
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 25 April 2022
Sec. Public Health Education and Promotion
Volume 10 - 2022 | https://doi.org/10.3389/fpubh.2022.890773
This article is part of the Research TopicAn Insight into University Medical and Health Science CoursesView all 15 articles
Background: Virtual simulation has been widely used in nursing education and nursing training. This study aims to characterize the publications in terms of countries, institutions, journals, authors, collaboration relationships, and analyze the trends of virtual simulation in nursing research.
Methods: Publications regarding virtual simulation in nursing were retrieved from Web of Science core collection. Microsoft Excel 2010, VOSviewer were used to characterize the contributions of the authors, journals, institutions, and countries. The trends, hot-spots and knowledge network were analyzed by Citespace and VOSviewer.
Results: We identified 677 papers between 1999 and 2021. The number of publications grew slowly until 2019, after that, it got a sharp increase in 2020 and 2021. The USA, Canada and Australia were three key contributors to this field. Centennial College and University of San Paulo, University of Ottawa and Ryerson University were top major institutions with a larger number of publications. Verkuyl M was the most productive and highest cited author. Clinical Simulation in Nursing, Nurse Education Today, Journal of Nursing Education were the three productive journals. The foundational themes of virtual simulation research in nursing are “virtual learning during COVID-19, clinical nursing care, education in nurse practitioners, education technology”.
Conclusion: Virtual simulation in nursing field has attracted considerable attention during COVID-19 pandemic. The research hotspot is gradually shifting from clinical nursing care to studies of nursing education using different virtual simulation technologies
Virtual simulation (VS) is defined by a kind of computer simulation systems involving real people operating simulated systems, it could provide immersive, highly visual, 3D characteristics that allow the users to explore the role and changes within a seemingly real or physical world (1). Generally, it included three technologies [e.g., virtual reality (VR), augmented reality (AR), and mixed reality (MR)] (2, 3). In the last decades, with the adoption, application, and maturity of these technologies, nursing educators have increasingly used VS for nursing education and clinical training. For example, Girao et al. (4) developed a serious virtual reality game for medication preparation and administration training. Weston and Zauche (5) conducted a virtual simulation with clinical practice for pediatric nursing students. Chao et al. (6) applied the immersive three-dimensional interactive video program to help nursing students better acquire nasogastric tube feeding skills. Compared to traditional teaching approaches, VS has the advantage of minimal requirement of medical equipments or consumables. What's more, the sense of immersion is enhanced by wearable displays, interactivity, and haptic devices. And users can practice it anywhere and anytime as long as the device is available (1). In 2018, Tiffany and Forneris (7) forecast that the adoption of VR in nursing education will from the current 10% use to 45% in the next 5 years. Specifically, The COVID-19 (coronavirus disease) pandemic has spurred a transition from face-to-face teaching to virtual learning (5, 8). As a burgeoning area, more and more educators and policymakers prefer using VS to assist teaching. To this end, there is an urgent need to investigate the performance (e.g., primary contributors and highly cited articles) and scientific map (collaborations, research themes, and trends) to show the past, present, and future direction in this field.
Bibliometric analysis is widely accepted for reviewing big data of articles in a field or publications in a journal using quantitative techniques (9, 10). It usually applies bibliometric tools (e.g., Bibliometrix R, Gephi, Pajek, CiteSpace, Leximancer, and VOSviewer) to analyze the publication trend, the top articles, primary contributors, and major theme and frontier topics in a given field (11–13). There are several existing bibliometric analysis about nursing topics (14–16). However, no study focused on bibliometric analysis to provide a state-of-the-art review for VS research in nursing field. Therefore, in this study, we utilized the popular bibliometric tools, Citespace and Vosviewer (17, 18), to comprehensively analyze VS research in nursing based on the Web of Science Core Collection (WoSCC). We hope this paper will uncover the following research questions (RQ).
RQ1. What is the publication trend for virtual simulation research in nursing?
RQ2. Which are the most influential articles and primary contributing authors, institutions, countries, journals for virtual simulation research in nursing?
RQ3. What are the potential collaborators (author, institutions, countries/regions) for virtual simulation research in nursing?
RQ4. What are the major themes and frontier topics for virtual simulation research in nursing?
The aims of this study are as following: (1) to uncover the major contributors (e.g., countries, institutions, journals, authors, articles) in VS related to nursing research. (2) To analyze the co-operation relationships in this field. (3) To map the knowledge network and identify the frontier topics, and point the future directions in this field.
A descriptive bibliometric analysis of publications in virtual simulation related to nursing research.
The data in this research were retrieved from Web of Science database, so no participants were involved.
The advanced search was performed using Web of Science (Thomson Reuters, New York, USA) on March 15th, 2022. Formula: (((TS= (“virtual simulation” or “virtual realit*” or “virtual reality simulation” or “virtual learning” or “augmented realit*” or “mixed reality”) and TS= (“nurs*”)) AND DOP=(1999-01-01/2021-12-31)) AND DT=(Article OR Review)) AND LA=(English) was used to screen out publications associated with VS in nursing. Two team members (Qian Zhang and Jing Liu) searched and screened the database independently. Any discrepancies were resolved by discussion with Jia Chen until consensus was reached.
(1) Peer-reviewed articles involving VS related to nursing
(2) Original articles and review articles
(3) Written in English.
(4) Web of Science core collection (WoSCC).
(1) Unpublished papers
(2) Articles required a manual research.
The following bibliometric parameters were extracted, such as title, keywords, journal, publication year, citation counts, citations per paper, H-index, author, institution, country, and references. And then these data were imported into Microsoft Excel 2010 (Redmond, Washington, USA) to analyze the contributions of different countries, institutions, journals, and authors. VOSviewer (Leiden University, Leiden, the Netherlands) was applied to visualize the maps of coauthor-authorship, coauthor-institution, coauthor-country, co-citation references, and keywords co-occurrence. In the VOSviewer map, node size indicates the number of articles produced. The wider links between nodes means stronger cooperation strength. The color means the average publication year for the node. Blue represents the early and yellow represents the late. Citespce (Version 5.8. R1) was used to identify the keywords burst and co-cited references burst (18).
An initial research of the WoSCC identified 848 publications. After excluded meeting abstract, early access and limited English language, 677 articles were finally enrolled into analysis. Original article accounts for 86.1% of the total (n = 583) (Figure 1). These papers were published from 1999 to 2021. The timing of publication could be divided into three periods (Phase I, 1999–2008; Phase II, 2009–2019; Phase III, 2020–2021). 1999–2008, the number of articles per year was below 10 publications. 2009–2019, the annual output of this field has grown consistently to over 50 publications. The growth is evident since 2020, with more than 100 papers published each year (126 publications in 2020 and 217 publications in 2021). In other words, more than half of papers were published in these 2 years. The peak year was 2021 (n = 217) (Figure 2A). The total number of citations was 8885, with 13.1 citations per paper and 47 H-index. The annual year publications of the top 10 countries were shown in Figure 2B. The USA was the major contributor in this field, and almost leading this field since its inception.

Figure 1. Data screening flow chart. The literature search was performed on WoSCC and language limited to English, and steps of bibliometric analysis.
