- 1Department of Psychology, Chapman University, Orange, CA, United States
- 2Department of Health Sciences, Chapman University, Orange, CA, United States
Racial and ethnic health disparities are fundamentally connected to neighborhood quality. For example, as a result of historical systemic inequities, racial and ethnic minorities are more likely to live in neighborhoods with signs of physical disorder (e.g., graffiti, vandalism), and physically disordered environments have been noted to associate with increased risk for chronic illness. Degree of exposure to neighborhood disorder may alter peoples' perception of their neighborhoods, however, with those most exposed (e.g., historically marginalized racial/ethnic groups) perhaps perceiving less threat from signs of neighborhood disorder. The purpose of the present study was to examine the complex interrelationships between people and place by investigating whether exposure to neighborhood physical disorder relates to residents' (1) perceptions of neighborhood safety and (2) perceptions of their health, and (3) examining whether these links vary by race/ethnicity. Using 2016–2018 Health and Retirement Study (HRS) data, a representative sample of US adults aged 51 years and older (n = 9,080, mean age 68 years), we conducted a series of weighted linear regressions to examine the role of neighborhood disorder in relation to both perceived neighborhood safety and self-rated health. Results indicated that greater neighborhood physical disorder was statistically significantly related to feeling less safe among non-Hispanic Whites and Hispanics, but not non-Hispanic Blacks. Regarding self-rated health, neighborhood physical disorder was statistically significantly related to poorer health among all racial/ethnic groups. These findings suggest that, despite differential interpretation of neighborhood disorder as a threat to safety, this modifiable aspect of peoples' environment is related to poor health regardless of one's race/ethnicity.
Introduction
According to the World Health Organization (1), the conditions in which people grow up, live, and age are linked to health. Many forms of institutionalized discriminatory practices have contributed to neighborhood disparities where members of marginalized racial/ethnic groups live with more disadvantage in their neighborhoods (2–5). Furthermore, racial/ethnic disparities exist for many health outcomes, whereby non-Hispanic Whites often have better health than those of other racial/ethnic groups (6–8). Moreover, some evidence suggests that racial/ethnic health disparities are no longer evident once socioeconomic factors are considered (9). Critically, neighborhood disadvantage (e.g., poverty, disorder) is associated with poor health among residents (10–12). Researchers have long theorized that economic disinvestment in specific residential areas often leads to the deterioration of those areas, including an increase in signs of neighborhood physical disorder. Neighborhood physical disorder is, in turn, considered the more proximal factor that relates more directly to health than socioeconomic status (SES) (11). Although not the focus of the present study, social aspects of the neighborhood, such as crime, drug use, and loitering, have documented relationships with residents' health as well (3, 4) As such, the neighborhood features with known associations with health, such as neighborhood physical disorder (i.e., neighborhoods with more vandalism, litter, and run-down buildings and property) (4, 11, 13, 14), may be the starting point for understanding persistent connections between racial and ethnic health disparities and place (15–17).
Neighborhoods exhibiting signs of physical disorder, evidenced by signs of decay and lack of social controls (e.g., litter, vandalism), are related to people's withdrawal from public spaces and subsequent health problems (3, 12, 18). Some evidence suggests that neighborhood physical disorder is more normative of marginalized racial/ethnic groups compared to non-Hispanic Whites (19). In fact, some researchers have observed racial/ethnic differences in the report of, and concern about signs of neighborhood disorder (20, 21). For example, when asking a diverse sample of participants about signs of physical disorder in their neighborhoods, researchers observed that non-Hispanic Whites were more likely than other racial/ethnic groups, particularly non-Hispanic Blacks, to report such problems in their neighborhoods (22). This observation suggests that greater exposure to neighborhood disorder may result in different schematic processes whereby neighborhood disorder is more psychological distressing for those least exposed to it. One seemingly obvious question, then, is whether there are racial/ethnic differences in the relationship between neighborhood physical disorder and health.
