- 1Hunan Provincial Key Laboratory of Clinical Epidemiology, Xiangya School of Public Health, Central South University, Changsha, China
- 2Department of Medical Statistics and Epidemiology, School of Public Health, Sun Yat-sen University, Guangzhou, China
- 3Hunan Center for Disease Control and Prevention, Changsha, China
- 4Department of Microbiology, Immunology and Transplantation, Rega Institute for Medical Research, KU Leuven, Leuven, Belgium
- 5Hunan Children's Hospital, Changsha, China
- 6Department of Infectious Disease, The First Hospital of Changsha, Changsha, China
Objective: HIV epidemiology in South-Central China is rarely reported. This study aims to characterize epidemiological and clinical features of HIV-infected patients in Hunan Province, located in South-Central China, for better management of HIV infections.
Methods: This retrospective study retrieved multi-center records of laboratory-confirmed HIV-infected patients in Hunan province. Information on HIV-associated mortality and antiretroviral therapies was also collected.
Results: Among 34,297 patients diagnosed with HIV infections from 2003 to 2018, 73.9% were males, 41.3% were older adults (≥50 years), and 71.2% were infected by heterosexual transmission. Despite a slow growth of new HIV infections in the overall population, annual percentages of HIV infections increased in older males (85.3% through heterosexual transmission) and young patients <30 years (39.9% through homosexual transmission). At baseline, serum levels of CD4+ T-cell counts were lower in older adults (191.0 cells/μl) than in young patients (294.6 cells/μl, p-value < 0.0001). A large proportion (47.2%, N = 16,165) of HIV-infected patients had advanced HIV disease (CD4+ T-cell counts < 200 cells/μl) from 2003 to 2018. All-cause mortality (57.0% due to AIDS-related illnesses) was reported among 4411 HIV-infected patients, including 2619 older adults. The 10-year survival rate was significantly lower in elderly males than in other patients (59.0 vs. 78.4%, p-value < 0.05).
Conclusions: Elderly males are prone to HIV infections with a high risk of HIV-associated fatality. Our findings support early prevention and critical care for elderly populations to control HIV infections.
Introduction
Human immunodeficiency virus (HIV) infection causes progressive damage to the immune system, characterized by massive depletion of CD4+ T-cells, sustained immune activation, and systemic inflammation (1). As of today, more than 37 million patients are living with HIV globally and ~1.1 million cases are living in China (http://www.unaids.org). Since the introduction of antiretroviral therapies (ART) in the 1980s (2, 3), the mortality among people living with HIV has decreased significantly (4) and the life expectancy of HIV-infected patients has improved dramatically (5, 6). Most antiretroviral regimens consist of three oral compounds, including two nucleoside reverse transcriptase inhibitors (NRTIs) plus either one non-nucleoside reverse transcriptase inhibitor (NNRTI), one integrase inhibitor, or one protease inhibitor boosted by ritonavir or cobicistat (7–9). Although many highly active antiretroviral therapies have been approved in the past decades (3, 9), an effective drug or vaccine remains unavailable to “cure” HIV infections (10). To curb HIV infections, it remains important for epidemiological studies to identify high-risk populations in different countries and regions.
Since the first report of HIV infection in China in 1989 (11), HIV has spread across the country in the past decades. In 2018, 64,170 patients and 18,780 HIV-related deaths were reported in China (12). The overall incidence of HIV in China was not high but on the rise over time, and the fatality rate of HIV was ranked among the top five notifiable infectious diseases (13). A series of prevention and treatment strategies have been implemented in China (14). In 2003, China launched the “four free and one care” policy for HIV (free treatment, free voluntary counseling and testing, free prevention of mother-to-child transmission, free schooling for AIDS orphans, and social care for HIV-infected patients) (15). In 2011, the “five expand six strengthen” policy was implemented in China to strengthen the national coverage, including HIV testing and surveillance, health education, blood administration and safety, prevention of mother-to-child transmission, antiretroviral therapies, as well as health care and social support (16). Since 2003, the National Free Antiretroviral Treatment Program (NFATP) has been implemented in China, despite the limited variety of free antiretroviral drugs. With the support of NFATP, the ART has undergone continuous evaluation and improvement (17). Over the past decades, China has made substantial achievements in the prevention and treatment of HIV. However, it remains a challenge to prevent and control HIV infections in China because of dynamic transportation, economic development, and social and cultural dynamics (16, 18). In the past 20 years, the incidences of intravenous drug use, mother-to-child transmission, and blood transmission decreased substantially in China (19), but an increase in HIV infections can be found in the elderly population (14, 20) and young students (21). Sexual transmission remains the primary route of HIV transmission in China (22), but the incidences of homosexual transmission are growing in recent years (23–25). Furthermore, the geographical distribution of HIV infections varies in different provinces and regions in China (14). For instance, homosexual transmission in a province in northeast China accounted for the majority (69%) of HIV infections from 2011 to 2012 (26). Another epidemiological feature is that 77.1% of HIV infections in Southeastern China were found in patients aged 19–50 years (27). Taken together, it remains important to explore local epidemiological features to control HIV infections.
Hunan province, located in South-Central China, is known for its large population and is one of the most popular tourist destinations in China. Since the first report of HIV infection in Hunan Province in 1992, there is a growing trend of HIV incidences. However, no report has published epidemiological and clinical features of HIV-infected patients in Hunan province. Here, we analyzed a large-scale cohort of 32,419 HIV-infected patients who were diagnosed from 2003 to 2018 in Hunan province. Our study will provide the first comprehensive survey of the temporal trend, spatial distribution, and population characteristicsof HIV infection, virological responses, and survival status of HIV-infected patients who received standard ART. This study will shed light on the temporal trend of HIV infections in a high-risk population for better management and prevention of HIV infections in Hunan province.
Methods
Study Design and Patients
We performed a retrospective study to collect epidemiological and clinical records of HIV-infected patients based on the official database from the Centers for Disease Control in Hunan province. This database includes patient information on demographic records, serum blood biomarkers, ART records, HIV-associated death dates, and virological responses. All patients were confirmed to have laboratory-confirmed HIV infection during the period from 2003 to 2018. According to the national regulation, any HIV-positive case should be officially reported to the Centers for Disease Control in China. Serum levels of CD4+ T-cells and CD8+ T cells were assessed using the BD FACSCalibur flow cytometer. HIV viral loads were quantified using the COBAS® AmpliPrep instrument. This retrospective study was conducted under the Helsinki Declaration and was approved by the Ethics Committees of The First Hospital of Changsha (Approval ID: 202160).
Definitions
Failure of immune reconstitution was defined by the persistent CD4 level <100 cells/μl (28). As described previously (29), HIV-infected patients experienced the status of poor immune reconstruction if two conditions were fulfilled: (i) CD4+ T-cell counts < 350 cells/μl; and (ii) CD4+ T-cell increases < 100 cells/μl in those patients with HIV RNA <50 copies/ml for more than 1 year. Advanced HIV disease was defined as presenting for HIV care with CD4+ T-cell counts <200 cells/μL or WHO stage 3/4 conditions.
Statistical Analysis
Categorical variables were presented as frequencies and percentages, while continuous variables were analyzed by mean and standard deviations. To analyze the temporal trend of new HIV infections per year, we used Joinpoint regression models (https://surveillance.cancer.gov/joinpoint/) to calculate the annual percentage changes (APC) as well as the trend test of APC. The grid search method was used to determine the joinpoint, and permutation tests were used to select the optimal model. Paired-t-tests were used to detect differences in CD4 levels before and after treatment. Chi-square tests were applied to compare the proportion of virological responses in patients receiving different ART. Welch's ANOVA methods were used to compare the means of multiple groups, while Games-Howell tests were used for pairwise comparisons between groups. P-values of multiple comparisons were corrected by the Holm method. The survival rate was estimated by the Kaplan-Meier method, while log-rank tests were used to evaluate any difference. Our statistical analyses used the pairwise deletion approach to handle missing data. All statistical analyses were descriptive, and no random sampling was conducted. A statistical significance was considered when a p-value was below 0.05. We performed statistical analyses using the Joinpoint Regression Program 4.9.0.0, R x64 4.1.0, and GraphPad prism 8.0.1.