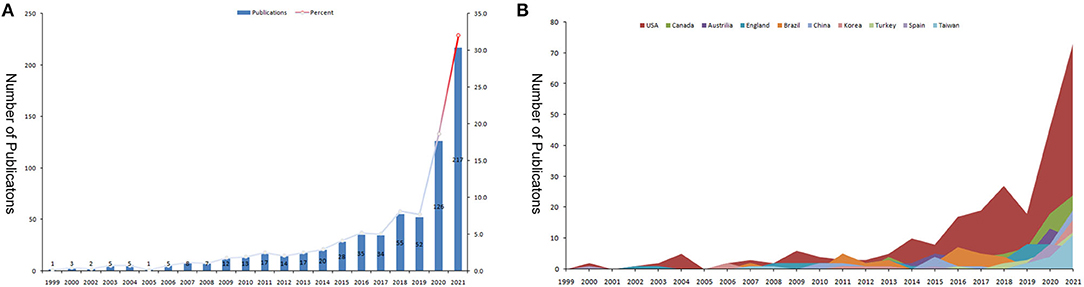
Figure 2. The number of publications and total citations related to virtual simulation in nursing studies. (A) The number of papers published and total citations each year. (B) The top 10 countries/regions annual publications.
The top 10 prolific authors in this area were all from North America (Table 1). Of them, there were nine from Canada, and one from the USA. They published 84 papers and accounted for 12.4% of the total papers. Verkuyl M. from Centennial College was the most productive author in this scope with 15 publications. Followed by Luctkar-flude M from Queens University and Tyerman J from University of Ottawa with 12 papers. In terms of co-cited authors, Verkuyl, M, Hoffman HG, and Foronda, Cl were ranked the first three. Supplementary Figure 1 showed the author cooperation network and co-cited author network. There were scattered co-operations between them, and authors who work together have strong citation ties.
The top 10 active and co-cited journals were identified by VOSviewer. Altogether, 269 journals contributed to VS in nursing. The top 10 most productive journals hosts 235 (34.7%) papers. Clinical Simulation in Nursing is the most productive journal (n = 89; 888 citations), followed by Nurse Education Today (n = 49; 584 citations), Journal of Nursing Education and Cin-Computers Informatics Nursing share the third position (n = 15). The top three co-cited journals were the same top three prolific journals, with 820, 667, 339 co-citations, respectively (Table 2).
The top 10 most productive institutions were presented in Figure 3A. Among the top 10 institutions, there were five located in Canada, three in the USA, and one in Australia, Brazil, respectively. Centennial College and University of San Paulo were the most prolific institution (n = 15 publications), followed by University of Ottawa and Ryerson University (n = 14). In terms of total citations and citations per paper, University of Toronto (Canada, 595 citations, 54 citations/paper), University of Queensland (Australia, 383 citations, 38.3 citations/paper), University of Washington (Canada, 266 citations, 24.2 citations/paper) ranked in the top three. The co-authorship for organization module in VOSviewer was used to visualize the collaboration relationship among 38 institutions, which published at least five papers. As shown in Figure 3B, There were few and sporadic connecting lines between different institutions.
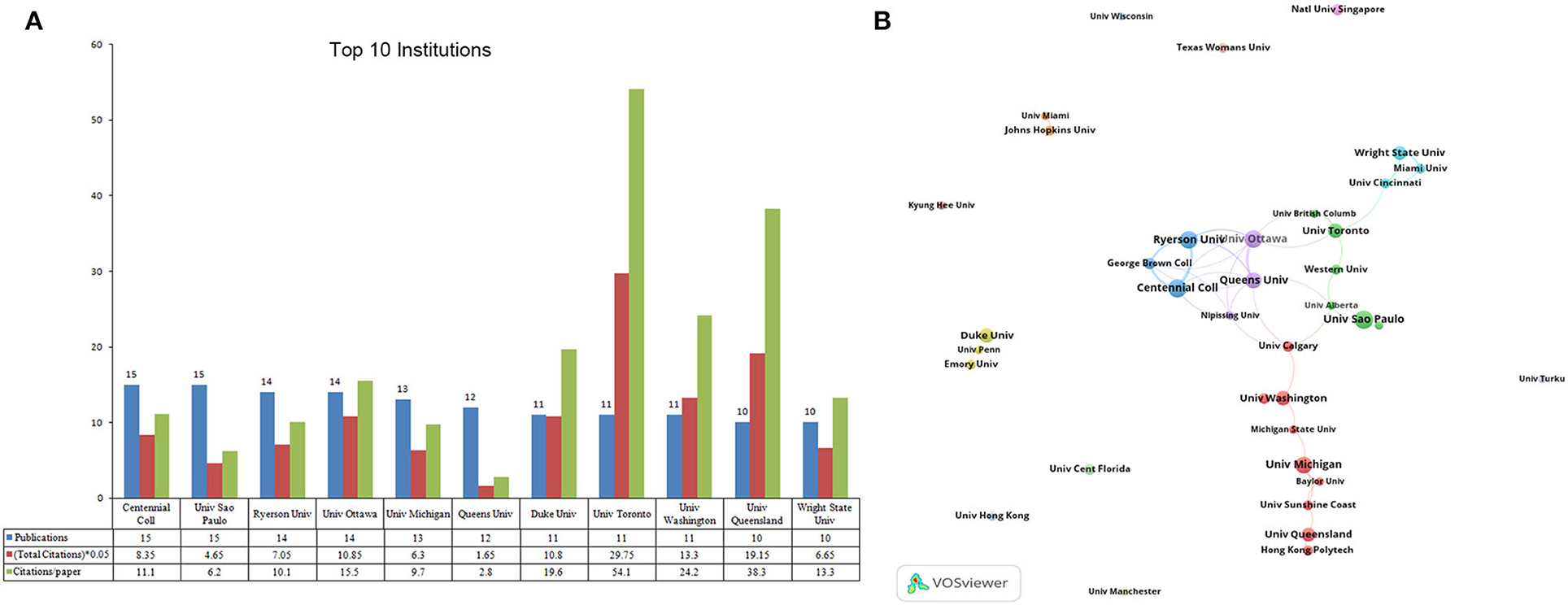
Figure 3. The top 10 most productive institutions and inter-institution co-operation relationships on virtual simulation in nursing research. (A) The number of publications, total citations, and citations per paper in top 10 institutions. (B) The co-authorship network visualization map of institution for virtual simulation in nursing research. Node size indicated the number of articles produced. The distance between any two nodes positively associated with the cooperation strength.
A total of 58 countries/regions participated in these publications. The top 10 were shown in Figure 4A. Obviously, the USA led in this field with 256 publications (37.8% of the total), followed by Canada (n = 73), Australia and England (n = 45). In terms of total citations, the USA ranked the first (4201), followed by Canada (1418) and England (816). In regard to citations per paper, Canada ranked first (19.4), followed by England (18.1) and the USA (16.4). The module of co-authorship for country in VOSviewer was used to map the countries' collaboration network. The smallest number of publications was settled as five, total link strength. Finally, 26 countries/regions meet our criterion. The USA, Canada, Australia, and England presented as the largest node. The strongest cooperation was between the USA and Canada and the USA and Australia (Figure 4B).