Few existing studies investigate racial/ethnic differences in links between neighborhood physical disorder and residents' racial and ethnic characteristics, and none to our knowledge investigate health outcomes. Further, the paucity of research examining perceived disorder by racial and ethnic characteristics has been inconclusive. In one investigation, perceived neighborhood disorder was related to greater depletion of personal control, or the perception that one has control over their life outcomes (23). This relationship was greater among non-Hispanic Whites than non-Whites, however. The authors attributed this racial difference to a greater mismatch between personal and neighborhood statuses (e.g., SES) among non-Hispanic Whites compared to non-Hispanic Blacks, with this mismatch leading to greater cognitive dissonance among non-Hispanic Whites. The authors coined the term “Status Discord” to describe this phenomenon (23). Others have similarly posited that neighborhood disorder may be more detrimental to non-Hispanic Whites than non-Hispanic Blacks, but with a different rationale (24). The “epidemiological paradox” is described as a process by which marginalized racial/ethnic groups, given their greater exposure to disordered neighborhoods, develop greater coping and resilience and may thus fare better than their non-Hispanic White counterparts (24). In a more recent investigation, greater perceived neighborhood disorder was related to a depletion of personal mastery, or the belief that life chances are under a degree of personal influence (25). Although this investigation also observed a racial difference, the direction was markedly different; the disorder-mastery link was more evident among non-Hispanic Blacks than non-Hispanic Whites. Gilster (25) argued that the racial/ethnic difference observed in the disorder-mastery link can be explained by a situation of compound risk, or that non-Whites experience a greater accumulation of personal and neighborhood stressors than do non-Hispanic Whites. The Stress Process Model has long posited that those with fewer personal resources, those with more chronic or repeated stressors, and certainly those with both, will fare the worse health outcomes than those with more resources or fewer stressors. The Stress Process Model may thus be a suitable model to inform our understanding of when and how neighborhood physical disorder may be worse for non-Whites than non-Hispanic Whites (26).
Yet, some studies have reported no racial/ethnic differences in links between neighborhood features and indices of health (smoking, drinking, depression & walking behaviors) (27). The paucity of research on potential racial/ethnic differences in relationships between neighborhood physical disorder and health creates a critical gap in our understanding of health disparities. For example, scholars such as Millar (24) have argued that “taken together, there are limited and inconsistent findings on the relationship between neighborhood-level contexts and health and health-promoting behaviors across race and ethnicity.” The goals of the present study are both theoretically and policy motivated. The theoretical goal of the present analyses is to further characterize the subjective experience of neighborhood disorder among a diverse group of older US adults. An additional project goal is to identify differential vulnerability to physical disorder, a modifiable aspect of peoples' neighborhoods, among various racial/ethnic groups to inform policies that attend to neighborhood-level contextual conditions, focusing here on trash, vandalism, and safety concerns. As such, using national data from the Health and Retirement Study (HRS), this study investigated both perceptions of neighborhood safety and self-rated health in the context of neighborhood physical disorder as rated by third-party surveyors. The hypothesized relationships were assessed separately by groups of people self-identifying as non-Hispanic White, non-Hispanic Black, and Hispanic. Specifically:
1. To what extent does neighborhood physical disorder relate to residents' perceptions of safety in their neighborhoods?
2. To what extent does neighborhood physical disorder relate to residents' perceptions of their health?
3. To what extent do the above hypothesized links differ by race/ethnicity?
Materials and methods
Data
The HRS is a nationally representative sample of more than 20,000 US men and women aged 51 years and older, with data collected biannually since 1992 (28). HRS recruited households using a four-stage area probability sample design (29). The purpose of the HRS study is to examine the socioeconomic and health status of the older US population. HRS introduced enhanced face-to-face interviews (EFTF) in 2006 with a random half of the sample, and completed the EFTF with the other half in 2008. The EFTF allows for HRS interviewers to survey the area surrounding the participants' homes, as well as to leave behind a psychosocial questionnaire asking for participants' perceptions of neighborhood safety. HRS health records are linked to contextual data resources (CDR) that involves multiple sources of data, such as the American Community Survey (ACS) used in the current analyses (30). The present study uses the most recent 2016/2018 waves of HRS data to investigate relationships between HRS interviewer ratings of neighborhood physical disorder on participants' perceptions of neighborhood safety and self-rated health. Participants signed consent forms prior to data collection and research procedures were approved by the University of Michigan's Institutional Review Board.
Measures
Perceived neighborhood safety
HRS participants answered a single item from the psychosocial leave-behind questionnaire, “People feel safe walking alone in this area after dark” (31). Responses ranged from 1 to 7, and these values were reverse-coded such that higher values indicated feeling safer.
Self-rated health
Health and Retirement Study participants reported their health with the following item, “Would you say your health is excellent, very good, good, fair, or poor?” These responses ranged from 1 to 5 and were revere-coded so that higher values indicated better health.
Race/ethnicity
Racial/ethnic categories were coded as the following: non-Hispanic Whites (1), non-Hispanic Blacks (2), and Hispanics (3).
