- 1Department of Ophthalmology, The Third People's Hospital of Dalian, Dalian, China
- 2Department of Ophthalmology, Dalian Third People's Hospital Affiliated to Dalian Medical University, Dalian, China
- 3Department of Ophthalmology, Guangdong Eye Institute, Guangdong Provincial People's Hospital, Guangzhou, China
- 4Department of Ophthalmology, The First Affiliated Hospital of Dalian Medical University, Dalian, China
- 5He Eye Hospital, Dalian, China
- 6Beijing Center for Diseases Prevention and Control, Beijing, China
Purpose: To assess the prevalence of refractive errors (REs) in school children aged 6–18 years in urban and rural settings in Dalian, Northeast of China.
Methods: This is a school-based cross-sectional survey using multi-stage randomization technique. Six- to eighteen-year-old school children from elementary schools, junior and senior high schools from a rural area and an urban area in Dalian were included in December 2018. All subjects underwent a comprehensive questionnaire and eye examination.
Results: A total of 4,522 school children with 6–18 years of age were investigated. The age, gender-adjusted prevalence of myopia, and anisometropia were 82.71 and 7.27% among the urban students as compared to 71.76% and 5.41% among the rural ones (OR = 1.80, 95 % CI = 1.53 - 2.11, P < 0.001; OR = 1.29, 95 % CI = 1.00–1.67, P = 0.049), respectively. The hyperopia was less common in urban students than in rural ones (5.63 vs. 10.21%; OR = 0.54, 95 % CI: 0.43–0.67, P < 0.001). However, there was no significant difference in prevalence of astigmatism between urban (46.07%) and rural (44.69%) participants (OR = 0.96, 95 % CI: 0.84–1.10, P = 0.559). The differences on prevalence of REs were attributed to different social-demographic and physiologic factors.
Conclusions: The students from urban settings are more likely to have myopia and anisometropia but less likely to have hyperopia than their rural counterparts. Although considerable attention had been paid to controlling REs, it is necessary to further consider the urban-rural differences in REs.
Introduction
The refractive errors (REs), especially myopia, have become the primary cause of vision impairment (VI) and preventable blindness in children. Myopia suggests a significant increase in prevalence globally in the past 50 years and become a significant public health problem across the globe, especially in East Asian countries like Singapore and China (1, 2). In Singapore, the incidence of myopia in children is about 62% (3), and Chinese having higher rates compared with Indians and Malays (4). In Guangzhou China, the prevalence of myopia among schoolchildren is 49.7%, much higher than the United States (20%) (5), Australia (11.9%) (6), and Nigeria (1.9%) (7). Among them, the increase in school children is particularly remarkable, 73.9–90% of high school students were myopia in urban areas of Aisa (8–10).
Various factors, including genetic and environmental factors play a role in the etiology of myopia. Genetically, the prevalence of myopia in children is greater if their parents are myopic (11, 12). Rapidly changing environmental factors are predominant in determining the current patterns of myopia (13). Near-work, time outdoors have shown to be associated with the occurrence and development of myopia (14, 15). Region of habitation, are also thought to influence presence of REs (16). In China, there were two population-based studies reported the rural-urban prevalence of REs among children and adolescents. According to Beijing Pediatric Eye Study, first, they found that prevalence of myopia was significantly associated with urban region (17). However, in further analysis on factors for myopia, prevalence of myopia was not significantly associated with urban region of habitation after adjusting for age, gender, school type, family income, and parental myopia (18). Although separate prevalence rates of REs in rural vs. urban children were reported in Shandong Children Eye Study (19), there remain some gaps in this study. Those prevalence rates were crude rates without adjusting age, gender and other potential confounders.
At present, the prevalence and risk factors of REs in urban and rural school children in Northeast China are still unclear. Whether there are differences in the associated factors of REs in different regions needs further research. In order to understand the prevalence of REs and the risk factors disparity among school children (6–18 years old) between urban and rural settings, we performed this school-based survey in the urban and rural areas of Dalian, Northeast China.
Methods
Participants
This school-based study was initially performed in December 2018. Multi-stage random cluster approach was conducted for sampling. In the first step, one district from each of the rural (Wafangdian County) and urban (Xigang District) regions of Dalian was randomly selected. In the second step, one primary school, one junior high school, and one senior high school were randomly selected from each of the two selected districts. In the third step, two classes of each grade were of randomly selected from each of the including schools. In the final step, all students of the selected classes with age of 6–18 years were sampled. The exclusion criteria were the followings: (1) Participants who reported eye conditions within the last month (e.g., optical correction with othokeratology, eye injuries, conjunctivitis, and corneal irritation); (2) Participants whose parents refused to sign the informed consents.
The study was approved by the respective ethics committees of The Third People‘s Hospital of Dalian and the Health commission of Dalian. This study followed the Declaration of Helsinki. Written consent was obtained from the parents of all children and teenagers.
Interview and data collection
In current study, all participants and their parents completed a detailed questionnaire form. The quality of the questionnaire was controlled by head teacher in each class. The questionnaires are conducted at home.
The questionnaire included two parts (participants' information section and parents' information section). Basic socio-demographic data, such as age, gender, ethnic origin, habitation in urban or rural areas, degree of class and grade, and medical history was included in the first part of the questionnaire. Moreover, this questionnaire section additionally included questions on near-work activities such as the amount of time spent on studying or watching television, mobile phone and on computer activities per day. The first part of the questionnaire also includes questions about outdoor activities such as how long the children spent in outdoor activities per day. The first part of the questionnaire was filled in by the children and assisted by their parents. For very young children who could not read or understand the questionnaire very well (e.g., the youngest children of 6 years old), help was sought from their parents.
In the second part, information of parents' education level, refractive error history (e.g., myopia, hyperopia, astigmatism) were obtained using questionnaire from participants‘ parents.
