- 1Anhui Provincial Center for Disease Control and Prevention, Department of Chronic Non-communicable Disease Prevention and Control, Hefei, China
- 2Department of Rheumatology and Immunology, The First Affiliated Hospital of Anhui Medical University, Hefei, China
- 3Major of Preventive Medicine, School of Public Health, Anhui Medical University, Hefei, China
- 4Department of Radiation Oncology, The First Affiliated Hospital of Anhui Medical University, Hefei, China
- 5First Clinical Medical College, Anhui Medical University, Hefei, China
- 6Department of Epidemiology and Biostatistics, School of Public Health, Anhui Medical University, Hefei, China
Objective: To investigate the detection rate and influencing factors of high-risk population of cardiovascular disease in Anhui province.
Methods: From March 2017 to August 2019, the residents aged 35–75 years old were selected using the multi-stage stratified cluster sampling method in 8 counties and districts of Anhui Province, and questionnaire survey, anthropometric measurement, and collection of biological samples were carried out among them.
Results: A total of 99,821 residents in Anhui Province were finally investigated, and among them 21,426 residents were detected to be high-risk groups of cardiovascular disease. The detection rate of high-risk groups was 21.46%. According to the high-risk types, the high-risk groups can be clustered. 74.57% of them had only one high-risk type, 22.57% of them had two high-risk types, and 2.86% had three or more high-risk types. The results of Generalized Linear Mixed Model (GLMM) showed that male, age ≥45 years old, not married, occupation as a farmer, annual family income <25,000 yuan, drinking, overweight and obesity, pre-central obesity and central obesity, snoring, feeling fatigued, sleepiness, and self-reported history of diabetes were more likely to be risk factors of cardiovascular disease (all P value < 0.05).
Conclusion: The detection rate of high-risk groups of cardiovascular disease in Anhui Province is relatively high. Individualized intervention measures as well as comprehensive prevention and control strategies should be adopted focusing on the distribution characteristics of risk factors of high-risk groups.
Introduction
Cardiovascular disease (CVD) is one of the most important public health issues in the world, which is the leading global cause of mortality, being responsible for 46% of non-communicable disease deaths (1). In China, the CVD mortality ranks first among all causes, accounting for more than 40% of resident disease deaths and the morbidity and mortality of CVD are still on the rise (2–4). China is also one of the countries with the heaviest CVD burden (5). In recent decades, CVD has been a serious health problem in China and the situation has not been alleviated (6). As we all know, people at high risk of CVD are very susceptible to CVD. Increasing evidences showed that early identification of high-risk groups and reasonable intervention and management for their corresponding risk factors can reduce the occurrence of cardiovascular events and premature the death caused by them (7). CVD is also the first cause of deaths in Anhui Province, and the crude mortality rate is still on the rise from 2013 to 2018 (8). However, there are few large-scale epidemiological studies on the investigation of high-risk groups of CVD in Anhui Province. The morbidity and mortality of CVD also vary among provinces or regions due to differences in geographical environment and dietary habits (9). This study organized the early screening of high-risk groups of CVD among community residents in Anhui Province from 2017 to 2019, and analyzed the current situation and related risk factors of high-risk groups, so as to detect high-risk groups in time, take corresponding intervention measures to reduce the occurrence of cardiovascular events in high-risk groups, and provide a basis for the prevention and control of CVD.
