- 1Department of Ultrasonics, Tianjin Fifth Central Hospital, Tianjin, China
- 2Dean's Office, Tianjin Fifth Central Hospital, Tianjin, China
- 3Department of Nutrition, Tianjin Fifth Central Hospital, Tianjin, China
- 4Department of Epidemiology and Statistics, School of Public Health, Tianjin Medical University, Tianjin, China
Background: There were few studies to report whether drinking water sources and habits affected health outcomes. Therefore, this study aimed to examine how boiled water and lifespan water sources affected the risks of cardiovascular disease (CVD) and all-cause mortality in the elderly.
Methods: This study was a 20-year cohort study. All participants aged ≥60 years were eligible. Exposures of interest included lifespan drinking water sources and habits, which were collected using a validated questionnaire. Drinking water sources included wells, surface water, spring, and tap water in childhood, around the age of 60 years, and at present. Drinking habits included boiled and un-boiled water. The main end events included CVD and all-cause mortality.
Results: There were 33,467 participants in this study. Compared to tap water, drinking well and surface water around the age of 60 years were associated with a higher risk of all-cause mortality (HR: 1.092, 95% CI: 1.051–1.134, P < 0.001; and HR: 1.136, 95% CI: 1.081–1.194, P < 0.001, respectively). However, only drinking spring around aged 60 years and drinking well at present were associated with a lower CVD mortality (HR: 0.651, 95% CI: 0.452–0.939, P = 0.022; and HR: 0.757, 95% CI: 0.665–0.863, P < 0.001, respectively). Boiled water was not associated with mortality.
Conclusions: Drinking water from well and surface water around the age of 60 years were associated with increased all-cause mortality. Drinking water from spring around the age of 60 years and well at present was associated with a decreased CVD mortality. However, boiled water was not associated with mortality.
Introduction
As drinking water is an essential issue for human beings, access to safe drinking water is the most fundamental requirement for public health. It is reported that about 2.2 billion people have no access to improved drinking water worldwide (1). It is estimated that 785 million people suffer from the drinking water crisis, especially in rural areas of low- and middle-income countries (2). Contaminated water is still a major cause of infectious diarrheal diseases. As a result, there were approximately 500 thousand deaths attributed to inadequate safe water, which accounted for one-third of diarrhea-attributed deaths in 2016 (3). Therefore, access to sustainable and safe drinking water is still a major goal and global challenge of public health.
The associations of water, sanitation, and hygiene with health outcomes are critical for the prevention of diseases and improvement of life expectancy. Until now, there were many studies to report the associations of drinking water with health outcomes, including mortality and cardiovascular disease (CVD) (4–7). However, these studies are limited and have not investigated the associations of disinfection byproducts, compositions, hardness, and temperature of drinking water with health outcomes (7–11). In fact, investigating how drinking water sources and habits affect health outcomes is more significant from the perspective of public health. Furthermore, the quality of drinking water has been considerably improved due to the efforts of governments. For example, a large amount of capital has been spent to improve drinking water treatment and supply infrastructure in the last few decades in China (12). The main source of drinking water has changed from unimproved water, such as wells, rivers, and lakes, to improved water. Therefore, investigating the impact of lifespan drinking water sources and habits on health outcomes is particularly important, especially for frail populations, such as children and the elderly.
In this study, the Chinese Longitudinal Healthy Longevity Survey (CLHLS) was used to examine how boiled water and lifespan water sources affect CVD and all-cause mortality. As a result, this study would contribute to the improvement of health in the elderly.
Materials and Methods
Study Design and Population
The CLHLS was first conducted in 1998, and followed by waves in 2000, 2002, 2005, 2008–2009, 2011–2012, 2014, and 2017–2018. Twenty-three provinces/ municipalities were randomly selected from 31 provinces/ municipalities in China. Then, about half of the counties and city districts were randomly sampled within 23 provinces/ municipalities. In a healthy longevity survey, there were 19.5 thousand centenarians, 26.8 thousand nonagenarians, and 29.7 thousand octogenarians. The older people aged 80 years or older accounted for 67.4% of the total sample. A validated questionnaire was used to collect information on family structure, physical performance, health status, history of chronic diseases, and so on.
