- 1School of Nursing and Midwifery, Institutes of Health Sciences, Wollega University, Nekemte, Ethiopia
- 2Department of Public Health, Institutes of Health Sciences, Wollega University, Nekemte, Ethiopia
- 3Deakin Health Economics, School of Health and Social Development, Institute for Health Transformation, Deakin University, Geelong, VIC, Australia
Background: Women's HIV-positive disclosure plays a pivotal role to achieve the goal of preventing mother-to-child transmission (PMTCT) among pregnant women in particular. Although several primary studies were conducted in the different countries of East Africa, no study concluded the prevalence of women's HIV status disclosure and associated factors in East Africa. Therefore, the current study aimed to assess the pooled prevalence of disclosure status and associated factors among women in East Africa.
Objectives: To assess the pooled prevalence of HIV sero-status disclosure and associated factors among women in East Africa.
Methods: HINARI, PubMed, and Cochrane Library databases were searched. The data were extracted using a Microsoft Excel spreadsheet and STATA v 14.1 was used for the analysis. The Funnel plots and Egger's statistical test was used to check publication bias. Heterogeneity was assessed by conducting sensitivity and subgroup analyses.
Result: The pooled prevalence of sero-status disclosure among women in East Africa was 73.77% (95%CI 67.76, 79.77). Knowing partner's sero-status (OR = 10.04(95%CI 3.36, 31.84), married (OR = 2.46 (95%CI 1.23, 4.89), smooth relationship (OR = 3.30 (95%CI 1.39, 7.84), and discussion on HIV before the test (OR = 6.96 (95%CI 3.21, 15.05) were identified determinants of HIV sero-status disclosure.
Conclusion: The current systematic and meta-analysis revealed that nearly one-fourth of women had not disclosed HIV sero-status to at least one individual. Knowing the partner's HIV sero-status, being married, having a smooth relationship, and discussing on HIV before the test were determinants of disclosure status. Therefore, disclosure of HIV-positive sero-status among women living with HIV needs to be strengthened.
Introduction
Human Immunodeficiency virus (HIV) continues to be one of the health and development challenges globally. By 2020, about 37.7 million people were living with HIV/AIDS (1). Eastern and Southern Africa is the epicenter of the HIV burden; they contributed nearly 20.7 million HIV/AIDS clients to a global total (2).
In addition to lifelong therapy, the role of sero-status disclosure to reduce onward HIV transmission is witnessed in literature particularly in preventing mother-to-child transmission (PMTCT) (3). Disclosure is the process of enlightening HIV-positive status to a sexual partner, family members, and in one's social networks over time (4). It is a personal and intimate process that engages the soul, the mind, and the body that shapes the self-image, self-efficacy, self-perception, and confidence of HIV-infected individuals (5).
Disclosing HIV seropositive status has an imminent role in both prevention and management (6); smoothing social support, increasing adherence, expanding awareness, and reducing risky behaviors (7).
Studies exposed that HIV-positive disclosure among pregnant women is attributed to different factors including residence (8), educational level (9), low- income (10), Fear of stigma (11), and disturbed relationships (12–15). In other literature, disclosure status is explained by adherence to antiretroviral therapy (ART), confidentiality problems, and the provider's expressed anxiety (16–18). Additionally, social context can be a key dimension of disclosure as an impression for financial, social support, and emotional support, and help with medical care or counseling; disclosure is higher when hoping to receive help and lower when expecting blame and discrimination (19, 20).
Therefore, this systematic review and meta-analysis aimed to determine the pooled prevalence and associated factors of disclosure status among HIV-positive Women in East Africa. The finding will enable scholars, clinicians, and policymakers to appraise the existing approach and create a new HIV prevention and control strategy for PMTCT.
Methods
Search strategies
PubMed, HINARI, and Cochrane Library databases were searched. The literature search was performed from March 1 to March 30, 2021. Searches were conducted using terms such as “HIV sero-status disclosure,” “disclosure status,” “magnitude,” “prevalence,” “associated factors,” “determinants” “Pregnant women,” “Lactating women,” Women,” HIV positive,” and “lists of all East African countries.” Boolean operators like “AND” and “OR” were used. PRISMA checklist and flow diagram were used for reporting the procedure (Figure 1).
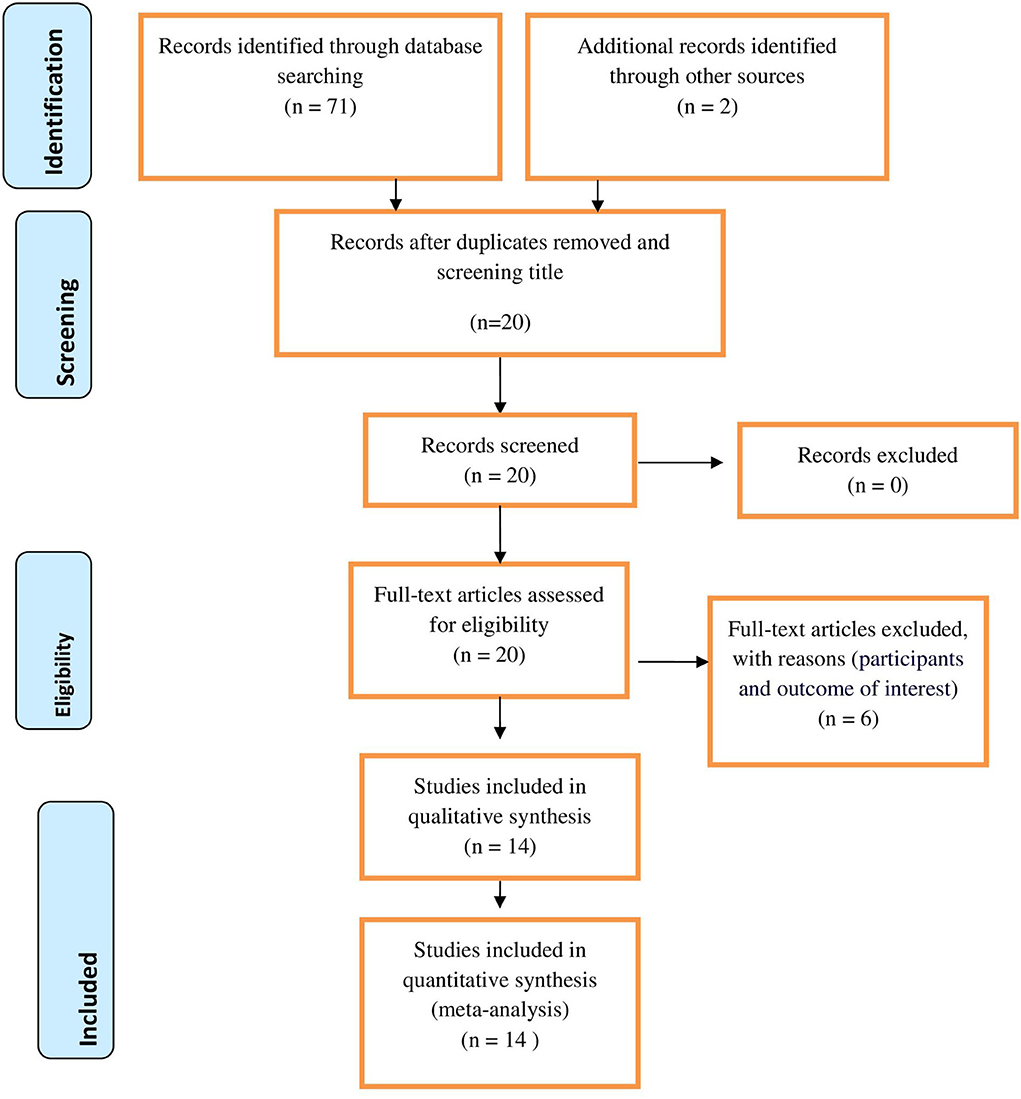
Figure 1. PRISMA flow diagram of included studies for the systematic review and meta-analysis of disclosure status and associated factors among Women in East Africa, 2021.
