- 1Department of Health Policy and Management, School of Public Health, Hangzhou Normal University, Hangzhou, China
- 2Department of Administration, School of Public Administration, Hangzhou Normal University, Hangzhou, China
Background: Patient-centered care (PCC) is globally recognized as a high-quality and high-value healthcare service. It emphasizes the broad participation of patients and families in health-related decision-making and the provision of healthcare services that cater to patients' needs, preferences, and values. However, the mechanisms driving healthcare workers' provision of PCC are yet to be fully uncovered.
Methods: Using stratified random sampling, we recruited 1,612 healthcare workers from different levels of public hospitals in Hangzhou. We conducted survey interviews using questionnaires based on psychometrically sound scales. Structural equation modeling was used to analyze the effects of hospital culture, self-efficacy, and achievement motivation on the perceived provision of PCC by healthcare workers and to explore the mechanisms underlying their relationships.
Results: Self-efficacy had a positive mediating effect in the relationship between hospital culture and healthcare workers' perceived provision of PCC (β = 0.424, p < 0.001). Furthermore, the pursuit of success positively moderated the mediating role of self-efficacy (β = 0.128, p < 0.001), whereas, the avoidance of failure negatively moderated the mediating role of self-efficacy (β = -0.017, p < 0.001).
Conclusion: The findings suggest that hospitals should foster patient-centered and innovative cultures and develop strategies focusing on both internal motivation (self-efficacy and achievement motivation) and external environments (hospital culture) to help and encourage healthcare workers to implement PCC. For example, hospitals could further communication skills training, enhance leadership, build team spirit, and promote collaboration among healthcare workers.
Introduction
The notion of patient-centered care (PCC) was first proposed by Balint in 1995 to express the belief that healthcare workers—who are involved in the process of treatment—should be familiar with patients' living conditions, social environments, and disease progression; that is, healthcare workers must deliver services that recognize and cater to the preferences, needs, and values of patients (1). PCC is a high-value healthcare service that is crucial to improving the quality of care and building harmonious doctor-patient relationships (2, 3). However, PCC calls for substantial competence among healthcare workers as it is complex and can be characterized as integrated medicine that is multi-leveled and comprehensive, covering the entire life cycle (4, 5). Therefore, clarifying the driving mechanism for the provision of healthcare is necessary to effectively intervene in the behaviors of healthcare workers. Furthermore, it is important to gain thorough and systematic insights into the factors driving PCC from different aspects, such as outer contexts and intrinsic motivation.
In recent years, many scholars have tried to elucidate the concept of PCC and explore the factors influencing behaviors of healthcare professionals pertaining to the provision of PCC; for example, in 2000, Ma studied the development and improvement of the hospital service system based on insights from the patient-centered approach, proposing a basic framework and solutions for the establishment of a patient-centered hospital service system (6). In 2002, Wang and Liu (7) argued that “patient-centeredness” involves improving doctor-patient communication, which can facilitate doctors' understanding of their patients and help doctors and patients reach a consensus on medical decisions. In 2019, Liang (8) summarized Western studies on patient-centered medical services and administration at the theoretical level and outlined practice guidelines for the implementation of PCC in China. Gender, grade, empathy, and communication skills were found to have statistically significant effects on dental students' attitudes regarding patient-centered services, which could be improved via a focus on enhancing empathy, emphasizing positive attitudes toward learning communication skills, and conducting patient-centered learning seminars (9). Furthermore, Kanat et al. (10) found that the doctor-patient relationship and communication, doctors' characteristics, and patients' engagement were important determinants of PCC. Paiva et al. (11) investigated the factors facilitating and inhibiting healthcare workers' implementation of PCC; they contended that the creation of an atmosphere that is conducive to communication, engagement of patients in medical decisions, and enhancement of medical personnel's ability to communicate effectively might foster the provision of PCC by medical workers.
Studies have linked PCC with various positive patient outcomes, including empowerment and engagement (10, 12) favorable health outcomes, diminished socioeconomic, and racial disparities, shorter hospitalization periods and earlier discharge, and lower treatment costs (13, 14). However, the existing literature on PCC has the following drawbacks. First, while many studies have identified various external (contextual) and internal (personal) factors associated with PCC provision, comparatively fewer studies have considered both contextual and personal factors holistically and identified the pathways linking them. It is extremely important to better understand how these factors interact to facilitate (or undermine) healthcare workers' provisions of PCC. Second, among the studies focusing on the factors influencing PCC, few have focused on organizational culture, which is an important factor that facilitates service ability by valuing people, stimulating new thoughts, fostering team spirit, and adopting systems that are recognized by employees. Third, studies focusing on the driving mechanisms of healthcare workers' provision of PCC have not investigated the impact of their intrinsic motivation. Thus, several studies so far have revealed that self-efficacy and achievement motivation have joint effects on personal behaviors (15, 16). However, few have been conducted in the field of hospital administration, and the mechanisms underlying the synergy between self-efficacy and achievement motivation are yet to be fully uncovered; for example, it is unclear whether hospital culture has different effects on the self-efficacy of and provision of care by healthcare professionals based on their level of achievement motivation. Therefore, the pathways of effects between hospital culture and healthcare workers' implementation of PCC are worth investigating.
Motives—both physiological and social—have been identified as major internal driving forces of human behavior in diverse domains (17). Achievement motivation refers to the perceived motivation that drives individuals to undertake challenging and meaningful work tasks and/or activities and surpass others to attain satisfactory outcomes (18). Thus, achievement motivation is an important internal variable that is positively associated with quality and initiative at work (19, 20). With regard to individual consciousness, achievement motivation is embodied in two opposing psychological tendencies: the pursuit of success and avoidance of failure (21). Schone (22) contended that strong achievement motivation is a positive predictor of employees' job engagement, work performance, and organizational behaviors, among others. Wang (20) explored the correlation between doctors' achievement motivation and sense of responsibility and found that achievement motivation is positively associated with service initiative. Feng (19) found that achievement motivation is one of the factors driving community practitioners to deliver first-contact services. Song et al. (23) showed that doctors with high achievement motivation maintain a positive outlook toward work, are friendlier with patients, and can overcome emotional exhaustion. According to McClelland's (24) theory of needs (also known as the theory of motivation), healthcare workers with a high (vs. low) level of achievement motivation are more devoted to work and are more focused, proactive, and persistent in delivering PCC owing to positive feedback (25).
In light of the aforementioned findings, we advocated the importance of considering the effects of achievement motivation while assessing the influence of hospital culture on patient-centered practice among medical staff. In addition, we included self-efficacy as an essential factor in the proposed model as this—as another intrinsic variable—could reflect healthcare personnel's level of confidence in the provision of PCC (26). Self-efficacy is an individual's belief in their capacity to set and achieve certain goals, that is, confidence in one's abilities (10). It is important to note that self-efficacy affects people's mindsets, responsiveness to emotions, and choice of behaviors (27). From a behavioral science perspective, self-efficacy might be a predictive factor for the adoption of and changes in health-related behaviors (28). For example, Ham and Tak (29) suggested that low self-efficacy could lead to avoidance behaviors and ineffective communication, resulting in poor clinical outcomes. Additionally, Afsar and Masood (30) found that enhancements in self-efficacy can facilitate innovative work-related behaviors such as PCC. Furthermore, Zhang et al. (31) demonstrated that self-efficacy is positively associated with health protection behaviors among pharmacists during the coronavirus disease 2019 pandemic.
Self-efficacy can be influenced by several contextual factors associated with hospital culture. For example, Meurling et al. (32) suggested that teamwork (or collaboration) and communication can contribute to the enhancement of self-efficacy among healthcare workers. Zhao et al. (33) proposed that the provision of external support to healthcare workers can enhance their self-efficacy and reduce job burnout. Additionally, the engagement and behaviors of leaders can influence the vitality, caliber, performance, and cohesion of their team (34). Xue et al. (35) found that leaders who favor and encourage changes can set a positive example for their coworkers and employees, fostering unity, and initiative in the organization; these factors are conducive to the organization's future. They also suggested that work atmosphere is positively correlated with initiative among employees. Furthermore, Liang and Gu (36) found that innovative organizational culture has positive effects on creativity and motivation (to perform) among employees. Therefore, an efficient hospital culture serves several functions—including guidance, bonding, stimulation, constraint, regulation, and security—which can contribute to the enhancement of self-efficacy among healthcare workers.