Neighborhood physical disorder
Health and Retirement Study interviewers indicated whether the following were present within sight of the participant homes: vandalism, trash/litter/junk in the street/road, trash/litter/junk around the buildings in neighborhood, abandoned cars, and rundown yards. These items were coded as 0 = not present or 1 = present. A neighborhood physical disorder scale was then constructed by summing across the five indicators, with higher scores indicating more neighborhood physical disorder.
Covariates
Three census tract-level variables were included as covariates and were available via the ACS 2012–2016 5-year estimates (30). First, concentrated disadvantage was constructed by averaging three standardized scores: proportion unemployed, proportion female-headed households, and proportion in poverty. This measure adjusts for area SES to demonstrate the disorder-health link above and beyond associations with area SES. In order to achieve this, each of the three individual scores were standardized from the mean. Next, population density was defined as the total population per square mile. Lastly, racial/ethnic diversity was constructed by subtracting from the total population the proportions of the following racial/ethnic groups: non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, non-Hispanic “Other,” and Hispanic (32). Several individual-level sociodemographic variables from the 2016 HRS tracker file were included as covariates. Age was coded in years and sex was coded as 0 = men and 1 = women. Education was coded as the following: 0 = no degree, 1 = General Educational Development (GED), 2 = high school diploma, 3 = 2-year college degree, 4 = 4-year college degree, 5 = master's degree, 6 = professional degree (Ph.D., M.D., J.D).
Statistical analysis
To account for HRS's complex survey design, weighted analyses were conducted in Stata 17 using the svy: suite of commands. A series of linear regressions stratified by race/ethnicity examined the hypothesized relationships between neighborhood physical disorder and the two outcomes, perceived neighborhood safety and self-rated health. The first model investigated the hypothesis that greater neighborhood physical disorder would be related to more safety concerns among participants. The second model examined whether greater neighborhood physical disorder would be related to poorer self-rated health. Finally, stratified regression coefficients were investigated to determine the presence of racial/ethnic differences in these hypothesized relationships. All models adjusted for age, sex, and highest educational degree as well as census tract concentrated disadvantage, population density, and racial/ethnic diversity.
Results
Participant description
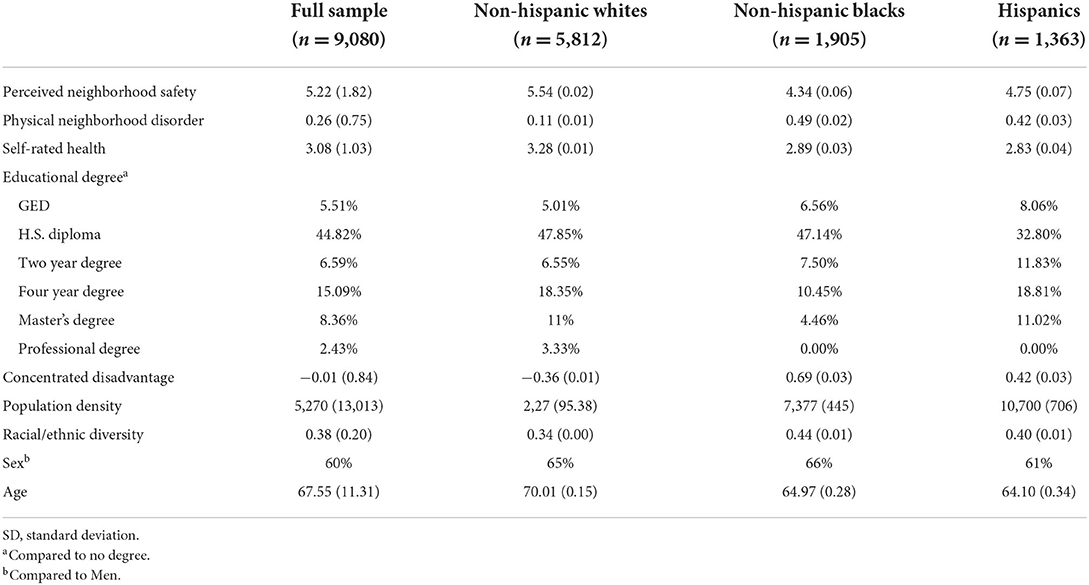
The sample (n = 9,080) had an average age of 68 years and was 60% female. The majority of the sample were non-Hispanic Whites (n = 5,812), followed by non-Hispanic Blacks (n =1,905), and Hispanics (n =1,363). Overall, the HRS participants reported good/fair health and feeling somewhat safe in their neighborhoods. Interviewer ratings of neighborhood physical disorder was generally low. A description of the analytic variables reported separately by race/ethnicity can be found in Table 1.
