- 1Department of Pathology, Taizhou Central Hospital (Taizhou University Hospital), Taizhou, China
- 2College of Pharmaceutical Sciences, Zhejiang University, Hangzhou, China
- 3School of Public Health, Hangzhou Medical College, Hangzhou, China
- 4Department of Non-communicable Chronic Disease Control and Prevention, Taizhou Municipal Center for Disease Control and Prevention, Taizhou, China
- 5Department of Cancer Prevention/Zhejiang Cancer Institute, Cancer Hospital of the University of Chinese Academy of Sciences (Zhejiang Cancer Hospital), Hangzhou, China
- 6Institute of Basic Medicine and Cancer (IBMC), Chinese Academy of Sciences, Hangzhou, China
- 7Department of Preventative Medicine, School of Medicine, Ningbo University, Ningbo, China
Objectives: While timely assessment of long-term survival for patients with cervical cancer is essential for the evaluation of early detection and screening programs for cervical cancer, those data are extremely scarce in China. We aimed to timely and accurately assess long-term survival for patients with cervical cancer in eastern China, using cancer registry data from Taizhou, eastern China.
Methods: Patients diagnosed with cervical cancer during 2004–2018 from four cancer registries with high-quality data from Taizhou, eastern China were included. A period analysis was used to calculate the 5-year relative survival (RS) overall and on stratification by sex, age at diagnosis, and region. Additionally, the projected 5-year relative survival (RS) of patients with cervical cancer during 2019–2023 was evaluated, using a model-based period analysis.
Results: Overall 5-year RS for patients with cervical cancer during 2014–2018 reached 90.9%. When stratified by age at diagnosis, we found a clear age gradient for 5-year RS, declining from 95.6% for age <45 years to 68.7% for age >74 years, while urban areas had higher 5-year RS compared to rural areas (92.9 vs. 88.6%). We found a clear increasing trend of 5-year RS during 2004–2018 overall and on stratification by region and age at diagnosis. The projected overall 5-year RS is expected to reach 94.2% for the period 2019–2023.
Conclusions: We found that, for the first time in China, using period analysis, the most up-to-date (during 2014–2018) 5-year RS for patients with cervical cancer reached 90.9%. Our data have important implications for the timely evaluation of early detection and screening programs for patients with cervical cancer in eastern China.
Introduction
Cervical cancer ranks as the second most common type of cancer in women and predominantly occurs in postmenopausal women in less developed countries (1–3). According to estimates by GLOBOCAN 2018, ~570,000 women developed cervical cancer and an estimated 311,000 deaths occurred in 2018 (3.2% of all female cancer cases) (4). Cervical cancer is also one of the most common types of cancer in women in China, comprising one-third of global new cases of cervical cancer (5). While the incidence of cervical cancer in China increased from 3.06 per 100,000 in 1989 to 15.3 per 100,000 in 2014 (6, 7), a high incidence rate of cervical cancer was found in rural areas of the central and western regions of China (2, 7, 8), which could be mainly attributed to the absence of effective screening and vaccinations against human papillomavirus (HPV) before 2017.
Cervical cancer is associated with HPV infection due to sexual activity and reproductive factors (1, 2, 9). Declining incidence and mortality rates of cervical cancer are mainly found in Europe, Australia/New Zealand, and North America (4), which could be mainly due to the successful implementation of population-based cytological screening programs. Long-term survival estimates assessed using population-based cancer registry data are essential for the evaluation of cancer burden. A 5-year relative survival (RS) is the most important index for assessing cancer burden and is essential for the evaluation of early detection and screening programs for cervical cancer, which shall be as up to date as possible. Studies of 5-year RS data on patients with cervical cancer mainly involved the Western population, such as Germany and the United Kingdom (1, 10, 11), while data on the Chinese population are scarce (12).