“Hospital culture” refers to the sum of collective consciousness, values, ethics, and norms in medical practice held by hospital employees under certain socioeconomic conditions (37). Studies have shown that hospital cultures based on internal communication, cross-team collaboration, innovation, and charismatic leadership (38–43) can facilitate the implementation of PCC by enhancing patient-centered consciousness among healthcare workers. Thus, the following hypothesis was formulated.
Hypothesis 1 (H1): Hospital culture has a positive effect on healthcare workers' implementation of PCC. In sum, on the one hand, hospital culture has a direct positive effect on the provision of PCC by healthcare professionals; on the other hand, self-efficacy mediates the effect of hospital culture on healthcare workers' implementation of PCC. Therefore, the following hypotheses were formulated.
H2: Hospital culture positively affects self-efficacy among healthcare workers.
H3: Self-efficacy among healthcare workers has a positive effect on the delivery of PCC.
H4: Self-efficacy mediates the relationship between hospital culture and healthcare workers' implementation of PCC.
Furthermore, achievement motivation moderates the relationship between hospital culture and healthcare workers' self-efficacy for the provision of PCC. Gong and Xue (44) explored the mechanism underlying the effect of empowering leadership on creativity among employees; they found that achievement motivation moderated the relationship between empowering leadership and self-efficacy. In addition, Sommaruga et al. (45) suggested that patient-centered practice among medical personnel can be enhanced by emotional intelligence. In sum, a good hospital culture has a relatively weaker positive effect on self-efficacy among healthcare workers with low achievement motivation. On the contrary, a good hospital culture has a stronger positive effect on the self-efficacy of healthcare professionals with high achievement motivation. Therefore, the following hypotheses were formulated.
H5: Achievement motivation moderates the relationship between hospital culture and self-efficacy among healthcare workers.
H6: Achievement motivation moderates the relationship between self-efficacy among healthcare workers and their implementation of PCC.
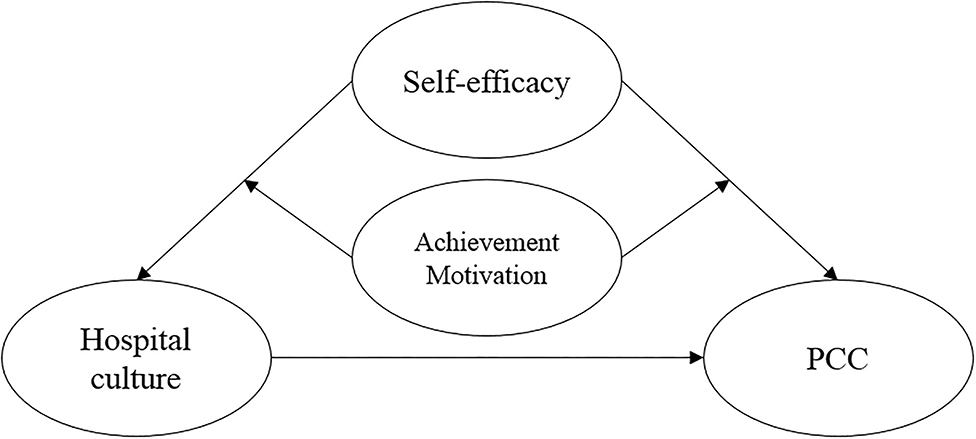
Thus, we surveyed healthcare workers from 27 public hospitals (of different levels) in Hangzhou to explore the pathways linking inner communication, cross-team collaboration, innovative organizational culture, charismatic leaders, self-efficacy, and achievement motivation to healthcare personnel's provision of PCC, considering intrinsic motivation and hospital culture. In light of theories of motivation, we proposed a theoretical model with hospital culture as the independent variable, healthcare professionals' implementation of PCC as the dependent variable, self-efficacy as the mediating variable, and achievement motivation as the moderating variable (Figure 1).
Materials and Methods
Sample Characteristics
Healthcare workers—including doctors, nurses, and medical technicians from different levels of public hospitals in Hangzhou city—voluntarily participated in this study. Hangzhou is a provincial capital located in coastal southeast China. It is economically well-developed and had a per capita GDP of 134,900 yuan in 2021. It is known for its quality of healthcare and high-ranked hospital administration, rendering it an apt setting for this study. The inclusion criteria were as follows: (1) providing informed consent; (2) being employed in the target hospital; and (3) having work experience of more than 6 months. The exclusion criteria were as follows: (1) being off-duty during the survey period owing to reasons like maternity leave, personal affairs, sick leave, learning, holiday, and/or business trips; and (2) questionnaires from interns or trainees from other organizations.
Stratified random sampling was used to select healthcare institutions based on three hospital levels; six tertiary and six secondary hospitals and 15 community health centers were randomly selected from among the medical organizations in Hangzhou. Convenience sampling was then used to select healthcare workers from each institution; 200 healthcare workers were selected from each tertiary hospital, 50 from each secondary hospital, and 20 from each community health center. Accordingly, 1,800 questionnaires were sent to these institutions through a face-to-face survey approach, of which 1,612 qualifying questionnaires were retrieved. The criteria for considering questionnaires invalid were: (1) incomplete responses; (2) same responses for more than 50% of the completed questions; and (3) obvious contradictions in responses across questions. If a questionnaire met even one of these criteria, it was deemed invalid.
Measures
General Information
The form for general information comprised items pertaining to gender, marital status, age, level of education, title, post, department, years of experience, type of employment, daily working hours, monthly income, hospital level, teaching status of the hospital, communication skills training, and familiarity with PCC.
