- 1Geriatric Diseases Institute of Chengdu/Cancer Prevention and Treatment Institute of Chengdu, Department of Anesthesiology, Chengdu Fifth People's Hospital (The Second Clinical Medical College, Affiliated Fifth People's Hospital of Chengdu University of Traditional Chinese Medicine), Chengdu, China
- 2Department of Anesthesiology, The Second Affiliated Hospital of Kunming Medical University, Kunming, China
- 3Department of Anesthesiology, The Second Affiliated Hospital of Chongqing Medical University, Chongqing, China
Background: Postoperative pneumonia is a preventable complication associated with adverse outcomes, that greatly aggravates the medical expenses of patients. The goal of our study is to identify risk factors and outcomes of postoperative pneumonia.
Methods: A matched 1:1 case-control study, including adult patients who underwent surgery between January 2020 and June 2020, was conducted in the Second Affiliated Hospital of Kunming Medical University in China. Cases included all patients developing postoperative pneumonia within 30 days after surgery, defined using consensus criteria. Controls were selected randomly from the matched eligible population.
Results: Out of 17,190 surgical patients, 264 (1.54%) experienced postoperative pneumonia. Increased age, chronic obstructive pulmonary disease, emergency surgery, postoperative reduced albumin, prolonged ventilation, and longer duration of bed rest were identified as significant risk factors independently associated with postoperative pneumonia. Regarding prognostic implications, postoperative pneumonia was associated with longer length of hospital stay, higher ICU occupancy rate, higher unplanned re-operation rate, and higher in-hospital mortality rate. Postoperative pneumonia was most commonly caused by Gram-negative pathogens, and multidrug resistant bacteria accounted for approximately 16.99% of cases.
Conclusions: Postoperative pneumonia is associated with severe clinical outcomes. We identified six independent risk factors that can aid in risk stratification and management of patients at risk of postoperative pneumonia, and the distribution of causative pathogens can also help in the implementation of effective interventions.
Clinical Trial Registration: www.chictr.org.cn, identifier: chiCTR2100045986.
Background
Every year, more than 300 million patients worldwide undergo surgery (1). Estimates of procedure-related mortality in surgical patients range from 1 to 4%, of which more than one-fifth are due to perioperative complications, with an incidence ranging from 3 to 16% (1, 2). Studies have shown (3) that almost half of perioperative complications can be effectively prevented, and the current incidence of permanent disability or death caused by these complications still accounts for 0.4% to 0.8%. Even with timely treatment, related complications will still reduce the long-term survival time of surgical patients.
Postoperative pneumonia (POP) is one most common complication of these and it is defined as hospital-acquired pneumonia or ventilator-associated pneumonia in post-surgical patients. Currently, postoperative pneumonia has the highest incidence of hospital-acquired pneumonia in the world, accounting for approximately 50% of all nosocomial pneumonias, with an incidence of 1.5 to 15.8% (4–7). Postoperative pneumonia can adversely affect the outcomes of surgical patients and may even threaten their lives. Mortality related to postoperative pneumonia among surgical patients has been reported to range from 20 to 50%, and the mortality rate varies by the type of surgery (8). Studies have shown that the fatality rate caused by postoperative pneumonia can be up to 9–50%, and even after risk adjustment, the patients' 5-year survival rate after surgery is reduced by 66% (9). Among the remaining survivors, there is also evidence that postoperative pneumonia adversely affects the patients' early postoperative recovery and late quality of life. In addition, postoperative pneumonia can significantly prolong the hospital stay of surgical patients and significantly increase their postoperative ICU occupancy rate, readmission rate, reoperation rate and mortality rate (8, 9), which greatly aggravate the burden of medical expenses of patients and leads to an average increase by approximately 2–10 times of additional medical expenses (5, 9).
Therefore, it is obviously worthwhile to identify the perioperative risk factors for postoperative pneumonia and investigate the distribution of causative bacteria. The result would suggest the measures for risk reduction through action on modifiable factors, or increase vigilance in the presence of non–modifiable conditions. The result of causative bacteria could also aid in selection of antibiotics for post-infection treatment especially considered against the worldwide escalation of infection caused by multidrug resistant microorganisms. Our primary aim was to identify perioperative risk factors and outcomes of postoperative pneumonia. Our secondary aim was to investigate the distribution of causative bacteria and surgical specialty.