After the interview, comprehensive ophthalmological examinations were conducted on the school premises by two trained optometrists. Refractive error measurements, uncorrected visual acuity as well as best corrected visual acuity (BCVA) were tested using non-cycloplegic auto-refractometry (AR-1, NIDEK, Japan) by a senior experienced optometrist. Moreover, intraocular pressure (IOP) was measured by non-contact tonometry (NT-510, NIDEK, Japan). Axial length was tested by IOL Master (Carl Zeiss Meditec, Jena, Germany). The mean of three readings were taken.
Measured variables
The definitions of refractive error vary across the selected prevalence studies, we choose the definition that is common in clinical use (19, 20). The spherical equivalent (SE) of the refraction was calculated as the spherical refractive error plus half of the minus cylindrical refractive error. Myopia was defined as SE < −0.5 dioptres (D), and hyperopia was defined as SE > +0.5 D in one or both eyes. Myopia can be classified as low, moderate, or high myopia. Low myopia was defined as SE −0.75 D to −2.75 D, moderate myopia was defined as SE −3.00 D to −4.75 D, and high myopia was defined as SE ≤ -5.0 D. Astigmatism was defined as ≥ +0.75 D of the cylinder in either eye. Anisometropia was defined as difference between right eye to left eye in refractive error (SE) of ≥1.0 D.
Statistics
The data were analyzed using a commercially available statistical program SAS 9.3 (SAS institute, Cary, NC, USA) and SPSS 20.0 (SPSS Inc., Chicago, IL). Only the data for eye with high severity of refraction is presented. Participants included in the final analysis were divided into three age groups (6–10, 11–15, and 16–18 years old, respectively) which were consistent with the distribution of education level for including participants. The age- and gender-specific prevalence rates of REs and subtypes were assessed. The difference of the variables (age groups, gender and region) with REs was assessed using the Student's t-test for the continuous variables and the Pearson's χ2 test for the categorical variables. Logistic regression analysis was performed to determine risk factors using odds ratio (OR) estimates with 95% confidence intervals (CI). A multivariate regression analysis was performed with P-value < 0.05 being required for entering the model. All P-values were 2-sided and considered statistically significant when <0.05.
Results
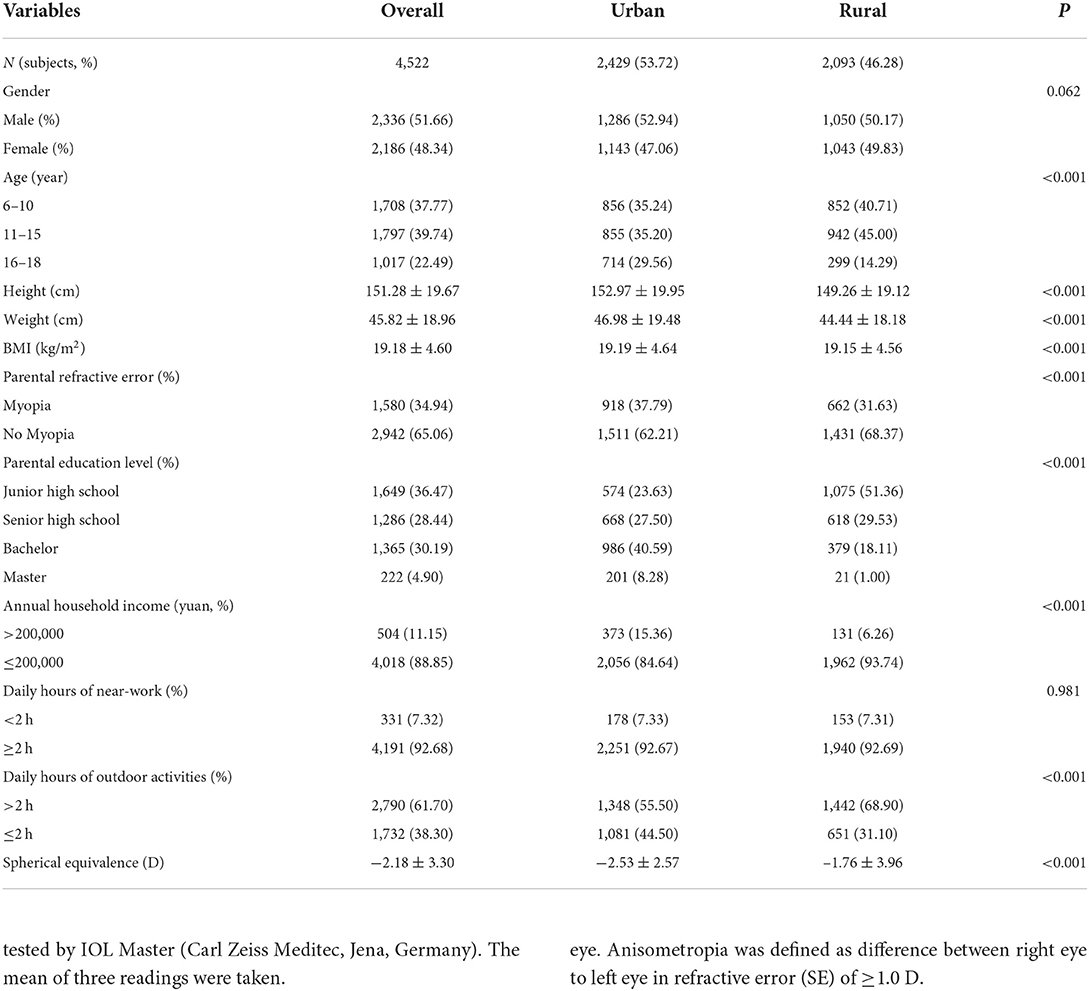
In our study, the seven schools had a total student of 4,583 individuals 6–18 years old, and all of participants were given offers to accept the body and eye examination. In total, 4,522 students (2,336 boys) participated in the all examination, corresponding to an overall response rate of 98.7% (98.9% for urban and 98.4% for rural, respectively). Socio-demographic characteristics were compared between urban students and rural students (Table 1). The rural students and the urban students group varied significantly in the level of age with a significantly higher frequency of 6–10 and 11–15 years old in the rural students, and complementarily, a significantly higher frequency of 16–18 years old in the urban students. The urban students were more likely to be with higher frequency of parental refractive error (P < 0.001), annual household income exceeds Renminbi (RMB) 200,000 Yuan ($ 28,982 USD) (P < 0.001), higher parental education level (P < 0.001), daily hours of outdoor activities ≤ 2 h (P < 0.001), and have higher level of height, weight as well as BMI (P < 0.001) but lower refractive status (P < 0.001) than those rural students. Further, there is no significant difference in gender (P = 0.062), and daily hours of near-work (P = 0.981) distribution between urban and rural students.
