- 1Key Laboratory of Shaanxi Province for Craniofacial Precision Medicine Research, College of Stomatology, Xi'an Jiaotong University, Xi'an, Shaanxi, China
- 2Chongqing Key Laboratory for Oral Diseases and Biomedical Sciences, College of Stomatology, Chongqing Medical University, Chongqing, China
- 3Department of Orthodontics, School of Stomatology, Xi'an Jiaotong University, Xi'an, Shaanxi, China
- 4Department of Breast Surgery, Peking Union Medical College Hospital (Xidan Campus), Beijing, China
- 5State Key Laboratory of Trauma, Burn and Combined Injury, Institute of Burn Research, Southwest Hospital, Third Military Medical University (Army Medical University), Chongqing, China
- 6Department of Plastic Surgery, State Key Laboratory of Trauma, Burns and Combined Injury, Southwest Hospital, Third Military Medical University (Army Medical University), Chongqing, China
- 7School of Nursing, Chongqing Medical University, Chongqing, China
- 8Department of Critical Care Medicine, Shanghai Jiao Tong University Affiliated Sixth People's Hospital, Shanghai, China
- 9Guangzhou Women and Children Medical Center, Guangzhou Medical University Affiliated Women and Children Medical Center, Guangzhou, China
- 10Department of Nursing, The First Affiliated Hospital of Chongqing Medical University, Chongqing, China
Objective: Excessive fear of progression can affect the mental health, social function, and wellbeing of patients with chronic diseases. This study investigated the fear of progression (FoP) and the socio-demographic and clinical predictors among patients with type 2 diabetes mellitus (T2DM).
Method: The present study is a multi-center cross-sectional study. Inpatients with T2DM were recruited by a multi-stage convenience sampling method from the department of endocrinology in 5 tertiary hospitals in Southwest China. 459 T2DM patients were consecutively enrolled. Socio-demographic, clinical data, and answers to the fear of progression questionnaire (FoP-Q) were collected.
Results: 385 patients with complete data were eligible. The average score of FoP-Q-SF was 26.84 and 23.1% of patients reached the dysfunctional fear of progression criterion. The greatest fears were worrying about “disease progression,” “the adverse reactions of medication,” and “relying on strangers for activities of daily living.” Health education (P < 0.001), age (P = 0.002), hypoglycemia history (P = 0.006), employment status (P = 0.025) and duration since being diagnosed with type 2 diabetes mellitus (P = 0.032) were the related factors of fear of progression.
Conclusion: Early assessment of the fear of progression was imperative to identify dysfunctional fear of progression in patients with type 2 diabetes mellitus. Meanwhile, the meaning of these predictors for strengthening healthcare professions education and patients self-management might help healthcare givers timely perform related interventions and help patients reduce their fear of progression thus actively cooperate with T2DM treatments.
Introduction
Diabetes mellitus is a global epidemic with ~463 million adults worldwide suffering from the disease (1). China is the country with the largest number of diabetic people in the world, and the prevalence of diabetes in China in 2019 was 10.9% (1). Type 2 diabetes mellitus (T2DM), as the most common type of diabetes, the incidence will increase with the aging population (1, 2).
T2DM patients face various threats. First is the complexity of the diabetes therapeutic schedule, which combines diet, exercise, medication, blood sugar testing, oral care, and foot care (1, 3). Moreover, the age-standardized disability-adjusted life-years of diabetes was lower than expected in China in 2017, but all-cause mortality in diabetic patients was still significantly higher than in people without diabetes (4, 5). T2DM patients have a high risk of multiple crucial organ damage because of long-term hyperglycemia, which increases hospitalization rates and the economic burden on patients (2, 6, 7). These problems are not imaginary because of patients' mental anxiety, but real in daily life. Patients are facing real threats, and the resulting fear is neither inappropriate nor irrational. The above threats often lead to patients with T2DM experiencing negative emotional outcomes.
Fear of progression (FoP) refers to the patients' fear of biological or psychological consequences due to the development or recurrence of their diseases, which is a fully conscious, non-neurophobic response (8–10). The level of FoP often ranges between functional and dysfunctional ends, when it elevates to a dysfunctional degree (e.g., affecting treatment or life), it is necessary to take measures. It grows recognition that FoP is one of the significant emotional difficulties facing patients with chronic progressive diseases (8), and it is also a disease experience that threatens the life of individuals (10, 11). Moreover, high FoP will affect the patient's behavioral dysfunction, wellbeing, mental health, and health-related quality of life (9, 10, 12, 13).