Methods
Study Design and Participants
This study protocol was approved by the Institutional Ethics Committee of the Second Affiliated Hospital of Kunming Medical University (Kunming, China, approval number: PJ-2021-39). Informed consent was waived due to the retrospective design of the study. The study was registered in the Chinese Clinical Trial Registry (Clinical Trials identifier: ChiCTR2100045986). This study is a single-center retrospective 1:1 case-control study. From the hospital's complete electronic medical record “Donghua”, a total of 17,190 patients who underwent surgery from January 1, 2020 to June 31, 2020 were included. The case group included all adult patients who followed for hospital acquired pneumonia (HAP) occurrence for 30 days after surgery. Controls were matched by surgical specialty and randomly selected at 1:1 from the remaining surgical patients without pneumonia. Exclusion criteria were age under 18 years, procedures outside an operating room, patients already intubated, procedures related to postoperative complications of previous surgery, outpatient procedures (hospital stay <24 h), patient's medical records missing or inadequate.
Diagnosis of Pneumonia
The US Centers for Disease Control definition of pneumonia was used (7). Two or more serial chest radiographs with at least one of the following (one radiograph is sufficient for patients with no underlying pulmonary or cardiac disease): (i) New or progressive and persistent infiltrates, (ii) consolidation, (iii) cavitation; and at least one of the following: (a) fever (>38°C) with no other recognized cause, (b) leucopenia (white cell count < 4 × 109 liter−1) or leukocytosis (white cell count > 12 × 109 liter−1), (c) for adults > 70 years old, altered mental status with no other recognized cause; and at least two of the following: (a) new onset of purulent sputum or a change in character of the sputum, or increased respiratory secretions, or increased suctioning requirements, (b) new onset or worsening cough, or dyspnea, or tachypnea, (c) rales or bronchial breath sounds, (d) worsening gas exchange (hypoxemia, increased oxygen requirement, increased ventilator demand).
Data Collection
Perioperative data were collected retrospectively. Demographic factors, including age, sex, weight, height, body mass index (BMI) and factors assessing general condition [such as the Glasgow Coma Scale (GCS) and American Society of Anesthesiologists (ASA) classification], were recorded. Patients' past medical history, including smoking, drinking, hypertension, diabetes, malignancy, stroke, chronic obstructive pulmonary disease (COPD), coronary heart disease, liver disease and renal dysfunction was assessed. Laboratory measurements were reviewed as last values before operation or first values after operation, such as albumin, hemoglobin (Hb), blood urea nitrogen and creatinine levels. Factors associated with surgery, including surgical specialty, duration of surgery, type of surgery (scheduled or emergency), surgery period (day or night), were also evaluated. Intraoperative variables, including blood loss, red blood cells (RBC) transfusions, human albumin infusion, amount of liquid input and invasive procedure (such as radial artery cannulation, deep vein catheterization and gastric tube intubation) were recorded. Additionally, perioperative factors pertaining to the respiratory system, such as the duration of mechanical ventilation (duration until tracheal extubation) and duration of bed rest (duration until patients' first off-bed activity) were also evaluated. Causative bacteria and Multi-drug-resistance (MDR, defined as non-susceptibility to at least one agent in three or more antimicrobial categories) were recorded. To assess the prognostic implications of postoperative pneumonia, length of hospital stay, admission to the intensive care unit (ICU) and in-hospital mortality rates were reviewed.
Statistical Analysis
In this study, the mean and standard deviation (x ± s) were used to represent the measurement data conforming to a normal distribution and a homogenous variance, and the independent sample t-test was used for comparisons between the case group and the control group. The median (interquartile range) was used to represent the measurement data with a non–normal distribution, and the two groups were compared by the rank-sum test. All enumeration data were represented by frequency and percentage, and the two groups were compared by X2 test. All statistically significant factors on univariate analysis were selected for inclusion in the multivariate regression analysis conducted by a binary logistic regression analysis model. Bivariate odds ratios (OR) and 95% confidence intervals (CI) were also estimated. P < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS software (version 24, SPSS Inc., United States).