Selection and eligibility criteria
Studies that were conducted on the disclosure status among women living with HIV in East Africa were included. Each article was independently reviewed by two investigators (GM & DM). The Study populations were all WLHIV in East Africa. Studies conducted in East Africa were included in the review. All observational studies reporting disclosure status among WLHIV in East Africa were included. Articles reported in the English language were included. Articles that were not fully accessible, after at least two email contact attempts with the primary authors, were excluded.
Outcome measurement
Disclosure status among WLHIV was the primary outcome of this study. It was categorized as “yes” if the HIV-positive women disclosed their status to at least one individual including sexual partner, family, husband, and relatives, and “no” if not disclosed to a least one of them. It is measured as the total number of disclosed cases over a total number of all women multiplied by 100. The second outcome was factors associated with disclosure status among WLHIV. For the second outcome, the log odds ratio was determined to see the association between disclosure status and associated factors. Factors included in this review include knowing the partners sero-status (know vs. not know), educational status (no education/primary vs. secondary and above), the relationship before the test (smooth vs. disagreement), marital status (married vs. unmarried), residence (rural vs. urban), and discussion on HIV before the test (absence vs. presence).
Data extraction and quality assessment
Joanna Briggs Institute Critical Appraisal Checklist for Analytical Cross-Sectional Studies was used to assess the quality of included studies (21). The data were extracted by two authors (GM and DM) using data extraction checklists on Microsoft excel. Reference management software (Endnote version X7.2) was used to combine search results from databases and to remove duplications. Studies were screened using abstracts and titles. Then, the eligibility of the studies was evaluated using predetermined inclusion and exclusion criteria. For the outcome, disclosure status, and associated factors, data were extracted in the format of two-by-two tables. The log odds ratio was calculated based on the findings of the primary studies. The data extraction checklist contains the author's name, country, study design, year of publication, sample size, response rate, and the number of participants with the outcome. Any disagreement between two independent reviewers was resolved by involving a third reviewer (AO).
Statistical analysis
Data were extracted from original articles and then exported to STATA v 14 for analysis. The prevalence of disclosure status with a 95% confidence interval (CI) and OR of the associated factors was presented in the form of a forest plot. Cochran Q test (chi-squared statistic) and I2 statistic on forest plots were used to check heterogeneity among the included studies. Sensitivity and subgroup analyses were conducted to assess the presence of heterogeneity among primary studies. A country-based sub-group analysis was performed as heterogeneity was observed. As heterogeneity was observed for the first outcome, a random-effects model was used to determine the prevalence of disclosure status. To test publication bias, a funnel plot and Egger's weighted regression tests were computed.
Results
Study selection
Seventy-one articles were identified through different database searches. Of those, 51 articles were removed due to duplications. Then, 6 articles were removed because they failed to meet the eligibility criteria. Fourteen articles that have a score of seven and above on the JBI quality appraisal were included in the analysis. PRISMA flow diagram was used to present the selection process.
Characteristics of included studies
About 4,365 study populations were involved in this review. The sample size ranges from a minimum of 42 to a maximum of 665 from Ethiopia. Of all studies, eight (22–29) were from Ethiopia, three (30–32) were from Uganda and three (33–35) were from Tanzania. All included articles were cross-sectional studies (Table 1).
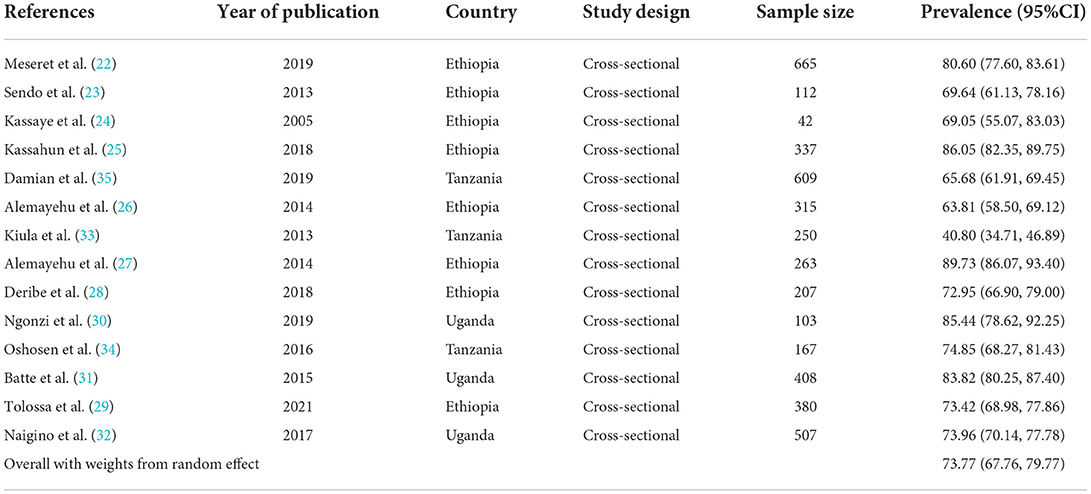
Table 1. Summary of included studies on magnitude of HIV sero-status disclosure among women in East Africa, 2021.
Prevalence of HIV sero-status disclosure among WLHIV
The pooled prevalence of HIV-positive disclosure status among women in East Africa was 73.77% (95% CI: 67.76, 79.77). The largest prevalence was observed from Ethiopia 89.73% (95% CI: 86.07, 93.40) (27), while the smallest was from Tanzania 40.80% (95% CI: 34.71, 46.89) (33). Due to heterogeneity, the magnitude of HIV-positive disclosure among women was computed using a random-effect model (I2= 95.7%, P = < 0.001) (Figure 2).