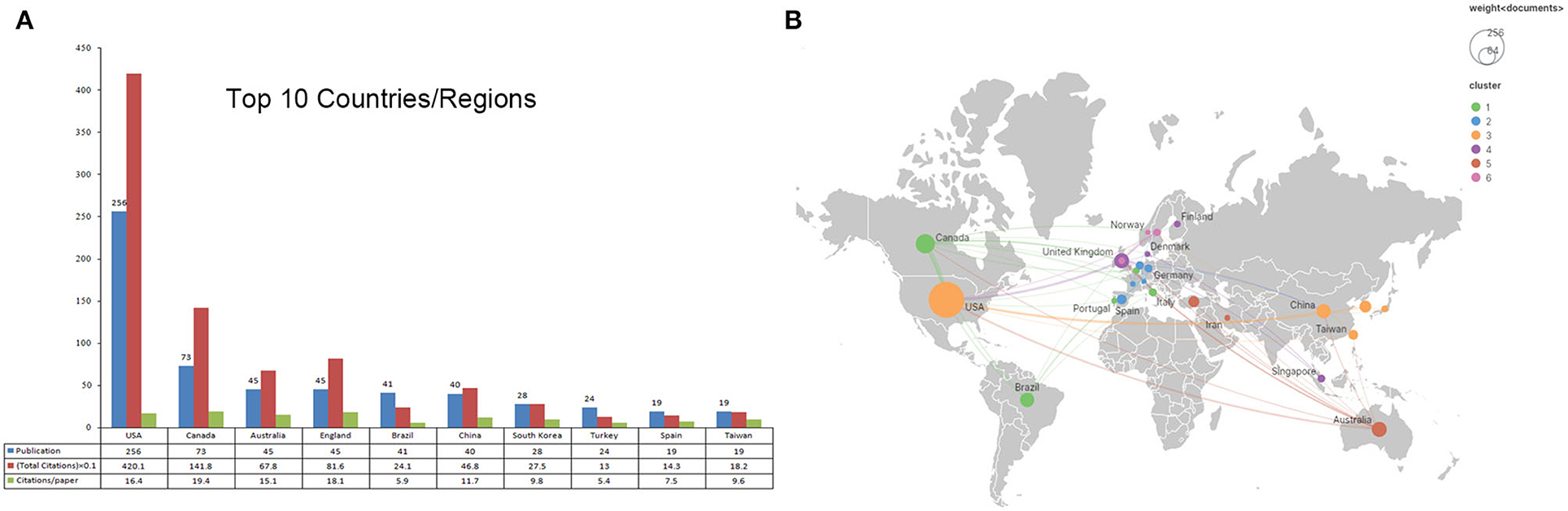
Figure 4. The top 10 prolific countries/regions and inter-national collaboration network on virtual simulation in nursing research. (A) The number of publications, total citations, and citations per paper in top 10 countries/regions. (B) The co-authorship network visualization map of countries for virtual simulation in nursing research. Node size indicated the number of articles produced. The distance between any two nodes positively associated with the cooperation strength. The color indicated the average publication year for the author, The blue color represented for early stage and yellow color represented late stage.
High-frequency keywords was usually used to describe hot-spots, and construct a knowledge map in a given field (19). We identified 1,540 keywords in total, 92 keywords occurred more than five times were enrolled into analysis. As shown in Figure 5A, the keywords were classified into nine clusters. The core keywords in the top five largest clusters, which ranked by the number of occurrences, are virtual reality (n = 183), simulation (n = 108), nurse education (n = 95), nursing (n = 92), virtual simulation (n = 88). As shown in Figure 5B, keywords were colored according to their average publication years. We observed although the concept of virtual simulation was built up early (colored by blue), there are lots of frontier topics spring up in recent years (colored by yellow), such as “nurse education, clinical simulation, augmented reality, and virtual learning”. Also, Citespace burst module was used to identify the research trends and shift of center topics in a given field (20). The burst duration was set to 2 years. The blue and red bar indicated infrequently and frequently cited time. The top 22 keywords with strongest citation bursts were identified and displayed in Figure 5C. Among them, virtual reality simulation has the highest burst strength (n = 4.8). The topics gradually shifted from “distress, cancer, model, and technology” to “education, quality, clinical simulation, and student”.
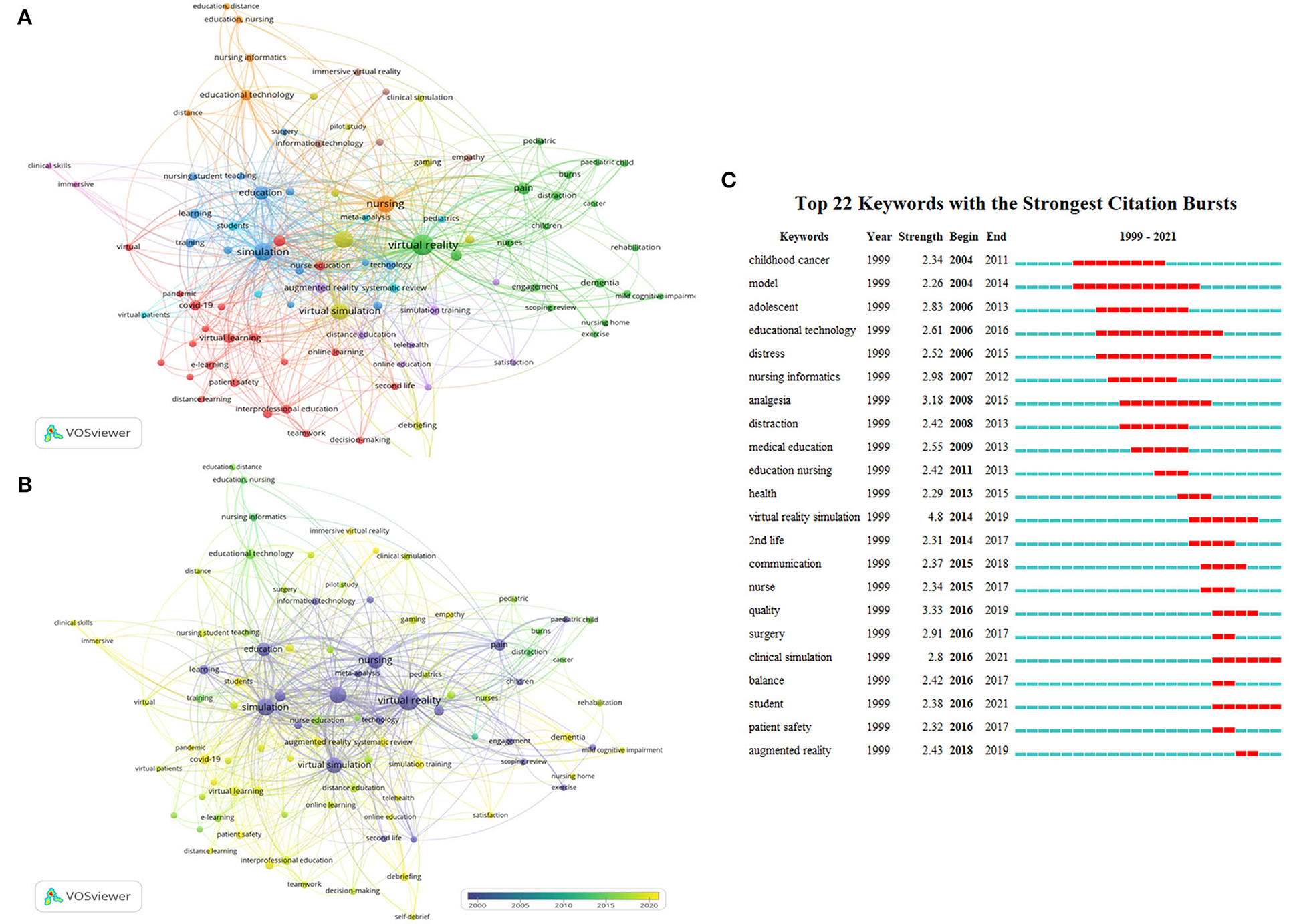
Figure 5. Analysis of keywords related to publications of virtual simulation in nursing field. (A) The co-occurrence network visualization map of keywords related to virtual simulation in nursing field. The keywords clustered into nine groups according to their color. Large nodes represented keywords with high frequency; (B) Keywords were colored according to the appearance for the average time. The blue color represented for early stage and yellow color represented late stage. (C) The top 22 keywords with the strongest citation bursts on virtual simulation in nursing field between 1999 and 2021. The red segment of the blue line denoted the burst duration of a keyword.