Results
Patient Characteristics
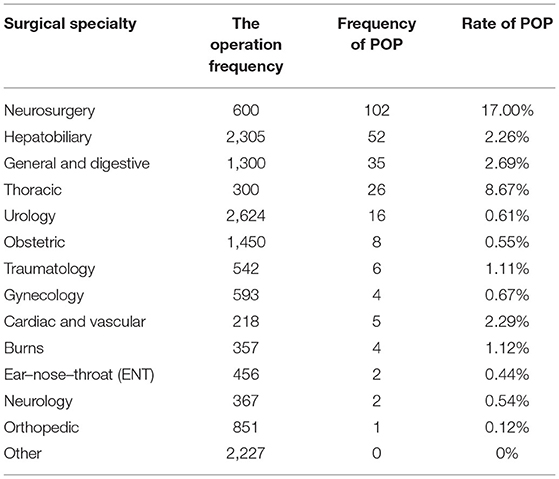
A total of 17,190 surgical patients were selected for the study, of which 264 patients were diagnosed with postoperative pneumonia. Overall, the incidence of postoperative pneumonia was 1.54% (264/17,190). Table 1 summarizes the operative frequency and the incidence of postoperative pneumonia in each surgical specialty. Among patients undergoing neurosurgery, the frequency (102/600) and incidence (17.00%) of postoperative pneumonia were much higher than the others, followed by the thoracic (8.67%), general and digestive (2.69%), cardiac and vascular (2.29%), and hepatobiliary (2.26%). The postoperative pneumonia rates of these five surgical specialty all exceeded 2%.
Causative Pathogens
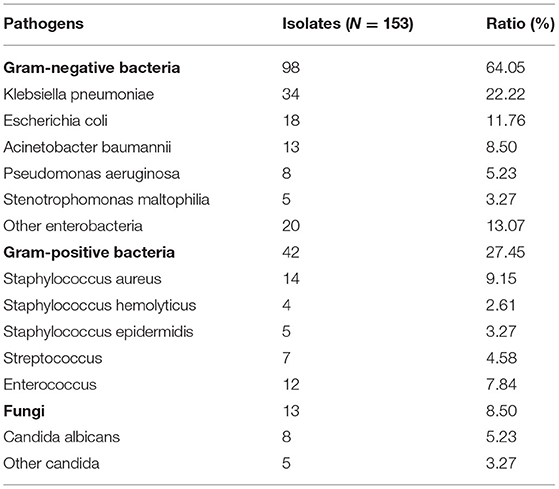
The distribution of pathogenic bacteria is shown in Table 2. A total of 153 different strains of pathogens were isolated from the sputum specimens of patients with postoperative pneumonia by coculture. Among which 98 isolates (64.05%) were Gram-negative bacteria, 42 isolates (27.45%) were Gram-positive bacteria, and 13 isolates (8.50%) were fungi. The main pathogens were Klebsiella pneumoniae (22.22%, 34/153), followed by Escherichia coli (11.76%, 18/153), Staphylococcus aureus (9.15%, 14/153) and Acinetobacter baumannii (8.50%, 13/153). In addition, the results showed that a total of 26 isolates (16.99%) were multidrug resistant bacteria, of which 13 isolates (50%) were carbapenem-resistant Enterobacteriaceae, 8 isolates (30.77%) were carbapenem-resistant Acinetobacter baumannii, 3 isolates (11.54%) were methicillin-resistant Staphylococcus aureus, and 2 isolates (7.69%) were carbapenem-resistant Pseudomonas aeruginosa. We found that 73.08% (19/26) of the multidrug-resistant bacteria were isolated from neurosurgery patients.