Results
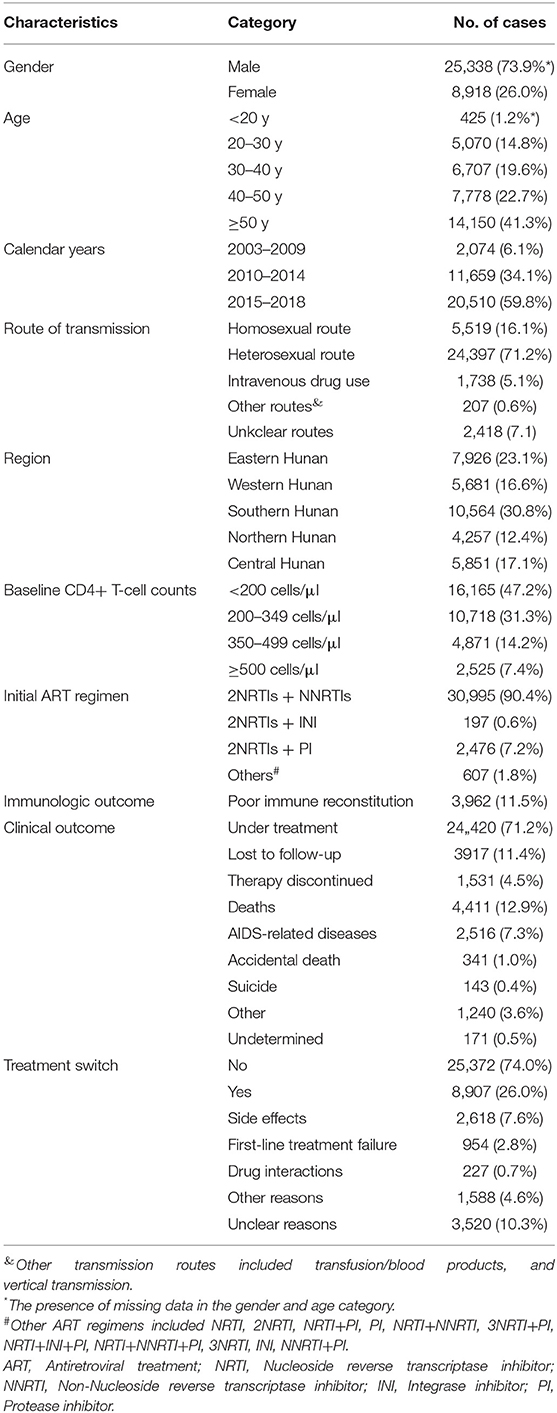
From 2003 to 2018, a total of 34,297 HIV-infected patients were treated at the designated hospitals in Hunan province. Patient information is summarized in Table 1. Gender disparity was observed with a large proportion of male patients (N = 25,338, 73.9%). The number of HIV infections in both males and females increased over time, whereas the increasing numbers grew faster in males (Figure 1A). At the time of their first HIV-positive diagnosis, the youngest and oldest patients were 7 and 95 years of age, respectively. The median age at the first diagnosis of HIV infection was 46 years old. Among all age groups, patients aged ≥50 years accounted for the largest proportion at all times, the number of HIV-infected patients aged <30 years increased steadily from 2010 to 2018 (Figure 1B).
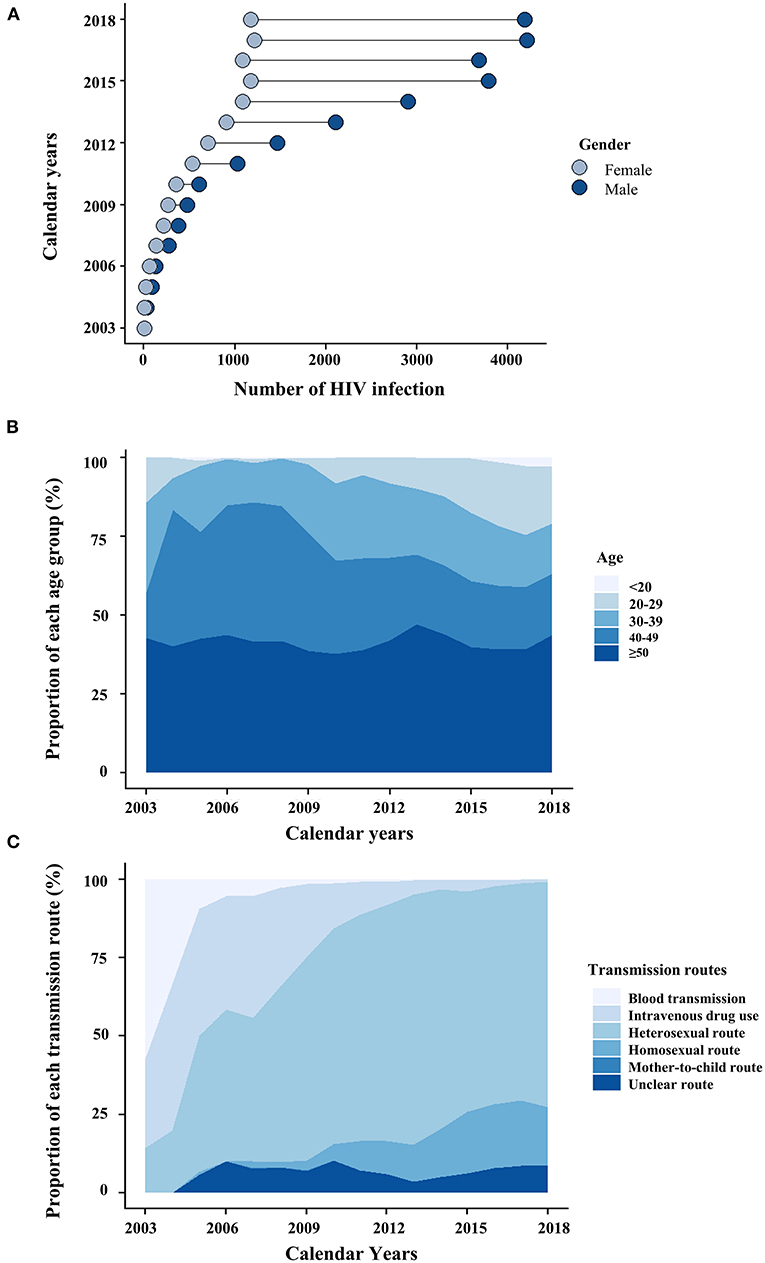
Figure 1. The dynamics of HIV-infected patients are categorized by gender (A), age (B), and transmission routes (C).
Epidemiological Characteristics of New HIV Cases
Temporal Trend of New HIV Cases
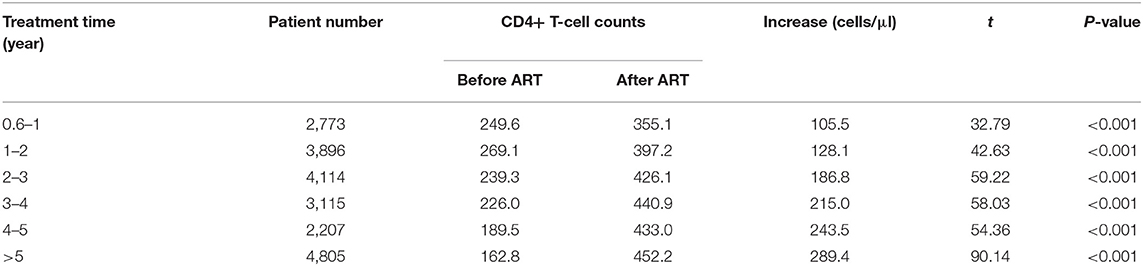
The proportion of new HIV cases was only 6.1% from 2003 to 2009, but a steady increase (34.1%, N = 11,659) was observed from 2010 to 2014. The majority of these new cases (N = 20,510, 59.8%) were observed from 2015 to 2018, indicating a substantial increase of new HIV cases during this period (Table 1). The Joinpoint regression estimated 46.1% of the average annual percentage change from 2003 to 2018 (AAPC2003−2018), suggesting the increasing number of HIV infections in Hunan province (Figure 2A). In contrast, the annual percentage change from 2004 to 2018 (APC2014−2018) was 6.62%, indicating a decreasing growth rate from 2014 to 2018 (Table 2). Although new HIV cases seemed to increase in both males and females, the number and the growth trend of HIV cases in males were significantly higher (Figure 2A). As shown in Figure 2B, the incidences of HIV new cases increased in all age groups (<30 years, 30–39 years, 40–49 years, ≥50 years). A significant increase in HIV infections was identified among patients <30 years (AAPC2013−2018: 60.9%) (Figure 2B).