Because traditional cohort and complete methods use 5-year follow-up data, the approaches may have a 5-year delay, at least for survival estimates (in addition to other time requests for data collection, calculation, and publication). Period analysis, which does not require 5-year follow-up data to calculate survival estimates, is the gold standard for the assessment of long-term survival of patients with cancer using data from population-based cancer registries and has been widely used in the Western populations (10, 13–15). However, its application in China has been scarce. Our group found, for the first time, by systematically using period analysis and cancer registry data from eastern China, that period analysis is superior to traditional cohort and complete methods, which can provide more up-to-date precise estimates of long-term survival overall and on stratification by sex, age at diagnosis, region, and cancer sites (including cervical cancer) (16).
In the current study, we aimed to provide the most up-to-date (during 2014–2018) estimates of 5-year RS for patients with cervical cancer from the Chinese population using period analysis and population-based cancer registry data from Taizhou city, eastern China. We also aimed to predict 5-year RS for the upcoming 2019–2023 period using the data during 2004–2018 and a model-based period analysis.
Methods
Data Sources
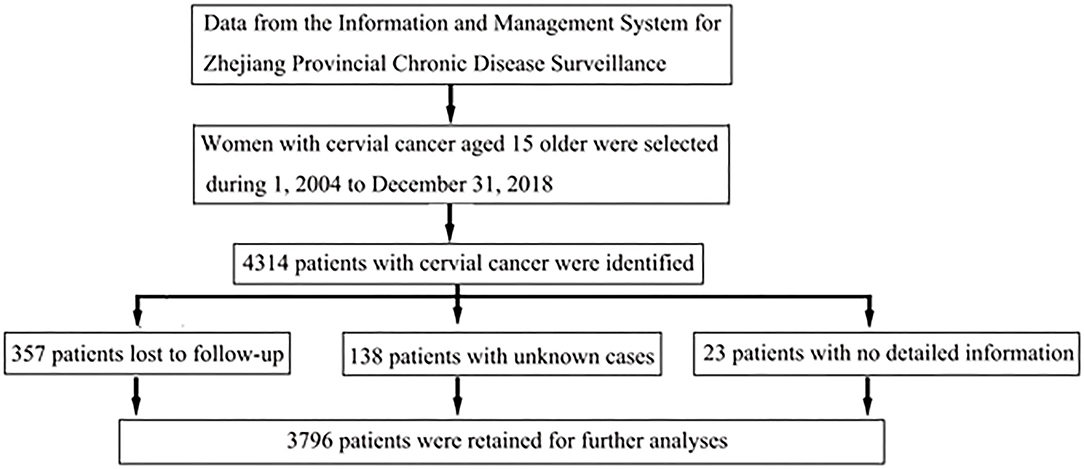
The Information and Management System for Zhejiang Provincial Chronic Disease Surveillance was a platform for monitoring the incidence and mortality rates of chronic diseases (including cancer) for inhabitants living in Zhejiang province. This population-based cancer surveillance system was used to assess incidence rates for cancer from nine registries in Taizhou. According to the inclusion criteria on the proportions of cases notified by death certificate only (DCO) under 13% throughout the study period, data from four (Luqiao, Yuhuan, Xianju, and Wenling) out of nine registries from the Taizhou region were included for further analyses. Women aged 15 or older when diagnosed with cervical cancer from 1 January 2004 to 31 December 2018 were included in this study. Mortality follow-up concerning vital status was available until the end of 31 December 2018. Using the ICD-10 code C53, we identified a total of 4,314 patients with cervical cancer, and among them, 357 patients lost to follow-up, 23 patients with no detailed information, and 138 patients with unknown cases were eventually excluded. Thus, 3,796 cases were retained for further analyses (Figure 1).
Statistical Analyses
Throughout this study, relative survival (RS), which represents disease-specific survival within a patient population where cancer is the only cause of death, was used to present long-term survival estimates. The RS is derived as the ratio of absolute survival of patients with cancer to the expected survival of individuals corresponding to the patients with cancer with similar characteristics in the calendar period of observation. Throughout this article, 5-year RS estimates for patients with cervical cancer were calculated as the ratio of the observed survival in the patient group with cervical cancer and the expected survival from a comparable group in the general population (2) (Supplementary Material). Estimates of expected survival were derived using the Ederer II method from the life table of the population of four cities of Taizhou (Luqiao, Yuhuan, Xianju, and Wenling). The model-based period analysis makes full use of the data from the cancer registry system and improves the accuracy and timeliness of survival analysis. The analyses were carried out by use of the Generalized Linear Model (GLM) function and the package “period” of R version 3.13 (R Foundation for Statistical Computing, Vienna, Austria) (17), improving the accuracy and timeliness of period survival analysis.