Univariate Analysis
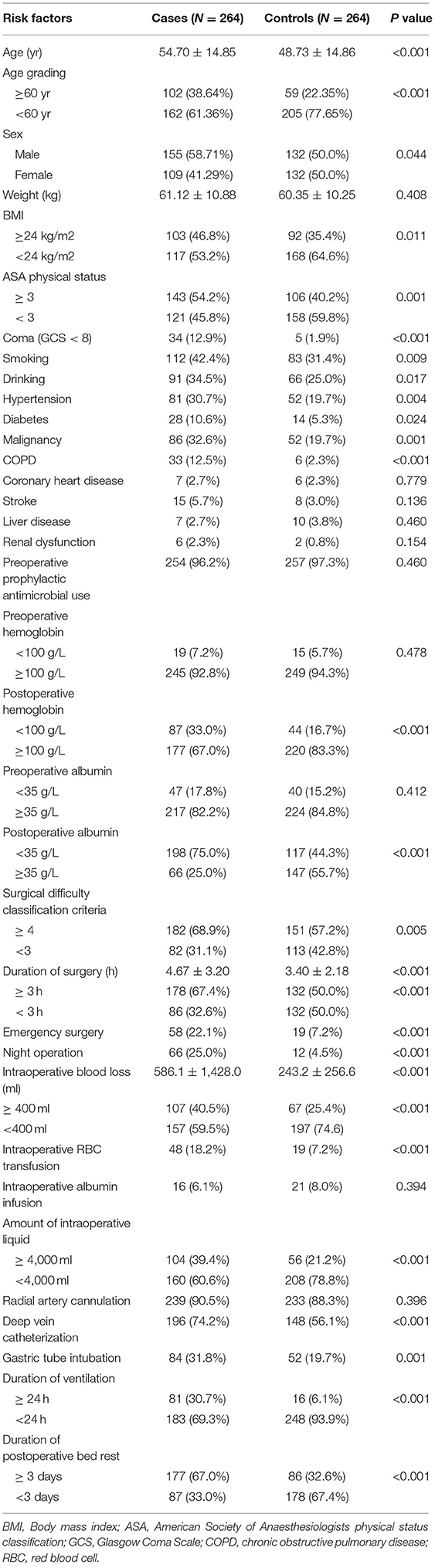
Significant risk factors associated with postoperative pneumonia on univariate analysis are presented in Table 3. We found 25 perioperative risk factors that were significantly associated with postoperative pneumonia (P < 0.05), as follows: age, sex, BMI, smoking, drinking, hypertension, diabetes, malignancy, COPD, coma (GCS < 8), Surgical difficulty classification criteria, duration of surgery, emergency surgery, night operation, intraoperative blood loss, ASA physical status, duration of ventilation, deep vein catheterization, gastric tube intubation, amount of intraoperative liquid input, intraoperative RBC transfusion, postoperative hemoglobin level, postoperative albumin level and duration of postoperative bed rest.
Multivariate Regression Analysis
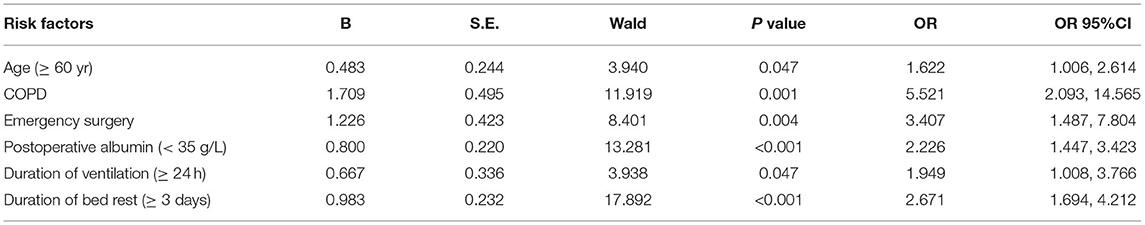
To further identify the independent risk factors for postoperative pneumonia, multivariate logistic regression analysis was performed using the 25 factors significantly associated with postoperative pneumonia in the univariate analysis. The results of the multivariate analysis are presented in Table 4. We found that there were six independent risk factors for postoperative pulmonary disease, as follows: increased age (P = 0.047, OR = 1.622, 95% CI: 1.006–2.614), COPD (P = 0.001, OR = 5.521, 95% CI: 2.093–14.565), emergency surgery (P = 0.004, OR = 3.407, 95% CI: 1.487–7.804), postoperative reduced albumin (P < 0.001, OR = 2.226, 95% CI: 1.447–3.423), prolonged mechanical ventilation (P = 0.047, OR = 1.949, 95% CI: 1.008–3.766), and longer duration of bed rest (P < 0.001, OR = 2.671, 95% CI: 1.694–4.212).