Objects and methods
Objects
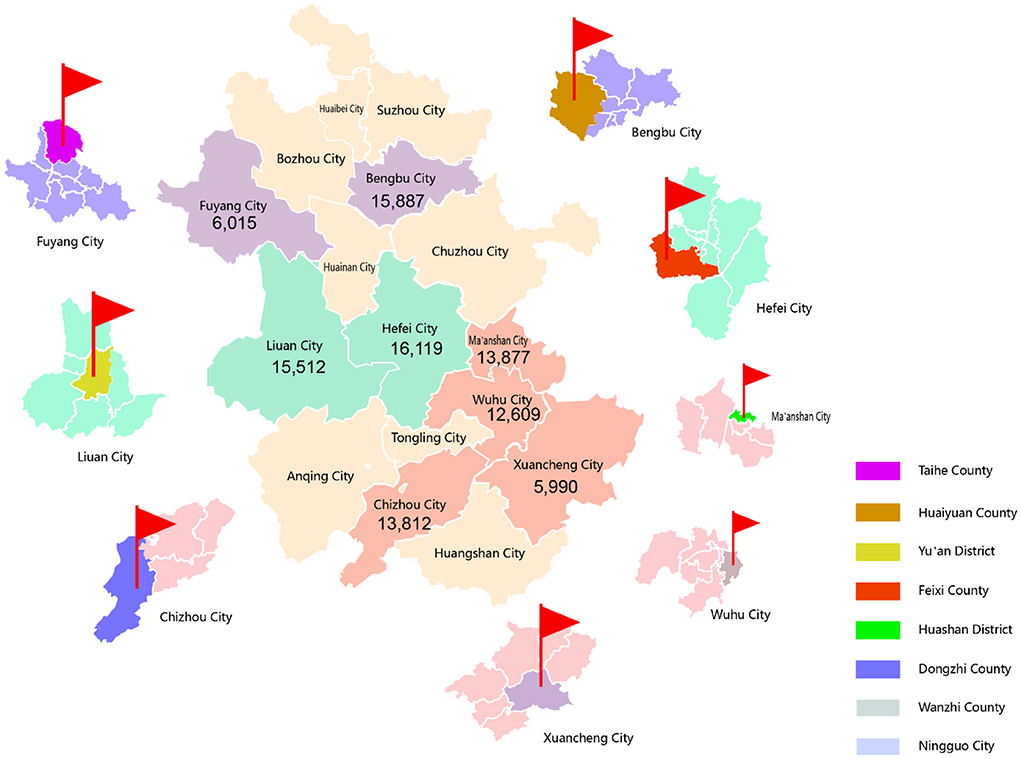
When selecting samples, our investigation employed a convenience sampling approach with a four-level quality control (10). In addition, factors such as geographic location, economy, urban and rural resident population ratio, quality of disease and death registration, and local capacity to support programs were also considered. Ultimately, 8 out of 104 counties/districts in Anhui Province were selected between March 2017 and August 2019 (Figure 1). Among these 8 counties/districts, 4 counties/districts are in southern Anhui (Dongzhi County, Huashan District, Wanzhi County, Ningguo City), 2 counties/districts are in central Anhui (Feixi County, Yu'an District), and 2 counties/districts are in northern Anhui (Taihe County, Huaiyuan County). Among them, 2 counties/districts are urban areas (referring to prefecture-level cities) and six are rural areas. Secondly, we selected 2 to 8 townships or sub-districts from each county/district according to the size and the stability of local residents. Thirdly, the permanent residents aged 35–75 years old in these counties/districts were investigated. Written informed consent was obtained from all participants on entry into the project based on the principle of voluntary.
Methods
Face-to-face investigations were conducted in a centralized post-appointment manner using an electronic data collection system. The main process and content of the primary screening included object identification, informed consent, information registration (collecting basic information such as name, gender, age, education level, occupation, marital status and so on), blood pressure, height, weight, waist circumference measurement, biological sample collection and biochemical indicator detection (detection of blood sugar and lipids and so on), questionnaire survey (collect information on smoking, drinking, hypertension, diabetes and so on). Cardiovascular risk calculation is based on WHO/ISH Cardiovascular Risk Prediction Charts for the Western Pacific Region B (11).
Since any personal identifiable information was not interviewed in this study, participants were informed that their participation was totally voluntarily and they can withdraw from the research during the investigation process without providing any reason, and it had no any adverse effects on the study subjects, thus only verbal informed consent was obtained from the research subjects prior to study commencement. All procedures were undertaken following the ethical standards of the Helsinki Declaration. Verbal informed consents were recorded and the study protocol was approved by The Committee on Medical Ethics of The First Affiliated Hospital of Anhui Medical University.
Indicators and definitions
According to the criteria of high-risk subjects of CVD (12–14), since some survey objects can meet two or more high-risk types at the same time, there is overlap among objects of the four high-risk types, and high-risk subjects can be defined as one, two or more of the following four types at the same time: (1) CVD history: at least one disease history of myocardial infarction (MI), percutaneous coronary intervention (PCI), coronary artery bypass grafting (CABG), and stroke (ischemic or hemorrhagic); (2) hypertension: systolic blood pressure (SBP) ≥160 mmHg or diastolic blood pressure (DBP) ≥100 mmHg; (3)dyslipidemia: low-density lipoprotein cholesterol (LDL-C) ≥160 mg/dL (4.14 mmol/L) or high-density lipoprotein cholesterol (HDL-C) <30 mg/dL (0.78 mmol/L); and (4) high risk: using the information of age, gender, SBP and total cholesterol, smoking status and diabetes or not, the risk of CVD can be determined by a predetermined algorithm derived from the WHO/ISH Cardiovascular Risk Prediction Charts for the Western Pacific Region B (11). Individuals with a 10-years risk of CVD ≥20% are defined as high-risk subjects (10).