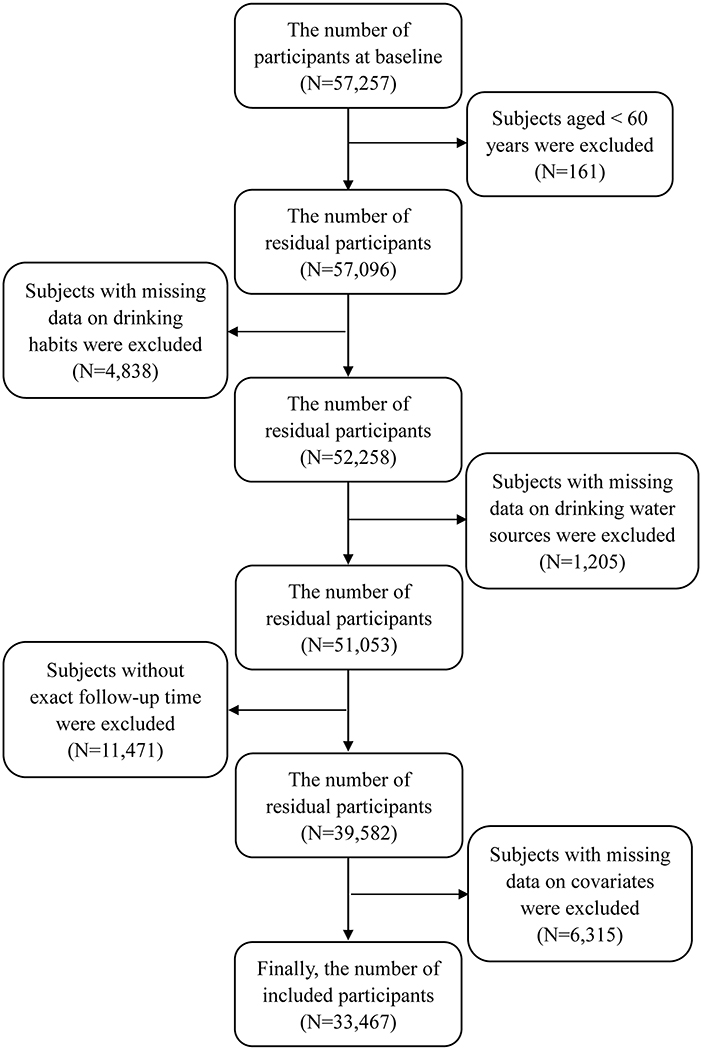
This study included all participants aged 60 years or older. If subjects had incomplete data on drinking water sources, drinking habits, and other covariates, they would be excluded. Meanwhile, subjects with abnormal data on covariates, such as weight and blood pressure, were also excluded. The detailed screening procedure is shown in Figure 1. This study was approved by the Institutional Review Board, Duke University (Pro00062871), and the Biomedical Ethics Committee, Peking University (IRB00001052–13074). All participants provided written informed consent.
Measures
Exposures of interest included drinking water sources and drinking habits. Drinking water sources in childhood, around the age of 60 years, and at present were identified via a similar question: Water you drink is mainly from? Participants were required to select an answer from the following options: 1. well, 2. rivers or lakes, 3. spring, 4. pond or pool, and 5. tap water. In the final analysis, drinking water sources were classified as follows: tap water, well, surface water, and spring. Similarly, a question “What kind of water you usually drink?” was used to identify drinking habits, including boiled and un-boiled water.
Death Assessment
End-events of interest included CVD mortality and all-cause mortality. In each wave, survival status was checked for each participant in a face-to-face interview. If someone died before a certain survey, the ascertainable date of death was identified by interviewing a close family member or local doctors. Furthermore, cause-specific mortality was further interviewed. Deceased participants caused by CVD were considered to have an end-event of CVD mortality.
Covariates
In this study, information on age, sex, and ethnicity was collected according to participants' identification cards. Education levels and living areas were measured by self-report. Weight was measured by the study staff according to the standardized protocol. Dietary intakes at present were collected via the following questions: How often do you eat fresh fruit at present? How often do you eat vegetables at present? How often do you eat meat at present? How often do you eat fish at present? Information on alcohol consumption, current smoking habits, physical activity, self-rated health, and history of hypertension, diabetes, and CVD were collected using a validated questionnaire, which was described in detail elsewhere (13).
Statistical Analysis
A Kolmogorov-Smirnov test was used to test for the normality of continuous variables. Continuous data with normal distribution, such as age and weight, were expressed as means ± standard deviations and were compared with the differences between-group using a t-test. Categorized variables were presented as frequencies (constituent ratios) and were compared with the differences between-group using the chi-square test. Hazard ratios (HRs) and 95% CIs of drinking water sources and habits on the risks of CVD and all-cause mortality were estimated using Cox regressions with adjustments for age, sex, weight, ethnicity, education levels, marital status, living areas, current smoker, current alcohol consumer, physical activity, dietary intakes including fruits, vegetables, meat, and fish, history of hypertension, history of diabetes, self-reported health, and waves. Based on the adjusted factors mentioned above, drinking water source was additionally adjusted when drinking habits as the main exposure. Meanwhile, drinking habits were further adjusted based on the common- adjusted factors mentioned above when drinking water source as the main exposure. The Fine-Gray competing risk model was used to correct the competitive risk of death caused by other causes when CVD mortality is the end event. Cox regressions were further stratified by sex and living areas. In this study, the proportional hazards assumption was confirmed to hold in all Cox regressions. To prevent the possibility that deaths were caused by other fatal illnesses, sensitivity analysis was conducted with participants who died within the first 2 years after baseline being excluded from the analysis. All analyses were conducted using SAS 9.4 (SAS Institute Inc., Cary, NC, USA.). A two-tailed P ≤ 0.05 indicated a statistical significance.