Herschbach et al. (14) formally proposed the Fear of Progression Questionnaire (FoP-Q) to determine FoP in patients with cancer, diabetes mellitus, and rheumatic diseases. Researches have explored the FoP and its related factors in patients with chronic diseases, especially in malignant tumors. Previous studies found that cancer patients and their partners had higher FoP than other chronic progressive diseases (e.g., diabetes mellitus) (8, 11, 15). Furthermore, the level of FoP was consistently related to their age, education status, new physical symptoms, employment status, and income (16–20). Kalra et al. (21) defined that disease progression of T2DM includes not only a gradual deterioration of cellular function, but also an increase in the dosage, frequency, and the amount of drugs used, and the occurrence or worsening of complications. Herschbach et al. suggested that diabetic patients shared specific fears about the future course of their illness (14), and the study of Dankert et al. indicated that fear of an increasing disease progression (fear of progression) was among the primary psychological distresses in patients with diabetes mellitus (8). Moreover, concrete consequences of dysfunctional fear of progression in diabetes mellitus may include affecting the mental health and quality of life of patients, and the emotional reactions of the partner of patients (8, 11).
In short, FoP is vital for the physical and mental health of patients with diabetes mellitus. However, it is poorly known about FoP and its related factors among patients with T2DM in mainland China. Therefore, our study intended to investigate FoP and explore its related factors. The results of this study may enhance understanding of the status of FoP in patients with T2DM and help healthcare givers develop more effective interventions and strategies to avoid the adverse effects of FoP.
Methods
Participants and procedures
The present cross-sectional survey was held in 2019. The sample size was determined through power analysis and calculated using the G*Power program (22). Linear multiple regression in the G*Power program was conducted using a random model. When using a two-tailed test, considering an effect size of 0.10, 13 independent variables related to FoP based on the relevant published work (16, 19, 20), significance level (p) of 0.05, and 95% power, at least 287 participants were required.
All the inpatients with T2DM were recruited by multi-stage convenience sampling method from the department of endocrinology in five tertiary hospitals in Southwest China. The inclusion criteria were listed below:
(1) Diagnosis of type 2 diabetes;
(2) Age ≥ 18 years;
(3) Education level of primary school or above;
(4) Informed consent.
And the exclusion criteria were following:
(1) T2DM with pregnancy or malignant tumors;
(2) History of mental illness and family history;
(3) Other serious medical conditions make it difficult to talk and fill out questionnaires.
Finally, 426 T2DM patients were enrolled from five tertiary hospitals in Southwest China, and 385 patients with complete data were eligible for data analysis.
Data collection
Socio-demographic and clinical data
Socio-demographic characteristics were collected including age, gender, marital status, education attainment, and employment status. Clinical characteristics were collected from patients' medical records.
Fear of progression questionnaire-short form
FoP-Q-SF, developed by Mehnert et al. (23), is a 12-item self-reporting questionnaire. Each item is rated on a 5-point Likert scale ranging from 1 point (never) to 5 points (very often). The overall score is calculated as the sum of all item scores. Patients will suffer from psychological dysfunction when the overall score is ≥34 points in the FoP-Q-SF (10). Moreover, FoP-Q-SF has been translated into multiple languages, and it is an appropriate and valuable tool for measuring FoP (14, 24, 25). The psychometric properties of the Chinese version of FoP-Q-SF among patients with T2DM have been verified by Zeng et al. (25). The Cronbach's α coefficient, split-half reliability, and test-retest reliability were 0.876, 0.828, and 0.837, separately (25). FoP-Q-SF had satisfactory psychometric properties in Chinese patients with T2DM.
Data analysis
Data were analyzed using the Statistical Package for the Social Sciences (SPSS) version 25.0 (IBM Corporation, Armonk, NY, USA). Descriptive statistics were used to calculate the sample characteristics and FoP-Q-SF score. For univariate analysis, the independent-sample t-test and one-way analysis of variance (ANOVA) were conducted to contrast the differences in FoP (continuous variables in this study showing a normal distribution). Subsequently, the variables with P < 0.05 in the univariate analysis were included in the multiple linear regression model to determine factors independently associated with FoP. Notably, the following assumptions were tested before multiple linear regression analysis: (1) drawing scatter plots to test the linearity of the model; (2) A histogram to test the normally distributed standardized residuals; (3) a Durbin-Watson value of about two to verify no autocorrelation in the residuals; (4) variance inflation factor (VIF) < 10 to verify no multicollinearity between independent variables. If all assumptions were satisfied, multiple linear regression analysis would be used.
Ethical considerations
All the study procedures were reviewed and approved by the Ethics Committee of the target University. Informed consent has been obtained from the patients or their guardians before data collection. The research conforms to the provisions of the Declaration of Helsinki in 1995 (as revised in Edinburgh 2000).