Results
Basic Characteristics of Patients With Cervical Cancer
The basic characteristics of patients diagnosed with cervical cancer during 2004–2018 are presented in Table 1. Overall, we included 3,796 patients with cervical cancer, consisting of 287 cases during 2004–2008, 1,387 during 2009–2013, and 2,122 during 2014–2018. While the average age at diagnosis was 53.2 years, age at diagnosis <45 years accounted for only 25%, and 56% of the patients ranged from 45 to 64 years. Only 14% of patients were from an urban area, compared to 86% of them from a rural area.
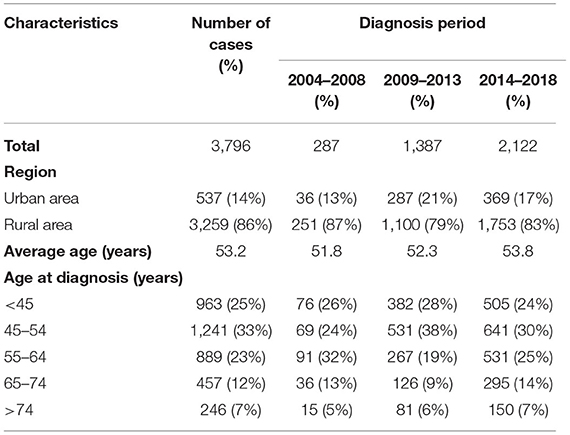
Table 1. Basic characteristics of patients diagnosed with cervical cancer during 2004–2018 from Taizhou, eastern China.
5-Year Relative Survival for Patients With Cervical Cancer During 2014–2018
Overall, 5-year relative survival rate during 2014–2018 reached 90.9% (Table 2). When stratified by age at diagnosis, we found an age gradient, with 5-year RS decreasing to 95.6% for age <45 years and to 68.7% for age >74 years. Urban areas had a higher 5-year RS, compared to rural areas (92.9 vs. 88.6%).
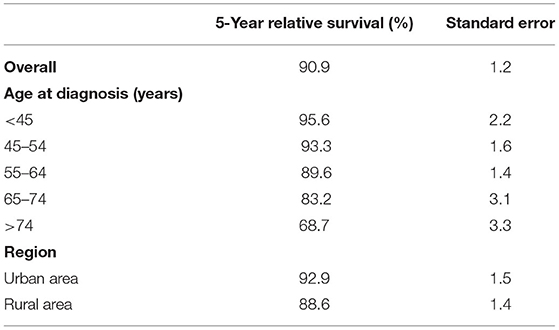
Table 2. Five-year relative survival of patients with cervical cancer during 2014–2018 in Taizhou, eastern China.
Trends of 5-Year RS During 2004–2018 and Projection During 2019–2023
We found a clear increasing trend of 5-year RS during 2004–2018 (2004–2008, 2009–2013, and 2014–2018) overall and on stratification by region (Figure 2) and age at diagnosis (Figure 3).