The top 10 most cited articles are listed in Table 3. The most cited article was produced by Gold et al. (21) published in Cyberpsychology and Behavior by 2006 with 174 citations, entitled Effectiveness of virtual reality for pediatric pain distraction during IV placement. In this study, the author reported virtual reality's positive efficacy and suitability as a pain relief tool during the pediatric intravenous placement. The co-cited reference is the article which cited by the included papers of VS in nursing, which formed the knowledge base in this field. The top16 co-cited references were identified through 20,249 references which co-cited more than 20 times by the included 677 papers. As shown in Figure 6A, the article with highest co-citations (n = 35) was published by INACSL Stand Comm (22) in Clinical Simulation in Nursing in 2016, entitled INACSL Standards of Best Practice: Simulation (SM) Simulation Design. In this work, they provide a standard framework and guideline for developing effective simulation-based experiences. Similarly, CiteSpace citation burst could identify references focused by researchers in a specific period (17, 23). The burst duration was set to 2 years. At last, 20 references with strongest citation bursts were identified in Figure 6B. Among them, Foronda Cynthia, 2014, Nurse Educ Today, V34, P0 (24) has the highest burst strength (n = 6.11), entitled Use of virtual clinical simulation to improve communication skills of baccalaureate nursing students: A pilot study. There are eight articles with citation bursts ending in 2021 which means they were get more attention in recent years. They are “Caylor S, 2015, CLIN SIMUL NURS, V11, P163 (25)”, “Smith PC, 2015, CLIN SIMUL NURS, V11, P52 (26)”, “Shin S, 2015, NURS EDUC TODAY, V35, P176 (27)”, “Irwin P, 2015, J NURS EDUC, V54, P572 (28)”, “Cooper S, 2015, CLIN SIMUL NURS, V11, P97 (29)”, “Rebenitsch L, 2016, VIRTUAL REAL-LONDON, V20, P101 (30)”, “Butt AL, 2018, CLIN SIMUL NURS, V16, P25 (31)”, “Padilha JM, 2018, CLIN SIMUL NURS, V15, P13 (3)”.
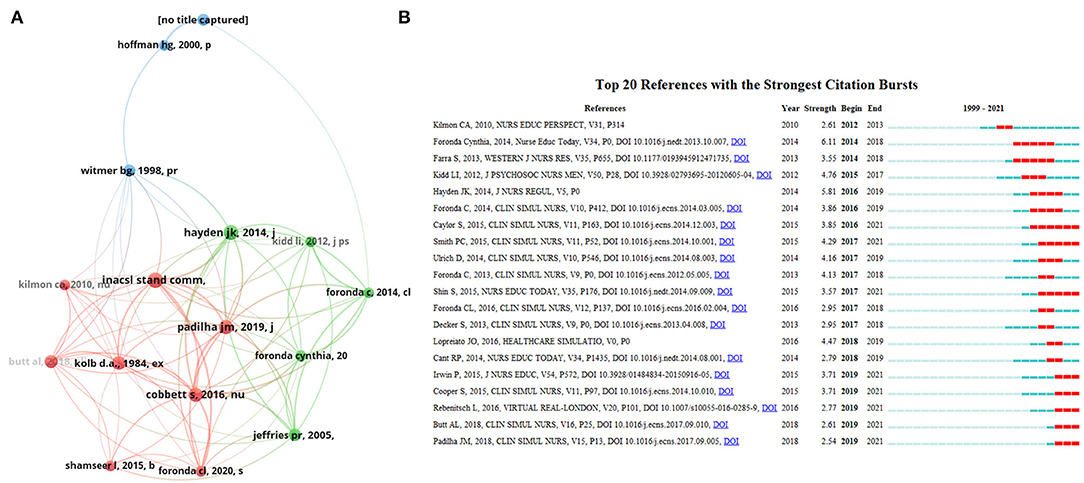
Figure 6. (A) The co-citation network visualization map of references on virtual simulation in nursing field between 1999 and 2021. (B) The top 20 references with the strongest citation bursts on virtual simulation in nursing field between 1999 and 2021. The blue line represented the time from its first appearance to 2021, the red line represented the burst time.
The number of publications in a field reflects the activity and productivity over the years (23). We observed the overall trend of publication in this filed was upward, and could divided into three phases. Before 2008, the number of articles per year slightly increased. It may be restricted by technology such as internet access or computer popularity. Likewise, a previous study found before the year of 2005, the applications of virtual patient in medical education are small (32). Since 2020, the number of papers got a sharp increase to over 200 publications in 2021. We speculate several reasons account for this. First, because of social isolation during the COVID-19 pandemic, it is difficult for students to enter clinical practice. In addition, educators were forced to change the way of program delivery (33). Numerous online programs has emerged during the COVID-19, such as virtual lab environments (34), three-dimensional virtual world (3DVW) (35), personal protective equipment (PPE) virtual simulation games (36). Such VS programs effectively enhanced nursing student interest and provided nurse educators with novel and engaging means of content delivery (33). Second, COVID-19 pandemic accelerated the demand for more nursing staff and higher quality nursing care. Indeed, not all nurses or medical staff have the opportunity to be in the frontline battle with such an pandemic. It is difficult to educate and train these back-ups with any physical touch. However, the greatest strength of VS could provide an almost real environment that simulated any emergency in COVID-19.
Without surprising, the USA leads the VS in nursing research, which requires the collaboration of multiple disciplines, such as medical informatics, education, computer science, and software engineering. Other areas displayed the similar leading position of the USA, such as radiation-induced lung injury (37), and human-computer interaction (38), etc. Interestingly, in terms of the number of productive authors and institutions, Canada ranked ahead of the USA. Extensively studies showed that collaborations tends to be stronger between institutions or countries with shorter geographical distances (15). We speculated the cooperation links between authors and institutions within Canada were stronger than that in the USA. As expected, Supplementary Figure 1 and Figure 4B further corroborated our hypothesis. There are scattered links between numerous American authors and institutions, but relative close relationships between Canadian authors and institutions. Previous study reported studies with regional and international collaborations had a significantly higher mean number of citations than sole local collaborations. In fact, it suggested that collaborations among scholars can lead to improvements in research and contribute to greater clarity and richer insights in a field (39). Considering the scattered collaborations in this field, we hope there will be more inter-institutions and international research in the future.
Key journals, institutions, and authors provide the essential information for a given field. Clinical Simulation in Nursing, Nurse Education Today, and Journal of Nursing Education are the top three productive and co-cited journals. Researchers should continue to pay particular attention on them, because some frontier articles may be published in these journals. In addition, researchers could choose these journals for their draft submission. Institutions like University of Toronto, University of Queensland, University of Washington, and scholars like Verkuyl M, Luctkar-flude M, Tyerman J, Foronda, Cl, and Hoffman, HG should be followed and maybe the potential cooperation partner.
Keyword and reference analysis provides a graphical map of what knowledge existed and how they are interrelated in a given field. It facilitates researchers to get insight into a certain field quickly (18). The major themes generated from VOSviewer keyword co-occurrence characterize the body of knowledge structure of VS in nursing research. Specifically, the top four biggest clusters represent the whole body of this field.