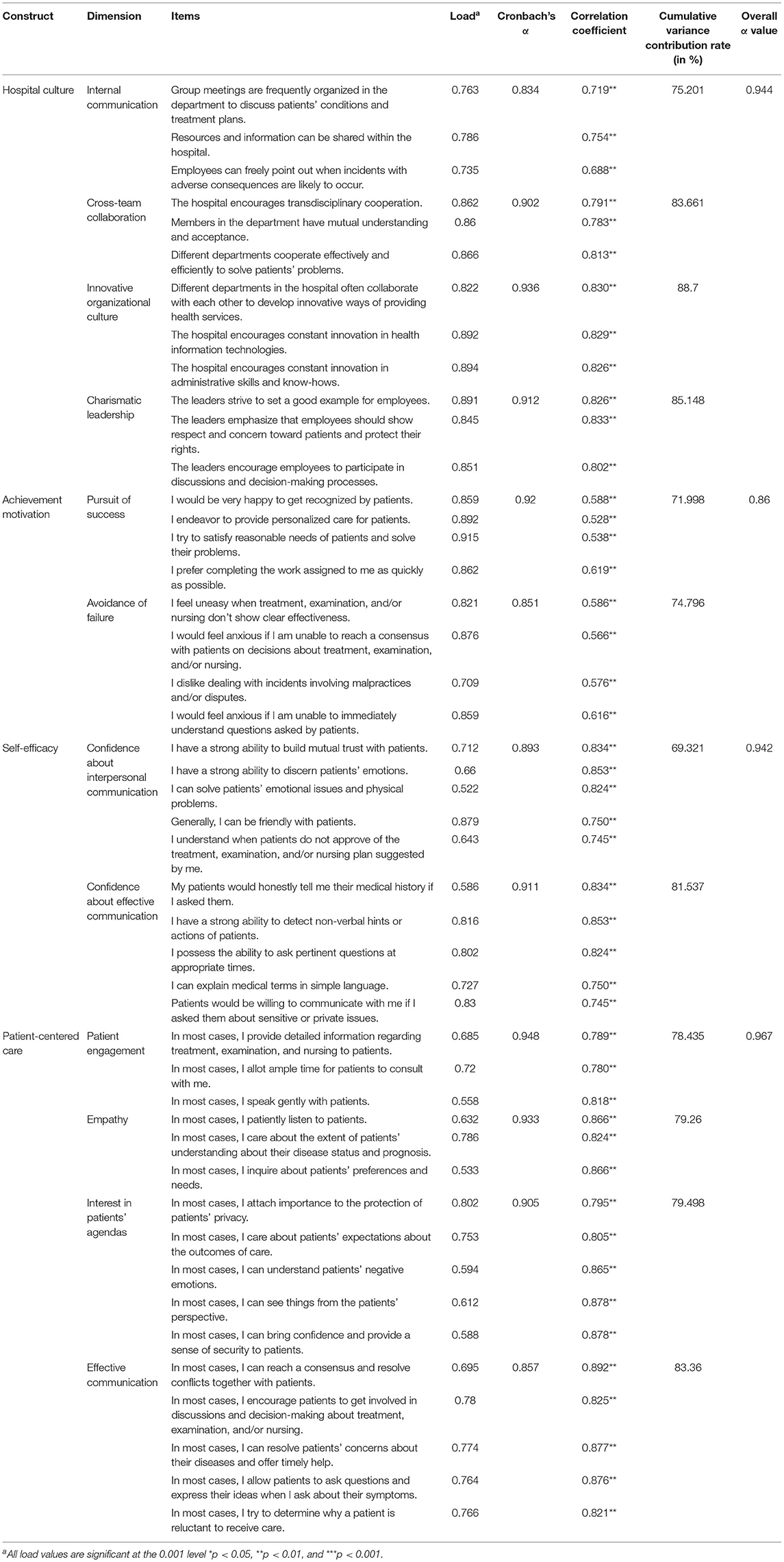
Provider-Patient Relationship Questionnaire
To evaluate the healthcare personnel's perceptions of their provision of PCC, we used the Provider-Patient Relationship Questionnaire (PPRQ), developed by Gremigni et al. (46). The PPRQ includes four dimensions: effective communication (four items), interest in the patient's agenda (four items), empathy (four items), and patient involvement in care (four items). Items are scored on a five-point Likert scale, ranging from one (never) to five (always); higher scores reflect better patient-centered services. The PPRQ has good reliability and validity (Table 1).
Hospital Culture
A self-developed hospital culture questionnaire (38–43) was used to evaluate hospital culture based on four dimensions: internal communication (three items), cross-team collaboration (three items), innovative organizational culture (three items), and charismatic leadership (three items). Items are rated on a five-point Likert scale, ranging from one (strongly disagree) to five (strongly agree); higher scores represent better hospital culture. The scale had good reliability and validity (Table 1).
General Self-Efficacy Scale
Self-efficacy among healthcare workers was evaluated using the General Self-Efficacy Scale (GSES), developed by Schwarzer and Jerusalem (47). The GSES has two components: confidence about interpersonal communication (five items) and confidence about effective communication (five items). Items are rated on a five-point Likert scale, ranging from one (strongly disagree) to five (strongly agree), and higher scores represent higher self-efficacy. The scale had good reliability and validity (Table 1).
Achievement Motivation Measurement Scale
Healthcare workers' achievement motivation was evaluated using the Achievement Motivation Measurement Scale, developed by Huang (21). This scale includes two sub-dimensions: pursuit of success (four items) and avoidance of failure (four items). Items are rated on a five-point Likert scale, ranging from one (“strongly disagree”) to five (“strongly agree”); items in the avoidance of failure subscale are reverse scored. Higher scores reflect higher achievement motivation. The scale had good reliability and validity (Table 1).
Quality Control
Prior to data collection, we conducted a pilot study. We gathered and analyzed the problems that were identified in the preliminary study. We then discussed the results of the preliminary study, revised the questionnaire, established a specific study plan, and finalized the questionnaire. Questionnaire distribution was performed by postgraduates with adequate experience in conducting personal surveys. The survey was conducted between July 1 and September 30, 2021. Furthermore, concentrated training sessions were conducted prior to the commencement of the official survey to ensure that the investigators had a clear understanding of the project, questionnaire, and key points during investigation; this process also ensured that they followed unified standards and methods. The survey was conducted via one-on-one interviews after obtaining informed consent from the participants. After the questionnaires were filled out, the investigators inspected them and checked with participants regarding the questionnaires that did not meet the study requirements. Subsequently, the questionnaires were coded and data were double-entered.
Statistical Analyses
Preliminary Analyses
Data were coded and entered in the database. The demographic data were evaluated and compared by descriptive analysis, one-way analysis of variance, and independent t-test. In addition, SPSS version 22 (IBM Corp., Armonk, NY, United States) was used to test the Pearson's correlations between hospital culture, self-efficacy, achievement motivation, and PCC. Statistical significance was set at p < 0.01.
Mediation and Moderation Analyses
Structural equation modeling was used to analyze the mediating effect of self-efficacy among medical staff and the moderating effect of achievement motivation. Hayes' Process Macro Model 4 was employed to conduct mediation analysis, and Model 58 was employed for moderated mediation analysis (48). The aforementioned program is suitable for a variety of mediation, moderation, and moderated mediation models. Hypothesis testing for the regression coefficients was conducted using the bias-corrected percentile bootstrap method with 5,000 replicates at the 95% confidence interval (CI). If it did not include 0, the difference in effect was considered statistically significant.
Ethical Considerations
The study was approved by the Institutional Review Board of Hangzhou Normal University. All participants provided informed consent, and the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Results
Demographic Characteristics
Of the 1,612 participants included in the study, 419 (54.3%) were male, 1,154 (71.6%) were married, and 182 (11.3%) were aged 46 or older. Additionally, 1,142 participants (70.8%) had a bachelor's degree, 602 (37.3%) had a junior title, 591 (36.5%) were doctors, and 501 (31.1%) were placed in the internal medicine unit. Moreover, 231 participants (14.3%) had work experience of 20 years or more, 1,199 (74.4%) held an officially budgeted post, and 1,175 (72.9%) worked for 8–10 h per day. Furthermore, 1,179 participants (73.1%) worked in tertiary hospitals and 1,259 (78.1%) in teaching hospitals; 581 participants (36.0%) had a monthly income of 5,001–7,000 yuan. Lastly, 958 participants (59.4%) had received training in patient-centered communication skills, 285 participants (17.7%) took 5–10 min on average to see one patient, and 132 participants (8.2%) were “very familiar” with PCC.
The healthcare workers' perceptions of their provision of PCC were evaluated based on their scores on the PPRQ (M = 66.70, standard deviation (SD) = 9.23). There were significant differences in participants' PPRQ scores based on age (F = 5.77, p < 0.01), title (F = 5.99, p < 0.01), post (F = 6.10, p < 0.01), and level of familiarity with PCC (F = 38.07, p < 0.01). Senior healthcare workers (M = 68.92, SD = 9.10) obtained higher scores than those with relatively junior titles (M = 67.18, SD = 8.88). Doctors (M = 67.98, SD = 8.55) obtained higher scores than nurses (M = 65.90, SD = 9.02). Furthermore, participants who were “very familiar” with PCC obtained the highest scores (M = 73.10, SD = 8.78), and those who were “very unfamiliar” with PCC obtained the lowest scores (M = 60.32, SD = 10.84) on the PPRQ. The PPRQ scores based on participants' demographic characteristics have been presented in Table 2.
