
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 22 July 2022
Sec. Public Health Education and Promotion
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.923815
This article is part of the Research TopicImproving Immunization Programmes Uptake and Addressing Vaccine HesitancyView all 17 articles
Background: Aside from the pandemic's negative health effects, the world was confronted with public confusion since proper communication and favorable decisions became an ongoing challenge. As a result, the public's perceptions were influenced by what they knew, the many sources of COVID-19 information, and how they interpreted it. With cancer patients continuing to oppose COVID-19 vaccines, we sought to investigate the COVID-19 pandemic and vaccine sources of this information in adult cancer patients, which either helped or prevented them from taking the vaccine. We also assessed the relevance and impact of their oncologists' recommendations in encouraging them to take the vaccine.
Methods: From June to October 2021, an online survey was conducted at King Hussein Cancer Center. A total of 441 adult cancer patients took part in the study. Patients who had granted their consent were requested to complete an online questionnaire, which was collected using the SurveyMonkey questionnaire online platform. Descriptive analysis was done for all variables. The association between categorical and continuous variables was assessed using the Pearson Chi-square and Fisher Exact.
Results: Our results showed that 75% of the patients registered for the COVID-19 vaccine, while 12% refused vaccination. The majority of participants acquired their information from news and television shows, whereas (138/441) got their information through World Health Organization websites. Because the SARS-CoV-2 vaccines were made in such a short period, 54.7 % assumed the vaccines were unsafe. Only 49% of the patients said their oncologists had informed them about the benefits of SARS-CoV-2 vaccines.
Conclusions: We found that SARS-CoV-2 vaccine hesitancy in cancer patients might be related to misinformation obtained from social media despite the availability of supportive scientific information on the vaccine's benefits from the physicians. To combat misleading and unreliable social media news, we recommend that physicians use telehealth technology to reach out to their patients in addition to their face-to-face consultation, which delivers comprehensive, clear, and high-quality digital services that guide and help patients to better understand the advantages of COVID-19 vaccines.
Coronavirus Disease 2019 (COVID-19) began in Wuhan, China, in 2019 and was caused by a novel strain of coronaviruses called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). In March 2020, the World Health Organization (WHO) announced COVID-19 as a worldwide pandemic, with cases ranging from asymptomatic to symptomatic infections with mild, moderate, or severe symptoms (1, 2). By the middle of October 2021, more than 239 million cases of SARS-CoV-2 infections were confirmed worldwide, and nearly 4.87 million deaths had been declared (3).
Since the outbreak of the COVID-19 pandemic began, national and international efforts have been taken to develop effective vaccines against SARS-CoV-2, and the development of vaccines has become the most realistic chance for the world to prevent the transmission of the virus and hence, return to normality (4).
Jordan reported 856,450 cases and 10,986 deaths until October 31st, 2021, accounting for about 5.2% of all confirmed cases and 3.6% of all deaths in the WHO Eastern Mediterranean Region (EMR) (5). Jordan was also one of the first 40 nations to get the vaccines, thus the Jordanian Ministry of Health began a vaccination campaign on January 13th, 2021, targeting healthcare workers, individuals with chronic illnesses, and those over the age of 60 (6). According to a survey conducted in Jordan between December 2nd and December 29th, 2020 (before the start of the vaccine campaign), 72.3 % of Jordanians were willing to receive COVID-19 immunization, and COVID-19 risk of infection was significantly associated with vaccine acceptance (7). Immunocompromised patients, particularly cancer patients, were given special attention because, when infected with the SARS-CoV-2 virus, they have a higher risk of needing mechanical ventilation and admission to the intensive care unit (ICU), and the mortality rates are higher than people without cancer (8–10). COVID-19-related mortality rates among cancer patients are as high as 25.6 % (11). Consequently, national and international efforts emerged to develop practical guidelines to assist healthcare institutions in decreasing cancer patients' exposure to SARS-CoV-2. The most common guideline, derived from Cancer Care Ontario, involved prioritizing clinical management of cancer patients during the pandemic and thus reducing the impact of the pandemic upon healthcare workers and hospitals (12, 13).
Aside from the pandemic's negative health effects, the world faced another issue which was the spread of COVID-19 misinformation, hence increasing the likelihood of worse outcomes for vulnerable groups, such as cancer patients. As a result, public confusion emerged globally since proper communication and favorable decisions became an ongoing challenge (14).