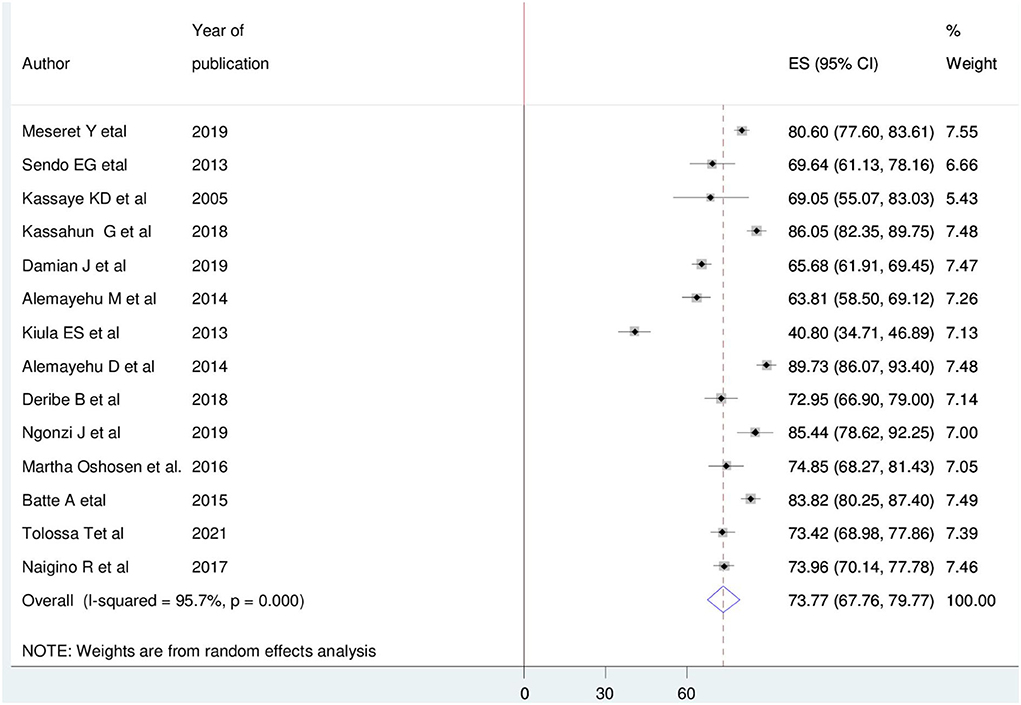
Figure 2. Forest plot of the pooled magnitude of HIV positive sero-status disclosure among women in East Africa, 2021.
Factors related with heterogeneity
High heterogeneity was observed (I-squared = 95.7%, p = < 0.001). However, the source of heterogeneity is not due to sample size and year of publication (Table 2).
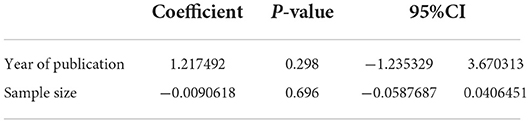
Table 2. Factors related with heterogeneity of HIV-positive sero-status disclosure among women in East Africa, 2021.
Subgroup analysis and publication bias
Country-based subgroup analysis was conducted. Accordingly, the prevalence ranged from the smallest in Tanzania 60.46% (95% CI: 42.71, 78.20) (33–35) to the largest in Uganda 80.83% (95% CI: 73.40, 88.26) (30–32) (Figure 3). The funnel plot and Egger test were computed to assess the publication bias. As a result, the funnel plot shows a shape of symmetry (Figure 4), and the Egger test showed no statistical significance for the presence of publication bias (p-value = 0.16).
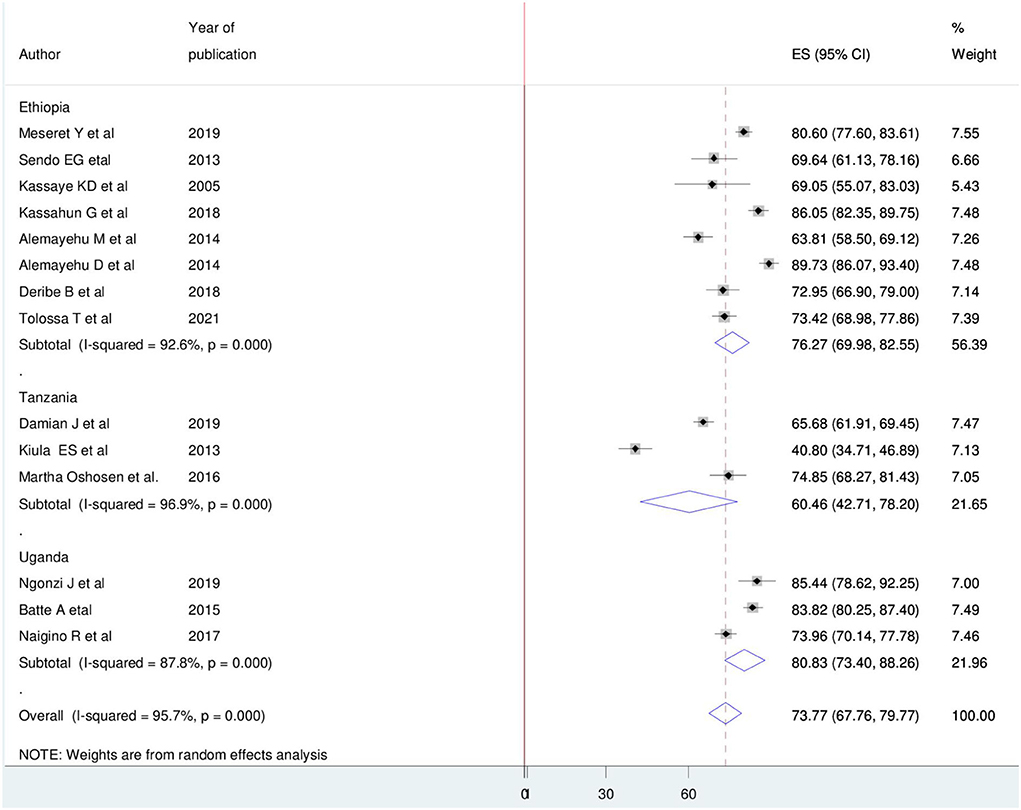
Figure 3. Subgroup analysis on pooled magnitude of HIV positive sero-status disclosure among women in East Africa, 2021.