In this study, some survey objects can meet two or more high-risk types at the same time, so there is overlap among objects of the four high-risk types. The body mass index (BMI) (15) was used to determine overweight and obesity, and the standard adopted the National Health and Family Planning Commission of China (NHFPC) for Chinese adults, among which low weight: BMI <18.5 kg/m2, normal weight: 18.5 kg/m2 ≤ BMI <24.0 kg/m2, overweight: 24.0 kg/m2 ≤ BMI <28.0 kg/m2, obesity: BMI ≥ 28.0 kg/m2 (10). Using waist circumference to judge central obesity, waist circumference (WC) can be classified as normal (men: waist circumference <85 cm, women: waist circumference <80 cm), pre-central obesity (men: 85 cm ≤ waist circumference <90 cm, women: 80 cm ≤ waist circumference <85 cm), central obesity (men: waist circumference ≥90cm, women: waist circumference ≥85cm). The BMI categories of WHO for adults were as follows, low weight: BMI <18.5 kg/m2, normal weight: 18.5 kg/m2 ≤ BMI <24.9 kg/m2, overweight: 25.0 kg/m2 ≤ BMI <29.9 kg/m2 and obesity: BMI ≥ 30.0 kg/m2. Internationally, WC values >102 cm for men and >88 cm for women are generally classified as abdominal obesity (16). Person that self-reported current smoking and those who had smoked at least 1 day within the past 30 days was defined as smoker. Self-reported drinking alcohol within the past year when surveying was defined as drinker. A person with an affirmative answer of “Over the past 30 days, do you often feel tired, fatigued and sleepy?” would be classified as the person with fatigued and tired (10).
Quality control
The procedures and the methods of investigation were uniform and strictly controlled. The investigators were all doctors or nurses, and they must undergo uniform training and pass the assessment before they participated in this survey. Moreover, we established a four-levels quality control system of province, city, county (district) and individuals in our survey. Quality control teams were set up at each level and professional quality supervisors were trained for quality control. Electronic questionnaires were used in our survey, so the data can be uploaded and updated in a timely manner.
Statistical analysis
Socio-demographic characteristics were described using frequencies for categorical variables, mean and standard deviation (SD) for continuous variables. The χ2 test was used to compare the rate of residents at high risk of CVD in populations with different characteristics. Statistical analysis above all were performed using SPSS 23.0 software. Furthermore, since the sample in this study has a multi-level structure (urban vs. rural, 3 regions of Anhui province), Generalized Linear Mixed Model (GLMM) was used to further analyze the relationship between potential influencing factors of the high-risk groups of CVD, which were found in univariate analysis (P < 0.20), and the high-risk groups of CVD. In GLMM analysis, the two factors, “Urban or rural” and “Region” were analyzed as random intercepts. GLMM analysis were carried out with R 4.1.1 statistical analysis software. The significance tests are two-sided, with a P value ≤ 0.05 considered statistically significant.
Results
Socio-demographic characteristics of participants
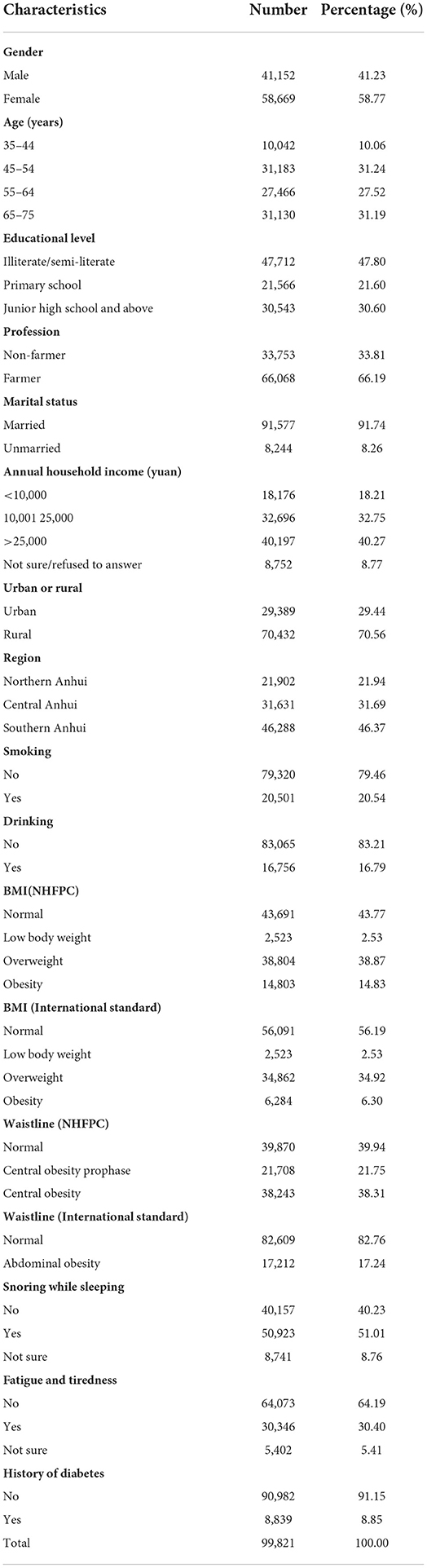
In this study, a total of 99,821 residents in 8 counties (districts) were surveyed. There were 41,152 males (41.23%) and 58,669 females (58.77%), aged between 35 and 75 years, with an average age of (57.72 ± 9.91) years. The majority educational level of the residents was illiterate/semi-literate (47.80%). Among the residents, 66.19% of them were farmers, 91.74% of them were married, 40.27% of them had annual family income > 25,000 yuan, 70.56% of them lived in rural areas, 31.69% of them lived in middle Anhui, 46.37% of them lived in southern Anhui, 20.54% of them were smokers, 16.79% of them were drinkers, 53.70% of them were overweight and obese, and 38.31% of them were central obesity; 30.40% of them felt fatigue/asthenia/drowsiness, 8.85% of them had a self-reported history of diabetes. The demographic characteristics of all participants were shown in Table 1.