COVID-19 infection had indeed a negative impact on the psychology of cancer patients who had higher levels of stress and anxiety due to their critical health situation (15, 16). For example, coronaphobia, which is described as an extreme fear of COVID-19 (17), was linked to a lot of vaccination skepticism. The lack of evidence on the safety and efficacy of the COVID-19 vaccination in cancer patients who were excluded from the early clinical trials created a knowledge gap, allowing misconceptions and false assumptions to emerge (18). In other words, the world faced a digital pandemic because of the tremendous amount of misinformation in different forms that have been spread worldwide. As a result, the attitudes and behaviors of the population depended on what they know, the various sources of COVID-19 information, and how they understand this information (19, 20).
Internationally, different studies have been conducted in countries such as England, Portugal, and Serbia to investigate the impact of COVID-19 and acceptance of COVID-19 vaccination in adult patients with cancer (21–23). Tunisia and Lebanon, for example, undertook similar investigations throughout the Arab region (24, 25). Both studies concluded that better communication with patients, whether directly through their oncologists or national campaigns and media, can lead to increased vaccination acceptability. Most patients appear to follow their oncologist's vaccine recommendations, indicating that the oncologist's influence is significant. A cross-sectional survey of 364 adult patients with cancer in Bosnia and Herzegovina found that 85.60% of study participants were willing to follow their oncologist's guidance on COVID-19 vaccination (26).
This issue dramatically increased the need to survey people's attitudes toward the COVID-19 pandemic to enhance the role of healthcare institutions and workers (HCWs) in raising awareness. This study aims to describe the attitudes, and knowledge, related to the COVID-19 pandemic and vaccination in adult patients with cancer, as obtained through survey analysis, to guide the best approaches for relaying COVID-19 information in this vulnerable population. We hypothesize that, despite physicians' advice to their patients to get the COVID-19 vaccine, cancer patients still refuse to get vaccinated because they depend on other sources of information other than their oncologists.
This is an online survey analysis study conducted at King Hussein Cancer Center (KHCC) between June and October 2021 with 441 cancer patients treated at KHCC, regardless of their vaccination status or vaccine type taken. The SurveyMonkey questionnaire tool (San Mateo, California, USA) online platform was used to collect the data. All participants provided their informed consent, which was recorded electronically (https://www.surveymonkey.com/summary/eIPeQ x3KkZN1nVl4F6NhevYb2Osxfh_2FjYRjTSwh97mk_3D).
Cancer patients aged 18 or over were eligible to participate. A hybrid model of data collection was followed including; Electronic SMS messages, social media platforms (WhatsApp and Facebook), and face-to-face interaction with patients. During their routine clinical visit, the research assistant explained the study's purpose to the patient, and once they consented to participate, they were provided the data collection link. To avoid redundancy and ensure data quality, participants were only allowed to submit one response.
Using the SurveyMonkey sample size calculator the recommended sample size should be 306 participants, based on the following assumption: alpha=0.05, Power 95%, using an estimated population size of 1,500 patients visiting the breast, lung, leukemia, lymphoma, and colon outpatient clinics during the survey study. Nevertheless, over the study period, we were able to collect responses from 441 cancer patients (https://www.surveymonkey.com/mp/sample-size-calculator/).
The survey questions were designed to learn about cancer patients' attitudes toward SARS-CoV-2 vaccines, discover the primary source of SARS-CoV-2 vaccine information for cancer patients, and investigate current physician practices for SARS-CoV-2 vaccine counseling as well as compare perception and attitude between the pro-vaccine and anti-vaccine groups of patients.
This survey consisted of 29 closed-format questions divided into five sections. (a) Four questions about the demographic features of the participants, such as age, gender, income, and education level. (b) Three questions regarding the patients' medical conditions, such as the type of cancer, treatment status, and current treatment. (c) Seven questions about vaccination history, with a focus on the flu vaccine and the intention to be vaccinated against COVID-19. (d) Nine questions on vaccine evolution, safety, and importance; and (e) Six questions about COVID-19 information. It was necessary to conduct a pilot study to assess the survey's questionnaire validity and internal consistency. Thirty cancer patients were chosen at random and were not included in the study. A panel of specialists was assembled to review the tool's validity (two physicians, two nurses, a psychosocial support technician, a research assistant, and a survey specialist), and minor language changes were made as a result. Furthermore, we calculated internal consistency and a Cronbach alpha test on the pilot sample, and the result was 0.729, indicating good reliability. The survey and consent form was approved by the Research Ethics Committee (IRB) of King Hussein Cancer Center (IRB # 21 KHCC 053). A translated copy of the survey is provided in the supplementary data (Supplementary Data 1).
To collect data, the questionnaire was uploaded to SurveyMonkey, and to ensure quality, it was set to receive only one response from each device to avoid redundancy. The amount of missing data was negligible, and the research team accepted up to 5% of missing data. Categorical data were summarized in tables as proportions and percentages. Statistical analysis was performed using SPSS 26 (IBM, New York, USA). Descriptive analysis was done for all variables, Pearson Chi-square tests of association, and Fisher Exact measured association among categorical and continuous variables respectively. A p-value of < 0.05 was defined as the level of statistical significance. Data were anonymously collected, stored, and analyzed in compliance with the General Data Protection Regulations.