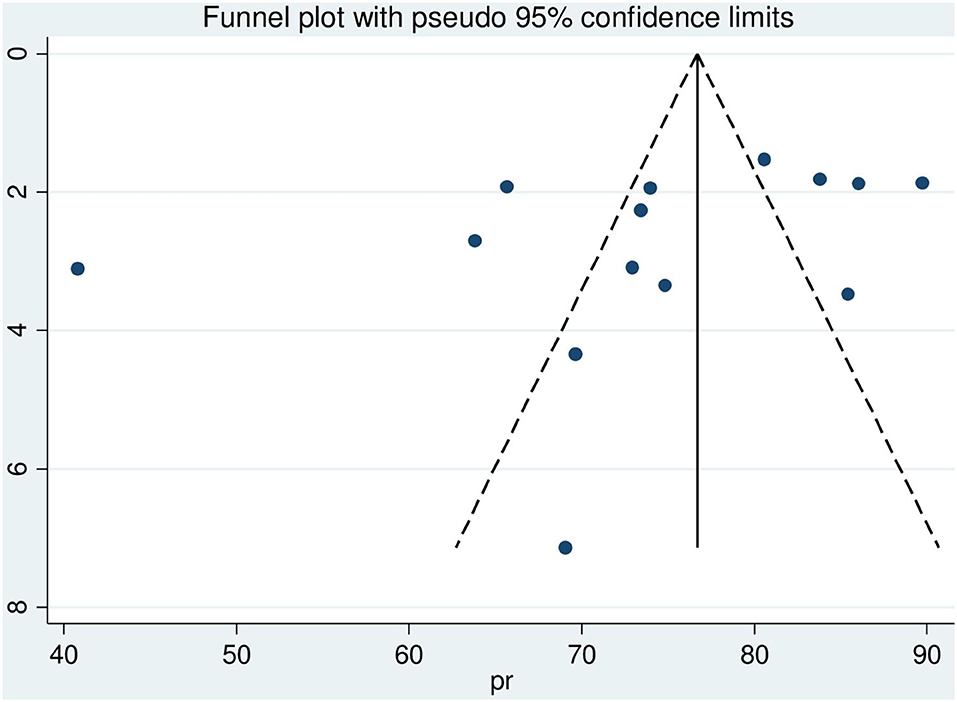
Figure 4. Funnel plot with 95% confidence limit of HIV sero-status disclosure women in East Africa, 2021.
Sensitivity analysis
In this review, to identify the influence of a single study on the overall meta-analysis, sensitivity analysis was performed using a random-effects model. The result showed there was no strong evidence for the effect of a single study's influence on the overall meta-analysis (Figure 5).
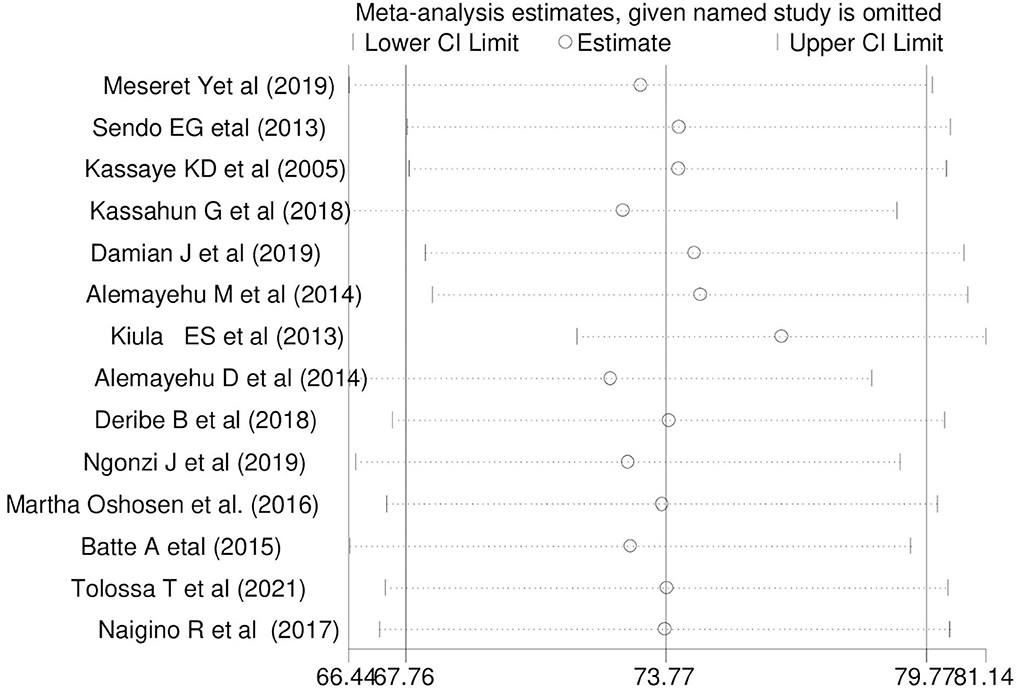
Figure 5. Sensitivity analysis for single study influence of the pooled magnitude of HIV sero-status disclosure women in East Africa, 2021.
Factors associated with HIV sero-status disclosure among women
Association between HIV sero-status disclosure and knowing partner HIV status
Five articles were included (22, 26–28, 34) and the pooled finding indicated that there is a significant association between HIV sero-status disclosure and knowing the partner's HIV status. The result indicated that women who know their partner's HIV status were 10.04 times more likely to disclose HIV sero-status than those who do not know their partner's status OR = 10.04(95%CI 3.36, 31.84) Cite. In this finding, a random-effect model was used (I2 = 92.5%, P = < 0.001) (Figure 6).
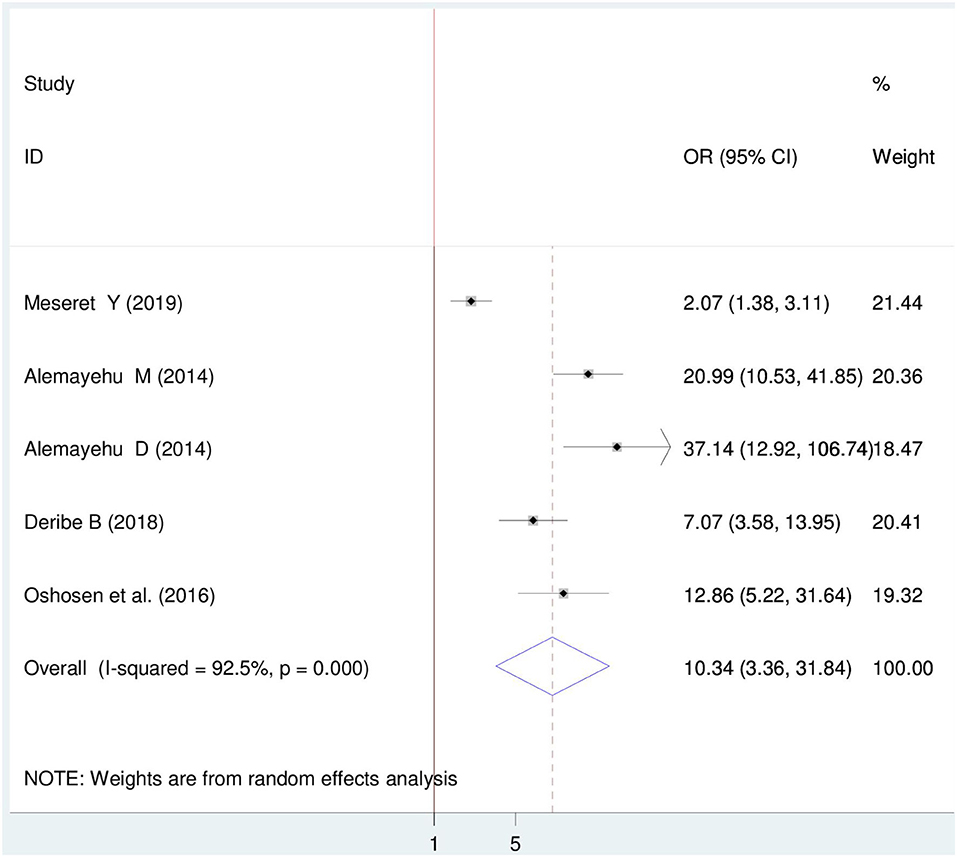
Figure 6. Forest plot of association between HIV sero-status disclosure and knowing partner HIV status among women in East Africa, 2021.