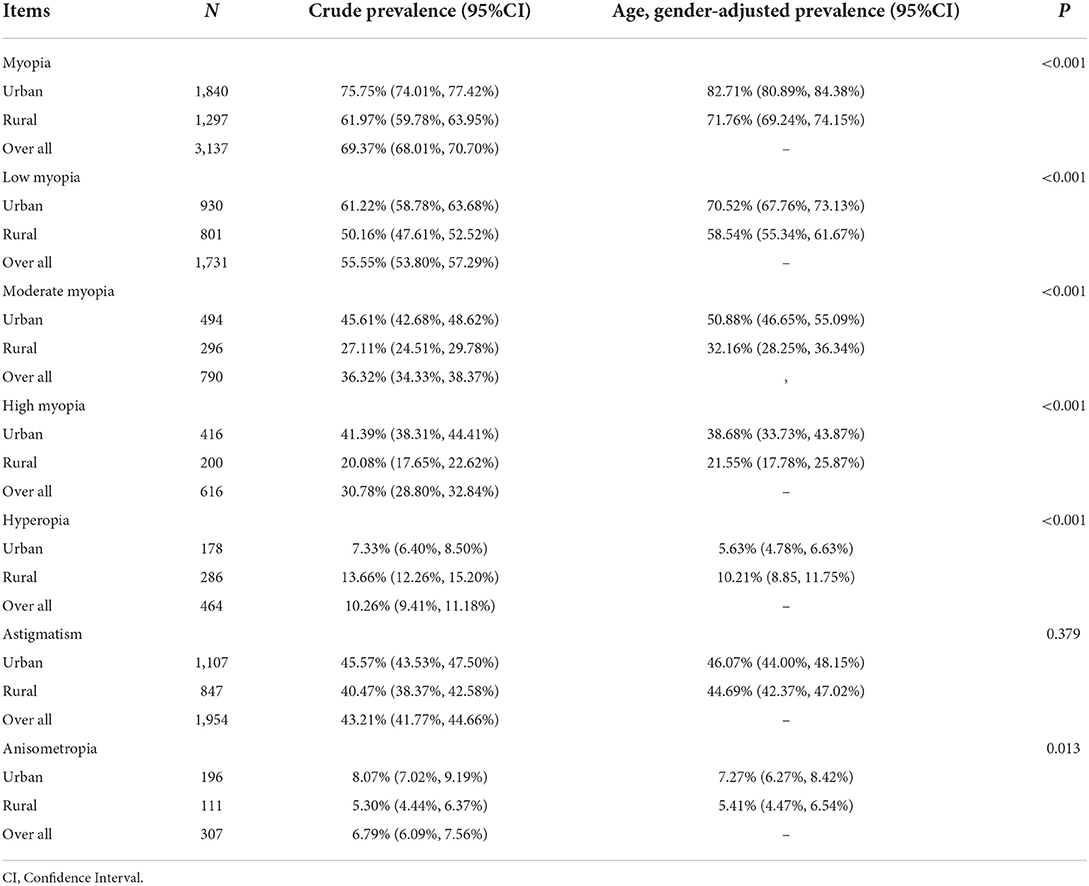
Crude and adjusted-prevalence of REs distributed by region is shown in Table 2. There were differences in the prevalence of different REs values between the urban and rural students. After adjusted for age and gender, the prevalence of overall myopia, low myopia, moderate myopia and high myopia among urban students was 82.71, 70.52, 50.88, and 38.68%, and it was higher than that among rural students (71.76, 58.54, 32.16, and 21.55%, respectively). Similar results were found in anisometropia, the age, gender-standardized prevalence of anisometropia was higher in the urban students than in the rural students (7.27 vs. 5.41%, P = 0.013). However, the age, gender-adjusted prevalence of hyperopia in the rural students was higher than that in the urban students (10.21 vs. 5.63%, P < 0.001). Additionally, no difference was found in astigmatism between the rural and urban students (44.69 vs. 46.07%, P = 0.379).