Results
Characteristics of All Participants
Finally, there were 33,467 participants included in this study. The median time of follow-up was 5 years. The averages of age and weight were 86.38 ± 11.53 years and 49.60 ± 11.18 kg, respectively. The proportions of males and females were 43.33 and 56.67%, respectively. There were 31,904 and 1,563 participants drinking boiled and un-boiled water, respectively. There were 20,295 and 1,210 deceased participants caused by all-cause mortality and CVD, accounting for 60.64 and 3.80%, respectively. There were significant differences between censoring and end-event caused by all-cause mortality in all baseline characteristics, except a history of hypertension (P = 0.480). Meanwhile, significant differences between censoring and end-event caused by CVD were observed in all baseline characteristics, except weight (P = 0.141), marital status (P = 0.224), education (P = 0.065), ethnicity (P = 0.425), current smoking habits (P = 0.194), current alcohol consumption (P = 0.613), self-reported health (P = 0.238), history of diabetes (P = 0.905), and drinking habits (P = 0.185) as shown in Table 1.
The Associations of Lifespan Drinking Water Sources and Habits With All-Cause Mortality
Compared to unboiled water, boiled water was not associated with all-cause mortality (HR: 1.060, 95% CI: 0.995–1.129, P = 0.071). Compared to tap water, drinking well, surface water, and spring in childhood was not associated with all-cause mortality (HR: 1.044, 95% CI: 0.931–1.171, P = 0.461; HR: 1.075, 95% CI: 0.957–1.208, P = 0.225; and HR: 1.018, 95% CI: 0.892–1.162, P = 0.791, respectively). However, drinking well (HR: 1.092, 95% CI: 1.051–1.134, P < 0.001) and surface water (HR: 1.136, 95% CI: 1.081–1.194, P < 0.001) around the age of 60 years, but not drinking spring (HR: 0.990, 95% CI: 0.913–1.073, P = 0.801), was associated with all-cause mortality. Furthermore, drinking surface water at present was associated with a lower all-cause mortality (HR: 0.884, 95% CI: 0.789–0.991, P = 0.034) (Table 2).

Table 2. The associations of lifespan drinking water sources and habits with all-cause mortality (N = 33,467).
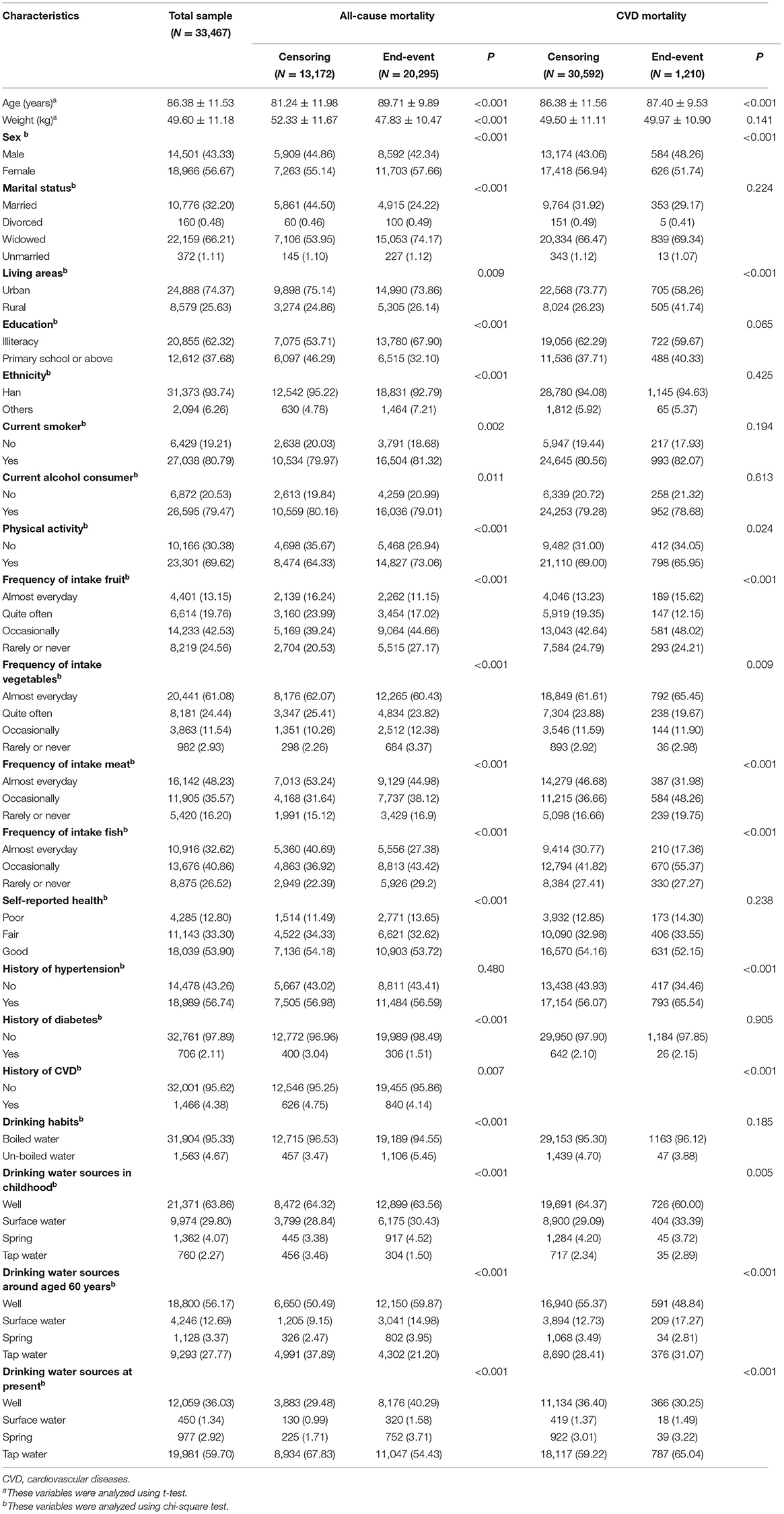
Figure 2 shows the associations of lifespan drinking water sources and habits with all-cause mortality stratified by sex and living areas. The results stratified by sex were similar to those in the total sample. Drinking well in males and boiled water in females were associated with higher all-cause mortality (HR: 1.055, 95% CI: 1.007–1.106, P = 0.026; HR: 1.112, 95% CI: 1.024–1.207, P= 012, respectively). The results stratified by living areas were compared with those in the total sample.