Race/ethnicity, neighborhood disorder, perceived safety, and self-rated health
Results of the weighted linear regressions predicting perceived neighborhood safety are presented in Table 2. Among non-Hispanic Whites (coef. = −0.42, p < 0.001) and Hispanics (coef. = −0.24, p < 0.05), greater neighborhood physical disorder was significantly related to feeling less safe in one's neighborhood. The relationship between neighborhood physical disorder and perceived neighborhood safety was not significant among non-Hispanic Blacks. Among non-Hispanic Blacks and Hispanics, level of education was not statistically significantly related to perceived neighborhood safety. Results of the weighted linear regressions predicting self-rated health can be found in Table 3. Greater neighborhood physical disorder was significantly related to poorer self-rated health among non-Hispanic Whites (coef. = −0.15, p < 0.001), non-Hispanic Blacks (coef. = −0.13, p < 0.001), and Hispanics (coef. = −0.11, p < 0.05). Greater concentrated disadvantage was statistically significantly related to lower ratings of health, but only for non-Hispanic Whites. For non-Hispanic Whites and non-Hispanic Blacks, greater age was statistically significantly related to poorer health evaluations.
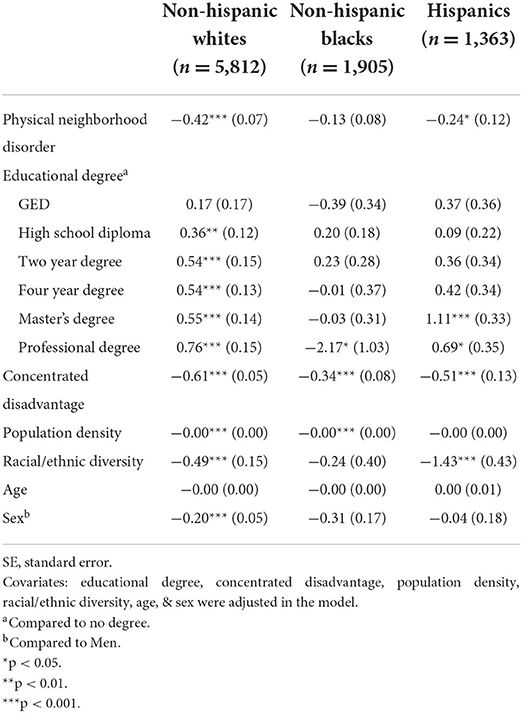
Table 2. Weighted linear regressions predicting perceived neighborhood safety by neighborhood physical disorder, [coefficient (SE)].
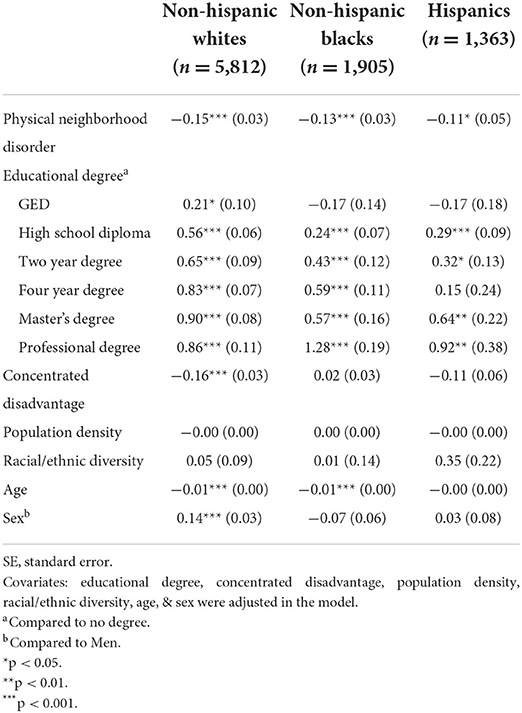
Table 3. Weighted linear regressions predicting self-rated health by neighborhood physical disorder, [coefficient (SE)].
Discussion
This study adds new knowledge in understanding racial/ethnic health disparities among older adults, particularly for the two largest health disparity populations in the US. Older adults may spend more time in their neighborhoods as they transition out of the workforce, thus rendering neighborhoods a potentially more important determinant of health at this point in the lifespan (33, 34). There are racial/ethnic differences in neighborhood quality and health, and the neighborhood disparities may explain the health disparities. Yet, few studies have investigated racial/ethnic differences in the link between neighborhood disorder and older adults' health. Results of these scant studies have sometimes found that neighborhood physical disorder is worse for psychosocial outcomes among non-Hispanic Whites than non-Hispanic Blacks. Some researchers argued that the racial/ethnic difference in the effect of neighborhood disorder is explained by non-Hispanic Whites finding disorder as more threatening to personal safety (22). However, that assumption has never been empirically tested. Thus, we set out to test this assumption by comparing racial/ethnic groups on the link between neighborhood physical disorder as rated by third parties on (1) perceived neighborhood safety and (2) a specific health outcome, self-rated health. One strength of the current analysis was use of a neighborhood physical disorder scale rated by third parties to minimize concerns regarding common source bias (13), as one of the primary outcomes investigated herein was neighborhood safety as rated by the participants. The present study found that, although greater neighborhood physical disorder was related to more safety concerns among non-Hispanic Whites and Hispanics, the same was not true for non-Hispanic Blacks. That said, greater neighborhood physical disorder was related to worse self-rated health among all racial/ethnic groups.