A total of 441 patients participated in the study and filled out the questionnaire. Females made up 288 (65.3 %) of the participants, while males made up 153 (34.7 %). Almost half of the participants, 217 (49.2%), were aged between 41 and 60 years, 82 (18.6%) age was between 61 and 70 years, and a minority, 37 (8.4%), were aged between 20 and 30 years. About one-third of participants 150 (33.8 %) have university degrees, followed by 124 (27.4%) who have completed secondary education, while around 47 (10.7 %) of them are below primary education. More than half of the participants had salaries below $705 (251 (57.3%), while 103 (23.6%) had a monthly income between $705.1 and $1,410, and 45 (10.3%) received a salary between $1,410.1 and $2,116. Finally, only 38 (8.7%) have monthly income more than $2,116 [38 (8.7%)] (Table 1).
The majority of recruited subjects were diagnosed with breast cancer, 202 (40.3%), followed by lymphoma, 55 (11%), lung cancer, 46 (9.2%), leukemia, 39 (7.8%), and colon cancer, 38 (7.6%). Three hundred and forty-six (78.5%) were on active cancer treatment, with only 95 (21.5%) survivors (no current treatment) (Table 1).
Our data showed that almost two-thirds of 297 (69.2%) did not get COVID-19 infection, while 132 (30.8%) had already been infected at the study time. Of the 321 cancer patients who registered for the SARS-CoV-2 vaccine, of them; 296 (92.2%) had already received their first dose of the vaccine at the time of the survey, and 287 (97.6%) of participants were planning to take the second dose (Table 2). Moreover, our data demonstrated a significant association between cancer patients who got the flu vaccine and those who took the first dose of SARS-CoV-2 vaccines (p < 0.05) (Table 3).
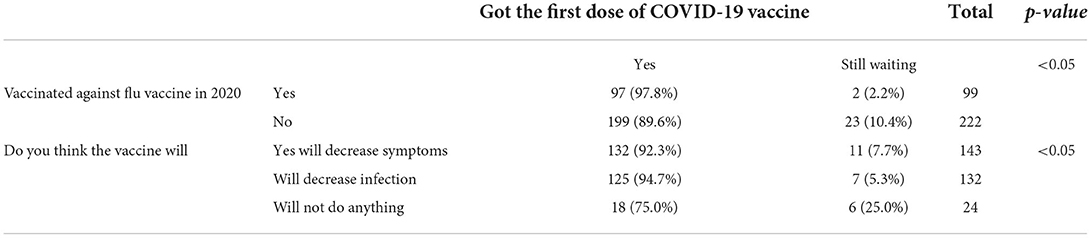
Table 3. Association between patients who got the first dose of COVID-19 vaccine and who got the flu vaccine and their opinion on the effectiveness of the COVID-19 vaccine.
Participants who did not register via the platform to get COVID 19 vaccines 105 (24.6%) reported different reasons for not taking the COVID-19 vaccine. For example, 20 cancer patients did not feel the vaccines were safe, 19 were concerned about unspecified adverse effects, and 16 believed the vaccine was manufactured in a short period, rendering them suspicious (Figure 1).
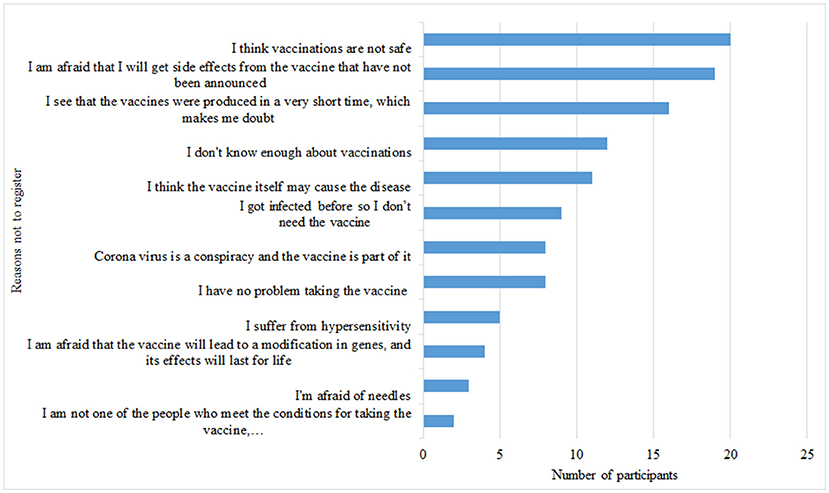
Figure 1. Reasons for not registering for the COVID-19 vaccine. Participants had the option of choosing more than one reason not to register for the vaccine.
