols and activities needed for the implementation of key Target:BP objectives. These activities included training and re-training of CHC's staff on proper BP techniques, EHR optimization, and the development of tailored Target:BP materials. While Target:BP materials may be readily available for adaptation through the AHA (i.e., targetbp.org), we worked with the CHCs to ensure proper wording and design of certain materials (e.g., flyers on proper BP techniques) to target the CHC's hypertension management goals, clinical setting, and patient population. To ensure the appropriate selection of the intended audience, target determinants, change objectives, and material content, we closely collaborated with the CHCs in the development of protocols, workflows, and materials used for the implementation of Target:BP. The workflows identified potential adopters, implementers, and maintainers and visually depicted how Target:BP would be integrated into the CHC's current or new hypertension care management process. These workflows were then communicated and used to guide Target:BP implementation at the clinic. We carefully reviewed with the CHCs to ensure future uptake and dissemination and promote adoption and use as well as to help with future implementation and impact evaluation.
Ongoing evaluation of implementation outcomes for Target:BP use within CHCs has identified several key areas to improve reach, engagement, and impact, including the integration of key clinic specific team members and community partners to promote use of data and inform strategies to implement at each clinic. The collection of process data including reach of patients in most need will allow the team to identify the impact of implementation strategies as well as essential preconditions and changes at the CHC level that facilitated implementation, fidelity, and reach of the patient population. We expect that CHC organizational process evaluation and impact data will allow us to better identify barriers and enabling factors for Target:BP adoption, implementation, and sustainability outcomes. Once we complete the evaluation, we will use findings to improve Target:BP delivery and for interpreting patient-level outcomes. We will be able to better identify whom the program reached, assess fidelity of implementation, and determine organizational factors that influence intervention, adoption, use, and or maintenance (Figure 2).
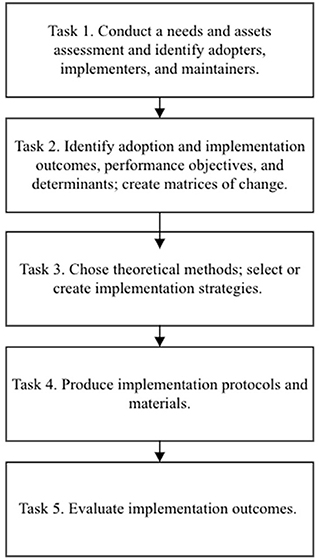
Figure 2. Implementation mapping process from Fernandez et al. (18).
The implementation of the Target:BP program provides an example of the use of Implementation Mapping for the development and adoption of evidence-based strategies to increase successful implementation of evidence-based programs within CHCs. The use of implementation strategies can increase the use of Target:BPTM in CHCs (organizational level) and improve hypertension control outcomes (patient level). The steps of Implementation Mapping allowed us to carefully integrate and address the specific needs of CHCs at their pace while addressing the importance of fidelity and reach of not only patients, but also adopters and implementers, to ensure success.
Team meetings ensured that both the CHC's leadership and the UTHealth team listened to implementer needs and facilitated changes in information technology (IT), EHR, and training. This fostered the development of successful training to address the needs of facilitators as well as strategies to overcome adoption and implementation barriers encountered by the CHC teams including IT, managers, nurses, and other health care providers. The Target:BP implementation at CHCs allowed the research team to test the conceptual and practical gaps between identifying barriers and facilitators, and developing strategies for immediate communication and problem solving to strengthen and increase the ease for adoption and implementation of Target:BP. The CHCs identified and addressed changes in implementation to contextual factors that allow for greater learning, openness, and identification of CHC setting needs to impact health and quality of life of patients.
Given the ongoing challenges to implement EBIs successfully, the use of Implementation Mapping may help (a) increase the confidence, capacity, and readiness of CHCs to use EBIs by elucidating mechanisms for change within their CHC, (b) inform the planning process to ensure the identification of determinants of change, and (c) select implementation strategies with the greatest potential for impact on health outcomes over time.
As this is an ongoing program, we expect that our iterative approach to Implementation Mapping across additional CHCs will allow us to reach and expand our knowledge of the use of Implementation Mapping as a planning framework for the successful delivery of EBIs aimed to improve health. Ongoing process and impact evaluations using the Reach, Effectiveness, Adoption, Implementation, and Maintenance framework (RE-AIM) are underway to evaluate the Target:BPTM program (19).
It is well documented that EBIs may not be adapted or adopted in settings that may most benefit from their impact (20–23). However, Implementation Mapping outlines a practical step-by-step method for planning of implementation to optimize reach, appropriateness, and impact over time, and that simultaneously will build capacity at CHCs and similar settings to adopt, implement and sustain evidence- and guidelines-based practices to improve health outcomes.
The CHCs implementing the Target:BPTM program will have tools to ensure maintenance and reach of patients with the most need.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by University of Texas Health Science Center Houston, Institutional Review Board. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
This publication was supported by the Centers for Disease Control and Prevention of the U.S. Department of Health and Human Services (HHS).
We would like to acknowledge our partners the Texas Department of State Health Services (DSHS), American Heart Association (AHA), Amistad Community Center, HHM, HOPE Clinic of Waxahachie, and Urban Inter-Tribal Center of Texas for their support.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by Texas Department of State Health Services (DSHS), CDC/HHS, or the U.S. Government.