Neighborhood physical disorder and safety
Neighborhood physical disorder can be measured or defined in different ways. For example, some researchers have used the term “physical decay” and have included items such as “cigarettes in the street,” “protest or political message grafitti”) (13, 35). The current study defined neighborhood physical disorder using the presence of vandalism, trash on the streets/yards, and abandoned cars that build upon another well-established definition (3). Despite these nuanced differences in the definition, the presence of neighborhood physical disorder is known to be associated with an array of health-related outcomes such as decreased physical fitness (14), and diminishes a sense of trust and security in the surrounding area (36). Less literature has examined the link between neighborhood physical disorder and health among diverse racial/ethnic groups.
The theories of Status discord (23) and Epidemiological paradox (24) both argue that non-Hispanic Whites are more threatened than non-Hispanic Blacks by signs of neighborhood physical disorder. To our knowledge, no formal investigation exists regarding whether or not racial/ethnic groups differ in their perceptions of safety in relation to neighborhood physical disorder to substantiate these claims. The present study is among the first to investigate this argument, and in support of this hypothesis, results indicated that non-Hispanic White and Hispanic residents embedded in areas with greater physical disorder reported significantly greater perceived neighborhood safety concerns. Although our findings somewhat support the Status Discord and Epidemiological Paradox theories, we were unable to further compare the two theories, as HRS does not contain measures of cognitive dissonance or resilience, the proposed mechanisms for the racial/ethnic differences posited in these theories.
Neighborhood physical disorder and self-rated health
All three groups (non-Hispanic White, non-Hispanic Black, and Hispanic) reported significantly worse health if they were living in areas with more signs of neighborhood physical disorder. To our knowledge, this is among one of the first studies to investigate racial/ethnic differences in links between neighborhood physical disorder and health. The only other investigation similar to the present study was Echeverria's et al. (27) which examined neighborhood characteristics (e.g., neighborhood problems and neighborhood cohesion) and found no racial/ethnic differences in lifestyle behaviors (e.g., smoking, depression, drinking, and exercise activity). Our results are consistent with these past findings as there were no racial/ethnic differences in the disorder-self-rated health link. On average, non-Hispanic Whites live in relatively economically advantaged neighborhoods with less disorder than non-Whites (20, 37, 38). In addition, non-Hispanic Whites have better health compared to other racial/ethnic groups (39, 40). So, although we found that neighborhood physical disorder elicits more safety concerns among non-Hispanic Whites and Hispanics than non-Hispanic Blacks, our results clearly do not suggest that signs of disorder should only be ameliorated in primarily non-Hispanic White neighborhoods. Conversely, given no significant differences in the association between neighborhood physical disorder and self-reported health across the racial/ethnic groups assessed in the current study, our results suggest that community-level interventions targeting neighborhood physical disorder may not only improve community-level health, but minimize racial/ethnic health disparities. However, these neighborhood-level interventions should be dovetailed by policies that ensure equitable housing policies for affected communities. Established forms of interventions include modeling and strengthening a sense of community among neighbors in order to promote higher usage of public spaces and increasing attachment (41). Community organized efforts may also include the remediation of disordered environments (e.g., cleaning up litter, removing graffiti) (2, 14).