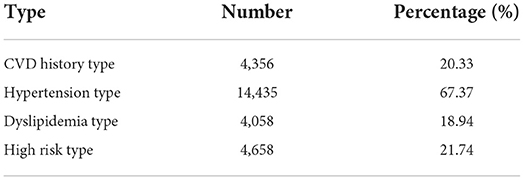
Rate and classification of high-risk groups of CVD
Among the 99,821 participants, the detection rate of high-risk groups was 21.46%. Among high-risk groups, the proportions of CVD history type, hypertension type, dyslipidemia type and high-risk type were 20.33%, 67.37%, 18.94%, and 21.74%, respectively (Table 2). According to the high-risk types, the high-risk groups can be clustered. 74.57% of them had only one high-risk type, 22.57% of them had two high-risk types, and 2.86% had three or more high-risk types.
Detection rate of high-risk groups of CVD among residents with different characteristics
Regarding the detection rate of high-risk groups of CVD, men was higher than women, farmers were higher than other occupational groups, rural areas were higher than urban areas, smokers were higher than non-smokers, drinkers were higher than non-drinkers, and married residents was lower than those of other marital status (all P < 0.05). There were significant differences in detection rates among residents with different BMI, waist circumference, region, different snoring status, and different fatigue and sleepiness status (all P < 0.05). The detection rate of high-risk groups increased with age, and decreased with educational level and annual family income (all P < 0.05). The detection rates of high-risk groups are listed in Table 3.
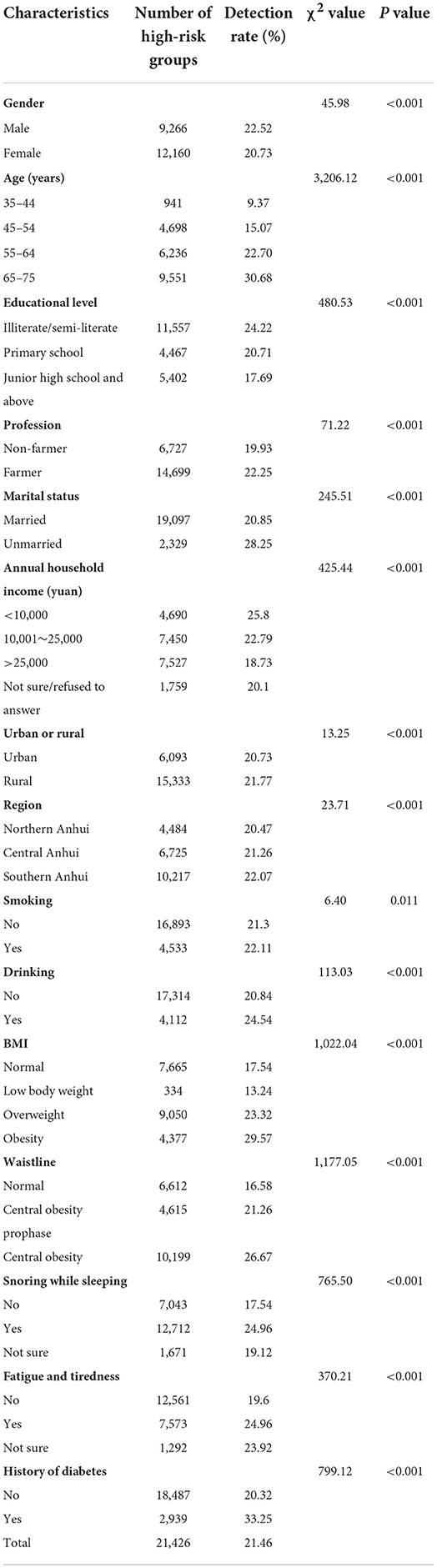
Table 3. Comparison of the detection of high-risk groups of CVD among residents with different characteristics.
The interaction analysis
Given that gender may interact with other factors, the interaction between gender and other influencing factors was analyzed and interactions between gender and marital status, educational level, profession, drinking, snoring and history of diabetes were observed (Supplementary Table 1). Considering the correlation between BMI and waistline, we have analyzed the interaction of BMI and waistline as well. However, no interaction between BMI and waistline was found in the result (Supplementary Table 1).
The stratified analysis by gender
Due to the interaction between gender and some factors, GLMM analysis was conducted separately in male and female (Tables 4, 5). The result in male indicated that age ≥ 45 years old, not married, obtained primary school educational level, annual family income > 25,000 yuan, drinking, low body weight, overweight and obesity, pre-central obesity and central obesity, snoring, feeling fatigued, sleepiness, and self-reported history of diabetes are statistically related to the risk of CVD (Table 4). While in female, age ≥ 45 years old, obtained junior high school and above educational level, occupation as a farmer, annual family income >25,000 yuan, low body weight, overweight and obesity, pre-central obesity and central obesity, snoring, feeling fatigued, sleepiness, and self-reported history of diabetes may be influencing factors of CVD (Table 5).