The COVID-19 vaccination will help control the pandemic, according to 322 (77.6%) of the participants. Two hundred sixty-three (65.8%) participants believed the SARS-CoV-2 virus was created by humans, whereas 137 (34.2%) disagree. Half of the participants, 221 (54.7%), considered that the SARS-CoV-2 vaccinations are unsafe because they were developed in such a short period. The COVID-19 vaccines do not contain nanoparticles that are robots or miniature computers that may record essential human data, according to 338 (84.5%) survey participants. Similarly, 335 (84%) of those surveyed disagree that vaccinations cause infertility. More than half of the participants 244 (60.6%) disagree that published studies and vaccine manufacturers are unreliable (Figure 2).
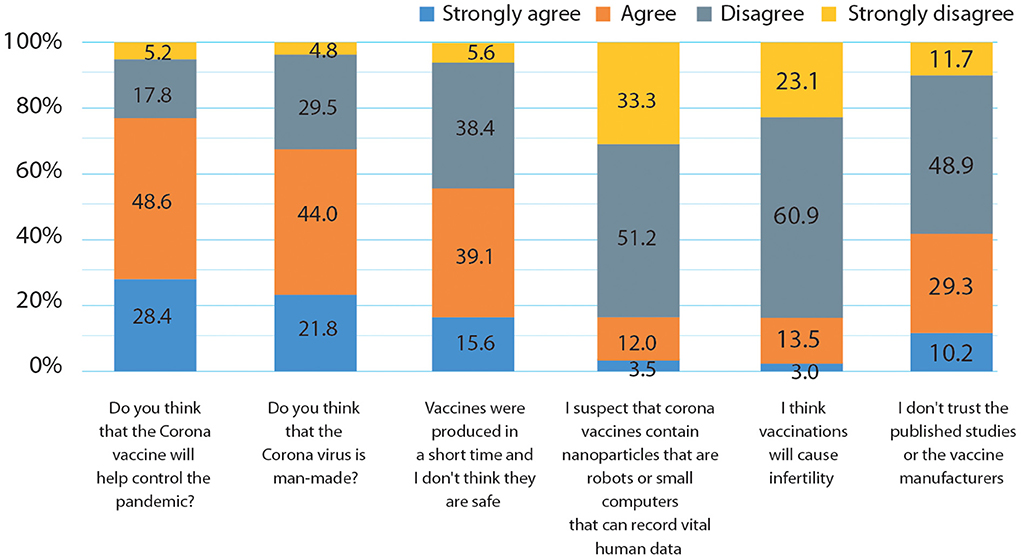
Figure 2. Questions and statements reflect patients' attitudes towards SARS-CoV-2 virus and vaccines.
Most of the participants, 285 (71.8%), believed that the vaccine will protect them for a short time, while 25 (6.3%) only thought that the vaccine will protect them for a lifetime. Furthermore, a vast majority of the participants, 186 (46.9%), thought that the vaccine will reduce the disease symptoms, but will not protect them from being infected, and 159 (40.1%) patients believed it would reduce and protect against COVID-19 infection. Almost half of the participants, 202 (50.9%), thought that they had enough information regarding the vaccine. Nevertheless, 141 (35.5 %) of the cancer patients indicated that they preferred attending awareness lectures on COVID-19 vaccines (Table 4). Results from this survey demonstrated a significant positive association between participants who thought that COVID-19 vaccines would protect them from infection and reduce the signs and symptoms of the disease and those who got the SARS-CoV-2 vaccine (p < 0.05) (Table 3).
The sources of information about the SARS-CoV-2 virus vary, as shown in Figure 3; for instance, a substantial number of patients (180/441) got their information from News and TV shows, and (138/441) got their information from the world health organization sites. Moreover, 117 and 116 patients said that their main source of information on COVID-19 was from their oncologists or scientific publications respectively. On the other hand, 98 patients claimed that they relied on social media for their information and 58 admitted they trusted the circulating news to gather the information about the COVID-19 pandemic and vaccines. The participants could choose more than one answer; hence, no percentage was calculated for each subgroup.