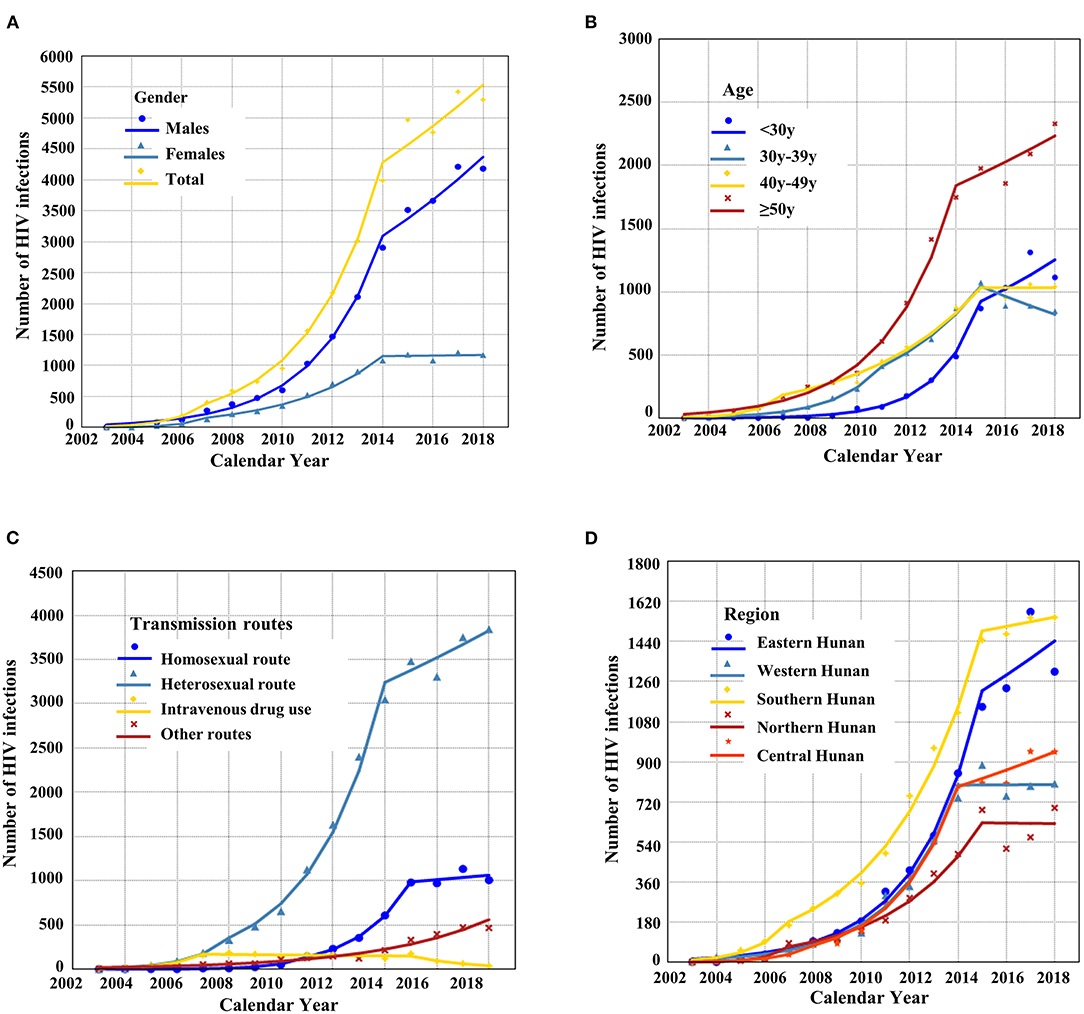
Figure 2. The temporal trend of the total number of HIV-1 infections (A) and HIV infections is stratified by gender (A), age (B), transmission (C), and region (D).
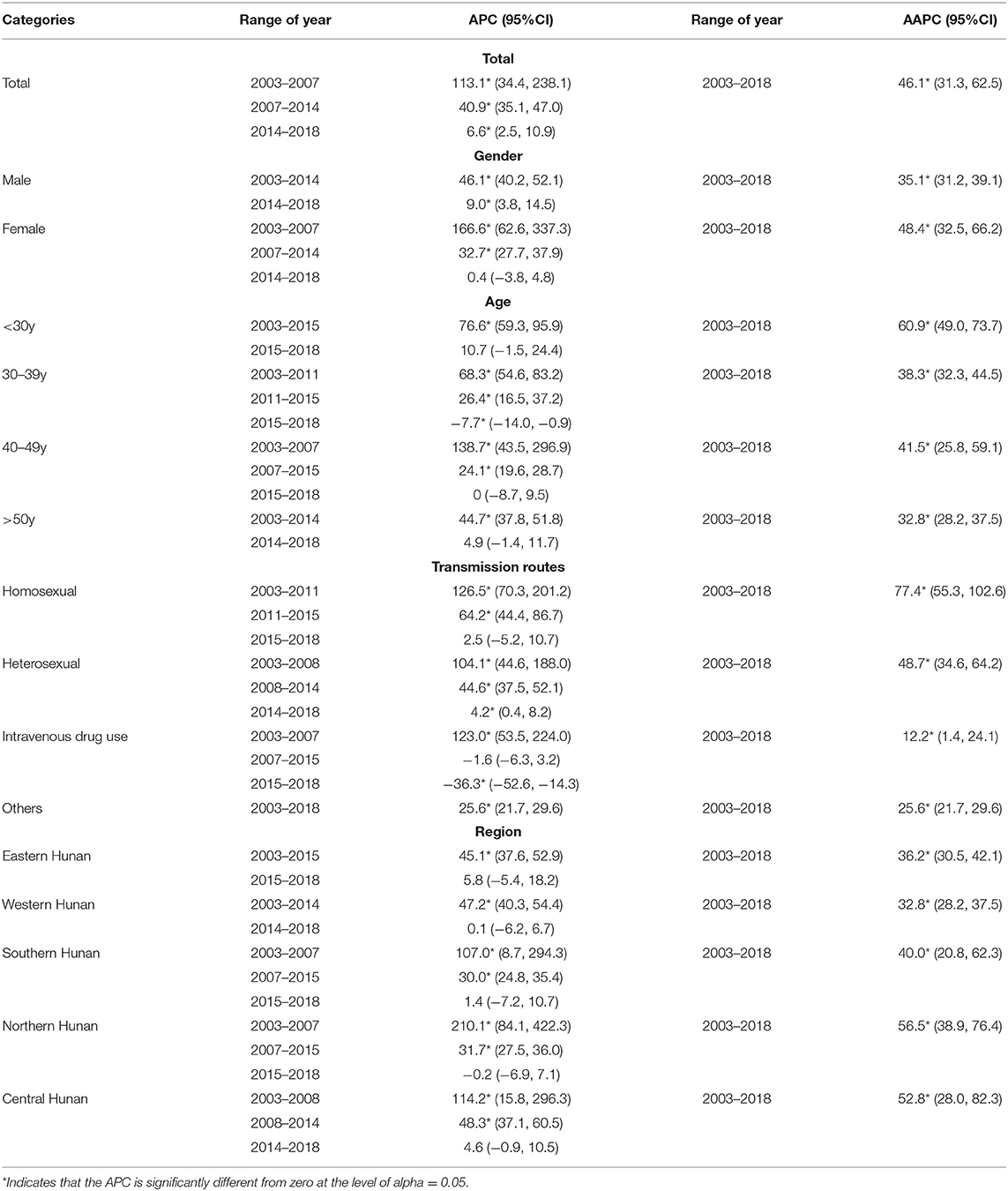
Table 2. Temporal trend analysis of HIV cases stratified by gender, age, transmission routes, and geographical regions.