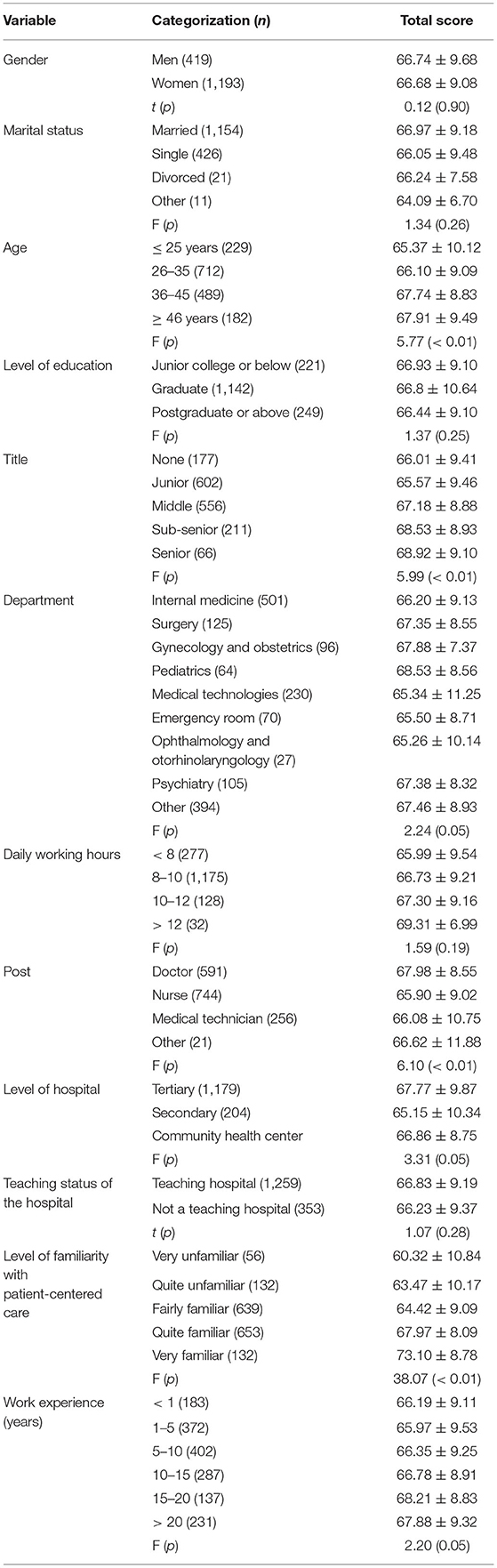
Table 2. Comparison of healthcare workers' mean scores on the provider-patient relationship questionnaire based on different demographic variables.
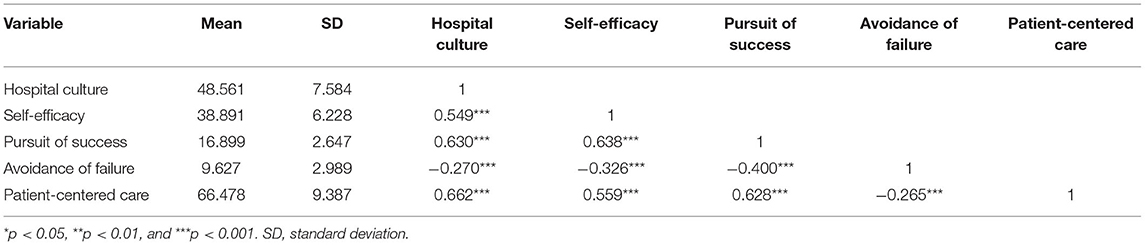
The means, SDs, and correlation coefficients of the variables under study have been presented in Table 3. Hospital culture was positively associated with self-efficacy (r = 0.549, p < 0.001) and healthcare workers' perceived provision of PCC (r = 0.662, p < 0.001). Similarly, there was a significant positive association between self-efficacy and healthcare workers' perceived provision of PCC (r = 0.559, p < 0.001). Additionally, significant positive correlations were observed between the variables (hospital culture, self-efficacy, pursuit of success, avoidance of failure, and PCC).
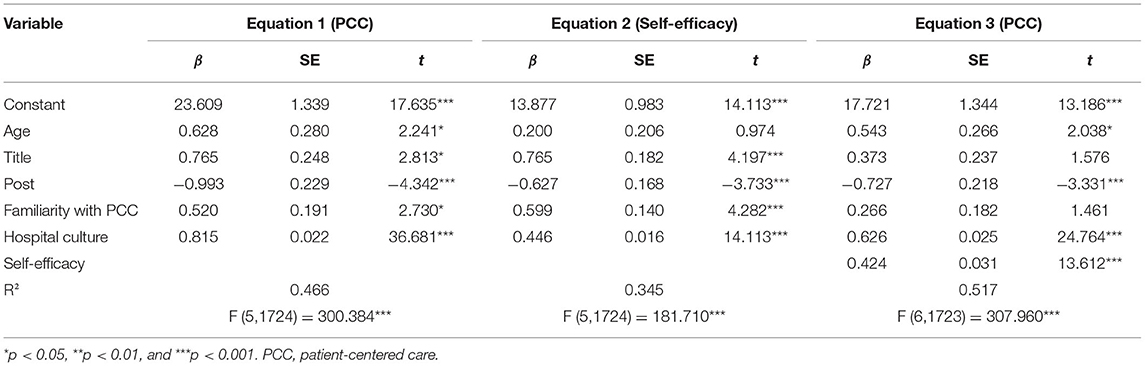
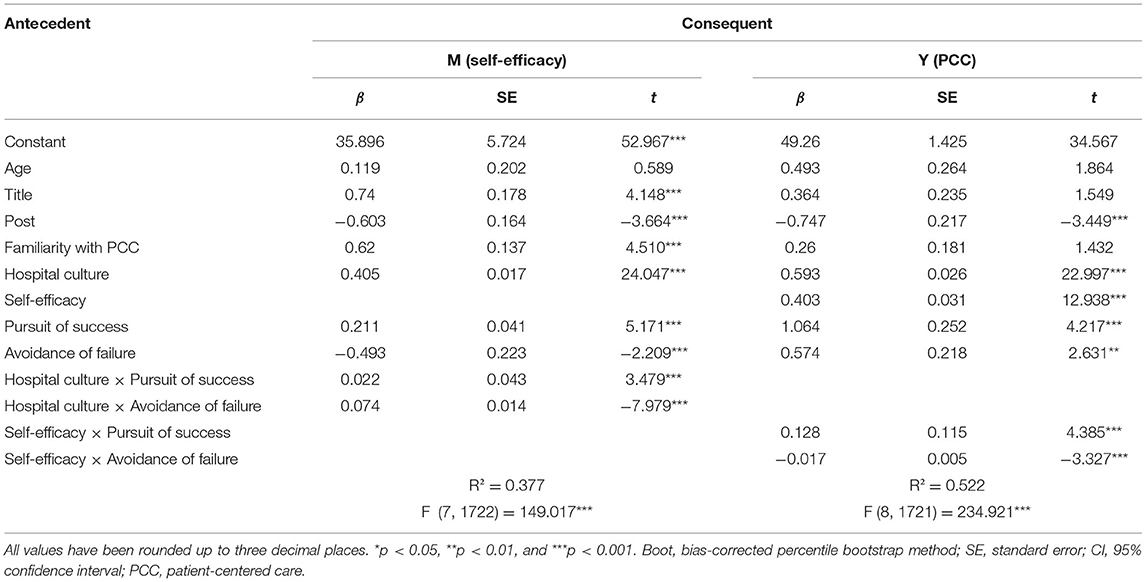
Analysis of the Mediating Effect of Self-Efficacy
First, a mediation model was constructed with hospital culture as the independent variable and the perceived provision of PCC as the dependent variable after controlling for age, title, post, and level of familiarity with PCC (Table 4). The results of Equation 1 showed that hospital culture had a significant positive effect on healthcare workers' perceived provision of PCC (β = 0.815, p < 0.001). Bootstrapping was performed using 5,000 bootstrap replicates (as parameter estimation). The 95% CI was 0.772–0.859 and did not include 0; thus, the results supported H1, suggesting that hospital culture had a positive effect on healthcare workers' perceived provision of PCC.