1. Whelton PK, Carey RM, Aronow W, Casey DE, Collins KJ, Himmelfarb CD, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American heart association task force on clinical practice guidelines. AHA. (2018) 71:e13–115. doi: 10.1161/HYP.0000000000000065
2. Kirkland EB, Heincelman M, Bishu KG, Schumann SO, Schreiner A, Axon RN, et al. Trends in Healthcare Expenditures Among US Adults With Hypertension: National Estimates, 2003–2014. J Am Heart Assoc. (2018) 7:e008731. doi: 10.1161/JAHA.118.008731
3. Mueller M, Purnell TS, Mensah GA, Cooper LA. Reducing racial and ethnic disparities in hypertension prevention and control: what will it take to translate research into practice and policy? Am J Hypertens. (2015) 28:699–716. doi: 10.1093/ajh/hpu233
4. Centers for Disease Control Prevention. Multiple Cause of Death Data on CDC WONDER. Available online at: https://wonder.cdc.gov/controller/datarequest/D77 (accessed February 8, 2022).
5. Centers for Disease Control Prevention. Facts About Hypertension. (2021). Available online at: https://www.cdc.gov/bloodpressure/facts.htm (accessed February 8, 2022).
6. Johnston EM, Kenney GM, Gonzalez D, Wengle E. Employer-sponsored insurance access, affordability, and enrollment in 2018 state and national estimates and implications for low-income working families. Urban Institute (2020). p. 1–69.
7. Centers for Disease Control and Prevention. Blood Pressure Control: Million Hearts. (2022). Available online at: https://millionhearts.hhs.gov/about-million-hearts/optimizing-care/bp-control.html (accessed February 8, 2022).
8. YMCA. Blood Pressure Self-Monitoring. Available online at: https://www.ymca.org/what-we-do/healthy-living/fitness/self-monitoring (accessed February 8, 2022).
9. Centers for Disease Control Prevention. Well-Integrated Screening and Evaluation for WOMen Across the Nation. (2020). Available online at: https://www.cdc.gov/wisewoman/index.htm (accessed February 8, 2022).
10. American Heart Association, American Medical Association. Act Rapidly. Target:BP. Available online at: https://targetbp.org/Blood-Pressure-Improvement-Program/Control-BP/Act-Rapidly/ (accessed February 13, 2022).
11. American Medical Association, American Heart Association. Partner with Patients. Target:BP. Available online at: https://targetbp.org/Blood-Pressure-Improvement-Program/Control-BP/Partner-with-Patients/ (accessed February 13, 2022).
12. American Heart Association. Target:BP Fact Sheet. Available online at: http://www.heart.org/idc/groups/heart-public/@wcm/@mwa/documents/downloadable/ucm_482030.pdf (accessed February 13, 2022).
13. Evidence-Based BP Activities Recognition Resources Examples. (2021). Available online at: https://targetbp.org/tools_downloads/recognition-resources-and-examples/ (accessed February 13, 2022)
14. American Heart Association, American Medical Association. Data Collection Worksheet. (2021). Available online at: https://targetbp.org/tools_downloads/data-collection-worksheet/ (accessed February 12, 2022)
15. American Heart Association, American Medical Association. Race & Ethnicity Data Collection Essentials. (2021). Available online at: https://targetbp.org/tools_downloads/race-ethnicity-data-collection-essentials/ (accessed February 13, 2022).
16. American Heart Association, American Medical Association. Target: BP Recognition Fact Sheet 2022. (2021). Available online at: https://targetbp.org/tools_downloads/target-bp-recognition-fact-sheet/ (accessed February 13, 2022).
17. Bartholomew Eldredge LK. Planning Health Promotion Programs: An Intervention Mapping Approach. 4th Ed. San Francisco, CA: Jossey-Bass & Pfeiffer Imprints, Wiley (2016). p. 1.
18. Fernandez ME, ten Hoor GA, van Lieshout S, Rodriguez SA, Beidas RS, Parcel G, et al. Implementation mapping: using intervention mapping to develop implementation strategies. Front Public Health. (2019) 7:158. doi: 10.3389/fpubh.2019.00158
19. Gaglio B, Shoup JA, Glasgow RE. The RE-AIM framework: a systematic review of use over time. Am J Public Health. (2013) 103:e38–46. doi: 10.2105/AJPH.2013.301299
20. Card JJ, Solomon J, Cunningham SD. How to adapt effective programs for use in new contexts. Health Promot Pract. (2011) 12:25–35. doi: 10.1177/1524839909348592
22. Solomon J, Card JJ, Malow RM. Adapting Efficacious Interventions: advancing translational research in HIV prevention. Eval Health Prof. (2006) 29:162–94. doi: 10.1177/0163278706287344
Keywords: implementation mapping, Target:BP, hypertension, community health centers, evidence-based interventions, hypertension management
Citation: Valerio-Shewmaker MA, Heredia NI, Pulicken C, Mathews PD, Chenier R, Swoboda TL, Garza ER, Velasco-Huerta F and Fernandez ME (2022) Using implementation mapping for the adoption and implementation of Target:BP in community health centers. Front. Public Health 10:928148. doi: 10.3389/fpubh.2022.928148
Received: 25 April 2022; Accepted: 27 October 2022;
Published: 24 November 2022.
Edited by:
Melanie Boeckmann, University of Bremen, GermanyReviewed by:
Debbie L. Humphries, Yale University, United StatesCopyright © 2022 Valerio-Shewmaker, Heredia, Pulicken, Mathews, Chenier, Swoboda, Garza, Velasco-Huerta and Fernandez. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Melissa A. Valerio-Shewmaker, TWVsaXNzYS5BLlZhbGVyaW9AdXRoLnRtYy5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.