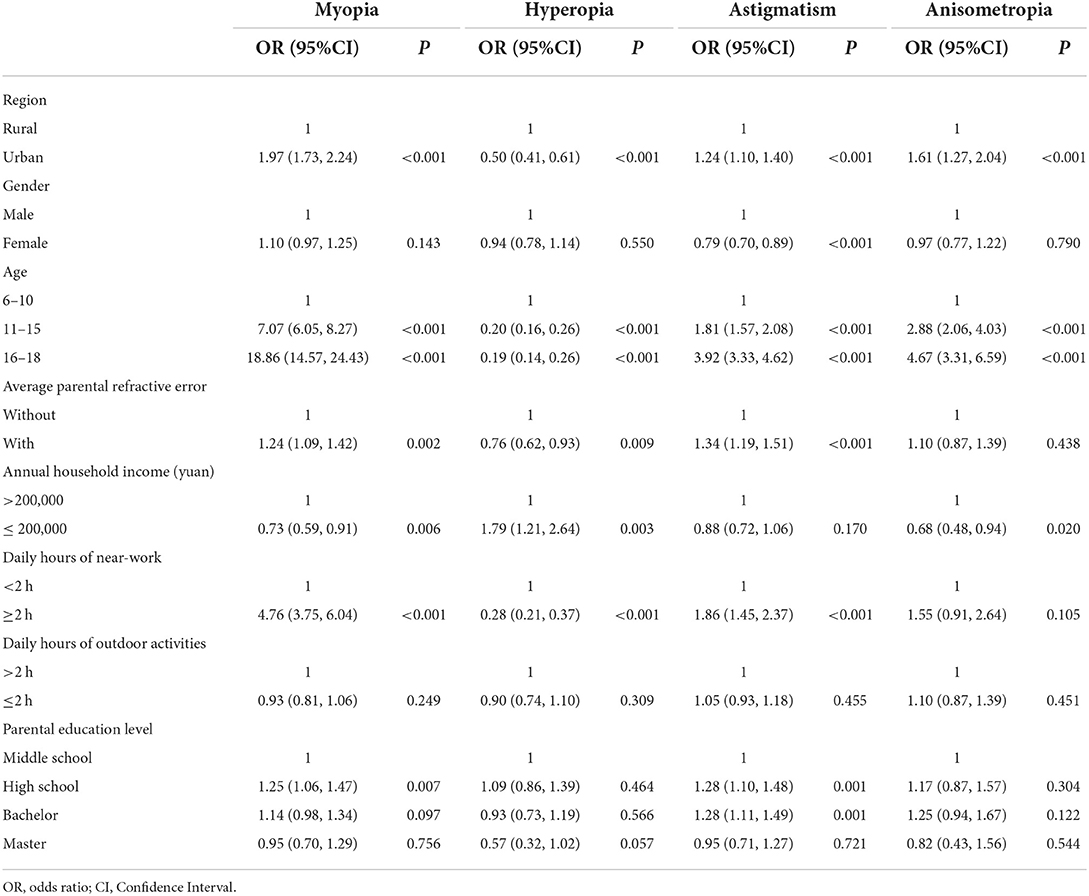
Bivariate analysis showed factors associated with REs among all subjects (Table 3). Currently, students‘ age, region of habitation, average parental refractive error, parental education level, annual household income and daily hours of near-work were associated with myopia (all P < 0.05). However, students‘ age, region of habitation, average parental refractive error, annual household income and daily hours of near-work were associated with hyperopia (all P < 0.05). Further, students‘ age, gender, region of habitation, average parental refractive error, parental education level and daily hours of near-work were associated with astigmatism (all P < 0.05). In addition, there was a significant correlation between age, region of habitation, annual household income and anisometropia (all P < 0.05).
Stepwise multiple logistic models were used to analyze the correlation between region and REs (Table 4). In model 1, after controlling for age and gender, the risk of students living in urban setting developing myopia, hyperopia, and anisometropia were 1.88 (95%CI: 1.62–2.18, P < 0.001), 0.53 (95%CI: 0.43–0.65, P < 0.001), 1.07 (95%CI: 0.94–1.21, P = 0.300), and 1.37 (95%CI: 1.07–1.76, P = 0.013), respectively. However, there is no significant difference on presence of astigmatism between students in rural and urban settings (OR: 1.07, 95%CI: 0.94–1.21, P = 0.300). In model 2 adjusting with age, gender and any variables analyzed significantly in the bivariate analysis (Table 3), students living in urban were 1.80 (95% CI: 1.53–2.11, P < 0.001) times more likely to be myopic, 1.29 (95% CI: 1.00, 1.67, P = 0.049) times more likely to be anisometropia, but 0.54 (95% CI: 0.43–0.67, P < 0.001) times less likely to be hyperopia. Further, there was no significant association between the student's area of residence and astigmatism (OR: 0.96, 95%CI: 0.84–1.10, P = 0.559).
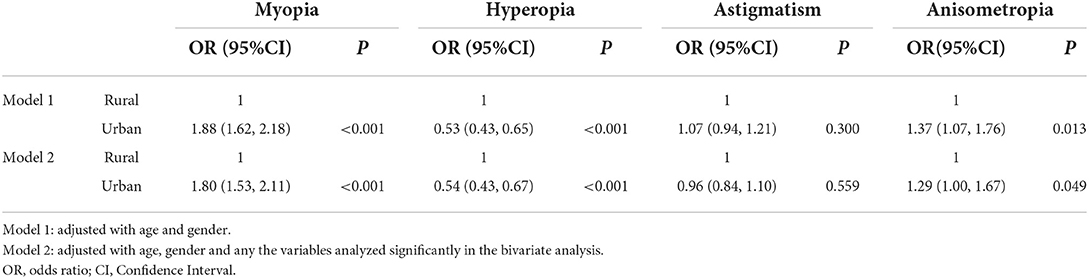
Table 4. Multivariate regression results for the differences on the risk for REs by region of habitation.
Bivariate and multivariate analyses identified the risk factors for the presence of any REs in the urban (Supplementary Table S1) and rural (Supplementary Table S2) students. After multivariate analysis, increasing age and daily hours of near-work were found to be a risk factor for myopia in both the rural and urban groups but with parental refractive error was a risk factor for myopia only in the rural group (all P < 0.001). Increasing age, daily hours of near-work and lower annual household income were independent risk factors for hyperopia in the urban participants while increasing age, daily hours of near-work and average parental refractive error were independent risk factors for hyperopia in the rural participants (all P < 0.05). Female gender was found to be reduced risk for astigmatism in the urban population (P < 0.001). Further, increasing age (P < 0.001) and average parental refractive error (P < 0.05) were independent risk factors for astigmatism in the urban participants. However, increasing age, higher level of annual household income, parental education level and with average parental refractive error were independent risk factors for astigmatism in the rural participants (all P < 0.001).