Second, self-efficacy was entered into the model as the mediating variable. The results for the mediating effects of self-efficacy have been depicted in Table 4 (Equations 2, 3). Hospital culture had a significant positive effect on self-efficacy (β = 0.446, p < 0.001) with the 95% CI within the 0.414–0.478 range; thus, the results supported H2, validating that hospital culture positively influenced self-efficacy among healthcare workers. As shown in Equation 3, self-efficacy had a significant positive effect on healthcare workers' perceived provision of PCC (β = 0.424, p < 0.001); the estimated 95% CI was within the 0.363–0.485 range, and did not include zero. Thus, the results supported H3, reflecting that self-efficacy among healthcare workers had a positive effect on the delivery of PCC. Self-efficacy had a partial mediating effect in the relationship between hospital culture and PCC implementation. The size of the mediating effect has been presented in Table 5. Additionally, 76.81% of the total effects of hospital culture on the perceived provision of PCC were direct effects and 23.19% were indirect effects, mediated by self-efficacy. These results supported H4, suggesting that self-efficacy mediated the relationship between hospital culture and healthcare workers' PCC implementation.
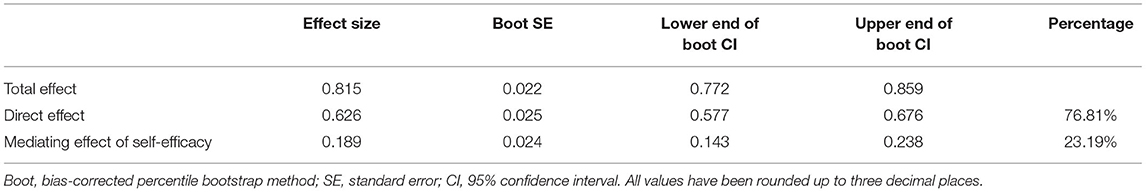
Table 5. Total, direct, and mediating effects of self-efficacy in the relationship between hospital culture and healthcare workers' perceived provision of patient-centered care.
Analysis of the Moderating Effect of Achievement Motivation
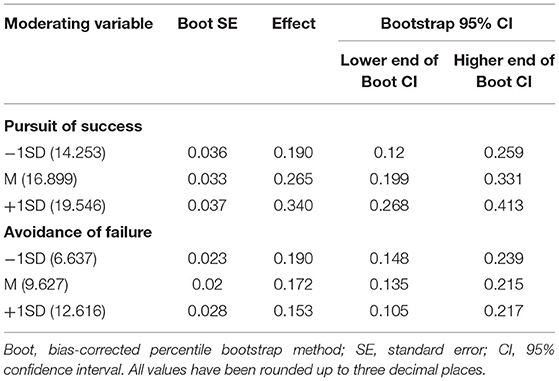
The moderating effect of healthcare workers' achievement motivation was examined using the mediation model. The two dimensions of achievement motivation were analyzed separately as the pursuit of success was positively correlated with the perceived provision of PCC, whereas the avoidance of failure was negatively correlated with the perceived provision of PCC. A moderated mediation model was constructed after decentering the pursuit of success, avoidance of failure, and hospital culture and including the interaction terms. The results of the moderated mediation model have been displayed in Table 6. The interactions between hospital culture and the pursuit of happiness and the avoidance of failure had significant effects on self-efficacy (β = 0.022, p < 0.001; β = −0.493, p < 0.001). Simple slope tests (Figure 2A) further revealed that hospital culture had a relatively weaker effect on healthcare workers' self-efficacy when the pursuit of success was low whereas hospital culture had a relatively stronger effect on healthcare workers' self-efficacy when the pursuit of success was high. Furthermore, Figure 2B shows that hospital culture had a relatively stronger effect on healthcare workers' self-efficacy when the avoidance of failure was low, whereas hospital culture had a relatively weaker effect on healthcare workers' self-efficacy when the avoidance of failure was high. Thus, these results supported H5, indicating that achievement motivation moderated the relationship between hospital culture and healthcare workers' self-efficacy. Additionally, the pursuit of success had a positive effect in the relationship between the aforementioned variables, whereas the avoidance of failure had a negative effect.
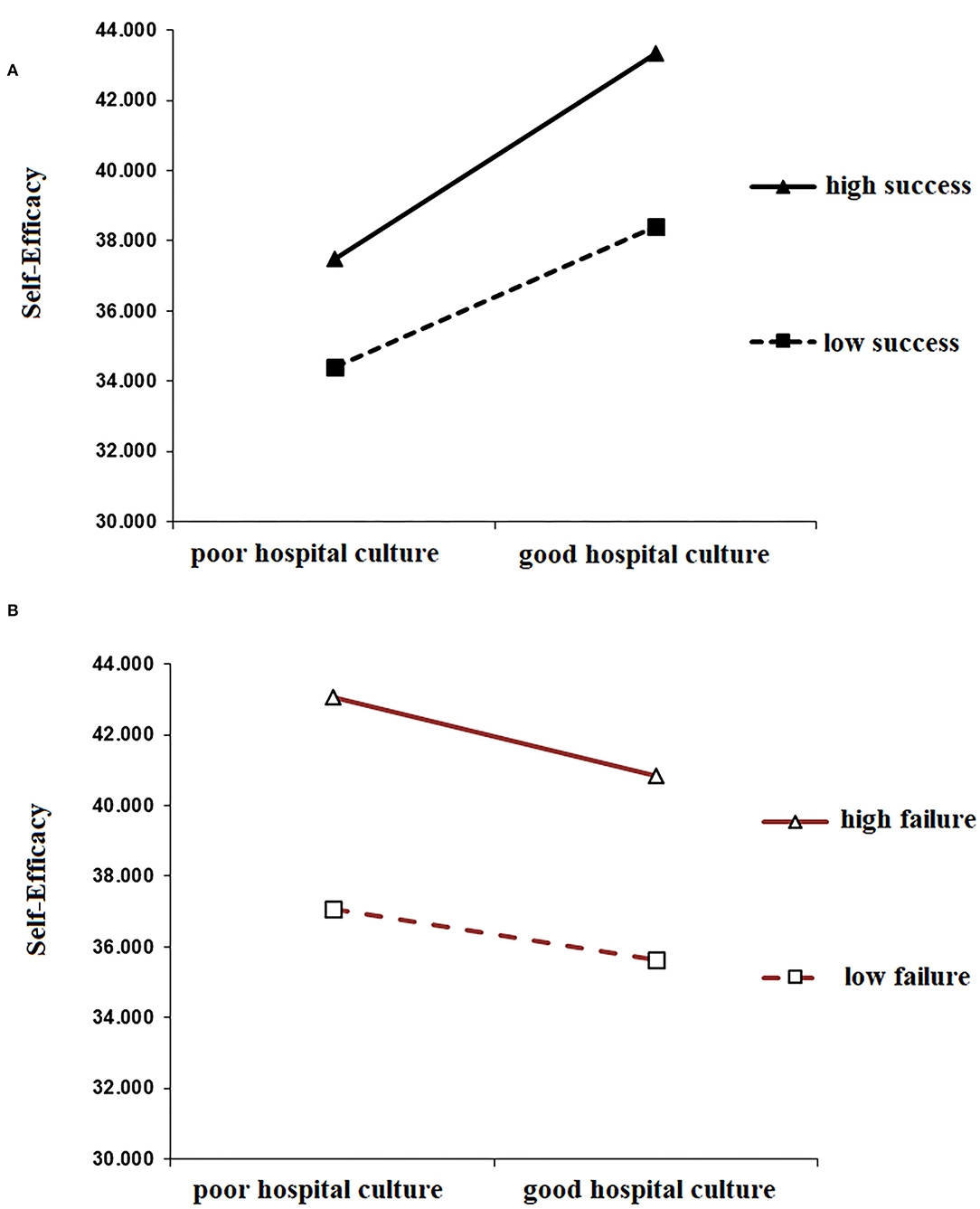
Figure 2. (A) Moderating effect of the pursuit of success in the relationship between hospital culture and healthcare workers' self-efficacy. (B) Moderating effect of the avoidance of failure in the relationship between hospital culture and healthcare workers' self-efficacy.