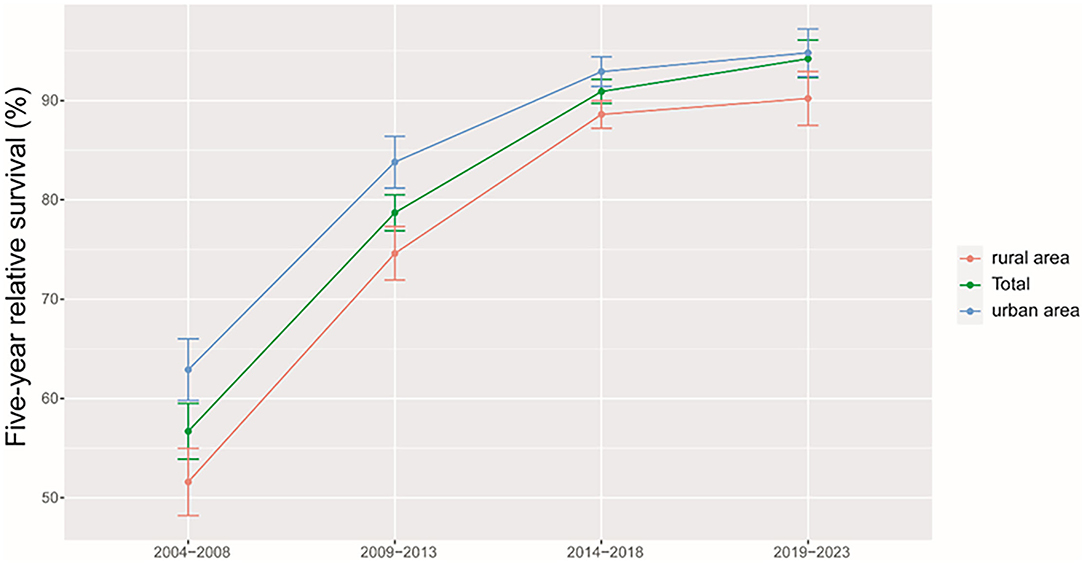
Figure 2. Trends of 5-year relative survival for patients with cervical cancer from Taizhou, eastern China during 2004–2008, 2009–2013, 2014–2018, and 2019–2023 by region (urban areas vs. rural areas).
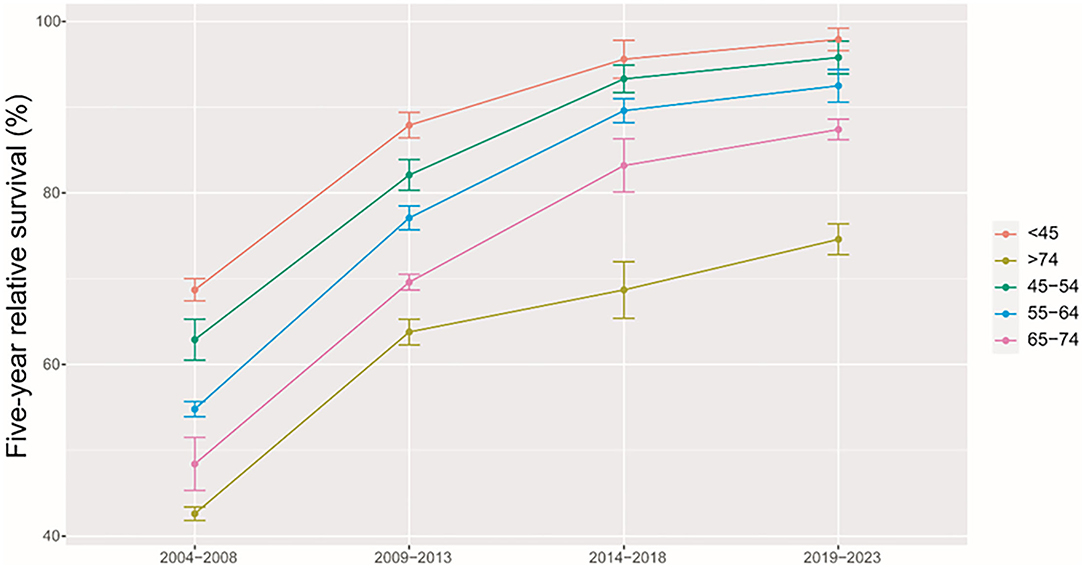
Figure 3. Trends of 5-year relative survival for patients with cervical cancer from Taizhou, eastern China during 2004–2008, 2009–2013, 2014–2018, and 2019–2023 by age at diagnosis.
Using the data of 5-years RS during 2004–2018 and a model-based period analysis, we projected that the overall 5-year RS during 2019–2023 could reach 94.2% (Table 3). When stratified by age at diagnosis, we also found an age gradient, with 5-year RS decreasing to 97.9% for age <45 years and to 74.6% for age >74 years. Urban areas also had a higher 5-year RS compared to rural areas (94.8 vs. 90.2%).