For anisometropia, we found that only increasing age was a risk factor for urban students but both increasing age and higher level of annual household income were risk factor anisometropia in the rural students (all P < 0.05).
Discussion
Currently, our study provides the population-based cross-sectional data on the region-specific prevalence of REs and its associated risk factors among the urban and rural school children and adolescents across several gradients of age groups which have different socio-cultural factors in Northeast China. First, our findings revealed that the students living in urban setting have higher prevalence rates and risk for myopia and anisometropia than students living in rural, while the prevalence and risk of hyperopia in the urban students was lower than that in the rural students. Moreover, there is no difference on the prevalence and risk of astigmatism between the urban and rural students. Secondly, the prevalence disparities of REs may be due to the various factors between rural and urban areas. Thirdly, there appeared to be significant difference in factors of REs between study participants residing in urban and rural settings.
Consistent with our findings, a previous meta-analysis reported that children from urban environments have 2.6 times the odds of myopia compared with those from rural environments (16). Similarly, the prevalence of myopia in urban setting was higher compared with rural setting based in other region of China (Shandong and Guangzhou) (19, 21). In southern China, the prevalence of myopia in urban children was 73.1% (15 years old), while the prevalence of myopia in rural children was 36.8% (13 years old) and 53.9% (17 years old) (21, 22). However, this disparity was did not adjusted comprehensive variables. Furthermore, we found studies regarding the other prevalence of REs between urban and rural students in China are limited. Table 5 shows the comparison of prevalence of REs between rural and urban settings among school children and adolescents in mainland China. The crude prevalence of myopia, hyperopia, astigmatism, and anisometropia in urban ranges from 5 to 87.7%, 1 to 35.9%, 2.0 to 42.7%, and 7.9%, while in rural ranges from 13.75 to 60%, 1 to 49.2%, 3.75 to 32.1%, and 6.1%, respectively. Our prevalence astigmatism was higher than the surveys while prevalence of myopia, hyperopia and anisometropia data fall somewhere in between. Further, the prevalence disparity of astigmatism between rural and urban areas is still controversial. In Shandong children eye study, students with urban habitation had higher prevalence of astigmatism (40.7%) than those with rural habitation (32.1%) (19). In Dezful County of Iran, school children with urban habitation also had higher prevalence of astigmatism (21%) than those with rural habitation (14.8%) (38). The varying difference in the prevalence of REs between rural and urban habitation may be attributed to the different living environments and variability in the cut-off point adopted to define the presence of REs. In Shandong study, the generational REs shift was measured to by cycloplegia while in our study without cycloplegia (19).
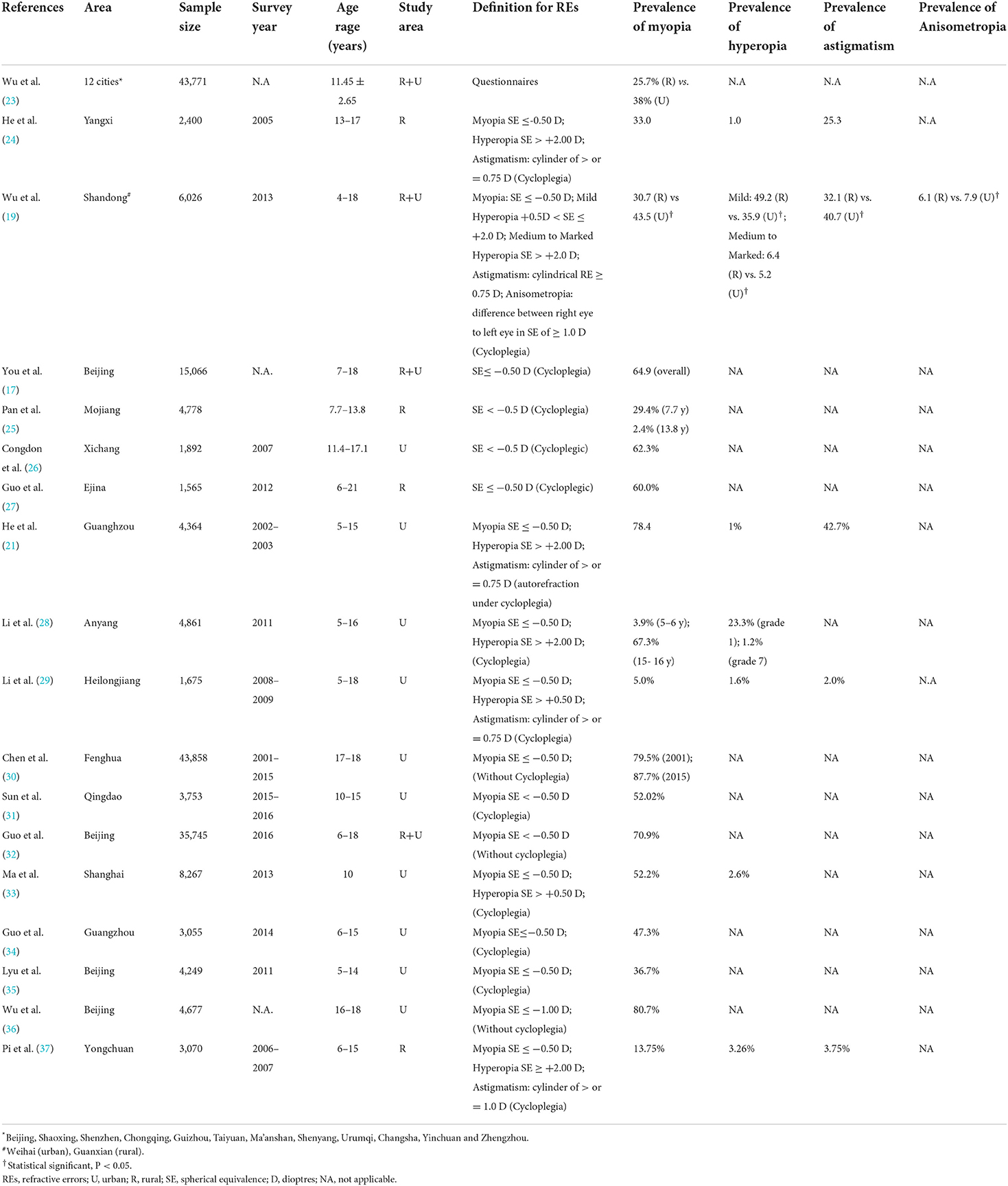
Table 5. Comparison of the reported prevalence of refractive errors in selected population-based studies in school children and adolescents in mainland China.