Results
Socio-demographic and clinical characteristics
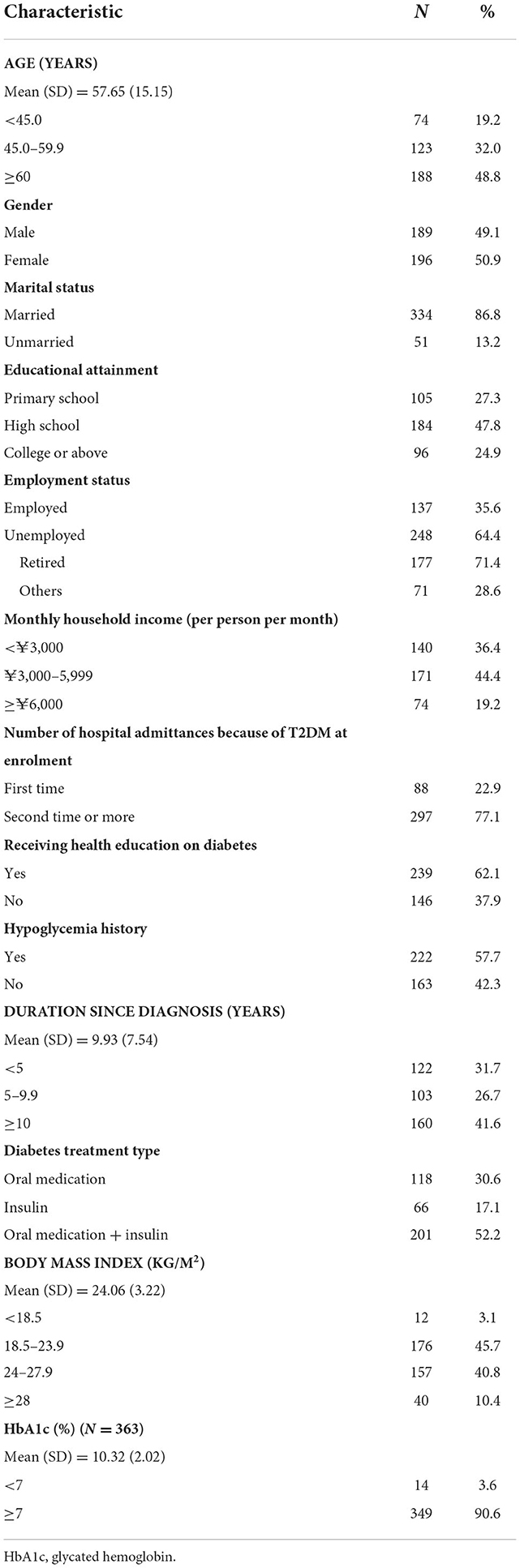
As is shown in Table 1, a total of 385 patients completed this study. The mean age was 57.65 (SD = 15.15). Many patients (More than 60%) are unemployed, including more than 70% of retirees. The mean duration since being diagnosed of the patients was 9.93 years (SD = 7.54), and the mean body mass index was 24.06 (SD = 3.22). Most of the patients (90.6%) had poor glycemic control (HbA1c ≥ 7%) (Table 1).
Fear of progression
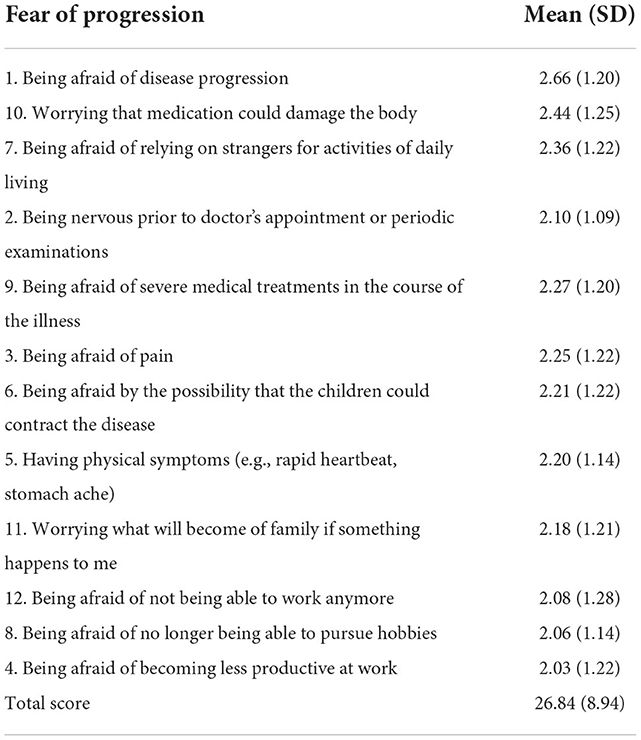
Table 2 shows FoP among patients with T2DM. The mean score of FoP was 26.84 (SD = 8.94). Eighty-nine patients (23.1%) had the score of FoP-Q-SF ≥ 34 points. The three items, named “Being afraid of disease progression,” “Worrying that the adverse reactions of medication,” and “Relying on strangers for activities of daily living,” with the highest score were 2.66 (SD = 1.20), 2.44 (SD = 1.25), and 2.36 (SD = 1.22) (Table 2).