Moreover, Table 6 demonstrates that the interaction effects between self-efficacy and the pursuit of success and avoidance of failure had significant moderating effects on PCC (β = −0.128, p < 0.001; β = −0.017, p < 0.001). These results indicated that the mediating effect of self-efficacy in the relationship between hospital culture and the provision of PCC was moderated by achievement motivation (comprising the pursuit of success and avoidance of failure). To further evaluate the moderating effect of achievement motivation on the mediating effect of self-efficacy, we performed bootstrap testing and explored the indirect effect of the pursuit of success and avoidance of failure on three levels of self-efficacy. As shown in Table 7, the results demonstrate that self-efficacy had a stronger mediating effect on the perceived provision of PCC among healthcare workers with a high need for pursuing success (ρ = 0.340, 95% CI not including 0) as compared to healthcare workers with a low need for pursuing success (ρ = 0.190, bootstrap 95% CI not including 0). On the contrary, self-efficacy had the weakest mediating effect on the perceived provision of PCC among healthcare workers with a high need for avoidance of failure; that is, the indirect effect of self-efficacy was lowest when the avoidance of failure was 1SD above the mean (ρ = 0.153, 95% CI not including 0).
Discussion
Effects of Hospital Culture on PCC
The present study found that hospital culture played an important role in healthcare workers' care delivery. As a manifestation of healthcare personnel's collective values and norms, hospital culture can deeply influence their mindset and behaviors. Consistent with Zhang's study (13), innovative organizational culture was found to have a positive effect on healthcare workers' provision of PCC. This could be because an open atmosphere stimulates positivity and creativity among employees, creating a favorable environment for them to work on new projects and develop new skills, and especially to implement innovative patient-focused treatment plans. Additionally, the present findings are corroborated by those of Zhu's study (14) as charismatic leadership facilitated empathy for patients among healthcare workers; participants reported that they could think from the patients' perspective, and listen to and communicate effectively with them. Leaders effectively enhanced their employees' awareness of PCC and the importance of empathy by urging them to respect and care about patients and protect patients' rights.
Healthcare workers who had received training to develop their communication skills scored higher than those who had not received such training. This finding is consistent with Jeong and Park's study (49), suggesting that a healthy atmosphere involving communication is conducive to healthcare workers' efficiency in the provision of healthcare services as it boosts understanding and togetherness, fostering tolerance and unity. Additionally, in line with the conclusions drawn by Fralicx (50), cross-team collaboration was associated with effective communication among healthcare workers. Thus, hospitals can set up multidisciplinary teams and construct streamlined communication or feedback mechanisms to enhance cooperation among different departments and facilitate the implementation of PCC.
Mediating Effects of Self-Efficacy
While exploring the mechanisms for the adoption of PCC, it is beneficial to examine the mediating effects of self-efficacy in the relationship between hospital culture and healthcare personnel's provision of PCC. Consistent with Yang et al. (51), the current study revealed that hospital culture affected healthcare workers' perceived provision of PCC, which was mediated by their self-efficacy. Self-efficacy can have direct effects on an individual's choices, goals, mindset, and attribution style, among others. Good hospital culture can foster healthcare professionals' self-efficacy, further enabling them to implement PCC.
The positive influence of hospital culture on self-efficacy can be explained in two ways. First, a supportive environment within a healthy hospital culture could increase healthcare workers' self-efficacy (52). When leaders highlight and champion the use of PCC in addition to advances in medical technologies and services that empower cross-team collaboration, healthcare workers might experience high levels of meaningfulness and confidence in completing their work; this could accelerate their ability to deliver healthcare services. Second, communication is an important factor in patient-centered medicine and calls for healthcare personnel's transition from traditional attitudes to attitudes of respect and care for patients' preferences, needs, and values (53). Open-minded leaders, innovative culture, and multidisciplinary cooperation can boost medical workers' confidence in effective communication, and thus, increase their willingness to implement PCC.
Meanwhile, self-efficacy had a positive effect on PCC; this is consistent with Sommaruga et al.'s findings (45), suggesting that healthcare providers with high self-efficacy had good interpersonal relationships and professional skills. Welsh (54) suggested that the enhancement of self-efficacy among doctors was effective in improving their communication skills; for example, doctors with high self-efficacy—consistent with the requirements of PCC—provided more disease-related information and medical knowledge to patients; encouraged them to communicate; and were responsive to their questions, suggestions, needs, and worries.
Moderating Effects of Achievement Motivation
According to McClelland's (45) achievement need theory, achievement motivation among social members stems from specific social and cultural environments. In this study, we constructed a moderated mediation model based on achievement theories. Achievement motivation exerted significant moderating effects in the relationship between hospital culture and self-efficacy. In the same culture, healthcare workers with high achievement motivation and self-efficacy were highly willing to communicate with patients. This could be because they cared about the patients' feelings and were mindful about responding to them and meeting patients' preferences and needs. This is in line with Wang's study (20), suggesting that healthcare workers' self-efficacy, and hence, achievement motivation, are reinforced when they overcome problems and difficulties in services. On the contrary, when issues keep sustaining, achievement motivation is triggered among healthcare workers with high self-efficacy owing to their confidence, whereas healthcare workers with low self-efficacy might adopt negative attitudes concerning the provision of PCC to avoid failure.
In line with Khongsamai et al.'s findings (55), in the current study, an innovative organizational culture contributed to an increase in effective communication. This could be because an open and innovative work environment facilitates initiatives among healthcare workers, improves their consciousness about communication, fosters innovation in communication styles and skills, and thus, promotes doctor-patient communication. On the contrary, achievement motivation moderated the relationship between self-efficacy and patient-centered practice among healthcare workers. Similar to Yim and Lee's findings (56), we found that healthcare workers who pursued success tended to have strong social responsibility, introspected about their actions based on patients' feedback, showed progress in ethical values and skills, and encouraged patients to participate in discussions and express their feelings.
The avoidance of failure was found to negatively moderate the relationship between self-efficacy and the provision of PCC; this has repeatedly been demonstrated in the fields of psychology and education (57, 58). In the current study, this could be because medical personnel with a strong need to avoid failure might have anticipated job burnout owing to the patient-centered services that might require several emotional resources in addition to concentration; they might also have been worried about the status of rewards and outcomes of the long-term input. However, the negative effect of avoidance of failure was not stronger than the positive effect of pursuit of success, implying that the healthcare workers' need to pursue success primarily influenced their achievement motivation.
Implications and Limitations
We believe that the present results have theoretical and practical significance. To begin with, the findings have strong implications for the development of strategies for stimulating healthcare workers' provision of PCC, which might be effective in transforming hospital administration methods and enhancing the efficiency of healthcare services. For example, to strengthen patient services, hospitals should establish an innovative culture, constantly work on creativity, encourage healthcare workers to innovate, and stimulate healthcare workers' internal achievement motivation by challenging them. Second, hospitals should establish a charismatic leadership culture. Hospital leaders should set an example and fully mobilize healthcare workers' consciousness and enthusiasm to serve patients. Moreover, hospital leaders should pay attention to their own quality improvement, respect healthcare workers, and be sensitive to their needs. Third, hospitals should establish a multidisciplinary diagnosis and treatment team to foster a culture of cooperation. By facilitating information exchange and providing a sharing platform for each department, a good communication and feedback mechanism is formed within the hospital, promoting internal cooperation. A good internal communication atmosphere is helpful for healthcare workers to understand each other, cultivate team spirit, and improve patient service efficiency. Our study found that the external hospital culture drives healthcare workers' attitudes and behaviors. It is not combined with the viewpoint of motivation theory, which adds further value to the literature on motivation theories.
The study also has some limitations. First, the recruited healthcare workers were from hospitals in Hangzhou; this could limit the representativeness of the sample and generalizability of our findings. Thus, further research should be conducted in other regions of China. Second, this study adopted a cross-sectional design; consequently, we could not capture the causal effect of changes over time. Therefore, future studies must adopt longitudinal, experimental, or cross-sequential designs and employ hierarchical linear models; studies must also test for the confounding and mediating effects of different variables. Third, this study explored healthcare workers' perceptions of their provision of PCC; future studies must focus on the perspectives of both healthcare providers and patients. Fourth, all the variables were assessed through self-report, and although surveys were answered anonymously, social desirability bias may still have influenced the responses to some extent.