Outcomes
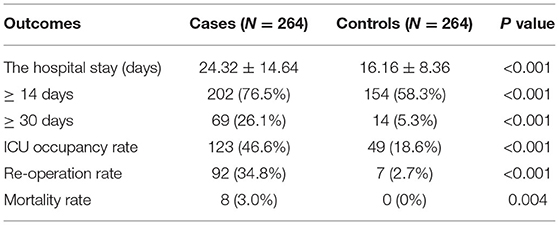
The outcomes of the patients with postoperative pneumonia were retrospectively analyzed and are presented in Table 5. The results show that the hospital stay of patients in the case group (24.32 ± 14.64) was significantly longer than that in the control group (16.16 ± 8.36). In the case group, the proportion of patients with hospital stays over 14 days or 30 days were significantly higher than those in the control group (P < 0.05). In addition, the postoperative ICU occupancy rate, re-operation rate and postoperative mortality rate of patients in the case group were significantly higher than those in the control group (P < 0.05).
Discussion
Among the 17,190 surgical patients included in this study, 264 cases of postoperative pneumonia occurred, with an incidence of 1.54%, which is similar to previously reported rates (5–7, 10). The incidence of postoperative pneumonia in neurosurgery (17.00%) was significantly higher than that in other surgical specialties. Obviously, neurosurgery patients are susceptible to pneumonia after surgery. Such patients usually suffer from complicated diseases and long coma, impairing their respiratory and immune function. In addition, the neurosurgery (102 cases), hepatobiliary (52 cases), general and digestive (35 cases), and thoracic (26 cases) were the four surgical specialties with the highest frequency of postoperative pneumonia, accounting for approximately 81.44% of the total. This suggests that it is particularly important to strengthen the management of patients at risk of postoperative pneumonia in these four surgical specialties.
The main pathogens were Klebsiella pneumoniae (22.22%), followed by Escherichia coli (11.76%), Staphylococcus aureus (9.15%) and Acinetobacter baumann (8.50%), accounting for half of the total pathogens. These four pathogens are conditional pathogenic bacteria that usually exist in the hospital environment and oropharynx of patients. Obviously, surgical trauma destroys the integrity of the body's skin and tissues, damaging the patient's first line of immune defense and providing opportunities for these bacterial infections. Meanwhile, Staphylococcus aureus can be transmitted by hand contact, indicating the need for strict hand hygiene prior to invasive procedures such as tracheal intubation. The drug resistance of pathogens has also become a serious problem, which makes clinical treatment more difficult. In this study, the incidence of multidrug-resistant bacteria was approximately 16.99%, of which 73.08% occurred in neurosurgery patients.
This study has demonstrated that age over 60 years old is an independent risk factor for postoperative pneumonia, which is consistent with previous research (11–13). Kunisaki C et al. (11) reported a significant variation in the postoperative pneumonia rate between patients aged over 75 years and those aged 45–65 years (13.3% and 6.3%). Furthermore, Yamada H et al. (12) reported that the postoperative pneumonia incidence in patients aged over 85 years was significantly higher than that in patients aged 75 to 85 years (16.7% and 3.3%). These two studies showed that the risk of postoperative pneumonia increased significantly with patient age, which was also confirmed by Miki Y et al. (13).
Our study found that the incidence of postoperative pneumonia in patients with COPD was 4.5 times greater than that in unaffected patients (P = 0.001, OR = 5.521, 95% CI: 2.093–14.565). Pulmonary chronic inflammation in patients with COPD is a characteristic pathological change that will continue to destroy the alveolar wall septum and result in pulmonary interstitial fibrosis (9, 14). Some previous studies have confirmed that preoperative treatment for COPD can reduce the incidence of postoperative pneumonia (15, 16). Numata T et al. (15) have demonstrated that long-acting anticholinergic drugs and long-acting β2 receptor agonists can effectively reduce the rate of postoperative pulmonary complications in patients with COPD. Du Z et al. (16) have further demonstrated that perioperative aerosol inhalation of ipratropium bromide can reduce the incidence of postoperative pneumonia in COPD patients undergoing thoracic surgery.
We also found that the rate of postoperative pneumonia in emergency surgery patients was 2.4 times greater than that in non–emergency surgery patients (P = 0.004, OR = 3.407, 95% CI: 1.487–7.804), which is similar to the results reported by Kim Th et al. (17). Due to the urgency of the surgery, the preoperative preparations appear to be particularly poor, and the prevention of infection is usually not strict enough. Furthermore, McCoy CC et al. (18) reported that compared with elective surgery, emergency surgery was associated with an increased risk of serious postoperative complications and increased the risk of postoperative death by approximately 1.39 times.