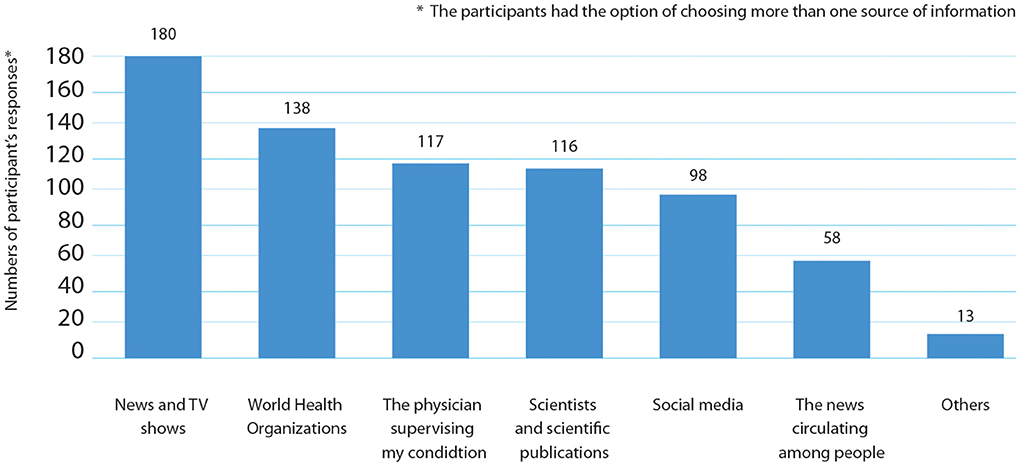
Figure 3. Personal stated sources of information about SARS-CoV-2) vaccines declared by cancer patients.
There was a positive correlation between patients who got the COVID-19 vaccine and stated that they had enough knowledge about COVID-19 [162/299 (54.2%)] compared to the participants who thought they had good information about the COVID-19 vaccines but did not register for the vaccine [40/98 (40.8%)], p < 0.05.
Figure 4 shows the physicians' and patients' practices concerning counseling on SARS-CoV-2 vaccines. Almost half of the participants, 201 (49.3%), indicated that their physicians counseled them about the advantages of SARS-CoV-2 vaccines. Although 190 patients (74.5%) thought the vaccine information they received from their oncologists was sufficient, a chi-square test of independence revealed that there was no significant association between claiming to have received sufficient information from their oncologists and their actual registration and willingness to take the COVID-19 vaccine [X2 (2, N = 255) = 2.2, p > 0.05]. Moreover, 152 (37.8%) patients did not ask their physicians about the vaccine, and 141 (35.5%) showed interest to attend awareness lectures about COVID-19 vaccines.
In our study; 53 patients [53/357 (14.8%)] could be classified as COVID-19 anti-vaxxers (anti-vaccine) because they did not register for vaccines and have no plans to do so (Table 2). We found that there was a significant difference in the perception between the pro-vaccine and anti-vaccine (anti-vaxxers) groups on claims listed in Table 5. For example, 32.6 % (16/53) of the anti-vaxxers participants thought that the COVID-19 vaccine would help contain the pandemic, while 85% (260/305) of pro-vaccine participants thought that the vaccine would control the pandemic (p < 0.05). Furthermore, 45.5 % (20/53) of anti-vaccine participants believed that vaccination would result in infertility, whereas 89.2 % (227/305) of pro-vaccine participants did not feel that vaccination would result in infertility (p < 0.05). Our data also revealed an association between receiving COVID-19 vaccination and trusting manufacturing companies, with a considerable percentage of anti-vaccine participants (77%) expressing mistrust in these companies (p < 0.05) (Table 5).
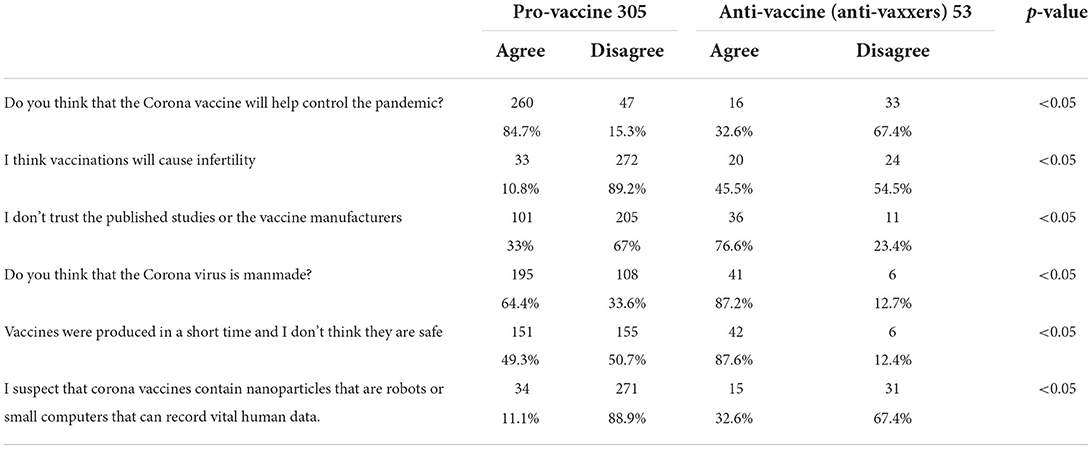
Table 5. Perception to ward COVID-19 vaccine, comparison between the pro vaccine and anti-vaccine (anti-vaxxers) groups in the sample.