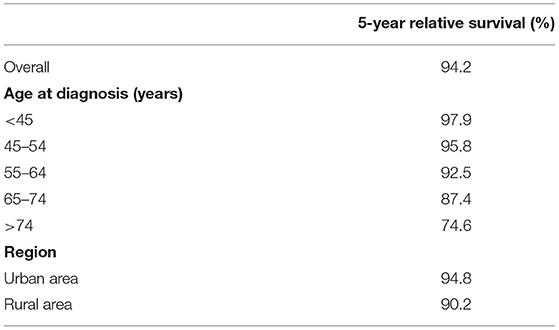
Table 3. Projected 5-year relative survival of patients with cervical cancer during 2019–2023 in Taizhou, eastern China.
Discussion
We provided, for the first time in China, using period analysis, the most up-to-date (during 2014–2018) estimates of 5-year RS for patients with cervical cancer from Taizhou, eastern China, reaching 90.9%. When stratified by age at diagnosis, we found a clear age gradient for 5-year RS, declining to 95.6% for age <45 years and to 68.7% for age >74 years, while urban areas had higher 5-year RS compared to rural areas (92.9 vs. 88.6%). We found a clear increasing trend of 5-year RS during 2004–2018 overall and on stratification by region and age at diagnosis. Additionally, we estimate that the overall 5-year RS during 2019–2023 could reach 94.2%, using the data during 2004–2018 and a model-based period analysis.
We found that a 5-year RS during 2014–2018 for patients with cervical cancer from Taizhou, eastern China reached 90.9%. To our knowledge, this is the most up-to-date 5-year RS for Chinese patients with cervical cancer. Indeed, substantial improvements in survival for patients with cervical cancer could be likely attributed to improvements in surveillance, screening, and early detection. In our study, 58% of patients were diagnosed at <55 years (33% for 45–54 years), consisting of previous reports of peak incidence ranging 40–60 years old (12, 18). We found a clear age gradient for 5-year RS, declining to 95.6% for age <45 years and to 68.7% for age >74 years, which is in line with the previous report of a strong increase in mortality for those aged >75 years old (19).
We found that urban areas had higher 5-year RS compared to rural areas (92.9 vs. 88.6%). While the HPV vaccine was introduced into China in 2017, women in rural areas usually married at a young age and had an increased risk of HPV infection. Additionally, women in rural areas had limited access to screening programs for cervical cancer compared to women in urban areas. However, survival differences by region may narrow down shortly along with the implementation of China's rural cooperative medical system (20, 21).
We found a clear increasing trend of 5-year RS during 2004–2018 overall and on stratification by region and age at diagnosis. First, substantial investment in the health care system over decades by the Chinese government shall be the main reason (22). Additionally, increased access to effective treatment, medical care, and large-scale screening programs for cervical cancer at the population level may be other reasons.
Our study has several strengths and limitations. First, we provided, for the first time in China using period analysis, the most up-to-date (during 2014–2018) 5-year RS for patients with cervical cancer from Taizhou, eastern China. Second, we found that 5-year RS for patients with cervical cancer have improved greatly during 2004–2008, 2009–2013, and 2014–2018. Third, we projected the upcoming 5-year RS for patients with cervical cancer during 2019–2023. Although the projection is interesting, it was based on a pandemic-free scenario, and as we all noted, the pandemic may substantially limit the medical access both in urban and rural regions from 2020 until at least 2022 this year. Therefore, the projection may be influenced by the pandemic, providing less meaningful evidence in the real world. We also have limitations. First, we could not provide stratified survival data on stage, histology, and treatment of patients with cervical cancer. Nevertheless, population-based cancer registries commonly do not include clinical information on stage (such as TNM), histology, and treatment of patients with cancer. Hopefully, hospital-based cancer registries including detailed information on patients with cancer will be available soon in the future. Second, we only provided the most up-to-date survival data for patients with cervical cancer from Taizhou city. Therefore, further investigations using provincial or national data are also highly warranted.