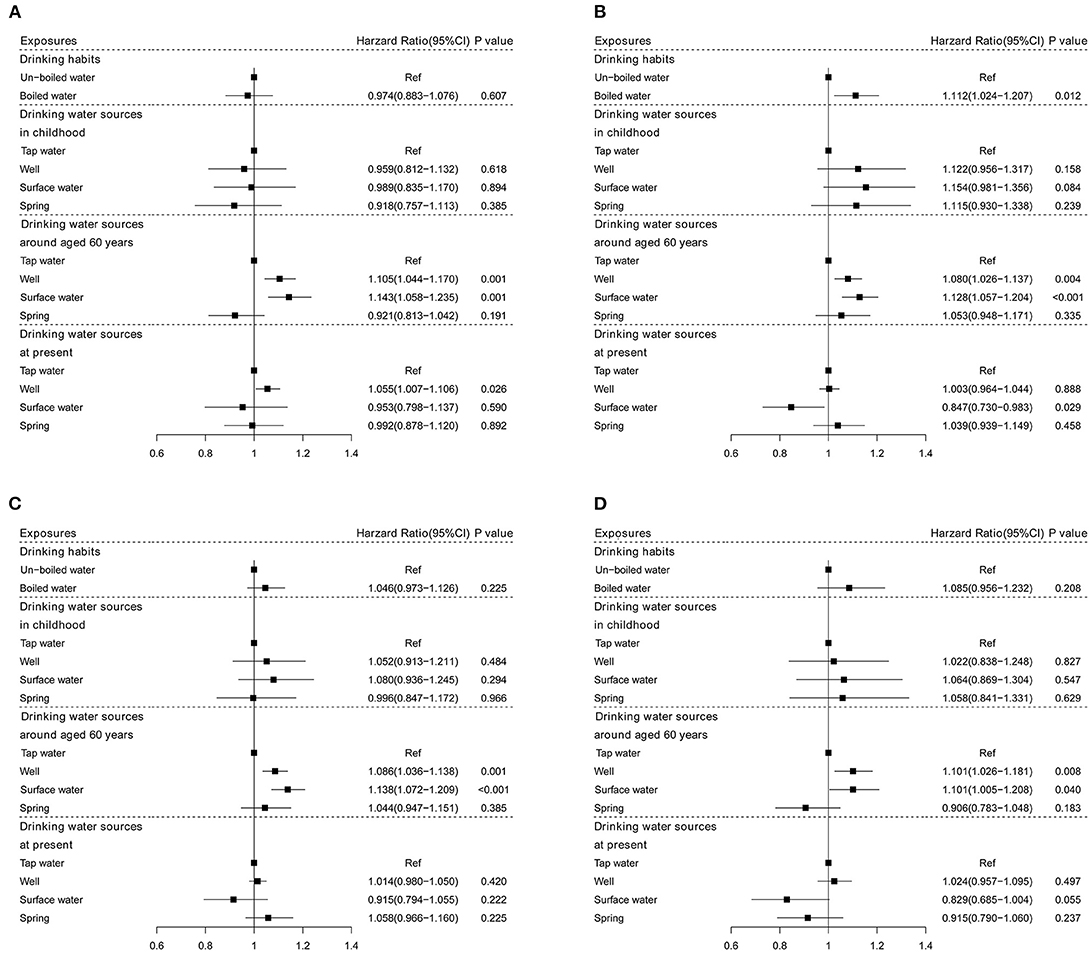
Figure 2. The associations of drinking water sources and habits with all-cause mortality stratified by sex and living areas. (A) Males; (B) females; (C) urban; and (D) rural.
The Associations of Lifespan Drinking Water Sources and Habits With CVD Mortality
Table 3 shows that boiled water was not associated with CVD mortality (HR: 1.280, 95% CI: 0.948–1.729, P < 0.107). Furthermore, drinking spring around the age of 60 years and drinking well at present were associated with a lower CVD mortality (HR: 0.651, 95% CI: 0.452–0.939, P = 0.022; and HR: 0.757, 95% CI: 0.665–0.863, P < 0.001, respectively).