The largest cluster refers to virtual learning in COVID-19 pandemic, which accounts for 23.9% of the total keywords. The primary keywords in this cluster are “nursing student (n = 26), virtual learning (n = 19), and COVID-19 (n = 19), nurse education (n = 14)” Under this cluster, researchers have explored the online virtual learning for nurse students (40–44). Studies showed their positive aspect of virtual learning. That is, virtual learning is essential at the height of the pandemic and may prove useful in other circumstances that limit clinical site availability (45, 46). Digital platforms strengthen the involvement of students (47). Herbert (48) reported their Augmented Reality (AR) app on heart failure for remote training of nursing students. Likewise, they find it could encourage students engagement during the learning process. Shamsaee et al. (49) reported virtual education had significant positive feedback on information-seeking skills and knowledge about search operators in nursing students. However, researchers also point out their worries. Amerson et al. (50) reports up to 94% of nursing students experienced a moderate level of stress in a time of virtual learning. Thus, he reminds the faculty must be attention to the mental health needs of nursing students in virtual learning during COVID-19. Also, another study discussed the negative comments regarding virtual learning from a personal level. It includes internet login and web conferencing logistics, lack of motivation to study, family difficulties, and faculty inexperience teaching in an online environment (8). Therefore, with the advent of widespread use of VS in nursing education, these problems should be fixed and pay more attention to psychological problems on students in the future.
The second largest cluster refers to cure or clinical use for virtual reality. It includes 20.6% keywords of the total. The primary keywords in this cluster are “virtual reality (n = 183), pain (n = 33), anxiety (n = 20), dementia (n = 18), distraction (n = 15).” Under this cluster, researchers focused on its clinical applications. Studies from Nilsson et al. (51) and Gershon et al. (52) showed that VR could effectively relieve the needle-related procedural pain and distress in children and adolescents with cancer diseases. Also, studies reported VR could effectively reduce children's pain and distress during flu vaccinations (53) and burn wound care procedures (54). Apart from the applications for caring for children, older people also benefit from VR programs. Loggia et al. (55) reported the use of VR could help able-bodied older people to achieve physical activity recommendations, even with moderate cognitive impairments. Davis and Ohman (56) and Hannans et al. (57) reported VR could help persons with Alzheimer's disease find their way more effectively, help them maintain independence and enhance their cognitive and affective knowledge. Brimelow et al. (58) reported VR could reduce apathy and improve mood in aged care. Although many benefits may get from VR in older people's nursing, difficulties still exist in dementia older people caring, like less empathy in nurses. Previous studies show VR could enhance nursing students' effectiveness and interest in working with older people (59). Also, Campbell et al. (60) reported using a VR dementia experience system could increase nursing student awareness, knowledge, and sensitivity of Alzheimer's disease. Further exploration is how these VR programs translate into improved care for those older people.
The third-largest cluster related to education in nurse practitioners using VS. It includes 15.2% keywords of the total. The primary keywords in this cluster are ”simulation (n = 108), education (n = 51), learning (n = 16), training (n = 15).“ Under this cluster, researchers focused on clinical education in nurse practitioners. Tsai et al. (61) developed a computer-assisted protocol using VR in performing Port-A catheter inserting. Results suggested it could reduce fear of performing the Port-A catheter technique, significantly reduce error rates and increase correct equipment selection in novice nurses. Samosornet al. (62) developed a VR airway Laboratory to teach difficult airway management skills to nursing students. For cardiopulmonary resuscitation (CPR), researchers explored the effects of VR (63) and AR (64) in training nursing students. Compared with the traditional teaching approach, VR and AR CPR training systems get positive feedback as experienced in a realistic environment. Again, studies report the 3D virtual environment such as 2nd Life laboratory is a good way to practice the students' experience of learning decision-making skills (65–68). Another virtual simulation program is virtual patients. It developed to provide a realistic standard clinical situation to train the ability of nursing students [e.g., clinical reasoning (69–71), communication skills (72–74) situation awareness, and teamwork capability (75)]. However, there are still lingering questions remain to elucidate. Currently, the predominant methods for assessing learning outcomes are combinations of paper-based exams and observations from clinical teachers (76), effective and objective assessment methods related to learning outcomes are still lacking (77–79). Thus, as a promising teaching approach, we call for nurse managers, policymakers, and nurse educators to develop more VS programs to train nursing students and build more reliable and objective assessment methods to validate learning outcomes.
The fourth cluster associated with the education technology for nursing research, which consists of 6.3% keywords of the total. The primary keywords are “nursing (n = 92) and educational technology (n = 24)”. Under this cluster, researchers focused on technologies on VS. The major virtual technologies used in nursing education are VR and AR. VR technologies have three common features: “(1) immersion, (2) perception to be present in an environment, (3) interaction with that environment.” AR technologies have three defining characteristics: “(1) combines real and virtual, (2) interactive in real-time, (3) registered in 3D.” The main difference between VR and AR is that AR merged the real world with virtual experience (80). Different terms [e.g., virtual learning spaces (81); virtual worlds (82); immersive three-dimensional (3D) interactive video program (6)] have been used to refer to VR and AR technologies, and sometimes the distinction between VR and AR is unclear. Thus, there is a call to unify the definition of VR and AR (1). Contrary to being used with VR and AR in education, MR is less used, but recently got concerned. Wunder et al. (83) using an AR headsets to simulate fire in the operating room to train nurse anesthesia students. Although VR, AR, and MR provide a chance to revolutionize nursing education delivery, and promote student-centered learning (84). There are some shared challenges among the three virtual technologies. (1) Faculty and their institutions involved need to be able to invest significant time, money, and resources to successfully develop and launch VS technologies for nursing education. (2) Faculty need to be adequately trained before using VS technology to manage and prevent VR technology difficulties (e.g., poor video and sound quality, poor network connectivity, low fidelity of the virtual experience, or computer problems). (3) End-users for virtual technologies may experience cybersickness or digital motion sickness (e.g., feeling disoriented, dizzy, nauseous, and sore eyes). These issues warrant further research in the future.
First, the papers on virtual simulation in nursing were searched based on the WoSCC. Although WoSCC is recognized as one of the most authoritative databases, PubMed, Scopus, and Google scholar are also widely accepted by scientists. Second, the number of citations and citations per paper are influenced by time and remain controversial as a comprehensive indicator of the quality of one paper or the author. Likewise, the larger number of publications was not the only indicator of influence for the journal, as other indicators (e.g., impact factor, SNIP, CiteScore, SJR) are widely used (85). Third, we included only English papers in this study, several papers with non-English languages were excluded, such as Chinese, Portuguese (n = 8), and Spanish (n = 4). Finally, database updates may result in discrepancies.
This bibliometric analysis identified major contributing authors, institutions, countries, journals and mapped the knowledge network of virtual simulation in nursing research. The research hotspot is gradually shifting from clinical nursing care to studies of nursing education using different virtual simulation technologies. Further research directions are as following: (1) Strengthen the co-operation between authors, institutions, and countries. (2) Reducing psychological problems and physical sickness of end-users. (3) Developing more VS programs to train nursing students and build more reliable and objective assessment methods to validate learning outcomes. (4) Strengthen the training of faculty abilities to VS technology to manage and prevent VS technology difficulties.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
QZ conceived of the study, participated in its design, and drafted the manuscript. JL involved in study design, obtained data and contributed to interpretation, and helped to draft the manuscript. JC provided the theoretical frameworks and performed much of the editing of the manuscript. All authors read and approved the final manuscript.