Conclusion
In this study, we provided, for the first time in China using period analysis, the most up-to-date 5-year RS for patients with cervical cancer from Taizhou, eastern China, reaching 90.9%. We found a clear increasing trend of 5-year RS during 2004–2018 overall and on stratification. Our finding of the projection during 2019–2023 reaches 94.2%, which may be influenced by the pandemic, providing less meaningful evidence in the real world, while the projection provided survival data to compare with estimated survival in the future. Our timely data on 5-year RS for patients with cervical cancer from Taizhou, eastern China is essential for the evaluation of early detection and screening programs for cervical cancer in Taizhou, eastern China. Further investigations using provincial or national data are also highly warranted.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available upon reasonable request to the corresponding author (TC).
Author Contributions
TC was responsible for the study concept, design, and obtained funding. LW and TC acquired data. YC analyzed the data. HL, LL, LW, and TC drafted the manuscript. All authors revised it for important intellectual content. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by grants from the Ten-Thousand Talents Plan of Zhejiang Province (2021R52020), the Joint Key Program of Zhejiang Province-Ministry of Health (WKJ-ZJ-1714), and the Start-up Funds for Recruited Talents in Zhejiang Cancer Hospital. The funding agencies had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.926058/full#supplementary-material
Abbreviations
DCO, proportion of death certificate only; RS, relative survival; ICD-10, International Classification of Diseases 10th Revision; GLM, the generalized linear model.
References
1. Chen T, Brenner H, Fallah M, Jansen L. Risk of second primary cancers in women diagnosed with endometrial cancer in German and Swedish cancer registries. Int J Cancer. (2017) 141:2270–80. doi: 10.1002/ijc.30930
2. Zeng H, Chen W, Zheng R, Zhang S, Ji JS, Zou X, et al. Changing cancer survival in China during 2003–15: a pooled analysis of 17 population-based cancer registries. Lancet Glob Health. (2018) 6:e555–67. doi: 10.1016/S2214-109X(18)30127-X
3. Benedetti Panici P, Basile S, Angioli R. Pelvic and aortic lymphadenectomy in cervical cancer: the standardization of surgical procedure and its clinical impact. Gynecol Oncol. (2009) 113:284–90. doi: 10.1016/j.ygyno.2008.12.014
4. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2018) 68:394–424. doi: 10.3322/caac.21492
5. Li S, Hu T, Lv W, Zhou H, Li X, Yang R, et al. Changes in prevalence and clinical characteristics of cervical cancer in the People's Republic of China: a study of 10,012 cases from a nationwide working group. Oncologist. (2013) 18:1101–7. doi: 10.1634/theoncologist.2013-0123
6. Hu SY, Zheng RS, Zhao FH, Zhang SW, Chen WQ, Qiao YL. Trend analysis of cervical cancer incidence and mortality rates in Chinese women during 1989-2008. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. (2014) 36:119–25. doi: 10.3881/j.issn.1000-503X.2014.02.001
7. Chen WQ, Sun KX, Zheng RS, Zhang SW, Zeng HM, Zou XN, et al. Report of cancer incidence and mortality in different areas of China, 2014. China Cancer. (2018) 27:1–14. doi: 10.11735/j.issn.1004-0242.2018.01.A001
8. Li X, Deng Y, Tang W, Sun Q, Chen Y, Yang C, et al. Urban-Rural disparity in cancer incidence, mortality, and survivals in Shanghai, China, during 2002 and 2015. Front Oncol. (2018) 8:579. doi: 10.3389/fonc.2018.00579
9. Dossus L, Lukanova A, Rinaldi S, Allen N, Cust AE, Becker S, et al. Hormonal, metabolic, and inflammatory profiles and endometrial cancer risk within the EPIC cohort-a factor analysis. Am J Epidemiol. (2013) 177:787–99. doi: 10.1093/aje/kws309