Predictors of fear of progression
Univariate analysis identified a range of factors that were significantly associated with FoP: patients who aged <60, who were employed, and who had higher educational attainment reported higher FoP (P < 0.001). Patients hospitalized twice or more due to T2DM showed a higher level of FoP (P = 0.009). Patients had a higher level of FoP if they had hypoglycemia history, higher HbA1c, shorter time since being diagnosed with T2DM, and did not receive health education (P < 0.001) (Table 3).
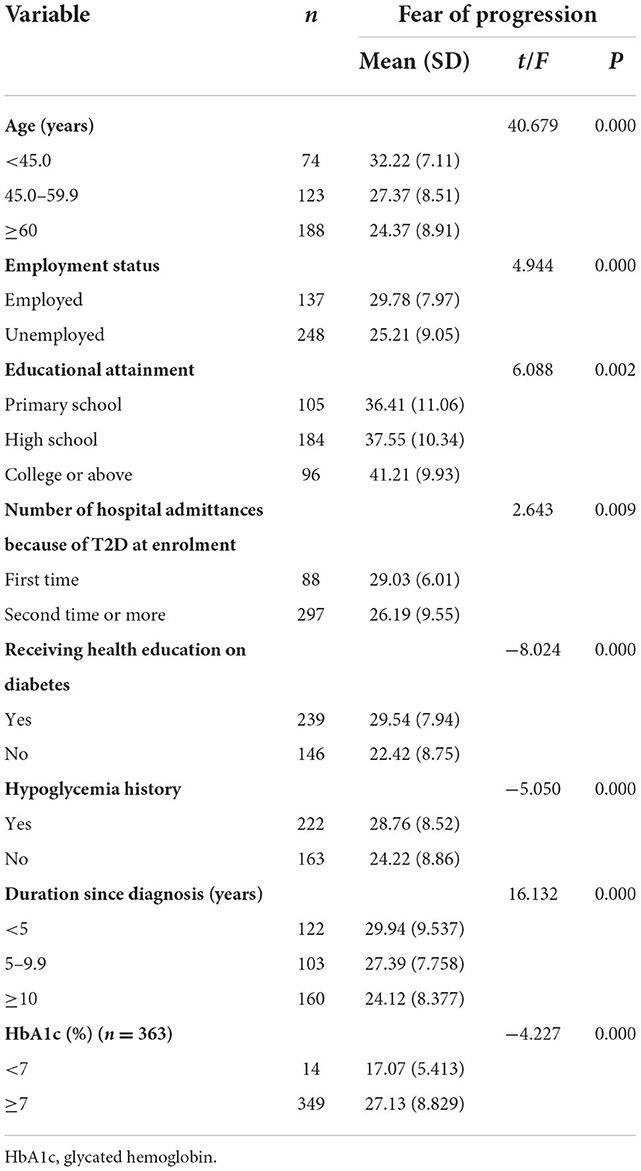
Table 3. Differences in fear of progression among various socio-demographic and clinical sub-groups (n = 385).
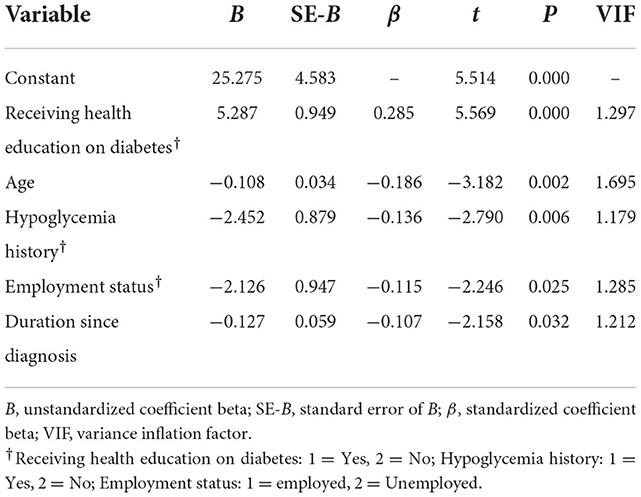
Then, the above variables with P < 0.05 were included in the multiple linear regression model. And the best-fit multiple linear regression model included five variables (Table 4). Receiving health education (β = 0.285, P < 0.01), age (β = −0.186, P = 0.002), hypoglycemia history (β = −0.136, P = 0.006), employment status (β = −2.126, P = 0.025) and duration since being diagnosed with T2DM (β = −0.107, P = 0.032) were the predictors of FoP. The variables co–explained the 26.8% variation of FoP.