The Spatial Disparity of HIV-Infected Patients
We analyzed the spatial disparity of HIV-infected patients using geographical distribution maps (Figure 3). As shown in Table 1, the accumulated number of HIV infections (2003–2018) and HIV-associated fatality rates varied significantly between five geographical regions (Eastern Hunan, Southern Hunan, Western Hunan, Northern Hunan, Central Hunan). By 2018, Northern Hunan had the lowest number (N = 4,257) of HIV infections (Figure 3A). Western Hunan had the second-lowest number of HIV infections, but its case fatality rate was the highest (Figure 3B). Southern Hunan had the most cases of HIV infections and HIV-associated deaths. The growth rate of HIV infections in the above five regions varied (Figure 2D), but the growth trend slowed down or decreased from 2014 to 2018 (Supplementary Table S1).
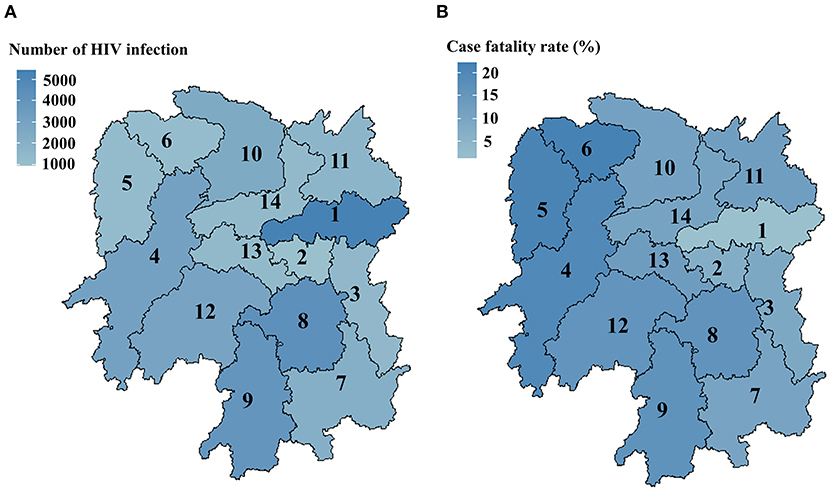
Figure 3. Geographical distribution maps of HIV-1 infections (A) and the case fatality rate (B) in Hunan province from 2003 to 2018. Eastern Hunan included region 1, region 2, and region 3; Western Hunan included region 4, region 5, and region 6; Southern Hunan included region 7, region 8, and region 9; Northern Hunan included region 10 and region 11; Central Hunan included region 12, region 13, and region 14.
Dynamic Changes in HIV Transmission Routes
From 2003 to 2005, intravenous drug use and blood transmission were the major transmission routes (>50%) of HIV infections in Hunan province. From 2006 to 2018, sexual transmission dominated the transmission route over time (Figure 1C). The absolute number of HIV infections through heterosexual transmission was far more common than that through other routes (Figure 2C). In 2018, the most common route of infection was heterosexual transmission (71.8%, N = 3,844), followed by homosexual transmission (18.8%, N = 1,007). Heterosexual transmission occurred mainly in male patients (67.2%, N = 16,414) and elderly patients aged ≥50 years (49.5%, N = 12,070). In contrast, the homosexual transmission was mostly found among young patients (age ≤30 years) (39.7%, N = 2,192) compared with elderly patients (14.6%, N = 806). Among all transmission routes, the homosexual transmission had the highest annual percentage change (Table 2).
Clinical Characteristics and Outcomes of HIV Patients
ART Regimens
The ART regimen of two nucleoside reverse transcriptase inhibitors (NRTIs) plus one non-nucleoside reverse transcriptase inhibitor (NNRTI) was administered to a majority of HIV-infected patients (90.4%, N = 30,995). The most frequently prescribed NRTI backbones were a fixed combination of tenofovir and lamivudine (60.3%, N = 20,657). The most commonly prescribed third drug was an NNRTI such as efavirenz (68.2%, N = 23,380). Among 34,297 patients who received standard ART, 3,962 (11.5%) patients developed poor immune reconstitution. Moreover, 8,907 patients switched their treatment regimens because of adverse effects (29.3%, N-2618), followed by the first-line treatment failure (10.7%, N = 954), drug-drug interactions (227, 2.5%), and other reasons (Table 1).
CD4 Dynamics Before and After ART
At baseline, a large proportion (47.2%, N = 16,165) of HIV-infected patients CD4+ T cell counts < 200 cells/μl at baseline (Table 1). From 2003 to 2018, there was a steady decline in the proportion of advanced HIV disease from 71.4% (2003) to 42.8% (2018) (Supplementary Figure S1). Although the number of advanced HIV disease increased over time, the proportion of advanced HIV disease from 2003 to 2018 showed decreasing patterns (Figure 4). In 2018, the proportion of advanced HIV disease was 31.9% in young patients aged <30 years (Supplementary Table S2). The median CD4+ T-cell counts at baseline were 212 cells/μl. CD4+ T-cell counts differed significantly in different age groups (Figure 5A) and elderly patients had lower CD4+ T-cell counts at baseline (elderly patients: 191.0 cells/μl, young patients: 294.6 cells/μl, p-value < 0.0001). As shown in Figure 5B, baseline CD4+ T-cell counts were higher in homosexual male patients (297.47 cells/μl), followed by heterosexual females (225.36 cells/μl), and heterosexual males (209.42 cells/μl).
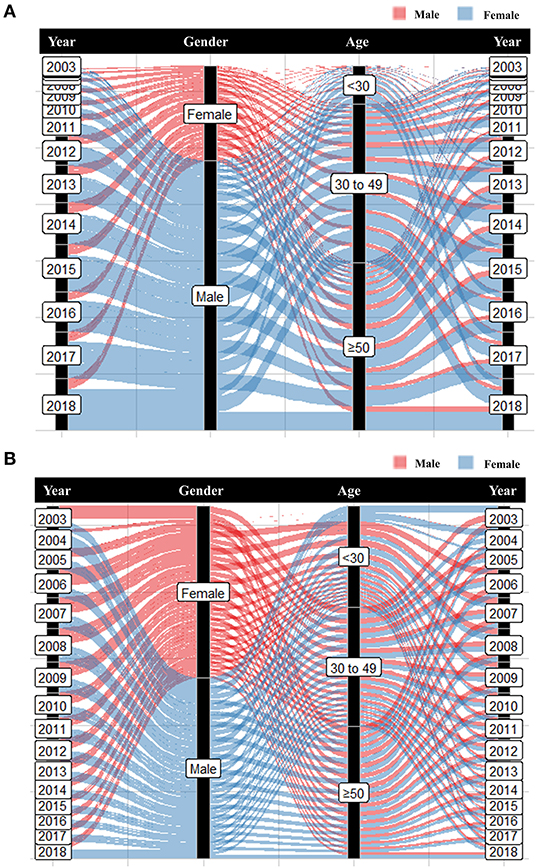
Figure 4. The distribution of advanced HIV disease in age and gender in Hunan Province from 2003 to 2018. (A) The number of advanced HIV disease from 2003 to 2018; (B) Proportions of advanced HIV disease from 2003 to 2018.