The serum albumin level is the most common indicator used to evaluate the nutritional status of patients. A serum albumin level below 35 g/L is generally considered malnutrition and has been identified as a potential risk factor for poor postoperative outcomes (19, 20). Our findings suggest that postoperative albumin levels under 35 g/L in surgical patients is an independent risk factor for postoperative pneumonia. A decrease in postoperative albumin can directly reflect that the metabolism of the body is in a negative nitrogen balance and engaged in high protein consumption. The results of univariate analysis in our study showed that intraoperative albumin infusion did not increase the risk of postoperative pneumonia, indicating that a timely albumin infusion can be applied to correct hypoalbuminemia if necessary.
Our study demonstrated that the duration of mechanical ventilation over 24 h was an independent risk factor for postoperative pneumonia (P = 0.047, OR = 1.949, 95% CI: 1.008–3.766). For patients sent to the ICU after surgery, the duration of ventilation usually exceeds 24 h. Thus, extubation timely after surgery can significantly reduce the incidence of postoperative pneumonia. Vera Urquiza R et al. (21) found that extubation 6 h later was an independent risk factor for postoperative pneumonia (P = 0.005, OR: 15.81, 95% CI: 2.2–110.7). Savardekar A et al. (22) confirmed that endotracheal intubation for more than 48 h was an independent risk factor for pneumonia (P = 0.041, OR = 6.638, 95% CI: 1.08–40.8).
Duration of bed rest after surgery over 3 days was an independent risk factor for postoperative pneumonia (P < 0.001, OR = 2.671, 95% CI: 1.694–4.212).
Therefore, patients ought to start off-bed activity early after surgery if there is no special contraindication. When it is necessary to stay in bed for a long time, the patient should be encouraged to expectorate regularly and clear their airway secretions. Cassidy MR et al. (23) implemented a multidisciplinary team cooperation model, proving that early out of bed after surgery can effectively reduce the occurrence of postoperative pneumonia.
Furthermore, we found that postoperative pneumonia usually caused poor outcomes. The hospital stay of cases (24.32 ± 14.64) was significantly longer than that of the matched controls (16.16 ± 8.36), and postoperative pneumonia significantly increased the ICU occupancy rate, reoperation rate, and perioperative mortality rate. A retrospective analysis of 1,415 consecutive gastric cancer patients reported that postoperative pneumonia was associated with poor long-term outcomes (24). Fujishima S et al. (25) found that postoperative pneumonia in patients with esophageal cancer was associated with skeletal muscle consumption and asymptomatic pneumonia within 6 months after surgery, and the survival time of patients with postoperative pneumonia was significantly lower than that of patients without pneumonia. Obviously, the real value of study is in improving quality of life (26).
A formal statement of shortcomings could keep authors and the public from overstating a study's claims (27). As a single-center study, the external validity of the findings is limited. Due to the retrospective collection of most clinical data, information on the exposures is subject to observation bias. Specifically, although our diagnostic criteria are very specific, our researchers may still make diagnostic errors, even in the same patient. In addition, the rate of postoperative pneumonia varied greatly in each surgical department, and the representation of patients included in the study is prone to bias. Many surgical patients receive prophylactic antibiotics, which tends to skew the study results and obscure the risk factors associated with postoperative pneumonia. Furthermore, this study did not follow up on the long-term outcomes of patients with postoperative pneumonia.
Conclusions
Postoperative pneumonia is associated with severe clinical outcomes. In this retrospective single-center study, we identified six independent risk factors that can aid in risk stratification and management of patients at risk of postoperative pneumonia. The distribution of causative pathogens can also help in the implementation of effective preventions and interventions, which has great implications for the formulation of infection control policies.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
BX collected, analyzed and interpreted all data, and was a major contributor in writing the manuscript. YS participated in study design and data analysis. FY was involved in data acquisition and analysis. RC was involved in data acquisition and manuscript writing. YY conducted statistics and analysis of data. SJ guided paper writing and provided financial and technical support. All authors read and approved the final submitted manuscript. All authors contributed to the article and approved the submitted version.
Funding
Project supported by the Applied Basic Research Foundation of Yunnan Province (CN) (2014FZ027). The funder was not involved in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors wish to thank the members of staff from the infection control department and records management department at the hospital for helping us carry out this investigation.