The world currently faces an “infodemic” (19, 27) regarding sources of information on COVID-19 infection and vaccination. Considering that cancer patients infected with SARS-CoV-2 have a higher risk for complications and higher mortality rates, we chose to investigate their attitudes, knowledge, and practices related to the pandemic (28).
Our data showed that 108 patients (25.2%) acknowledged that they took the seasonal influenza vaccine in 2020, similar to the percentage reported in cancer patients from Cyprus (29). A similar number was found in a study of Jordanian university students, with 28.8% having already gotten the flu vaccine (30).
As for SARS-CoV-2 vaccination, most participants in our study, 296 (92.2%), reported that they had already taken the first COVID-19 vaccine shot, which was the only one available at the time of the survey. These results were in line with other published data showing that cancer patients are more willing to take the COVID-19 vaccine than the influenza vaccine (25). On the other hand, a survey performed by Gheorghe et al. on cancer patients in Romania showed that those patients believed that getting the seasonal influenza vaccine would prevent the spread of SARS-CoV-2, and 27.8% declared that they would not get vaccinated against SARS-CoV-2 if a vaccine would become available in Romania (31).
Similar to earlier studies, our findings revealed that the news, TV shows, and the media, in general, were the most common sources of information on the SARS-CoV-2 virus and the COVID-19 pandemic reported by cancer patients (25, 32–34). However, according to a study from Cyprus, social networks were the most prominent source of information for cancer patients (41.2%), while official government websites were the least popular (8.1%) (29). The supervising oncologist was the third most common source of information in our study regarding the SARS-CoV-2 virus similar to data published by Kelkar et al. (35).
The most crucial data in our study found that participants who obtained advice from their doctors and asked their doctors about Coronavirus were 49 and 26%, respectively, which was similar to a study published in Poland (32).
Although, 51% of the participants believed that they had enough information regarding the COVID-19 vaccine, and 75% of those who asked their doctors about the COVID-19 vaccine reported that they got enough information about the vaccine, 35% were still interested in attending awareness lectures, unlike a previous study performed in Jordan on community members where 85% requested more information about COVID-19 vaccines (36).
Our study is the first in Jordan to assess cancer patients' attitudes and knowledge related to the COVID-19 pandemic. It demonstrates the potential influence of sources of information on the tendency to take the vaccines. Although most cancer patients registered for the COVID-19 vaccine, almost 15% of patients still opposed vaccinations. This opposition is most likely due to reliance on misinformation from social media and TV shows based on survey results. We recommend that physicians utilize telehealth technology as an additional resource to their consultation to communicate with their patients, which is akin to online media. Telehealth technology delivers comprehensive, clear, and high-quality digital services that guide and assist patients in better understanding the benefits of COVID-19 vaccines while also saving time during consultations. In addition, involving other hospital services that focus on patients' physical and mental well-being could aid in offering one-on-one guidance to patients during this vital time of uncertainty.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The Institutional Review Board approved this study of King Hussein Cancer Center, Amman, Jordan Center (IRB # 21 KHCC 053) on August 19, 2021. The questionnaire was fully anonymized to protect participants' privacy, and only the collected data were used for analyses and statistical tests. The patients/participants provided their written informed consent to participate in this study.
Concept and study design and review and editing: LS and MS. Literature search and data collection: LS, SB, and MA. Data analysis, figures, tables, and interpretation of the data: LS and KA. Data validation, visualization, and writing—original draft: LS. All authors approved the final version of the manuscript.
Partially funded by the Scientific Research and Innovation Support Fund at the Ministry of Higher Education and Scientific Research (MPH/1/06/2021).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.923815/full#supplementary-material
1. Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. (2020) 91:157–60. doi: 10.23750/abm.v91i1.9397
2. Zhou M, Zhang X, Qu J. Coronavirus disease 2019 (COVID-19): a clinical update. Front Med. (2020) 14:126–35. doi: 10.1007/s11684-020-0767-8
3. WHO Coronavirus (COVID-19) Dashboard. World Health Organization (2022). Available online at: https://covid19.who.int/ (accessed February, 2022).