Conclusions
The present study indicated that hospital culture can affect healthcare workers' implementation of PCC. Accordingly, hospitals could organize activities for healthcare workers to discuss hospital culture; this would strengthen their understanding of the importance of hospital culture. Additionally, hospital culture can boost the provision of PCC via the enhancement of self-efficacy and achievement motivation among healthcare workers. Therefore, hospital administrators should pay attention to the psychological status of their staff and develop their confidence in interpersonal networking and effective communication to help them build their self-efficacy for PCC and motivation for success.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The study was approved by the Institutional Review Board of Hangzhou Normal University. All study participants provided informed consent, and the study was performed in accordance with the Ethical Standards as laid down in the 1964 Declaration of Helsinki and its later amendments. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
XH conceptualized the study, drafted the methodology, and operated the software. YG performed the statistical analysis and prepared the first draft of the manuscript. HC helped with visualization and investigation. HZ operated the software and validated the findings. XZ helped in writing, reviewing, and editing the manuscript. All authors approved the submitted version of the manuscript.
Funding
This study was supported by the National Natural Science Foundation of China Project (Grant No. 72004051) and the Soft Science Research Program of Zhejiang Provincial Science and Technology Plan (Grant No. 2021C35012).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer XW declared a shared affiliation with all authors at the time of review.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to express our deepest gratitude to the Health Commission of Zhejiang Province for their support in conducting the research. We would like to thank the participants for their valuable time and effort in completing the questionnaire. We are also grateful to Jixiang Lai who helped us improve the manuscript.
References
1. Sowerby P. Balint reassessed: the doctor, his patient, and the illness: a reappraisal. J R Coll Gen Pract. (1977) 27:583–9.
2. Benson T. Principles of Health Interoperability HL7 and SNOMED. London: Springer (2012). p. 802–3. doi: 10.1007/978-1-4471-2801-4
3. Berghout M, van Exel J, Leensvaart L, Cramm JM. Health care professionals' views on patient-centered care in hospitals. BMC Health Serv Res. (2015) 15:e385. doi: 10.1186/s12913-015-1049-z
4. Jeske L, Kolmer V, Muth M, Cerns S, Moldenhaur S, Hook ML. Partnering with patients and families in designing visual cues to prevent falls in hospitalized elders. J Nurs Care Qual. (2006) 21:236–41. doi: 10.1097/00001786-200607000-00008
5. Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc Sci Med. (2000) 51:1087–110. doi: 10.1016/s0277-9536(00)00098-8
6. Ma XS. Construction of patient-centered care system in hospital. Med Soc. (2000) 1:57–9. Available online at: https:// /kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&dbname=CJFD2000&filename=YXSH200001024&uniplatform=NZKPT&v=yOVmzoHFGx-MnvFrCa5mnsbwHzTso0Kwh6P6acyEsKZPVAjNIspfgLvZ-Km88Suf
7. Wang XW, Liu LH. Development and conception of medical care model of patient centered medicine. Med Philos. (2002) 3:24–7. Available online at: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&dbname=CJFD2002&filename=YXZX200203007&uniplatform=NZKPT&v=1hiib4dgXEG66FNU2IKxsJvSBetoIWIqljjxtzkO3Fg1Jtr-jHJqVkigB1pDqZEy/33.nsdetail.aspx?dbcode=CJFD&dbname=CJFDLAST2019&filename=YYGL201911021&uniplatform=NZKPT&v= qPq4aSA9xIVd28eNhFH6GN6plCtxR43D1JYlVh_FmYDlqO5hNpHugGUMorm7cYSm
9. Lee M, Ihm J. Empathy and attitude toward communication skill learning as a predictor of patient-centered attitude: a cross-sectional study of dental students in Korea. BMC Med Educ. (2021) 21:e225. doi: 10.1186/s12909-021-02674-z
10. Kanat M, Schaefer J, Kivelitz L, Dirmaier J, Voigt-Radloff S, Heimbach B, et al. Patient-centeredness in the multimorbid elderly: a focus group study. BMC Geriatr. (2021) 21:e567. doi: 10.1186/s12877-021-02448-8
11. Paiva D, Abreu L, Azevedo A, Silva S. Patient-centered communication in type 2 diabetes: the facilitating and constraining factors in clinical encounters. Health Serv Res. (2019) 54:623–35. doi: 10.1111/1475-6773.13126
12. Yan YH, Yang CW, Fang SC. Patient-centered e-health supports value cocreation and quality of medical care in Taiwan. Health Info Libr J. (2022) 39:68–78. doi: 10.1111/hir.12372
13. Epstein RM, Fiscella K, Lesser CS, Stange KC. Why the nation needs a policy push on patient-centered health care. Health Aff. (2010) 29:1489–95. doi: 10.1377/hlthaff.2009.0888
14. Tomaselli G, Buttigieg SC, Rosano A, Cassar M, Grima G. Person-centered care from a relational ethics perspective for the delivery of high quality and safe healthcare: a scoping review. Front Public Health. (2020) 8:e44. doi: 10.3389/fpubh.2020.00044
15. Zhang R. The Influence of Patient-Centered Hospital Culture on the Professionalism of Doctors in Public Hospitals. Dissertation, Huazhong University of Science and Technology,Wuhan (2017).
16. Zhu Y. Practice of empathy in staff management of public hospitals. China Health Ind. (2018) 339:199–200. doi: 10.16659/j.cnki.1672-5654.2018.04.193
17. Ryan RM. Motivation and the organization of human behavior: three reasons for the reemergence of a field. In: Ryan RM, editor. The Oxford Handbook of Human Motivation. Oxford: Oxford University Press (2012). p. 3–10. doi: 10.1093/oxfordhb/9780195399820.013.0001
19. Feng W. Study on the formative mechanism and incentives of the community doctor first contact service motivation (dissertation). Hangzhou Normal University, Hangzhou (2017).
20. Wang H. Research on the relationship of doctors' achievement motivation and sense of responsibility in the city of Qingdao (dissertation). Southwest University, Chongqing (2009).
21. Huang YZ. Study on professional commitment and its relationship with achievement motivation for male undergraduates toward nursing in Xuzhou (dissertation). Xuzhou Normal University, Xuzhou (2011).
22. Schoen JL. Effects of implicit achievement motivation, expected evaluations, and domain knowledge on creative performance. J Organ Behav. (2015) 36:319–38. doi: 10.1002/job.1982
23. Song H, Xu YX, Song J. Study on the relationship between achievement motivation and job burnout of standardized training residents. China Contin Educ. (2017) 9:1–3. doi: 10.3969/j.issn.1674-9308.2017.12.001
24. McClelland DC, Koestner R. The achievement motive. In: Smith CP, editor. Motivation and Personality: Handbook of Thematic Content Analysis. Cambridge: Cambridge University Press (1992). p. 143–52. doi: 10.1017/CBO9780511527937.010
25. Guo B, Qiang B, Zhou J, Yang X, Qiu X, Qiao Z, et al. The relationship between achievement motivation and job performance among Chinese physicians: a conditional process analysis. BioMed Res Int. (2021) 2021:6646980. doi: 10.1155/2021/6646980
26. Guo BY, Jiang FY. Self-efficacy Theory and its Application. Shanghai: Shanghai Education Press (2008). p. 263–7.
27. Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Hoboken NJ: Prentice Hall (1986). p. 10–1.
28. Wang CL. Conceptual model of information framing effect in different stages of health behavior change. Libr Inf Serv. (2019) 63:23–31. doi: 10.13266/j.issn.0252-3116.2019.05.003
29. Ham HJ, Tak SH. Factors influencing transcultural self-efficacy among nurses with foreign patient care experience. J Transcult Nurs. (2022) 33:87–95. doi: 10.1177/10436596211016514
30. Afsar B, Masood M. Transformational leadership, creative self-efficacy, trust in supervisor, uncertainty avoidance, and innovative work behavior of nurses. J Appl Behav Sci. (2018) 54:36–61. doi: 10.1177/0021886317711891
31. Zhang N, Yang H, Hong D, Huang X, Wang L. Risk perception, self-efficacy, lay theories of health, and engagement in health-protective behaviors among hospital pharmacists during the COVID-19 pandemic. Int J Behav Med. (2021) 23:1–6. doi: 10.1007/s12529-021-10004-2
32. Meurling L, Hedman L, Sandahl C, Felländer-Tsai L, Wallin CJ. Systematic simulation-based team training in a Swedish intensive care unit: a diverse response among critical care professions. BMJ Qual Saf. (2013) 22:485–94. doi: 10.1136/bmjqs-2012-000994
33. Zhao YG, Li XX, Cui Y, Qiu YQ. Analysis of the impact of social support on job burnout among doctors and nurses: based on mediation effect of self-efficacy. Chin Hosp Manag. (2019) 39:48–50.