Abbreviations
POP, postoperative pneumonia; HAP, hospital acquired pneumonia; BMI, body mass index; GCS, Glasgow Coma Scale; ASA, American Society of Anesthesiologists; COPD, chronic obstructive pulmonary disease; Hb, hemoglobin; RBC, red blood cells; MDR, Multi-drug-resistance; ICU, Intensive Care Unit; OR, odds ratio; CI, confidence interval.
References
1. Abbott TEF, Fowler AJ, Dobbs TD, Harrison EM, Gillies MA, Pearse RM. Frequency of surgical treatment and related hospital procedures in the UK: a national ecological study using hospital episode statistics. Br J Anaesth. (2017) 119:249–57. doi: 10.1093/bja/aex137
2. Weiser TG, Regenbogen SE, Thompson KD, Haynes AB, Lipsitz SR, Berry WR, et al. An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet. (2008) 372:139–44. doi: 10.1016/S0140-6736(08)60878-8
3. Boehm O, Baumgarten G, Hoeft A. Epidemiology of the high-risk population: perioperative risk and mortality after surgery. Curr Opin Crit Care. (2015) 21:322–7. doi: 10.1097/MCC.0000000000000221
4. Murff HJ, FitzHenry F, Matheny ME, Gentry N, Kotter KL, Crimin K, et al. Automated identification of postoperative complications within an electronic medical record using natural language processing. JAMA. (2011) 306:848–55. doi: 10.1001/jama.2011.1204
5. Wakeam E, Hyder JA, Tsai TC, Lipsitz SR, Orgill DP, Finlayson SR. Complication timing and association with mortality in the American college of surgeons' national surg ical quality improvement program database. J Surg Res. (2015) 193:77–87. doi: 10.1016/j.jss.2014.08.025
6. Redelmeier DA, McAlister FA, Kandel CE, Lu H, Daneman N. Postoperative pneumonia in elderly patients receiving acid suppressants: a retrospective cohort analy sis. BMJ (Clin Res ed). (2010) 340:c2608. doi: 10.1136/bmj.c2608
7. Abbott TEF, Fowler AJ, Pelosi P, Gama de, Abreu M, Møller AM, Canet J, et al. A systematic review and consensus definitions for standardised end-points in perioperative medicine: pulmonary complications. Br J Anaesth. (2018) 120:1066–79. doi: 10.1016/j.bja.2018.02.007
8. Russotto V, Sabaté S, Canet J. Development of a prediction model for postoperative pneumonia: a multicentre prospective observational study. Eur J Anaesthesiol. (2019) 36:93–104. doi: 10.1097/EJA.0000000000000921
9. Sabaté S, Mazo V, Canet J. Predicting postoperative pulmonary complications: implications for outcomes and costs. Curr Opin anesthesiol. (2014) 27:201–9. doi: 10.1097/ACO.0000000000000045
10. Ackland GL, Iqbal S, Paredes LG, Toner A, Lyness C, Jenkins N, et al. Individualised oxygen delivery targeted haemodynamic therapy in high-risk surgical patients: a multicentre, randomised, double-blind, controlled, mechanistic trial. Lancet Respir Med. (2015) 3:33–41. doi: 10.1016/S2213-2600(14)70205-X
11. Kunisaki C, Akiyama H, Nomura M, Matsuda G, Otsuka Y, Ono HA, et al. Comparison of surgical outcomes of gastric cancer in elderly and middle-aged patients. Am J Surg. (2006) 191:216–24. doi: 10.1016/j.amjsurg.2005.09.001
12. Yamada H, Shinohara T, Takeshita M, Umesaki T, Fujimori Y, Yamagishi K. Postoperative complications in the oldest old gastric cancer patients. Int J Surg. (2013) 11:467–71. doi: 10.1016/j.ijsu.2013.04.005
13. Miki Y, Makuuchi R, Tokunaga M, Tanizawa Y, Bando E, Kawamura T, et al. Risk factors for postoperative pneumonia after gastrectomy for gastric cancer. Surg Today. (2016) 46:552–6. doi: 10.1007/s00595-015-1201-8
14. Sandberg J, Engström G, Ekström M. Breathlessness and incidence of COPD, cardiac events and all-cause mortality: a 44-year follow-up from middle age throughout life. PLoS ONE. (2019) 14:e0214083. doi: 10.1371/journal.pone.0214083