Association between HIV sero-status disclosure and marital status
Six articles were included (22, 29, 31, 33–35). Four articles indicated a positive association (29, 31, 34, 35) while one article showed a negative association with disclosure status. The pooled finding showed a significant association between HIV sero-status disclosure and marital status. Thus, married women were 2.46 times more likely to disclose HIV sero-status than those who are single OR = 2.46 (95%CI 1.23, 4.89). In this finding, a random effect model was used (I2 = 90.01%, P = < 0.001) (Figure 7).
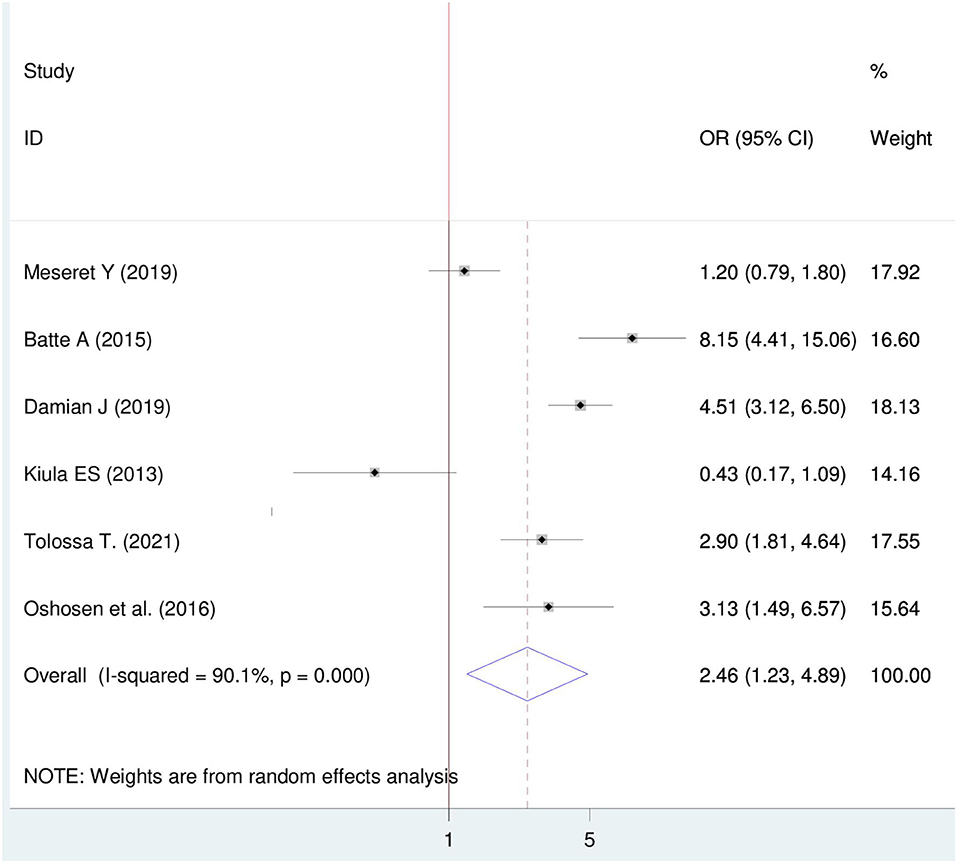
Figure 7. Forest plot of association between HIV sero-status disclosure and marital status, among women in East Africa 2021.
Association between HIV sero-status disclosure and relationship before the test
Four articles were included (22–24, 28) in which three articles showed a significant association between HIV sero-status disclosure and the relationship before the test. The Meta-regression finding showed that there is a significant association between HIV sero-status disclosure and a relationship before the test. Though, women who have a smooth relationship were 3.30 times more likely to disclose HIV sero-status than those who have disagreements with their partner OR = 3.30 (95%CI 1.39, 7.84). In this finding, a random effect model was used (I2 = 68.04%, P = 0.023) (Figure 8).
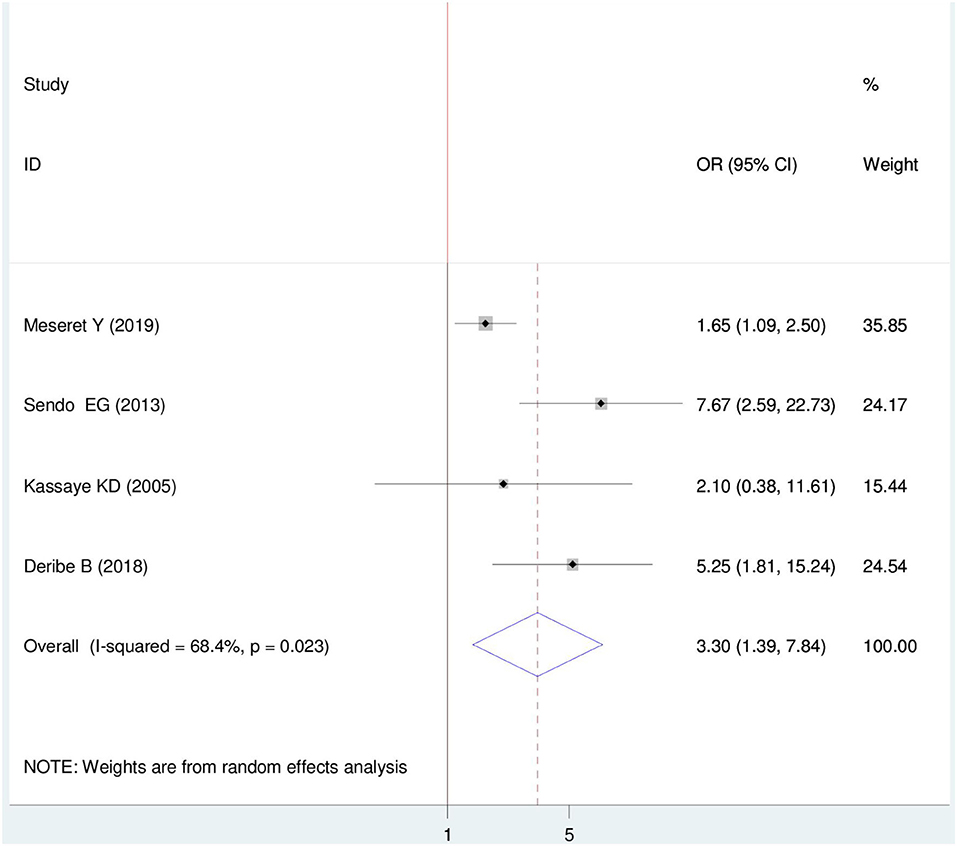
Figure 8. Forest plot of association between HIV sero-status disclosure and relationship before test among women in East Africa, 2021.