Table 3. The associations of lifespan drinking water sources and habits with CVD mortality (N = 31,802).
In males, there was a significant association between drinking spring water around 60-years-old and CVD mortality (HR: 0.461, 95% CI: 0.251–0.846, P = 0.013). In females, subjects drinking well at present had a lower CVD mortality (HR: 0.674, 95% CI: 0.562–0.808, P < 0.001) (Figures 3A,B).
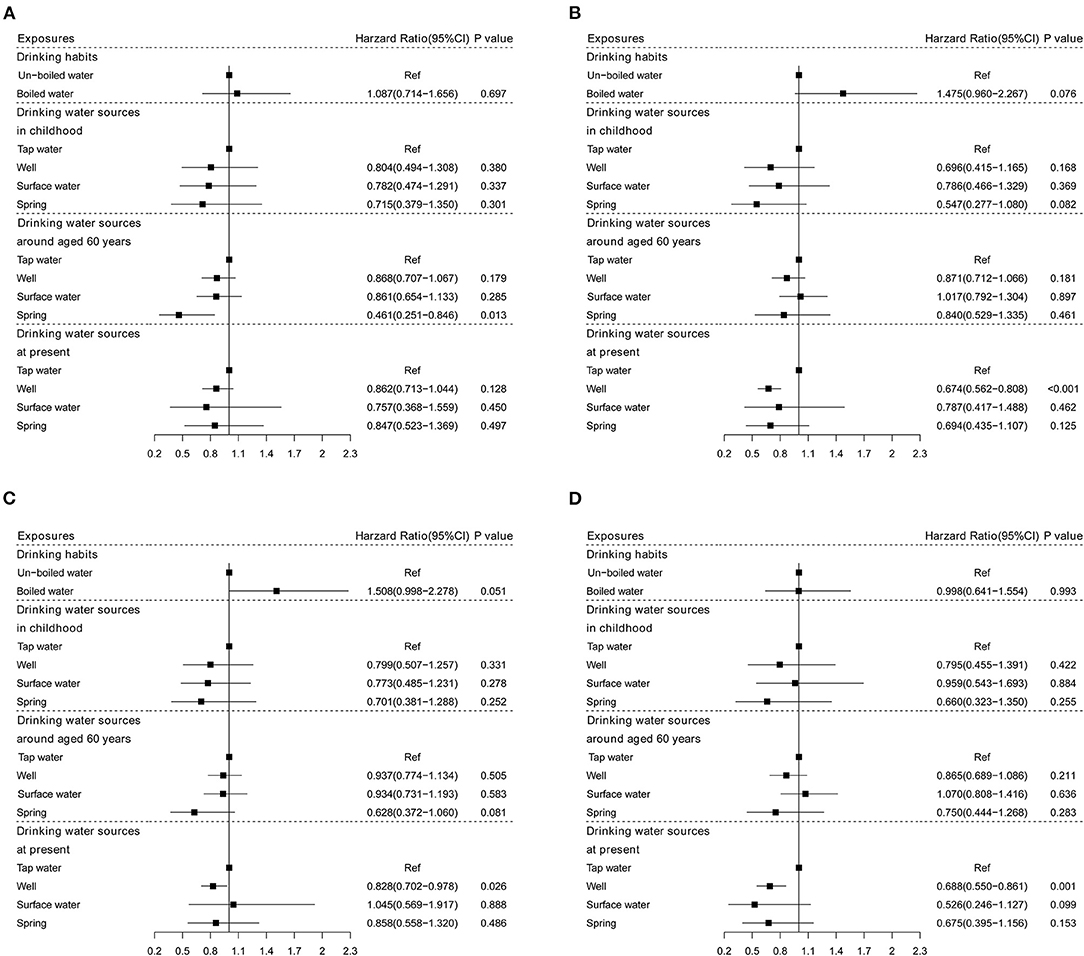
Figure 3. The associations of drinking water sources and habits with CVD mortality stratified by sex and living areas. (A) Males; (B) females; (C) urban; and (D) rural.
When stratified by living areas, only the drinking well was associated with a lower CVD mortality in urban and rural areas (HR: 0.828, 95% CI: 0.702–0.978, P = 0.026; HR: 0.688, 95% CI: 0.550–0.861, P = 0.001, respectively) (Figures 3C,D).
Sensitivity Analysis
By repeating the analysis after excluding participants dying within 2 years after baseline, Supplementary Table 1 implies that subjects drinking well and surface water around the age of 60 years and drinking well at present had higher all-cause mortality (HR: 1.132, 95% CI: 1.076–1.191, P < 0.001; HR: 1.202, 95% CI: 1.130–1.278, P < 0.001; and HR: 1.043, 95% CI: 1.006–1.082, P = 0.022, respectively), which was consistent with the main results. Meanwhile, subjects drinking spring around the age of 60 years and drinking well at present had a lower CVD mortality (HR: 0.612, 95% CI: 0.383–0.978, P = 0.040; and HR: 0.767, 95% CI: 0.647–0.910, P = 0.002, respectively), which was comparable with the main results (Supplementary Table 2).