This study was supported by the Hunan Science and Technology Innovation Platform and Talent Plan (Grant: 2017TP1004).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.890773/full#supplementary-material
Supplementary Figure 1. Author co-operation network and co-cited author network on virtual simulation in nursing research. (A) Co-authorship network visualization map of authors for virtual simulation in nursing field. (B) Co-cited author network visualization map of virtual simulation in nursing field. Node size indicated the number of articles produced. The distance between any two nodes positively associated with the cooperation strength.
WoSCC, Web of Science core collection; VS, virtual simulation; VR, virtual reality; AR, augmented reality; MR, mixed reality; IF, impact factor; CPR, cardiopulmonary resuscitation.
1. Kardong-Edgren S, Farra SL, Alinier G, Young HM. A call to unify definitions of virtual reality. Clin Simul Nurs. (2019) 31:28–34. doi: 10.1016/j.ecns.2019.02.006
2. Kilmon CA, Brown L, Ghosh S, Mikitiuk A. Immersive virtual reality simulations in nursing education. Nurs Educ Perspect. (2010) 31:314–7.
3. Padilha JM, Machado PP, Ribeiro AL, Ramos JL. Clinical virtual simulation in nursing education. Clin Simul Nurs. (2018) 15:13–8. doi: 10.1016/j.ecns.2017.09.005
4. Girao ALA, Dos Santos MNO, Chaves EMC, Gomes EB, de Oliveira SKP, de Carvalho REFL. NurseVR: development of a serious virtual reality game for medication preparation and administration training. Comput Inform Nurs. (2021). doi: 10.1097/CIN.0000000000000820. [Epub ahead of print].
5. Weston J, Zauche LH. Comparison of virtual simulation to clinical practice for prelicensure nursing students in pediatrics. Nurse Educ. (2021) 46:E95–8. doi: 10.1097/NNE.0000000000000946
6. Chao YC, Hu SH, Chiu HY, Huang PH, Tsai HT, Chuang YH. The effects of an immersive 3d interactive video program on improving student nurses' nursing skill competence: A randomized controlled trial study. Nurse Educ Today. (2021) 103:104979. doi: 10.1016/j.nedt.2021.104979
7. Tiffany J, Forneris S. The Forecast for Tech Usage Growth in Nursing Education. (2018). Retrieved from: https://nlnteq.org/2018/02/07/the-forecast-for-tech-usage-and-growth-in-nursing-education-part-4-of-the-series-the-future-of-technology-in-nursing-education/ (accessed February 19, 2019).
8. Fogg N, Wilson C, Trinka M, Campbell R, Thomson A, Merritt L, et al. Transitioning from direct care to virtual clinical experiences during the COVID-19 pandemic. J Prof Nurs. (2020) 36:685–91. doi: 10.1016/j.profnurs.2020.09.012
9. Emich KJ, Kumar S, Lu L, Norder K, Pandey N. Mapping 50 years of small group research through small group research. Small Group Res. (2020) 51:659–99. doi: 10.1177/1046496420934541
10. Donthu N, Kumar S, Mukherjee D, Pandey N, Lim WM. How to conduct a bibliometric analysis: An overview and guidelines. J Bus Res. (2021) 133:285–96. doi: 10.1016/j.jbusres.2021.04.070
11. Cumming DJ, Kumar S, Lim WM, Pandey N. Venture Capital Private Equity Research: A Bibliometric Review Future Research Agenda. (2022). Available online at: https://ssrn.com/abstract=4034812 (accessed January 14, 2022).
12. Kumar S, Sahoo S, Lim WM, Dana L-P. Religion as a social shaping force in entrepreneurship and business: insights from a technology-empowered systematic literature review. Technol Forecast Soc Change. (2022) 175:121393. doi: 10.1016/j.techfore.2021.121393
13. Kumar S, Sharma D, Rao S, Lim W, Mangla S. Past, present, and future of sustainable finance: insights from big data analytics through machine learning of scholarly research. Ann Operat Res. (2022) 1–44. doi: 10.1201/9781003156291
14. Taskaya S, Aksoy A. A bibliometric analysis of workplace incivility in nursing. J Nurs Manag. (2021) 29:518–25. doi: 10.1111/jonm.13161
15. Yanbing S, Hua L, Chao L, Fenglan W, Zhiguang D. The state of nursing research from 2000 to 2019: a global analysis. J Adv Nurs. (2021) 77:162–75. doi: 10.1111/jan.14564
16. Jarden R, Narayanan A, Sandham M, Siegert R, Koziol-McLain J. Bibliometric mapping of intensive care nurses' wellbeing: development and application of the new iAnalysis model. BMC Nurs. (2019) 18:21. doi: 10.1186/s12912-019-0343-1
17. Chen CM. CiteSpace II: Detecting and visualizing emerging trends and transient patterns in scientific literature. J Am Soc Inf Sci Technol. (2006) 57:359–77. doi: 10.1002/asi.20317
18. van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. (2010) 84:523–38. doi: 10.1007/s11192-009-0146-3
19. Liao HC, Tang M, Luo L, Li CY, Chiclana F, Zeng XJ. A bibliometric analysis and visualization of medical big data research. Sustainability. (2018) 10:166. doi: 10.3390/su10010166
20. Dong J, Wei W, Wang C, Fu Y, Li Y, Li J, et al. Research trends and hotspots in caregiver studies: a bibliometric and scientometric analysis of nursing journals. J Adv Nurs. (2020) 76:2955–70. doi: 10.1111/jan.14489
21. Gold JI, Kim SH, Kant AJ, Joseph MH. Rizzo AS. Effectiveness of virtual reality for pediatric pain distraction during iv placement. Cyberpsychol Behav. (2006) 9:207–12. doi: 10.1089/cpb.2006.9.207
22. Comm IS, INACSL. Standards of best practice: simulation (SM) simulation design. Clin Simul Nurs. (2016) 12:S5–12. doi: 10.1016/j.ecns.2016.09.005
23. Chen D, Zhang G, Wang J, Chen S, Wang J, Nie H, et al. Mapping trends in Moyamoya angiopathy research: a 10-year bibliometric and visualization-based analyses of the web of science core collection (WoSCC). Front Neurol. (2021) 12:637310. doi: 10.3389/fneur.2021.637310
24. Foronda C, Gattamorta K, Snowden K, Bauman EB. Use of virtual clinical simulation to improve communication skills of baccalaureate nursing students: a pilot study. Nurse Educ Today. (2014) 34:e53–7. doi: 10.1016/j.nedt.2013.10.007
25. Caylor S, Aebersold M, Lapham J, Carlson E. The use of virtual simulation and a modified TeamSTEPPS (TM) training for multiprofessional education. Clin Simul Nurs. (2015) 11:163–71. doi: 10.1016/j.ecns.2014.12.003
26. Smith PC, Hamilton BK. The effects of virtual reality simulation as a teaching strategy for skills preparation in nursing students. Clin Simul Nurs. (2015) 11:52–8. doi: 10.1016/j.ecns.2014.10.001
27. Shin S, Park J-H, Kim J-H. Effectiveness of patient simulation in nursing education: Meta-analysis. Nurse Educ Today. (2015) 35:176–82. doi: 10.1016/j.nedt.2014.09.009
28. Irwin P, Coutts R. A. systematic review of the experience of using second life in the education of undergraduate nurses. J Nurs Educ. (2015) 54:572–7. doi: 10.3928/01484834-20150916-05