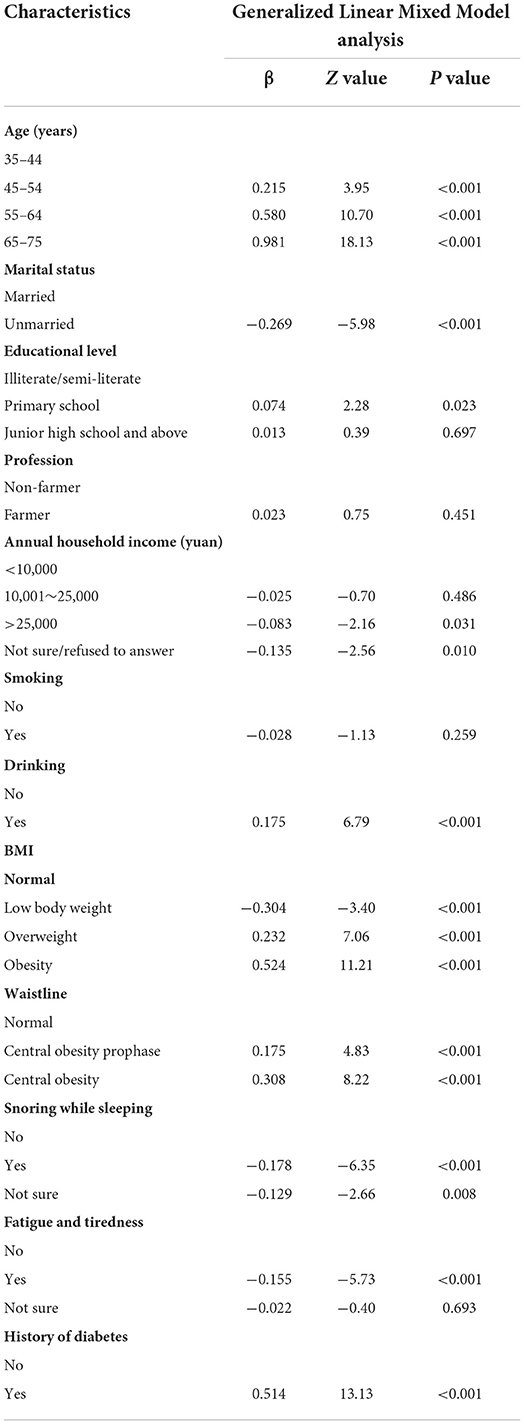
Table 4. Generalized Linear Mixed Model analysis of influencing factors among high-risk groups of CVD in male.

Table 5. Generalized Linear Mixed Model analysis of influencing factors among high-risk groups of CVD in female.
Discussion
The impact of location and environmental conditions, and the differences in socioeconomic development, geographical environment, dietary habits, health resources, and health services among different provinces in China lead to a complex geographic distribution of CVD risk in China. The risk levels of the population in each region are significantly different (9). Anhui Province has a relatively high CVD mortality rate among provinces in China (17, 18). In our study, the detection rate of high-risk groups was 21.46% among 8 counties (districts) of Anhui Province.
It was found that the detection rate of high-risk groups of CVD among male and female was significant different in this survey, which has been suggested to be related to higher tobacco consumption, higher drinking frequency and alcohol consumption in men (19, 20). The result of this study also confirmed that drinking was the influencing factor of CVD in male while no significance in female. However, in this study we did not observe any interaction between gender and smoking, which may be because that the data of smoking we used was qualitative and did not perform quantitative analysis on smoking. It has been reported that heavy drinking has a dose-dependent effect on the increasing of blood pressure, and can increase the risk of diabetes, which all contribute to the increased risk of CVD (20–22). Excessive drinking can also trigger ventricular arrhythmias and sudden cardiac arrest by prolongating QT interval and shortening the atrial effective refractory period (23). Similar evidences were also observed in this study, that the most common type of high-risk groups of CVD was the high blood pressure type (67.37%), suggesting that high blood pressure may be a primary risk factor for CVD. Ettehad D et al. (24) have pointed out that every 10 mmHg decrease in systolic blood pressure is associated with a reduced risk of CVD events, and hypertension is associated with a continuous and graded risk of CVD (25). These all suggest us that through early graded intervention, improving the behavioral habits of high-risk groups and controlling the blood pressure level of hypertensive people, the incidence of CVD may be reduced.