15. Numata T, Nakayama K, Fujii S, Yumino Y, Saito N, Yoshida M, et al. Risk factors of postoperative pulmonary complications in patients with asthma and COPD. BMC Pul Med. (2018) 18:4. doi: 10.1186/s12890-017-0570-8
16. Du Z, Huang X, Feng Y, Yan W, Xu D, Sun X, et al. Effects of ipratropium bromide on the occurrence of postoperative respiratory complications in craniectomy patients with COPD: a nationwide multicenter retrospective study. Medicine. (2020) 99:e20836. doi: 10.1097/MD.0000000000020836
17. Kim TH, Lee JS, Lee SW, Oh YM. Pulmonary complications after abdominal surgery in patients with mild-to-moderate chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. (2016) 11:2785–96. doi: 10.2147/COPD.S119372
18. McCoy CC, Englum BR, Keenan JE, Vaslef SN, Shapiro ML, Scarborough JE. Impact of specific postoperative complications on the outcomes of emergency general surgery patients. J Trauma Acute Care Surg. (2015) 78:912–8. doi: 10.1097/TA.0000000000000611
19. Baba H, Tokai R, Hirano K, Watanabe T, Shibuya K, Hashimoto I, et al. Risk factors for postoperative pneumonia after general and digestive surgery: a retrospective single-center study. Surg Today. (2020) 50:460–8. doi: 10.1007/s00595-019-01911-9
20. Bohl DD, Shen MR, Hannon CP, Fillingham YA, Darrith B, Della Valle CJ. Serum albumin predicts survival and postoperative course following surgery for geriatric hip fracture. J Bone Joint Surg Am. (2017) 99:2110–8. doi: 10.2106/JBJS.16.01620
21. Vera Urquiza R, Bucio Reta ER, Berríos Bárcenas EA, Choreño Machain T. Risk factors for the development of postoperative pneumonia after cardiac surgery. Arch Cardiol Mex. (2016) 86:203–7. doi: 10.1016/j.acmx.2015.12.005
22. Savardekar A, Gyurmey T, Agarwal R, Podder S, Mohindra S, Gupta SK, et al. Incidence, risk factors, and outcome of postoperative pneumonia after microsurgical clipping of ruptured intracranial aneurysms. Surg Neurol Int. (2013) 4:24. doi: 10.4103/2152-7806.107894
23. Cassidy MR, Rosenkranz P, McCabe K, Rosen JE, McAneny D, I COUGH. reducing postoperative pulmonary complications with a multidisciplinary patient care program. JAMA Surg. (2013) 148:740–5. doi: 10.1001/jamasurg.2013.358
24. Kiuchi J, Komatsu S, Ichikawa D, Kosuga T, Okamoto K, Konishi H, et al. Putative risk factors for postoperative pneumonia which affects poor prognosis in patients with gastric cancer. Int J Clin Oncol. (2016) 21:920–6. doi: 10.1007/s10147-016-0987-8
25. Fujishima S, Tsujimoto H, Nagata K, Sugasawa H, Nomura S, Ito N, et al. Postoperative pneumonia causes the loss of skeletal muscle volume and poor prognosis in patients undergoing esophagectomy for esophageal cancer. Gen Thorac Cardiovasc Surg. (2021) 69:84–90. doi: 10.1007/s11748-020-01482-4
26. Vuong QH. The (ir)rational consideration of the cost of science in transition economies. Nat Hum Behav. (2018) 2:5. doi: 10.1038/s41562-017-0281-4
Keywords: postoperative pneumonia, perioperative, risk factors, pathogen distribution, outcomes
Citation: Xiang B, Jiao S, Si Y, Yao Y, Yuan F and Chen R (2022) Risk Factors for Postoperative Pneumonia: A Case-Control Study. Front. Public Health 10:913897. doi: 10.3389/fpubh.2022.913897
Received: 06 April 2022; Accepted: 20 June 2022;
Published: 08 July 2022.
Edited by:
Xiaojiong Jia, Harvard Medical School, United StatesReviewed by:
Quan-Hoang Vuong, Phenikaa University, VietnamEirini Christaki, University of Ioannina, Greece
Copyright © 2022 Xiang, Jiao, Si, Yao, Yuan and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shulan Jiao, eW5rbWpzbDVAMTYzLmNvbQ==
 Bingbing Xiang1
Bingbing Xiang1 Shulan Jiao
Shulan Jiao Feng Yuan
Feng Yuan