To date, there are few studies investigating the different associated factors for REs between rural and urban participants. The current study performed in Dalian reports the effect and possible factors on REs in a wide age range among the Chinese urban and rural students. For both rural and urban students, we found that increasing age and longer daily hours of near-work were independently associated with myopia, which was consistent with previous reports in Beijing urban students (39, 40). However, in another rural study (Handan), there was no significant association between daily near work and presence of myopia even adjusted with potential confounders (22). Interestingly, significant association between parental refractive error and myopia was found in rural participants rather than urban individuals. Further, myopia was associated with senior high parental education among our rural participants which was consistent with Yangxi County eye study (24). In addition, increasing age and longer daily hours of near-work were protective factors for hyperopia in both rural and urban students. Moreover, the prevalence rates of hyperopia for urban students were higher with lower annual household income which was consistent with study outcomes among adults in Sumatra, Indonesia (41). In both rural and urban children and adolescents, risk factors that were related to astigmatism were age and parental refractive error. Interestingly, female gender has lower risk for astigmatism among urban students and lower annual household income level has lower risk for astigmatism among rural ones. In study in Singaporean children (7–9 years), girls had significantly greater progression of astigmatism than did boys (42) which was inconsistent with our findings. Increasing age was an independent risk factor for anisometropia in both rural and urban participants. Protective factor, only in the rural arm, was lower annual household income level. These socio-demographic and lifestyle factors disparities may contribute to the prevalence disparities of REs between rural and urban students in this study.
A noteworthy finding is that the prevalence of REs including myopia was not significant with daily hours of outdoor activities in both urban and rural children and adolescents. In contrast, outdoor activities are negatively associated with myopia after adjustment for potential factors in both urban regions such as Hubei (43) and Qingdao (31)and rural settings e.g., Handan (22). Three cross section studies [mainland China (44), Taiwan (45) and Singapore (46)] did not find any relationship between outdoor activities and presence of myopia.
The major strength of this study included a comprehensive population-based sample from a large city, urban and rural areas; reasonable response rates; and reliable demographic data. This data are extremely useful for healthcare providers to develop long-term strategies to combat avoidable visual impairments due to REs. It is heartening to see a declining prevalence of REs as compared to epidemiological studies done in past worldwide. The study also found socio-demographic and health-related factors for REs between rural and urban students. It is possible that modulating this variable may control the occurrence of RE, however, this warrants longitudinal studies. A limitation of the study is the inability to validate the causal relationship between the significant risk factors and presence of REs. Cohort studies are recommended for the future. In addition, we excluded those participants with optical correction using othokeratology which may lower-evaluating the prevalence of myopia.
Conclusions
Our study investigated the overall prevalence of REs including myopia, hyperopia, astigmatism and anisometropia in rural and urban areas in Dalian China in children and adolescents aged 6–18 years. The students with urban habitation had a higher prevalence of myopia and anisometropia but a lower risk of hyperopia than those with rural habitation. With multivariate logistic regression, the factors regarding REs between rural and urban participants were different. Herein, the implementation and findings from this screen will guide the efficient prevention strategy of refractive error and eye care services in urban and rural school children and adolescents.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Dalian Third People's Hospital. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author contributions
LZhan, LL, XM, JW, and WL contributed to the conception of the study. YW, ZL, YQ, JW, YL, WL, YX, NZ, LJ, LW, JS, JY, and LZhao performed the experiment. YW, LL, XR, and LZhan contributed significantly to analysis and manuscript preparation. YW, LL, and XR performed the data analyses and wrote the manuscript. LZhan, LL, and XM helped perform the analysis with constructive discussions. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by Dalian Health Commission Department; Ministry of Education of Dalian. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.917781/full#supplementary-material
References
1. Morgan IG, He M, Rose KA. Epidemic of pathologic myopia: what can laboratory studies and epidemiology tell us? Retina. (2017) 37:989–97. doi: 10.1097/IAE.0000000000001272
2. Wong Y-L, Saw S-MJT. Epidemiology of pathologic myopia in Asia and worldwide. Asia Pac J Ophthalmol. (2016) 5:394–402. doi: 10.1097/APO.0000000000000234
3. Ramamurthy D, Lin Chua SY, Saw SMJC, Optometry E. A review of environmental risk factors for myopia during early life, childhood and adolescence. Clin Exp Optom. (2015) 98:497–506. doi: 10.1111/cxo.12346
4. Wu H-M, Seet B, Yap EP-H, Saw S-M, Lim T-H, Chia K-S. Does education explain ethnic differences in myopia prevalence? A population-based study of young adult males in Singapore. Optom Vis Sci. (2001) 78:234–9. doi: 10.1097/00006324-200104000-00012
5. Zadnik KJO, Science V. Myopia development in childhood. Optom Vis Sci. (1997) 74:603–8. doi: 10.1097/00006324-199708000-00021
6. Ip JM, Huynh SC, Robaei D, Kifley A, Rose KA, Morgan I, et al. Ethnic differences in refraction and ocular biometry in a population-based sample of 11–15-year-old Australian children. Eye. (2008) 22:649–56. doi: 10.1038/sj.eye.6702701
7. Ezegwui I, Oguego N, Okoye O, Maduka-Okafor F, Udeh N, Aghaji A, et al. Prevalence of refractive errors and visual impairment in school children in Enugu South-East Nigeria. Niger J Clin Pract. (2021) 24:380. doi: 10.4103/njcp.njcp_521_19
8. Quek TP, Chua CG, Chong CS, Chong JH, Hey HW, Lee J, et al. Prevalence of refractive errors in teenage high school students in Singapore. Ophthalmic Physiol Opt. (2004) 24:47–55. doi: 10.1046/j.1475-1313.2003.00166.x
9. Lin LL-K, Shih Y-F, Hsiao CK, Chen C. Prevalence of myopia in Taiwanese schoolchildren: 1983 to 2000. Ann Acad Med Singapore. (2004) 33:27–33.