29. Cooper S, Cant R, Bogossian F, Kinsman L, Bucknall T, Team FAR. Patient deterioration education: evaluation of face-to-face simulation and e-simulation approaches. Clin Simul Nurs. (2015) 11:97–105. doi: 10.1016/j.ecns.2014.10.010
30. Rebenitsch L, Owen C. Review on cybersickness in applications and visual displays. Virtual Real. (2016) 20:101–25. doi: 10.1007/s10055-016-0285-9
31. Butt AL, Kardong-Edgren S, Ellertson A. Using game-based virtual reality with haptics for skill acquisition. Clin Simul Nurs. (2018) 16:25–32. doi: 10.1016/j.ecns.2017.09.010
32. Su W-S, Chang C-Y. Virtual patient in interactive learning environments: a review of 1989-2020 publications in selected SSCI journals. Interact Learn Environ. (2021) X:1–7. doi: 10.1080/10494820.2021.1879873
33. Saab MM, Hegarty J, Murphy D, Landers M. Incorporating virtual reality in nurse education: a qualitative study of nursing students' perspectives. Nurse Educ Today. (2021) 105:7. doi: 10.1016/j.nedt.2021.105045
34. Cantey DS, Sampson M, Vaughn J, Blodgett NP. Skills, community, and rapport: prelicensure nursing students in the virtual learning environment. Teach Learn Nurs. (2021) 16:384–8. doi: 10.1016/j.teln.2021.05.010
35. Liaw SY, Choo T, Wu LT, Lim WS, Choo H, Lim SM, et al. Wow, woo, win”- Healthcare students' and facilitators' experiences of interprofessional simulation in three-dimensional virtual world: a qualitative evaluation study. Nurse Educ Today. (2021) 105:6. doi: 10.1016/j.nedt.2021.105018
36. Tyerman J, Luctkar-Flude M, Baker C. Rapid development of a COVID-19 assessment and PPE virtual simulation game. Clin Simul Nurs. (2021) 56:125–32. doi: 10.1016/j.ecns.2021.03.002
37. Wang D, Li Z, Zhang Y, Li Y, Wang X, Wang S, et al. Bibliometric analysis of research relating to radiation-induced lung injury (2001-2020). Ann Palliat Med. (2021) 10:11166–76. doi: 10.21037/apm-21-1682
38. Wang J, Cheng R, Liu M, Liao P. Research trends of human-computer interaction studies in construction hazard recognition: a bibliometric review. Sensors. (2021) 21:6172. doi: 10.3390/s21186172
39. Annalingam A, Damayanthi H, Jayawardena R, Ranasinghe P. Determinants of the citation rate of medical research publications from a developing country. Springerplus. (2014) 3:140. doi: 10.1186/2193-1801-3-140
40. Smith TS, Holland AC, White T, Combs B, Watts P, Moss J, et al. Distance accessible education model: teaching skills to nurse practitioners. J Nurse Pract. (2021) 17:999–1003. doi: 10.1016/j.nurpra.2021.05.018
41. Zwart DP, Goei SL, Noroozi O, Van Luit JEH. The effects of computer-based virtual learning environments on nursing students' mathematical learning in medication processes. Res Pract Technol Enhanc Learn. (2021) 16:4. doi: 10.1186/s41039-021-00147-x
42. Castillo J, Gomar C, Rodriguez E, Trapero M, Gallart A. Cost minimization analysis for basic life support. Resuscitation. (2019) 134:127–32. doi: 10.1016/j.resuscitation.2018.11.008
43. MacRae D, Jara MR, Tyerman J, Luctkar-Flude M. Investing in engagement: integrating virtual learning experiences across an undergraduate nursing program. Clin Simul Nurs. (2021) 52:17–32. doi: 10.1016/j.ecns.2020.12.005
44. Dreifuerst KT, Bradley CS, Johnson BK. Using debriefing for meaningful learning with screen-based simulation. Nurse Educ. (2021) 46:239–44. doi: 10.1097/NNE.0000000000000930
45. Hinic K. Evidence-based virtual learning experiences for the clinical nurse leader capstone. J Nurs Care Qual. (2021) 36:E59–62. doi: 10.1097/NCQ.0000000000000552
46. Shea KL, Rovera EJ. Preparing for the COVID-19 pandemic and its impact on a nursing simulation curriculum. J Nurs Educ. (2021) 60:52–5. doi: 10.3928/01484834-20201217-12
47. Manakatt BM, Carson ZW, Penton RL, Demello AS. Virtual learning experiences in population health nursing course during the COVID-19 pandemic. Int Nurs Rev. (2021) 68:557–62. doi: 10.1111/inr.12725
48. Herbert VM, Perry RJ, LeBlanc CA, Haase KN, Corey RR, Giudice NA, et al. Developing a smartphone app with augmented reality to support virtual learning of nursing students on heart failure. Clin Simul Nurs. (2021) 54:77–85. doi: 10.1016/j.ecns.2021.02.003
49. Shamsaee M, Mangolian Shahrbabaki P, Ahmadian L, Farokhzadian J, Fatehi F. Assessing the effect of virtual education on information literacy competency for evidence-based practice among the undergraduate nursing students. BMC Med Inform Decis Mak. (2021) 21:48. doi: 10.1186/s12911-021-01418-9
50. Amerson R, Fisher B, Bible J, Burgess L, Ravan L, Ward L. Nursing education amid a pandemic: mental health in a time of virtual learning. Nurse Educ. (2021) 46:255–60. doi: 10.1097/NNE.0000000000001039
51. Nilsson S, Finnstrom B, Kokinsky E, Enskar K. The use of virtual reality for needle-related procedural pain and distress in children and adolescents in a paediatric oncology unit. Eur J Oncol Nurs. (2009) 13:102–9. doi: 10.1016/j.ejon.2009.01.003
52. Gershon J, Zimand E, Pickering M, Rothbaum BO, Hodges L A. pilot and feasibility study of virtual reality as a distraction for children with cancer. J Am Acad Child Adolesc Psychiatry. (2004) 43:1243–9. doi: 10.1097/01.chi.0000135621.23145.05
53. Beran TN, Ramirez-Serrano A, Vanderkooi OG, Kuhn S. Reducing children's pain and distress towards flu vaccinations: a novel and effective application of humanoid robotics. Vaccine. (2013) 31:2772–7. doi: 10.1016/j.vaccine.2013.03.056
54. Chan EA, Chung JW, Wong TK, Lien AS, Yang JY. Application of a virtual reality prototype for pain relief of pediatric burn in Taiwan. J Clin Nurs. (2007) 16:786–93. doi: 10.1111/j.1365-2702.2006.01719.x
55. Loggia G, Gauthier A, Lemiere F, Drigny J, Desvergee A, Leconte P, et al. Cycle more with virtual reality: a proof of concept study in an institutionalised able-bodied geriatric population. Age Ageing. (2021) 50:1422–5. doi: 10.1093/ageing/afab040
56. Davis R, Ohman J. Wayfinding in ageing and Alzheimer's disease within a virtual senior residence: study protocol. J Adv Nurs. (2016) 72:1677–88. doi: 10.1111/jan.12945
57. Hannans JA, Nevins CM, Jordan K. See it, hear it, feel it: embodying a patient experience through immersive virtual reality. Inf Learn Sci. (2021) 122:565–83. doi: 10.1108/ILS-10-2020-0233
58. Brimelow RE, Dawe B, Dissanayaka N. Preliminary research: virtual reality in residential aged care to reduce apathy and improve mood. Cyberpsychol Behav Soc Netw. (2020) 23:165–70. doi: 10.1089/cyber.2019.0286