Discussion
FoP is an appropriate response to the real threats of diagnosis, treatment, and course of illness, and nearly all patients have feelings ranging from very mild upset to severe worries. Nevertheless, excessive fear can induce significant adverse effects on glycemic control, behavioral dysfunction, wellbeing, and health-related quality of life in diabetic patients (9, 10, 12, 13, 26). Patients with T2DM rely on a complexity of diabetes therapeutic schedule (e.g., a combination of multiple drugs and/or insulin therapy) to achieve glycemic control (1, 3). With the development of T2DM, original symptoms become aggravated and new symptoms or complications will appear to reduce the quality of life (e.g., high risk of disability). These reasons may lead to patients' high FoP. Therefore, it is essential to understand and control FoP in patients with T2DM.
We can use questionnaire scores to initially assess the degree of fear in patients. In this study, the score of FoP-Q-SF was lower than a Chinese study among 636 cancer patients (20), and a German study among partners of chronically ill patients (11). A possible explanation is that T2DM is a common disease, and there are currently mature treatment plans. Although it cannot be completely cured, patients can delay the progression of the disease and control its recurrence through various methods, which significantly reduces the psychological pressure of T2DM patients.
Moreover, 23.1% of patients in our study developed psychological dysfunction due to FoP. The findings of the present study suggested that FoP among patients with T2DM, especially those with psychological dysfunction, need paid more attention to and timely identified using FoP-Q-SF by health caregivers to distinguish with anxiety disorder. Previous studies also found that health caregivers might use protective motivation theory and cognitive behavioral psychotherapy to reduce patients' FoP (11, 27).
In the present study, the three items with the highest score were “Being afraid of disease progression,” “Being worried about side effects of medication,” and “Relying on strangers for activities of daily living.” However, the findings in our study were different from brain cancer patients, and they worried about “what will become of family if something happens to me” and “severe medical treatments in the course of the illness” (28). This difference may be related to the different psychology of patients caused by different severity and prognosis of the disease. Patients with diabetes have better prognosis and less serious life-threatening conditions, so the patients are more concerned about changes in quality of life, while cancer patients are more concerned about survival rates and the impact on their families. Therefore, different psychological problems should be addressed for patients with different chronic diseases. Furthermore, a significant discrepancy between our research and a previous study from Thailand is that being afraid of relying on strangers for activities of daily living is the most infrequent fear in the previous study, even though there was a common phenomenon that three or four generations under one roof (29), which may be related to our traditional culture.
People from different backgrounds have different levels of FoP, probably due to different levels of awareness of the disease. Therefore, when we make a control plan, it is essential to be concerned about their sociodemographic elements. Our study found that health education is crucial to avoiding high FoP. Health education on diabetes is recognized as an essential measure to improve knowledge and awareness of diabetes and further reduce the risk of developing FoP (30–32). However, more than 35.0% of patients in our study had not received health education on diabetes. Winkley et al. (33) found that newly diagnosed patients with T2DM showed low attendance at structured education, which might increase their fear of the unknown disease. This result could also be ascribed to the fact that the number of qualified diabetes educators was very limited in China. Considering the massive population of individuals with diabetes in mainland China, cultivating more high-quality certified diabetes educators is warranted. Moreover, limited health resources can be used maximum by health caregivers with new technology (e.g., online health education based on mobile phones or computers) (34, 35).
The other clinical related factor of FoP is hypoglycemia history. Hypoglycemia is a common complication of diabetes treatment, and it often accompanies unpleasant experiences and negative consequences (36). Further, severe hypoglycemia is associated with the rapid progression of diabetes (37), even cause serious acute and chronic complications. Close monitoring of blood glucose might be used to avoid FoP due to hypoglycemia history (38).
Our study showed that age and employment status were related to FoP. Patients who were younger and employed had a higher level of FoP. At present, most employed patients with T2DM are middle-aged (39). Patients often thought that their life expectancy might be longer, and the negative impact of T2DM would be more far-reaching (40), but Seuring et al. (41) found that T2DM had limited their labor productivity, particularly in developing countries. In China, patients with T2DM, employed in recent decades, were born in the period of implementation of the one-child policy and faced unprecedented financial pressure (e.g., children's tuition and parents' pensions) (42). The above reasons might result in their higher level of FoP.
This study investigated the source and extent of FoP among T2DM patients, and further clarified FoP related factors. The present study's findings may be useful for targeting and tailoring FoP interventions of specific population groups.
Despite the supportive finding of the study, there were some limitations need to be acknowledged. Compared with outpatients, hospitalized T2DM may be a more serious condition (e.g., higher HbA1C). Thus, we only enrolled inpatients with T2DM from the department of endocrinology in five tertiary hospitals in Southwest China, the ability to generalize the study results may be limited. Furthermore, the R2 value of the multiple linear regression model was relatively small, and further studies were warranted to identify other predictors of FoP.