Association between HIV sero-status disclosure and discussion before the test
Six primary articles were included (22–24, 26, 33, 35). The pooled finding from this research showed that there is a relationship between discussing before the test and HIV sero-status disclosure (OR = 6.96 (95%, CI: 3.21, 15.05). The odds of disclosing HIV sero-status were 6.96 times higher among women who had a discussion on HIV before the test than their counterparts. For this Meta-regression, a random effect model was used (I2 = 86.3%, P = < 0.001) (Figure 9).
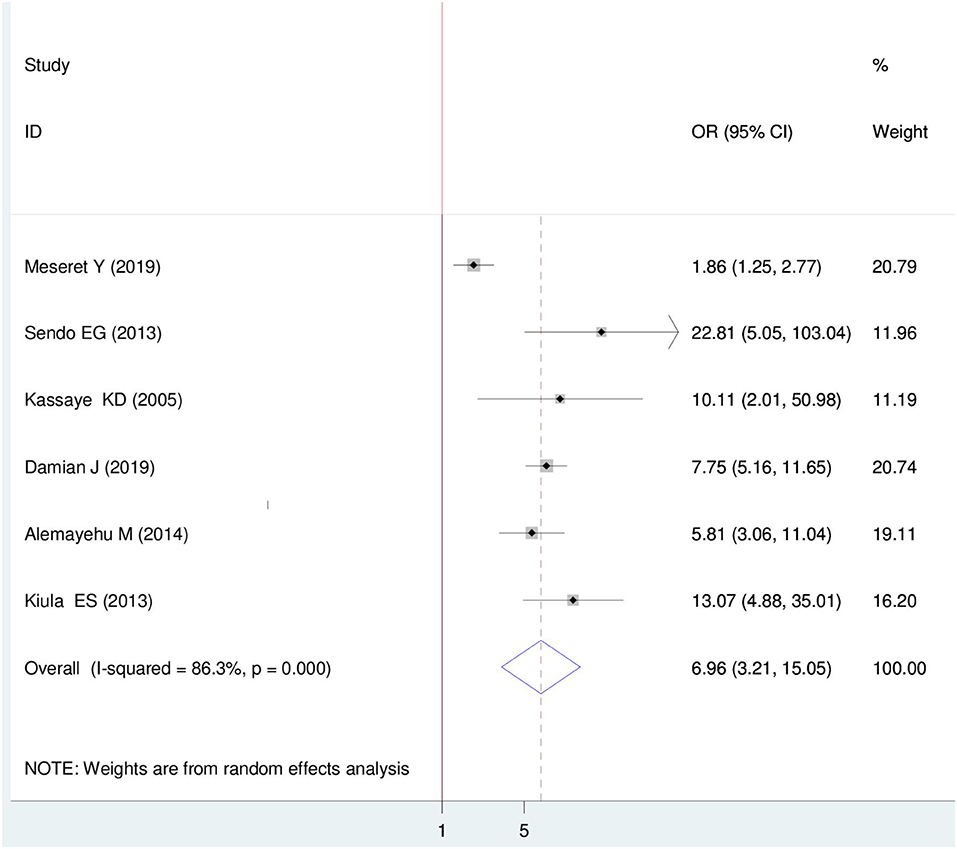
Figure 9. Forest plot of association between HIV sero-status disclosure and discussion on HIV before test among women in East Africa, 2021.
Discussion
Despite major interventions that have been made to confront HIV epidemics; it remains a major public health problem globally. Disclosure of HIV positive among WLHIV is fundamental in PMTCT and to reduce HIV spreads within the community. Literature from East Africa reports the prevalence and factors associated with HIV sero-status disclosure differently and there is no pooled evidence regarding this issue. This systematic review and meta-analysis aimed to assess the pooled prevalence of HIV sero- positive disclosure status among women in East Africa. Accordingly, the pooled magnitude of HIV sero-positive disclosure among women in East Africa was 73.77% (95% CI: 67.76, 79.77). This is similar to the meta-analysis result conducted in Ethiopia (73%) (36) and South Africa (74.4%) (37), but lower than the study from Nigeria (88%) (38), Northern Nigeria (89%) (39), Enugu, Nigeria (96.7%) (40) and Southeastern Nigeria (97.1%) (41). Conversely, the current review finding was higher than the study conducted in sub-Saharan Africa (67%) (42) and Barbados (28.8%) (43). The possible reason for the variation might be the socio-economic, cultural, access to health care services, and year difference in primary studies.
Several factors contributed to the disclosure status of Women Living with HIV. Likewise, knowing the partner(s) sero-status, marital status, relationship before the test, and having a discussion on HIV with the sexual partner before the test were among identified factors. Those women who know their partners' HIV status were 10 times more likely to disclose their HIV sero-status. This is supported by a study from sub-Saharan Africa (42), and South Africa (44). This is probably because women who have HIV-positive partner can easily disclose their HIV sero-status as HIV-positive individual prefers to disclose to a partner with a known HIV-positive than to a negative or unknown HIV sero-status partner. Women who know their partner's status may have a discussion about HIV testing; this could facilitate the disclosure process. Furthermore, married women were more than two times more likely to disclose their HIV sero-status than those who are single. This is supported by study findings in Ogun Nigeria (45). Married couples have known each other and have common things together which may ease the disclosure process.
Additionally, having a smooth relationship with a partner increases HIV sero-status disclosure. A study from sub-Saharan Africa (42), and urban Nigeria (38) support this finding. The possible explanation; a smooth relationship between the couples encourages discussion on HIV testing and that might simplify the disclosure course. Moreover, women who have a discussion about HIV with their partners were seven times more likely to disclose their HIV sero-status than those who had no discussion. This finding is supported by previous meta-analyses (36). Discussion leads to agreement and trustworthiness. Couples who discussed HIV tests may also discuss the way to disclose their status.
HIV sero-status disclosure following voluntary counseling and testing has a great contribution in preventing the onward HIV infection community transmission; particularly averting MTCT. Therefore, the current review has an implication for policymakers and health care providers to further strengthen counseling and guiding couples, particularly women on further HIV sero-status disclosure.
Strengths and limitations of the study
Even though various databases were extensively searched for both published articles, but not without limitations. The majority of the primary studies included in this review were cross-sectional in design; therefore, it is not possible to conclude the temporal relationship between the disclosure status and associated factors. As well, only articles published in the English language were included. Finally, some variables related to disclosure were not included in this review as we analyzed variables shown in the primary studies.
Conclusion
Significant numbers of women are not disclosed their HIV sero-status. Knowing the partner's HIV sero-status, being married, having a smooth relationship, and discussion on HIV before the test were identified factors of disclosure status among WLHIV in East Africa. Therefore, policymakers and health care providers need to strengthen further disclosure of HIV sero-status among women.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
GM conceptualized the topic of the study. DB, DM, and BW searched and extracted articles. GM, EM, AT, and LB analyzed the data. AO, DC, and GF participated in data extraction, analysis, and write-up of the manuscript. All authors read and approved the final manuscript.