10. Chen TH, Jansen L, Gondos A, Emrich K, Holleczek B, Luttmann S, et al. Survival of cervical cancer patients in Germany in the early 21st century: a period analysis by age, histology, and stage. Acta Oncol. (2012) 51:915–21. doi: 10.3109/0284186X.2012.708105
11. Peto J, Gilham C, Fletcher O, Matthews FE. The cervical cancer epidemic that screening has prevented in the UK. Lancet. (2004) 364:249–56. doi: 10.1016/S0140-6736(04)16674-9
12. Liu P. Big data evaluation of clinical epidemiology of cervical cancer in China in the past 13 years. Chin J Prac Gynecol Obstetr. (2018) 34:41–5. doi: 10.19538/j.fk2018010111
13. Brenner H, Hakulinen T. Up-to-date and precise estimates of cancer patient survival: model-based period analysis. Am J Epidemiol. (2006) 164:689–96. doi: 10.1093/aje/kwj243
14. Brenner H, Hakulinen T. Maximizing the benefits of model-based period analysis of cancer patient survival. Cancer Epidemiol Biomarkers Prev. (2007) 16:1675–81. doi: 10.1158/1055-9965.EPI-06-1046
15. Gondos A, Bray F, Brewster DH, Coebergh JW, Hakulinen T, Janssen-Heijnen ML, et al. Recent trends in cancer survival across Europe between 2000 and 2004: a model-based period analysis from 12 cancer registries. Eur J Cancer. (2008) 44:1463–75. doi: 10.1016/j.ejca.2008.03.010
16. Jiang X, Wang L, Cheng Y, Tang H, Chen T. Assessment of long-term survival of cancer patients using cancer registry data from eastern China: period analysis is superior to traditional methods. Int J Cancer. (2020) 147:996–1005. doi: 10.1002/ijc.32866
17. Holleczek B, Gondos A, Brenner H. periodR - an R package to calculate long-term cancer survival estimates using period analysis. Methods Inf Med. (2009) 48:123–8. doi: 10.3414/ME0563
18. Chen TH, Jansen L, Gondos A, Emrich K, Holleczek B, Katalinic A, et al. Survival of ovarian cancer patients in Germany in the early 21st century: a period analysis by age, histology, laterality, and stage. Eur J Cancer Prev. (2013) 22:59–67. doi: 10.1097/CEJ.0b013e3283552e28
19. Zheng WL, Zhang H, Wang DZ, Zhang S, Pang S, Li CK, et al. Analysis on long-term trends of cervical cancer mortality and years of life lost in Tianjin, 1999-2015. Zhonghua Liu Xing Bing Xue Za Zhi. (2019) 40:64–9. doi: 10.3760/cma.j.issn.0254-6450.2019.01.013
20. Dong H, Duan S, Bogg L, Wu Y, You H, Chen J, et al. The impact of expanded health system reform on governmental contributions and individual copayments in the new Chinese rural cooperative medical system. Int J Health Plann Manage. (2016) 31:36–48. doi: 10.1002/hpm.2259
21. Liu X, Wong H, Liu K. Outcome-based health equity across different social health insurance schemes for the elderly in China. BMC Health Serv Res. (2016) 16:9. doi: 10.1186/s12913-016-1261-5
Keywords: cervical cancer, cancer registry, survival, 5-year relative survival, period analysis
Citation: Lu H, Li L, Cheng Y, Yang Z, Cao X, Zhang H, Qiao D, Wang L and Chen T (2022) Timely Estimates of 5-Year Relative Survival for Patients With Cervical Cancer: A Period Analysis Using Cancer Registry Data From Taizhou, Eastern China. Front. Public Health 10:926058. doi: 10.3389/fpubh.2022.926058
Received: 22 April 2022; Accepted: 22 June 2022;
Published: 25 July 2022.
Edited by:
Yanfeng Jiang, Fudan University, ChinaReviewed by:
Xiaorong Yang, Shandong University, ChinaQing Shen, Karolinska Institutet (KI), Sweden
Copyright © 2022 Lu, Li, Cheng, Yang, Cao, Zhang, Qiao, Wang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liangyou Wang, MTM1NjY4NzcxNTFAMTYzLmNvbQ==; Tianhui Chen, Y2hlbnRoQHpqY2Mub3JnLmNu
†These authors have contributed equally to this work
 Hongsheng Lu
Hongsheng Lu Lu Li
Lu Li Yongran Cheng3†
Yongran Cheng3† Liangyou Wang
Liangyou Wang Tianhui Chen
Tianhui Chen