In this study, stratified analysis showed that with primary school level in male and with junior high school or above educational level in female may be protective factors for CVD, which was consistent with the results of previous studies (26, 27). This may be attribute to the fact that people with higher education levels tend to pay more attention to their health and willing to adopt a healthy lifestyle to reduce the risk of CVD. The study found that farmers are more likely to be a high-risk group of CVD than non-farmers in female, but not in male. It has also been indicated that women who worked in agriculture trend to have a higher risk of cerebral infarction, while man did not (28). The specific reason for the difference between male and female needed to be further explored. According to GLMM analysis, it was also found that people with lower annual family income are more likely to become a high-risk group of CVD, suggesting a relationship between the level of income and CVD. This result was similar to a previous result in China (29) and was explained that may be related to the imbalanced distribution of educational and medical resources in their region (30). The univariate analysis showed that the detection rate of high-risk groups of CVD among rural population were higher compared with urban population, which is consistent with the results of previous study (31). The reasons may be related to the rapid urbanization of rural areas in recent years, economic development, changes in consumption levels and lifestyles, lower education levels and the level of medical services in the region. These results suggest that we should strengthen the intervention on the controllable risk factors of CVD in rural populations, especially farmers. Above evidences indicated that targeted measures should be taken to prevent CVD according to the distribution of medical and educational resources in different regions, and more medical resources should be devoted to individuals living in rural areas and with low education levels.
This survey found that sleep snoring is a risk factor for high-risk groups of CVD. Previous study also found that the reduction of sleep time and sleep quality caused by sleep snoring can lead to an increased risk of CVD, possibly by accelerating the metabolism of glucose and lipids, accelerating obesity, causing metabolic disorders, and triggering type 2 diabetes (32). In this survey, it was also found that the detection rate of high-risk groups of CVD is elevated accompanied with the increase of BMI and waistline. It might be result from that individual with higher BMI have higher circulating blood volume, which in turn increases cardiac output, leading to increased burden on the heart, and resulting in a series of CVD events (33, 34). As we all know, obesity is one of the most important public health problems with increasing trend worldwide (35). Obesity is not only an independent risk factor for CVD, but also closely associated with several other risk factors, such as hypertension and diabetes. People with a self-report history of diabetes were observed to be at a higher risk of CVD than those without the history in this survey. Studies reported that diabetes increases the risk of CVD three to four–fold in female and two to three–fold in male (36) and CVD is also the main death reason in diabetic patients (37). In conclusion, the prevention of obesity and diabetes is a key link in the prevention of cardiovascular disease. Although population-wide strategies have been adopted to educate people of all ages, especially children, pregnant women and the elderly (38), with the aging of the population, changes in lifestyle, reduction in physical activity and changes in dietary habits, leading to the increasing incidence of obesity and the prevalence of diabetes year by year (39). Therefore, for high-risk groups, it is necessary to actively take primary and secondary preventive measures to prevent obesity and diabetes, so as to further reduce the incidence of cardiovascular disease, and provide targeted dietary guidance and behavioral interventions.
There are some limitations in the study. Firstly, a convenience sampling approach was employed to recruit amounts of participants in this study, so the representativity and generalizability of our study for the whole Anhui province are limited. Secondly, as a kind of observational study, the ability of confirming the causal relationship between these influencing factors and CVD is restricted. We make up for these limitations through the following aspects. Firstly, the sample of our study is considerable huge to reflect the detection rate and influencing factors of high-risk groups of CVD in Anhui to some extent. Second, the interaction between multiple influencing factors was analyzed to reduce the influence of confounding factors on the results. In addition, GLMM analysis was conducted separately in different gender populations.
Conclusions
The results of this study suggest that the detection rate of high-risk groups of cardiovascular disease in Anhui Province is relatively high, the high risk-groups of CVD in different regions of Anhui Province have different epidemiological characteristics. Therefore, in the future, we should combine the high-risk group strategy with the whole population strategy and take targeted preventive strategies and measures. We should strengthen publicity and education to promote healthy lifestyles, such as no smoking or drinking, strengthening exercise, preventing obesity, etc. We also can identify high-risk groups through early screening in areas with high incidence of CVD, especially those who are already at high risk of hypertension or diabetes.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the Anhui Medical University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
S-ST and Z-RL guided on the design and statistical analyses. X-YX, Z-XW, and Y-WC wrote the manuscript. X-YX had primary responsibility for final content. X-YW, LZ, Y-JC, H-DW, J-QX, and M-XN contributed to data collection and interpretation of findings. All authors contributed to the manuscript editing, read, and approved the final manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.921038/full#supplementary-material
References
1. Kahleova H, Levin S, Barnard ND. Vegetarian dietary patterns and cardiovascular disease. Prog Cardiovasc Dis. (2018) 61:54–61. doi: 10.1016/j.pcad.2018.05.002
2. Du A, Patel SA. D C, Jda E, Cm A. Epidemiology of cardiovascular disease in China and opportunities for improvement. J Am Coll Cardiol. (2019) 73:3135–47. doi: 10.1016/j.jacc.2019.04.036
3. Chen WW, Gao RL, Liu LS, Zhu ML, Wang W, Wang YJ, et al. Report on cardiovascular disease in China (2013). Zhongguo Xun Huan Za Zhi. (2015) 29:487–91.