4. Yi Y, Lagniton PNP, Ye S, Li E, Xu RH. COVID-19: what has been learned and to be learned about the novel coronavirus disease. Int J Biol Sci. (2020) 16:1753–66. doi: 10.7150/ijbs.45134
5. Eastern Mediterranean Regional Office COVID-19 Dashboard. World Health Organization, Health Emergencies Programme (2021). Available online at: https://app.powerbi.com/view?r=eyJrIjoiN2ExNWI3ZGQtZDk3My00YzE2LWFj YmQtNGMwZjk0OWQ1MjFhIiwidCI6ImY2MTBjMGI3LWJkMjQtNGIzOS04 MTBiLTNkYzI4MGFmYjU5MCIsImMiOjh9 (accessed October 31, 2021).
7. Nusair MB, Arabyat R, Khasawneh R, Al-Azzam S, Nusir AT, Alhayek MY. Assessment of the relationship between COVID-19 risk perception and vaccine acceptance: a cross-sectional study in Jordan. Hum Vaccin Immunother. (2022) 18:2017734. doi: 10.1080/21645515.2021.2017734
8. Kuderer NM, Choueiri TK, Shah DP, Shyr Y, Rubinstein SM, Rivera DR, et al. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet. (2020) 395:1907–18. doi: 10.1016/S0140-6736(20)31187-9
9. Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. (2020) 21:335–7. doi: 10.1016/S1470-2045(20)30096-6
10. Zhang L, Zhu F, Xie L, Wang C, Wang J, Chen R, et al. Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann Oncol. (2020) 31:894–901. doi: 10.1016/j.annonc.2020.03.296
11. Saini KS, Tagliamento M, Lambertini M, McNally R, Romano M, Leone M, et al. Mortality in patients with cancer and coronavirus disease 2019: a systematic review and pooled analysis of 52 studies. Eur J Cancer. (2020) 139:43–50. doi: 10.1016/j.ejca.2020.08.011
12. Gosain R, Abdou Y, Singh A, Rana N, Puzanov I, Ernstoff MS. COVID-19 and cancer: a comprehensive review. Curr Oncol Rep. (2020) 22:53. doi: 10.1007/s11912-020-00934-7
13. Ontario Health CCO. Pandemic Planning Clinical Guideline for Patients with Cancer. Ontario: Ontario Health (2020).
14. Ioannidis JPA. Coronavirus disease 2019: the harms of exaggerated information and non-evidence-based measures. Eur J Clin Invest. (2020) 50:e13222. doi: 10.1111/eci.13222
15. Ayubi E, Bashirian S, Khazaei S. Depression and anxiety among patients with cancer during COVID-19 pandemic: a systematic review and meta-analysis. J Gastrointest Cancer. (2021) 52:499–507. doi: 10.1007/s12029-021-00643-9
16. Miaskowski C, Paul SM, Snowberg K, Abbott M, Borno H, Chang S, et al. Stress and symptom burden in oncology patients during the COVID-19 pandemic. J Pain Symptom Manage. (2020) 60:e25–34. doi: 10.1016/j.jpainsymman.2020.08.037
17. Turan GB, Aksoy M, Ozer Z, Demir C. The association between coronaphobia and attitude towards COVID-19 vaccine: a sample in the east of Turkey. Encephale. (2022) 48:38–42. doi: 10.1016/j.encep.2021.04.002
18. Barriere J, Gal J, Hoch B, Cassuto O, Leysalle A, Chamorey E, et al. Acceptance of SARS-CoV-2 vaccination among French patients with cancer: a cross-sectional survey. Ann Oncol. (2021) 32:673–4. doi: 10.1016/j.annonc.2021.01.066
19. Banerjee D, Meena KS. COVID-19 as an “Infodemic” in public health: critical role of the social media. Front Public Health. (2021) 9:610623. doi: 10.3389/fpubh.2021.610623
20. Sentell T, Vamos S, Okan O. Interdisciplinary perspectives on health literacy research around the world: more important than ever in a time of COVID-19. Int J Environ Res Public Health. (2020) 17:3010. doi: 10.3390/ijerph17093010
21. de Sousa MJ, Caramujo C, Julio N, Magalhaes JC, Basto R, Fraga T, et al. Acceptance of SARS-CoV-2 vaccination among cancer patients in Portugal: attitudes and associated factors. Support Care Cancer. (2022) 30:4565–70. doi: 10.1007/s00520-022-06886-x
22. Erdem D, Karaman I. Impact of corona-phobia on attitudes and acceptance towards COVID-19 vaccine among cancer patients: a single-center study. Future Oncol. (2022) 18:457–69. doi: 10.2217/fon-2021-1015
23. Matovina Brko G, Popovic M, Jovic M, Radic J, Bodlovic Kladar M, Nikolic I, et al. COVID-19 vaccines and cancer patients: acceptance, attitudes and safety. J BUON. (2021) 26:2183–90.