10. Pan CW, Ramamurthy D, Saw SMJO, Optics P. Worldwide prevalence and risk factors for myopia. Ophthalmic Physiol Opt. (2012) 32:3–16. doi: 10.1111/j.1475-1313.2011.00884.x
11. Saw S, Gazzard G, Eong KA, Tan D. Myopia: attempts to arrest progression. Br J Ophthalmol. (2002) 86:1306–11. doi: 10.1136/bjo.86.11.1306
12. Saw S-M, Javier Nieto F, Katz J, Schein OD, Levy B, Chew S-J. Familial clustering and myopia progression in Singapore school children. Ophthalmic Epidemiol. (2001) 8:227–36. doi: 10.1076/opep.8.4.227.1609
13. Morgan I, Rose K. How genetic is school myopia? Prog Retin Eye Res. (2005) 24:1–38. doi: 10.1016/j.preteyeres.2004.06.004
14. Guggenheim JA, Northstone K, McMahon G, Ness AR, Deere K, Mattocks C, et al. Time outdoors and physical activity as predictors of incident myopia in childhood: a prospective cohort study. Invest Ophthalmol Vis Sci. (2012) 53:2856–65. doi: 10.1167/iovs.11-9091
15. French AN, Morgan IG, Mitchell P, Rose KA. Risk factors for incident myopia in Australian schoolchildren: the Sydney adolescent vascular and eye study. Ophthalmology. (2013) 120:2100–8. doi: 10.1016/j.ophtha.2013.02.035
16. Rudnicka AR, Kapetanakis VV, Wathern AK, Logan NS, Gilmartin B, Whincup PH, et al. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: implications for aetiology and early prevention. Br J Ophthalmol. (2016) 100:882–90. doi: 10.1136/bjophthalmol-2015-307724
17. You QS, Wu LJ, Duan JL, Luo YX, Liu LJ, Li X, et al. Prevalence of myopia in school children in greater Beijing: the Beijing childhood eye study. Acta Ophthalmol. (2014) 92:e398–406. doi: 10.1111/aos.12299
18. You QS, Wu LJ, Duan JL, Luo YX, Liu LJ, Li X, et al. Factors associated with myopia in school children in China: the Beijing childhood eye study. PLoS ONE. (2012) 7:e52668. doi: 10.1371/journal.pone.0052668
19. Wu JF, Bi HS, Wang SM, Hu YY, Wu H, Sun W, et al. Refractive error, visual acuity and causes of vision loss in children in Shandong, China. The Shandong Children Eye Study. PLoS ONE. (2013) 8:e82763. doi: 10.1371/journal.pone.0082763
20. Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. (2016) 123:1036–42. doi: 10.1016/j.ophtha.2016.01.006
21. He M, Zeng J, Liu Y, Xu J, Pokharel GP, Ellwein LB, et al. Refractive error and visual impairment in urban children in southern China. Invest Ophthalmol Vis Sci. (2004) 45:793–9. doi: 10.1167/iovs.03-1051
22. Lin Z, Gao TY, Vasudevan B, Ciuffreda KJ, Liang YB, Jhanji V, et al. Near work, outdoor activity, and myopia in children in rural China: the Handan offspring myopia study. Br J Ophthalmol. (2017) 17:1–8. doi: 10.1186/s12886-017-0598-9
23. Wu X, Gao G, Jin J, Hua W, Tao L, Xu S, Tao F. Housing type and myopia: the mediating role of parental myopia. BMC Ophthalmol. (2016) 16:151. doi: 10.1186/s12886-016-0324-z
24. He M, Huang W, Zheng Y, Huang L, Ellwein LB. Refractive error and visual impairment in school children in rural southern China. Ophthalmology. (2007) 114:374–82. doi: 10.1016/j.ophtha.2006.08.020
25. Pan C-W, Wu R-K, Li J, Zhong H. Low prevalence of myopia among school children in rural China. BMC Ophthalmol. (2018) 18:140. doi: 10.1186/s12886-018-0808-0
26. Congdon N, Wang Y, Song Y, Choi K, Zhang M, Zhou Z, et al. Visual disability, visual function, and myopia among rural Chinese secondary school children: the Xichang Pediatric Refractive Error Study (X-PRES)—report 1. Invest Ophthalmol Vis Sci. (2008) 49:2888–94. doi: 10.1167/iovs.07-1160
27. Guo K, Wang Y, Yang XR, Jing XX, Guo YY, Zhu D, et al. Prevalence of myopia in schoolchildren in Ejina: the Gobi Desert children eye study. Invest Ophthalmol Vis Sci. (2015) 56:1769–74. doi: 10.1167/iovs.14-15737
28. Li S-M, Liu L-R, Li S-Y, Ji Y-Z, Fu J, Wang Y, et al. Design, methodology and baseline data of a school-based cohort study in Central China: the Anyang Childhood Eye Study. Ophthalmic Epidemiol. (2013) 20:348–59. doi: 10.3109/09286586.2013.842596
29. Li Z, Xu K, Wu S, Lv J, Jin D, Song Z, et al. Population-based survey of refractive error among school-aged children in rural northern China: the Heilongjiang eye study. Clin Exp Ophthalmol. (2014) 42:379–84. doi: 10.1111/ceo.12198
30. Chen M, Wu A, Zhang L, Wang W, Chen X, Yu X, et al. The increasing prevalence of myopia and high myopia among high school students in Fenghua city, eastern China: a 15-year population-based survey. BMC Ophthalmol. (2018) 18:159. doi: 10.1186/s12886-018-0829-8