4. Collaborators GMaCoD. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the global burden of disease study 2013. Lancet. (2015) 385:117–71. doi: 10.1016/S0140-6736(14)61682-2
5. He L, Tang X, Song Y, Li N, Li J, Zhang Z, et al. Prevalence of cardiovascular disease and risk factors in a rural district of Beijing, China: a population-based survey of 58,308 residents. BMC Public Health. (2012) 12:34. doi: 10.1186/1471-2458-12-34
6. Bundy JD, He J. Hypertension and related cardiovascular disease burden in China. Ann Glob Health. (2018) 82:227–33. doi: 10.1016/j.aogh.2016.02.002
7. World Health Organization. Prevention of Recurrent Heart Attacks and Strokes in Low-and Middle-Income Populations: Evidence-Based Recommendations for Policy-Makers and Health Profissionals. Geneva: Publications of the World Health Organization. (2003)
8. Qin H, Chen Y, Da ND, Wei X, Liu Z. Analysis on death causes of residents in Anhui province, 2013. Zhonghua Liu Xing Bing Xue Za Zhi. (2015) 36:976. doi: 10.3760/cma.j.issn.0254-6450.2015.09.015
9. Zhao D, Liu J, Wang M, Zhang X, Zhou M. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol. (2019) 16:203–12. doi: 10.1038/s41569-018-0119-4
10. Lu J, Xuan S, Downing NS, Wu C, Li L, Krumholz HM, et al. Protocol for the China PEACE (patient-centered evaluative assessment of cardiac events) million persons project pilot. BMJ Open. (2016) 6:e010200. doi: 10.1136/bmjopen-2015-010200
11. Ghorpade AG, Shrivastava SR, Kar SS, Sarkar S, Majgi SM, Roy G. Estimation of the cardiovascular risk using world health organization/international society of hypertension (WHO/ISH) risk prediction charts in a rural population of South India. Int J Health Policy Manag. (2015) 4:531–6. doi: 10.15171/ijhpm.2015.88
12. Li X, Wu C, Lu J, Chen B, Li Y, Yang Y, et al. Cardiovascular risk factors in China: a nationwide population-based cohort study. Lancet Public Health. (2020) 5:e672–81. doi: 10.1016/S2468-2667(20)30191-2
13. World Health Organization cardiovascular disease risk charts: revised models to estimate risk in 21 global regions. Lancet Glob Health. (2019) 7:e1332–45. doi: 10.1016/S2214-109X(19)30318-3
14. WorldHealthOrganization. Prevention of Cardiovascular Disease. Guidelines for Assessment and Management of Cardiovascular risk. Geneva: WHO Press, World Health Organization (2007).
15. BeiFan Z. China CM-AGotWGoOi. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. (2002) 15:83–96. doi: 10.1046/j.1440-6047.11.s8.9.x
16. Ross R, Neeland IJ, Yamashita S, Shai I, Seidell J, Magni P, et al. Waist circumference as a vital sign in clinical practice: a consensus statement from the IAS and ICCR working group on visceral obesity. Nat Rev Endocrinol. (2020) 16:177–89. doi: 10.1038/s41574-019-0310-7
17. Zhou M, Wang H, Zhu J, Chen W, Wang L, Liu S, et al. Cause-specific mortality for 240 causes in China during 1990-2013: a systematic subnational analysis for the global burden of disease study 2013. Lancet. (2016) 387:251–72. doi: 10.1016/S0140-6736(15)00551-6
18. Liu S, Li Y, Zeng X, Wang H, Yin P, Wang L, et al. Burden of cardiovascular diseases in China, 1990-2016: findings from the 2016 global burden of disease study. JAMA Cardiol. (2019) 4:342–52. doi: 10.1001/jamacardio.2019.0295
19. Moran AE, Forouzanfar MH, Roth G, Ezzati M, Mensah G, Flaxman A, et al. PM278 The global burden of ischemic heart disease in 1990 and 2010: the global burden of disease 2010 study. Glob Heart. (2014) 9:e117. doi: 10.1016/j.gheart.2014.03.1641
20. Li Z, Bai Y, Guo X, Zheng L, Sun Y, Roselle AM. Alcohol consumption and cardiovascular diseases in rural China. Int J Cardiol. (2016) 215:257–62. doi: 10.1016/j.ijcard.2016.04.095
21. Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA, Ronksley PE, et al. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ. (2011) 342:d671. doi: 10.1136/bmj.d671
22. Polsky S, Akturk HK. Alcohol consumption, diabetes risk, and cardiovascular disease within diabetes. Curr Diab Rep. (2017) 17:136. doi: 10.1007/s11892-017-0950-8
23. O'Keefe EL, DiNicolantonio JJ, O'Keefe JH, Lavie CJ. Alcohol and CV health: Jekyll and Hyde J-curves. Prog Cardiovasc Dis. (2018) 61:68–75. doi: 10.1016/j.pcad.2018.02.001
24. Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. (2016) 387:957–67. doi: 10.1016/S0140-6736(15)01225-8