59. Edwards H, Nash R, Sacre S, Courtney M, Abbey J. Development of a virtual learning environment to enhance undergraduate nursing students' effectiveness and interest in working with older people. Nurse Educ Today. (2008) 28:672–9. doi: 10.1016/j.nedt.2007.11.009
60. Campbell D, Lugger S, Sigler GS, Turkelson C. Increasing awareness, sensitivity, and empathy for Alzheimer's dementia patients using simulation. Nurse Educ Today. (2021) 98:104764. doi: 10.1016/j.nedt.2021.104764
61. Tsai SL, Chai SK, Hsieh LF, Lin S, Taur FM, Sung WH, et al. The use of virtual reality computer simulation in learning Port-A cath injection. Adv Health Sci Educ Theory Pract. (2008) 13:71–87. doi: 10.1007/s10459-006-9025-3
62. Samosorn AB, Gilbert GE, Bauman EB, Khine J, McGonigle D. Teaching airway insertion skills to nursing faculty and students using virtual reality: a pilot study. Clin Simul Nurs. (2020) 39:18–26. doi: 10.1016/j.ecns.2019.10.004
63. Keys E, Luctkar-Flude M, Tyerman J, Sears K, Woo K. The integration of virtual simulation gaming into undergraduate nursing resuscitation education: a pilot randomised controlled trial. Clin Simul Nurs. (2021) 54:54–61. doi: 10.1016/j.ecns.2021.01.013
64. Balian S, McGovern SK, Abella BS, Blewer AL, Leary M. Feasibility of an augmented reality cardiopulmonary resuscitation training system for health care providers. Heliyon. (2019) 5:e02205. doi: 10.1016/j.heliyon.2019.e02205
65. Jenson C, Forsyth D. Virtual reality simulation: using three-dimensional technology to teach nursing students. Comp Informat Nurs. (2012) 30:312–8; quiz 319–20. doi: 10.1097/NXN.0b013e31824af6ae
66. McCallum J, Ness V, Price T. Exploring nursing students' decision-making skills whilst in a Second Life clinical simulation laboratory. Nurse Educ Today. (2011) 31:699–704. doi: 10.1016/j.nedt.2010.03.010
67. Wiecha J, Heyden R, Sternthal E, Merialdi M. Learning in a virtual world: experience with using second life for medical education. J Med Internet Res. (2010) 12:e1. doi: 10.2196/jmir.1337
68. Bahrami M, Hadadgar A, Fuladvandi M. Designing virtual patients for education of nursing students in cancer course. Iran J Nurs Midwifery Res. (2021) 26:133–6. doi: 10.4103/ijnmr.IJNMR_327_20
69. Forsberg E, Georg C, Ziegert K, Fors U. Virtual patients for assessment of clinical reasoning in nursing – a pilot study. Nurse Educ Today. (2011) 31:757–62. doi: 10.1016/j.nedt.2010.11.015
70. Forsberg E, Ziegert K, Hult H, Fors U. Clinical reasoning in nursing, a think-aloud study using virtual patients - a base for an innovative assessment. Nurse Educ Today. (2014) 34:538–42. doi: 10.1016/j.nedt.2013.07.010
71. Everett-Thomas R, Joseph L, Trujillo G. Using virtual simulation and electronic health records to assess student nurses' documentation and critical thinking skills. Nurse Educ Today. (2021) 99:104770. doi: 10.1016/j.nedt.2021.104770
72. Shorey S, Ang E, Ng E, Yap J, Lau L, Chui C. Communication skills training using virtual reality: a descriptive qualitative study. Nurse Educ Today. (2020) 94:104592. doi: 10.1016/j.nedt.2020.104592
73. Shorey S, Ang E, Yap J, Ng E, Lau S, Chui C, et al. Virtual counseling application using artificial intelligence for communication skills training in nursing education: development study. J Med Internet Res. (2019) 21:e14658. doi: 10.2196/14658
74. Chapelain P, Morineau T, Gautier C. Effects of communication on the performance of nursing students during the simulation of an emergency situation. J Adv Nurs. (2015) 71:2650–60. doi: 10.1111/jan.12733
75. Peddle M, Mckenna L, Bearman M, Nestel D. Development of non-technical skills through virtual patients for undergraduate nursing students: an exploratory study. Nurse Educ Today. (2019) 73:94–101. doi: 10.1016/j.nedt.2018.11.008
76. Stayt L, Merriman C, Ricketts B, Morton S, Simpson T. Recognizing and managing a deteriorating patient: a randomized controlled trial investigating the effectiveness of clinical simulation in improving clinical performance in undergraduate nursing students. J Adv Nurs. (2015) 71:2563–74. doi: 10.1111/jan.12722
77. Cook DA, Triola MM. Virtual patients: a critical literature review and proposed next steps. Med Educ. (2009) 43:303–11. eng. doi: 10.1111/j.1365-2923.2008.03286.x
78. Ward R, Muckle T, Kremer M, Krogh M. Computer-based case simulations for assessment in health care: a literature review of validity evidence. Eval Health Prof. (2019) 42:82–102. doi: 10.1177/0163278717718609
79. Chen S, Huang T, Liao I, Liu C. Development and validation of the simulation learning effectiveness inventory. J Adv Nurs. (2015) 71:2444–53. doi: 10.1111/jan.12707
80. Mendez KJW, Piasecki RJ, Hudson K, Renda S, Mollenkopf N, Nettles BS, et al. Virtual and agumended reality: implication for the feature on nursing education. Nurse Educ Today. (2020) 93:104531. doi: 10.1016/j.nedt.2020.104531
81. Gdanetz LM, Hamer MK, Thomas E, Tarasenko LM, Horton-Deutsch S, Jones J. Technology, educator intention, and relationships in virtual learning spaces: a qualitative metasynthesis. J Nurs Educ. (2018) 57:197-+. doi: 10.3928/01484834-20180322-02
82. De Gagne JC, Oh J, Kang J, Vorderstrasse AA, Johnson CM. Virtual worlds in nursing education: a synthesis of the literature. J Nurs Educ. (2013) 52:391-+. doi: 10.3928/01484834-20130610-03
83. Wunder L, Gomez NAG, Gonzalez JE, Mitzova-Vladinov G, Cacchione M, Mato J, et al. Fire in the operating room: use of mixed reality simulation with nurse anesthesia students. Informatics. (2020) 7:40. doi: 10.3390/informatics7040040
84. Foronda CL, Alfes CM, Dev P, Kleinheksel AJ, Nelson DA Jr, O'Donnell JM, et al. Virtually nursing: emerging technologies in nursing education. Nurse Educ. (2017) 42:14–7. doi: 10.1097/NNE.0000000000000295
Keywords: virtual simulation, nursing, bibliometric analysis, hot-spots, Citespace, VOSviewer
Citation: Zhang Q, Chen J and Liu J (2022) Global Trends and Hot-Spots in Research on Virtual Simulation in Nursing: A Bibliometric Analysis From 1999 to 2021. Front. Public Health 10:890773. doi: 10.3389/fpubh.2022.890773
Received: 06 March 2022; Accepted: 29 March 2022;
Published: 25 April 2022.
Edited by:
Sunjoo Kang, Yonsei University, South KoreaReviewed by:
Satish Kumar, Malaviya National Institute of Technology, Jaipur, IndiaCopyright © 2022 Zhang, Chen and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jing Liu, bGl1amluZ194eWhsQGNzdS5lZHUuY24=; Jia Chen, aGx4eWNqaWFAY3N1LmVkdS5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.