24. Khiari H, Cherif I, M'Ghirbi F, Mezlini A, Hsairi M. COVID-19 vaccination acceptance and its associated factors among cancer patients in Tunisia. Asian Pac J Cancer Prev. (2021) 22:3499–506. doi: 10.31557/APJCP.2021.22.11.3499
25. Moujaess E, Zeid NB, Samaha R, Sawan J, Kourie H, Labaki C, et al. Perceptions of the COVID-19 vaccine among patients with cancer: a single-institution survey. Future Oncol. (2021) 17:4071–9. doi: 10.2217/fon-2021-0265
26. Marijanovic I, Kraljevic M, Buhovac T, Sokolovic E. Acceptance of COVID-19 vaccination and its associated factors among cancer patients attending the oncology clinic of University Clinical Hospital Mostar, Bosnia and Herzegovina: a cross-sectional study. Med Sci Monit. (2021) 27:e932788. doi: 10.12659/MSM.932788
27. Jackson T, Steed L, Pedruzzi R, Beyene K, Chan AHY. Editorial: COVID-19 and behavioral sciences. Front Public Health. (2022) 9:830797. doi: 10.3389/fpubh.2021.830797
28. Russell B, Moss CL, Shah V, Ko TK, Palmer K, Sylva R, et al. Risk of COVID-19 death in cancer patients: an analysis from Guy's Cancer Centre and King's College Hospital in London. Br J Cancer. (2021) 125:939–47. doi: 10.1038/s41416-021-01500-z
29. Roupa Z, Noula M, Nikitara M, Ghobrial S, Latzourakis E, Polychronis G. Acceptance of coronavirus disease. vaccination by cancer patients in Cyprus: a cross-sectional study. J Oncol Pharm Pract. (2019) 2021:10781552211039489. doi: 10.1177/10781552211039489
30. Sallam M, Dababseh D, Eid H, Hasan H, Taim D, Al-Mahzoum K, et al. Low COVID-19 vaccine acceptance is correlated with conspiracy beliefs among University Students in Jordan. Int J Environ Res Public Health. (2021) 18:2407. doi: 10.3390/ijerph18052407
31. Gheorghe AS, Negru SM, Nitipir C, Mazilu L, Marinca M, Gafton B, et al. Knowledge, attitudes and practices related to the COVID-19 outbreak among Romanian adults with cancer: a cross-sectional national survey. ESMO Open. (2021) 6:100027. doi: 10.1016/j.esmoop.2020.100027
32. Brodziak A, Sigorski D, Osmola M, Wilk M, Gawlik-Urban A, Kiszka J, et al. Attitudes of patients with cancer towards vaccinations-results of online survey with special focus on the vaccination against COVID-19. Vaccines. (2021) 9:411. doi: 10.3390/vaccines9050411
33. Fernandez-Penny FE, Jolkovsky EL, Shofer FS, Hemmert KC, Valiuddin H, Uspal JE, et al. COVID-19 vaccine hesitancy among patients in two urban emergency departments. Acad Emerg Med. (2021) 28:1100–7. doi: 10.1111/acem.14376
34. Hong J, Xu XW, Yang J, Zheng J, Dai SM, Zhou J, et al. Knowledge about, attitude and acceptance towards, and predictors of intention to receive the COVID-19 vaccine among cancer patients in Eastern China: a cross-sectional survey. J Integr Med. (2022) 20:34–44. doi: 10.1016/j.joim.2021.10.004
35. Kelkar AH, Blake JA, Cherabuddi K, Cornett H, McKee BL, Cogle CR. Vaccine enthusiasm and hesitancy in cancer patients and the impact of a webinar. Healthcare. (2021) 9:351. doi: 10.3390/healthcare9030351
Keywords: survey, COVID-19, cancer patients, vaccine, SARS-CoV-2
Citation: Souan L, Sughayer MA, Abu Alhowr M, Ammar K and Bader SA (2022) An update on the impact of SARS-CoV-2 pandemic public awareness on cancer patients' COVID-19 vaccine compliance: Outcomes and recommendations. Front. Public Health 10:923815. doi: 10.3389/fpubh.2022.923815
Received: 19 April 2022; Accepted: 29 June 2022;
Published: 22 July 2022.
Edited by:
Alessandra Casuccio, University of Palermo, ItalyReviewed by:
Yuan Cao, Hong Kong Polytechnic University, Hong Kong SAR, ChinaCopyright © 2022 Souan, Sughayer, Abu Alhowr, Ammar and Bader. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maher A. Sughayer, bXN1Z2hheWVyQGtoY2Muam8=; Lina Souan, bHNvdWFuQGtoY2Muam8=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.