Acknowledgments
We would like to thank all authors of the primary studies.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer ET declared a shared affiliation with the authors to the handling editor at time of review.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
HIV, Human Immunodeficiency Virus; PMTCT, Preventing mother-to-child transmission; AOR, Adjusted Odds ratio; CI, Confidence Interval; JBI, Joanna Briggs Institute; WHO, World Health Organization; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; WLHIV, Women Living with HIV.
References
1. Global H. AIDS Statistics−2021 Fact Sheet. Geneva. Availbale online at: https://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf (accessed April 1,2021).
2. Buvé A, Bishikwabo-Nsarhaza K, Mutangadura G. The spread and effect of HIV-1 infection in sub-Saharan Africa. Lancet. (2002) 359:2011–7. doi: 10.1016/S0140-6736(02)08823-2
3. Medley A, Garcia-Moreno C, McGill S, Maman S. Rates, barriers and outcomes of HIV serostatus disclosure among women in developing countries: implications for prevention of mother-to-child transmission programmes. Bull World Health Organiz. (2004) 82:299–307.
4. Obermeyer CM, Baijal P, Pegurri E. Facilitating HIV disclosure across diverse settings: a review. Am J Public Health. (2011) 101:1011–23. doi: 10.2105/AJPH.2010.300102
5. Tshisuyi ET. Disclosure of HIV Positive Status to Sexual Partners Among Pregnant Women in a Health District Botswana. Stellenbosch: Stellenbosch University (2014).
6. Bassett MT. Ensuring a public health impact of programs to reduce HIV transmission from mothers to infants: the place of voluntary counseling and testing. Am J Public Health. (2002) 92:347–51. doi: 10.2105/AJPH.92.3.347
7. Arrivé E, Dicko F, Amghar H, Aka AE, Dior H, Bouah B, et al. HIV status disclosure and retention in care in HIV-infected adolescents on antiretroviral therapy (ART) in West Africa. PLoS ONE. (2012) 7:e33690. doi: 10.1371/journal.pone.0033690
8. Norman A, Chopra M, Kadiyala S. Factors related to HIV disclosure in 2 South African communities. Am J Public Health. (2007) 97:1775–81. doi: 10.2105/AJPH.2005.082511
9. Akani C, Erhabor O. Rate, pattern and barriers of HIV serostatus disclosure in a resource-limited setting in the Niger delta of Nigeria. Trop Doct. (2006) 36:87–9. doi: 10.1258/004947506776593378
10. Antelman G, Fawzi MCS, Kaaya S, Mbwambo J, Msamanga GI, Hunter DJ, et al. Predictors of HIV-1 serostatus disclosure: a prospective study among HIV-infected pregnant women in Dar es Salaam, Tanzania. AIDS. (2001) 15:1865. doi: 10.1097/00002030-200109280-00017
11. Nyblade L, Kerry M. Can we Measure HIV/AIDS-Related Stigma and Discrimination? Current Knowledge About Quantifying Stigma in Developing Countries. Washington, DC: International Center for Research on Women (ICRW) (2006).
12. Körner H. Negotiating cultures: disclosure of HIV-positive status among people from minority ethnic communities in Sydney. Cult Health Sex. (2007) 9:137–52. doi: 10.1080/13691050600975462
13. Ouedraogo T, Ouedraogo A, Ouedraogo V, Kyelem N, Soubeiga A. HIV infection and modification of social relationships: study of 188 HIV-infected persons in Ouagadougou (Burkina Faso). Cahiers d'études Recherches Francophones/Santé. (2005) 15:253–7.
14. Obi SN, Ifebunandu NA. Consequences of HIV testing without consent. Int J STD AIDS. (2006) 17:93–6. doi: 10.1258/095646206775455649
15. Semrau K, Kuhn L, Vwalika C, Kasonde P, Sinkala M, Kankasa C, et al. Women in couples antenatal HIV counseling and testing are not more likely to report adverse social events. AIDS. (2005) 19:603. doi: 10.1097/01.aids.0000163937.07026.a0
16. Ammassari A, Trotta MP, Murri R, Castelli F, Narciso P, Noto P, et al. Correlates and predictors of adherence to highly active antiretroviral therapy: overview of published literature. J Acquired Immune Defic Syndromes. (2002) 31:S123–7. doi: 10.1097/00126334-200212153-00007
17. Mill JE. Shrouded in secrecy: breaking the news of HIV infection to Ghanaian women. J Transcult Nurs. (2003) 14:6–16. doi: 10.1177/1043659602238345
18. Bishop GD, Oh H, Swee H. Attitudes and beliefs of Singapore health care professionals concerning HIV/AIDS. Singap Med J. (2000) 41:55–63. Available online at: http://www.smj.org.sg/sites/default/files/4102/4102a1.pdf
19. Miller AN, Rubin DL. Motivations and methods for self-disclosure of HIV seropositivity in Nairobi, Kenya. AIDS Behav. (2007) 11:687–97. doi: 10.1007/s10461-006-9198-z
20. Chandra PS, Deepthivarma S, Manjula V. Disclosure of HIV infection in South India: patterns, reasons and reactions. AIDS Care. (2003) 15:207–15. doi: 10.1080/0954012031000068353