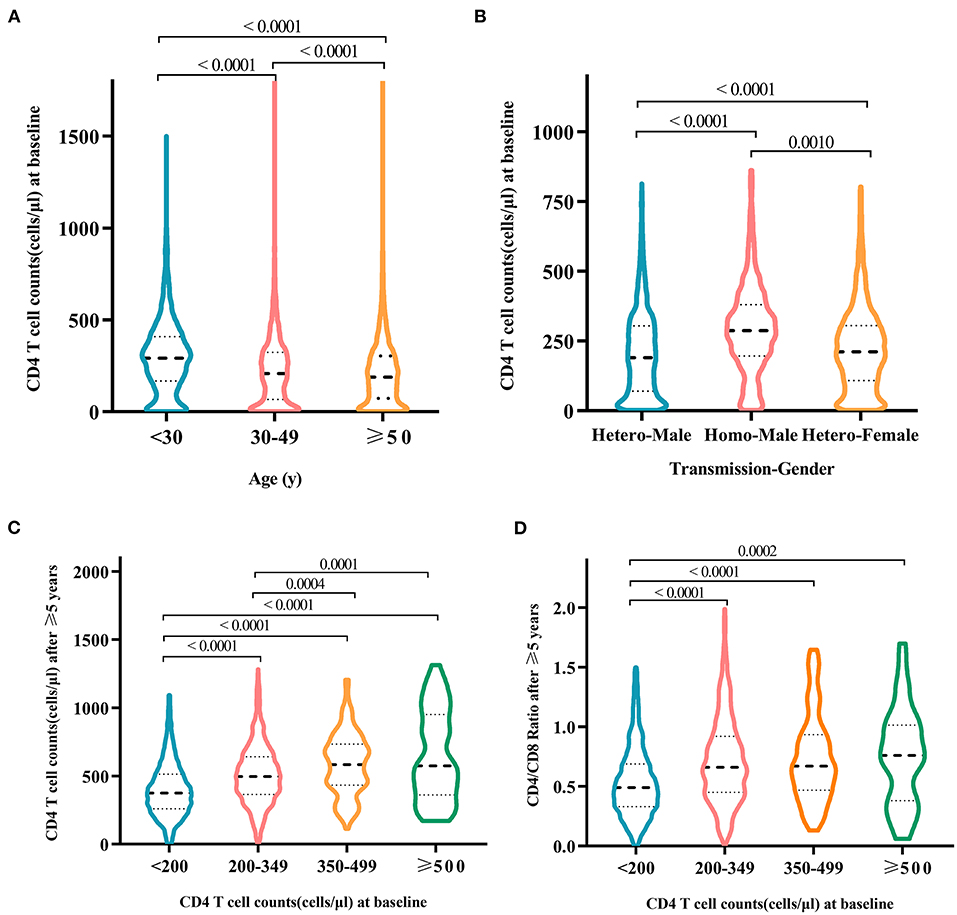
Figure 5. Differences in baseline CD4+ T-cell counts among HIV-infected patients at different ages (A) and patients of different genders infected by different transmission routes (B). After treatment for more than 5 years, patients with different baseline CD4 counts were diagnosed with the follow-up of CD4 counts (C) and CD4/CD8 ratio (D). Only statistically significant groups were labeled.
After laboratory-confirmed diagnosis, HIV-positive patients received antiviral treatment with regular follow-up of CD4 counts every 6 months. First, CD4 counts increased significantly by comparing serum levels before treatment initiation and after 6-month treatment (252.9 vs. 349.1 cells/μl, p-value < 0.0001). Second, an average increase in CD4 levels of 105.5 cells/μl was observed among those patients who received treatment for 0.5–1 year. A significant increase in CD4 counts (452.2 cells/μl) was also observed among those patients treated for >5 years (Table 3). Third, higher levels of CD4 counts at baseline were associated with a higher increase in CD4 counts (Figure 5C) and CD4/CD8 ratio (Figure 5D; Supplementary Table S3). After >5 years of treatment, except for the patient group with baseline CD4 levels below 200 cells/μl, CD4 counts in other groups reached >500 cells/μl (Figure 5C). Those patients with baseline CD4 levels >200 cells/μl experienced the recovery of the CD4/CD8 ratio to 0.75 after >5 years of antiviral treatment (Figure 5D).
Survival Time of HIV-Infected Patients Under ART
In our cohort of 34,297 HIV-infected patients, 24,420 (71.2%) patients were under treatment, 4,411 (12.9%) died, and 3,917 (11.4%) were lost to follow-up. Analysis of 4,411 deaths revealed AIDS-related illnesses (2,516, 57.0%), accidental deaths (341, 7.7%), suicides (143, 3.2%), or other causes (1,240, 28.1%) (Table 1). The highest proportion of deaths occurred in patients aged >50 years (Figure 6A).
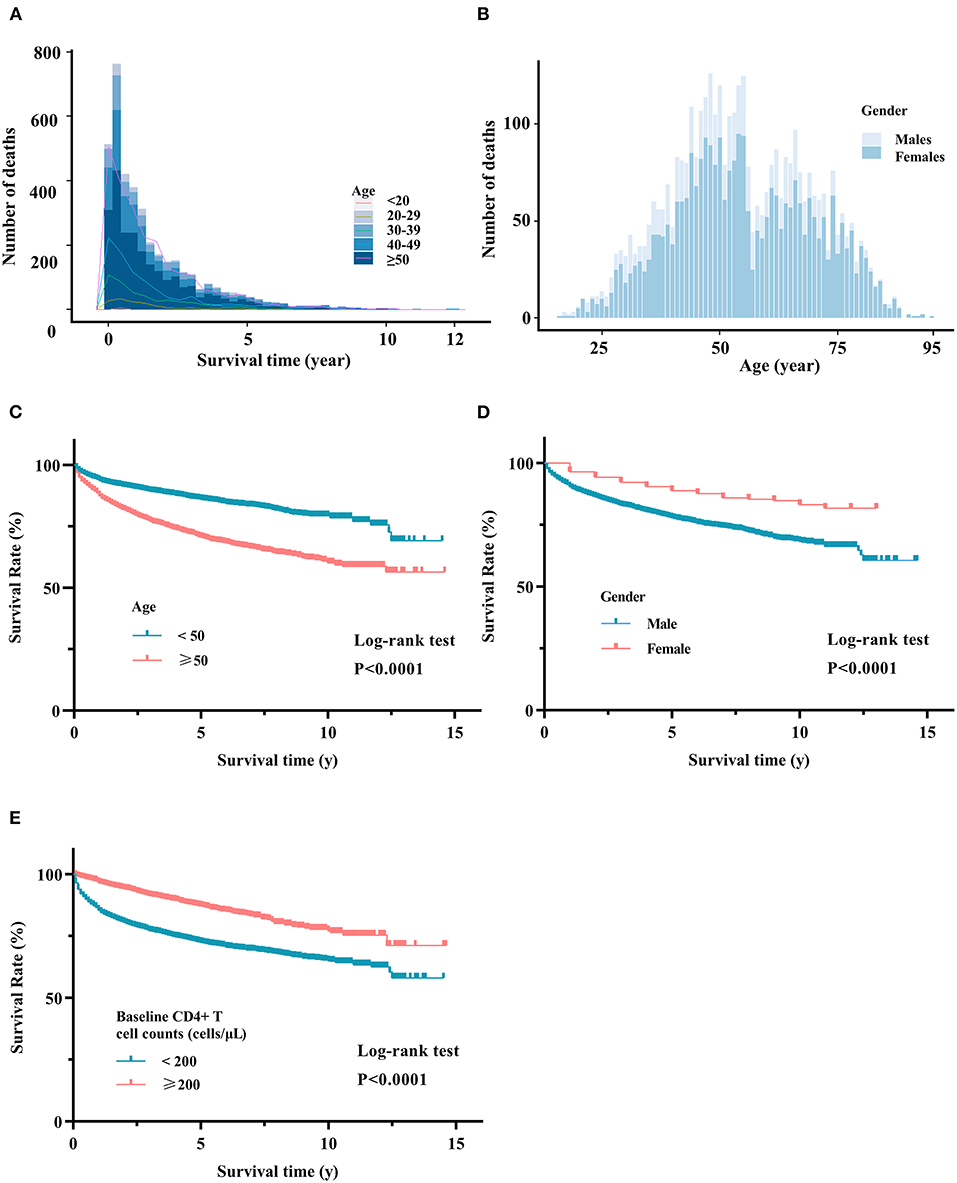
Figure 6. Survival analysis of HIV-associated death. (A) Distribution of HIV-associated death in different age groups. (B) Distribution of HIV-associated death in males and females. Kaplan-Meier curves in different age groups (C), gender groups (D), and baseline CD4 groups (E). Log-rank tests were used to measure the statistical difference.
Our survival analyses revealed the survival rate of HIV-infected patients categorized by gender, age, region, transmission route, and baseline CD4 levels (Figures 6C–E). The overall 10-year survival rate was estimated to be 70.0%. The estimated 10-year survival rate was significantly higher in females vs. males (75.9 vs. 67.1%, p-value < 0.0001), patients <50 vs. ≥50 years (78.4 vs. 59.0%, p-value < 0.0001), and patients with baseline CD4 level >200 cells/μl vs. <200 cells/μl (76.9 vs. 63.2%, p-value < 0.0001) (Supplementary Table S6). As shown in Figure 7, our subgroup analyses revealed that the 10-year survival rate was significantly lower in older males (55%) than in young males (77%) and young females (81%). A low 10-year survival rate of 55% was also found in older patients with baseline CD4 levels <200 cells/μl.