Discussion
This study was designed to examine how boiled water and lifespan water sources affected CVD and all-cause mortality among older adults. The results suggested that drinking well and surface water around the age of 60 years was linked to higher all-cause mortality. Meanwhile, subjects drinking from the spring around the age of 60 years and drinking well at present had a lower CVD mortality. There was not enough evidence to support the association of boiled water with CVD and all-cause mortality.
Since there is a lack of access to clean drinking water, boiling water is the most common method for water treatment, especially in rural areas (14). The findings from a national survey revealed that over 85% of households in rural China regularly drink boiled water (12). However, a previous study found that there was no significant association between boiled water and the biomarkers of health, including eosinophilia, anemia, and obesity (15). Other studies noted that boiling water failed to reduce the risk of waterborne pathogens (16, 17). These findings supported the results of this study, which showed that drinking boiled water was not associated with mortality.
The results of this study implied that drinking well and surface water around the age of 60 years was linked to higher all-cause mortality. Well and surface water are considered unimproved water sources, while tap water is an improved water source (18, 19). It is known that surface water and groundwater are more susceptible to pathogenic microorganisms. Contaminated water is the leading cause of infectious diarrheal diseases, which directly or indirectly lead to 2.2 million deaths per year (20). It is suggested that the type of water source is a predictor of contaminated water (21). Furthermore, compared to unimproved water, an improved water source was linked to fewer microorganisms (21). A recent study indicated that the overall qualification rate of drinking water is not high, and the main challenge is still microbial pollution (1). It is documented that the major rivers and lakes in China suffer from different degrees of pollution. Approximately 9.1% of drinking water sources were not up to the quality standards of surface water or groundwater in 2018 (22). Furthermore, the treatment process of drinking water was conventional in China and failed to fully remove the harmful substances in drinking water (23, 24). On the other hand, the deficit of Ca and Mg contents in groundwater is common, which can increase oncological disease mortality (25, 26). As an endocrine disturber, the average level of the total phthalates was higher in surface water and groundwater (27). Therefore, it was rational that drinking surface water and groundwater was linked to higher all-cause mortality.
Another striking finding of this study was that drinking water from spring around 60 years of age was associated with a lower CVD mortality. The underlying mechanisms of the association of drinking water sources with CVD mortality were unknown. Tap water is commonly treated by disinfection of chlorination and fluoride. Serum chloride was considered a strong prognostic factor of heart failure (28, 29). Furthermore, chronic fluoride exposure might be associated with atherosclerosis and the cardiovascular system (30). Since long-term fluoride exposure would decrease glutathione peroxidase levels, which in turn causes systemic inflammation and endothelial activation, fluoride exposure could induce oxidative stress and promote the pathogenesis of atherosclerosis (31). Moreover, it has been documented that fluoride can accumulate in the cardiovascular system (32). Therefore, the disinfectant in tap water might be a reason why tap water was associated with a higher CVD mortality compared to spring. On the other hand, spring water is rich in minerals, such as Ca and Mg, which play a role in the prevention of CVD (33). Of course, the underlying mechanisms need to be further studied through laboratory research in the future.
Strengths and Limitations
This study had some strengths. Firstly, this is the first study to examine the associations of boiled water and lifespan water sources with CVD and all-cause mortality in the elderly. Therefore, this study would contribute to the prevention of chronic diseases and the improvement of drinking water hygiene. Secondly, this study provided the lifespan drinking water sources for all participants. Therefore, this study provided a comprehensive picture of the associations of drinking water sources with health outcomes.
However, there were some limitations in this study. Firstly, since causes of death failed to be collected in waves 2014 and 2017–2018, the sample size of CVD mortality was not the same as that of the all-cause mortality. Secondly, public health policy in China, such as improving access to clean water and drinking water treatment, failed to be considered in this study, which might confound the observed associations. Thirdly, given that there were many elders in this study, caution should be observed when extrapolating the findings of this study to other populations. Fourthly, since information on pollutants from various resources of drinking water was not collected in the CLHLS, the underlying mechanisms of the associations of drinking water sources and habits with CVD and all-cause mortality were unknown and were not fully explained.
In conclusion, drinking water sources around 60 years of age, but not in childhood and at present, could affect mortality. Subjects drinking well and surface water around the age of 60 years had higher all-cause mortality. However, subjects drinking spring around 60 years of age and drinking well at present had a lower CVD mortality. Meanwhile, boiled water was not associated with mortality. Therefore, specific water sources and drinking habits should be proposed for populations at risk of different chronic diseases. Furthermore, more attention should be given to drinking water sources for the elderly aged around 60 years to prevent chronic diseases and increase their life expectancy.
Data Availability Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://opendata.pku.edu.cn/dataverse/CHADS.
Ethics Statement
The studies involving human participants were reviewed and approved by the Institutional Review Board, Duke University (Pro00062871) and the Biomedical Ethics Committee, Peking University (IRB00001052–13074). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
XL contributed to writing the original draft. ZP contributed to reviewing and editing the draft. ZZ contributed to data curation and formal analysis. YZ contributed to data and results interpretation. YC contributed to the study design and conceptualization. All authors read and approved the final manuscript.