Conclusion
As a common chronic disease, T2DM poses great danger to human health. With its incidence increasing yearly, many prevention and treatment measures and educational activities have been carried out. More and more studies have focused on the negative psychological effects of the disease, including fear of all aspects of the disease (commonly referred to as fear of progression, FoP), in addition to its serious complications. Our study based on socio-demographic and clinical data, FoP-Q-SF completion, and data analysis of 385 patients. Finally, 23.1% of patients with T2DM reported high FoP. FoP among patients with T2DM varied from different socio-demographic and clinical characteristics, especially health education, hypoglycemia history, employment status, age and duration since being diagnosed with T2DM. Interventions should be based on patients varying socio-demographic and clinical profiles and tailored to the circumstances of the individual patients. The findings of this study may provide new insights on how to care for dysfunctional FoP patients with T2DM. Future research may continuously focus on the FoP of patients and their partners with T2DM, and for the predictors explore more effective interventions to decrease high FoP.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of Chongqing Medical University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
YW and JT contributed to the conception and design of the data analysis and analyzed the data. YW and QY searched literature and prepared the manuscript. ZZ, RY, RW, and JC performed the investigation and collected the data. ZZ collated and supervised the data and other materials. YW, JT, and HZ prepared the revised manuscript. All authors have read and approved the manuscript.
Funding
This study was supported by Program for Youth Innovation in Future Medicine, Chongqing Medical University (W0008) and Humanities and Social Sciences Research Project of Chongqing Municipal Education Commission in 2022 (22SKGH062).
Acknowledgments
Our heartfelt thanks go out to all the participants, as well as to other colleagues and experts who have helped us with our program.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. International Diabetes Federation. IDF. Diabetes Atlas. 9th ed. (2019). Available online at: https://diabetesatlasorg/en (accessed December 6, 2021).
2. Gregg EW, Li Y, Wang J, Burrows NR, Ali MK, Rolka D, et al. Changes in diabetes-related complications in the United States, 1990-2010. N Engl J Med. (2014) 370:1514–23. doi: 10.1056/NEJMoa1310799
3. Dobrica EC, Gaman MA, Cozma MA, Bratu OG, Pantea SA, Diaconu CC. Polypharmacy in type 2 diabetes mellitus: insights from an internal medicine department. Medicina. (2019) 55:436. doi: 10.3390/medicina55080436
4. Bragg F, Holmes MV, Iona A, Guo Y, Du H, Chen Y, et al. Association between diabetes and cause-specific mortality in rural and urban areas of China. JAMA. (2017) 317:280–9. doi: 10.1001/jama.2016.19720
5. Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2019) 394:1145–58. doi: 10.1016/S0140-6736(19)30427-1
6. Afroz A, Alramadan MJ, Hossain MN, Romero L, Alam K, Magliano DJ, et al. Cost-of-illness of type 2 diabetes mellitus in low and lower-middle income countries: a systematic review. BMC Health Serv Res. (2018) 18:972. doi: 10.1186/s12913-018-3772-8
7. Hu WS, Lin CL. Use of the progression of adapted Diabetes Complications Severity Index to predict acute coronary syndrome, ischemic stroke, and mortality in Asian patients with type 2 diabetes mellitus: a nationwide cohort investigation. Clin Cardiol. (2018) 41:1038–43. doi: 10.1002/clc.22991
8. Dankert A, Duran G, Engst-Hastreiter U, Keller M, Waadt S, Henrich G, et al. Fear of progression in patients with cancer, diabetes mellitus and chronic arthritis. Rehabilitation. (2003) 42:155–63. doi: 10.1055/s-2003-40094
9. Herschbach P, Dinkel A. Fear of progression. Recent results in cancer research. Psychooncology. (2014) 197:11–29. doi: 10.1007/978-3-642-40187-9_2
10. Hinz A, Mehnert A, Ernst J, Herschbach P, Schulte T. Fear of progression in patients 6 months after cancer rehabilitation-a- validation study of the fear of progression questionnaire FoP-Q-12. Support Care Cancer. (2015) 23:1579–87. doi: 10.1007/s00520-014-2516-5
11. Zimmermann T, Herschbach P, Wessarges M, Heinrichs N. Fear of progression in partners of chronically ill patients. Behav Med. (2011) 37:95–104. doi: 10.1080/08964289.2011.605399