25. Vasan RS. High blood pressure in young adulthood and risk of premature cardiovascular disease: calibrating treatment benefits to potential harm. JAMA. (2018) 320:1760–3. doi: 10.1001/jama.2018.16068
26. Delpierre C, Lauwers-Cances V, Datta GD, Berkman L, Lang T. Impact of social position on the effect of cardiovascular risk factors on self-rated health. Am J Public Health. (2009) 99:1278–84. doi: 10.2105/AJPH.2008.147934
27. Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet. (2020) 395:795–808. doi: 10.1016/S0140-6736(19)32008-2
28. Fukai K, Furuya Y, Nakazawa S, Kojimahara N, Hoshi K, Toyota A, et al. A case control study of occupation and cardiovascular disease risk in Japanese men and women. Sci Rep. (2021) 11:23983. doi: 10.1038/s41598-021-03410-9
29. Yan R, Li W, Yin L, Wang Y, Bo J. Cardiovascular diseases and risk-factor burden in urban and rural communities in high-, middle-, and low-income regions of China: a large community-based epidemiological study. J Am Heart Assoc Cardiovascul Cerebrovascular Disease. (2017) 6:e004445. doi: 10.1161/JAHA.116.004445
30. Li W, Gu H, Teo KK, Bo J, Wang Y, Yang J, et al. Hypertension prevalence, awareness, treatment, and control in 115 rural and urban communities involving 47 000 people from China. J Hypertens. (2016) 34:39–46. doi: 10.1097/HJH.0000000000000745
31. Wu J, Cheng X, Qiu L, Xu T, Zhu G, Han J, et al. Prevalence and clustering of major cardiovascular risk factors in China: a recent cross-sectional survey. Medicine (Baltimore). (2016) 95:e2712. doi: 10.1097/MD.0000000000002712
32. Yu X, Li ZB, Cjl C, Xin QC, Yqf A, Jiang S. et al. Predicted 10-year cardiovascular disease risk and its association with sleep duration among adults in Beijing-Tianjin-Hebei Region, China. Sci Direct. (2021) 34:803–13. doi: 10.3967/bes2021.109
33. Salvadori A, Fanari P, Mazza P, Agosti R, Longhini E. Work capacity and cardiopulmonary adaptation of the obese subject during exercise testing. Chest. (1992) 101:674–9. doi: 10.1378/chest.101.3.674
34. Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss - sciencedirect. J Am Coll Cardiol. (2009) 53:1925–32. doi: 10.1016/j.jacc.2008.12.068
35. Ortega FB, Lavie CJ, Blair SN. Obesity, Diabetes, and Cardiovascular Diseases Compendium. Circ Res. (2016) 118:1703–5. doi: 10.1161/CIRCRESAHA.116.308999
36. Norhammar A, Schenck-Gustafsson K. Type 2 diabetes and cardiovascular disease in women. Diabetologia. (2013) 56:1–9. doi: 10.1007/s00125-012-2694-y
37. Rao Kondapally Seshasai S, Kaptoge S, Thompson A, Di Angelantonio E, Gao P, Sarwar N, et al. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med. (2011) 364:829–41. doi: 10.1056/NEJMoa1008862
38. Pearce C, Rychetnik L, Wutzke S, Wilson A. Obesity prevention and the role of hospital and community-based health services: a scoping review. BMC Health Serv Res. (2019) 19:453. doi: 10.1186/s12913-019-4262-3
39. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the international diabetes federation diabetes atlas, 9(th) edition. Diabetes Res Clin Pract. (2019) 157:107843. doi: 10.1016/j.diabres.2019.107843
Keywords: cardiovascular disease, high-risk groups, epidemiological characteristics, influencing factors, health education and promotion
Citation: Xing X-Y, Wang Z-X, Cao Y-W, Wang X-Y, Zhang L, Chen Y-J, Wang H-D, Xu J-Q, Niu M-X, Liu Z-R and Tao S-S (2022) The detection rate and influencing factors of high-risk groups of cardiovascular disease in Anhui, China: A cross-sectional study of 99,821 residents. Front. Public Health 10:921038. doi: 10.3389/fpubh.2022.921038
Received: 15 April 2022; Accepted: 11 August 2022;
Published: 25 August 2022.
Edited by:
Xiaodong Sun, Affiliated Hospital of Weifang Medical University, ChinaReviewed by:
Valery Bocquet, Luxembourg Institute of Health, LuxembourgPoobalan Naidoo, King Edward VIII Hospital, South Africa
Copyright © 2022 Xing, Wang, Cao, Wang, Zhang, Chen, Wang, Xu, Niu, Liu and Tao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhi-Rong Liu, bGl1emhpcm9uZzY2JiN4MDAwNDA7MTI2LmNvbQ==; Sha-Sha Tao, dGFvc2hhc2hhMTIxMiYjeDAwMDQwOzEyNi5jb20=
†These authors have contributed equally to this work and share first authorship
 Xiu-Ya Xing1†
Xiu-Ya Xing1† Xin-Yi Wang
Xin-Yi Wang Zhi-Rong Liu
Zhi-Rong Liu Sha-Sha Tao
Sha-Sha Tao