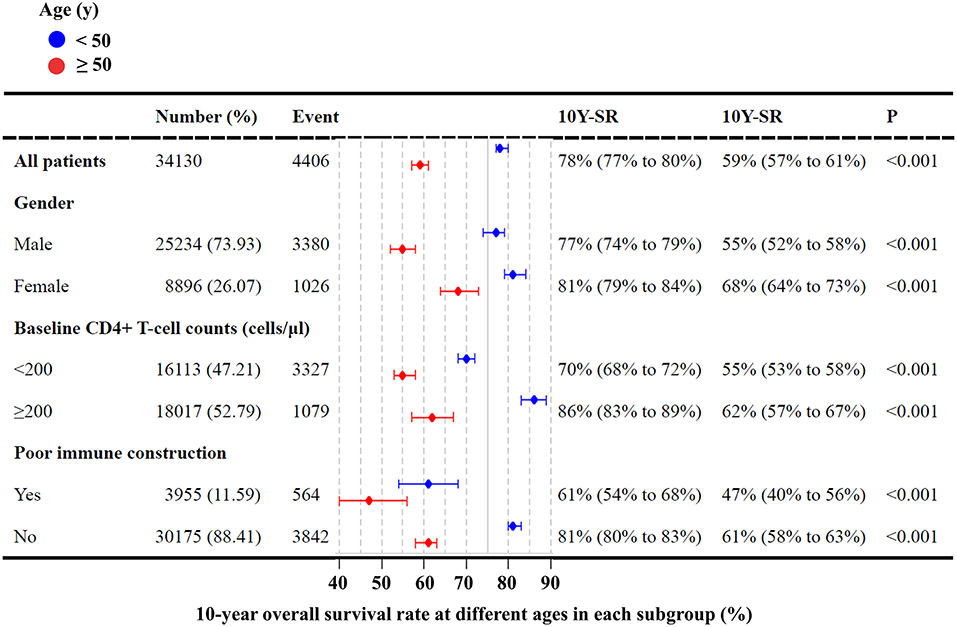
Figure 7. Survival rates of HIV-infected patients in different groups. 10Y-SR indicates the 10-year survival rate.
Discussion
Based on a large-scale cohort of 34,297 HIV-infected patients, our study presents the first survey of HIV infections (2003–2018) in Hunan province. Compared with other provinces in China, the HIV epidemic in Hunan province is not considered severe (30). Although there seems a growing number of HIV incidences, the overall growth rate in Hunan province has slowed down in recent years, implying the effectiveness of HIV prevention and control strategies. Most HIV infections in Hunan province are diagnosed in male patients, in agreement with other studies conducted from other provinces in China (27, 31). Our study finds that the majority of HIV infections in Hunan province are elderly patients aged ≥50 years, which is agreement with other national surveys (32–34). However, young males are considered the key population for HIV prevention given the increasing proportion of homosexual transmission. Although the mortality rate in young patients aged <30 years was relatively low, a significant increase in HIV infections can be traced to young populations, especially those high school and college students (21, 35).
Due to the long incubation period from HIV infection to the onset of AIDS and related symptoms, early HIV diagnosis remains difficult in the absence of routine screening (17). Our study showed that the proportion of HIV-infected patients with CD4+ T cell counts < 200 cells/μl at baseline was 42.8% in 2018 in Hunan Province, which was relatively higher than that in other regions (36, 37). In response to the national prevention strategies, free HIV testing services are currently available in Hunan to reduce the risk of advanced HIV disease. Early intervention, early detection, early control, and early treatment are strongly advocated in China, leading to better management of HIV infections in the future.
We observed a dynamic change in HIV transmission routes in the past decade. Before 2005, blood transmission and intravenous drug use are the main routes of transmission in China (16). To date, sexual transmission has become the predominant route of HIV transmission (22). Nevertheless, there is a growing trend of homosexual transmission across the country (25). In agreement with previous studies (22, 25), we found that homosexual transmission was more likely to occur in young males in Hunan province. We also observed a higher level of baseline CD4+ T-cell counts in male patients infected by homosexual transmission than those infected by heterosexual transmission, as well as a better immune outcome and a lower risk of deaths after ART. The possible reasons might be explained by the large proportion of young patients infected through homosexual transmission, and the proliferation of HIV drug resistance strains might be associated with transmission routes (38–44). For effective HIV prevention in China, more efforts are still needed to control both heterosexual and homosexual transmissions among high-risk populations.
Our study observed a difference in the case fatality rate among five geographical regions in Hunan province (Figure 3). The number of HIV infections was most in Southern Hunan, but the HIV-associated fatality rate was the highest in Western Hunan. This regional disparity might be explained by several reasons. (i) Economic and medical conditions are discrepant in different regions. (ii) Social stigma in different regions may play a role in HIV prevention and treatment. A recent study found that college students with higher education levels still hold negative attitudes toward HIV-infected patients (45). Previous studies suggest that HIV-related stigma and lack of social support have the potential to harm the health and wellbeing of HIV-infected patients (46, 47). (iii) HIV is known for its high genetic diversity (48), and the distribution of circulating HIV subtypes and strains exhibit regional differences (49–52). Further studies need to address the impact of diversified anti-HIV strategies and HIV strains on HIV prevention and treatment in different regions.
It is known that wide applications of HIV prevention and treatment strategies have reduced HIV-associated mortality and morbidity, not only in China but also in many other countries (53). We estimated 70.0% of the overall 10-year survival rate of treated patients using a large-scale cohort in Hunan province. Compared with other patient groups, elderly males in Western Hunan had a lower survival rate (Figure 6). It is known that HIV infection can impair the human immune system (54), and the elderly are more vulnerable to infectious diseases because aging can affect the innate and adaptive immune system (55). As expected, we observed an age-related decrease in CD4 levels at baseline. In agreement with previous studies (56, 57), we found that baseline CD4 levels were associated with the recovery of CD4 levels and CD4/CD8 after ART. Furthermore, elderly patients are unlikely to achieve the same virological and immune responses as young patients, probably due to the low CD4 levels at baseline and relatively poor immune function (58).
There are limitations to our study. First, our database included the majority (>70%) of laboratory-confirmed HIV-infected patients in Hunan province, but this official database does not include undiagnosed cases or those immigrant patients who were not designated to local health facilities in Hunan province. Second, our database only included HIV-associated factors, but not other factors such as ethnicity, occupation, degree of education, marital status, or traveling history. Therefore, our analysis cannot address all potential risk factors associated with HIV prevention and treatment. Third, our retrospective study could not reveal clinical efficacies of ART because HIV-infected patients were not randomized and treatment switch is often considered at different timepoints in clinical practice. Fourth, our study only focused on HIV epidemiology in Hunan Province, and future studies need to report HIV epidemiology from a global perspective.
Conclusion
This study reveals epidemiological and clinical characteristics of HIV-infected patients in Hunan province, shedding light on the focus of HIV prevention and treatment in certain high-risk populations and geographical regions. Although the overall growth rate of new HIV cases slows down in Hunan province, a special focus should be taken on elderly males who were infected mainly by heterosexually transmission. Furthermore, a high proportion of advanced HIV disease indicates the importance of HIV routine testing and surveillance. Better management strategies are still needed to effectively control the spread of HIV infections from a regional and global perspective.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available after the approval of the Ethics Committees.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committees of The First Hospital of Changsha (Approval ID: 202160). Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author Contributions
TY performed statistical analyses and drafted the manuscript. PZ, TYH, and ED contributed with data interpretation and discussions of the manuscript. JH, JZ, and FZ performed data acquisition. XYH and FZ supervised the study. GL obtained funding and revised the manuscript. All authors contributed to the final article. All authors contributed to the article and approved the submitted version.
Funding
This research was funded by the National Nature Science Foundation of China (31871324, 81730064, and 31571368), and the National Science and Technology Major Project (2018ZX10715004). The funders had no role in the study design, data collection, data analysis, data interpretation, or writing of the report.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We appreciate the Hunan Center for Disease Control and Prevention and the First Hospital of Changsha to support the data and the technical guidance.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.902537/full#supplementary-material
Abbreviations
AIDS, Acquired immune deficiency syndrome; AAPC, Annual percentage changes; APC, Annual percentage changes; ART, Antiretroviral therapies; HIV, Human immunodeficiency virus; INI, Integrase inhibitor; MSM, Men who sex with men; NFATP, The National Free Antiretroviral Treatment Program; NNRTIs, Non-Nucleoside reverse transcriptase inhibitors; NRTI, Nucleoside reverse transcriptase inhibitor.