Funding
This study was supported by the National Natural Science Foundation of China (81903416).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.921738/full#supplementary-material
References
1. Wang T, Sun D, Zhang Q, Zhang Z. China's drinking water sanitation from 2007 to 2018: a systematic review. Sci Total Environ. (2021) 757:143923. doi: 10.1016/j.scitotenv.2020.143923
2. WHO/UNICEF. Progress on Household Drinking Water, Sanitation and Hygiene 2000-2017: Special Focus on Inequalities. New York, NY: United Nations Children's Fund (UNICEF) and World Health Organization(2019).
3. Pruss-Ustun A, Wolf J, Bartram J, Clasen T, Cumming O, Freeman MC, et al. Burden of disease from inadequate water, sanitation and hygiene for selected adverse health outcomes: an updated analysis with a focus on low- and middle-income countries. Int J Hyg Environ Health. (2019) 222:765–77. doi: 10.1016/j.ijheh.2019.05.004
4. Liu J, Li Y, Jiang J, Zhang X, Sharma VK, Sayes CM. Effects of ascorbate and carbonate on the conversion and developmental toxicity of halogenated disinfection byproducts during boiling of tap water. Chemosphere. (2020) 254:126890. doi: 10.1016/j.chemosphere.2020.126890
5. El-Tawil AM. Colorectal cancers and chlorinated water. World J Gastrointest Oncol. (2016) 8:402–9. doi: 10.4251/wjgo.v8.i4.402
6. Li XF, Mitch WA. Drinking water disinfection byproducts (DBPs) and human health effects: multidisciplinary challenges and opportunities. Environ Sci Technol. (2018) 52:1681–9. doi: 10.1021/acs.est.7b05440
7. Liu J, Zhang X. Comparative toxicity of new halophenolic DBPs in chlorinated saline wastewater effluents against a marine alga: halophenolic DBPs are generally more toxic than haloaliphatic ones. Water Res. (2014) 65:64–72. doi: 10.1016/j.watres.2014.07.024
8. Liu H, Gao Y, Sun L, Li M, Li B, Sun D. Assessment of relationship on excess fluoride intake from drinking water and carotid atherosclerosis development in adults in fluoride endemic areas, China. Int J Hyg Environ Health. (2014) 217:413–20. doi: 10.1016/j.ijheh.2013.08.001
9. Gillette-Guyonnet S, Andrieu S, Nourhashemi F, de La Gueronniere V, Grandjean H, Vellas B. Cognitive impairment and composition of drinking water in women: findings of the EPIDOS Study. Am J Clin Nutr. (2005) 81:897–902. doi: 10.1093/ajcn/81.4.897
10. Sauvant MP, Pepin D. Drinking water and cardiovascular disease. Food Chem Toxicol. (2002) 40:1311–25. doi: 10.1016/S0278-6915(02)00081-9
11. Catling LA, Abubakar I, Lake IR, Swift L, Hunter PR. A systematic review of analytical observational studies investigating the association between cardiovascular disease and drinking water hardness. J Water Health. (2008) 6:433–42. doi: 10.2166/wh.2008.054
12. Cohen A, Pillarisetti A, Luo Q, Zhang Q, Li H, Zhong G, et al. Boiled or bottled: regional and seasonal exposures to drinking water contamination and household air pollution in rural China. Environ Health Perspect. (2020) 128:127002. doi: 10.1289/EHP7124
13. Feng T, Feng Z, Liu Q, Jiang L, Yu Q, Liu K. Drinking habits and water sources with the incidence of cognitive impairment in Chinese elderly population: the Chinese longitudinal healthy longevity survey. J Affect Disord. (2020) 281:406–12. doi: 10.1016/j.jad.2020.12.044
14. Cohen A, Colford JM. Effects of boiling drinking water on diarrhea and pathogen-specific infections in low- and middle-income countries: a systematic review and meta-analysis. Am J Trop Med Hyg. (2017) 97:1362–77. doi: 10.4269/ajtmh.17-0190
15. Dinkel KA, Costa ME, Kraft TS, Stieglitz J, Cummings DK, Gurven M, et al. Relationship of sanitation, water boiling, and mosquito nets to health biomarkers in a rural subsistence population. Am J Hum Biol. (2020) 32:e23356. doi: 10.1002/ajhb.23356
16. Heitzinger K, Rocha CA, Quick RE, Montano SM, Tilley DH, Mock CN, et al. The challenge of improving boiling: lessons learned from a randomized controlled trial of water pasteurization and safe storage in Peru. Epidemiol Infect. (2016) 144:2230–40. doi: 10.1017/S0950268816000236
17. Rosa G, Miller L, Clasen T. Microbiological effectiveness of disinfecting water by boiling in rural Guatemala. Am J Trop Med Hyg. (2010) 82:473–7. doi: 10.4269/ajtmh.2010.09-0320
18. WHO/UNICEF. Safely Managed Drinking Water: A Thematic Report on Drinking Water 2017 (2017). Available online at: https://data.unicef.org/wp-content/uploads/2017/03/safelymanaged-drinking-water-JMP-2017-1.pdf
19. WHO/UNICEF. Progress on Household Drinking Water, Sanitation and Hygiene, 2000–2020: five years into the SDGs. (2021). Available online at: https://data.unicef.org/wp-content/uploads/2022/01/jmp-2021-wash-households_3.pdf
20. Selendy JM. Water and Sanitation-Related Diseases and the Environment: Challenges, Interventions, and Preventive Measures. Hoboken: New Jersey: John Wiley & Sons (2011).