21. JBI. Critical Appraisal Checklist for Analytical Cross Sectional Studies. The Joanna Briggs Institute (2017).
22. Meseret Y, Dulla D, Nega B. Prevalence and factors affecting disclosure of HIV status among pregnant women attending antenatal care in Addis Ababa public health centres: a cross sectional survey. Obstet Gynecol Int J. (2019) 10:317–24. doi: 10.15406/ogij.2019.10.00460
23. Sendo EG, Cherie A, Erku TA. Disclosure experience to partner and its effect on intention to utilize prevention of mother to child transmission service among HIV positive pregnant women attending antenatal care in Addis Ababa, Ethiopia. BMC Public Health. (2013) 13:765. doi: 10.1186/1471-2458-13-765
24. Kassaye KD, Lingerh W, Dejene Y. Determinants and outcomes of disclosing HIV-sero positive status to sexual partners among women in Mettu and Gore towns, Illubabor Zone southwest Ethiopia. Ethiopian J Health Dev. (2005) 19:126–31. doi: 10.4314/ejhd.v19i2.9981
25. Kassahun G, Tenaw Z, Belachew T, Sinaga M. Determinants and status of HIV disclosure among reproductive age women on antiretroviral therapy at three health facilities in Jimma Town, Ethiopia, 2017. Health Sci J. (2018) 12(2). doi: 10.21767/1791-809X.1000558
26. Alemayehu M, Aregay A, Kalayu A, Yebyo H. HIV disclosure to sexual partner and associated factors among women attending ART clinic at Mekelle hospital, Northern Ethiopia. BMC Public Health. (2014) 14:746. doi: 10.1186/1471-2458-14-746
27. Alemayehu D, Tadesse S, Adefris M, Birhanu Z. HIV serostatus disclosure and associated factors among HIV positive pregnant women attending antenatal care services in northwest Ethiopia. Int J Infect Control. (2014) 10:1–8. doi: 10.3396/ijic.v10i4.028.14
28. Deribe B, Ebrahim J, Bush L. Outcomes and factors affecting HIV status disclosure to regular sexual partner among women attending antiretroviral treatment clinic. J AIDS Clin Res. (2018) 9:2. doi: 10.4172/2155-6113.1000760
29. Tolossa T, Wakuma B, Besho M, Mulisa D, Fekadu G, Bayisa L, et al. HIV serostatus disclosure and associated factors among HIV positive pregnant and lactating women at Nekemte public health facilities, western Ethiopia. PLoS ONE. (2021) 16:e0248278. doi: 10.1371/journal.pone.0248278
30. Ngonzi J, Mugyenyi G, Kivunike M, Mugisha J, Salongo W, Masembe S, et al. Frequency of HIV status disclosure, associated factors and outcomes among HIV positive pregnant women at Mbarara Regional Referral Hospital, southwestern Uganda. Pan Afr Med J. (2019) 32. doi: 10.11604/pamj.2019.32.200.12541
31. Batte A, Katahoire AR, Chimoyi A, Ajambo S, Tibingana B, Banura C. Disclosure of HIV test results by women to their partners following antenatal HIV testing: a population-based cross-sectional survey among slum dwellers in Kampala Uganda. BMC Public Health. (2015) 15:63. doi: 10.1186/s12889-015-1420-3
32. Naigino R, Makumbi F, Mukose A, Buregyeya E, Arinaitwe J, Musinguzi J, et al. HIV status disclosure and associated outcomes among pregnant women enrolled in antiretroviral therapy in Uganda: a mixed methods study. Reprod Health. (2017) 14:1–11. doi: 10.1186/s12978-017-0367-5
33. Kiula ES, Damian DJ, Msuya SE. Predictors of HIV serostatus disclosure to partners among HIV-positive pregnant women in Morogoro, Tanzania. BMC Public Health. (2013) 13:433. doi: 10.1186/1471-2458-13-433
34. Oshosen M, Sabasaba A, JSN, Mmbaga BT. Prevalence and factors associated with hiv status disclosure among pregnant and lactating women on antiretroviral treatment after rollout of option B plus in Urban Moshi Tanzania. Glob J Epidemiol Public Health. (2016) 3:8–15. doi: 10.12974/2313-0946.2016.03.01.2
35. Damian DJ, Ngahatilwa D, Fadhili H, Mkiza JG, Mahande MJ, Ngocho JS, et al. Factors associated with HIV status disclosure to partners and its outcomes among HIV-positive women attending Care and Treatment Clinics at Kilimanjaro region, Tanzania. PLoS ONE. (2019) 14:e0211921. doi: 10.1371/journal.pone.0211921
36. Mekonnen FA, Lakew AM, Muchie KF, Teshome DF. Sero-positive HIV result disclosure to sexual partner in Ethiopia: a systematic review and meta-analysis. BMC Public Health. (2019) 19:1743. doi: 10.1186/s12889-019-8097-y
37. Adeniyi OV, Ajayi AI, Selanto-Chairman N, Goon DT, Boon G, Fuentes YO, et al. Demographic, clinical and behavioural determinants of HIV serostatus non-disclosure to sex partners among HIV-infected pregnant women in the Eastern Cape, South Africa. PLoS ONE. (2017) 12:e0181730. doi: 10.1371/journal.pone.0181730
38. Olagbuji B, Ezeanochie M, Agholor K, Olagbuji Y, Ande A, Okonofua F. Spousal disclosure of HIV serostatus among women attending antenatal care in urban Nigeria. J Obstetr Gynaecol. (2011) 31:486–8. doi: 10.3109/01443615.2011.563637
39. Sagay AS, Musa J, Ekwempu C, Imade GE, Babalola A, Daniyan G, et al. Partner disclosure of HIV status among HIV positve mothers in Northern Nigeria. Afr J Med Med Sci. (2006) 35(Suppl.):119–23. Available online at: https://irepos.unijos.edu.ng/jspui/bitstream/123456789/849/1/Sagay_Partner%20Disclosure%20of%20HIV%20Status%20Among%20HIV%20Positive%20mothers%20in%20northern%20Nigeria.pdf
40. Ezegwui H, Nwogu-Ikojo E, Enwereji J, Dim C. HIV serostatus disclosure pattern among pregnant women in Enugu, Nigeria. J Biosoc Sci. (2009) 41:789. doi: 10.1017/S0021932009990137
41. Igwegbe A, Ugboaja J. Rate and correlates of HIV serostatus disclosure among HIV positive pregnant women in Nnewi southeastern Nigeria. J Med Med Sci. (2010) 1:296–301. Available online at: https://www.interesjournals.org/articles/rate-and-correlates-of-hiv-serostatus-disclosure-among-hiv-positive-pregnant-women-in-nnewi-southeastern-nigeria.pdf
42. Tam M, Amzel A, Phelps BR. Disclosure of HIV serostatus among pregnant and postpartum women in sub-Saharan Africa: a systematic review. AIDS Care. (2015) 27:436–50. doi: 10.1080/09540121.2014.997662
43. Kumar A, Waterman I, Kumari G, Carter AO. Prevalence and correlates of HIV serostatus disclosure: a prospective study among HIV-infected postparturient women in Barbados. AIDS Patient Care & STDs. (2006) 20:724–30. doi: 10.1089/apc.2006.20.724
44. Vu L, Andrinopoulos K, Mathews C, Chopra M, Kendall C, Eisele TP. Disclosure of HIV status to sex partners among HIV-infected men and women in Cape Town, South Africa. AIDS Behav. (2012) 16:132–8. doi: 10.1007/s10461-010-9873-y
Keywords: disclosure status, HIV, women, East Africa, meta-analysis
Citation: Mosisa G, Mulisa D, Oluma A, Bayisa L, Merdassa E, Bayisa D, Tamiru A, Tolossa T, Chala Diriba D, Fetensa G and Wakuma B (2022) HIV sero-status disclosure and associated factors among HIV positive women in East Africa: Systematic review and meta-analysis. Implications for prevention of mother-to-child HIV transmission. Front. Public Health 10:919410. doi: 10.3389/fpubh.2022.919410
Received: 13 April 2022; Accepted: 31 October 2022;
Published: 22 November 2022.
Edited by:
Margaret Ip, The Chinese University of Hong Kong, ChinaReviewed by:
Muki Shey, University of Cape Town, South AfricaEdosa Kifle Tola, Wollega University, Ethiopia
Deborah Konopnicki, Hôpital Saint-Pierre, Belgium
Copyright © 2022 Mosisa, Mulisa, Oluma, Bayisa, Merdassa, Bayisa, Tamiru, Tolossa, Chala Diriba, Fetensa and Wakuma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Getu Mosisa, getumosisa344@gmail.com
 Getu Mosisa
Getu Mosisa