References
1. Pino M, Paiardini M, Marconi VC. Progress in achieving long-term HIV remission. Curr Opin HIV AIDS. (2018) 13:435–45. doi: 10.1097/COH.0000000000000487
2. Deeks SG, Overbaugh J, Phillips A, Buchbinder S. HIV infection. Nat Rev Dis Primers. (2015) 1:15035. doi: 10.1038/nrdp.2015.35
3. Li G, Wang Y, De Clercq E. Approved HIV reverse transcriptase inhibitors in the past decade. Acta Pharmaceutica Sinica B. (2022) 14:1567–90. doi: 10.1016/j.apsb.2021.11.009
4. Mocroft A, Ledergerber B, Katlama C, Kirk O, Reiss P, d'Arminio Monforte A, et al. Decline in the AIDS and death rates in the EuroSIDA study: an observational study. Lancet. (2003) 362:22–9. doi: 10.1016/S0140-6736(03)13802-0
5. Sabin CA. Do people with HIV infection have a normal life expectancy in the era of combination antiretroviral therapy? BMC Med. (2013) 11:251. doi: 10.1186/1741-7015-11-251
6. Cooper DA. Life and death in the cART era. Lancet. (2008) 372:266–7. doi: 10.1016/S0140-6736(08)61086-7
7. De Clercq E, Li G. Approved antiviral drugs over the past 50 years. Clin Microbiol Rev. (2016) 29:695–747. doi: 10.1128/CMR.00102-15
8. Li G, De Clercq E. HIV genome-wide protein associations: a review of 30 years of research. Microbiol Mol Biol Rev. (2016) 80:679–731. doi: 10.1128/MMBR.00065-15
9. Wang Y, De Clercq E, Li G. Current and emerging non-nucleoside reverse transcriptase inhibitors (NNRTIs) for HIV-1 treatment. Expert Opin Drug Metab Toxicol. (2019) 15:813–29. doi: 10.1080/17425255.2019.1673367
10. Pace M, Frater J. A cure for HIV: is it in sight? Expert Rev Anti Infect Ther. (2014) 12:783–91. doi: 10.1586/14787210.2014.910112
11. Wu Z, Sullivan SG, Wang Y, Rotheram-Borus MJ, Detels R. Evolution of China's response to HIV/AIDS. Lancet. (2007) 369:679–90. doi: 10.1016/S0140-6736(07)60315-8
12. Xu B, Li J, Wang M. Epidemiological and time series analysis on the incidence and death of AIDS and HIV in China. BMC Public Health. (2020) 20:1906. doi: 10.1186/s12889-020-09977-8
13. Jiang Y, Dou X, Yan C, Wan L, Liu H, Li M, et al. Epidemiological characteristics and trends of notifiable infectious diseases in China from 1986 to 2016. J Glob Health. (2020) 10:020803. doi: 10.7189/jogh.10.020803
14. Chen H, Wu X, Chen L, Lu H, Tang Z, Shen Z, et al. Rapidly spreading human immunodeficiency virus epidemic among older males and associated factors: a large-scale prospective cohort study in rural Southwest China. Sex Transm Dis. (2019) 46:234–9. doi: 10.1097/OLQ.0000000000000957
15. Shao Y. AIDS epidemic at age 25 and control efforts in China. Retrovirology. (2006) 3:87. doi: 10.1186/1742-4690-3-87
16. Ding Y, Ma Z, He J, Xu X, Qiao S, Xu L, et al. Evolving HIV Epidemiology in Mainland China: 2009-2018. Curr HIV/AIDS Rep. (2019) 16:423–30. doi: 10.1007/s11904-019-00468-z
17. Cao W, Hsieh E, Li T. Optimizing treatment for adults with HIV/AIDS in China: successes over two decades and remaining challenges. Curr HIV/AIDS Rep. (2020) 17:26–34. doi: 10.1007/s11904-019-00478-x
18. Wu Z, Wang Y. Introduction: China meets new AIDS challenges. J Acquir Immune Defic Syndr. (2010) 53 Suppl 1:S1–3. doi: 10.1097/QAI.0b013e3181c7d379
19. Burki T. HIV in China: a changing epidemic. Lancet Infect Dis. (2018) 18:1311–2. doi: 10.1016/S1473-3099(18)30680-7
20. Wang LY, Qin QQ, Ge L, Ding ZW, Cai C, Guo W, et al. Characteristics of HIV infections among over 50-year-olds population in China. Zhonghua Liu Xing Bing Xue Za Zhi. (2016) 37:222–6. doi: 10.3760/cma.j.issn.0254-6450.2016.02.015
21. Li G, Jiang Y, Zhang L. HIV upsurge in China's students. Science. (2019) 364:711. doi: 10.1126/science.aay0799
22. Wu ZY. Characteristics of HIV sexually transmission and challenges for controlling the epidemic in China. Zhonghua Liu Xing Bing Xue Za Zhi. (2018) 39:707–9. doi: 10.3760/cma.j.issn.0254-6450.2018.06.002
23. He N, Detels R. The HIV epidemic in China: history, response, and challenge. Cell Res. (2005) 15:825–32. doi: 10.1038/sj.cr.7290354
24. Yang HT, Tang W, Xiao ZP, Jiang N, Mahapatra T, Huan XP, et al. Worsening epidemic of HIV and syphilis among men who have sex with men in Jiangsu Province, China. Clin Infect Dis. (2014) 58:1753–9. doi: 10.1093/cid/ciu175
25. Dong MJ, Peng B, Liu ZF, Ye QN, Liu H, Lu XL, et al. The prevalence of HIV among MSM in China: a large-scale systematic analysis. BMC Infect Dis. (2019) 19:1000. doi: 10.1186/s12879-019-4559-1
26. Shao B, Li Y, Yu L, Wang K, Chang M, Wang B, et al. The HIV/AIDS epidemic characteristics in a northeast province of China–men who have sex with men have made a tremendous contribution to the growth of the HIV epidemic. J Infect. (2014) 68:273–80. doi: 10.1016/j.jinf.2013.10.014
27. Yan Y, Wu S, Chen L, Yan P, Qiu Y, Xie M, et al. Shift in HIV/AIDS Epidemic in Southeastern China: a longitudinal study from 1987 to 2015. Int J Environ Res Public Health. (2016) 13:794. doi: 10.3390/ijerph13080794
28. TEAM W. Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating Preventing HIV Infection. (2016). Available online at: https://www.who.int/publications/i/item/97892415496842016
29. Yang X, Su B, Zhang X, Liu Y, Wu H, Zhang T. Incomplete immune reconstitution in HIV/AIDS patients on antiretroviral therapy: challenges of immunological non-responders. J Leukoc Biol. (2020) 107:597–612. doi: 10.1002/JLB.4MR1019-189R
30. Qiao YC, Xu Y, Jiang DX, Wang X, Wang F, Yang J, et al. Epidemiological analyses of regional and age differences of HIV/AIDS prevalence in China, 2004-2016. Int J Infect Dis. (2019) 81:215–20. doi: 10.1016/j.ijid.2019.02.016
31. Lu Z, Ji W, Yin Y, Jin X, Wang L, Li Z, et al. Analysis on the trend of AIDS incidence in Zhejiang, China based on the age-period-cohort model (2004-2018). BMC Public Health. (2021) 21:1077. doi: 10.1186/s12889-021-11050-x
32. Xing J, Li YG, Tang W, Guo W, Ding Z, Ding G, et al. HIV/AIDS epidemic among older adults in China during 2005-2012: results from trend and spatial analysis. Clin Infect Dis. (2014) 59:e53–60. doi: 10.1093/cid/ciu214
33. Chen H, Luo L, Pan SW, Lan G, Zhu Q, Li J, et al. HIV epidemiology and prevention in Southwestern China: trends from 1996-2017. Curr HIV Res. (2019) 17:85–93. doi: 10.2174/1570162X17666190703163838
34. Ma Y, Cui Y, Hu Q, Mubarik S, Yang D, Jiang Y, et al. Long-term changes of HIV/AIDS incidence rate in China and the U.S. population from 1994 to 2019: a join-point and age-period-cohort analysis. Front Public Health. (2021) 9:652868. doi: 10.3389/fpubh.2021.652868