21. Morgan CE, Bowling JM, Bartram J, Kayser GL. Attributes of drinking water, sanitation, and hygiene associated with microbiological water quality of stored drinking water in rural schools in Mozambique and Uganda. Int J Hyg Environ Health. (2021) 236:113804. doi: 10.1016/j.ijheh.2021.113804
22. Ministry of Ecology and Environment. The 2018 Report on the State of the Ecology and Environment in China. Beijing: Ministry of Ecology and Environment (2019).
23. Su HC, Liu YS, Pan CG, Chen J, He LY, Ying GG. Persistence of antibiotic resistance genes and bacterial community changes in drinking water treatment system: from drinking water source to tap water. Sci Total Environ. (2018) 616–7:453–61. doi: 10.1016/j.scitotenv.2017.10.318
24. Shang L, Feng M, Xu X, Liu F, Ke F, Li W. Co-occurrence of microcystins and taste-and-odor compounds in drinking water source and their removal in a full-scale drinking water treatment plant. Toxins. (2018) 10:26. doi: 10.3390/toxins10010026
25. Yang CY, Chiu HF, Cheng MF, Hsu TY, Cheng MF, Wu TN. Calcium and magnesium in drinking water and the risk of death from breast cancer. J Toxicol Environ Health A. (2000) 60:231–41. doi: 10.1080/00984100050027798
26. Rapant S, Cveckova V, Dietzova Z, Fajcikova K, Hiller E, Finkelman RB, et al. The potential impact of geological environment on health status of residents of the Slovak Republic. Environ Geochem Health. (2014) 36:543–61. doi: 10.1007/s10653-013-9580-5
27. Abtahi M, Dobaradaran S, Torabbeigi M, Jorfi S, Gholamnia R, Koolivand A, et al. Health risk of phthalates in water environment: occurrence in water resources, bottled water, and tap water, and burden of disease from exposure through drinking water in tehran, Iran. Environ Res. (2019) 173:469–79. doi: 10.1016/j.envres.2019.03.071
28. Grodin JL, Simon J, Hachamovitch R, Wu Y, Jackson G, Halkar M, et al. Prognostic role of serum chloride levels in acute decompensated heart failure. J Am Coll Cardiol. (2015) 66:659–66. doi: 10.1016/j.jacc.2015.06.007
29. Ferreira JP, Girerd N, Duarte K, Coiro S, McMurray JJ, Dargie HJ, et al. Serum chloride and sodium interplay in patients with acute myocardial infarction and heart failure with reduced ejection fraction: an analysis from the high-risk myocardial infarction database initiative. Circ Heart Fail. (2017) 10:e003500. doi: 10.1161/CIRCHEARTFAILURE.116.003500
30. Bouaziz H, Croute F, Boudawara T, Soleilhavoup JP, Zeghal N. Oxidative stress induced by fluoride in adult mice and their suckling pups. Exp Toxicol Pathol. (2007) 58:339–49. doi: 10.1016/j.etp.2006.11.004
31. Gamkrelidze M, Mamamtavrishvili N, Bejitashvili N, Sanikidze T, Ratiani L. Role of oxidative stress in pathogenesis of atherosclerosis. GeorgianMedNews. (2008) 163:54–7.
32. Amini H, Taghavi Shahri SM, Amini M, Ramezani Mehrian M, Mokhayeri Y, Yunesian M. Drinking water fluoride and blood pressure? An environmental study. Biol Trace Elem Res. (2011) 144:157–63. doi: 10.1007/s12011-011-9054-5
Keywords: groundwater, surface water, tap water, boiled water, mortality
Citation: Liu X, Pei Z, Zhang Z, Zhang Y and Chen Y (2022) Associations of Boiled Water and Lifespan Water Sources With Mortality: A Cohort Study of 33,467 Older Adults. Front. Public Health 10:921738. doi: 10.3389/fpubh.2022.921738
Received: 16 April 2022; Accepted: 27 May 2022;
Published: 27 June 2022.
Edited by:
Fabrizio Bianchi, Italian National Research Council, ItalyReviewed by:
Iman Parseh, Behbahan Faculty of Medical Sciences (BEHUMS), IranNiti B. Jadeja, Ashoka Trust for Research in Ecology and the Environment (ATREE), India
Copyright © 2022 Liu, Pei, Zhang, Zhang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yongjie Chen, Y2hlbnlvbmdqaWVAdG11LmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
 Xun Liu1†
Xun Liu1† Yongjie Chen
Yongjie Chen