12. Donald M, Dower J, Coll JR, Baker P, Mukandi B, Doi SA. Mental health issues decrease diabetes-specific quality of life independent of glycaemic control and complications: findings from Australia's living with diabetes cohort study. Health Qual Life Outcomes. (2013) 11:170. doi: 10.1186/1477-7525-11-170
13. Grammes J, Schafer M, Benecke A, Low U, Klostermann AL, Kubiak T, et al. Fear of hypoglycemia in patients with type 2 diabetes: the role of interoceptive accuracy and prior episodes of hypoglycemia. J Psychosom Res. (2018) 105:58–63. doi: 10.1016/j.jpsychores.2017.12.010
14. Herschbach P, Berg P, Dankert A, Duran G, Engst-Hastreiter U, Waadt S, et al. Fear of progression in chronic diseases: psychometric properties of the Fear of Progression Questionnaire. J Psychosomat Res. (2005) 58:505–11. doi: 10.1016/j.jpsychores.2005.02.007
15. Hall DL, Lennes IT, Pirl WF, Friedman ER, Park ER. Fear of recurrence or progression as a link between somatic symptoms and perceived stress among cancer survivors. Support Care Cancer. (2017) 25:1401–7. doi: 10.1007/s00520-016-3533-3
16. Crist JV, Grunfeld EA. Factors reported to influence fear of recurrence in cancer patients: a systematic review. Psychooncology. (2013) 22:978–86. doi: 10.1002/pon.3114
17. Esser P, Gotze H, Mehnert-Theuerkauf A, Knoop H, Kuba K. Fear of progression and its role in the relationship of cancer-related fatigue with physical functioning and global quality of life - A register-based study among hematological cancer survivors. J Psychosomat Res. (2019) 127:109844. doi: 10.1016/j.jpsychores.2019.109844
18. Garcia S. The effects of education on anxiety levels in patients receiving chemotherapy for the first time: an integrative review. Clin J Oncol Nurs. (2014) 18:516–21. doi: 10.1188/14.CJON.18-05AP
19. Hefner J, Csef EJ, Kunzmann V. Fear of progression in outpatients with chronic myeloid leukemia on oral tyrosine kinase inhibitors. Oncol Nurs Forum. (2016) 43:190–7. doi: 10.1188/16.ONF.190-197
20. Yang Y, Sun H, Liu T, Zhang J, Wang H, Liang W, et al. Factors associated with fear of progression in chinese cancer patients: sociodemographic, clinical and psychological variables. J Psychosomat Res. (2018) 114:18–24. doi: 10.1016/j.jpsychores.2018.09.003
21. Kalra S, Kamaruddin NA, Visvanathan J, Santani R. Defining disease progression and drug durability in type 2 diabetes mellitus. Eur Endocrinol. (2019) 15:67–9. doi: 10.17925/EE.2019.15.2.67
22. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. (2007) 39:175–91. doi: 10.3758/BF03193146
23. Mehnert A, Herschbach P, Berg P, Henrich G, Koch U. Fear of progression in breast cancer patients–validation of the short form of the Fear of Progression Questionnaire (FoP-Q-SF). Zeitschrift Psychosomat Med Psychother. (2006) 52:274–88. doi: 10.13109/zptm.2006.52.3.274
24. Clever K, Schepper F, Pletschko T, Herschbach P, Christiansen H, Martini J. Psychometric properties of the Fear of Progression Questionnaire for parents of children with cancer (FoP-Q-SF/PR). J Psychosomat Res. (2018) 107:7–13. doi: 10.1016/j.jpsychores.2018.01.008
25. Zeng ZH, Wang YH, Yuan RZ, Chen JL, Wang RD, Tang J. The reliability and validity of the Chinese version of Fear of Progression Questionnaire-Short Form among patients with type 2 diabetes mellitus. J Qilu Nurs. (2022) 28:48–52. doi: 10.3969/j.issn.1006-7256.2022.09.014
26. Indelicato L, Dauriz M, Santi L, Bonora F, Negri C, Cacciatori V, et al. Psychological distress, self-efficacy and glycemic control in type 2 diabetes. Nutr Metab Cardiovasc Dis. (2017) 27:300–6. doi: 10.1016/j.numecd.2017.01.006
27. Dinkel A, Herschbach P. Fear of progression in cancer patients and survivors. Recent results in cancer research. Psychooncology. (2018) 210:13–33. doi: 10.1007/978-3-319-64310-6_2
28. Goebel S, Mehdorn HM. Fear of disease progression in adult ambulatory patients with brain cancer: prevalence and clinical correlates. Support Care Cancer. (2019) 27:3521–9. doi: 10.1007/s00520-019-04665-9
29. Hanprasertpong J, Geater A, Jiamset I, Padungkul L, Hirunkajonpan P, Songhong, N. Fear of cancer recurrence and its predictors among cervical cancer survivors. J Gynecol Oncol. (2017) 28:e72. doi: 10.3802/jgo.2017.28.e72
30. Attridge M, Creamer J, Ramsden M, Cannings-John R, Hawthorne K. Culturally appropriate health education for people in ethnic minority groups with type 2 diabetes mellitus. Cochr Database Syst Rev. (2014) 4:CD006424. doi: 10.1002/14651858.CD006424.pub3
31. Ding X, Shen Z, Zhang C, Qi L, Jiao Y, Mao D. Impact of health educators' intervention on non-communicable diseases-related knowledge, attitude and behavior among rural residents. Zhonghua Yu Fang Yi Xue Za Zhi. (2015) 49:1098–103.