35. Li Y, Xu J, Reilly KH, Zhang J, Wei H, Jiang Y, et al. Prevalence of HIV and syphilis infection among high school and college student MSM in China: a systematic review and meta-analysis. PLoS ONE. (2013) 8:e69137. doi: 10.1371/journal.pone.0069137
36. Xie J, Hsieh E, Sun MQ, Wang HL, Lv W, Fan HW, et al. Delays in HIV diagnosis and associated factors among patients presenting with advanced disease at a tertiary care hospital in Beijing, China. PLoS ONE. (2017) 12:e0182335. doi: 10.1371/journal.pone.0182335
37. Tang H, Mao Y, Tang W, Han J, Xu J, Li J. “Late for testing, early for antiretroviral therapy, less likely to die”: results from a large HIV cohort study in China, 2006-2014. BMC Infect Dis. (2018) 18:272. doi: 10.1186/s12879-018-3158-x
38. Zhang L, Wang YJ, Wang BX, Yan JW, Wan YN, Wang J. Prevalence of HIV-1 subtypes among men who have sex with men in China: a systematic review. Int J STD AIDS. (2015) 26:291–305. doi: 10.1177/0956462414543841
39. Lu X, Zhao C, Wang W, Nie C, Zhang Y, Zhao H, et al. HIV-1 genetic diversity and its distribution characteristics among newly diagnosed HIV-1 individuals in Hebei province, China. AIDS Res Ther. (2016) 13:3. doi: 10.1186/s12981-015-0087-2
40. Jiang Y, Zhang L, Hou Z, Tu A, Qiao R, Dai C, et al. Prevalence of different genotypes of HIV-1 in injection drug users in china: a systematic review and meta-analysis. Curr HIV Res. (2019) 17:240–57. doi: 10.2174/1570162X17666190919115036
41. Xiao P, Zhou Y, Lu J, Yan L, Xu X, Hu H, et al. HIV-1 genotype diversity and distribution characteristics among heterosexually transmitted population in Jiangsu province, China. Virol J. (2019) 16:51. doi: 10.1186/s12985-019-1162-4
42. Zhang Y, Lu L, Ba L, Liu L, Yang L, Jia M, et al. Dominance of HIV-1 subtype CRF01_AE in sexually acquired cases leads to a new epidemic in Yunnan province of China. PLoS Med. (2006) 3:e443. doi: 10.1371/journal.pmed.0030443
43. Zhao B, Han X, Xu J, Hu Q, Chu Z, Zhang J, et al. Increase of RT-related transmitted drug resistance in non-CRF01_AE among HIV type 1-infected men who have sex with men in the 7 cities of China. J Acquir Immune Defic Syndr. (2015) 68:250–5. doi: 10.1097/QAI.0000000000000467
44. Rahman M, Rahman S, Reza MM, Khan SI, Sarker MS. HIV-1 drug resistance and genotypes circulating among HIV-positive key populations in Bangladesh: 2016 update. Int J Infect Dis. (2021) 104:150–8. doi: 10.1016/j.ijid.2020.12.037
45. Zhang L, Yu H, Luo H, Rong W, Meng X, Du X, et al. HIV/AIDS-related knowledge and attitudes among Chinese college students and associated factors: a cross-sectional study. Front Public Health. (2022) 9:804626. doi: 10.3389/fpubh.2021.804626
46. Zhang YX, Golin CE, Bu J, Emrick CB, Nan Z, Li MQ. Coping strategies for HIV-related stigma in Liuzhou, China. AIDS Behav. (2014) 18(Suppl. 2):S212–20. doi: 10.1007/s10461-013-0662-2
47. Jin C, Zhao G, Zhang F, Feng L, Wu N. The psychological status of HIV-positive people and their psychosocial experiences in eastern China. HIV Med. (2010) 11:253–9. doi: 10.1111/j.1468-1293.2009.00770.x
48. Li G, Piampongsant S, Faria NR, Voet A, Pineda-Pena AC, Khouri R, et al. An integrated map of HIV genome-wide variation from a population perspective. Retrovirology. (2015) 12:18. doi: 10.1186/s12977-015-0148-6
49. Xiao P, Li J, Fu G, Zhou Y, Huan X, Yang H. Geographic distribution and temporal trends of HIV-1 subtypes through heterosexual transmission in China: a systematic review and meta-analysis. Int J Environ Res Public Health. (2017) 14:830. doi: 10.3390/ijerph14070830
50. Yuan R, Cheng H, Chen LS, Zhang X, Wang B. Prevalence of different HIV-1 subtypes in sexual transmission in China: a systematic review and meta-analysis. Epidemiol Infect. (2016) 144:2144–53. doi: 10.1017/S0950268816000212
51. Vrancken B, Zhao B, Li X, Han X, Liu H, Zhao J, et al. Comparative circulation dynamics of the five main HIV types in China. J Virol. (2020) 94:e00683–20. doi: 10.1128/JVI.00683-20
52. Yuan D, Yu B, Li Y, Wang Z, Liu M, Ye L, et al. Prevalence and molecular epidemiology of transmitted drug resistance and genetic transmission networks among newly diagnosed people living with HIV/AIDS in a minority Area, China. Front Public Health. (2021) 9:731280. doi: 10.3389/fpubh.2021.731280
53. Danforth K, Granich R, Wiedeman D, Baxi S, Padian N. Global mortality and morbidity of HIV/AIDS. In: Holmes KK, Bertozzi S, Bloom BR, Jha P, editors. Major Infectious Diseases. Washington. DC (2017).
54. Moir S, Chun TW, Fauci AS. Pathogenic mechanisms of HIV disease. Annu Rev Pathol. (2011) 6:223–48. doi: 10.1146/annurev-pathol-011110-130254
55. Justice JN, Gubbi S, Kulkarni AS, Bartley JM, Kuchel GA, Barzilai N, et al. geroscience perspective on immune resilience and infectious diseases: a potential case for metformin. Geroscience. (2021) 43:1093–112. doi: 10.1007/s11357-020-00261-6
56. Ceccherini-Silberstein F, Cozzi Lepri A, Alteri C, Merlini E, Surdo M, Marchetti G, et al. Pre-ART HIV-1 DNA in CD4+ T cells correlates with baseline viro-immunological status and outcome in patients under first-line ART. J Antimicrob Chemother. (2018) 73:3460–70. doi: 10.1093/jac/dky350
57. Cobre AF, Pedro CAA, Fachi MM, Vilhena RO, Marson BM, Nicobue V, et al. Five-year survival analysis and predictors of death in HIV-positive serology patients attending the Military Hospital of Nampula, Mozambique. AIDS Care. (2020) 32:1379–87. doi: 10.1080/09540121.2020.1761938
Keywords: HIV, epidemiology, elderly males, heterosexual transmission, HIV-associated fatality
Citation: Yue T, Zhang P, Hao Y, He J, Zheng J, De Clercq E, Li G, Huang Y and Zheng F (2022) Epidemiology and Clinical Outcomes of HIV Infection in South-Central China: A Retrospective Study From 2003 to 2018. Front. Public Health 10:902537. doi: 10.3389/fpubh.2022.902537
Received: 23 March 2022; Accepted: 09 May 2022;
Published: 09 June 2022.
Edited by:
Francisco Antunes, Universidade de Lisboa, PortugalReviewed by:
Massimiliano Lanzafame, Santa Chiara Hospital, ItalyHonghong Wang, Central South University, China
Copyright © 2022 Yue, Zhang, Hao, He, Zheng, De Clercq, Li, Huang and Zheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Guangdi Li, bGlndWFuZ2RpLnJlc2VhcmNoQGdtYWlsLmNvbQ==; Yaxiong Huang, MzE0NjI1NzE3QHFxLmNvbQ==; Fang Zheng, emhlbmdmODQ4MkAxNjMuY29t
 Tingting Yue1
Tingting Yue1 Yuantao Hao
Yuantao Hao Erik De Clercq
Erik De Clercq Guangdi Li
Guangdi Li Yaxiong Huang
Yaxiong Huang Fang Zheng
Fang Zheng