Limitations and future directions
Health and Retirement Study is a national sample of US older adults. Although older adults have a lower likelihood of being victimized, they nevertheless report more safety concerns in their neighborhoods compared to younger adults (42). As such, findings from the present study may not generalize to younger samples of US residents. While the current study has many strengths, there are some notable limitations. First, HRS participants self-reported non-Hispanic White, non-Hispanic Black, and Hispanic status, and when these categories do not accurately capture a participant's racial/ethnic status, the participant selects “other.” The “other” category likely includes a diverse sample of individuals, including those who may be multi-racial, and were not included in the present study given the inability to make meaningful comparisons. Additionally, HRS lacks sufficient data to further disentangle different racial groups who each identify as Hispanic, and as such, those groups were equated for the purposes of the present analyses. Future studies with appropriate data may benefit from additional within- and between-group comparisons. Second, HRS lacks adequate data to operationalize other forms of disorder that have been identified in the neighborhood literature (e.g., social disorder, including drug use) and the pattern of relationships between neighborhood social disorder and various health outcomes, and racial/ethnic differences therein, may differ from that of neighborhood physical disorder. Third, both of the outcomes evaluated in the present study, perceived neighborhood safety and health, were self-reported. Although HRS collects data on classic single-item perceived neighborhood safety and self-rated health items, with the latter receiving substantial validation in published research (43), we acknowledge that these items are subjective, and more comprehensive measures of these constructs may increase reliability of the outcomes measured in the present study. Fourth, HRS does not ask participants how long they have lived in their current neighborhoods, precluding the ability to investigate whether participants may acclimate to signs of disorder in their neighborhoods, or whether the associations with disorder may accumulate over time in relation to residents' health. Lastly, future research should investigate objectively-assessed health outcomes to overcome potential self-report biases which may further vary systematically by race/ethnicity. Future research should incorporate more comprehensive scales of perceived neighborhood safety and health. Nevertheless, the current study is among the first to characterize the nuanced ways in which neighborhood physical disorder relates to people's subjective experiences of their environments and their health.
Conclusion
The theoretical aim of the study was to examine the subjective experience of neighborhood physical disorder among a diverse group of older US adults, as neighborhood environments are viewed in the eyes of the beholder. The policy aim was to identify potential differential vulnerability to neighborhood physical disorder, which is a modifiable aspect of neighborhoods. The significant association between neighborhood physical disorder and self-rated health highlights that all racial/ethnic groups may benefit from neighborhood-level interventions. As racial/ethnic disparities continue to be a national concern, it is imperative to include interventions for those living in disordered areas. Feeling safe may promote health-promoting behaviors which can improve health and wellbeing for all members of society. Given that neighborhood factors such as neighborhood physical disorder is part and parcel of the social determinants of health framework, this work aligns with the Healthy People 2030 goal for promoting better health for all individuals, community health, and in turn improving the quality of life for all (Social determinants 2030) (44).
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by University of Michigan, Institutional Review Board. The patients/participants provided their written informed consent to participate in this study.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Funding
This research was based on work supported by a National Institutes of Health/National Institute on Aging Career Development Grant (4R00AG055699-03) to JR, Ph.D, and further supported by NIA (U01AG009740 and R21AG045625) to support Health & Retirement Study (HRS) data collection and the development of the HRS contextual data resource. Further, this research was also supported by Chapman University's Innovation in Diversity and Inclusion Research, Scholarship, and Creative Activity awarded to AV and JR. Not all data used in the present study are publicly available, but rather are accessible via a restricted data use agreement. Both public and restricted data are acquired via the HRS website (https://hrs.isr.umich.edu). These analyses were not preregistered.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Health equity considerations and racial and ethnic minority groups. Centers for Disease Control and Prevention. Available online at: https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html (accessed March 31, 2022).
2. Douglas JA, Subica AM, Franks L, Johnson G, Leon C, Villanueva S, et al. Using participatory mapping to diagnose upstream determinants of health and prescribe downstream policy-based interventions. Prev Chronic Dis. (2020) 17:E138. doi: 10.5888/pcd17.200123
3. Ross CE, Mirowsky J. Disorder and decay: the concept and measurement of perceived neighborhood disorder. Urban Aff Rev. (1999) 34:412–32. doi: 10.1177/107808749903400304
4. Steve SL, Tung EL, Schlichtman JJ, Peek ME. Social disorder in adults with type 2 diabetes: building on race, place, and poverty. Curr Diab Rep. (2016) 16:1–9. doi: 10.1007/s11892-016-0760-4
5. Groos M, Wallace M, Hardeman R, Theall KP. Measuring inequity: a systematic review of methods used to quantify structural racism. J Health Dispar Res Pract. (2018) 11:13. Available online at: https://digitalscholarship.unlv.edu/jhdrp/vol11/iss2/13
6. Williams DR, Sternthal M. Understanding racial-ethnic disparities in health: Sociological contributions. J Health Soc Behav. (2010) 51(1_suppl): S15–27. doi: 10.1177/0022146510383838
7. Williams DR, Mohammed SA, Leavell J, Collins C. Race, socioeconomic status, and health: Complexities, ongoing challenges, and research opportunities. Ann N Y Acad Sci. (2010) 1186:69–101. doi: 10.1111/j.1749-6632.2009.05339.x
8. CDC Health Disparities inequalities report —United States 2011. (2011). Available online at: https://www.cdc.gov/mmwr/pdf/other/SU6001.pdf (accessed March 31, 2022).