34. Liu YA. Research on the relationship between authentic leadership and team innovation from the perspective of positive cultural atmosphere. Leadersh Sci. (2018) 11:24–6. doi: 10.19572/j.cnki.ldkx.2018.11.006
35. Xue X, Xue W, Yao C. Study on relationship between transformational leadership and individual initiative—achievement motivation as mediating variable. J Zhejiang Sci Tech Univ. (2015) 34:385–9. Available online at: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&dbname=CJFDLAST2015&filename=ZJSG201510004&uniplatform=NZKPT&v=2oQqchrh0gNI5EYGLm1sekqeiQoPFhsKuryUPcvQaV6UyTiyymRxSHgnHTz8y0hZ
36. Liang BQ, Gu QX. Influence of innovative cultural awareness on the intrinsic motivation and creativity from the performance-oriented perspective. Shanghai Manag Sci. (2016) 38:89–96. doi: 10.3969/j.issn.1005-9679.2016.03.018
38. Burton D, Blundell N, Jones M, Fraser A. Elwyn G. Shared decision-making in cardiology: do patients want it and do doctors provide it? Patient Educ Couns. (2010) 80:173–9. doi: 10.1016/j.pec.2009.10.013
39. Peek ME, Wilson SC, Gorawara-Bhat R, Odoms-Young A, Quinn MT, Chin MH. Barriers and facilitators to shared decision-making among African-Americans with diabetes. J Gen Intern Med. (2009) 24:1135–9. doi: 10.1007/s11606-009-1047-0
40. Hower KI, Vennedey V, Hillen HA, Kuntz L, Stock S, Pfaff H, et al. Implementation of patient-centered care: which organizational determinants matter from decision maker's perspective? Results from a qualitative interview study across various health and social care organizations. BMJ Open. (2019) 9:e027591. doi: 10.1136/bmjopen-2018-027591
41. Jakimowicz S, Perry L, Lewis J. An integrative review of supports, facilitators and barriers to patient-centered nursing in the intensive care unit. J Clin Nurs. (2017) 4:25–6. doi: 10.1111/jocn.13957
42. Bokhour BG, Fix GM, Mueller NM, Barker AM, Lavela SL, Hill JN, et al. How can healthcare organizations implement patient-centered care? Examining a large-scale cultural transformation. BMC Health Serv Res. (2018) 18:e168. doi: 10.1186/s12913-018-2949-5
43. Alharbi TSJ, Ekman I, Olsson LE, Dudas K, Carlström E. Organizational culture and the Implementation of person centered care: results from a change process in Swedish hospital care. Health Policy. (2012) 108:294–301. doi: 10.1016/j.healthpol.2012.09.003
44. Gong W, Xue J. The impact of empowering leadership on employee creativity: roles of personal learning and achievement motivation. J Technol Econ. (2020) 39:21–9. Available online at: https:/ /kns.cnki.net/kcms/detail/detail. aspx?dbcode=CJFD&dbname=CJFDLAST2020&filename=JSJI202002004&uniplatform=NZKPT&
45. Sommaruga M, Casu G, Giaquinto F, Gremigni P. Self-perceived provision of patient centered care by healthcare professionals: the role of emotional intelligence and general self-efficacy. Patient Educ Couns. (2017) 100:974–80. doi: 10.1016/j.pec.2016
46. Gremigni P, Casu G, Sommaruga M. Dealing with patients in healthcare: a self-assessment tool. Patient Educ Couns patient ed. (2016) 99:1046–53. doi: 10.1016/j.pec.2016.01.015
47. Schwarzer R, Jerusalem M. (1995). Generalized self-efficacy scale. In: Weinman J, Wright S, Johnston M, editors. Measures in Health Psychology: A User's Portfolio. Causal and Control Beliefs. Windsor: NFER-NELSON (1995). p. 35–7.
48. Hayes AF. Introduction to mediation, moderation, and conditional process analysis. J Educ Meas. (2013) 51:335–7. doi: 10.1111/jedm.12050
49. Jeong H, Park M, A. predictive model on patient-centered care of hospital nurses in Korea. J Korean Acad Nurs. (2019) 49:191–202. doi: 10.4040/jkan.2019.49.2.191
50. Fralicx R. Strange bed(side) fellows physician-finance collaboration. Healthc Financ Manage. (2012) 66:90–4, 96.
51. Yang MJ, Ge M, Yang XQ. Study on the correlation between self-leadership and self-efficacy of nursing students. Nurs Res. (2018) 32:1753–7. Available online at: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&dbname=CJFDLAST2018&filename=SXHZ201811025&uniplatform=NZKPT&v=goEPf2dkHs-Fkbw0wxAVQ1my7XSLQuZ8HKGH2TK51JB6v9XONB111wDT1tY5HeAJ
52. Rahmer BM. Integrative exploration of the primary care interaction: tensions and ideals in patient-centered care (dissertation). University of Delaware, Ann Arbor (MI) (2014).
53. Liu JH. Building a new doctor-patient relationship empowers the construction of a healthy China. Peoples Tribune. (2021) 724:86–8. doi: 10.3969/j.issn.1004-3381.2021.33.020
54. Welsh JA, Nelson JM, Walsh S, Sealer H, Palmer W, Vos MB. Brief training in patient-centered counseling for healthy weight management increases counseling self-efficacy and goal setting among pediatric primary care providers: results of a pilot program. Clin Pediatr. (2015) 54:425–9. doi: 10.1177/0009922814553432
55. Khongsamai T, Intarakamhang U. Causal model of cultural competence and behavior among Thai nurses in international hospitals. J Behav Aci. (2020) 15:1–5. Available online at: https://www.researchgate.net/publication/346410346
56. Yim KH, Lee I. The effect of achievement motivation on learning agility of nursing students: The mediating effect of self-leadership. The effect of achievement motivation on learning agility of nursing students: the mediating effect of self-leadership. J Korean Acad Soc Nurs Educ. (2021) 27:80–90. doi: 10.5977/jkasne.2021.27.1.80
57. Capa RL, Audiffren M, Ragot S. The interactive effect of achievement motivation and task difficulty on mental effort. Int J Psychophysiol. (2008) 70:144–50. doi: 10.1016/j.ijpsycho.2008.06.007
Keywords: hospital culture, healthcare worker, patient-centeredness, self-efficacy, achievement motivation
Citation: Huang X, Gao Y, Chen H, Zhang H and Zhang X (2022) Hospital Culture and Healthcare Workers' Provision of Patient-Centered Care: A Moderated Mediation Analysis. Front. Public Health 10:919608. doi: 10.3389/fpubh.2022.919608
Received: 13 April 2022; Accepted: 13 May 2022;
Published: 06 June 2022.
Edited by:
Carmen María Galvez-Sánchez, University of Jaén, SpainReviewed by:
Xiaohe Wang, Hangzhou Normal University, ChinaCatalina Sau Man Ng, The Education University of Hong Kong, Hong Kong SAR, China
Roslina Othman, International Islamic University Malaysia, Malaysia
Copyright © 2022 Huang, Gao, Chen, Zhang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoting Zhang, enh0YmluZ0Boem51LmVkdS5jbg==
†These authors share first authorship
 Xianhong Huang
Xianhong Huang Yuan Gao
Yuan Gao Hanlin Chen1
Hanlin Chen1 Xiaoting Zhang
Xiaoting Zhang