31. Sun JT, An M, Yan XB, Li GH, Wang DB. Prevalence and related factors for myopia in school-aged children in Qingdao. J Ophthalmol. (2018) 2018:9781987. doi: 10.1155/2018/9781987
32. Guo Y, Duan JL, Liu LJ, Sun Y, Tang P, Lv YY, et al. High myopia in greater Beijing school children in 2016. PLoS ONE. (2017) 12:e0187396. doi: 10.1371/journal.pone.0187396
33. Ma Y, Qu X, Zhu X, Xu X, Zhu J, Sankaridurg P, et al. Age-specific prevalence of visual impairment and refractive error in children aged 3–10 years in Shanghai, China. Invest Ophthalmol Vis Sci. (2016) 57:6188–96. doi: 10.1167/iovs.16-20243
34. Guo L, Yang J, Mai J, Du X, Guo Y, Li P, et al. Prevalence and associated factors of myopia among primary and middle school-aged students: a school-based study in Guangzhou. Eye. (2016) 30:796–804. doi: 10.1038/eye.2016.39
35. Lyu Y, Zhang H, Gong Y, Wang D, Chen T, Guo X, et al. Prevalence of and factors associated with myopia in primary school students in the Chaoyang District of Beijing, China. Jpn J Ophthalmol. (2015) 59:421–9. doi: 10.1007/s10384-015-0409-x
36. Wu LJ, You QS, Duan JL, Luo YX, Liu LJ, Li X, et al. Prevalence and associated factors of myopia in high-school students in Beijing. PLoS ONE. (2015) 10:e0120764. doi: 10.1371/journal.pone.0120764
37. Pi L-H, Chen L, Liu Q, Ke N, Fang J, Zhang S, et al. Refractive status and prevalence of refractive errors in suburban school-age children. Int J Med Sci. (2010):342–53. doi: 10.7150/ijms.7.342
38. Fotouhi A, Hashemi H, Khabazkhoob M, Mohammad K. The prevalence of refractive errors among schoolchildren in Dezful, Iran. Ophthalmology. (2007) 91:287–92. doi: 10.1136/bjo.2006.099937
39. Guo Y, Liu LJ, Xu L, Lv YY, Tang P, Feng Y, et al. Outdoor activity and myopia among primary students in rural and urban regions of Beijing. PLoS ONE. (2013) 120:277–83. doi: 10.1016/j.ophtha.2012.07.086
40. Guo Y, Liu LJ, Xu L, Tang P, Lv YY, Feng Y, et al. Myopic shift and outdoor activity among primary school children: one-year follow-up study in Beijing. BMC Ophthalmol. (2013) 8:e75260. doi: 10.1371/journal.pone.0075260
41. Saw S-M, Gazzard G, Koh D, Farook M, Widjaja D, Lee J, et al. Prevalence rates of refractive errors in Sumatra, Indonesia. Invest Ophthalmol Vis Sci. (2002) 43:3174–80.
42. Tong L, Saw S-M, Lin Y, Chia K-S, Koh D, Tan DJIo, et al. Incidence and progression of astigmatism in Singaporean children. Invest Ophthalmol Vis Sci. (2004) 45:3914–8. doi: 10.1167/iovs.04-0492
43. Zeng C, Zhou L, Zhang P, Wang J, Ye M, Yi B, et al. The epidemiology of myopia in primary school students of grade 1 to 3 in Hubei province. Zhonghua Yan Ke Za Zhi. (2018) 54:756–61. doi: 10.3760/cma.j.issn.0412-4081.2018.10.007
44. Zhang M, Li L, Chen L, Lee J, Wu J, Yang A, et al. Population density and refractive error among Chinese children. Invest Ophthalmol Vis Sci. (2010) 51:4969–76. doi: 10.1167/iovs.10-5424
45. Cheng C-Y, Huang W, Su K-C, Peng M-L, Sun H-Y, Cheng H-MJO, et al. Myopization factors affecting urban elementary school students in Taiwan. Optom Vis Sci. (2013) 90:400–6. doi: 10.1097/OPX.0b013e3182873449
Keywords: prevalence, refractive errors, risk factors, schoolchildren, urban-rural disparity
Citation: Wang Y, Liu L, Lu Z, Qu Y, Ren X, Wang J, Lu Y, Liang W, Xin Y, Zhang N, Jin L, Wang L, Song J, Yu J, Zhao L, Ma X and Zhang L (2022) Rural-urban differences in prevalence of and risk factors for refractive errors among school children and adolescents aged 6–18 years in Dalian, China. Front. Public Health 10:917781. doi: 10.3389/fpubh.2022.917781
Received: 11 April 2022; Accepted: 08 August 2022;
Published: 29 August 2022.
Edited by:
Radwan Qasrawi, Al-Quds University, PalestineReviewed by:
Diala Abu Al-Halawa, Al-Quds University, PalestineMaysaa Nemer, Birzeit University, Palestine
Copyright © 2022 Wang, Liu, Lu, Qu, Ren, Wang, Lu, Liang, Xin, Zhang, Jin, Wang, Song, Yu, Zhao, Ma and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lijun Zhang, bGlqdW56aGFuZ3dAc2luYS5jb20=; Lei Liu, bGl1bGVpamlhb0AxNjMuY29t; Xiang Ma, eG1hOTQ2N0B2aXAuc2luYS5jb20=
†These authors have contributed equally to this work and share first authorship
 Yachen Wang1,2†
Yachen Wang1,2† Lei Liu
Lei Liu Lijun Zhang
Lijun Zhang