9. Conley D. Getting into the Black: Race, wealth, and public policy. Polit Sci Q. (1999) 114:595–612. doi: 10.2307/2657785
10. Hill TD, Ross CE, Angel RJ. Neighborhood disorder, psychophysiological distress, and health. J Health Soc Behav. (2005) 46:170–86. doi: 10.1177/002214650504600204
11. Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. (2010) 1186:125–45. doi: 10.1111/j.1749-6632.2009.05333.x
12. Robinette JW, Charles ST, Gruenewald TL. Neighborhood cohesion, neighborhood disorder, and cardiometabolic risk. Soc Sci Med. (2018) 198:70–6. doi: 10.1016/j.socscimed.2017.12.025
13. Marco M, Gracia E, Tomás JM, López-Quílez A. Assessing neighborhood disorder: Validation of a three-factor observational scale. Eur J Psychol Appl Leg Context. (2015) 7:81–9. doi: 10.1016/j.ejpal.2015.05.001
14. Douglas JA, Briones MD, Bauer EZ, Trujillo M, Lopez M, Subica AM. Social and environmental determinants of physical activity in urban parks: testing a neighborhood disorder model. Prev Med. (2018) 109:119–24. doi: 10.1016/j.ypmed.2018.01.013
15. Acevedo-Garcia D, Lochner KA, Osypuk TL, Subramanian SV. Future directions in residential segregation and health research: a multilevel approach. Am J Public Health. (2003) 93:215–21. doi: 10.2105/AJPH.93.2.215
16. Schulz A, Northridge ME. Social determinants of health: implications for environmental health promotion. Health Educ Behav. (2004) 31:455–71. doi: 10.1177/1090198104265598
17. LaVeist TA, Thorpe RJ, Galarraga JE, Bower KM, Gary-Webb TL. Environmental and socio-economic factors as contributors to racial disparities in diabetes prevalence. J Gen Intern Med. (2009) 24:1144–8. doi: 10.1007/s11606-009-1085-7
18. Ellen IG, Mijanovich T, Dillman K-N. Neighborhood effects on health: exploring the links and assessing the evidence. J Urban Aff. (2001) 23:391–408. doi: 10.1111/0735-2166.00096
19. Cho W, Ho AT. Does neighborhood crime matter? A multi-year survey study on perceptions of race, victimization, and public safety. Int J Law Crime Justice. (2018) 55:13–26. doi: 10.1016/j.ijlcj.2018.08.002
20. Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. (2001) 116:404–16. doi: 10.1016/S0033-3549(04)50068-7
21. Roosa MW, Burrell GL, Nair RL, Coxe S, Tein J-Y, Knight GP. Neighborhood disadvantage, stressful life events, and adjustment among Mexican American early adolescents. J Early Adolesc. (2009) 30:567–92. doi: 10.1177/0272431609338177
22. Sullivan DM, Bachmeier JD. Racial differences in perceived disorder in three gentrifying neighborhoods. Adv Appl Soc. (2012) 02:229–36. doi: 10.4236/aasoci.2012.23030
23. Kim J, Conley ME. Neighborhood disorder and the sense of personal control: which factors moderate the association? J Community Psychol. (2011) 39:894–907. doi: 10.1002/jcop.20476
24. Millar RJ. Neighborhood cohesion, disorder, and physical function in older adults: an examination of racial/ethnic differences. J Aging Health. (2019) 32:1133–44. doi: 10.1177/0898264319890944
25. Gilster ME. Racial and ethnic differences in the neighborhood context of mastery. J Community Psychol. (2015) 44:38–50. doi: 10.1002/jcop.21741
26. Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT. The stress process. J Health Soc Behav. (1981) 22:337. doi: 10.2307/2136676
27. Echeverría S, Diez-Roux AV, Shea S, Borrell LN, Jackson S. Associations of neighborhood problems and neighborhood social cohesion with mental health and health behaviors: the multi-ethnic study of Atherosclerosis. Health Place. (2008) 14:853–65. doi: 10.1016/j.healthplace.2008.01.004
28. Juster FT, Suzman R. An overview of the Health and Retirement Study. J Hum Resour. (1995) 30:S7. doi: 10.2307/146277
29. Heeringa SG, Connor JH. Technical Description of the Health and Retirement Study Sample Design. Ann Arbor, MI: Institute for Social Research (1995). doi: 10.7826/ISR-UM.06.585031.001.05.0001.1995
30. Ailshire J, Mawhorter S, Choi EY. Contextual Data Resource (CDR): US Decennial Census and American Community Survey Data, 1990-2018, Version 2.0. Los Angeles, CA: USC/UCLA Center on Biodemography and Population Health (2020).