32. Dizdar OS, Gul OO, Baspinar O, Cander S, Sisman P, Eker B, et al. Assessment of factors related to the understanding of education and knowledge of self-care among patients with diabetes mellitus: a cross-sectional prospective study. Adv Therapy. (2016) 33:1565–78. doi: 10.1007/s12325-016-0378-6
33. Winkley K, Stahl D, Chamley M, Stopford R, Boughdady M, Thomas S, et al. Low attendance at structured education for people with newly diagnosed type 2 diabetes: general practice characteristics and individual patient factors predict uptake. Patient Educ Counsel. (2016) 99:101–7. doi: 10.1016/j.pec.2015.08.015
34. Dong Y, Wang P, Dai Z, Liu K, Jin Y, Li A, et al. Increased self-care activities and glycemic control rate in relation to health education via Wechat among diabetes patients: a randomized clinical trial. Medicine. (2018) 97:e13632. doi: 10.1097/MD.0000000000013632
35. Pal K, Eastwood SV, Michie S, Farmer AJ, Barnard ML, Peacock R, et al. Computer-based diabetes self-management interventions for adults with type 2 diabetes mellitus. Cochr Database Syst Rev. (2013) 3:CD008776. doi: 10.1002/14651858.CD008776.pub2
36. Wild D, von Maltzahn R, Brohan E, Christensen T, Clauson P, Gonder-Frederick L. A critical review of the literature on fear of hypoglycemia in diabetes: implications for diabetes management and patient education. Patient Educ Couns. (2007) 68:10–5. doi: 10.1016/j.pec.2007.05.003
37. Kornelius E, Yang YS, Lo SC, Peng CH, Lai YR, Chiou JY, et al. Progress of diabetes severity associated with severe hypoglycemia in Taiwan. Am J Manag Care. (2018) 24:e99–106.
38. Torimoto K, Okada Y, Hajime M, Tanaka K, Tanaka Y. Risk factors of hypoglycemia in patients with type 2 diabetes mellitus: a study based on continuous glucose monitoring. Diabetes Technol Ther. (2018) 20:603–12. doi: 10.1089/dia.2018.0017
39. Kouwenhoven-Pasmooij TA, Burdorf A, Roos-Hesselink JW, Hunink MG, Robroek SJ. Cardiovascular disease, diabetes and early exit from paid employment in Europe; the impact of work-related factors. Int J Cardiol. (2016) 215:332–7. doi: 10.1016/j.ijcard.2016.04.090
40. Vickberg SM. The Concerns About Recurrence Scale (CARS): a systematic measure of women's fears about the possibility of breast cancer recurrence. Ann Behav Med. (2003) 25:16–24. doi: 10.1207/S15324796ABM2501_03
41. Seuring T, Goryakin Y, Suhrcke M. The impact of diabetes on employment in Mexico. Econ Hum Biol. (2015) 18:85–100. doi: 10.1016/j.ehb.2015.04.002
Keywords: predictors, fear of progression, type 2 diabetes mellitus (T2DM), multi-center, cross-sectional study, healthcare professions education, self-management
Citation: Wang Y, Yu Q, Zeng Z, Yuan R, Wang R, Chen J, Zhou H and Tang J (2022) Predictors of fear of diabetes progression: A multi-center cross-sectional study for patients self-management and healthcare professions education. Front. Public Health 10:910145. doi: 10.3389/fpubh.2022.910145
Received: 13 May 2022; Accepted: 21 November 2022;
Published: 19 December 2022.
Edited by:
Wulf Rössler, Charité Universitätsmedizin Berlin, GermanyReviewed by:
Dominik Fugmann, Heinrich Heine University of Düsseldorf, GermanyKsenia Zagorodnikova, Almazov National Medical Research Centre, Russia
Copyright © 2022 Wang, Yu, Zeng, Yuan, Wang, Chen, Zhou and Tang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hengyu Zhou, emhvdWhlbmd5dUBjcW11LmVkdS5jbg==; Jiao Tang, dGFuZ2ppYW85MjA5QGNxbXUuZWR1LmNu
 Yanhao Wang1,2,3
Yanhao Wang1,2,3 Zihuan Zeng
Zihuan Zeng Jiao Tang
Jiao Tang