31. Mendes de. Leon CF, Cagney KA, Bienias JL, Barnes LL, Skarupski KA, Scherr PA, et al. Neighborhood Social Cohesion and disorder in relation to walking in community-dwelling older adults. J Aging Health. (2009) 21:155–71. doi: 10.1177/0898264308328650
32. Subica AM, Douglas JA, Kepple NJ, Villanueva S, Grills CT. The geography of crime and violence surrounding tobacco shops, medical marijuana dispensaries, and off-sale alcohol outlets in a large, urban low-income community of color. Prev Med. (2018) 108:8–16. doi: 10.1016/j.ypmed.2017.12.020
33. Nathan A, Villanueva K, Rozek J, Davern M, Gunn L, Trapp G, et al. The role of the built environment on health across the life course: a call for collaboraction. Am J Health Promot. (2018) 32:1460–8. doi: 10.1177/0890117118779463a
34. Velasquez AJ, Douglas JA, Guo F, Robinette JW. What predicts how safe people feel in their neighborhoods and does it depend on functional status? SSM Popul Health. (2021) 16:100927. doi: 10.1016/j.ssmph.2021.100927
35. Kubrin Charise. Making order of disorder: a call for conceptual clarity. Criminol Public Policy. (2008) 7:203–13. doi: 10.1111/j.1745-9133.2008.00502.x
36. Fritz H, Cutchin MP, Cummins ER. Loss of trust in the neighborhood: the experience of older African Americans in Detroit. J Gerontol B. (2018) 73:e108–19. doi: 10.1093/geronb/gby019
37. Karriker-Jaffe KJ, Liu H. Johnson RM. Racial/ethnic differences in associations between neighborhood socioeconomic status, distress, and smoking among US adults. J Ethn Subst Abuse. (2015) 15:73–91. doi: 10.1080/15332640.2014.1002879
38. Ferraro KF, Kemp BR, Williams MM. Diverse aging and health inequality by race and ethnicity. Innov Aging. (2017) 1:igx002. doi: 10.1093/geroni/igx002
39. Cagney KA, Browning CR, Wen M. Racial disparities in self-rated health at older ages: what difference does the neighborhood make? J Gerontol B Psychol Sci Soc Sci. (2005) 60:S181–90. doi: 10.1093/geronb/60.4.S181
40. Health United States 2015: 2015: With special feature on racial and ethnic health disparities. National Center for Biotechnology Information. U.S. National Library of Medicine (2016). Available online at: https://pubmed.ncbi.nlm.nih.gov/27308685/ (accessed March 31, 2022).
41. Francis J, Giles-Corti B, Wood L, Knuiman M. Creating sense of community: the role of public space. J Environ Psychol. (2012) 32:401–9. doi: 10.1016/j.jenvp.2012.07.002
42. Snedker KA. Neighborhood conditions and fear of crime. Crime Delinquency. (2010) 61:45–70. doi: 10.1177/0011128710389587
43. Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. (1997) 38:21–37. doi: 10.2307/2955359
44. Social Determinants of Health. Social Determinants of Health - Healthy People 2030. Available online at: https://health.gov/healthypeople/objectives-and-data/social-determinants-health (accessed March 31, 2022).
Keywords: race/ethnicity, neighborhood physical disorder, self-rated health, perceived neighborhood safety, vulnerability
Citation: Velasquez AJ, Douglas JA, Guo F and Robinette JW (2022) In the eyes of the beholder: Race, place and health. Front. Public Health 10:920637. doi: 10.3389/fpubh.2022.920637
Received: 14 April 2022; Accepted: 27 July 2022;
Published: 12 August 2022.
Edited by:
Yvonne Baumer, National Heart, Lung, and Blood Institute (NIH), United StatesReviewed by:
Marcus R. Andrews, National Heart, Lung, and Blood Institute (NIH), United StatesNicole Farmer, Clinical Center (NIH), United States
Copyright © 2022 Velasquez, Douglas, Guo and Robinette. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alfredo J. Velasquez, YWp2ZWxhc3F1ZXpAdXRleGFzLmVkdQ==
 Alfredo J. Velasquez
Alfredo J. Velasquez Jason A. Douglas
Jason A. Douglas Fangqi Guo1
Fangqi Guo1 Jennifer W. Robinette
Jennifer W. Robinette